Abstract
This study aimed to examine the effects of adding growth hormone (GH) into the in vitro maturation (IVM) culture medium of mouse oocytes on pregnancy outcomes. Cumulus-oocyte complexes (COCs) were cultured in a medium with (GH group, 100 ng/mL) or without (Con group) GH. Thereafter, chromosome morphology, spindle morphology, and mitochondrial function were examined. Embryo development and blastocyst quality after in vitro fertilization were evaluated. After the embryo transfer, the implantation sites and pregnancy outcomes were evaluated. The oocyte maturation rate of the GH group (81.8 ± 9.6%) was compared to that of the Con group (81.3 ± 6.9%, P = 0.928). The proportion of morphologically abnormal spindles in GH-treated oocytes (7.1 ± 0.9%) was significantly lower than control oocytes (13.7 ± 1.3%, P = 0.032), whereas the proportion of morphologically abnormal chromosomes and mitochondrial distribution was similar between the groups. The mitochondrial membrane potential (P < 0.001) and ATP concentration (P < 0.001) in GH-exposed oocytes were higher than those in control oocytes. After fertilization, the blastocyst rate in the GH group (33.8 ± 13.2%) was significantly higher than the Con group (16.2 ± 2.0%, P = 0.003). In addition, inner cell mass (ICM) number (13.91 ± 3.48 vs. 7.00 ± 1.91, P < 0.001), total cell number (47.45 ± 8.39 vs. 37.71 ± 4.15, P = 0.007), and the ratio of ICM/total cell number (29.9 ± 8.2% vs. 18.6 ± 5.0%, P = 0.002) of blastocyst were all higher in GH group. The implantation rate (71.2 ± 1.9% vs. 39.4 ± 16.4%, P < 0.001) and litter size (8.50 ± 3.99 vs. 3.00 ± 1.22, P = 0.018) were significantly higher in the GH group. Although addition of GH into IVM culture medium does not improve oocyte maturation rate, it improves oocyte and embryo quality, which leads to better embryo development and pregnancy outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro maturation (IVM) is not commonly used because it associates with poor oocyte maturation and developmental competence compared with traditional in vitro fertilization (IVF) [1, 2]. Researchers have reported many attempts to improve IVM culture systems by adding different growth factors [3, 4] or hormones [5, 6] into media or altering culture protocols [7]. Growth hormone (GH) has been reported to improve human oocyte potential competence [8]. A high GH concentration in human follicular fluid was reported to be associated with a high developmental competence in oocytes [9]. Hou et al. [10] demonstrated that daily injections of GH to aged mice for 8 weeks improved oocyte quality, probably by enhancing mitochondrial function. Furthermore, Weall et al. [11] illustrated that GH administration before oocyte retrieval could increase the number of mitochondria in oocytes from aged women with decreased GH receptor (GHR) expression. As for the poor responders undergoing assisted reproductive technology treatments, GH could significantly increase the number of oocytes retrieved, and thus the number of transferable embryos [12], pregnancy rate, and live birth rate [13]. Although GH pretreatment could not improve the live birth rate [14], we observed an increase in the number of retrievable oocytes and transferable embryos, as well as the clinical pregnancy rate [15], consistent with the results of previous studies reporting an improvement in oocyte development by GH.
In the aforementioned studies, GH was administered systemically over the course of several weeks, instead of locally. As GH can affect organs other than the ovary, long-term systemic administration may cause unwanted effects. Therefore, adding GH into the IVM culture medium may represent a better approach to understanding the effects of this hormone on the developmental capacity of oocytes.
The effects of GH on oocyte function are not entirely known. Although GH supplementation (100 ng/mL) can accelerate the kinetics of meiosis in bovine COCs, there was no improvement in the maturation rate [16], cleavage rate, and embryo production rate after culturing for 24 h [17]. However, the addition of GH at the same concentration to culture medium accelerated the meiotic resumption in immature rat cumulus-enclosed oocytes, but not in denuded oocytes [18]. Furthermore, GH has been reported to improve the maturation rate of equine [19,20,21], mouse [22], and human [8] oocytes, although the developmental potential of mature oocytes was not examined in these studies. Furthermore, few studies [23, 24] have reported improved embryo development by GH.
Most in vitro studies have investigated the effects of GH supplementation in the culture medium on the maturation of oocytes, and few have examined its effects on the later embryo development. In addition, implantation and pregnancy outcomes of embryos derived from IVM oocytes have not been examined yet. This study was designed to explore the effects of GH supplementation on oocyte maturation, oocyte quality, subsequent embryo development, and pregnancy outcomes after embryo transfer in mice.
