Abstract
Background
Unplanned readmissions and reoperations are known to be associated with undesirable costs and potentially inferior outcomes in complex adult spinal deformity (ASD) surgery. A paucity of literature exists on the impact of readmissions/reoperations on patient-reported outcomes (PRO) in this population.
Methods
Consecutively treated adult patients who underwent complex ASD surgery at a single institution from 2015–2018 and minimum 2-year follow-up were studied. Demographics/comorbidities, operative factors, inpatient complications, and postoperative clinical and patient-reported outcomes (SRS-22r, ODI) were assessed for those with and without readmission/reoperation.
Results
175 patients (72% female, mean age 52.6 ± 16.4) were included. Mean total instrumented/fused levels was 13.3 ± 4.1, range 6–25. The readmission and reoperation rates were 16.6% and 12%, respectively. The two most common causes of reoperation were pseudarthrosis (5.1%) and PJK (4.0%). Predictors for readmission within 2 years following surgery included pulmonary, cardiac, depression and gastrointestinal comorbidities, along with performance of a VCR, and TLIF. At 2 years postoperatively, those who required a readmission/reoperation had significant increases in SRS and reductions in ODI compared to 1-year and preoperative values. Inpatient complications did not negatively impact 2-year PRO’s. The 2-year MCID in PROs was not significantly different between those with and without readmission/reoperation.
Conclusion
Complex ASD surgery carries risk, but the vast majority can achieve MCID (SRS-86.4%, ODI-68.2%) in PROs by 2 years. Importantly, even those with inpatient complications and those who required unplanned readmission/reoperation can improve PROs by 2-year follow-up compared to preoperative baseline and 1-year follow-up and achieve similar improvements compared to those who did not require a readmission.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Improving clinical outcomes and reducing excessive costs are especially relevant in providing value-based care for complex adult spinal deformity (ASD) patients. According to current literature, complications after ASD surgery are frequent in the early (24–36%) and late (11–15%) postoperative settings [1]. These include medical and surgery-related complications (pseudarthrosis, proximal junctional kyphosis (PJK), wound complications, DVT/PE, infection, pneumonia, ileus) often resulting in costly readmissions which may be avoidable [2,3,4,5,6,7]. This has led to a number of studies investigating risk factors for unplanned readmissions, but much of this data is limited by a lack of spine-specific factors and rigorous complication data, single-surgeon data, and short-term follow-up periods [8,9,10,11,12].
In recent decades, there has been a growing focus on patient-reported outcomes (PROs) in ASD patients [13]. A multicenter database study found that ASD operative candidates scored lower in every domain of the Short Form-36 Health-Survey compared to other chronic conditions (arthritis, chronic lung disease, diabetes, and congestive heart failure) [14]. Although it is well known that surgery can significantly reduce disability, pain, and improve overall quality of life compared to nonoperative management, the impact of unplanned readmissions and reoperations on PROs in the complex ASD population remains unclear [15,16,17,18,19,20,21,22].
Compared to prior literature, our study focuses on complex ASD surgical patients and evaluates the clinical data and PROs with a minimum 2-year postoperative follow-up. The purpose of this study was to assess the impact of readmissions and reoperations on PROs. In addition, we sought to provide an in-depth analysis on underlying reasons and risk factors for readmissions occurring anytime in the first 2 years following surgery.
Materials and methods
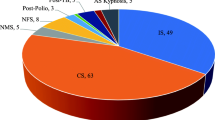
In this study, we retrospectively reviewed a prospectively accrued data set of a consecutive group of complex ASD (≥ 18 years) surgeries performed between 2015 and 2018. These patients were treated by three experienced spinal deformity surgeons at a single-institution. “Complex ASD” cases had a primary or revision diagnosis of ASD and underwent ≥ 6-level fusion surgery with either posterior column osteotomy (PCO), pedicle subtraction osteotomy (PSO), vertebral column resection (VCR), pelvic fixation, and/or interbody fusion (e.g., TLIF). Common diagnoses included adult idiopathic scoliosis, degenerative lumbar scoliosis, congenital spine deformity, kyphoscoliosis, fixed sagittal imbalance, fixed coronal imbalance, flat back deformity, neuromuscular scoliosis, and Scheuermann’s kyphosis (Table 1). Patients were excluded if they had a diagnosis of spinal trauma, active infection, and spinal tumor. The minimum follow-up was 2 years after the index hospital discharge date. This study was approved by the institutional review board at Columbia University Medical Center.
