Abstract
The aim of this study was to investigate the effect of delaying maturation by extended culture of immature bovine oocytes in prematuration medium (PMC) containing single maturation inhibitor on their meiotic resumption and embryonic development. Bovine immature oocytes were cultured in M199 containing 10 μM of either inhibitor (roscovitine, cilostamide, or forskolin) for either 72 or 120 h followed by up to 48 h in maturation media supplemented with 7.5 IU follicle-stimulating hormone (FSH)/luteinizing hormone (LH). Two control groups were used. In untreated control, immature oocytes were cultured in the same medium as the experimental group without any inhibitors. In the FSH/LH control group, oocytes were cultured directly in the maturation medium supplemented with FSH/LH up to 48 h. In vitro matured oocytes were then inseminated with frozen–thawed bull sperm. Fertilization, defined as two-cell division 48 h post-insemination, and blastocyst formation were recorded. Total maturation rate for the 72-h group was 73%, 70%, 66%, and 69% for roscovitine, forskolin, cilostamide, and FSH/LH control, respectively, with no significant difference indicating that inhibitors have no negative effect on the oocyte maturation rate. The total fertilization rate for the 72-h group revealed that cilostamide (47%) and roscovitine (35%) were significantly higher than FSH/LH control (20%). The total blastocyst formation rates per inseminated oocytes revealed that among treatment groups, roscovitine (20%) had significantly higher rate than forskolin (9%). Overall, 72-h exposure period had better outcomes than 120 h in all the treated groups. In conclusion, prematuration culture of the bovine oocytes in the presence of maturation inhibitor for 72-h period at 10 μM concentration is sufficient in improving the bovine oocyte developmental competence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro maturation of oocytes (IVM) has been offered as an alternative to the traditional controlled ovarian stimulation and in vitro fertilization. However, in vivo matured oocytes are more competent than in vitro matured ones in producing better quality embryos and hence higher pregnancy outcome (Trounson et al. 2001). Competent oocytes have synchronized nuclear and cytoplasmic maturation, a necessary process for successful fertilization and subsequent developments (Edwards 1965a).
Cytoplasmic maturation, a poorly understood physiological process, supports the fertilization of the oocyte and early embryonic development. This process comprises accumulation of mRNA and proteins, redistribution of the organelles, and cellular metabolic changes during preovulatory follicle stage (Edwards 1965b). The morphological nuclear maturation alone does not necessarily indicate cytoplasmic maturation, hence developmental competence.
In vitro maturation of oocytes retrieved from the antral follicles has a shorter period of growth than preovulatory follicles in the conventional in vitro fertilization (IVF) (Miller et al. 2000; Teissier et al. 2000; Cekleniak et al. 2001). During the preovulatory period, oocyte meiosis resumption is dependent on the level of cyclic adenosine monophosphate (AMP), produced by somatic granulosa cells and passed through the gap junctions to inhibit premature resumption (Mehlmann 2005). Cyclic AMP activates the cAMP-dependent protein kinase (PKA) by releasing two active catalytic subunits (Rose-Hellekant and Bavister 1996).
Maintaining high level of oocyte intracellular cAMP is facilitated by two mechanisms of production of cAMP, and prevention of its degradation. cAMP analogues (dbcAMP) (Kim et al. 2008), adenlylate cyclase activators (forskolin) (Bilodeau et al. 1993; Shu et al. 2008), and invasive adenyl cyclase (Aktas et al. 1995a, b) was used in production of intracellular cAMP during in vitro maturation of oocyte to maintain intracellular cAMP. These studies were able to show that high level of cAMP and PKA is responsible for preventing meiotic resumption. Phosphodiesterase enzyme inhibitor family including (cilostamide, milirnone, and Org9935) has shown to effectively maintain high level of intracellular cAMP by preventing its degradation by phosphodiesterase enzyme, hence attenuating meiotic resumption in porcine (Laforest et al. 2005), mouse (Tsafriri et al. 1996; Nogueira et al. 2003a), macaque (Jensen et al. 2002), bovine (Mayes and Sirard 2002; Albuz et al. 2010), and human oocytes (Nogueira et al. 2003b).
Ovulation by rupturing of the leading follicle in response to gonadotropin surge is associated with nuclear maturation by resumption of meiosis which is characterized by germinal vesicle breakdown (GVBD) and extrusion of first polar body. The nuclear maturation process is controlled by activity of the maturation-promoting factor (MPF). MPF plays an important role in GVBD, chromatin condensation, formation, and organization of microtubules (Brunet and Maro 2005). Multiple phosphorylation cascades and second messenger signaling pathways triggered by gonadotropin surge are very important for oocyte maturation. These phosphorylation cascades are activated by MPF and mitogen-activated protein kinase (MAPK) which is believed to be involved in chromatin condensation and microtubule formation (Fan and Sun 2004).
