Abstract
This paper evaluates the impact of battery charging and discharging times on the availability of mechanical respirators in the Intensive Care Unit (ICU). The availability of these life-saving devices is crucial for ensuring optimal patient care in critical situations. This study aims to assess how the duration of battery charging and discharging cycles affects the availability of mechanical respirators and explore potential strategies to optimize their maintainability. We analyze the system’s behavior in eight scenarios that consider changes to optimize repair times, battery charge and discharge times, and power system redundancy. The results showed 98% improvements in availability and reduced system downtime. The outcomes of this research contribute to understanding the critical factors impacting the availability of mechanical respirators in the ICU. By addressing the issues related to battery charging and discharging times and maintaining these devices, healthcare facilities can enhance the availability and reliability of respiratory support systems. Ultimately, this study aims to improve patient outcomes and promote efficient resource utilization in the ICU setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Patients’ admission to Intensive Care Units (ICUs) can be a challenging and stressful experience for patients and their families. Several concerns are associated with ICU hospitalizations, including physical and emotional stress, risks of medical complications, and communication challenges, for instance, [1]. Essential variables concerning reducing mortality in ICUs are the number of beds, availability of respirators, and the qualification of health professionals [2].
Mechanical ventilation is an essential component for treating critically ill patients in ICUs. It involves using a machine to support the patient’s breathing when they cannot continue independently due to respiratory failure or other conditions. MV also helps to maintain oxygenation and carbon dioxide levels within safe ranges and avoid invasive procedures, such as tracheostomies. In addition, MV is critical during surgery and other procedures that require anesthesia to maintain the patient’s airway and ensure adequate oxygenation. Finally, MV also allows healthcare providers to closely monitor the patient’s respiratory status to support early warning of potential complications, such as oxygen desaturation or airway obstruction [3].
The respirator has proven to be the primary tool for treating critically ill patients, especially those with respiratory failure [4]. For example, it has played a crucial role in treating patients with COVID-19 who developed severe respiratory symptoms, providing respiratory support by enabling proper ventilation, precise monitoring, and managing treatment protocols [5]. However, the lack of regular maintenance services may expose the patient to more significant risks [6].
Batteries are essential for the functioning of Respirators’ Lung. RLs are usually used in critical care situations, such as power outages or other disruptions to the electrical supply. In such cases, batteries play a crucial role in ensuring that the mechanical respirator continues functioning and delivering oxygen to the patient. They also allow the transportation of patients between hospitals or within a hospital [7].
Redundant batteries are additional sets of backup batteries for a mechanical respirator. These batteries provide an extra layer of protection against power outages or other disruptions to the electrical supply. Redundant batteries are essential in critical care situations where the patient’s life depends on the continuous operation of the mechanical respirator. Without redundant batteries, any disruption in the power supply could have life-threatening consequences for the patient [8].
The authors of [9] studied the batteries in respirators used in the operating room to keep the patient breathing during general anesthesia. They discuss the importance of the availability of batteries in respirators and anesthesia devices, emphasizing the need for the batteries to be reliable, efficient, and capable of providing sufficient power to these essential medical devices often used in emergencies. In addition, the authors argue that monitoring battery levels and replacing them when necessary is crucial to ensure that the devices remain operational. They also emphasize the importance of the availability and reliability of batteries in respirators and anesthesia devices. They also discuss if healthcare professionals should be trained to monitor battery levels and troubleshoot battery-related problems.
In this context, we highlight the importance of analyzing the performance and availability of mechanical ventilators in intensive care units. The proper functioning of these devices is critical for saving the lives of patients with respiratory failure. They are also essential for reducing further damage to the health of critically ill patients, who require uninterrupted mechanical ventilation to maintain life. In addition, we highlight the importance of the scenarios described in this work, enabling tests about better system functioning without incurring greater economic costs for hospital services. In this work, we investigate the availability of a mechanical respirator by considering the power utility, a power generator subsystem, and a two-module battery subsystem. The proposed model is employed to evaluate the occurrence of failures and repair activities on the power system. The model encompasses the impact analysis of the battery charging and discharging times on the mechanical respirator system availability.
Section 2 summarizes the works most related to our proposal. Section 3 presents the theoretical basis to support the understanding of the solution presented in this article. Section 4 presents the methodology used in this article. Section 5 presents the proposed model, with each system component represented as a Stochastic Petri Nets representation. Section 6 presents the results obtained, with a detailed description of each scenario. Section 7 presents the summary discussion of scenarios. Finally, Sect. 8 presents conclusions and highlights future research directions.
2 Related works
The utilization of hierarchical modeling to enhance availability has been extensively investigated over the years. In this section, we consolidate a selection of relevant works focusing on modeling and performance evaluation in hospital technology.
