Abstract
Purpose
Surgical correction for AIS has evolved from all hooks to hybrids or all screw constructs. Limited literature exists reporting outcomes using PHDS for posterior spinal fusion (PSF). This is the largest series in evaluating results of PHDS technique.
Methods
A retrospective review of consecutive AIS patients undergoing PSF by a single surgeon between 2006 and 2015 was performed. All eligible patients met a minimum 2-year follow-up. Patient demographics and radiographical parameters (radiographic shoulder height (RSH), T1 tilt, clavicle angle) at baseline, 6-week and 2-year post-operation were recorded. The primary outcome was difference in RSH from baseline measurements evaluated using repeated measures one-way analysis of variance with Bonferroni correction.
Results
A total of 219 patients (mean age at surgery: 13.68 years; 82% female) were included. The mean follow-up was 41.2 months (range 24–108 months). The RSH was significantly improved from − 14.7 ± 10.38 mm to 8.0 ± 6.9 mm (P < 0.0001). Clavicle angle was improved from 2.13° to 1.31° (P < 0.0001). T1 tilt was improved from 5.6° to 2.2° (P < 0.0001). At last follow-up, 95.8% of patients were shoulder balanced. There was a significant improvement of Cobb angle with an average correction of the upper thoracic curve of 42% and main thoracic curve of 67%.
Conclusion
The PHDS demonstrates the potential for additional shoulder balance improvement. Extension of fusion to structural proximal thoracic spine is the key to success for shoulder balance. It remains to be seen whether these improvements will translate into improved clinical outcomes in the longer term.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The goals of surgical treatment for adolescent idiopathic scoliosis (AIS) are to obtain a solid fusion while maintaining correction and balance in the coronal and sagittal planes [1]. After the era of Harrington instrumentation, hook instrumentation systems became the gold standard for AIS treatment. Over the last two decades, pedicle screw systems have replaced all-hook constructs.
Pedicle screws can be used alone or in combination with hooks which is often referred to as a hybrid [2, 3]. These systems allow for deformity correction in the coronal, sagittal and axial planes [2, 4].
Compared to the all-hook constructs, the hybrid hook-screw construct can further increase the degree of correction possible and decrease the length of the fusion necessary through distraction of the key vertebrae on the concave side and appropriate compression on the convex side. Several studies have tried to prove the superiority of correction of pedicle screws by comparing all-pedicle screw fixation with previous other constructs, such as hook or hybrid instrumentation. Results, however, are inconsistent [2, 5, 6].
Shoulder balance is a major concern in AIS patients as it is associated with patient appearance and patient satisfaction [7, 8]. Ending the construct with hooks at the proximal 2 or 3 levels and with screws distally is a technique we use to provide ligamentotaxis effect on correction of both the sagittal and coronal plane. This theoretically also reduces the potential adverse effects of all screw technique such as pedicle screw malposition and proximal junctional kyphosis (by transitioning from a rigid to less rigid construct) while providing for deformity and shoulder imbalance correction.
Our hypothesis is that this proximal hook screws distally (PHDSs) with a standard arthrodesis technique will provide to improve shoulder balance while allowing for curve correction. In this paper, we will report our results using PHDS technique and its effects on shoulder balance over the follow-up period.
To our knowledge, there are no clinical and radiologic outcome reports using this technique. This study is the largest series in evaluating results of hybrid in AIS patients.
Materials and methods
Patient population
After obtaining institutional review board approval, the medical records and spinal radiographs of patients with AIS surgically treated between 2006 and 2015 were retrospectively reviewed. Inclusion criteria were as follows: (1) patients undergoing instrumented posterior spinal fusion with PHDS construct, (2) minimum 2-year follow-up and (3) all patients treated by the same surgeon (senior author). Patients who underwent spine surgery before the index surgery were excluded. PHDS was defined as hooks being used for proximal fixation (2 or 3 segments) with pedicle screws used distally. In a query of 440 spinal fusion for AIS cases performed between 2006 and 2015, 252 PHDS patients were identified. For this investigation, a total of 219 patients were included. Thirty patients with poor visualization radiograph and three patients had previous spine surgery were excluded.
