Abstract
Introduction
There are few lacunae in the Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) staging system for Carcinoma of cervix, as the patients are not assessed for lymph node as well as distant metastases, though these are important prognostic factors. Magnetic resonance imaging (MRI) as well as Flurodeoxy glucose positron emission tomography/computed tomography (FDG PET/CT) has been used for evaluation of local tumor extent and nodal as well as distant metastasis in case of cervical cancer.
Objectives
To compare the usefulness of MRI and FDG PET/CT for detection of parametrial involvement and lymph node metastasis in increasing the accuracy of staging of patients with cervical cancer.
Methods and Materials
In this prospective hospital-based study, 38 patients with cervical cancer were prospectively enrolled. Patients were studied in two groups; Group A (22 cases) included recently diagnosed cases for initial workup and base line staging (prior to any treatment). Group B (16 cases) included treated cases of cervical cancer, on follow-up, suspected clinically to have recurrence, at 6 months or more after completion of planned standard treatment. MRI and FDG PET/CT scan were performed within 1-week interval of each other for all enrolled patients. The criterion for lymph node metastases on MRI was size > 10 mm in short axis diameter and abnormal signal or contrast enhancement in parametrium for involvement. On FDG PET/CT, only areas with FDG uptake significantly higher than the background and FDG uptake visible on at least two consecutive axial slices were considered as positive for malignancy. MRI and FDG PET/CT findings were compared with histopathologic examination (HPE).
Results
Group A: On patient-based analysis, MRI versus FDG PET/CT sensitivity for detection of lymph node metastases was: 57 versus 86%, specificity was 71 versus 71% and diagnostic accuracy was 64 versus 78%, respectively. On lymph node-based analysis, MRI versus FDG PET/CT sensitivity was 50 versus 87%, specificity 98 versus 98 and diagnostic accuracy 97 versus 98%, respectively. The efficacy of MRI for detecting parametrial invasion was (sensitivity = 67%, specificity = 91%, diagnostic accuracy was 86%) and for FDG PET/CT was (sensitivity = 0%, specificity = 91%, diagnostic accuracy = 71%). The FIGO staging was found to be inaccurate in 21% cases. Group B: For local disease recurrence: MRI versus FDG PET/CT, the sensitivity was 83 versus 92%, specificity was 75 versus 75% and accuracy was 81 versus 87%. Sensitivity and accuracy of MRI was better than FDG PET/CT in detection of local disease recurrence. When MRI and FDG PET/CT were compared for detecting nodal recurrence, according to cases, the sensitivity was 83 versus 92%, specificity was 75 versus 75% and accuracy was 81 versus 87%. FDG PET/CT had higher sensitivity and accuracy than MRI in detection of lymph nodal recurrence.
Conclusion
FDG PET/CT is superior to MRI in detection of local as well as distant lymph node metastases. FDG PET/CT has ability to detect distant metastases beyond the true pelvis. MRI is superior to PET/CT for detection of early parametrial invasion and local recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is third commonest cancer involving the female population in the world with 78% of cases occurring in the developing world. It is the leading cause of cancer-related female death. Clinically, this cancer is staged by International Federation of Gynecology and Obstetrics (FIGO). The FIGO staging of disease decides the management, i.e., patients with local disease (stage I) will undergo surgery while locally advanced disease (stage II–IV A) is managed with definitive chemoradiation and patients with distant metastases (stage IV B) are managed with systemic chemotherapy. The commonest histopathologic type of cancer is squamous cell carcinoma (80–85%), while adeno/adenosquamous variety contributes to a lesser percentage (15–20%) [1]. Magnetic resonance imaging (MRI) has excellent soft tissue resolution and hence provides exact details of the local extent of disease as well as regional lymph node involvement.