Demographics included sex, age, American Society of Anesthesiologists grade (ASA), and Body Mass Index (BMI, kg/m2). Medical comorbidities included cardiac (myocardial infarction, hypertension, hyperlipidemia, coronary artery disease), pulmonary (asthma, chronic obstruction pulmonary disease, obstructive sleep apnea, prior pneumonia), gastrointestinal (GI) (gastroesophageal reflux disease/GERD, peptic ulcer disease, ulcerative colitis, celiac disease), osteoporosis/osteopenia, diabetes, hypothyroidism, anemia, depression, history of deep vein thrombosis/pulmonary embolism (DVT/PE), and history of cancer (non-spine tumor). Operative variables included total instrumented levels (TIL), pelvic fixation, osteotomy type (PCO, PSO, VCR), anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), transforaminal lumbar interbody fusion (TLIF), estimated blood loss (EBL), operative/anesthesia durations, and prior spine surgery.
Intraoperative/postoperative complications, which occurred during the same inpatient stay, included intraoperative dural tear, intraoperative motor/sensory loss, GI (ileus, nausea/vomiting), cardiac (cardiac/respiratory arrest, lower extremity edema, hypovolemic shock, pericardial effusion), pulmonary (respiratory distress/failure, pneumonia, pleural effusion), DVT/PE, hyponatremia, neurologic (motor deficit), infection (skin, urinary tract infection), acute kidney injury, and postoperative red blood cell transfusion.
Any readmission/reoperation within 2 years after the index hospital date of discharge was assessed. Reasons for readmission were reviewed carefully in each chart review by an orthopedic surgeon independent of the primary treatment team. χ2/Fisher’s exact test and t-tests/ANOVA were used for categorical and continuous variables, respectively. To determine the independent predictors for the outcomes of interest, stepwise multivariate logistic regression analysis was used. Statistical significance was defined as p value < 0.05. The C-statistic and Hosmer–Lemeshow (HL) value were used to measure concordance and goodness-of-fit for the final models. SAS Studio Version 3.4 (SAS Institute Inc, Cary, NC) was used for all statistical analyses.
PROs that included both the Scoliosis Research Society-22R (SRS-22R) and the Oswestry Disability Index (ODI) were recorded in both the preoperative and up to the 2-year postoperative period. For those with readmissions, the most recent PRO data were taken after the readmission discharge date. Several prior studies have demonstrated that both the SRS-22R and the ODI are reliable, valid, and responsive to change in patients undergoing adult spinal deformity surgery [23,24,25]. There are various proposed methods to calculate the minimum clinically important difference (MCID) for PRO’s. In this study, we used a difference of 0.5 times the standard deviation, which has been used in prior literature and known to be equivalent to 1-standard error of measurement for a reliability of 0.75 [26, 27].
Source of funding
No source of funding was provided for this study.
Results
A total 175 consecutive patients met inclusion criteria. The mean follow-up ± standard deviation was 2.5 ± 0.5 years (range 2–3.8 years). Percent follow-up for the 2-year postoperative period was 71.3%. The mean age was 52.6 ± 16.4 years and 72% were female. The two most common preoperative diagnoses included adult idiopathic scoliosis (51.4%) and fixed sagittal imbalance (42.3%) (Table 1). 40.6% had a prior spine surgery. The mean TIL was 13.3 ± 4.1 (range 6–25), with the majority of patients having pelvic fixation (76.6%), PCOs (84.6%, mean 5.4/patient), and TLIF (69.1%, mean 1.4/patient). A smaller number of patients had a 3-column osteotomy (3CO) [13.7% VCR (8.0%; mean 1.5/patient), PSO (5.7%; mean 1.0/patient)] and ALIF/OLIF (2.3%; mean 1.5/patient). Overall mean operative time was 473 ± 137 min with mean EBL of 1324 (24.6%) ± 822 mL (16.4%) (Table 2).