MPF levels fluctuate throughout the maturation process: it reaches to the highest levels at the time of GVBD and the end of first meiotic division to maintain metaphase II stage till sperm penetration (Sugiura et al. 2006). Roscovitine is a meiotic inhibitor that blocks MPF activation and can maintain the GVBD for 24–66 h (Oussaid et al. 2000; Coy et al. 2005a). It has been shown that roscovitine has no harmful effect on the embryonic and fetal development of animals (Coy et al. 2005a, b; Choi et al. 2006).
Accelerated nuclear maturation is a major problem in the IVM field when the oocytes are subjected to the in vitro environment, resulting in 24–48-h maturation following in vitro culture which may be responsible for poor outcome for downstream fertility treatments. Therefore, the aim of this study is to evaluate the effect of slowing the maturation process to better mimic the in vivo milieu utilizing maturation inhibitors including cilostamide, forskolin and roscovitine (maturation) inhibitors for 72 or 120 h prior to culturing in maturation medium to investigate the effect of extended prematuration culture on the maturation rate and subsequent development.
Materials and Methods
Oocyte source.
Immature bovine oocytes were purchased from Applied Reproductive Technology Company (Madison, WI). They were aspirated from early antral follicles (2–6 mm) and selected based on compactness of cumulus. A total of 1,133 were shipped to our institution in pre-labeled tubes containing the meiotic inhibitors incubated at 37°C. Incubation during shipment was included total PMC period.
Twenty-five to 30 oocytes were used in each group, and the experiment was replicated four times to achieve the targeted sample size for each group.
Chemicals and reagents.
All inhibitors were purchased from Sigma-Aldrich (St. Louis, MO). M199 medium (Invitrogen, Carlsbad, CA) supplemented with 10% serum protein substitute (Origio, Trumbull, CT) and 100 U/ml penicillin and 100 μg/ml streptomycin (Pen Strep, Invitrogen) was used as base medium. Prematuration culture medium (PCM) consisted of base medium containing a final concentration of 10 μM of one of meiotic inhibitors of phosophodiesterase 3A (cilostamide), adenylate cyclase activator (forskolin), and MPF inhibitor (roscovitine). The complete maturation medium (CMM) was base medium containing 7.5 IU follicle-stimulating hormone (FSH)/luteinizing hormone (LH) (Menopure) (Ferring, San Diego, CA).
Experimental design.
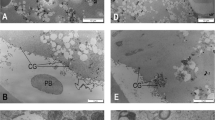
The immature oocytes were cultured in PMC containing either of each inhibitor (total of three PMC cultures) for either 72 or 120 h before culturing in CMM in a 37°C and 5.5% CO2 in humidified air for 48 h. There were two controls. In untreated control (inhibitor-free) group, the immature oocytes were cultured in base medium for same PMC duration, while in FSH/LH control group, they were cultured in CMM medium for up to 48 h. Following CMM culture, the oocytes were checked for maturity, and those matured oocytes were inseminated with frozen–thawed bull sperm overnight (COBA Inc., Columbus, OH). Maturation was defined by cumulus expansion and extrusion of first polar body. The inseminated oocytes were washed from sperm and denuded mechanically to remove cumulus cell and culture in base medium for 24 h. They were then checked for fertilization, defined as two-cell embryos. It is very difficult to visualize pronuclear formation (as a sign of fertilization) in unstained bovine oocyte as cytoplasm is dark brown. The two-cell embryos were then cultured for 8 d, and their development into blastocysts was monitored. Cleaved embryos were transferred to a fresh cleavage media every 2 d (Fig. 1). The whole culture period was under 37°C and 5.5% CO2 in humidified air incubators.
Statistical analysis.
Chi-square and Fischer’s exact test statistical analysis were used to evaluate differences between groups using Vassarstats website for statistical analysis (http://faculty.vassar.edu/lowry/VassarStats.html). The significance level of the test was targeted at 0.05 (P value is <0.05). The sample size was calculated using the two-sided Z test with pooled variance.
Results
A total of 1,133 cumulus-enclosed bovine oocytes were used in this study to evaluate the effect of 72- and 120-h exposure to either maturation inhibitors of roscovitine, cilostamide, or forskolin on the in vitro maturation outcome of the immature oocytes.
Maturation rates of the oocytes after exposure to the meiotic inhibitors.
Spontaneous maturation (matured while oocyte exposed to inhibitors), maturation (at 24 and 48 h) in complete maturation medium, total maturation (combination of maturation at 24 and 48 h), and overall maturation (spontaneous maturation + total maturation) were monitored in this study.
Spontaneous maturation.
