Abstract
Purpose
To investigate the effect of a prehabilitation program on peri- and post-operative outcomes in adult cervical deformity (CD) surgery.
Methods
Operative CD patients ≥ 18 years with complete baseline (BL) and 2-year (2Y) data were stratified by enrollment in a prehabilitation program beginning in 2019. Patients were stratified as having undergone prehabilitation (Prehab+) or not (Prehab−). Differences in pre and post-op factors were assessed via means comparison analysis. Costs were calculated using PearlDiver database estimates from Medicare pay-scales.
Results
115 patients were included (age: 61 years, 70% female, BMI: 28 kg/m2). Of these patients, 57 (49%) were classified as Prehab+. At baseline, groups were comparable in age, gender, BMI, CCI, and frailty. Surgically, Prehab+ were able to undergo longer procedures (p = 0.017) with equivalent EBL (p = 0.627), and shorter SICU stay (p < 0.001). Post-operatively, Prehab+ patients reported greater reduction in pain scores and greater improvement in quality of life metrics at both 1Y and 2Y than Prehab− patients (all p < 0.05). Prehab+ patients reported significantly less complications overall, as well as less need for reoperation (all p < 0.05).
Conclusion
Introducing prehabilitation protocols in adult cervical deformity surgery may aid in improving patient physiological status, enabling patients to undergo longer surgeries with lessened risk of peri- and post-operative complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adult cervical spinal deformity (ACSD) is a potentially debilitating disorder of multifactorial etiology that can cause severe discomfort and disability, including loss of horizontal gaze and neurologic compromise [1]. The health impact of symptomatic ACSD is substantial, with negative impact across all health-related quality of life metric domains [2]. The mean ACSD EQ-5D index is comparable to the bottom 25th percentile values for blindness/low vision, emphysema, renal failure, and stroke [2].
ACSD surgery has been shown to provide benefits in radiographic alignment and most importantly, clinical outcomes by improving a patient’s disability, pain symptoms, and overall quality of life [3]. Complications following ACSD surgery include dysphagia, distal junctional kyphosis (DJK), respiratory failure, deep wound infections and nerve deficits, with a reported reoperation rate of ~ 17% [4]. Frailty is also more prevalent in the ACSD population compared to the adult spinal deformity (ASD) cohort [5]. As a result, these patients are good candidates to evaluate the utility and success of pre-habilitation protocols and their effect on outcomes.
Pre-habilitation (prehab) in spine surgery has been applied with mixed results. For patients that are eligible to participate, prehab may reduce length of stay, improve post-op recovery and reduce risks of nosocomial infection [6]. The protocols and regimens applied in prehab for spine patients have been varied in the literature with no consensus established [6]. They have included cardiovascular training, resistance training, bone density therapy or cognitive behavioral training (CBT). Protocols continue to evolve and no specific ACSD prehab methodology has been established that has shown improvement in post-operative outcomes. In a recent prospective randomized study, PREPARE, that looked at the effects of pre-surgery physiotherapy on walking ability and lower extremity strength in patients with degenerative spine disorders, the authors found that pre-habilitation increased walking ability and lower extremity strength compared to controls in the pre-operative setting [7]. At 1 year after surgery, prehab accounted for 27.5% of the variation in physical activity level between the prehab and non-prehab group [7]. In an 18-year scoping review of the literature across different databases, including the Cochrane database, results showed that prehabilitation programs are feasible, reduce medical expenditures, and improve patients’ postoperative pain, disability, self-efficacy, psychological behaviors, and satisfaction post-operatively [6, 8].
The available literature suggests there is an opportunity to improve patient experience, clinical outcomes and reduce medical costs with the use of prehabilitation in spine surgery. Although protocols have been investigated in lumbar spine surgery, protocols for cervical deformity patients are lacking. The objective of this study was to assess the effects of prehabilitation on peri and post-operative outcomes in adult cervical deformity surgery.