The metastatic involvement of local as well as distant lymph nodes carry a vital role in tumor staging as it tweaks the choice of therapy and finally dictating the outcome of overall disease. Though histopathologic examination (HPE) is regarded as gold standard for tissues, it has its disadvantages being invasive, time consuming and often expensive [2]. Valid screening programs and rapid surveillance of the diagnosed cases have lead to early detection of disease before metastatic involvement in the lymph nodes. In early cervical cancer, the lymph nodes have been found free of disease in 80% of cases [3]. There have been questions raised about the use of invasive methods of lymph node dissection in these subsets of patients. This has lead to more stress on the use of structural imaging like ultrasonography (USG), computed tomography (CT) scan, MRI as well as metabolic imaging like fluoro-deoxy glucose positron emission tomography/computed tomography (FDG PET/CT). The concept of sentinel lymph node biopsy which involves removal of single early draining lymph node has also gained importance.
Traditionally, for a lymph node to be labeled as involved by metastasis in the structural imaging like MRI various criteria like increase in the short axis diameter laid down for the region, loss of fatty hilum as well as oval shape is regarded as tale–tale evidence. The fact that metastasis can be present in the normal-sized lymph node precludes the use of size as a lone criteria to decide upon the normal vis-a-vis a pathological node [4]. In general, it can be said that a low-size threshold provides higher sensitivity with low specificity while using a larger size as the threshold will inevitably lower sensitivity but improve specificity. The specificity of MRI to exclude lymph node metastasis in cervical cancer patients is estimated to be as high as 90% [5]. The sensitivity on the other hand drops due to the inability of MRI to detect lymphatic metastasis in normal-sized nodes [6].
FDG PET/CT on the other hand is a metabolic imaging which has high sensitivity in detecting malignant lesions. Various studies have quoted different statistics regarding the sensitivity and specificity of PET/CT in evaluation of nodal involvement in early cervical cancer [7,8,9,10]. PET CT is still used sparingly in the routine chain of investigation for cervical cancer staging despite its superb advantages. In this context, we conducted this study at a tertiary care hospital to assess the efficacy of MRI versus PET CT to detect parametrial involvement as well as lymph node involvement in the cases of carcinoma of cervix.
Aims and Objectives
To compare the usefulness of magnetic resonance imaging (MRI) and 18 fluoro deoxy glucose positron emission tomography (18FDG PET/CT) for the detection of parametrial involvement and lymph node metastasis in patients detected to have cervical cancer.
Materials and Methods
The present study was conducted prospectively on 38 subjects at a tertiary care hospital having a fully equipped and functional malignant disease treatment center for a duration of 2 years. The institutional ethical committee approved the study. Prior consent was taken from all patients for inclusion in the study.
Inclusion Criteria:
All patients of cervical carcinoma who were registered as:
-
(a)
Fresh cases of biopsy proven carcinoma of cervix.
-
(b)
Treated cases of carcinoma of cervix (operated/post-radiotherapy/post-chemoradiotherapy etc.) detected to have recurrence on clinical examination.
-
(c)
Age group of 18–80 years.
Exclusion Criteria:
-
(a)
Patients with pacemaker, metallic implants in the body, Intracranial aneurysmal clips and other metallic devices incompatible with MRI.
-
(b)
Patients having claustrophobia.
-
(c)
Critically ill patients requiring continuous monitoring.
-
(d)
Uncooperative patients.
Method of Collection of Data
Thirty-eight cases with biopsy proven cervical cancer presenting to our oncogynecology department were prospectively enrolled based on the inclusion criteria. The patients were divided into two groups viz group A and group B
Group A (n = 22) All cases which were freshly diagnosed as carcinoma of cervix prior to any treatment. The cases that were included in this group were clinically classified as FIGO up to stage IIA1. These patients were taken up for radical hysterectomy with bilateral pelvic lymph node dissection. Cases beyond ‘operable stage’ were managed by radiotherapy or concurrent chemoradiotherapy.