The efficacy of the meiotic inhibitors was evaluated by monitoring spontaneous maturation rate of immature oocyte following exposure to meiotic inhibitor prior to culturing in maturation media (Table 1). There was no significant difference in spontaneous maturation rate among inhibitors groups at 72-h exposure; however, when compared to non-treated control, all inhibitors groups had a significant lower rate of spontaneous maturation indicating their effectiveness in maintaining meiotic arrest of immature oocyte (P < 0.05).
Spontaneous maturation for 120-h exposure groups showed no significant difference between treatment groups. However, untreated control had significantly higher rates indicating the inhibitors’ effectiveness to attenuate the maturation process (P < 0.05; Table 2).
Comparing each inhibitor at two different time exposures of 72 and 120 h (Tables 1 and 2) revealed no significant difference for cilostamide and forskolin (P > 0.05). However, exposure to roscovitine for 72 h had significantly higher efficacy than 120 h (P = 0.006).
Maturation.
Following prematuration culture (72 or 120 h), immature oocytes were cultured in CMM medium for up to 48 h. In the 72-h PMC period, roscovitine group had a significantly higher maturation rate than all treatments and control groups at 24-h culture (Fig. 2; P < 0.05).
Total maturation rate and maturation rate (at 24 and 48 h) of oocyte cultured for 72 h in prematuration culture containing either inhibitor. Total maturation rate was 73%, 66%, and 70% for roscovitine, cilostamide, and forskolin with no significant difference (P > 0.05). Roscovitine (55%) had significantly higher maturation rate at 24 h than cilostamide (40%) and forskolin (43%) (P < 0.05). There was no significant difference in maturation rate at 48 h between roscovitone (17%), cilostamide (26%), and forskolin (26%) (P > 0.05).
Cilostamide, forskolin, and FSH/LH control had significantly higher maturation rate than the untreated control at 48-h culture (P < 0.05). However, these rates are not significant when compared to roscovitone (P > 0.05; Table 1). In the 120-h PMC period, oocyte maturation rate in the first 24 h of CMM culture, roscovitine- and cilostamide-treated groups were significantly lower than FSH/LH-treated control (P < 0.05). However, it was not significantly different with forskolin (P > 0.05; Fig. 3).
Total maturation rate and maturation rate (at 24 and 48 h) of oocyte cultured for 120 h in prematuration culture in the presence of either inhibitors. Cilostamide (70%) had a significant higher total maturation rate than forskolin (57%; P < 0.05); however, this rate was not significant when compared with roscovitine (60%; P > 0.05). There was not a significant difference in maturation rate at 24 h for roscovitine (33%), cilostamide (36%), and forskolin (37%; P > 0.05). Cilostamide (37%) had significantly higher maturation rate than Foraskolin (19%) at 48 (P < 0.05). However, it was not significant with Roscovitin (27%) (P > 0.05).
The maturation rate at 48 h CMM after 120 h PMC for cilostamide group was significantly higher than both FSH/LH and untreated controls (P < 0.05). However, roscovitine and forskolin groups were not significantly different from the FSH/LH group.
The maturation rate of the cilostamide group was significantly higher than forskolin (P < 0.05). However, there was no significant difference between roscovitine and cilostamide or forskolin (P > 0.05).
Roscovitine had a significantly higher maturation rate in the 24 h of the 72-h period than the 120 h (P = 0.001). There was no significant difference in maturation rate following 24-h CMM culture for cilostamide and forskolin 72- and 120-h groups (P > 0.05; Table 3).
Roscovitine- and cilostamide-treated group for 120 h had significantly higher maturation rate at 48 h than 72-h period (17 and 26%; P < 0.05). On the other hand, forskolin group had lower rate for 120 h than 72-h group with no significant difference (P > 0.05).
Total maturation.
Total maturation rate was defined as combined maturation at 24- and 48-h CMM culture. There was no significant difference in maturation rate for the 72-h experimental and control groups indicating that inhibitors have no negative effect on the oocyte maturation rate (P > 0.05; Table 1).
In 120-h exposure group, cilostamide had a significant higher rate of maturation than forskolin (P < 0.05); however, this rate was not significant when compared with roscovitine (P > 0.05). FSH/LH control has highest maturation rate among all groups, although it is not significant if compared with cilostamide (P > 0.05), indicating that longer prematuration culture (120 h) may have adverse effect on the meiotic resumption rather than 72 h (Table 2).
Evaluation of the effect of each inhibitor on total maturation at the different exposure time revealed that roscovitine and forskolin had significantly higher rate at 72 h than 120 h (P < 0.05; Fig. 4). However, there was no significant difference between 72- and 120-h time exposure duration for cilostamide (P > 0.05; Table 3).