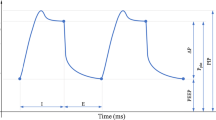
In a study conducted by Blakeman et al. [8], the authors evaluated the performance of batteries in four respirators equipped with volume and pressure-controlled ventilation, along with end-expiratory pressure (PEEP) values ranging from 0 to 20 cm H2O. The findings indicate that battery duration did not exhibit significant changes among respirators of the same model, even with variations in PEEP levels. The observed battery durations ranged from 5 to 69 min, with a mean period ± standard deviation of 80.4 ± 49.3. The authors concluded that utilizing a compressor diminishes battery duration and that no correlation was found between battery age and operating time. They emphasize the importance of the medical community being aware of these differences in scenarios involving power failures.
Araujo proposed a model with reliability analysis for multi-parameter monitoring systems in Intensive Care Units (ICU), measuring parameters, such as heart rate, respiratory rate, and temperature [10]. The study initially performed a reliability analysis, developing a parametric and modular model using the CHESS State-Based Analysis (CHESS-SBA) tool.
In another investigation by Sandelic et al. [11], the authors compared the reliability of a DC-coupled and an AC-coupled PV battery system. Through a case study of a 6 kW PV system integrated with a 3 kW/7.5 kWh battery system, they demonstrated that the DC-coupled configuration achieved superior reliability. The analysis presented provides a reference for evaluating the lifetime and reliability of power conversion units in such systems, emphasizing the necessity of conducting reliability assessments on these critical components to ensure the high efficiency and longevity of PV battery systems.
Nguyen et al. [12] conducted a study involving reliability and availability analysis for the infrastructure of the Internet of Medical Things (IoMT) in a healthcare system, utilizing hierarchical models such as Fault Tree (FT) and Continuous Time Markov Chain (CTMC). The study incorporated failure modes for systems, including cybersecurity attacks on software subsystems. This research contributes to enhancing the design and implementation of real-world IoMT infrastructures, comprising cloud, fog, and edge computing, and assists in securing autonomous operations in the healthcare domain.
In our study, we employ reliability and dependability analysis using an SPN (Stochastic Petri Net) model to examine the behavior of ICU respirators, their power supply system, and the operational dynamics of battery modules. Our objective is to identify potential bottlenecks that may impede availability and, based on this analysis, propose improvements to enhance overall availability.
3 Background
This section reviews some concepts from mathematics and statistics regarding availability, performance, and models [13, 14]. Moreover, we conceptualize aspects of an intensive care unit.
3.1 Availability and performability
Availability is the probability that a system is ready to work satisfactorily. This metric is used as an evaluation parameter in the operational environment and has been studied over the years. Critical systems do not tolerate extended periods of inactivity, requiring a higher availability [15, 16].
System availability can be represented by the ratio between Mean Time to Failure MTTF and Mean Time to Repair MTTR of the system [14]. The corresponding notation is expressed in Eq. (1):
We can calculate MTTF using the reliability R(t) as a function of time. We can also assess MTTR based on the values of MTTF, availability, and UA [17]. The corresponding notations are expressed in Eqs. (2) and (3):
Performability is used to evaluate more complete models composed of reliability and performance measures. The performability measure is best suited for systems that may suffer a failure due to the passage of time or exhaustion [18]. According to [19], performability analysis aims to capture the dynamics between failure behavior and repair and performance provided by the system.
3.1.1 Redundancy
Adopting redundant mechanisms is a strategy used to improve the reliability and availability of a system by replicating critical components or data. Such an approach involves creating backups or duplicates of essential elements, so that if one fails, the system can continue to operate without interruption [20].
Redundancy can be implemented at different system levels, including hardware, software, and data, involving the duplication of physical components, such as processors, memory, or storage devices. For example, the replication of software components, such as servers or applications, across multiple machines, creating copies of critical data, such as databases or files, and storing them in different locations to prevent loss or corruption [21].
One of the main benefits of redundancy is increased reliability and availability; by creating backups or duplicates of critical components, the system can continue to operate even if one or more components fail. This ability is essential in critical systems such as aviation, healthcare, or financial services, where downtime or outages can have serious consequences [22].
3.1.2 Stochastic petri nets
Stochastic Petri Nets (SPN) is a term that denotes a family of stochastic models that is part of a more prominent family of behavioral models named Petri nets. The first stochastic Petri net extensions were proposed independently by Symons, Natkin, and Molloy [23,24,25]. These models formed what were then named Stochastic Petri Nets. Subsequently, many other stochastic extensions were introduced. First, Marsan et al. extended the basic stochastic Petri nets by considering stochastic timed transitions and immediate transitions [26]. This model was named Generalized Stochastic Petri Nets (GSPN) [27]. Later on, Marsan and Chiola proposed an extension that also supported deterministic timed transitions [28], which was named Deterministic Stochastic Petri Nets (DSPN) [29]. Many other extensions followed, including eDSPN [30] and SRN [31].
3.1.3 Sensitivity analysis
When conducting sensitivity analysis, there are multiple techniques available, such as sensitivity measures one at a time, the relative deviation method, the relative deviation rate, the partial rank correlation coefficient, differential sensitivity analysis, and the Sensitivity Index [32]. For our research, we will be utilizing the Sensitivity Index.
