Abstract
Purpose
Pedicles on the concave side of the proximal thoracic (PT) curve in adolescent idiopathic scoliosis (AIS) patients with Lenke II and IV deformities tend to be narrow and dysplastic, making pedicle screw (PS) insertion challenging. The aim of this study was to evaluate the feasibility for PS placement in these patients using pedicle chord length, diameter, and channel morphology.
Methods
In this retrospective study, 56 consecutive AIS patients with Lenke II or IV curves who underwent instrumented posterior spinal fusion (PSF) were studied. The mean age at surgery was 14.8 years and the mean PT curve measured 45°. Two independent investigators evaluated all visible pedicles from T1 to T6 vertebral levels using axial images from intraoperative computed tomography-guided navigation recording the pedicle: (1) maximum transverse diameter ‘d’ at the isthmus, (2) maximum chord length ‘l’, and (3) qualitative assessment of the channel morphology (types A–D).
Results
Two hundred and sixty-eight concave and 264 convex pedicles were measured. The mean ‘d’ of the concave pedicles at T3 and T4 was < 3.0 mm, compared to > 5.0 mm for the convex counterparts (p < 0.001). Of all concave pedicle channels, 48% had morphology characteristics that were riskier for PS cannulation (type C or D) compared to 2% of all convex pedicle channels (type A or B) (p < 0.001).
Conclusion
Almost half of all concave pedicles have morphologic characteristics that make them too small to accommodate a PS. Though PSs could be inserted using an in–out–in technique in these patients, alternative fixation anchors may improve strength and safety.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Instrumented posterior spinal fusion (PSF) with pedicle screw (PS) fixation has been widely adopted as the preferred treatment for correcting spinal deformity in adolescent idiopathic scoliosis (AIS) [1]. PSs provide rigid, three-column fixation, imparting superior pull-out strength, and result in better curve correction compared to alternative anchors [2]. Most commercially available instrumentation systems for AIS have pedicle screws with diameters ranging from 4.35 to 7.5 mm.
AIS is classified by the system described by Lenke et al. [3] into six curve patterns in an attempt to guide surgical decision-making. Curve patterns II and IV are characterized by structural proximal thoracic (PT) curves that are typically included in the surgical construct to prevent PT curve progression and postoperative shoulder imbalance [4,5,6]. PT concave-sided pedicles are commonly narrow and dysplastic, while those on the convex side are wider and shorter [7, 8]. This remodeling is attributed to mechanical forces and other factors related to the developing deformity. Although PSs offer many advantages over hook and wires, a PS breech can damage neurologic structures medially, and thoracic or abdominal structures laterally or anteriorly [9,10,11,12,13,14]. While the overall accuracy of PS placement is relatively high, so is the per-patient rate of misplacement [15]. In addition, the misplacement rate is around 33% when pedicle diameter is < 5 mm [16], a common scenario found in structural PT curves. As compared to instrumentation of the thoracolumbar spine in pediatric scoliosis patients, screw placement in the PT spine has a higher risk for misplacement [17].
The feasibility of safe pedicle screw insertion can be evaluated on preoperative computed tomography (CT) or magnetic resonance imaging (MRI) studies. Additionally, intraoperative CT-guided navigation is a powerful tool to improve the safety of pedicle screw insertion in spine deformities [18,19,20,21]. Its use decreases the rate of severely misplaced screws and unplanned returns to the operating room [22]. Given the value of pedicle screw fixation, the need to include the PT curve in most Lenke II and IV curves, and the known risk of placing screws in narrow pedicles, our objective was to evaluate the feasibility for safe PS placement on the concave and convex sides of the PT curve using (1) pedicle chord length; (2) maximum transverse diameter; and (3) qualitative channel morphology.
Methods
Patient selection
We retrospectively evaluated a consecutive series of AIS patients treated with PSF from 2009 to 2020. Patients were included if they had a diagnosis of AIS, underwent PSF with an upper instrumented vertebra (UIV) of T2 or proximal, and had intraoperative CT-guided navigation with axial images available for review. Any patients who did not have a structural PT curve (Lenke II or IV) or were older than 21 years at the time of surgery were excluded. The final cohort consisted of 56 patients (38 females; 18 males) with a total of 672 pedicles (T1–T6) that potentially could be considered for screw fixation.