Materials and Methods
Oocyte Collection, Culture, and Maturation Assessment
This study was approved by the Institutional Animal Welfare and Ethics Committee Policies of Peking University Health Science Center (protocol no. LA2018256). Eight-week-old female Institute of Cancer Research (ICR) mice were sacrificed by cervical dislocation for 44–46 h after the intraperitoneal injection of pregnant mare serum gonadotropin (PMSG, 5 IU). In the M2 medium (Sigma-Aldrich, cat. no. M7167, USA), COCs were released from ovaries by puncture with a 1-mL syringe needle. COCs with an intact enclosed cumulus were collected and divided equally into two groups for culture at 37 °C in an incubator with 5% CO2 for 14 h. The maturation medium was TCM-199 (Gibco, cat. no. 11150059, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, cat. no. 10099141), 24.2 mg/mL sodium pyruvate (Sigma-Aldrich, cat. no. P4562), 1.5 IU/mL PMSG (Ningbo Second Hormone Factory, cat. no. Ymxq-0001, China), and 1.5 IU/mL hCG (ProSpec, cat. no. HOR-250, Israel). For the GH group, COCs were cultured in the maturation medium in the presence of recombinant mouse GH (100 ng/mL, Prospec, cat. no. CYT-540). For the Con group, COCs were cultured in the maturation medium in the absence of GH. After culturing for 14 h, several oocytes were denuded from cumulus cells with hyaluronidase (Sigma-Aldrich, cat. no. H4272) for maturity assessment. Mature oocytes (MII stage) were characterized as those with the first polar body but without the germinal vesicle.
Fertilization and Embryo Culture
To examine the effects of GH supplementation on embryo development, COCs were immediately fertilized (i.e., without maturity assessment) to avoid the adverse effects of hyaluronidase on oocyte competence. After culturing for 13 h, a 10-week-old fertile male ICR mouse was sacrificed, and a small incision was made in the cauda epididymis to collect sperms. Sperms were transferred to 0.3 mL of human tubal fluid (HTF) medium (Millipore, cat. no. MR-070-D, USA) containing 4 mg/mL of bovine serum albumin (BSA, Sigma-Aldrich, cat. no. A1933), covered with a drop of paraffin oil, and incubated at 37 °C for 1 h. COCs were subsequently transferred to fresh HTF medium (0.3 mL), and 3–5 μL of medium containing sperms was used for in vitro fertilization (IVF). After fertilizing for 3–4 h, the oocytes were washed with the HTF medium, transferred into KSOM medium (Millipore, cat. no. MR-121-D), and incubated at 37 °C. Zygote development was assessed, and the proportions of 2-cell and blastocysts were recorded.
Immunofluorescence Staining
For the staining of chromosomes and spindles, mature oocytes were fixed in 4% paraformaldehyde for 30 min, followed by permeabilization in phosphate-buffered saline (PBS) containing 0.5% Triton X-100 for 20 min and blocking in PBS containing 1% BSA for 1 h at room temperature. Oocytes were subsequently incubated in a fluorescein isothiocyanate-conjugated anti-α tubulin antibody (Sigma-Aldrich, cat. no. F2168, diluted 1:200 in PBS containing 1% BSA) at 37 °C for 1 h under dark conditions. After washing three times in PBS containing 1% Tween-20 and 0.01% Triton X-100, the oocytes were mounted in antifade mounting medium containing DAPI (4′6,-diamidino-2-phenylindole) (Beyotime, cat. no. P0131, China) on glass slides and visualized under a confocal microscope (Zeiss model LSM 710, USA).
For the analysis of mitochondrial distribution, the oocytes were cultured in the maturation medium containing 200 nM Mito-Tracker Green (Invitrogen, cat. no. M7514, USA) at 37 °C for 30 min under dark conditions. Oocytes were washed three times, transferred to a glass-bottom dish (NEST, cat. no. 801002, China) containing the maturation medium, and visualized under a confocal microscope.
For differential staining, blastocysts were washed twice with PBS and then fixed in 4% paraformaldehyde for 20 min at room temperature. They were washed in PBS with 0.1% Tween 20 for three times and permeabilized with 0.25% Triton X-100 for 30 min at 37 °C. After that, blastocysts were blocked with 3% BSA for 2 h at room temperature, followed by treating with primary antibodies overnight at 4 °C. After being washed with 0.1% Tween 20-PBS for three times, blastocysts were incubated with second antibodies for 1 h at room temperature. Primary antibodies used in this study were NANOG (CST, cat. no. 8822S, USA) and CDX2 (Santa Cruz, cat. no. sc-393572, USA). Second antibodies used were CyTM3-conjugated AffiniPure Goat Anti-Rabbit IgG (Jackson ImmunoResearch, cat. no. 111-165-144, USA) and CyTM2-conjugated AffiniPure Goat Anti-Mouse IgG (Jackson ImmunoResearch, cat. no. 115-225-146). Finally, blastocysts were mounted in an antifade mounting medium containing DAPI on glass slides and visualized under a confocal microscope (Zeiss model LSM 710, USA). The nuclei of the inner cell mass (ICM) cells that were labeled with NANOG appeared red, nuclei of the trophectoderm (TE) cells that were labeled with CDX2 appeared green, and the nuclei of the total cells that were stained with DAPI fluoresced blue.