The Sensitivity Index (\(S_y(A)\)) evaluates the effect of alterations in the input parameter (y) on a particular availability. It is expressed as a percentage difference. To calculate the sensitivity index for the metric y, we use Eq. 4. \(max_y\) and \(min_y\) represent the maximum and minimum output values achieved by adjusting the parameter y up to the maximum value \(max_y\):
When determining \(S_y(A)\), keeping the other model parameters constant is essential. This step is crucial for calculating all parameters and constructing the classification of sensitivity analysis. This classification enhances the accuracy of predicting increased availability.
3.1.4 Mechanical ventilation system
The intensive care unit is a hospital with specialized care for critically ill individuals who need life support [33]. The ICU is an environment with technical, human, and technological needs to provide adequate care. The need for an intensive care unit arose in the 50s with the polio outbreak, where patients needed mechanical help to breathe.
Mechanical ventilation is the most common intervention in the ICU, providing respiratory support to those who cannot manage it independently. According to [34], it has become clear that mechanical ventilation can attenuate lung damage and increase patient survival.
The operational process in an ICU using a mechanical ventilator involves the following steps: Assessment and preparation of the patient, where necessary preparations are made, such as securing the airway, checking the mechanical ventilator, and installing the necessary equipment. Start of mechanical ventilation, where the respirator lung is set up to deliver oxygen to the patient’s lungs and is programmed with the appropriate settings such as tidal volume, respiratory rate, and (PEEP) to ensure proper ventilation [35].
The mechanical ventilation system in an intensive care unit is a sophisticated and crucial life support system that assists patients who cannot breathe adequately independently or have respiratory failure. It comprises interconnected components that work harmoniously to deliver controlled and assisted ventilation tailored to each patient’s requirements [36]. When weaning and extubation, after the patient’s condition improves, the respirator lung settings are gradually reduced, and the patient is weaned from the Respirator. If the patient can breathe independently and maintain adequate oxygenation, the endotracheal tube is removed, and the patient is extubated [37].
Let us explore each element of the respirator lung in more detail:
The respirator is the central device in the mechanical ventilation system. It delivers a precise mixture of oxygen and air at controlled pressures and volumes to maintain appropriate oxygenation and ventilation. Modern respirators have advanced features, such as multiple ventilation modes (e.g., volume control, pressure control, and pressure support), adjustable inspiratory and expiratory times, and breath synchronization capabilities [38]. These functionalities allow healthcare providers to customize ventilation settings to suit the patient’s condition and optimize respiratory support.
The breathing circuit is the component that connects the ventilator and the patient’s airway. It consists of various components, including tubing, connectors, and filters. The circuit transports the pressurized gases from the ventilator to the patient’s lungs and allows for the removal of exhaled gases. It may incorporate additional features like heat and moisture exchangers or active humidifiers to provide optimal humidification of the inspired gases, ensuring patient comfort and maintaining the health of the respiratory tract [39].
Endotracheal tube or Tracheostomy tube establishes a secure airway for ICU patients requiring mechanical ventilation. Patients often have an endotracheal tube (inserted through the mouth) or a tracheostomy tube (inserted through a surgically created opening in the neck). These tubes deliver ventilator gases directly into the patient’s lungs, bypassing upper airway obstructions or other respiratory limitations [40].
The humidification system adds moisture to the delivered gases. Proper humidification is crucial to prevent drying and damage to the respiratory tract, particularly during prolonged mechanical ventilation. Humidifiers provide controlled humidification to maintain optimal lung function and reduce complications associated with dry airway passages [41].
Monitoring system assesses the effectiveness of ventilation. Oxygen saturation monitors (pulse oximeters) continuously measure the patient’s blood oxygen levels. In contrast, end-tidal CO2 monitors provide real-time monitoring of exhaled carbon dioxide levels, allowing for accurate assessment of ventilation adequacy. Pressure and volume sensors integrated into the breathing circuit monitor the applied pressures and delivered tidal volumes, helping healthcare providers optimize ventilator settings and detect potential issues promptly [42].
Alarms and safety features alert healthcare providers in case of abnormalities or emergencies. High or low-pressure alarms notify caregivers of significant changes in the patient’s lung mechanics, while disconnection alarms alert them to any unintentional disconnections between the patient and the ventilator. Additionally, apnea alarms can detect a lack of spontaneous respiratory efforts, triggering immediate intervention [43].
The control panel and user interface allow healthcare providers to adjust ventilation parameters, monitor patient parameters, and review trends. These interfaces are designed to be intuitive and user-friendly, providing visual displays of vital information such as respiratory rate, tidal volume, and oxygen saturation. Through the control panel, healthcare providers can make precise adjustments to ventilation settings, ensuring the delivery of optimal respiratory support [44].
The respirator lung system discussed in this paper provides mechanical ventilation for patients in intensive care units. The system consists of several components that facilitate breathing for critically ill patients, as shown in Fig. 1. We present a detailed system structure overview, including the power supply system, battery modules, and breathing circuit. In addition, we provide proposals for increasing the system’s availability, which could improve patient outcomes and reduce healthcare costs.
The power supply system of the lung respirator is an essential component of the system. The system consists of an electrical power supply, a power generator, and a switch, all maintained on hot standby. The battery modules are a safety feature when the power is interrupted, and the patient needs to continue treatment. Using hot standby ensures the system is always ready to provide ventilation during a power failure or other emergencies.