Group B (n = 16) All these cases were treated cases of cervical cancer (operated/post-radiotherapy/post-chemoradiotherapy) on follow-up, suspected clinically to have recurrence at 6 months or more after completion of planned standard treatment.
Histopathology
Group A In all operated cases (up to FIGO Stage II A1), the resected specimen as well as lymph nodes was sent for histopathology examination. Histopathology results of lymph nodes were classified as—normal/inflammatory (reactive)/malignant.
Group B Cases suspected clinically to have recurrence were subjected to tissue sampling by FNAC/biopsy to prove recurrence. MRI and PET/CT findings were compared with HPE findings.
Imaging Protocol
All enrolled cases were underwent MRI and FDG PET/CT within 1-week interval of each other.
-
1.
MRI: 1.5 Tesla Whole-Body MR Scanner (Siemen’s; Erlangen Germany)
Protocol
All the patients were subjected to MRI examination in a 1.5 Tesla magnet. The imaging parameters include axial T 2-weighted (TR = 5720 ms; TE = 92 ms), coronal and sagittal with a slice thickness of 4 mm, Field of view of 330 mm, Concatenation of 1. Spin Echo T1-weighted (TR = 457 ms; TE = 11 ms) axial, with a slice thickness of 4 mm, Field of view of 320 mm, Concatenation of 3. T2 fat saturated (FS) Axial, T2-weighted small FOV coronal. Pre-contrast T1 FS axial. Post-contrast T1 post-contrast FS images in all three planes. Introduction of water-based jelly per vaginum was used for better delineation of vaginal fornices and vaginal walls. Any lymph node > 1 cm in short axis diameter or any node showing abnormal signal/contrast enhancement with loss of fatty hilum was considered as abnormal. Images were analyzed on dedicated workstation by a single radiologist having experience of at least 10 years.
-
2.
PET/CT: 64 Slice Time of Flight Integrated PET/CT (GE Discovery 690 l)
Tracer used: 18FDG (18 Fluoro-deoxy-glucose)
Protocol
After 6 h of fasting, 5.5 MBq/kg tracer was administered intravenously. All cases were given intravenous diuretic (fursemide) along with FDG to wash-out the tracer from the urinary bladder. After 45 min of delay, scanning of the entire body was done from vertex till mid thighs. Whole-body CT images were acquired in a helical mode, followed by acquisition of PET images. Images were displayed and analyzed as CT only, PET only and fused PET/CT images in all three orthogonal planes using dedicated workstation by radiologist with experience in PET/CT for 12 years.
On FDG PET/CT, only areas with FDG uptake significantly higher than the background (as compared to liver or the background tissue) and FDG uptake visible on at least two consecutive axial slices were considered as positive and SUV measurement was done at these areas.
Statistical Analysis
Statistical analysis was performed with the SPSS, version 20 (SPSS inc., Chicago, illinois, USA). The categorical data were presented as numbers (percent) and were compared among groups using Chi-square test. Groups were compared for demographic data, presented as mean and standard deviation and were compared using Student’s t test. Concordance rate was used to evaluate the agreement between two provisional diagnosis on MRI and PET CT. The following criteria were used.
True-positive: positive for metastases/disease on PET/CT or MRI images and positive for cancer on HPE.
False-positive: positive for metastases/diseases on PET/CT or MRI images but negative for cancer on HPE.
True-negative: found negative for cancer at both PET/CT or MRI and HPE.
False-negative: negative for metastases/diseases on PET/CT or MRI but found positive for cancer on HPE.
Probability P value < 0.05 was considered statistically significant.
Results and Analysis
A total of 38 patients of biopsy proven carcinoma cervix were prospectively included in the study, which were divided into two groups as described ante. They were analyzed as follows:
Age Group The age group did not exhibit significant difference among both the groups. Maximum cases were observed in 51–60 years of age group interval in both group A and B (45 and 44%, respectively).