Comparison of total maturation at 72 and 120 h for each inhibitor. Roscovitine (73%) and forskolin (70%) had significantly higher total maturation rate at 72 h than 120 h (60 and 57% respectively) (P < 0.05). There was no significant difference in this rate for cilostamide between 72-h (66%) and 120-h (70%) time exposure period (P > 0.05).
Overall maturation.
Overall maturation rate, defined as summation of spontaneous and total maturation, in 72-h time exposure was significantly lower for FSH/LH control in comparison with cilostamide, roscovitine, forskolin, and untreated control groups (P < .005; Table 1). We did not attempt to evaluate the competency of the spontaneously matured oocytes.
In 120-h exposure time, the overall maturation rate of the FSH/LH-treated control was significantly lower than the all treated control groups (P < 0.05). However, the overall maturation of the roscovitine and cilostamide groups was significantly higher than the untreated control (P < 0.05; Table 2).
There was no difference in the overall maturation of each treatment and control groups between 72- and 120-h exposure duration (P < 0.05).
Oocyte wastage.
Some of the oocytes did not resume meiosis, arrested, cleaved, or degenerated; they were considered wastage (original number of oocyte minus overall matured). Our data shows that FSH/LH control had significantly high oocyte wastage that other treatment and untreated group in 72-h exposure time. Among treatment groups, cilostamide had higher oocyte wastage than roscovitine and forskolin with no significant difference (P > 0.05; Table 1).
In 120-h time exposure, there was no significant difference in oocyte wastage among experimental groups (P > 0.05). However, roscovitine had significantly lower oocyte wastage rate than FSH/LH-treated and untreated controls (P < 0.05). Comparison of each treatment group between two exposure times (72 and 120 h) reveled no significant difference in oocyte wastage rate.
Fertilization rates.
Matured oocytes were inseminated following 24- or 48-h culture in CMM according to their maturity. In 72-h exposure time, cilostamide had significantly higher fertilization rate than roscovitine, and FSH/LH control groups among the oocytes matured at 24 h (P > 0.05; Table 3). However, this rate was not significant in comparison with forskolin. For those oocytes matured at 48 h, cilostamide and roscovitine had significantly higher fertilization rate than FSH/LH. However, it was not significant with forskolin (Table 4).
Evaluating total fertilization rate (total number of fertilized egg per total number of inseminated at 24 and 48 h) revealed that cilostamide and roscovitine were significantly higher than FSH/LH control (P < 0.05). Among treatment groups, cilostamide was significantly higher than forskolin; however, it was not significant in comparison with roscovitine.
In 120-h exposure time, roscovitine had significantly higher fertilization rate than treatment groups of cilostamide and forskolin and FSH/LH control (P < 0.05; Table 4) among oocytes matured at 24 h CMM culture. This rate was not significant between all treatment and FSH/LH control groups (P > 0.05) for oocytes matured at 48 h.
Total fertilization rate for roscovitine was significantly higher than treatment and FSH/LH control groups (P < 0.05; Table 5).
Comparing each treatment group between two time exposures of 72 and 120 h revealed that roscovitine had significantly higher fertilization rate in 120-h exposure time than 72 h for those matured at 24 h (P < 0.05; Table 5). This rate was not significantly different for oocytes matured at 48 h between 72- and 120-h time exposure (P > 0.05). There was no significant difference in total fertilization rate between these two time exposures (P > 0.05). Cilostamide, on the other hand, had significantly higher fertilization rate at 24 h, 48 h, and total fertilization in 72 h than 120-h exposure time (P < 0.05; Table 5). There were no significant differences in fertilization rates at 24 h, 48 h, and total fertilization for 72-h exposure time when compared to 120-h exposure time in forskolin treatment group (P > 0.05; Table 6).
Blastocyst formation.
The blastocyst formation rate was calculated based on fertilized and inseminated oocyte according to their maturation timing (24 and 48 h). Total blastocyst formation rate referred to the combination of blastocyst formation at 24 and 48 h.
In 72-h exposure time, blastocyst formation (24 and 48 h) rate per fertilized oocytes was not significantly different among roscovitine, cilostamide, forskolin, and FSH/LH control (P > 0.05; Table 7). The total blastocyst rate per fertilized oocytes was not significantly different between all treatments and control groups (P > 0.05).
The blastocyst formation rate per inseminated oocytes at 24 and 48 h was not significant among treatments and control groups (P > 0.05; Table 7). Analyzing the total blastocyst formation rates per inseminated oocytes revealed that among treatment groups, roscovitine had significantly higher rate than forskolin (P < 0.05). However, there was no significant difference between cilostamide and forskolin groups (P > 0.05). Both roscovitine and cilostamide were significantly higher when compared with FSH/LH (P < 0.05).