4 Methodology
This section presents the methodology used to evaluate the given model based on previous work by [45, 46]. The proposed methodology presented in Fig. 2 has four phases divided into Understanding the system, where a detailed analysis of the individual components that constitute the mechanical respirator will be carried out; Acquiring the parameters is obtaining the specific values of the parts of the ventilator system; model-building, with the implementation of parameters aimed at developing an availability model that comprehensively represents the mechanical ventilator system and finally providing recommendation, which presents the results of the analyzed evaluations to identify potential improvements, and measures such as modifications design, operational procedures and redundancy implementations and in each of the mentioned phases will be detailed in the subsequent subchapters.
4.1 Understanding the system
In designing the mechanical ventilator system, conducting an in-depth analysis of the system itself is crucial. For this, it is necessary to understand each component that makes up the mechanical ventilator. This means thoroughly exploring the characteristics, functionalities, and inbuilt properties of each element that comprises the system.
Furthermore, it is necessary to examine how these different components interrelate. Understanding the connections and interactions between the parts is critical to forming a complete picture of the system’s dynamics, including its batteries and power supply systems.
As this phase is built into the assessment methodology, it is critical to document each aspect addressed to establish a foundation for the subsequent assessment. The detailed analysis of the components, interrelationships, and parameters will be crucial for the overall understanding of the mechanical ventilator system and, thus, for the accurate and careful evaluation of its performance and effectiveness, considering its energy supply system.
4.2 Acquiring the parameters
Obtaining the parameters constitutes a critical step in the evaluation methodology of the mechanical respirator system. In this phase, the focus turns to getting the specific values associated with each system component. This search for accurate values can encompass a variety of methods, including hands-on experimentation, empirical data collection, or even the search for specialized knowledge in the field. The accuracy of these parameters is important because they affect the overall behavior and performance of the system.
These parameters help us ensure our model accurately represents the actual system. Each captured value contributes to building a model and ensures that subsequent assessments are reliable and grounded. By incorporating these values directly from the reality of the mechanical ventilator system, we provide that the evaluation methodology is functional and that the results faithfully reflect the practical operation of the system.
During the get parameters process, the approach taken to capture the specific values of the components must be carefully selected. Direct experimentation, through practical tests and measurements, can be an effective approach to obtaining actual data from the system in operation. Furthermore, collecting data from real operating environments can provide valuable insights into system behavior in real situations. On the other hand, the specialized knowledge of professionals in the field also plays a crucial role in obtaining reliable information about the parameters. Whichever method you choose, getting these values accurately is essential to ensure that the resulting model is a faithful representation of the system and that subsequent evaluations are reliable to guide informed decisions.
4.3 Model-building
After the obtaining the parameters step, the model construction phase proceeds. An availability model is developed based on previously collected information at this stage. This model plays a crucial role in representing the system comprehensively, capturing its essential characteristics and behaviors.
The model-building process requires careful selection of an appropriate modeling technique, considering the nature and complexity of the mechanical ventilator system. In addition, it is essential to clearly define the system’s boundaries, delimiting which elements will be included and which will be excluded in the model. The specification between the components is another critical aspect, as this guarantees that the model faithfully represents the relationships between the different elements of the system.
The model evaluation is conducted considering a variety of scenarios of interest. These scenarios can cover operating conditions differing, external influences, and potential system failures. Simulating these scenarios in the model allows you to assess system performance, reliability, and availability under various circumstances. The results of this assessment allow identifying possible areas for improvement, optimizing configurations, and supporting decisions on the viability and improvement of the model for practical implementation.
In summary, the Model Building phase is essential to translate the collected data into an objective representation of the mechanical ventilator system. This permits a thorough examination of the system’s behavior in various circumstances, enabling a coherent course of action based on actual and pertinent scenarios.
4.4 Providing recommendations
The ending phase of the process is to Provide Recommendations to improve system availability. In this context, a careful analysis of the evaluation results is carried out, highlighting gaps or areas that could be improved. From this, appropriate measures are proposed to address these points, aiming to optimize the availability of the mechanical ventilator system. These recommendations can cover a range of actions, depending on the deficiencies identified. In some cases, changes in the system design can be suggested, aiming to improve specific aspects that impact its availability. In addition, modifications to operating procedures can be proposed to ensure the system’s most efficient and stable operation in varied scenarios.
Another approach is to implement additional redundancy measures. By introducing redundant components or backup systems, mitigating the impact of possible failures is possible, improving overall system availability. These other security measures ensure the system can operate reliably, even in unexpected events.
The recommendations aim to optimize system availability, ensuring it is aligned with established performance and reliability objectives. By implementing these measures, we seek to ensure that the mechanical ventilator system is prepared to meet operational demands effectively, minimizing potential risks and maximizing its effectiveness.