Clinical Presentation The most common presenting symptom of patients was vaginal bleeding/discharge in both the groups. A total of 18 patients (82%) in group A and seven patients in group B (44%) presented with vaginal bleeding/discharge.
Histopathologic Types of Cancer HPE revealed 20 cases (91%) in group A and 14 cases (88%) in group B had Squamous cell carcinoma, while two patients in each group (9 and 12%, respectively) had adenocarcinoma.
Distribution of Patients as Per FIGO Classification
In group A, majority of patients had early stage disease and nearly a third of patients (8/22) presented in stage IB. In Group B most patients (presenting with clinical recurrence) had higher base line FIGO staging (stage III B–IV A) (Table 1).
Group A
Operability
In group A, total of 14 cases (63%) were found to be in an ‘operable FIGO stage’ and underwent radical hysterectomy with bilateral pelvic lymph node dissection and eight cases (37%) were managed with chemoradiotherapy.
Lymph Nodes Involvement
Single metastatic lymph node was detected by MRI in 03 cases and by FDG PET/CT in 04 cases. Two metastatic lymph nodes were detected by MRI in 02 cases and by FDG PET/CT in 03 cases. Three metastatic lymph nodes were detected by MRI & FDG PET/CT in 01 case each. The mean number of disease positive lymph nodes on MRI per case was 1.67 (10 out of 6 cases), while on FDG PET/CT, it was 1.62 (13 out of 8) (Table 2).
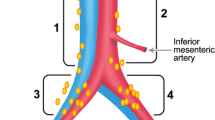
Most frequently involved group lymph node was found to be the iliac group on MRI as well as on PET/CT. Para-aortic lymph nodes (1 out of 13 lymph nodes, i.e., 8%) were detected only on PET/CT and not detected on MRI (MRI was done for pelvic region only, in all cases).
MRI Versus PET CT in Detection of Lymph Nodes
The sensitivity, positive predictive value, negative predictive value and diagnostic accuracy of FDG PET/CT were found to be better than MRI. However, specificity of both modalities was found to be similar in our study (Tables 3, 4).
Parametrial Involvement Detected by MRI, PET/CT Versus HPE
Out of 14 Cases that underwent surgery, 11 were found to be negative for parametrial invasion on HPE.
Clinical staging versus HPE: In 3 of 14 cases (21%), clinical examination under-staged the disease.
Distant Metastasis
Distant metastasis was found on FDG PET/CT in two out of eight cases. The case number 09 in our series showed skeletal (DV10 body) as well as liver metastases and case number 18 of our series showed pulmonary and mediastinal nodal metastases on FDG PET/CT. Hence, FDG PET/CT upgraded the disease to stage IVB leading to change in management in these two cases (Table 5).
In the pelvic region, all lymph nodes that were morphologically labeled positive for disease on MRI showed metabolic activity on FDG PET/CT. In addition, PET/CT showed four more positive lymph nodes, which were less than 10 mm in short axis diameter.
Group B
All cases suspected clinically to have recurrence, underwent MRI as well as FDG PET/CT. Thereafter all cases were subjected to tissue sampling by FNAC/biopsy for confirmation of recurrence of disease.
Clinically the cases were assessed for local recurrence as follows:
-
Central disease: involving cervix/uterus/vagina/parametrium.
-
Lateral disease: involving lateral pelvic wall.
-
Central and lateral disease: involving central region as well as lateral pelvic wall.
Nodal recurrence was assessed on imaging only (Table 6).
Though the sensitivity and specificity for detection of disease recurrence was similar for MRI & FDG PET/CT; the spatial resolution of the images on MRI was far superior to that of the PET/CT.
FDG PET/CT labeled 12 cases (35 lymph nodes) as positive for metastases. MRI labeled 11 cases (23 lymph nodes) as positive for metastases. A total of 11 out of 16 patients (69%) were confirmed to have metastatic lymph node disease on HPE. PET/CT detected more number of metastatic lymph nodes as compared to MRI (Table 7).