Clinical and radiographic assessment
All patients were evaluated preoperatively, immediately after surgery (at first postoperative visit 6 weeks after surgery), and at a minimum of 2 years after surgery with whole-spine erect posteroanterior and lateral radiographs. Preoperative radiographic evaluation also included supine right and left bending films.
Data were collected on age, sex, body weight, Race, Risser stage, digital skeletal age (Sanders maturity score), curve pattern (Lenke classification). Surgical data included operating room (OR) time and estimated blood loss (EBL) were recorded. Clinical outcomes were evaluated from SRS-22 scores at follow-up. Radiographic analysis included Cobb angle measurements of the main thoracic and proximal thoracic curves, radiographic shoulder height (RSH), T1 tilt and clavicle angle. RSH was defined as the difference in the soft tissue shadow directly superior to the acromioclavicular joint [9]. A positive RSH value was defined as right shoulder was higher, whereas a negative value was defined as left shoulder was higher. A shoulder imbalance was defined as RSH difference more than 20 mm. A positive T1 tilt and clavicle angle were defined as tilting or opening to the right, whereas a negative value was defined as tilting or opening to the left. On the lateral radiographs, the proximal junction angle was defined as the caudal endplate of the UIV to the cephalad endplate to vertebrae proximal. Abnormal proximal junctional kyphosis (PJK) was defined by proximal junction sagittal Cobb angle > 10° and at least 10° greater than the preoperative measurement [21].
All radiographic measurements were made by three of the authors who were not involved in the patient treatment. In addition, the following ratio was determined immediately postoperatively and at final follow-up:
Surgical technique
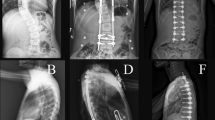
All operations were performed by the senior author. A standard midline posterior subperiosteal approach was performed followed by distal and proximal instrument insertion. Paravertebral muscle and posterior ligamentous complex of proximal junctional level including facet joint capsule were preserved during the surgery. Lamina hooks and pedicle hooks were used for proximal fixation, and pedicle screws were used distally. The technique of hooks placement is described in Fig. 1. Pedicle screws were inserted by standard free-hand technique. All inferior facets were resected, and cartilage was denuded from the superior facets for fusion. Segmental distraction and compression were performed for shoulder levelling. Intraoperative construct position, curve correction, truncal balance and shoulder balance were checked intraoperatively with the fluoroscope. All patients had motor and sensory monitoring intraoperatively.
A 16-year-old female with AIS Lenke 3, who underwent posterior spinal fusion using PHDS technique. Preoperatively, main thoracic Cobb was 65° and lumbar Cobb was 55°. Her RSH was 0.5 cm. (right shoulder is slightly higher than the left). On bending films, there was still a curve in the proximal thoracic curve and although it was less than 25° on side bending films; significant pedicle rotation persisted and we elected to fuse to T2. After surgery, she had good main thoracic curve correction and shoulder balance. a Before surgery, b immediately after surgery, c at the two-year follow-up. After all pedicle screws were inserted. An upgoing pedicle hook was placed at T3 on the left in the facet joint and medial to the pedicle and similarly at T2 on the right. A supralaminar hook is place over the superior lamina at T2 on the left to provide a “claw configuration” on the left side of the proximal curve. The initial corrective rod is placed through the claw configuration at T2, 3 on the left and then into the pedicle screws distally. The hooks are loosely held in place but stabilized to prevent displacement while the spine is manipulated through the pedicle screws distally with standard corrective maneuvers. Then with the left T2 hook locking screw is loosened. Distraction is applied across T3 against the T5 pedicle screw which pushes the left shoulder proximal. The second right sided rod is placed though the upgoing pedicle hook at T2 and into the pedicle screws distally. Once all distal screws have been secured and correction of the main thoracic curve obtained; distraction is applied across T2 on the right to push the R shoulder up and balance the shoulder height. Finally the claw is secured at T2 on the L, by compression of T2 against T3. Intraoperative fluoroscopy is checked to insure shoulder leveling
Statistical analysis
Repeated measures one-way analysis of variance (RM-ANOVA) and Friedman test were performed. Statistical significance was set at P ≤ 0.05.