Data collection
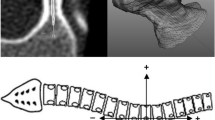
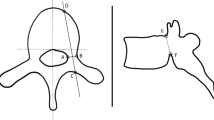
Preoperative clinic notes, imaging, and operative reports were examined to determine the PT curve magnitude, age at surgery, and levels fused. Demographic and preoperative information is presented in Table 1. The mean age at surgery was 14.8 years (11.2–20.1 years) and the mean Cobb angle of the PT curve was 45° (range, 30°–62°). The mean Cobb angle of the main thoracic curve was 61° (range, 50°–112°). Of the 672 eligible pedicles, 532 (268 concave and 264 convex) were visible on the intraoperative axial CT images. No multiplanar reconstruction was used in this study. All visible pedicles were measured independently by two investigators in the embedded PACS software (Intellispace PACS, Philips, Amsterdam, The Netherlands). Each set of measurements was performed using the axial slice in which the visualized pedicle was the widest. The following measurements or assessments were made for each pedicle (Figs. 1, 2):
-
(i)
Length ‘l’ of the pedicle from the posterior to anterior cortex of the vertebra along the longitudinal axis of the pedicle (i.e., chord length).
-
(ii)
Transverse diameter ‘d’ of the pedicle at its narrowest part (i.e., isthmus).
-
(iii)
Qualitative evaluation of pedicles by categorizing them into one of the following four types [23]:
-
Type A: Adequate cancellous channel.
-
Type B: Narrow cancellous channel.
-
Type C: Cortical channel.
-
Type D: No pedicle channel.
-
Statistical analysis
Each pedicle measurement was averaged between raters. These individual pedicle measurement averages were summarized using descriptive statistics. The distribution of concave measurements at each vertebral level was compared to their convex counterparts using independent sample t tests after confirming that the data were normally distributed. The proportions of concave and convex channel morphology types at each vertebral level were compared using χ2 tests. A χ2 test was also used to compare the proportion of pedicles < 4.0 mm on each side of the curve. Two-tail significance was considered at α = 0.05 for all analyses.
Interobserver reliability for pedicle diameter and length was calculated using the intraclass correlation coefficient (ICC) based on a two-way random effects model for absolute agreement. Interobserver reliability for pedicle morphology was calculated using the kappa statistic. ICC or kappa values of < 0.00, 0.00–020, 0.21–0.40, 0.41–0.60, 0.61–0.80, and > 0.80 were used to indicate no, slight, fair, moderate, substantial, and almost perfect agreement, respectively [24]. All statistical analyses were performed using Excel 2016 (Microsoft Corporation, Redmond, WA) and SPSS version 27 (IBM Corp., Armonk, NY).
Results
Measurements
The average pedicle chord length ‘l’ increased with descending vertebra on both the concave and convex sides of the PT curve (Table 2; Fig. 3A). The average concave pedicle ‘l’ increased from 29.0 mm at T1 to 38.4 mm at T6 compared to the convex side which increased similarly from 29.7 to 36.6 mm. The ‘l’ of the concave T4–T6 pedicles was larger than their convex counterparts (p < 0.05 at all three levels). However, the average concave and convex ‘l’ at each level from T4 to T6 was between 35.0 and 40.0 mm. Thus, the maximum length of a PS that could be inserted using standard trajectory in the PT curve was identical on both the concave and convex sides of the curve: 25 mm intraosseous at T1, 30 mm intraosseous at T2 and T3, and 35 mm intraosseous at T4–T6.
The average transverse diameter ‘d’ of the T3 and T4 concave pedicles were both < 3.0 mm, compared to their convex counterparts, which were ≥ 5.0 mm (p < 0.001 at both levels) (Table 2; Fig. 3B). In total, 67% of all T1–T6 concave pedicles were < 4.0 mm versus 17% on the convex side (p < 0.001).
Morphology
The proportion of concave and convex pedicles that could theoretically accommodate a commercially available PS within the channel at each PT vertebral level are depicted in Table 2 and Fig. 4. Among all pedicles, 48% of the concave pedicle channels had a morphology that would not accommodate intraosseous placement of the smallest diameter screw available (type C or D) compared to only 2% of all convex pedicles (p < 0.001). The pedicle with the highest proportion of type C or D channels was the concave pedicle of the T4 vertebra (87%; p < 0.001 as compared to its convex counterpart).
Interobserver reliability
The interobserver agreement for chord length, transverse diameter, and pedicle morphology was substantial (ICC = 0.70; 95% confidence interval [CI] 0.64–0.76), almost perfect (ICC = 0.85; 95% CI 0.82–0.87), and substantial (kappa = 0.76; 95% CI 0.72–0.80), respectively.