In 120-h exposure period, the blastocyst formation rate per fertilized oocytes at 24 h was not significantly different among roscovitine, cilostamide, forskolin, and FSH/LH control (P < 0.05; Table 8). This rate was not significantly different between roscovitine, cilostamide, and FSH/LH control groups for those oocytes inseminated at 48 h. There was no embryo developed to blastocyst in forskolin treatment group at 48 h. Total blastocyst rate per fertilized oocytes was not significantly different between all treatments and control groups (P > 0.05).
Blastocyst formation rate per inseminated oocytes at 24 h was not significantly different among all treatments and control groups (P < 0.05; Table 9). This rate was not significantly different between treatments and control groups for those inseminated at 48 h. Total blastocyst rate per inseminated oocytes was significantly different between roscovitine and forskolin (P < 0.05); however, this rate was not significant in comparison with cilostamide and FSH/LH controls (P > 0.05).
Comparing the blastocyst formation rates (per fertilized and per inseminated oocyte) for each inhibitor between two exposure times of 72 and 120 h revealed no significant difference for 24 h, 48 h, and total rate (P > 0.05; Tables 9 and 10).
Discussion
The final steps of in vivo oocyte development are still a mystery; understanding of these steps might be the key element in developing an optimum IVM culture system. In human, the implantation failure and miscarriage rates in IVM cycles are higher than conventional IVF cycles (Nogueira et al. 2003b, 2006; Jurema and Nogueira 2006). It is postulated that poor early embryonic development is related to incorrect microtubule and chromatin condensation in addition to abnormal activation of the embryonic genome (Combelles et al. 2002; Schramm et al. 2003).
In vitro matured oocytes presumably have an incomplete maturation due to deficiency of full cytoplasmic maturation (Mayes et al. 2007) which could be the explanation of the clinical unsatisfactory outcome. Consequently, extending meiotic arrest period by utilizing meiotic inhibitors may be beneficial for nuclear and cytoplasmic synchrony (Lonergan et al. 1997; Avery et al. 1998; Nogueira et al. 2003a).
In the present study, three types of meiotic inhibitors were used in PMC (phase I) for 72 or 120 h followed by up to 48 h of CMM (phase II) culture. The forskolin inhibitor is adenylate cycle enzyme activator which is responsible for synthesis of the intracellular cAMP to maintain meiotic arrest by keeping the intracellular cAMP to the level that prevents the GVBD. In the bovine oocytes, the adenylate cyclase activity has been proven to be localized in cumulus cells and the plasma membrane, suggesting culturing intact cumulus oocyte complex (without denudation) may have better maturation outcome (Kuyt et al. 1988; Bilodeau et al. 1993; Nogueira et al. 2006).
Cilostamide, a phosphodiesterase (PDE) 3 A inhibitor (a specific PDE isoenzyme), inhibits the action of the PDE by functioning as active site competitor with lower side effects, preventing degradation of cAMP in the intracellular component. Cilostamide is effective in keeping the cumulus oocyte gap junctions intact, thus allowing more time for metabolic exchange between the oocytes and the media which is completely broken in the spontaneous maturation process (Thomas et al. 2004a, b; Albuz et al. 2010).
MPF is composed of the two catalytic subunits p43 and cdc2 in addition to a regulatory subunit cyclin B. The activation of this factor is by binding of the cyclin B to the cdc2 and phosphorylation of threonine 161 and tyrosine 15. Roscovitine is a cyclin-dependant kinase inhibitor that can suppress the activity of MPF by blocking the action of cyclin B. MPF has an effect on both early and late stages of maturation; addition of roscovitine to the culture media before GVBD and 24 h after GVBD showed meiotic controlling effect on the oocytes (Zhang et al. 2011).
Our data revealed that roscovitine (MPF inhibitor) has superiority over the other two inhibitors by having the highest maturation rates among, second best fertilization rate (after cilostamide), and highest blastocyst formation rates. Cilostamide (PDE-3A inhibitor) comes second in its maturation rate after roscovitine with better fertilization but lower blastocyst formation rates. However, forskolin comes in last among all inhibitors with poor maturation and developmental outcomes. It was observed that the FSH/LH control group had a higher oocyte wastage rate in comparison to all the treated groups which leads us to believe that the current IVM system (which does not utilize inhibitors) is not the optimal on evident by the oocyte wastage.
Our results indicated that 72-h prematuration culture period is more optimum than 120-h exposure due to better outcome in terms of meiotic resumption, fertilization, and blastocyst formation rates at 10 μM concentration of inhibitors.