Results
Demographic data
There were 219 patients included in this study. The mean follow-up was 41.2 ± 19.66 months (range 24–108 months; median 33 months). The average age at the time of surgery was 13.66 years (range 13–16 years). There were 179 females (82%) and 40 males (18%). Most patients had Risser grade 4 (31.5%), followed by 5 (27.8%) and 0 (12.7%). The majority of patients presented with a Lenke type 1 curves (43%). The remainders were (13.2%) Lenke 2, (7.3%) Lenke 3, (4.1%) Lenke 4, (9.5%) Lenke 5 and (8.6%) Lenke 6. The mean main thoracic Cobb angle and proximal thoracic Cobb angle were 53.4° and 24.5°, respectively. The average preoperative flexibility was 52% (range 35–73%). The upper instrumented vertebra (UIV) was T2 in 123 cases (56.3%), T3 in 28 cases (12.6%) and T4 in 68 cases (31.09%). The median OR time for the procedures was 270 min. The mean EBL was 530 ml. More demographic and surgical information can be found in Table 1. The mean postoperative SRS-22 outcome scores at final follow-up were 4.2(3.8–4.6). No neurological complications occurred in any of the patients. No intraoperative and postoperative hooks pullout was identified.
Radiographic analysis
Shoulder balance
The RSH was significantly improved from − 14.7 to 8.0 mm (P < 0.0001). Preoperatively, the mean RSH was 14.7 ± 10.38. At 6 weeks after surgery, the mean RSH was 9.2 ± 7.7. At the final follow-up, the mean RSH was 8.0 ± 6.9. (Table 2). The median T1 tilt was improved from 5.6° to 2.2° (P < 0.0001).
The median clavicle angle was improved from 2.13° to 1.31° (P < 0.0001).
Prior to surgery, 31% of the patients had shoulder imbalance. At last follow-up, 95.8% of patients were balanced according to shoulder imbalance definition as mentioned above.
Curve correction
Before surgery, the median proximal thoracic Cobb angle was 24.51° (range 23.17–25.86). The median main thoracic Cobb was 53.46° (range 51.89–55.02). At 6 weeks after surgery, the median proximal thoracic Cobb angle was 14.25° (range 13.25–15.25). The median main thoracic Cobb was 17.81° (range 16.85–18.77). The difference of both proximal and main thoracic was significantly (P < 0.001) improved. At the last follow-up, the median proximal thoracic Cobb was measured 14.26° (range 13.22–15.30). The median main thoracic Cobb was 18.81° (range 17.78–19.84). There was a significant improvement of Cobb angle with an average correction of upper thoracic 44.21% and main thoracic 66.22% (P < 0.001).
PJK occurred in 10.3% at 6 weeks and 25.7% at final follow-up.
Four patients (3.3%) required revision surgery, two because of infections, one for pain and a significant metallosis reaction and one for proximal junctional kyphosis (PJK). There were no neurologic events with this technique.
Discussion
This study focused on early and sustained effect of one particular hook-screw construct using hooks at the proximal 2–3 levels and screws distally called PHDS. All patients included in this study were treated at the same institution by a single surgeon, providing consistency in surgical technique and patient selection criteria.
Pedicle screw fixation is considered biomechanically advantageous because it uses pedicles as the anchor engaging the vertebral body as well as posterior elements. Previous series have shown better major curve correction after all-pedicle screw fixation than after hybrid screw-hook constructs [10]. PHDS is a variation of the hybrid instrumentation construct. Hook constructs by our technique described herein provide a ligamentotaxis effect using a distraction and compression basis for shoulder leveling as described in surgical technique. We postulated that by use of this particular technique, we could better improve shoulder balance in AIS patients while still providing for coronal and sagittal and rotational deformity correction.