Measurement of the Mitochondrial Membrane Potential
JC-1 (BioVision, cat. no. 1130-5, USA), a cationic carbocyanine dye, was dissolved in dimethyl sulfoxide at a stock concentration of 5 mg/mL. Mature oocytes were cultured in the M2 medium containing JC-1 (10 μg/mL) at 37 °C for 15 min, and then confocal images were acquired at wavelengths of 488 nmEX/564 nmEM. The ImageJ 1.47 Software (National Institutes of Health, USA) was used to quantify the intensity of the fluorescent signal in each oocyte. The mitochondrial membrane potential was calculated as the ratio of red fluorescence to green fluorescence.
Measurement of the ATP Level in Oocytes
Five oocytes constituted one sample, and three samples were assayed for each time point. Lysis buffer (50 μL) was added to each sample on ice, and samples were centrifuged at 12000×g for 5 min. The supernatants were recovered, and the ATP level was measured using the Enhanced ATP Assay (Beyotime, cat. no. S0027) as previously described [25]. In brief, the ATP standard solution was diluted appropriately, and a standard curve of seven ATP concentrations was generated. Supernatants were combined with the ATP working solution (100 μL), and samples were incubated at room temperature for 3 min. The absorbance was measured with a multiscan spectral microplate reader. The ATP concentration was determined using the standard curve. The experiment was replicated three independent times.
Preparation of Pseudopregnant Mice and Embryo Transfer
One day before embryo transfer, 8-week-old virgin female ICR mice were mated with vasectomized males to induce pseudopregnancy, which was confirmed by the presence of a vaginal plug. Eighteen pseudopregnant mice were anesthetized with tribromoethanol (Sigma-Aldrich, cat. no. T48402), and a 1-cm incision was made along the dorsum midline. One ovary was partially removed, and 13 2-cell-stage embryos derived from 2-pronuclei zygotes were forced into the oviduct with a mouth-controlled capillary pipette under the guidance of a stereomicroscope. This process was repeated for the other oviduct.
Staining and Observation of the Implantation Site
Chicago Blue (Yuanye, cat. no. S19183, China) was dissolved in normal saline according to the manufacturer’s instructions. Five days after embryo transfer, 1% Chicago Blue dye (0.2 mL) was injected into the tail vein of three mice from each group. The mice were sacrificed after the eyes and lips turned blue. Uteri and bilateral ovaries were collected. Implantation sites were stained blue and identified easily.
Statistical Analysis
Data were analyzed with the SPSS 25.0 Software (IBM, USA). Comparisons between measurement data were performed by Student’s t-test or Mann–Whitney U test appropriately, whereas comparisons between categorical data were performed by chi-square test. All reported P-values were two tailed, and P < 0.05 was considered statistically significant.
Results
Effects of GH Supplementation on the Maturation Rate and Embryo Development
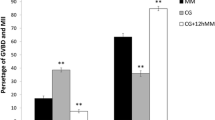
A total of 350 COCs were retrieved from 20 mice (5 per time). As shown in Fig. 1a, only cumulus-enclosed oocytes were used in this experiment. The maturation rate of GH-treated oocytes (81.8 ± 9.6%, n = 4) was similar to that of untreated oocytes (81.3 ± 6.91%, n = 4, P = 0.928; Fig. 1b)
Morphology of oocytes and comparison of oocyte maturation and embryo development. a Morphology of COCs and denuded oocytes. Red arrow (right panel) indicates an oocyte with the first polar body. Scale bar = 100 μm. b Comparison of the maturation rate between Con and GH groups. Normal data distribution, Student’s t-test. MII rate, ratio of mature oocytes to total oocytes cultured. c Comparison of 2-cell-stage embryo rate and blastocyst rate between Con and GH groups. Chi-square test. **P < 0.01. Con, control; GH, growth hormone
As mechanical or chemical denudation can adversely affect oocyte quality, COCs were immediately fertilized with epididymal sperms in vitro in the absence of maturity assessment. Twenty-five mice were sacrificed and 421 COCs were obtained. As shown in Fig. 1c, 66.8 ± 6.8% (n = 5) of GH-treated COCs developed into 2-cell-stage embryos compared to 61.9 ± 10.3% (n = 5) of Con COCs. The proportions of 2-cell-stage embryos in the GH group developing into blastocysts (33.8 ± 13.2%, n = 5) were significantly higher than that of the Con group (16.2 ± 2.0%, n = 5, P = 0.003).