Keeping the cumulus intact during the whole period of (PMC) has proved to be very effective as it plays a key role in either transporting or processing the inhibitory factors produced by the theca cell monolayer (Richard and Sirard 1996; Colleoni et al. 2004). Maintaining the high level of intracellular cAMP by exposing immature oocyte to adenylate cyclase activator (forskolin) or PDE-3A inhibitor points to possible cAMP role in regulating the meiotic process in the bovine oocytes (Hashimoto et al. 2002; Thomas et al. 2004b). It seems that concentration of 10 μM is sufficient to maintain meiotic arrest as there was no significant difference between 10 and 50 μM reported by Mario and Marc-André (2002) In human, Nogueira et al. reported 67% for both maturation and fertilization rates with intra-cytoplasmic sperm injection (ICSI) after a 24-h period of (PMC) (Nogueira et al. 2006) supporting the idea of temporary meiotic attenuation for human application. More recently, Yi-min Shu et al. extended the (PMC) period to 48 h and compared the effect of cilostamide, forskolin, and their combination on the IVM outcome of human oocytes in a controlled ovarian hyperstimulation cycles, reporting favorable effect of the combined treatment in terms of maturation rate (65.4%) and fertilization (76.4%) using ICSI over any of them alone (Shu et al. 2008). Mermillod et al. reported that no negative effect on the developmental outcome of oocytes after culture for 24 h with 25 μM roscovitine (Mermillod et al. 2000). Others reported adverse outcomes after exposure to higher concentration (>50 μM) for 24 h (Donnay et al. 2004; Kaedei et al. 2010). Coy et al. reported that roscovitine with doses ranging from 12.5 to 50 μM was not harmful in terms of zona pellucida hardening, nuclear maturation, fertilization, and blastocyst formation after culture for 48 h. However, they concluded that this period is not sufficient to improve the in vitro maturation outcome (Coy et al. 2005a) supporting our hypothesis to extend the duration of (PMC). Albuz et al. reported excellent results by 1–2-h culture of immature bovine oocyte harvested from intermediate antral follicle in the presence of adenylate cyclase activator (forskolin) and IBMX (a nonspecific PDE inhibitor), followed by cilostamide and FSH. They cultured in serum-free condition with 69% blastocyst formation rates (Albuz et al. 2010). In our study, we used oocyte from early antral follicle and cultured them in the presence of inhibitors in the PMC phase only (not the IVM phase) with lower maturation rate than Albuz et al. Our low maturation rate could be related to the source of oocyte as they were in earlier maturation and require longer time to mature.
It was observed in our study that 80% of the blastocysts resulted from oocytes matured at 24 h of culture in maturation medium suggesting that the earlier the oocytes resume meiosis the better developmental outcome. Our data shows that 120-h prematuration culture at 10 μM concentration of inhibitors may have a negative impact on the oocyte maturation rate at 24 h of CMM culture and require longer time to resume meiosis in comparison to 72-h period. We did not attempt to lower concentration of inhibitors for longer periods; however, it may have positive impact on the matured oocytes.
Prematuration culture of the bovine oocytes with maturation-promoting factor or phosphodiesterase-3A inhibitor for 72-h period at 10 μM concentration is sufficient in improving the bovine oocyte developmental competence. If applicable to human, this may improve the overall in vitro maturation outcome.
References
Aktas H, Wheeler MB, First NL, Leibfried-Rutledge ML (1995a) Maintenance of meiotic arrest by increasing [cAMP]i may have physiological relevance in bovine oocytes. J Reprod Fertil 105(2):237–245
Aktas H, Wheeler MB, Rosenkrans CF Jr, First NL, Leibfried-Rutledge ML (1995b) Maintenance of bovine oocytes in prophase of meiosis I by high [cAMP]i. J Reprod Fertil 105(2):227–235
Albuz FK, Sasseville M, Lane M, Armstrong DT, Thompson JG, Gilchrist RB (2010) Simulated physiological oocyte maturation (SPOM): a novel in vitro maturation system that substantially improves embryo yield and pregnancy outcomes. Hum Reprod 25(12):2999–3011
Avery B, Hay-Schmidt A, Hyttel P, Greve T (1998) Embryo development, oocyte morphology, and kinetics of meiotic maturation in bovine oocytes exposed to 6-dimethylaminopurine prior to in vitro maturation. Mol Reprod Dev 50(3):334–344