5 Performability model
This section presents a performability (availability and performance) model. This model is the SPN depicted in Fig. 3. The architecture comprises the Power Source system, corresponding to one utility, generator, and switch, representing a standard power architecture for hospitals. The Respirator Lung system shall have one respirator, two internal battery modules, and one breathing circuit. The system is available when the respirator lung represented by NR and the backup respirator lung characterized by M is greater than or equal to N. Moreover, the breathing circuit must be greater than zero. The following notations correspond to the metrics for availability, downtime, and number of 9’s expressed in Eqs. (5), (6), and (7).
Expression 5 refers to system availability. The expression shows that the system will be available when the probability of the default respirator RLU plus the backup respirator RLBU is greater than or equal to N, AND the breathing circuit exceeds zero.
Expression 6 refers to the time the system spends inactive. We use (1-)probability that the standard respirator RLU plus the backup respirator RLBU is greater than or equal to N, the breathing circuit is greater than zero, times the time (h) as Table 3.
Expression 7 refers to the number of “9” contained in the system availability calculation. This expression starts with the negative logarithm, 1 - (the probability of system availability), included in Expression 5.
The model corresponding to the Power Source is composed of: UT (Utility), represented by NUT, which can be up (UTU) or down (UTD); G (Generator), which can be up (GU) or down; or offline (GO); and the SW (Switch) which can be Up (SWU) or down (SWD). Only the guard corresponding to the UTU has service type ISS (infinite service semantics). The other guards of the power source system have service type SSS (single service semantics).
The model corresponding to the Respirator Lung is composed of the following components:
-
Two Battery (BT) modules represented by NB, which can be Discharged (BAUC); In charging (BALI) and we assume that from this stage, it can present defects and go to the Down state (BALID); Charged (BAC) and Down (BACD); and available for use (BAU) or Down (BAD);
-
The RL (Respirator Lung), represented by NR, can be Up (RLU) or Down (RLD) when there are defects due to machine maintenance, or it can be Down due to power source failure (RLDE);
-
And the BC (Breathing Circuit), a silicone circuit connecting the patient to the Respirator Lung, can be either Up (BCU) or Down (BCD). All guards of the respirator lung system have service type ISS. All transitions have the same priority 1.
In Fig. 3, we present a model depicting the initially suggested improvement for the system under study. This enhancement was identified following scenario evaluations to pinpoint the bottleneck. Subsequently, we successfully increased system availability by implementing a Cold Standby Respirator [47].
As a result, we can see an increase in availability and a reduction in downtime. When the system identifies an unavailable RL by maintenance failure, the backup RL takes over RLB (Respirator Lung Backup) represented by M without paralyzing the mechanical ventilation service in the ICU. To do so, we suggest 1 RLB (M=1) for every 10 RLs. We also recommend increasing the number of battery modules to optimize the service in cases of RL unavailability due to problems from the power source; in this sense, we suggest for each 1 RL, 2 NB, totalizing 20 batteries for 10 Respirator lungs. We use a variable represented by N to determine the minimum number of respirators in operation. Table 1 presents the guard of transitions.
The SPN comprises 22 places, 22 timed transitions, and seven immediate transitions. A token at place UTU indicates that a power supply is available. The firing of the UF transition represents the failure of a power utility. The firing of this transition removes a token from the UTU place and stores a token in the UTD place. This new token activates the TI6 transition, and its firing adds ten tokens to the RLED transition. The RLED transition indicates that the respirator is not functioning due to a power system failure. This place enables the TI2 transition, and its firing stores twenty tokens in the BAU place. The BAU place indicates that the battery modules are in user mode. Therefore, the TI7 transition is enabled, and when the TI7 transition is fired, ten tokens return to the RLU place. The RLU place indicates that the respirator is available.
Moreover, when a power grid failure occurs, the respirator can resume operation via the power generator. The GO place indicates that the generator is offline, whereas the GU place indicates that the generator is available. The GSO transition between the GO and GU places represents the time to activate the generator.
When the power system resumes operation, a token returns to the UTU place. With the return of power utility, the transition TI8 is enabled. When enabling the TI8 transition, the 20 tokens previously in the BAU place return to the BALI place. With the tokens in the BALI place, the TE10 transition is enabled, and when fired, the tokens from the BALI place to the BAC place individually until the total of 20 tokens. The firing of the RLF transition represents the failure of a respirator due to usage-related problems. The firing of this transition removes one token from the RLU place and stores one token in the RLD place. This new token enables transition TE18; its firing removes a token from place RLB and adds one at place RLBU. The RLB place represents the backup respirator in Cold Standby. The RLBU place represents the available backup respirator.
A token at the BCU place indicates that a breathing circuit is available. Firing the BCF transition represents the failure of a breathing circuit. Starting the BCF transition adds a token at the BCD place. Once again, this place enables the RLF transition, which, when fired, adds a token at the RLD place because a respirator is only available when the breathing circuit is available. This place again enables transaction TE18, which, when fired, adds a token at place RLBU. Transition TI9 returns the token from the RLBU place to the RLB place.
6 Results
The following section offers a sensitivity analysis of the system’s components using the percentage differentiation technique described in Eq. 4. We also present a sensitivity ranking highlighting each parameter’s impact on the system availability metric, as indicated in Table 2. These rankings guide in identifying components that require improvement and will inform the case studies to be conducted.