The 2-year readmission and reoperation rates were 16.6% and 12.0%, respectively (Table 3). The median number of days after index discharge date resulting in a readmission and reoperation were 173 days (range 6–716) and 227 days (range 16–716), respectively. Eight patients who were readmitted did not require a reoperation. These readmissions without reoperation were due to headache from a dural tear (1.7%), muscle spasms (0.6%), abdominal pain (0.6%), and poorly controlled pain (1.7%). Reoperations were due to pseudarthrosis (5.1%), PJK (4.0%), wound complication (2.3%), upper and/or lower extremity weakness (2.3%), prominence over incision (1.1%), postoperative fall (1.1%), radiculopathy (0.6%) (Table 4). For the two patients with prominence over incision, the wound closure was well healed; however, both had prominent spinous processes causing localized pain requiring excision.
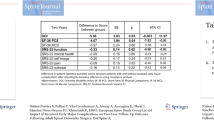
In the multivariate analysis for 2-year readmissions, GI comorbidity (OR: 12.6, 95%CI 3.1–50.7), TLIF (OR: 10.1, 95%CI 2.0–50.6), VCR (OR: 8.8, 95%CI 1.7–44.6), pulmonary comorbidity (OR: 5.4, 95%CI 1.7–17.1), depression (OR: 4.4, 95%CI 1.4–13.8), and cardiac comorbidity (OR: 3.3, 95%CI 1.2–9.2) were independent risk factors and demonstrated good model performance (C-statistic = 0.88; HL = 0.1). Of note, 82.4% of the GI complications were in patients with a history of GERD, and 85.3% of the pulmonary comorbidities were in patients with asthma/COPD. Prior spinal surgery increased readmission risk by 2.5-fold, but was not statistically significant (p = 0.097). Although age, PSO, operative time, postoperative transfusion, and postoperative inpatient neurologic complications were significant in the bivariate analysis, they were not statistically significant factors in the multivariate analysis (Tables 5, 6).
Inpatient complications (intraoperative and postoperative) were assessed to determine potential differences in PROs in those with and without complications (Table 7). Patients with “any” inpatient complication had worse ODI scores at baseline and at 1-year postoperative. However, no significant differences were seen by 2 years postoperative. For SRS, no significant differences were seen at baseline, 1 year, and 2 years postoperative for either any inpatient complications, intraoperative complications, or inpatient-postoperative complications. 2 patients required revision surgery for lower extremity pain/weakness, but neither sustained permanent neurologic deficit. The 2-year MCID PROs (SRS and ODI) were not significantly different between those with and without inpatient complications (Table 8).
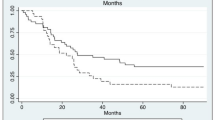
2 years after the index surgery, 86.4% and 68.2% of all patients reached MCID for SRS and ODI, respectively. At 1-year follow-up, patients who did not require a readmission had significantly better PROs compared to preoperative values (baseline PRO: SRS 59.9, ODI 33.4; 1-year PRO: SRS 85.9, ODI 18.0; p < 0.001) as well as those who required either a readmission (1-year SRS 78.5, p < 0.001; 1-year ODI 20.3; p < 0.001) or reoperation (1-year SRS 71; p < 0.001; 1-year ODI 23.8; p < 0.001) (Table 9). At 2 years postoperative, those who required a readmission had significant increases in SRS and reductions in ODI (2-year: SRS 90.6, ODI 15.5) compared to 1-year (SRS 78.5, ODI 20.3; p < 0.001) and preoperative values (SRS 60.1, ODI 44.9; p < 0.001). A similar significant difference was seen for revised patients as well (2-year Revised: SRS 90.9, ODI 13.4; 1-year Revised: SRS 71, ODI 23.8; p < 0.001; Baseline: SRS 56.6, ODI 45.6; p < 0.001). At 2 years postoperative, a substantial number of readmitted patients achieved MCID for SRS (100%) and ODI (83.3%). The same was seen for revised cases: MCID SRS 100%; ODI 85.7%. For those without readmission/reoperation, MCID was achieved in 83.4% for SRS and 64.9% for ODI. No statistically significant differences between those with and without readmission/reoperation were observed for 2-year PRO’s: SRS (readmission: 90.6 vs. non-readmission: 87.4; p = 0.586) or ODI (readmission: 15.5 vs. 16.9; p = 0.834) | SRS (reoperation: 90.9 vs. non-reoperation: 87.4; p = 0.585) or ODI (reoperation: 13.4 vs. non-reoperation: 16.9; p = 0.583).