Bilodeau S, Fortier MA, Sirard MA (1993) Effect of adenylate cyclase stimulation on meiotic resumption and cyclic AMP content of zona-free and cumulus-enclosed bovine oocytes in vitro. J Reprod Fertil 97(1):5–11
Brunet S, Maro B (2005) Cytoskeleton and cell cycle control during meiotic maturation of the mouse oocyte: integrating time and space. Reproduction 130(6):801–811
Cekleniak NA, Combelles CM, Ganz DA, Fung J, Albertini DF, Racowsky C (2001) A novel system for in vitro maturation of human oocytes. Fertil Steril 75(6):1185–1193
Choi YH, Love LB, Varner DD, Hinrichs K (2006) Blastocyst development in equine oocytes with low meiotic competence after suppression of meiosis with roscovitine prior to in vitro maturation. Zygote 14(1):1–8
Colleoni S, Luciano AM, Gandolfi F (2004) Cumulus-oocyte communications in the horse: role of the breeding season and of the maturation medium. Reprod Domest Anim 39(2):70–75
Combelles CM, Cekleniak NA, Racowsky C, Albertini DF (2002) Assessment of nuclear and cytoplasmic maturation in in-vitro matured human oocytes. Hum Reprod 17(4):1006–1016
Coy P, Romar R, Payton RR, McCann L, Saxton AM, Edwards JL (2005a) Maintenance of meiotic arrest in bovine oocytes using the S-enantiomer of roscovitine: effects on maturation, fertilization and subsequent embryo development in vitro. Reproduction 129(1):19–26
Coy P, Romar R, Ruiz S (2005b) Birth of piglets after transferring of in vitro-produced embryos pre-matured with R-roscovitine. Reproduction 129(6):747–755
Donnay I, Faerge I, Grondahl C (2004) Effect of prematuration, meiosis activating sterol and enriched maturation medium on the nuclear maturation and competence to development of calf oocytes. Theriogenology 62(6):1093–1107
Edwards RG (1965a) Maturation in vitro of mouse, sheep, cow, pig, rhesus monkey and human ovarian oocytes. Nature 208(5008):349–351
Edwards RG (1965b) Maturation in vitro of human ovarian oocytes. Lancet 2(7419):926–929
Fan HY, Sun QY (2004) Involvement of mitogen-activated protein kinase cascade during oocyte maturation and fertilization in mammals. Biol Reprod 70(3):535–547
Hashimoto S, Minami N, Takakura R, Imai H (2002) Bovine immature oocytes acquire developmental competence during meiotic arrest in vitro. Biol Reprod 66(6):1696–1701
Jensen JT, Schwinof KM, Zelinski-Wooten MB, Conti M, DePaolo LV, Stouffer RL (2002) Phosphodiesterase 3 inhibitors selectively block the spontaneous resumption of meiosis by macaque oocytes in vitro. Hum Reprod 17(8):2079–2084
Jurema MW, Nogueira D (2006) In vitro maturation of human oocytes for assisted reproduction. Fertil Steril 86(5):1277–1291
Kaedei Y, Fujiwara A, Tanhira F (2010) Effect of roscovitine pretreatment on the meiotic maturation of bovine oocytes and their subsequant development after somatic cell nuclear transfer. Anim Vet Adv 9(22):2848–2853
Kim JS, Cho YS, Song BS (2008) Exogenous dibutyryl cAMP affects meiotic maturation via protein kinase A activation; it stimulates further embryonic development including blastocyst quality in pigs. Theriogenology 69(3):290–301
Kuyt JR, Kruip TA, de Jong-Brink M (1988) Cytochemical localization of adenylate cyclase in bovine cumulus-oocyte complexes. Exp Cell Res 174(1):139–145
Laforest MF, Pouliot E, Gueguen L, Richard FJ (2005) Fundamental significance of specific phosphodiesterases in the control of spontaneous meiotic resumption in porcine oocytes. Mol Reprod Dev 70(3):361–372
Lonergan P, Khatir H, Carolan C, Mermillod P (1997) Bovine blastocyst production in vitro after inhibition of oocyte meiotic resumption for 24 h. J Reprod Fertil 109(2):355–365
Mario AM, Marc-André S (2002) Effect of type 3 and type 4 phosphodiesterase inhibitors on the maintenance of bovine oocytes in meiotic arrest. Biol Reprod 66:180–184
Mayes MA, Sirard MA (2002) Effect of type 3 and type 4 phosphodiesterase inhibitors on the maintenance of bovine oocytes in meiotic arrest. Biol Reprod 66(1):180–184
Mayes MA, Laforest MF, Guillemette C, Gilchrist RB, Richard FJ (2007) Adenosine 5′-monophosphate kinase-activated protein kinase (PRKA) activators delay meiotic resumption in porcine oocytes. Biol Reprod 76(4):589–597
Mehlmann LM (2005) Stops and starts in mammalian oocytes: recent advances in understanding the regulation of meiotic arrest and oocyte maturation. Reproduction 130(6):791–799