Materials and methods
Data source and study design
This is a retrospective study of a prospectively collected, single-center database containing adult cervical deformity (CD) patients enrolled between 2012 and 2021. Institutional Review Board (IRB) approval was obtained prior to patient enrollment and all patients provided informed consent. This database has been used for analyses in previously published studies [9,10,11]. Patients enrolled in the database were older than 18 years of age and had a plan to undergo surgical correction for cervical deformity. Cervical deformity was defined radiographically as meeting at least one of the following criteria: C2–C7 sagittal kyphosis > 15°, T1 slope minus cervical lordosis (TS-CL) > 35°, C2–C7 sagittal vertical axis (cSVA) > 40 mm, chin-brow vertical angle (CBVA) > 25°, McGregor’s slope (MGS) > 20°, or segmental cervical kyphosis > 15° across any 3 vertebrae between C2 and T1. The inclusion criteria of the present study required operative cervical deformity patients with complete radiographic and health related quality of life (HRQL) data preoperatively and at 2 years postoperatively.
Data collection and radiographic assessment
Standardized data collection forms assessed patient demographics, surgical parameters, and comorbidities at the initial presentation. Health-related quality of life (HRQL) metrics were collected via patient surveys at baseline and multiple follow-up time points, and included the Neck Disability Index (NDI), Euro-QOL 5-Dimension Questionnaire (EQ5D), and modified Japanese Orthopaedic Association (mJOA) assessment. The minimally clinically important difference (MCID) for the mJOA was set at 2 based on previously reported values [12]. The MCID for Neck Disability Index was set as 15; which is double previously published values because our NDI score was collected on a 0–100 scale as opposed to 0–50) [13]. The EQ-5D MCID was set as 0.1 per previously published values [14, 15].
Lateral spine radiographs were used to assess radiographic parameters at baseline and follow-up intervals. All images were analyzed with SpineView® (ENSAM, Laboratory of Biomechanics, Paris, France) [16,17,18]. Spinopelvic radiographic parameters assessed included pelvic tilt (PT: the angle between the vertical and the line through the sacral midpoint to the center of the two femoral heads), the mismatch between pelvic incidence and lumbar lordosis (PI-LL), and the sagittal vertical axis (SVA: C7 plumb line relative to the posteriosuperior corner of S1). Cervical spine parameters assessed included cervical lordosis (C2-C7 angle), T1 slope (T1S), McGregor’s Slope (MGS), and chin-brow vertical angle (CBVA).
Classification of cervical deformity
Preoperative cervical deformity severity was assessed using the Ames CD classification. This system consists of a cervical deformity descriptor that identifies the apex of the deformity, and five modifiers [19]. Patients were assigned a cervical deformity descriptor based on radiographic review and were stratified by deformity severity for each of the five modifiers.
Cohort selection and comparison
Operative CD patients ≥ 18 years with complete pre-(BL) and up to 2-year (2Y) postop radiographic/HRQL data were stratified by enrollment in a prehabilitation protocol beginning in 2019. Patients were stratified as having underwent prehabilitation (Prehab+), versus those who did not (Prehab−).
All patients presenting with cervical deformity from 2019 and needing surgical correction were offered the prehabilitation program. The final decision as to whether patients were ultimately enrolled into the program was made between the surgeons and the patients depending on the ability of the patient to undergo the full protocol, and also on the acuity of need for surgery based on severity of symptoms/disability. As a result, every patient enrolled in the prehabilitation program was able to fully complete it.
Pre-habilitation protocol
-
1.
Targeted physical therapist-guided strengthening protocol consisting of twice weekly sessions for at least ≥ 3 weeks preoperatively of:
-
Sternocleidomastoid muscle group
-
Trapezius muscle group
-
Levator scapulae muscle group
-
Erector spinae muscle group
-
Deep cervical flexors muscle group
-
Suboccipital muscles muscle group
-
-
2.
Psychological prehabilitation:
-
Psychiatric or psychological evaluation pre-operatively
-
Cognitive behavioral therapy (CBT) 1–2× a week for ≥ 3 weeks preop exploring thoughts and expectations surrounding upcoming surgery and expected postoperative course
-
Pain management consultation pre-operatively
-
-
3.