Significant improvements occurred in each SRS domain score, but the largest changes occurred in the pain and self-image domains. Similarly, the largest significant changes for ODI occurred in pain, standing, sleeping, and traveling domains (Figs. 1, 2). By 2 years postoperative, patients who experienced a transient complication versus a permanent complication had a significantly higher total SRS score (89.2 vs. 67.7; p = 0.016), higher MCID percentage (85.7% vs. 67.7%; p < 0.001), and a higher ODI MCID (66.7% vs. 15.4%; p = 0.001) (Table 10).
The findings of this study may be best represented by patient-AB, a 69-year-old female with severe thoracolumbar posttraumatic osteoporotic kyphosis (> 100°) (Fig. 3). Medical comorbidities included depression, osteoporosis, and GERD. Preoperatively, she suffered from severe back pain and difficulty breathing and eating because of her severe kyphotic posture. Her preoperative SRS/ODI was 69/40. Surgery involved posterior spinal instrumented fusion from T1-sacrum/ilium, multiple PCOs (8), T11 VCR, and L5-S1 TLIF, with an EBL of 800 mL, and operative time of 545mins(Fig. 3). Her hospital course was complicated by pleural effusion and acute blood loss anemia requiring blood transfusion, and a 9-day LOS. Post-discharge, she otherwise did well, until 2 years postoperative when she complained of new onset lower back pain with X-rays demonstrating rod fractures at L4-5(Fig. 4). She was readmitted to undergo revision instrumentation from L1-pelvis with repair of the L4-5 pseudarthrosis (Fig. 4). At the most recent follow-up visit (2 years after revision surgery), she was doing very well without major issues. Her postoperative SRS/ODI scores after revision at latest follow-up were 100/18, respectively.
Discussion
ASD is an increasingly common condition that is known to cause substantial pain and disability. Corrective surgery can improve health-related quality of life (HRQoL) outcomes; however, complications still occur requiring unplanned readmissions. Several large multicenter studies have reported on ASD outcomes, but there remains a paucity of literature on the impact of postoperative complications on PROs [28,29,30]. Furthermore, ASD patients are often defined by > 2 spinal fusion levels and/or radiographic parameters [6, 8, 31,32,33]. Within these cohorts, patients may undergo a range of procedures with more complex ones [e.g., extended fusions (≥ 6), 3COs] at greater risk for significant complications. The purpose of this study was to examine the impact of reoperation/readmission on HRQoL for complex ASD patients defined as those who had a minimum 6-level spinal fusion. We hypothesized that patients who experienced treatable postoperative medical or surgical complications would show significant improvement in HRQoL by 2 years despite the need for readmission/reoperation.
Based on our single-institutional analysis, the overall 2-year readmission (16.6%) and reoperation (12%) rates were relatively low given the surgical complexity involved [34]. The majority of reoperations were for pseudarthrosis (5.1%) and PJK (4%). By 2 years postoperative, the majority of patients reached MCID for SRS (86.4%) and ODI (68.2%). Patients who did not require a readmission had significantly higher PROs compared to preoperative values and to those who required a readmission or reoperation at 1-year follow-up. Those who required a readmission had significant increases in SRS and reductions in ODI at 2 years compared to 1-year and preoperative baseline values. For readmitted patients, the main drivers for improvement in the SRS-22r from 1 to 2 years were the pain (+ 1.0; p < 0.001) and the self-image (+ 0.7; p < 0.001) domains. In regards to the ODI scores, the main drivers of change from 1 to 2 years were pain (− 0.5; p = − 0.022), standing (− 0.7; p = 001), and sleeping (− 0.5; p = 0.026). The magnitude of the change appears small, but a single point can mean the difference between someone who could stand “as long as I want with extra pain” versus “pain prevents me from standing for more than 1 h.” Finally, TLIF was also found to be associated with readmission in the multivariate analysis (OR: 10.1, 95%CI 2.0–50.6). This could potentially be explained by the significantly higher rate of intraoperative complications associated with TLIFs (TLIF: 35.5% vs. No TLIF: 20.4%, p = 0.045) and specifically intraoperative durotomies (TLIF: 28.9 vs. No TLIF: 11.1, p = 0.01). Although there were higher rates for pseudarthrosis (8.3 vs 7.4, p = 0.847), postop extremity weakness (2.5 vs. 1.9, p = 0.798), pain requiring readmission (4.1 vs. 3.7, p = 0.894), wound complications (2.5% vs. 1.9, p = 0.798), and implant failure (5.0 vs. 3.7, p = 0.714), these were not statistically significant. Nearly every TLIF was performed with pelvic fixation (94.2%). Those with TLIF and pelvic fixation had a lower rate of pseudarthrosis (8.8% vs. 15%; p = 0.385) and higher rate of PJK (6.1% vs. 0%; p = 0.499) than those with pelvic fixation alone. However, these differences were also not statistically significant.