Mermillod P, Tomanek M, Marchal R, Meijer L (2000) High developmental competence of cattle oocytes maintained at the germinal vesicle stage for 24 hours in culture by specific inhibition of MPF kinase activity. Mol Reprod Dev 55(1):89–95
Miller MA, Technau U, Smith KM, Steele RE (2000) Oocyte development in Hydra involves selection from competent precursor cells. Dev Biol 224(2):326–338
Nogueira D, Cortvrindt R, De Matos DG, Vanhoutte L, Smitz J (2003a) Effect of phosphodiesterase type 3 inhibitor on developmental competence of immature mouse oocytes in vitro. Biol Reprod 69(6):2045–2052
Nogueira D, Albano C, Adriaenssens T (2003b) Human oocytes reversibly arrested in prophase I by phosphodiesterase type 3 inhibitor in vitro. Biol Reprod 69(3):1042–1052
Nogueira D, Ron-El R, Friedler S (2006) Meiotic arrest in vitro by phosphodiesterase 3-inhibitor enhances maturation capacity of human oocytes and allows subsequent embryonic development. Biol Reprod 74(1):177–184
Oussaid B, Lonergan P, Khatir H (2000) Effect of GnRH antagonist-induced prolonged follicular phase on follicular atresia and oocyte developmental competence in vitro in superovulated heifers. J Reprod Fertil 118(1):137–144
Richard FJ, Sirard MA (1996) Effects of follicular cells on oocyte maturation. I: effects of follicular hemisections on bovine oocyte maturation in vitro. Biol Reprod 54(1):16–21
Rose-Hellekant TA, Bavister BD (1996) Roles of protein kinase A and C in spontaneous maturation and in forskolin or 3-isobutyl-1-methylxanthine maintained meiotic arrest of bovine oocytes. Mol Reprod Dev 44(2):241–249
Schramm RD, Paprocki AM, VandeVoort CA (2003) Causes of developmental failure of in-vitro matured rhesus monkey oocytes: impairments in embryonic genome activation. Hum Reprod 18(4):826–833
Shu YM, Zeng HT, Ren Z (2008) Effects of cilostamide and forskolin on the meiotic resumption and embryonic development of immature human oocytes. Hum Reprod 23(3):504–513
Sugiura K, Naito K, Endo T, Tojo H (2006) Study of germinal vesicle requirement for the normal kinetics of maturation/M-phase-promoting factor activity during porcine oocyte maturation. Biol Reprod 74(3):593–600
Teissier MP, Chable H, Paulhac S, Aubard Y (2000) Comparison of follicle steroidogenesis from normal and polycystic ovaries in women undergoing IVF: relationship between steroid concentrations, follicle size, oocyte quality and fecundability. Hum Reprod 15(12):2471–2477
Thomas RE, Armstrong DT, Gilchrist RB (2004a) Bovine cumulus cell-oocyte gap junctional communication during in vitro maturation in response to manipulation of cell-specific cyclic adenosine 3′,5′-monophosophate levels. Biol Reprod 70(3):548–556
Thomas RE, Thompson JG, Armstrong DT, Gilchrist RB (2004b) Effect of specific phosphodiesterase isoenzyme inhibitors during in vitro maturation of bovine oocytes on meiotic and developmental capacity. Biol Reprod 71(4):1142–1149
Trounson A, Anderiesz C, Jones G (2001) Maturation of human oocytes in vitro and their developmental competence. Reproduction 121(1):51–75
Tsafriri A, Chun SY, Zhang R, Hsueh AJ, Conti M (1996) Oocyte maturation involves compartmentalization and opposing changes of cAMP levels in follicular somatic and germ cells: studies using selective phosphodiesterase inhibitors. Dev Biol 178(2):393–402
Zhang DX, Park WJ, Sun SC (2011) Regulation of maternal gene expression by MEK/MAPK and MPF signaling in porcine oocytes during in vitro meiotic maturation. J Reprod Dev 57(1):49–56
Authors’ contributions
Tarek Farghaly, MD participated in study design, execution, analysis, manuscript drafting, and critical discussion. Prof. Essam-Aldein M. Khalifa, MD participated in the study design and manuscript drafting. Prof. Sayed M. Mostafa, MD participated in the study design and manuscript drafting. Mostafa Hussien, MD participated in the study design and manuscript drafting. Mohamed A. Bedaiwy, MD participated in the study design and manuscript drafting. Ali Ahmady, PhD, HCLD participated in study design, analysis, manuscript drafting, and critical discussion.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor: T. Okamoto
Rights and permissions
About this article
Cite this article
Farghaly, T., Khalifa, E., Mostafa, S. et al. The effect of temporary meiotic attenuation on the in vitro maturation outcome of bovine oocytes. In Vitro Cell.Dev.Biol.-Animal 51, 662–671 (2015). https://doi.org/10.1007/s11626-015-9878-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-015-9878-y