Nutritional prehabilitation:
-
Preoperative dietetics assessment
-
Individualized dietary modification and supplementation
-
Preoperative bone density assessment via dual energy X-ray absorptiometry and treatment based on T-scores
-
Statistical analysis
Differences in demographics, clinical outcomes, radiographic alignment targets, peri-operative factors and complication rates were assessed via means comparison analysis.
Results
Cohort overview
115 CD pts met inclusion criteria (Mean age 61 years and BMI 28 kg/m2). Of these patients, 57 patients (49%) made up the Prehab+ group. In Figs. 1 and 2, we illustrate examples of patients in either group (Figs. 1 and 2).
Representative of good candidate for prehabilitation. 71 y/o female with past medical history of osteoporosis (receiving 2000 IU calcium daily and denosumab 60 mg injection every 6 months), hypothyroidism, hypertension, chronic kidney disease stage III, asthma and bilateral total knee arthroplasty. She also had no history of smoking or alcohol use and BMI 20 kg/m2. The patient underwent 6 months total of pre-operative prehabilitation. Patient met target goals for pain improvement and suffered no major peri or post-operative events or loss of alignment by 2Y
Representative of candidate not fit for prehabilitation. 69-year old male with past medical history of paroxysmal atrial fibrillation (on apixaban), hypertension, hyperlipidemia, a gastrointestinal glomus tumor s/p en block resection 2 years previously, alcohol abuse, chronic kidney injury, hyponatremia, BMI 24 kg/m2 and asthma. Patient was unable to undergo prehabilitation due to severe frailty and severity of neurological symptoms. He was still experiencing disability at 6 months and was subsequently lost to follow-up
Surgical descriptors
In terms of surgical characteristics, mean levels fused was 5.3 ± 3.3, mean estimated blood loss (EBL) was 733.3 ± 820.5 mL, and mean operative time was 337.7 ± 201.4 min. By surgical approach, 18.1% of patients underwent an anterior-only approach, 49.3% posterior-only, and 31.3% combined. The most common upper instrumented vertebra (UIV) was C3 and most common lower instrumented vertebra (LIV) was T1. 67.4% of patients underwent an osteotomy as part of their index procedure. 9.2% of patients underwent a 3-column osteotomy.
Cervical deformity severity and Ames classification
Preoperatively, Ames modifier breakdown by severity was as follows: For cSVA, 88.1% of the cohort were non-pathologic, while 11.9% had a moderate deformity. By TS-CL, 25.4% of patients had no deformity, 11.6% had moderate deformity, and 63.0% had a severe deformity. Examining the Horizontal Gaze modifier, 21.1% had no deformity, 52.1% moderate deformity, and 26.8% had severe deformity. By SVA, 91.8% of patients were non-pathologic and 8.2% had severe deformity. By myelopathy severity as measured via mJOA, 9.7% of the cohort had no myelopathy, 26.2% mild, 35.0% moderate, and 29.1% had severe myelopathy.
Baseline differences: Prehab+ versus Prehab−
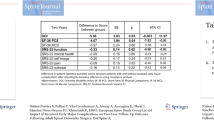
At baseline, groups were comparable in age, gender, BMI, CCI, and frailty. In terms of BL HRQLs, Prehab+ had significantly lower mJOA scores (p = 0.047), but both groups were equivalent in NDI and EQ5D scores (both p > 0.05) [Table 1]. Baseline opioid usage was comparable between both groups prior to prehab enrollment (p = 0.093).
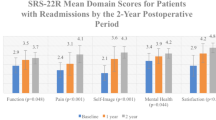
Peri and post-operative differences
Surgically, Prehab+ underwent longer procedures (p = 0.017), but with equivalent EBL (p = 0.627), shorter length of stay, and lower intensive care unit admission rates (p < 0.001) [Table 2]. Post-operatively, Prehab+ patients reported greater reduction in neck pain overall, and consistently better HRQL metrics at 1 and 2-year follow up (all p < 0.05). In terms of complications, Prehab+ patients reported significantly less post-operative complications overall, such as decreased pulmonary complications, as well as less need for reoperation compared to Prehab− patients.