Few prior studies directly examined the impact of complications on PROs in the complex ASD population, and the results are somewhat conflicting. In a single-center retrospective study, Riley et al. [35] examined HRQoL in complex ASD patients based on Scoli-RISK-1 (SR-1) criteria with minimum 2-year follow-up. Their ASD population was considerably more complex given that nearly 40% of patients underwent a 3CO and 23.4% of patients suffered a major complication. Nevertheless, significant improvements were observed in all SRS-22r domains, and more than 50% achieved MCID by 2 years postoperative. Similar to our study, the greatest improvements occurred in SRS pain and self-image domains. However, patients with postoperative neurological deficit or a major complication were unlikely to achieve MCID for the SRS function domain. It is possible that patients with permanent complications are less likely to experience substantial improvements in HRQoL. Auerbach et al. [36] studied outcomes in patients who underwent 3COs for ASD and showed that patients with permanent major complications seemed to have lower mean satisfaction rates, but the difference was not statistically different from those with transient complications. By 2 years, patients who experienced major complications were still able to achieve satisfactory clinical outcomes. In contrast, Glassman et al. demonstrated that major complications negatively impact PROs for ASD patients compared to those with only minor or no complications. This study was limited to a 1-year postoperative follow-up, which may not be sufficient time to account for potentially recoverable complications [37]. In our study, we found that those with “any inpatient” complication had worse ODI at 1 year, but the differences were not significant at 2 years. Furthermore, the 2-year MCID% was not significantly different between those with and without “any inpatient” complication, “intraoperative” complication, and “inpatient postoperative” complication for either SRS or ODI. These prior studies provide valuable information, but did not examine the impact of revision surgery or readmission on PROs.
In a prospective multicenter study, Passias et al. [34] reviewed the readmission and reoperation data in an ASD population defined by radiographic parameters. They reported a 22.8% readmission rate and 19.5% reoperation rate. Similar to our findings, a major reason for revision surgery was implant failure. HRQoL analysis revealed an overall improvement in the total population but less improvement in those who were readmitted. Undergoing reoperation following readmission did not have any impact on HRQoL. In our analysis, patients who required either a reoperation or readmission achieved significantly better PROs at 2 years compared to 1 year and baseline values. When comparing 2-year PROs for those readmitted versus not, there was no statistical difference for either SRS or ODI.
The fact that readmitted and revised patients were able to recover as well as those without readmission is likely attributed, at least in part, to the high-volume nature of our spine-focused hospital and aggressive attention for any complication requiring readmission and/or reoperation. Fluid communication between the surgeons and their staff, ancillary subspecialty teams, and the patient can lead to prompt and effective management of complications and overall improved patient outcomes.