Effects of GH Supplementation on Chromosome Morphology, Spindle Morphology, and Mitochondrial Distribution in Mature Oocytes
COCs were obtained from 40 mice and cultured in two groups for 14 h. After denuding oocytes and assessing maturity, 513 mature oocytes were selected for immunofluorescence staining, of which 388 oocytes were used for the co-staining of chromosomes and spindles and 125 oocytes were used for the staining of mitochondria. The rate of morphologically abnormal chromosomes in oocytes of the GH group (7.1 ± 0.9%, n = 4) was similar to that in cells of the Con group (10.5 ± 1.3%, n = 4; P = 0.229). The rate of morphologically abnormal spindles in oocytes of the GH group (7.1 ± 4.1%, n = 4) was lower than that in oocytes of the Con group (13.7 ± 6.2%, n = 4; P = 0.032). There was no significant difference in the mitochondrial distribution between the GH group (3.2 ± 3.2%, n = 4) and the Con group (1.6 ± 2.7%, n = 4; P > 0.999; Fig. 2)
Chromosome morphology, spindle morphology, and mitochondrial distribution of mature oocytes. (A) Immunofluorescent staining of chromosomes (blue) and spindles (green). a Normal chromosome and spindle morphologies are shown. b and c Abnormal chromosome and spindle morphologies are shown; scale bar = 20 μm. (B) Confocal microscopy images of mitochondrial distribution (green). a and b Normal mitochondrial distribution (mitochondria were distributed homogeneously within the cytoplasm) is shown. c Abnormal mitochondrial distribution (mitochondria were abnormally clustered within the cytoplasm) is shown; scale bar = 20 μm. (C) Proportions of oocytes with morphologically abnormal chromosomes and spindles, and oocytes with abnormally distributed mitochondria. Chi-square test. *P < 0.05. Con, control; GH, growth hormone
Effect of GH Supplementation on Mitochondrial Function in Mature Oocytes
COCs were retrieved from five mice and cultured in two groups. Thereafter, 65 mature oocytes were fluorescently stained with JC-1 (33 GH-treated oocytes and 32 Con oocytes). The red–green fluorescent intensity ratio, which reflects the mitochondrial membrane potential, was calculated according to the manufacturer’s instructions. As shown in Fig. 3b, the membrane potential of GH-treated oocytes (1.15 ± 0.14) was significantly higher than that of Con oocytes (0.80 ± 0.10, P < 0.001).
Mitochondrial membrane potential and ATP level in oocytes. a JC-1 immunofluorescent staining of oocytes cultured in the presence (GH) or absence (Con) of GH. Scale bar = 20 μm. b Comparison of the ratio of red-to-green immunofluorescence in oocytes as an indicator of the mitochondrial membrane potential. Normal data distribution, Student’s t test. c Comparison of the ATP level in oocytes between Con and GH groups. Normal data distribution, Student’s t test. ***P < 0.001. Con, control; GH, growth hormone
COCs were retrieved from two mice, and the ATP level was measured in mature oocytes. The ATP level in GH-treated oocytes (0.90 ± 0.02 pmol/oocyte) was significantly higher than that of Con oocytes (0.72 ± 0.03 pmol/oocyte, P < 0.001; Fig. 3c)
Effects of GH Supplementation on Blastocyst Quality
A total of 7 blastocysts in the Con group and 22 blastocysts in the GH group were stained for quality evaluation (Fig. 4a). Although numbers of TE cells (stained with CDX2) per blastocyst were similar between the Con group (30.71 ± 4.15) and the GH group (33.55 ± 8.50, P = 0.407), number of ICM cells (stained with NANOG, 13.91 ± 3.48) and number of total cells (stained with DAPI, 47.45 ± 8.39) were significantly higher than those in the Con group (7.00 ± 1.91, P < 0.001; 37.71 ± 4.15, P = 0.007, respectively). The ratio of ICM cell number/total cell number was also significantly higher in the GH group (29.9 ± 8.2%) than that in the Con group (18.6 ± 5.0%, P = 0.002; Fig. 4b and c)
Immunostaining and comparisons of ICM cells, TE cells, and total cells of blastocyst in Con and GH groups. a Blastocysts derived from oocytes in Con and GH groups were stained with NANOG for ICM cells, CDX2 for TE cells, and DAPI for total cells. Bar = 10 μm. b Comparison of numbers of ICM cells, TE cells, and total cells between two groups. c The ratio of ICM/total cells represents by mean ± SD in each group. Normal data distribution, Student’s t test. **P < 0.01. Con, control; GH, growth hormone; ICM, inner cell mass; TE, trophectoderm
Effect of GH Supplementation on Pregnancy Outcomes
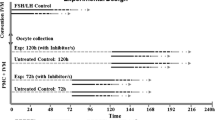
Twenty mice were primed and sacrificed for oocyte retrieval. After IVF, 2-cell-stage embryos were transferred into the oviducts of two pseudopregnant mice (one received 26 embryos derived from the GH group, and the other received 26 embryos derived from the Con group). The experiment was replicated nine times.