Discussion
Recent research has indicated that patient activity level prior to spine surgery can be an important predictor of postoperative complications and outcomes [20]. Studies in other surgical fields have demonstrated that for suitable patients, prehab may reduce the length of stay, improve post-op recovery, reduce complications and improve patient satisfaction [19]. However, the prehabilitation protocols in spinal fusion surgery are highly varied, making any conclusive evidence difficult to interpret and, therefore, are not always part of protocols aimed at enhancing recovery after surgery [21]. There is paucity in the literature investigating whether prehabillitation in spine fusion surgery decreases costs and improves functional outcomes. To our knowledge, no literature exists concerning prehabilitation protocols in adult spinal deformity surgery let alone cervical spine deformity. The goal of this study was to utilize a single-center approach to better assess the effects of prehabilitation on peri- and post-operative outcomes in adult cervical deformity surgery.
A general template for a prehab program involves a warm-up, cardiovascular component, resistance exercises and functional training rehabilitation [22]. Cognitive behavioral therapy (CBT) to help handle the stresses of surgery and postop expectations has also been adopted into prehabilitation programs. Rolving et al. compared the effects of a standard pre- and post-op treatment regimen versus an additional six CBT sessions for lumbar spine surgery candidates, and found that there was a statistically significant difference in Oswestry disability index (ODI) scores between both groups at 3 and 6 months in favor of the CBT group; but with similar scores at 1 year post-op [23]. Rolving and colleagues in a subsequent study performed an economic evaluation alongside their CBT randomized study to establish the cost effectiveness of pre and post-op CBT, with the primary outcome measure as Quality-Adjusted Life Years (QALY) based on EQ-5D scores and showed a significant difference of 0.071 QALY in favor of the CBT group [23, 24]. Nielsen et al. conducted a prehabilitation study on 60 patients undergoing lumbar spine surgery that included pre-physical therapy, smoking/alcohol cessation education, and dietary supplementation. They were able to demonstrate that the prehab cohort had a mean 2-day shorter hospital stay compared to the control group [25]. The patients in this study did not undergo spine deformity procedures, unlike in our study.
The use of a multi-faceted prehabilitation program in our study resulted in the prehab cohort being able to undergo longer surgeries with equivalent estimated blood loss (EBL) and still had a statistically significant (p < 0.001) shorter length of stay (3 days less in the Prehab+ group). The prehab group also had significantly (p < 0.05) less complications and need for reoperation compared to the prehab− negative group. This included any, major, or minor complications in the perioperative and postoperative setting. There was no statistically significant difference in the degree of deformity based on radiographic analysis, or in the baseline HRQL scores between the two groups pre-op. Complications in adult cervical spine deformity surgery can be high, with one study by Smith et al. reporting at least 1 complication in 56% of 133 patients at one-year post-op who underwent anterior only, posterior only and combined procedures [4]. Patient selection in spine deformity surgery plays a vital role in decreasing the overall rate of complications in the short and long term. Studies have shown that pre-operative screening programs have been able to decrease the rate of major complications in spine surgery [26]. Functional status prior to spine surgery also influences the likelihood of complications in the peri-operative and post-operative time frame. [27]
One of the primary goals of a pre-habilitation program such as the one instituted in our study is to improve function leading into surgery mainly from a physical component but also psychologically through CBT. The only statistically significant baseline difference between the groups in our study was seen in the mJOA score between the two groups. The mJOA score may have contributed to the ability or inability for patients to participate in the physical therapy component of the prehab program and therefore certain patients with a greater degree of myelopathy were unable to take part in the prehab program. Further studies would need to be performed to determine what benefit from baseline these patients would still potentially experience if they were able to fully complete the full prehab program.