Discussion
More than 20 years into the PS fixation era for deformity correction in AIS, the value of screw fixation is widely appreciated. Today, attention is primarily focused on increasing the safety of PS insertion in the distorted anatomy that spine deformity surgeons routinely encounter. As we show in this study, the narrow concave pedicles of the PT curve in Lenke II and IV spinal deformities are high risk for pedicle screw fixation. With the spinal cord resting against the medial wall of the concave pedicle [25] and vital thoracic structures at risk with anterior and lateral penetration, the stakes are particularly high for screw instrumentation in PT curves. The narrow pedicles of the PT curve have been shown to have some of the highest rates of critical medial and anterior perforation [26, 27]. The esophagus is at risk of injury in a PT curve with a positive T1 tilt when inserting a PS on the concavity [28]. In a PT curve with neutral or negative T1 tilt, the trachea is at risk while cannulating a concave pedicle and the esophagus is at risk on the convexity [12, 28]. The left subclavian artery is also at risk with excessively long PS use in the PT left pedicles of Lenke II patients [14]. Additionally, pedicle breech and poor osseous fixation will negatively impact the amount of force that can be imparted during correction maneuvers. The patient-specific detail afforded by image-guided navigation can optimize patient safety.
Ideal screw placement would be a screw that is entirely intraosseous inserted during the first attempt. PS selection and use should be influenced mainly by the maximum transverse diameter of the pedicle at its isthmus and the maximum length along its longitudinal axis (i.e., the chord length). Previous studies note that PS insertion to at least 80% of the chord length provides sufficient strength for most implants [29, 30]. However, the pedicle diameter is the critical factor that dictates the placement technique and screw size used. Screws with a larger diameter have better pull-out strength, increasing the rigidity of the construct [31]. We found at least 67% of concave pedicles and 17% of convex PT pedicles in Lenke II and IV curve patterns to be smaller (< 4.0 mm) than the smallest diameter screw available (4.35 mm). PS insertion techniques can create 1–2 mm of plastic deformation of the pedicle channel during screw insertion [8]. Therefore, some narrower native pedicles can safely accept a slightly larger diameter screw. Here, we show the average transverse diameter of the concave T3 and T4 pedicles to be < 3.0 mm, risking breech even when taking advantage of the plastic deformation phenomenon. In accordance with this study, a recent study by Lee et al. [32] showed the widest average endosteal transverse diameter on both the concave and convex sides of the structural PT curves from T1 to T4 to be no more than 4.0 mm. The PT spine also seems to commonly lack sufficient size for PS cannulation in adults. In a series of 18 human cadavers age 62–83 years, McLain et al. [7] observed that a high proportion of pedicles, including 61% of T4 pedicles, 67% of T5 pedicles, and 75% of T6 pedicles, had a minimum transverse diameter of < 5.5 mm, thus making transpedicular PS instrumentation riskier.
The pedicle screws in the PT spine can be inserted either by anatomical trajectory or at a trajectory that parallels the superior endplate of the vertebra. The latter has additional pull-out strength with better screw purchase based on biomechanical data [9]. Alternatively, an “in–out–in” technique can be employed, wherein there is an intentional lateral breech of the screw with re-entry into the vertebral body through its dorsolateral cortex [33]. Though an in–out–in insertional technique minimizes the risk of a medial wall breech and neurologic insult, injury to the sympathetic trunk remains a possibility [34]. This technique is also associated with reduced pull-out strength compared to PSs placed using an anatomical trajectory [35].
Pedicle channel morphology was first described by Watanabe et al. in 2014 [23]. They rank ordered four types of channels. Pedicles with an adequate cancellous channel (type A) or narrow cancellous channel (type B) could have a pedicle probe inserted and screw placed with low risk for breech or perforation. Pedicle channels with a cortical channel (type C) or no channel (type D) were riskier for attempting pedicle probe insertion and may require specialized insertion techniques, such as channel expansion by malleting a pedicle probe or using a small high-speed drill. When planning a construct for patients with pedicle channel types C or D, options include use of the “in–out–in” technique, skipping small pedicles, or using alternative anchors to minimize the risk of devastating injury. We found 48% of concave-sided pedicles of the PT curve, including 87% of the T4 pedicles, to have channel morphology type C or D, compared to only 2% of all convex-sided pedicles. This finding emphasizes the need for surgeons to proceed with caution or consider alternate fixation strategies on the concave side of the PT curve, especially at the T3–T5 levels.