Five days after ET, Chicago Blue was injected into four mice from each group. Mice were sacrificed, and the implantation sites were examined. The uteri and ovaries are shown in Fig. 5a. The implantation rate of mice that received embryos from the GH group (71.2 ± 1.9%, n = 4) was significantly higher compared to mice that received embryos from the Con group (39.4 ± 16.4%, n = 4, P < 0.001). The remaining six mice from each group were followed until delivery or confirmation of non-pregnancy. All six mice in the GH group gave birth to pups, and the litter size was 8.40 ± 3.60, whereas five of six mice in the Con group gave birth, and the litter size was 3.00 ± 1.22 (P = 0.018; Fig. 5b and c)
Images of implantation sites and comparison of pregnancy outcomes. a Images of uteri and ovaries from mice after injection with Chicago Blue (5 days after embryo transfer). Red arrows indicate implantation sites and black arrows indicate ovaries. b Comparison of implantation rate between Con and GH groups (n = 4, respectively). Chi-square test. c Comparison of litter size after embryo transfer between Con group (n = 5) and GH group (n = 6). Normal data distribution, Student’s t test. *P <0 .05, ***P < 0.001. Con, control; GH, growth hormone
Discussion
The supplementation of IVM culture medium with GH had a positive effect on pregnancy outcomes in the mouse model. Although there was no increase in the maturation rate and 2-cell embryo rate, exogenous GH could enhance oocyte quality, blastocyst rate, and blastocyst quality. Furthermore, the implantation rate and litter size after embryo transfer were improved after the addition of GH.
Our results on the maturation rate after the addition of GH into IVM culture medium are inconsistent with those of previous studies [19,20,21,22]. Although there was no improvement in oocyte maturation, mitochondrial function was enhanced in oocytes exposed to GH, as shown by an elevated mitochondrial membrane potential and an increased ATP level. Mitochondrial function is an index of both cytoplasmic maturation and oocyte quality. During oocyte maturation, there is extensive cytoskeletal reorganization and mitochondrial redistribution, and a high ATP level is required to meet the cells’ demands for energy [26]. Mitochondrial dysfunction can negatively affect oocyte competence and embryo development [27]. In our study, exogenous GH reduced the proportion of abnormal spindles, possibly by promoting mitochondrial function, as mitochondria have been reported to support spindle assembly [28].
Equally important, GH could enhance cytoplasmic maturity, thereby promoting the developmental capacity of oocytes. Thus, exogenous GH improved both blastocyst formation and blastocyst quality reflected by higher cell number of ICM and total cell number, consistent with the results of Shirazi et al. [23] and Mtango et al. [24]. In another study, Pozzobon et al. [17] revealed no improvement in the rates of bovine embryo cleavage and embryo production, although the embryo hatching rate was significantly higher in the IVM culture medium supplemented with GH. Presently, there is no study exploring the effects of GH supplementation on implantation and pregnancy outcomes after embryo transfer. We are the first to report that the addition of GH into IVM culture medium could significantly increase the implantation rate and litter size.
COCs, instead of denuded oocytes, were used in this study. Both oocytes and cumulus cells (CCs) have been reported to express GHR [29], and GH has been identified to play important roles in steroidogenesis and oocyte maturation through gap junctions between oocytes and surrounding CCs [30]. Cumulus expansion induced by GH associates with oocyte maturation [31, 32], and GH increases the kinetics of meiotic resumption in immature rat cumulus-enclosed oocytes, but not denuded oocytes [18]. As CCs can facilitate oocyte growth and development [33], most studies [16,17,18,19,20,21,22,23,24] employ COCs, instead of oocytes without CCs. Only one study [22] has reported the positive effect of GH on the maturation of denuded mouse oocytes; however, the results should be interpreted with caution as recombinant human GH was used, instead of recombinant mouse GH, and the maturation rate of control oocytes was only 44% after culturing for 27 h. By contrast, our study explored the effects of recombinant mouse GH on mouse COCs, and the oocyte maturation rate in both groups was about 81% after culturing for 14 h.