This technique showed the potential for shoulder balance improvement, with a mean improvement of RSH from preoperatively to final follow-up (14.7 baseline to 9.2 at 6 weeks and 8.0 at the final follow-up) (P < 0.001). Many studies defined shoulder imbalance as RSH difference more than 20 mm. Our technique created shoulder balance in 95.8% of our patients. Only 16 patients (4.2%) had postoperative shoulder imbalance. The improvement in shoulder balance in this study compares favorably to a weighted average improvement of 7–13% published in prior studies [11, 12]. We found the incidence of new shoulder imbalance (the post-op shoulder imbalance patient who was balanced before surgery) was 0.5% which is lower than a study of Benjamin et al. where they reported new shoulder imbalance of 8.8% [13].
The medial and lateral shoulder balance concept was reported by Ono et al.[14]. The T1 tilt correlated very well to medial trapezoidal prominence (medial balance) but not lateral shoulder balance. Our study found that not only RSH and clavicle angle (lateral balance) were improved, but medial balance from T1 tilt angle was also improved.
The shoulder balance immediately after surgery was also sustained until last follow-up (average 3.5 years). This study found that there was no change of shoulder balance parameters compared at 6 weeks after surgery and the last follow-up. Hence, patients who have shoulder balance after surgery were still balanced at their last follow-up by our technique (P < 0.001). Secondly, patients who have shoulder imbalance at 6 weeks after surgery will not improve with time. Thus, shoulder balance immediately after surgery is important for long-term outcome and cannot be expected to improve after 6 weeks.
In terms of degree of correction, there is no consensus which method provides the best correction [2, 5, 6]. A retrospective comparative study of 58 patients with AIS found that immediately after surgery, the average major curve correction was 70% for the all-pedicle screw group and 56% for the hybrid group [4]. Significant differences between the two groups were also noted at 2-year follow-up, with the all-pedicle screw construct achieving 65% of correction and hybrid instrumentation 46%. However, a retrospective study by Alvin et al. showed no difference between those two techniques [15]. Our results showed improvement of the primary curve of 67%, which is comparable to the previous studies using all-pedicle screw constructs [2, 4, 5, 16]. This particular construct seems to provide better correction of the major curve than previously reported hybrid constructs. We suspected this may be due to the fact that the major curve was corrected by pedicle screws and the shoulder balance was improved by the hooks. Moreover, the overall loss of correction in the major curve was 3.1% (1.5°). This is consistent with the loss associated with an all screw construct at around 5% from studies [2, 4]. The mean SRS-22 scores at final follow-up were 4.2. This may be because most patients obtained good correction of the main thoracic curve and shoulder balance. The clinical outcome was comparable with the previous report by Kuklo et al. that clinical outcome was improved when appearance of shoulder and curve correction has been corrected [9].
The UIV in our study was T2 in 123 cases (56.3%), T3 in 28 (12.6%) and T4 in 68 cases (31.1%). It might argue that only 13% of curves were Lenke 2 from our cohort; however, T2 was selected as UIV 56.3% of cases. We have two reasons: Firstly, there are studies published recently about the criteria of structural upper thoracic such as shoulder level, degree of upper thoracic Cobb angle and degree of vertebral rotation [17,18,19]. We have low threshold to go to a higher thoracic level to provide the best correction of shoulder and upper thoracic curve if we considered that the upper thoracic curve might be structural although the Cobb angle was less than 25 on bending film. Secondly, to the best of our knowledge, there is no report or specific study on the disadvantages of T2 fusion over T3 or T4 except the screw insertion complications. A study of screw malposition in pediatric population found that the higher the level in the thoracic spine, the higher the risk of screw malposition [6]. Our technique can reduce this complication by using the hooks and also reduce radiation exposure by using intraoperative fluoroscope which is often needed at the proximal levels to aid screw positioning.
Another strength of this technique is that the widely discussed complication of all-pedicle screws construct is PJK. A study by Kim et al. [20] retrospectively compared 410 cases of posterior segmental spinal instrumentation and fusions and found that pedicle screw-only constructs had the highest rate of PJK (35.1%) compared with hook-only constructs (24.1%) and hybrid constructs (29.1%). Rate of PJK from our technique was 10.3% at 6 weeks and 25.7% at final follow-up which was comparable with other hybrids but better than all-pedicle constructs. It seems that hooks are associated with lower rates of PJK, especially when utilized in the proximally instrumented vertebrae after long-segment instrumentation to create transition load at the upper levels. However, this study as well as most of the studies in the literature shows that even if it has a significant prevalence (26%) rarely, it produces symptoms [21, 22]. And we found one only revision surgery due to PJK. In other words, low reoperation rate (0.4%; 1/219) from PJK was noted in this study.