The morphology of PT spine (T1–T6) and thoracic pedicles has been extensively studied using cadavers and imaging (i.e., plain radiographs, CT, magnetic resonance imaging, and three-dimensional fluoroscopy) [36,37,38]. Striking differences have been observed in the dimensions between males versus females and Caucasians versus Asians [39,40,41]. As confirmed by our findings, the concave-sided T3, T4, and T5 pedicle have proven to be some of the narrowest. This has been shown to be especially true among Asians [42, 43].
This study has some limitations. We relied on intraoperative CT-guided axial images to study pedicle channels and thus were limited only to the pedicles captured with this technique. As a result, data reported for the T1 and T2 vertebral levels may be underpowered as they were not included in all of the CT spins despite T1 or T2 UIVs. In addition, the intraoperative axial images may not fully represent the information provided by real-time multiplanar imaging used to guide surgeons during PSF because the image data saved in the PACS does not optimize the gantry angle. Nonetheless, the intraoperative axial CT images offer the best available representation of the imaging used by surgeons in real-time. Lastly, systemic measurement bias may have been introduced when raters made measurements on different computer monitors with varying resolution. However, the interobserver reliability analysis showed substantial to almost perfect agreement across all measurements, so this is unlikely.
In summary, while pedicle screw instrumentation offers excellent fixation strength and deformity correction, the PT component of Lenke II and IV curves present anatomic challenges. Pedicles are narrower than the smallest available screw diameter in the majority of concave pedicles and in 17% of the convex pedicles. Pedicle channel morphology leads to higher risk PS insertion in 48% of the concave PT pedicles, including 87% of the pedicles on the concave side of T4. Alternate instrumentation type, instrumentation placement techniques, and/or deformity correction strategies in this area can reduce this risk of breech and injury to the spinal cord or other adjacent anatomic structures. Further comparative studies are needed to determine the optimal strategy to maximize pull-out strength, deformity correction and safety in the PT spine of AIS patients with Lenke II and IV curves.
References
de Kleuver M, Lewis SJ, Germscheid NM et al (2014) Optimal surgical care for adolescent idiopathic scoliosis: an international consensus. Eur Spine J 23(12):2603–2618. https://doi.org/10.1007/s00586-014-3356-1
Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H (2002) Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 11(4):336–343. https://doi.org/10.1007/s00586-002-0415-9
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am 83(8):1169–1181. https://www.ncbi.nlm.nih.gov/pubmed/11507125
Gajaseni P, Labianca L, Kalakoti P, Pugely AJ, Weinstein SL (2020) Deformity correction using proximal hooks and distal screws (PHDSs) improves radiological metrics in adolescent idiopathic scoliosis. Eur Spine J. https://doi.org/10.1007/s00586-020-06442-3
Trobisch PD, Ducoffe AR, Lonner BS, Errico TJ (2013) Choosing fusion levels in adolescent idiopathic scoliosis. J Am Acad Orthop Surg 21(9):519–528. https://doi.org/10.5435/JAAOS-21-09-519
Suk SI, Kim WJ, Lee CS et al (2000) Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis: recognition and treatment of double thoracic curve pattern in adolescent idiopathic scoliosis treated with segmental instrumentation. Spine 25(18):2342–2349. https://doi.org/10.1097/00007632-200009150-00012
McLain RF, Ferrara L, Kabins M (2002) Pedicle morphometry in the upper thoracic spine: limits to safe screw placement in older patients. Spine 27(22):2467–2471. https://doi.org/10.1097/00007632-200211150-00009
Takeshita K, Maruyama T, Chikuda H et al (2009) Diameter, length, and direction of pedicle screws for scoliotic spine: analysis by multiplanar reconstruction of computed tomography. Spine 34(8):798–803. https://doi.org/10.1097/BRS.0b013e3181895c36
Lehman RA Jr, Polly DW Jr, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ Jr (2003) Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine 28(18):2058–2065. https://doi.org/10.1097/01.BRS.0000087743.57439.4F
Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y (2005) Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech 18(6):522–526. https://doi.org/10.1097/01.bsd.0000154448.90707.a8
Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M (1999) Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J 8(2):156–159. https://doi.org/10.1007/s005860050147
Qian B, Jiang J, Zhu F, Zhu Z, Liu Z, Qiu Y (2013) How is the trachea at risk of injury from pedicle screw insertion in proximal thoracic curve of adolescent idiopathic scoliosis patients? Eur Spine J 22(2):338–344. https://doi.org/10.1007/s00586-012-2520-8
Cardoso MJ, Helgeson MD, Paik H, Dmitriev AE, Lehman RA Jr, Rosner MK (2010) Structures at risk from pedicle screws in the proximal thoracic spine: computed tomography evaluation. Spine J 10(10):905–909. https://doi.org/10.1016/j.spinee.2010.08.020
Jiang J, Qian B-P, Qiu Y, Wang B, Yu Y, Zhu Z-Z (2016) The potential risk of left subclavian artery injury from excessively long thoracic pedicle screws placed in the proximal thoracic regions of Lenke type 2 adolescent idiopathic scoliosis patients and normal teenagers: an anatomical study. Eur Spine J 25(10):3282–3287. https://doi.org/10.1007/s00586-016-4569-2
Sarwahi V, Wendolowski SF, Gecelter RC et al (2016) Are we underestimating the significance of pedicle screw misplacement? Spine 41(9):E548–E555. https://doi.org/10.1097/BRS.0000000000001318
Gonzalvo A, Fitt G, Liew S et al (2015) Correlation between pedicle size and the rate of pedicle screw misplacement in the treatment of thoracic fractures: can we predict how difficult the task will be? Br J Neurosurg 29(4):508–512. https://doi.org/10.3109/02688697.2015.1019414
Privitera DM, Matsumoto H, Gomez JA, Roye DP Jr, Hyman JE, Vitale MG (2013) Are breech rates for pedicle screws higher in the upper thoracic spine? Spine Deform 1(3):189–195. https://doi.org/10.1016/j.jspd.2013.04.002
Kuraishi S, Takahashi J, Hirabayashi H et al (2013) Pedicle morphology using computed tomography-based navigation system in adolescent idiopathic scoliosis. J Spinal Disord Tech 26(1):22–28. https://doi.org/10.1097/BSD.0b013e31823162ef
Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 9(3):235–240. https://doi.org/10.1007/s005860000146
Flynn JM, Sakai DS (2013) Improving safety in spinal deformity surgery: advances in navigation and neurologic monitoring. Eur Spine J 22(Suppl 2):S131–S137. https://doi.org/10.1007/s00586-012-2360-6
Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM (2012) Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine 37(8):E473–E478. https://doi.org/10.1097/BRS.0b013e318238bbd9
Baky FJ, Milbrandt T, Echternacht S, Stans AA, Shaughnessy WJ, Larson AN (2019) Intraoperative computed tomography-guided navigation for pediatric spine patients reduced return to operating room for screw malposition compared with freehand/fluoroscopic techniques. Spine Deform 7(4):577–581. https://doi.org/10.1016/j.jspd.2018.11.012
Watanabe K, Lenke LG, Matsumoto M et al (2010) A novel pedicle channel classification describing osseous anatomy: how many thoracic scoliotic pedicles have cancellous channels? Spine 35(20):1836–1842. https://doi.org/10.1097/BRS.0b013e3181d3cfde
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174. https://www.ncbi.nlm.nih.gov/pubmed/843571
Taniguchi Y, Matsubayashi Y, Kato S, Ono T, Oshima Y, Tanaka S (2020) Preoperative assessment of the feasibility of pedicle screw insertion at the proximal thoracic curve in Lenke type 2 idiopathic scoliosis. Glob Spine J 10(3):261–265. https://doi.org/10.1177/2192568219844989
Chan CYW, Kwan MK (2018) Zonal differences in risk and pattern of pedicle screw perforations in adolescent idiopathic scoliosis (AIS): a computerized tomography (CT) review of 1986 screws. Eur Spine J 27(2):340–349. https://doi.org/10.1007/s00586-017-5350-x
Chan CYW, Kwan MK (2017) Safety of pedicle screws in adolescent idiopathic scoliosis surgery. Asian Spine J 11(6):998–1007. https://doi.org/10.4184/asj.2017.11.6.998
Jiang J, Mao S, Zhao Q et al (2012) Different proximal thoracic curve patterns have different relative positions of esophagus to spine in adolescent idiopathic scoliosis: a computed tomography study. Spine 37(3):193–199. https://doi.org/10.1097/BRS.0b013e3182285fb9