Discussion
Cervical cancer is one of the commonest causes of death in the developing countries including India; more so in the low- and middle-income countries. In India as per the National Cancer Registry Programme (NCRP), the most common site of cancer among Indian women at present are breast and cervix. Every year in India 1,22,844 women are diagnosed with cervical cancer and nearly 67,477 deaths occur due to this disease [11].
We studied total of 38 patients of biopsy proven carcinoma cervix over a period of 2 years. Most of our patients were in the age group of 51–60 years in both the groups (45 and 43%, respectively). Pandit-Taskar et al. observed that in the West, most cases were diagnosed early with almost 47% of invasive cases detected before the age of 35 years and about 10% of patients were more than 65 years old. This may be due to aggressive screening procedures and more awareness about the disease in west [12].
Group A (Operated Cases)
In our study, PET/CT detected more number of regional as well as non regional positive lymph nodes as compared to MRI and most frequently involved lymph node group was found to be the iliac group of lymph nodes on both modalities. Rose et al. observed the use of FDG PET/CT accurately predicts the presence and absence of pelvic and para-aortic nodal metastatic disease [14]. Hyun Hoon Chung et al. documented in their study that 34 (28%) patients had pelvic lymph node metastasis and four (3%) patients had para-aortic lymph node metastases histologically [15]. Pandit-Taskar et al. on the contrary in their study observed that external iliac and obturator nodes were more frequently involved and bilateral nodal drainage was common [13].
On patient basis as well as lymph node-based analysis in our study, we observed that for detection of lymph node metastases, in MRI versus FDG PET/CT; the PET/CT had a higher sensitivity, positive predictive value, negative predictive value as well as diagnostic accuracy (Tables 3, 4) though the specificity (71 vs 71%) remained same in both modalities. Our study provides much better figures as compared to Hyun Hoon Chung et al. though observed that for preoperative lymph node staging, sensitivity of MRI was 40% (region-specific analysis) and 70% (patient-based analysis), respectively [15].
The reason for lower sensitivity and PPV for MRI can be possibly explained by the fact that MRI may have missed metastases in small sized (< 10 mm) lymph nodes. In our study, since MRI examination was done for pelvic region only, para-aortic lymph node disease was not assessed by MRI. Choi et al. carried out data meta-analysis of 41 studies and reported that PET or PET/CT had an overall higher diagnostic performance than CT or MRI for lymph node metastases detection in cervical cancer patients. PET or PET/CT had the highest pooled sensitivity (82%) and specificity (95%), whereas CT had 50 and 92%, and MRI had 56 and 91%, respectively in their study [16].
Parametrial Invasion
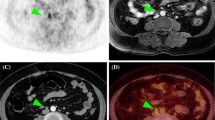
In our study, MRI correctly detected parametrial invasion in two cases, which were also found positive on histopathologic examination (Fig. 1 a and b). It is inferred that by clinical examination FIGO staging can miss early parametrial invasion, which could be detected on MRI. It is evident from our study that MRI is superior to FDG PET/CT in detection of parametrial invasion which is likely attributable to its inherent capability for better resolution and superior soft tissue discrimination (Fig. 1c). Park et al. observed that there were significant inaccuracies in FIGO staging, with a 33% error rate. MRI scans for 32 primary tumors had an accuracy of 84% compared with the surgical specimen (P < 0.0001). Only two patients (6%) were up-staged, but three patients (9%) including one patient with no visible tumor on MRI were down-staged on MRI scans [14] (Fig. 2). Hyun Hoon Chung et al. [15] showed that the sensitivity and NPV of MRI in the evaluation of parametrial invasion were 100% and the accuracy was 91%. However, MRI considerably overestimated the parametrial invasion (PPV 62%). Although the specificity and NPV of clinical staging by pelvic examination were almost the same as those of MRI, the sensitivity (44%) and PPV (42%) were inferior to those of MRI. It was predicted that use of newer available powerful magnets will further improve the parametrial invasion, however, studies using 3T MRI have found no significant improvement in accuracy [17].