Our study has some limitations. The study was retrospective in nature. In addition, the mean follow-up of 3.4 years is relatively short, and further long-term follow-up is warranted to demonstrate whether our radiographic findings remain durable. Finally, there were a fair number of patients who had missing radiographic data which should be noted when interpreting our clinical results.
Conclusion
This study demonstrates that favorable outcomes can be obtained with the use of proximal hooks and distal screws technique. The PHDS does demonstrate the potential for additional shoulder balance improvement. Extension of the fusion into structural proximal thoracic spine is the key to success for shoulder balance. It remains to be seen whether these improvements will translate into improved clinical outcomes in the longer term.
References
Kim HJ, Blanco JS, Widmann RF (2009) Update on the management of idiopathic scoliosis. Curr Opin Pediatr 21(1):55–64
Kim YJ, Lenke LG, Kim J et al (2006) Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 31(3):291–298
Hicks JM, Singla A, Shen FH et al (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 35(11):E465–470
Kim YJ, Lenke LG, Cho SK et al (2004) Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29(18):2040–2048
Lowenstein JE, Matsumoto H, Vitale MG et al (2007) Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 32:448–452
David MP, Hiroko M, Jaime AG et al (2013) Are breech rates for pedicle screws higher in the upper thoracic spine? Spine Deform 1(3):189–195
Akel I, Pekmezci M, Hayran M et al (2008) Evaluation of shoulder balance in the normal adolescent population and its correlation with radiological parameters. Eur Spine J 17:348–354
Li M, Gu S, Ni J et al (2009) Shoulder balance after surgery in patients with Lenke Type 2 scoliosis corrected with the segmental pedicle screw technique. J Neurosurg Spine 10:214–219
Kuklo TR, Lenke LG, Graham EJ et al (2002) Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 27(18):2013–202
Suk SI, Lee CK, Kim WJ et al (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 20:1399–405
Bago J, Carrera L, March B et al (1996) Four radiological measures to estimate shoulder balance in scoliosis. J Pediatr Orthop B 5(1):31–34
Lee CK, Denis F, Winter RB et al (1993) Analysis of the upper thoracic curve in surgically treated idiopathic scoliosis. A new concept of the double thoracic curve pattern. Spine (Phila Pa 1976) 18(12):1599–1608
Benjamin TB, Zoe BC, Grant DS et al (2015) Do current recommendations for upper instrumented vertebra predict shoulder imbalance? An attempted validation of level selection for adolescent idiopathic scoliosis. HSSJ 11:216–222
Ono T, Bastrom TP, Newton PO (2012) Defining 2 components of shoulder imbalance: clavicle tilt and trapezial prominence. Spine (Phila Pa 1976) 37:E1511–E1516
Alvin HC, Marios GL, Xu G et al (2013) All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery a comparative radiographical study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 38:1199–1208
Suk SI, Kim WJ, Lee SM et al (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976) 26:2049–2057
Lenke LG, Bridwell KH, O’Brien MF et al (1994) Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 19(14):1589–1597
Guixing Q, Jianguo Z, Yipeng W et al (2005) A new operative classification of idiopathic scoliosis: a Peking union medical college method. Spine (Phila Pa 1976) 30:1419–1426
Qianyu Z, Guixing Q, Qiyi L et al (2019) Modified PUMC classification for adolescent idiopathic scoliosis. Spine J 19:1518–1528
Kim YJ, Lenke LG, Bridwell KH et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32:2731–2738
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Helgeson MD, Shah SA, Newton PO et al (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid Instrumentation. Spine (Phila Pa 1976) 35:177–181
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No disclosure for this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gajaseni, P., Labianca, L., Kalakoti, P. et al. Deformity correction using proximal hooks and distal screws (PHDSs) improves radiological metrics in adolescent idiopathic scoliosis. Eur Spine J 30, 686–691 (2021). https://doi.org/10.1007/s00586-020-06442-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06442-3