Furthermore, we present results with eight different scenarios using the model shown in the previous section. The values for the components of the Respirator Lung system were taken from the document [48]. Scenarios 1, 2, and 3 were generated by stationary analysis [49]. Although structurally limited, scenarios 4, 5, 6, 7, and 8 were generated by simulation by structural analysis after a 28-h wait with over 380,000 states, within the confidence interval, and with a margin of error of 2%. We used the Mercury tool for the process [49]. Table 3 presents the parameters used to feed the proposed model.
6.1 First scenario
This scenario describes the baseline system corresponding to the usual model consisting of one utility, one generator, one switch, two battery modules, one respirator lung, and one breathing circuit. The model becomes a baseline with the following parameters: NR=1, NB=2, and M=0. Each battery module takes 3 h to charge (\(TTLB = 3\)) and has half an hour of operation (\(TTDCB = 0.5\)). Batteries take over when there is no utility and generator power supply, the switch is not working, and battery modules are charged. In this scenario, we consider the repair time for the respirator \(MTTR RL = 168hs\). The corresponding notation is expressed in Eq. (8):
Once power is restored, they return to charging mode automatically (BAUC). Availability of \(A = 0.9665821\) and downtime of \(DTyh = 292.740\).
6.2 Second scenario
This scenario describes that the system works with the same components: one utility, one generator, one switch, two battery modules, one respirator lung, and one breathing circuit. We found that a change in the RL MTTRRL repair time from 168 to 24 h promotes an increase in availability by \(A = 0.9942876\) and a reduction in downtime by \(DTyh = 50.040569\).
In this scenario, we make a change to MTTRRL. We could make the system availability higher by reducing the RL repair time from 168 to 24 h. The MTTR reduction can be achieved through a preventive maintenance system, an efficient repair service, and an adequate stock of spare parts. This means the respirator will be able to run longer with fewer interruptions in service.
6.3 Third scenario
This scenario describes the proposal of an additional RL, working as a RLB backup in a cold standby system. RLB is only available assuming mechanical ventilation once a failure of the RL pattern is identified. We mean 1 RLB for every 10 RL’s represented by NR. We used the variable N to represent the minimum number of respirators in operation. Suppose a 20-bed ICU environment has two RLBs, reducing service downtime. With this scenario, we present an increase in system availability for \(A = 0.9989537\) and, consequently, a reduction in downtime for \(DTyh = 9.164914\). The corresponding notations are expressed in Eqs. (5), (6), and (7).
6.4 Fourth scenario
This scenario describes the proposal of up to 5 lung respirators represented byN with only one running, without the backup Respirator, and we could observe an improvement in the system’s availability. The availability results are shown in Table 4.
In Fig. 4, it is possible to observe that from the fourth respirator onward, there is a decrease in N9s. This reduction is directly related to increased RL, which results in lower availability. In addition, it is important to highlight that the greater the number of equipment, the greater the probability of failures. In this context, stochastic simulations play a crucial role, allowing a development analysis with lower economic cost. This way, it is possible to see that future articles can benefit from this modeling to create new test environments.
6.5 Fifth scenario
This scenario describes a simulation of up to 5 lung respirators represented by N with only one working; however, this time with the backup respirator working. The obtained results are presented in Table 5. In Fig. 5 it is possible to observe that from the fifth respirator, there is a decrease in N9s.
6.6 Sixth scenario
This scenario describes a simulation of 10 respirators lungs represented by N, with at least 7 in operation. The backup Respirator is not used. The results are shown in Table 6. In Fig. 6, it is possible to observe that from the ninth respirator, there is a decrease in N9s.
6.7 Seventh scenario
This scenario describes a simulation of up to 10 lung respirators represented by N with at least 7 of them working with the use of the backup respirator. The results are shown in Table 7. In Fig. 7 it is possible to observe that from the 10th respirator, there is a decrease in N9s.
6.8 Eighth scenario
This scenario describes a simulation with the same configuration as scenario 3. However, we performed the stationary simulation, keeping an error of 2% in scenarios 4, 5, 6, and 7. We suggest changing the battery module timings, with an increase in run time and a decrease in charge time: TTTLB from 3.0 to 0.5 h and TTDCB from 0.5 to 3.0 h. We obtained an increase in availability for \(A = 0. 9993363\) with a confidence interval of \(CI = [0.999332, 0.999340]\) and a reduction in downtime for \(DTyh = 5.813390\) with a confidence interval of \(CI = [5.780200, 5.846579]\).
However, in these eight scenarios, we observed a gradual improvement in the performance of the service offered by the lung respirator. We start the first scenario by describing the usual functioning of the RL system. We suggest changes throughout the other scenarios regarding the MTTRRL, RLB, and timing of the battery modules. These changes positively impacted the RL system’s performance, with an increase in available time and a reduction in offline time. From the first to the eighth final scenario, we got a zero rise for three N9s. From the first scenario to the last one, we obtained a reduction of more than 286 h. The respirators spend less time unavailable, providing a safer hospital service with fewer interruptions during mechanical ventilation and increased patient survival probability.