a, b T2WI axial MRI images showing circumferential cervical wall thickening with bilateral parametrial invasion (bold arrows) (R > L). c PET/CT coronal, sagittal and axial images showed uptake in cervix (bold arrow) with pelvic and para-aortic lymph nodes (thin arrow). However, no parametrial involvement is seen on PET/CT
a–c MRI T2WI sagittal, coronal and axial images showing cervical mass with extension into lower uterine body (bold arrow in a) and upper vagina (thin arrow in a) and infiltration into rectum (arrow in b), pelvic lymph nodes (thin arrow in b) and parametrium (arrows in c). d–f Fused PET/CT sagittal axial images showing mass lesion in cervix with extension into vagina and lower uterus and infiltration (bold arrow in d, e) of mass lesion into rectum and parametrium with pelvic lymph nodes (arrow in f)
Non-operable Cases of Group A
MRI detected 24 metastatic lymph nodes in eight cases. Both MRI as well as PET/CT was concordant in 7 cases for 24 metastatic lymph nodes. As compared to the group that underwent surgery; PET/CT detected more number of metastatic lymph nodes than MRI.
In this group, distant metastases were found on FDG PET/CT in two out of eight cases. Hence, FDG PET/CT upgraded the disease to stage IVB in these two cases by detecting distant metastases and altering further management (Fig. 3).
Group B Cases
Diagnostic statistics for local disease recurrence for MRI versus FDG PET/CT reveled MRI had a higher sensitivity (93 vs 86%) and accuracy (94 vs 87%) than FDG PET/CT. Kaur et al. [18] concluded that MR imaging represents the single most effective modality for detection of primary tumor and local spread. In deciding the nodal involvement, CT and MR imaging were equally effective. If clinically available, PET/CT scanning improves the specificity and sensitivity of these techniques. The addition of newer imaging techniques like dynamic MR imaging improves specificity of the disease recurrence and provides prognostic information.
Newer available techniques in MRI like diffusion weighted imaging (DWI), perfusion-weighted imaging as well as dynamic contrast-enhanced imaging (DCE) are adding further dimension to the multiparametric imaging. The availability of hybrid PET MRI is further adding much more specificity to the diagnosis. The advantage of PET MRI over PET-CT is that it has more spatial resolution regarding the parametrial invasion. Kitajima et al. in their study of 30 patients using hybrid 18F PET MRI had a 100% detection rate for cervical cancer. In their study, they found that fused PET MRI had an accuracy of 83.3% as compared to 53.3% of PET with contrast-enhanced CT scan. The authors concluded that using PET MRI the detection rate for cervical cancer was higher; in delineation of other parameters like vaginal, pelvic side wall and bladder invasion, the differences were not statistically significant [19].
To conclude, we evaluated the use of MRI and PET/CT in fresh as well as recurrence cases for local as well as metastatic carcinoma of cervix. This study concludes that MRI is the modality of choice in local assessment of the disease, while PET/CT though compliments in local staging, it is invaluable for nodal as well as distant metastatic involvement. As far as possible, FDG PET/CT should be included in the diagnostic and staging algorithm of the cervical cancer staging especially for locally advanced disease (stage II–IV A) and suspected distant metastases.
References
Chaturvedi AK, et al. Second cancers after squamous cell carcinoma and adenocarcinoma of the cervix. J Clin Oncol. 2009;27(6):967–73.
Wunderbaldinger P. Problems and prospects of modern lymph node imaging. Eur J Radiol. 2006;58:325–37.
Quinn MA, Benedet JL, Odicino F, et al. Carcinoma of the cervix uteri: volume 26 of the FIGO annual report on the results of treatment in gynecological cancer. Int J GynecolObstet. 2006;95(26):S161–92.