In this in vitro study, GH was added directly into the IVM culture medium of oocytes. In many clinical studies [11,12,13,14,15], GH was administrated systemically to patients that with poor response or with diminished ovarian reserve before oocyte retrieval. According to previous studies from previous studies [14, 15], the medication of systemically administered GH lasts from a few weeks to months, and many patients cannot adhere to the regimen due to the high cost and pain caused by the systemic administration of GH. In addition, systemically administered GH can act on the endometrium, instead of the ovaries, to influence pregnancy outcomes [34]. As reported by Cui et al. [35], GH affects endometrial cells to promote endometrial receptivity, thereby improving the pregnancy rate of patients with a thin endometrium. Lan et al. [36] demonstrated that GH could improve endometrial imaging during ultrasonography, enhance endometrial receptivity, and reduce the cycle cancellation rate in women older than 40 years. In these cases, it is difficult to conclude whether GH influences pregnancy outcomes by affecting oocytes or the endometrium. In humans, the effects of exogenous GH administration remain unknown, as the confounding factors have not yet been established. Presently, our knowledge on the effects of GH on oocyte maturation and subsequent oocyte development is mostly derived from in vitro studies of media supplementation.
According to the study of Stewart et al. [37], FBS has high concentration of GH and 50 nM GH could replace FBS as a component of the differentiation cocktail for cell culture. To study the confounding effect of the potential GH contained in FBS in the present study, we designed two groups for preliminary comparison. For the FBS group, COCs were cultured in the same medium as the Con group. For the non-FBS group, COCs were cultured in a similar medium, but 50 nM GH was supplemented instead of 10% FBS. The culture procedure was the same as described in this study. As a result of 5 replicated experiments, in FBS group, mature oocytes could be fertilized and developed into blastocyst. In the non-FBS group, however, almost no 2-cell-stage embryo was produced and no blastocyst was found after IVF. The FBS seems to be necessary for the culture and could not be replaced by GH in the IVM medium. Thus, a group with GH and without FBS was not designed in the present study. We also found that in previous studies researching the effect of GH supplementation in IVM culture system [18,19,20,21,22,23], the culture media were all supplemented with FBS or FCS or BSA. The confounding effect of FBS in the study might be limited.
To our best knowledge, this is the first study to investigate the effects of GH supplementation in the IVM culture medium on pregnancy outcomes after embryo transfer. We found that exogenous GH supplementation in vitro could improve oocyte quality, embryo development, implantation, and live births. These findings provide compelling evidence for the use of exogenous GH in improving in vitro culture systems of human oocytes. A recent study evaluated the effects of GH in denuded immature human oocytes and reported that this hormone could promote oocyte maturation and the expression of genes associated with embryo development [8]. These results should be confirmed in future studies with immature human cumulus–oocyte complex.
In conclusion, the supplementation of IVM culture medium with GH could not enhance the maturation rate of mouse oocytes. However, it improved embryo development and pregnancy outcomes, probably by enhancing mitochondrial function in oocytes.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
References
Dahan MH, Tan SL, Chung J, Son WY. Clinical definition paper on in vitro maturation of human oocytes. Hum Reprod. 2016;31(7):1383–6. https://doi.org/10.1093/humrep/dew109.
Nogueira D, Sadeu JC, Montagut J. In vitro oocyte maturation: current status. Semin Reprod Med. 2012;30(3):199–213. https://doi.org/10.1055/s-0032-1311522.
Yu Y, Yan J, Li M, Yan L, Zhao Y, Lian Y, et al. Effects of combined epidermal growth factor, brain-derived neurotrophic factor and insulin-like growth factor-1 on human oocyte maturation and early fertilized and cloned embryo development. Hum Reprod. 2012;27(7):2146–59. https://doi.org/10.1093/humrep/des099.
Peluffo MC, Ting AY, Zamah AM, Conti M, Stouffer RL, Zelinski MB, et al. Amphiregulin promotes the maturation of oocytes isolated from the small antral follicles of the rhesus macaque. Hum Reprod. 2012;27(8):2430–7. https://doi.org/10.1093/humrep/des158.
Tkachenko OY, Delimitreva S, Heistermann M, Scheerer-Bernhard JU, Wedi E, Nayudu PL. Critical estradiol dose optimization for oocyte in vitro maturation in the common marmoset. Theriogenology. 2015;83(8):1254–63. https://doi.org/10.1016/j.theriogenology.2015.01.012.
Mota GB, Oliveira e Silva I, de Souza DK, Tuany F, Pereira MM, Camargo LSA, et al. Insulin influences developmental competence of bovine oocytes cultured in α-MEM plus follicle-simulating hormone. Zygote (Cambridge, England). 2015;23(4):563–72. https://doi.org/10.1017/S0967199414000239.
Vuong LN, Le AH, Ho VNA, Pham TD, Sanchez F, Romero S, et al. Live births after oocyte in vitro maturation with a prematuration step in women with polycystic ovary syndrome. J Assist Reprod Genet. 2020;37(2):347–57. https://doi.org/10.1007/s10815-019-01677-6.