Table 8 presents the number of components in each scenario, represented by the X values, and the parameters changed during the simulations.
The bar chart in Fig. 8 shows the availabilities of each scenario. The highest availability is obtained when we use more than one respirator.
7 Discussion of scenarios
When analyzing these eight different scenarios, a gradual improvement in the performance of the service offered by the lung respirator was evident. In the first scenario, we present the usual operating equipment of the RL system. We adopt parameters identified through a thorough analysis of documents, which serve as the basis for the scenario.
From the second scenario onwards, our focus shifts to introducing strategic changes designed to improve the overall functionality of the ventilator system. These modifications include changing the respirator’s repair time, the backup respirator’s introduction, and changes to the charging and discharging times for the batteries. With the changes in the baseline system, it was possible to observe a growing increase in system availability while at the same time reducing offline intervals. It became clear that the length of time required for ventilator repairs profoundly impacted the overall accessibility and uptime of the system. As we delve into subsequent scenarios, the ripple effects of these strategic adjustments become increasingly pronounced, underscoring their key role in optimizing system performance and ensuring its sustained operational efficiency.
From the first to the eighth final scenario, we saw an increase in availability from zero to three N9s. We reduced more than 286h of downtime from the first to the last scenario. Respirators spend less time unavailable, providing a safer hospital service with fewer interruptions during mechanical ventilation, more effective ventilatory intervention, and longer patient survival.
8 Conclusion and future works
This study aimed to evaluate the availability of a crucial life support system, specifically a lung respirator, within the intensive care setting. The availability of such equipment is vital in providing optimal care and treatment for critically ill patients. To achieve this goal, we developed analytical models using Stochastic Petri Nets to gain insights into the system and identify potential bottlenecks. These models served as a basis for proposing optimizations to enhance system availability and minimize downtime.
We conducted an evaluation of eight different configurations and observed a remarkable 98\(\%\) improvement in system availability. These findings hold significant implications for healthcare facilities, including ICUs, emergency rooms, and operating rooms, that rely on lung respirators. They can adopt a similar approach to assess the availability of their own systems and identify areas for optimization.
In conclusion, our study showcases the effectiveness of employing Stochastic Petri Nets for assessing the availability of life support systems and proposing strategies to enhance their reliability. Moving forward, we plan to explore alternative methods to optimize lung respirator usage time and examine the availability of additional life support systems in the intensive care setting.
Data Availability
Available upon request.
References
Ramírez M, Navarro S, Clavería C, Molina Y, Cox A, Ramírez M, Navarro S, Clavería C, Molina Y, Cox A (2018) Parental stressors in a pediatric intensive care unit. Revista chilena de pediatria 89(2):182–189
Abate SM, Ahmed Ali S, Mantfardo B, Basu B (2020) Rate of intensive care unit admission and outcomes among patients with coronavirus: A systematic review and meta-analysis. PloS one 15(7):0235653
Keszler M (2017) Mechanical ventilation strategies. In: Seminars in Fetal and Neonatal Medicine, vol. 22,267–274. Elsevier
Zuñiga QGP, Dreyer E, Colombrini M, Nishimura M, Pato N (2004) Ventilação mecânica básica para enfermagem. Atheneu, São Paulo
Chang R, Elhusseiny KM, Yeh Y-C, Sun W-Z (2021) Covid-19 icu and mechanical ventilation patient characteristics and outcomes-a systematic review and meta-analysis. PloS one 16(2):0246318
Coffey CC, Campbell DL, Zhuang Z (1999) Simulated workplace performance of n95 respirators. Am Ind Hygiene Assoc J 60(5):618–624
Savary D, Lesimple A, Beloncle F, Morin F, Templier F, Broc A, Brochard L, Richard J-C, Mercat A (2020) Reliability and limits of transport-ventilators to safely ventilate severe patients in special surge situations. Ann Intensive Care 10:1–10
Blakeman TC, Robinson BR, Branson RD (2010) Battery performance of 4 intensive care ventilator models. Respiratory Care 55(3):317–321
Karaböce B (2018) Inspection and testing of respirators and anaesthesia machines. Inspection of Medical Devices: For Regulatory Purposes, 181–201
Araujo MSd, et al (2020) Análise de confiabilidade de monitores multiparamétricos utilizados em unidades de terapia intensiva
Sandelic M, Sangwongwanich A, Blaabjerg F (2019) Reliability evaluation of pv systems with integrated battery energy storage systems: Dc-coupled and ac-coupled configurations. Electronics 8(9):1059