A number of limitations must be acknowledged for this study. First, although this was a retrospective review, all of the data was prospectively entered into a standardized electronic database on a continual basis and all patients were consecutively enrolled. Unfortunately, nearly 30% of patients were lost to follow-up by 2 years postoperative. Those without follow-up had a similar preoperative comorbidity burden (ASA > 2: 29.1% [with follow-up] vs. 26.4% [without follow-up]; p = 0.663) and baseline operative characteristics (TIL: 13.3 [with follow-up] vs. 13.7 [without follow-up]; p = 0.418; operative time: 473 min [with follow-up] vs. 461 min [without follow-up]; p = 0.504; PSO: 5.7% [with follow-up] vs. 5.6% [without follow-up]; p = 0.961; VCR: 8% [with follow-up] vs. 9.7% [without follow-up]; p = 0.659; TLIF: 69.1% [with follow-up] vs. 66.7% [without follow-up]; p = 0.643). Nevertheless, it is possible with lack of follow-up that we underestimated the true readmission/reoperation rates and overestimated the benefit of surgery based on PRO’s. Next, given the single-center nature of our study, our findings may not be generalizable to other institutions who treat ASD patients. Finally, complications including pseudarthrosis and PJK are known to occur beyond the 2-year follow-up period. Studies with extended follow-up periods are needed to understand the full extent of long-term complications.
Conclusion
Our results demonstrate that the vast majority of patients can achieve clinically significant improvement in HRQoL after complex ASD surgery. Major improvements were observed in every domain of the SRS survey and several domains of the ODI survey (pain, standing, sleeping, social life, and traveling). Several predictors were identified for unplanned readmissions which may help surgeons with preoperative risk-stratification. Furthermore, and somewhat surprisingly, our findings suggest that readmissions and revision surgery do not adversely affect PRO’s in complex ASD patients by 2 years postoperative. Those who require an unplanned readmission or reoperation can significantly improve their HRQoL by 2-year follow-up compared to preoperative-baseline and 1-year follow-up as well as achieve similar improvements compared to those who did not require a readmission. These findings can provide valuable insight for patients and providers during the shared decision-making process for these complex surgical cases.
References
Zanirato A, Damilano M, Formica M, Piazzolla A, Lovi A, Villafane JH, Berjano P (2018) Complications in adult spine deformity surgery: a systematic review of the recent literature with reporting of aggregated incidences. Eur Spine J 27(9):2272–2284
How NE, Street JT, Dvorak MF, Fisher CG, Kwon BK, Paquette S, Smith JS, Shaffrey CI, Ailon T (2019) Pseudarthrosis in adult and pediatric spinal deformity surgery: a systematic review of the literature and meta-analysis of incidence, characteristics, and risk factors. Neurosurg Rev 42(2):319–336
Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ (2017) Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine 14(4):126–132
Sebaaly A, Gehrchen M, Silvestre C, Kharrat K, Bari TJ, Kreichati G, Rizkallah M, Roussouly P (2019) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 29:904–913
Lee NJ, Shin JI, Kothari P, Kim JS, Leven DM, Steinberger J, Guzman JZ, Skovrlj B, Caridi JM, Cho SK (2017) Incidence, impact, and risk factors for 30-day wound complications following elective adult spinal deformity surgery. Global Spine J 7(5):417–424
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, Gupta MC, Deviren V, Schwab FJ, Lafage V (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 41(22):1718–1723
McCarthy IM, Hostin RA, Ames CP, Kim HJ, Smith JS, Boachie-Adjei O, Schwab FJ, Klineberg EO, Shaffrey CI, Gupta MC, Polly DW (2014) Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J 14(10):2326–2333
Elsamadicy AA, Adogwa O, Vuong VD, Sergesketter A, Reddy G, Cheng J, Bagley CA, Karikari IO (2017) Impact of alcohol use on 30-day complication and readmission rates after elective spinal fusion (>/=2 levels) for adult spine deformity: a single institutional study of 1,010 patients. J Spine Surg 3(3):403–410