Li Y, Liu H, Yu Q, Liu H, Huang T, Zhao S, et al. Growth hormone promotes maturation of human oocytes. Front Endocrinol. 2019;10:485. https://doi.org/10.3389/fendo.2019.00485.
Mendoza C, Ruiz-Requena E, Ortega E, Cremades N, Martinez F, Bernabeu R, et al. Follicular fluid markers of oocyte developmental potential. Hum Reprod. 2002;17(4):1017–22.
Hou H-Y, Wang X, Yu Q, Li H-Y, Li S-J, Tang R-Y, et al. Evidence that growth hormone can improve mitochondrial function in oocytes from aged mice. Reproduction (Cambridge, England). 2018;157(4):345–58. https://doi.org/10.1530/REP-18-0529.
Weall BM, Al-Samerria S, Conceicao J, Yovich JL, Almahbobi G. A direct action for GH in improvement of oocyte quality in poor-responder patients. Reproduction (Cambridge, England). 2015;149(2):147–54. https://doi.org/10.1530/REP-14-0494.
Eftekhar M, Aflatoonian A, Mohammadian F, Eftekhar T. Adjuvant growth hormone therapy in antagonist protocol in poor responders undergoing assisted reproductive technology. Arch Gynecol Obstet. 2013;287(5):1017–21. https://doi.org/10.1007/s00404-012-2655-1.
Yovich JL, Stanger JD. Growth hormone supplementation improves implantation and pregnancy productivity rates for poor-prognosis patients undertaking IVF. Reprod BioMed Online. 2010;21(1):37–49. https://doi.org/10.1016/j.rbmo.2010.03.013.
Zhu J, Wang Y, Chen L, Liu P, Li R, Qiao J. Growth hormone supplementation may not improve live birth rate in poor responders. Front Endocrinol. 2020;11:1. https://doi.org/10.3389/fendo.2020.00001.
Chen Y, Tao L, Lin Y, Li X, Ma C. Outcomes of fertilization-embryo transfer in women with diminished ovarian reserve after growth hormone pretreatment. Gynecol Endocrinol. 2020;36:1–4. https://doi.org/10.1080/09513590.2020.1737005.
Izadyar F, Colenbrander B, Bevers MM. In vitro maturation of bovine oocytes in the presence of growth hormone accelerates nuclear maturation and promotes subsequent embryonic development. Mol Reprod Dev. 1996;45(3):372–7. https://doi.org/10.1002/(SICI)1098-2795(199611)45:3<372::AID-MRD15>3.0.CO;2-0.
Pozzobon SE, Lagares MA, Brum DS, Leivas FG, Rubin MIB. Addition of recombinant human growth hormone to in vitro maturation medium of bovine oocytes. Reprod Domest Anim. 2005;40(1):19–22.
Apa R, Lanzone A, Miceli F, Mastrandrea M, Caruso A, Mancuso S, et al. Growth hormone induces in vitro maturation of follicle- and cumulus-enclosed rat oocytes. Mol Cell Endocrinol. 1994;106(1-2):207–12.
Pereira GR, Lorenzo PL, Carneiro GF, Bilodeau-Goeseels S, Kastelic JP, Esteller-Vico A, et al. Selection of developmentally competent immature equine oocytes with brilliant cresyl blue stain prior to in vitro maturation with equine growth hormone. Zygote. 2014;22(4):500–4. https://doi.org/10.1017/S096719941200072X.
Pereira GR, Lorenzo PL, Carneiro GF, Ball BA, Bilodeau-Goeseels S, Kastelic J, et al. The involvement of growth hormone in equine oocyte maturation, receptor localization and steroid production by cumulus-oocyte complexes in vitro. Res Vet Sci. 2013;95(2):667–74. https://doi.org/10.1016/j.rvsc.2013.06.024.
Marchal R, Caillaud M, Martoriati A, Gérard N, Mermillod P, Goudet G. Effect of growth hormone (GH) on in vitro nuclear and cytoplasmic oocyte maturation, cumulus expansion, hyaluronan synthases, and connexins 32 and 43 expression, and GH receptor messenger RNA expression in equine and porcine species. Biol Reprod. 2003;69(3):1013–22.
Kiapekou E, Loutradis D, Drakakis P, Zapanti E, Mastorakos G, Antsaklis A. Effects of GH and IGF-I on the in vitro maturation of mouse oocytes. Hormones (Athens, Greece). 2005;4(3):155–60.
Shirazi A, Shams-Esfandabadi N, Ahmadi E, Heidari B. Effects of growth hormone on nuclear maturation of ovine oocytes and subsequent embryo development. Reprod Domest Anim. 2010;45(3):530–6. https://doi.org/10.1111/j.1439-0531.2008.01290.x.