According to Flexman et al., approximately 4% of the spine population is deemed frail [5]. Cervical deformity patients are reported to have even higher baseline frailty than complex thoracolumbar patients [28]. One variable that accounts for this high frailty is malnutrition. Lack of proper nutritional status impacts tissue/bone healing and increases risk of infection in the post-operative setting. Therefore, we included nutritional therapy as part of the prehab program in our study that included bone density therapy. Nutritional deficiency in deformity patients is higher compared to the degenerative spine surgery population [29, 30], and has been associated with increased rates of peri-operative complications [29]. Studies published in other surgical specialties have demonstrated the positive benefits of nutritional intervention including: increasing ambulatory function, decreased complications, alleviated weight gain or weight loss, shortened the hospital stay, improved self-reported health, improved cost-effectiveness, and reduced readmission rates. [31, 32]
A limitation in spine surgery prehab programs seeking to show the benefits of incorporating physical therapy (PT) before surgery, is lack of standardization and oversight by trained professionals. The strength of this study relative to that by Nielsen et al. for example [25], was that all the patients enrolled in the prehab cohort were able to finish their PT prior to surgery and there was a zero-attrition rate. In addition, the prehab PT program was standardized and monitored by trained physical therapists.
We acknowledge limitations to the present study. This was a retrospective, single center database analysis without randomization. Selection into the two respective groups was based on the primary operating surgeon’s evaluation. Therefore, this could have led to selection bias affecting the end results. Future studies where enrollment is randomized from the beginning across multiple sites will need to be performed to avoid selection bias and avoid specific study site bias that can influence final results. We did not perform a cost analysis in this study due to institutional limitations restricting access to the complete cost data needed. Future studies will need an expanded analysis of all the financial costs from the time of entry to the time of exit in the study. Furthermore, longer follow-up time frame to gain a more accurate depiction of costs to the health care system will be needed to help distinguish the benefits in the prehabilitation group. Also, sub-analyses were not performed to help establish which component of the prehab program had a greater impact on the statistically significant results. Future studies will be needed to establish this and thereby help formulate a standardized, optimal prehab program for cervical spine deformity patients. Previous studies have focused on patients undergoing general spine procedures, however, this is the first study of its kind that analyzed the effect of prehabilitation in the ACSD population undergoing surgery.
Conclusion
This study demonstrates that introducing prehabilitation protocols in adult cervical deformity surgery may aid in improving patient physiological status, enabling patients to undergo longer surgeries with lessened risk of peri- and post-operative complications. Though cost-effectiveness of such programs should be further assessed, prehabilitation should be considered for eligible patients to assist in optimizing recovery and reducing complications and reoperations.
References
Scheer JK, Lau D, Ames CP (2021) Sagittal balance of the cervical spine. J Orthop Surg. https://doi.org/10.1177/23094990211024454
Smith JS, Line B, Bess S et al (2017) The health impact of adult cervical deformity in patients presenting for surgical treatment: comparison to united states population norms and chronic disease states based on the EuroQuol-5 dimensions questionnaire. Neurosurgery 80(5):716–725. https://doi.org/10.1093/neuros/nyx028
Elias E, Bess S, Line BG et al (2022) Operative treatment outcomes for adult cervical deformity: a prospective multicenter assessment with mean 3-year follow-up. J Neurosurg Spine 37(6):855–864. https://doi.org/10.3171/2022.6.Spine22422