Elsamadicy AA, Camara-Quintana J, Kundishora AJ, Lee M, Freedman IG, Long A, Qureshi T, Laurans M, Tomak P, Karikari IO (2019) Reduced impact of obesity on short-term surgical outcomes, patient-reported pain scores, and 30-day readmission rates after complex spinal fusion (>/=7 levels) for adult deformity correction. World Neurosurg 127:e108–e113
De la Garza Ramos R, Nakhla J, Echt M, Gelfand Y, Scoco AN, Kinon MD, Yassari R (2018) Risk factors for 30-day readmissions and reoperations after 3-column osteotomy for spinal deformity. Global Spine J 8(5):483–489
Phan K, Kim JS, Capua JD, Lee NJ, Kothari P, Dowdell J, Overley SC, Guzman JZ, Cho SK (2017) Impact of operation time on 30-day complications after adult spinal deformity surgery. Global Spine J 7(7):664–671
Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM (2016) Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J 16(7):862–866
Algattas H, Cohen J, Agarwal N, Hamilton DK (2017) Trends in the use of patient-reported outcome instruments in neurosurgical adult thoracolumbar deformity and degenerative disease literature. J Craniovertebr Junction Spine 8(2):103–107
Pellise F, Vila-Casademunt A, Ferrer M, Domingo-Sabat M, Bago J, Perez-Grueso FJ, Alanay A, Mannion AF, Acaroglu E (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24(1):3–11
Bridwell KH, Baldus C, Berven S, Edwards C 2nd, Glassman S, Hamill C, Horton W, Lenke LG, Ondra S, Schwab F, Shaffrey C, Wootten D (2010) Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976) 35(20):1849–1854
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 34(20):2171–2178
Liu S, Schwab F, Smith JS, Klineberg E, Ames CP, Mundis G, Hostin R, Kebaish K, Deviren V, Gupta M, Boachie-Adjei O, Hart RA, Bess S, Lafage V (2014) Likelihood of reaching minimal clinically important difference in adult spinal deformity: a comparison of operative and nonoperative treatment. Ochsner J 14(1):67–77
Smith JS, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, O’Brien M, Boachie-Adjei O, Akbarnia BA, Mundis GM, Errico T, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Sciubba D, Ailon T, Fu KM, Kelly MP, Zebala L, Line B, Klineberg E, Gupta M, Deviren V, Hart R, Burton D, Bess S, Ames CP (2016) Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 78(6):851–861
Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK, Protopsaltis T, Klineberg E, Gupta M, Hostin R, Fu KM, Mundis GM Jr, Kim HJ, Deviren V, Soroceanu A, Hart RA, Burton DC, Bess S, Ames CP (2015) Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine 23(3):349–359
Scheer JK, Smith JS, Clark AJ, Lafage V, Kim HJ, Rolston JD, Eastlack R, Hart RA, Protopsaltis TS, Kelly MP, Kebaish K, Gupta M, Klineberg E, Hostin R, Shaffrey CI, Schwab F, Ames CP (2015) Comprehensive study of back and leg pain improvements after adult spinal deformity surgery: analysis of 421 patients with 2-year follow-up and of the impact of the surgery on treatment satisfaction. J Neurosurg Spine 22(5):540–553
Teles AR, Mattei TA, Righesso O, Falavigna A (2017) Effectiveness of operative and nonoperative care for adult spinal deformity: systematic review of the literature. Global Spine J 7(2):170–178
Yanik EL, Kelly MP, Lurie JD, Baldus CR, Shaffrey CI, Schwab FJ, Bess S, Lenke LG, LaBore A, Bridwell KH (2020) Effect modifiers for patient-reported outcomes in operatively and nonoperatively treated patients with adult symptomatic lumbar scoliosis: a combined analysis of randomized and observational cohorts. J Neurosurg Spine 33:1–10
Arima H, Glassman SD, Bridwell K, Yamato Y, Yagi M, Watanabe K, Matsumoto M, Inami S, Taneichi H, Matsuyama Y, Carreon LY (2020) Reaching minimal clinically important difference in adult spinal deformity surgery: a comparison of patients from North America and Japan. J Neurosurg Spine 32:1–6
Repo JP, Ponkilainen VT, Hakkinen AH, Ylinen J, Bergman P, Kyrola K (2019) Assessment of Construct Validity of the Oswestry Disability Index and the Scoliosis Research Society-30 Questionnaire (SRS-30) in Patients With Degenerative Spinal Disease. Spine Deform 7(6):929–936
Baldus C, Bridwell KH, Harrast J, Edwards C 2nd, Glassman S, Horton W, Lenke LG, Lowe T, Mardjetko S, Ondra S, Schwab F, Shaffrey C (2008) Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: are all SRS domains disease specific? Spine (Phila Pa 1976) 33(20):2214–2218
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41(5):582–592
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7(5):541–546