Mtango NR, Varisanga MD, Dong YJ, Rajamahendran R, Suzuki T. Growth factors and growth hormone enhance in vitro embryo production and post-thaw survival of vitrified bovine blastocysts. Theriogenology. 2003;59(5-6):1393–402.
Liu Y, Han M, Li X, Wang H, Ma M, Zhang S, et al. Age-related changes in the mitochondria of human mural granulosa cells. Hum Reprod. 2017;32(12):2465–73. https://doi.org/10.1093/humrep/dex309.
Coticchio G, Dal Canto M, Mignini Renzini M, Guglielmo MC, Brambillasca F, Turchi D, et al. Oocyte maturation: gamete-somatic cells interactions, meiotic resumption, cytoskeletal dynamics and cytoplasmic reorganization. Hum Reprod Update. 2015;21(4):427–54. https://doi.org/10.1093/humupd/dmv011.
Van Blerkom J. Mitochondrial function in the human oocyte and embryo and their role in developmental competence. Mitochondrion. 2011;11(5):797–813. https://doi.org/10.1016/j.mito.2010.09.012.
Dalton CM, Carroll J. Biased inheritance of mitochondria during asymmetric cell division in the mouse oocyte. J Cell Sci. 2013;126(Pt 13):2955–64. https://doi.org/10.1242/jcs.128744.
Bevers MM, Izadyar F. Role of growth hormone and growth hormone receptor in oocyte maturation. Mol Cell Endocrinol. 2002;197(1-2):173–8.
Hull KL, Harvey S. Growth hormone and reproduction: a review of endocrine and autocrine/paracrine interactions. Int J Endocrinol. 2014;2014:234014–24. https://doi.org/10.1155/2014/234014.
Kölle S, Stojkovic M, Boie G, Wolf E, Sinowatz F. Growth hormone-related effects on apoptosis, mitosis, and expression of connexin 43 in bovine in vitro maturation cumulus-oocyte complexes. Biol Reprod. 2003;68(5):1584–9.
de Prada JKN, VandeVoort CA. Growth hormone and in vitro maturation of rhesus macaque oocytes and subsequent embryo development. J Assist Reprod Genet. 2008;25(4):145–58. https://doi.org/10.1007/s10815-008-9208-3.
Da Broi MG, Giorgi VSI, Wang F, Keefe DL, Albertini D, Navarro PA. Influence of follicular fluid and cumulus cells on oocyte quality: clinical implications. J Assist Reprod Genet. 2018;35(5):735–51. https://doi.org/10.1007/s10815-018-1143-3.
Liu F-T, Wu Z, Yan J, Norman RJ, Li R. The potential role of growth hormone on the endometrium in assisted reproductive technology. Front Endocrinol. 2020;11:49. https://doi.org/10.3389/fendo.2020.00049.
Cui N, Li AM, Luo ZY, Zhao ZM, Xu YM, Zhang J, et al. Effects of growth hormone on pregnancy rates of patients with thin endometrium. J Endocrinol Investig. 2019;42(1):27–35. https://doi.org/10.1007/s40618-018-0877-1.
Lan K-C, Lin P-Y, Chang Y-C, Chen Y-J, Tsai Y-R, Ismaeil Mohamed IS, et al. Growth hormone supplementation may improve the pregnancy rate and endometrial receptivity among women aged more than 40 years undergoing in vitro fertilization. Biom J. 2019;42(6):411–6. https://doi.org/10.1016/j.bj.2019.05.003.
Stewart WC, Baugh JE Jr, Floyd ZE, Stephens JM. STAT 5 activators can replace the requirement of FBS in the adipogenesis of 3T3-L1 cells. Biochem Biophys Res Commun. 2004;324(1):355–9. https://doi.org/10.1016/j.bbrc.2004.09.053.
Acknowledgements
The authors thank Tianjie Li, Qingyuan Qin, and Qianying Guo for the help in the study and thank International Science Editing for their help in improving the quality of English written.
Code Availability
Not applicable.
Funding
This work was supported by the National Key Research & Developmental Program of China (2017YFC1001504), Key Clinical Program of Peking University Third Hospital (BYSY2015002), and National Key Research & Developmental Program of China (2018YFC1003802).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Institutional Animal Welfare and Ethics Committee Policies of Peking University Health Science Center (protocol no. LA2018256). The approval file has been uploaded.
Consent to Participate
Not applicable.
Consent for Publication
All authors participated in the research and were qualified to be listed as co-authors. The manuscript has been approved by all authors for publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, Y., Xie, B., Li, X. et al. Supplementation of the In Vitro Maturation Culture Medium of Mouse Oocytes with Growth Hormone Improves Pregnancy Outcomes. Reprod. Sci. 28, 2540–2549 (2021). https://doi.org/10.1007/s43032-021-00507-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00507-4