Smith JS, Buell TJ, Shaffrey CI et al (2020) Prospective multicenter assessment of complication rates associated with adult cervical deformity surgery in 133 patients with minimum 1-year follow-up. J Neurosurg Spine. https://doi.org/10.3171/2020.4.Spine20213
Flexman AM, Charest-Morin R, Stobart L et al (2016) Frailty and postoperative outcomes in patients undergoing surgery for degenerative spine disease. Spine J 16(11):1315–1323. https://doi.org/10.1016/j.spinee.2016.06.017
Gometz A, Maislen D, Youtz C et al (2018) The effectiveness of prehabilitation (prehab) in both functional and economic outcomes following spinal surgery: a systematic review. Cureus 10(5):e2675. https://doi.org/10.7759/cureus.2675
Fors M, Enthoven P, Abbott A et al (2019) Effects of pre-surgery physiotherapy on walking ability and lower extremity strength in patients with degenerative lumbar spine disorder: secondary outcomes of the PREPARE randomised controlled trial. BMC Musculoskelet Disord 20(1):468. https://doi.org/10.1186/s12891-019-2850-3
Eubanks JE, Carlesso C, Sundaram M et al (2023) Prehabilitation for spine surgery: a scoping review. PM R J Injury Funct Rehabil 15(10):1335–1350. https://doi.org/10.1002/pmrj.12956
Passias PG, Williamson TK, Pierce KE et al (2023) The importance of incorporating proportional alignment in adult cervical deformity corrections relative to regional and global alignment: steps toward development of a cervical-specific score. Spine (Phila Pa 1976). https://doi.org/10.1097/brs.0000000000004843
Passias PG, Tretiakov PS, Smith JS et al (2023) Are we improving in the optimization of surgery for high-risk adult cervical spine deformity patients over time? J Neurosurg Spine. https://doi.org/10.3171/2023.5.Spine23457
Tretiakov PS, Budis E, Dave P et al (2023) Does the presence of cervical deformity in patients with baseline mild myelopathy increase operative urgency in adult cervical spinal surgery? A retrospective analysis. Neurosurg Focus 55(3):E9. https://doi.org/10.3171/2023.6.Focus23304
Tetreault L, Kopjar B, Côté P et al (2015) A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of an international prospective multicenter data set of 757 subjects. J Bone Jt Surg Am 97(24):2038–2046. https://doi.org/10.2106/jbjs.O.00189
Carreon LY, Glassman SD, Campbell MJ et al (2010) Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 10(6):469–474. https://doi.org/10.1016/j.spinee.2010.02.007
Le QA, Doctor JN, Zoellner LA et al (2013) Minimal clinically important differences for the EQ-5D and QWB-SA in Post-traumatic Stress Disorder (PTSD): results from a Doubly Randomized Preference Trial (DRPT). Health Quali Life Outcomes 11:59. https://doi.org/10.1186/1477-7525-11-59
Parker SL, Adogwa O, Paul AR et al (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604. https://doi.org/10.3171/2010.12.Spine10472
Champain S, Benchikh K, Nogier A et al (2006) Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J 15(6):982–991. https://doi.org/10.1007/s00586-005-0927-1
Rillardon L, Levassor N, Guigui P et al (2003) Validation of a tool to measure pelvic and spinal parameters of sagittal balance [Validation d’un outil de mesure des paramètres pelviens et rachidiens de l’équilibre sagittal du rachis]. Rev Chir Orthop Reparatrice Appar Mot 89(3):218–227
O’Brien MF KT, Blanke KM, Lenke LG (2022) Spinal Deformity Study Group radiographic measurement manual. Medtronic Sofamor Danek USA, Inc. https://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual.pdf?sfvrsn=2&sfvrsn=2. Accessed 4 Jan 2022
Santa Mina D, Clarke H, Ritvo P et al (2014) Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy 100(3):196–207. https://doi.org/10.1016/j.physio.2013.08.008
Raad M, Neuman BJ, Jain A et al (2018) The use of patient-reported preoperative activity levels as a stratification tool for short-term and long-term outcomes in patients with adult spinal deformity. J Neurosurg Spine 29(1):68–74. https://doi.org/10.3171/2017.10.Spine17830
Debono B, Wainwright TW, Wang MY et al (2021) Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J 21(5):729–752. https://doi.org/10.1016/j.spinee.2021.01.001