Krag MH, Beynnon BD, Pope MH, DeCoster TA (1988) Depth of insertion of transpedicular vertebral screws into human vertebrae: effect upon screw-vertebra interface strength. J Spinal Disord 1(4):287–294. https://doi.org/10.1097/00002517-198800140-00002
Weinstein JN, Rydevik BL, Rauschning W (1992) Anatomic and technical considerations of pedicle screw fixation. Clin Orthop Relat Res 284:34–46. https://www.ncbi.nlm.nih.gov/pubmed/1395312
Mohamad F, Oka R, Mahar A, Wedemeyer M, Newton P (2006) Biomechanical comparison of the screw-bone interface: optimization of 1 and 2 screw constructs by varying screw diameter. Spine 31(16):E535–E539. https://doi.org/10.1097/01.brs.0000225997.41924.eb
Lee CS, Cho JH, Hwang CJ, Lee D-H, Park J-W, Park K-B (2019) The importance of the pedicle diameters at the proximal thoracic vertebrae for the correction of proximal thoracic curve in Asian patients with idiopathic scoliosis. Spine 44(11):E671–E678. https://doi.org/10.1097/BRS.0000000000002926
Belmont PJ Jr, Klemme WR, Dhawan A, Polly DW Jr (2001) In vivo accuracy of thoracic pedicle screws. Spine 26(21):2340–2346. https://doi.org/10.1097/00007632-200111010-00010
Vaccaro AR, Rizzolo SJ, Balderston RA et al (1995) Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Jt Surg Am 77(8):1200–1206. https://doi.org/10.2106/00004623-199508000-00009
Jeswani S, Drazin D, Hsieh JC et al (2014) Instrumenting the small thoracic pedicle: the role of intraoperative computed tomography image–guided surgery. Neurosurg Focus 36(3):E6. https://doi.org/10.3171/2014.1.FOCUS13527
Lien S-B, Liou N-H, Wu S-S (2007) Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J 16(8):1215–1222. https://doi.org/10.1007/s00586-006-0245-2
Hassan E, Liau K-M, Ariffin I, Halim YA (2010) Internal morphometry of thoracic pedicles in the immature spine. Spine 35(13):1253–1256. https://doi.org/10.1097/BRS.0b013e3181c1172b
Zhang H, Sucato DJ, Nurenberg P, McClung A (2018) Morphometric analysis of vertebral growth using magnetic resonance imaging in the normal skeletally immature spine. Spine 43(2):133–140. https://doi.org/10.1097/BRS.0b013e3181c80ec5
Zhuang Z, Chen Y, Han H et al (2011) Thoracic pedicle morphometry in different body height population: a three-dimensional study using reformatted computed tomography. Spine 36(24):E1547–E1554. https://doi.org/10.1097/BRS.0b013e318210f063
Morales-Avalos R, Leyva-Villegas J, Sánchez-Mejorada G et al (2014) Age- and gender-related variations in morphometric characteristics of thoracic spine pedicle: a study of 4,800 pedicles. Clin Anat 27(3):441–450. https://doi.org/10.1002/ca.22359
Kim NH, Lee HM, Chung IH, Kim HJ, Kim SJ (1994) Morphometric study of the pedicles of thoracic and lumbar vertebrae in Koreans. Spine 19(12):1390–1394. https://doi.org/10.1097/00007632-199406000-00014
Huang J, Zhang P, Jian X, Jiang H (2018) The prevalence and distribution of vertebral pedicles in adolescent idiopathic scoliosis in CHINESE people: a computed tomography-based study of 2958 vertebral pedicles. World Neurosurg 119:e560–e567. https://doi.org/10.1016/j.wneu.2018.07.211
Datir SP, Mitra SR (2004) Morphometric study of the thoracic vertebral pedicle in an Indian population. Spine 29(11):1174–1181. https://doi.org/10.1097/00007632-200406010-00004
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
RHG, SLM, ARK, NSH, EJS, JMF: conception or design of work. RHG, SLM, ARK, NSH, EJS, JMF: acquisition, analysis, or interpretation of data for the work. RHG, SLM, ARK, NSH, EJS, JMF: drafting of work or revising it critically for important intellectual content. RHG, SLM, ARK, NSH, EJS, JMF: final approval of version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to the content of this article.
IRB approval
This study was approved by the Institutional Review Board at the Children’s Hospital of Philadelphia.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guzek, R.H., Mitchell, S.L., Krakow, A.R. et al. Morphometric analysis of the proximal thoracic pedicles in Lenke II and IV adolescent idiopathic scoliosis: an evaluation of the feasibility for pedicle screw insertion. Spine Deform 9, 1541–1548 (2021). https://doi.org/10.1007/s43390-021-00377-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00377-5