Koh DM, Hughes M, Husband JE. Cross-sectional imaging of nodal metastases in the abdomen and pelvis. Abdom Imaging. 2006;31:632–43.
Bipat S, Glas AS, van der Velden J, Zwinderman AH, Bossuyt PM, Stoker J. Computed tomography and magnetic resonance imaging in staging of uterine cervical carcinoma: a systematic review. Gynecol Oncol. 2003;91:59–66.
Scheidler J, Hricak H, Yu KK, Subak L, Segal MR. Radiological evaluation of lymph node metastases in patients with cervical cancer: a meta-analysis. JAMA. 1997;278(5):1096–101.
Sugawara Y, Eisbruch A, Kosuda S, Recker BE, Kison PV, Wahl RL. Evaluation of FDG PET in patients with cervical cancer. J Nucl Med. 1999;40:1125–31.
Rose PG, Adler LP, Rodriguez M, Faulhaber PF, Abdul-Karim FW, Miraldi F. Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: a surgicopathologic study. J Clin Oncol. 1999;17:41–5.
Kitajima K, Murakami K, Yamasaki E, Kaji Y, Sugimura K. Accuracy of integrated FDG-PET/contrast-enhanced CT in detecting pelvic and paraaortic lymph node metastasis in patients with uterine cancer. Eur Radiol. 2009;19:1529–36.
Boughanim M, Leboulleux S, Rey A, Pham CT, Zafrani Y, Duvillard P, Lumbroso J, Haie-Meder C, Schlumberger M, Morice P. Histologic results of para-aortic lymphadenectomy in patients treated for stage IB2/II cervical cancer with negative [18F]fluorodeoxyglucose positron emission tomography scans in the para-aortic area. J Clin Oncol. 2008;26:2558–61.
Sreedevi A, Javed R, Dinesh A. Epidemiology of cervical cancer with special focus on India. Int J Women’s Health. 2015;7:405–14.
De Gonzalez AB, Green J. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer. 2007;120:885–91.
Pandit-Taskar N. Oncologic imaging in gynecologic malignancies. J Nucl Med. 2005;46:1842–50.
Rose PG, Adler LP, Rodriguez M, Faulhaber PF, Abdul-Karim WF, Miraldi F. Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: a surgicopathologic. J Clin Oncol. 1999;17(1):41.
Chung HH, Kang SB, Cho JY, Kim JW, Park NH, Song YS, et al. Can preoperative MRI accurately evaluate nodal and parametrial invasion in early stage cervical cancer. Atlanta: American Cancer Society; 2003.
Choi HJ, Roh JW, Seo SS, et al. Comparison of the accuracy of magnetic resonance imaging and positron emission tomography/computed tomography in the presurgical detection of lymph node metastases in patients with uterine cervical carcinoma: a prospective study. Cancer. 2006;106(4):914–22.
Hori M, Kim T, Murakami T, et al. Uterine cervical carcinoma: preoperative staging with 3.0-T MR imaging- -comparison with 1.5-T MR imaging. Radiology. 2009;251(1):96–104.
Kaur H, Silverman PM, Iyer RB, Verschraegen CF, Eifel PJ, Charnsangavej C. Diagnosis, staging, and surveillance of cervical carcinoma. AJR Am J Roentgenol. 2003;180(6):1621–31.
Khiewvan B, Torigian AD, Emamzadehfard S, et al. Update of the role of PET CT & PET MRI in the management of patients with cervical cancer. Hell J Nucl Med. 2016;19(3):254–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sahu, S., Singh, H. & Kumar, P. Comparison of Magnetic Resonance Imaging (MRI) and Positron Emission Tomography-Computed Tomography (PET CT) for Detection of Parametrial Involvement and Lymph Node Metastasis in Patients with Cervical Cancer: A Prospective Study. Indian J Gynecol Oncolog 15, 73 (2017). https://doi.org/10.1007/s40944-017-0167-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-017-0167-4