Cabilan CJ, Hines S, Munday J (2015) The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. JBI Database Syst Rev Implement Rep 13(1):146–187. https://doi.org/10.11124/jbisrir-2015-1885
Rolving N, Nielsen CV, Christensen FB et al (2015) Does a preoperative cognitive-behavioral intervention affect disability, pain behavior, pain, and return to work the first year after lumbar spinal fusion surgery? Spine (Phila Pa 1976) 40(9):593–600. https://doi.org/10.1097/brs.0000000000000843
Rolving N, Sogaard R, Nielsen CV et al (2016) Preoperative cognitive-behavioral patient education versus standard care for lumbar spinal fusion patients: economic evaluation alongside a randomized controlled trial. Spine (Phila Pa 1976) 41(1):18–25. https://doi.org/10.1097/brs.0000000000001254
Nielsen PR, Jørgensen LD, Dahl B et al (2010) Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil 24(2):137–148. https://doi.org/10.1177/0269215509347432
Maitra S, Mikhail C, Cho SK et al (2020) Preoperative maximization to reduce complications in spinal surgery. Glob Spine J 10(1 Suppl):45s–52s. https://doi.org/10.1177/2192568219882349
Minhas SV, Mazmudar AS, Patel AA (2017) Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Jt J 99-B(6):824–828. https://doi.org/10.1302/0301-620x.99b6.Bjj-2016-1149.R1
Smith JS, Kelly MP, Buell TJ et al (2023) Adult cervical deformity patients have higher baseline frailty, disability, and comorbidities compared with complex adult thoracolumbar deformity patients: a comparative cohort study of 616 patients. Glob Spine J. https://doi.org/10.1177/21925682231214059
Oe S, Yamato Y, Hasegawa T et al (2020) Association between a prognostic nutritional index less than 50 and the risk of medical complications after adult spinal deformity surgery. J Neurosurg Spine. https://doi.org/10.3171/2020.1.Spine191410
Oe S, Watanabe J, Akai T et al (2022) The effect of preoperative nutritional intervention for adult spinal deformity patients. Spine (Phila Pa 1976) 47(5):387–395. https://doi.org/10.1097/brs.0000000000004227
Gillis C, Loiselle SE, Fiore JF Jr et al (2016) Prehabilitation with whey protein supplementation on perioperative functional exercise capacity in patients undergoing colorectal resection for cancer: a pilot double-blinded randomized placebo-controlled trial. J Acad Nutr Diet 116(5):802–812. https://doi.org/10.1016/j.jand.2015.06.007
Smedley F, Bowling T, James M et al (2004) Randomized clinical trial of the effects of preoperative and postoperative oral nutritional supplements on clinical course and cost of care. Br J Surg 91(8):983–990. https://doi.org/10.1002/bjs.4578
Funding
None to disclose.
Author information
Authors and Affiliations
Contributions
Pawel P. Jankowski, Peter S. Tretiakov, Oluwatobi O. Onafowokan, Ankita Das, Bailey Imbo, Oscar Krol, Rachel Joujon-Roche, Tyler Williamson, Pooja Dave, Jamshaid Mir, Stephane Owusu-Sarpong, Peter G. Passias: Active involvement in drafting and critical revision of manuscript, Provided final approval of version to be published, Study Design, Data Acquisition, Analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
None to disclose. Disclosures unrelated to current work: Peter G Passias: Cerapedics: Other financial or material support. Cervical Scoliosis Research Society: Research support. Globus Medical: Paid presenter or speaker. Medtronic: Paid consultant. Royal Biologics: Paid consultant. Spine: Editorial or governing board. Spinevision: Other financial or material support. SpineWave: Paid consultant. Terumo: Paid consultant.
Ethical approval
Institutional review board approval was gained prior to commencement of the study.
Informed consent
Gained from all patients prior to enrolment in study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jankowski, P.P., Tretiakov, P.S., Onafowokan, O.O. et al. Assessing the effects of prehabilitation protocols on post-operative outcomes in adult cervical deformity surgery: does early optimization lead to optimal clinical outcomes?. Spine Deform 12, 1107–1113 (2024). https://doi.org/10.1007/s43390-024-00845-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-024-00845-8