Smith JS, Klineberg E, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, Mundis GM Jr, Errico TJ, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Soroceanu A, Kelly MP, Line B, Gupta M, Deviren V, Hart R, Burton DC, Bess S, Ames CP (2016) Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 25(1):1–14
Smith JS, Shaffrey CI, Klineberg E, Lafage V, Schwab F, Lafage R, Kim HJ, Hostin R, Mundis GM Jr, Gupta M, Liabaud B, Scheer JK, Diebo BG, Protopsaltis TS, Kelly MP, Deviren V, Hart R, Burton D, Bess S, Ames CP (2017) Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 27(4):444–457
Fakurnejad S, Scheer JK, Lafage V, Smith JS, Deviren V, Hostin R, Mundis GM Jr, Burton DC, Klineberg E, Gupta M, Kebaish K, Shaffrey CI, Bess S, Schwab F, Ames CP (2015) The likelihood of reaching minimum clinically important difference and substantial clinical benefit at 2 years following a 3-column osteotomy: analysis of 140 patients. J Neurosurg Spine 23(3):340–348
Faldini C, Di Martino A, Borghi R, Perna F, Toscano A, Traina F (2015) Long vs. short fusions for adult lumbar degenerative scoliosis: does balance matters? Eur Spine J 24(Suppl 7):887–892
Elsamadicy AA, Adogwa O, Sergesketter A, Vuong VD, Lydon E, Behrens S, Cheng J, Bagley CA, Karikari IO (2017) Reduced impact of smoking status on 30-day complication and readmission rates after elective spinal fusion (>/=3 levels) for adult spine deformity: a single institutional study of 839 patients. World Neurosurg 107:233–238
Elsamadicy AA, Adogwa O, Behrens S, Sergesketter A, Chen A, Mehta AI, Vasquez RA, Cheng J, Bagley CA, Karikari IO (2017) Impact of surgical approach on complication rates after elective spinal fusion (>/=3 levels) for adult spine deformity. J Spine Surg 3(1):31–37
Passias PG, Klineberg EO, Jalai CM, Worley N, Poorman GW, Line B, Oh C, Burton DC, Kim HJ, Sciubba DM, Hamilton DK, Ames CP, Smith JS, Shaffrey CI, Lafage V, Bess S (2016) Hospital readmission within 2 years following adult thoracolumbar spinal deformity surgery: prevalence, predictors, and effect on patient-derived outcome measures. Spine (Phila Pa 1976) 41(17):1355–1364
Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP (2018) Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine 28(2):194–200
Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, Crawford CH 3rd, O’Shaughnessy BA, Buchowski JM, Chang MS, Zebala LP, Sides BA (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37(14):1198–1210
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32(24):2764–2770
Funding
There was no financial support for this research project.
Author information
Authors and Affiliations
Contributions
NL and MC: substantial contributions to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work, drafting the work and revising it critically for important intellectual content, final approval of the version to be published, contributed effort to the study; EL and ZS: substantial contributions to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work, revising the work critically for important intellectual content, final approval of the version to be published, contributed effort to the study; RAL and LGL: substantial contributions to the conception and design of the work, revising the work critically for important intellectual content, final approval of the version to be published, contributed cases or effort to the study.
Corresponding author
Ethics declarations
Conflict of interest
LGL reports being a consultant for Medtronic (money donated to charity); receiving royalties from Medtronic and Quality Medical Publishing; receiving reimbursement for airfare and hotels from Broadwater, the Seattle Science Foundation, Stryker Spine, the Spinal Research Foundation, AOSpine, and the Scoliosis Research Society; receiving grant support from the Scoliosis Research Society (money to his institution), EOS Imaging (money to his institution), the Setting Scoliosis Straight Foundation (money to his institution); and receiving grant and fellowship support from AOSpine (money to his institution). Authors RAL/ZMS/EL/NJL/MC report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, N.J., Cerpa, M., Leung, E. et al. Do readmissions and reoperations adversely affect patient-reported outcomes following complex adult spinal deformity surgery at a minimum 2 years postoperative?. Spine Deform 9, 789–801 (2021). https://doi.org/10.1007/s43390-020-00235-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00235-w