Nguyen TA, Min D, Choi E, Lee J-W (2021) Dependability and security quantification of an internet of medical things infrastructure based on cloud-fog-edge continuum for healthcare monitoring using hierarchical models. IEEE Internet Things J 8(21):15704–15748
Maciel PRM Performance, Reliability, and Availability Evaluation of Computational Systems, Volume 1: Performance and Background. Chapman and Hall/CRC
Maciel PRM Performance, Reliability, and Availability Evaluation of Computational Systems, Volume 2: Reliability, Availability Modeling, Measuring, and Data Analysis. Chapman and Hall/CRC
Avizienis A, Laprie J-C (1986) Dependable computing: From concepts to design diversity. Proc IEEE 74(5):629–638
Gray J, Siewiorek DP (1991) High-availability computer systems. Computer 24(9):39–48
Wang D, Trivedi KS (2005) Computing steady-state mean time to failure for non-coherent repairable systems. IEEE Trans Reliab 54(3):506–516
Smith R, Trivedi KS, Ramesh A (1988) Performability analysis: measures, an algorithm, and a case study. IEEE Trans Comput 37(4):406–417
Trivedi KS, Malhotra M (1993) Reliability and performability techniques and tools: A survey. In: Messung, Modellierung und Bewertung Von Rechen-und Kommunikationssystemen: 7. ITG/GI-Fachtagung, Aachen, 21.–23. September 1993, 27–48. Springer
Knight J (2012) Fundamentals of Dependable Computing for Software Engineers. CRC Press
Koren I, Krishna CM (2020) Fault-tolerant Systems. Morgan Kaufmann
Dodson B, Nolan D (1999) Reliability Engineering Handbook. Marcel Dekker New York
Symons FJW (1989) Modelling and analysis of communication protocols using numerical petri nets
Natkin S (1980) Les reseaux de petri stochastiques et leur application a l’evaluation des systém informatiques
Molloy MK (1981) On the integration of delay and throughput measures in distributed processing models. AAI8201138
Ajmone Marsan M, Conte G, Balbo G (1984) A class of generalized stochastic petri nets for the performance evaluation of multiprocessor systems. ACM Trans Comput Syst 2(2):93–122. https://doi.org/10.1145/190.191
Marsan MA, Balbo G, Conte G, Donatelli S, Franceschinis G (1994) Modelling with generalized stochastic petri nets, 1st edn. John Wiley & Sons Inc, USA
Marsan MA, Chiola G (1986) On petri nets with deterministic and exponentially distributed firing times. Advances in Petri Nets 1987. Covers the 7th European Workshop on Applications and Theory of Petri Nets. Springer, Berlin, Heidelberg, pp 132–145
Lindemann C (1998) Performance Modelling with Deterministic and Stochastic Petri Nets. John Wiley & Sons, Inc.
German R (2000) Performance Analysis of Communication Systems with Non-Markovian Stochastic Petri Nets. John Wiley & Sons, Inc., Inc. New York, NY, USA
Muppala J, Ciardo G, Trivedi KS (1994) Stochastic reward nets for reliability prediction. Commun Reliab Maintain Serviceability 1(2):9–20
Hamby DM (1994) A review of techniques for parameter sensitivity analysis of environmental models. Environ Monit Assess 32:135–154
Barrett M, Smith M, Elixhauser A, Honigman L, Pines J (2011) Utilization of intensive care services. Healthcare Cost and Utilization Project
Papadakos PJ, Lachmann B (2007) The open lung concept of mechanical ventilation: the role of recruitment and stabilization. Critical Care Clin 23(2):241–250
Brochard L, Slutsky A, Pesenti A (2017) Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respiratory Crit Care Med 195(4):438–442
Pham T, Brochard LJ, Slutsky AS (2017) Mechanical ventilation: state of the art. In: Mayo Clinic Proceedings, v92,1382–1400. Elsevier
Azoulay É, Kouatchet A, Jaber S, Lambert J, Meziani F, Schmidt M, Schnell D, Mortaza S, Conseil M, Tchenio X (2013) Noninvasive mechanical ventilation in patients having declined tracheal intubation. Intensive Care Med 39:292–301
Bates JH, Smith BJ (2018) Ventilator-induced lung injury and lung mechanics. Ann Trans Med 6(19)
Glenski TA, Diehl C, Clopton RG, Friesen RH (2017) Breathing circuit compliance and accuracy of displayed tidal volume during pressure-controlled ventilation of infants: a quality improvement project. Pediatric Anesthesia 27(9):935–941
Ahmed RA, Boyer TJ (2019) Endotracheal tube
Lee JJ, Choi GJ, Lee WJ, Choi SB, Kang H (2022) Effect of active airway warming with a heated-humidified breathing circuit on core body temperature in patients under general anesthesia: a systematic review and meta-analysis with trial sequential analysis. Korean J Anesthesiol
Bertoni M, Spadaro S, Goligher EC (2020) Monitoring patient respiratory effort during mechanical ventilation: lung and diaphragm-protective ventilation. Ann Update Intensive Care Emergency Med 2020:21–35
Srinivasan S, Ramadi KB, Vicario F, Gwynne D, Hayward A, Langer R, Frassica JJ, Baron RM, Traverso G (2020) Individualized system for augmenting ventilator efficacy (isave): a rapidly deployable system to expand ventilator capacity. BioRxiv, 2020–03
Ng QA, Chiew YS, Wang X, Tan CP, Nor MBM, Damanhuri NS, Chase JG (2021) Network data acquisition and monitoring system for intensive care mechanical ventilation treatment. IEEE Access 9:91859–91873
Lee AS (1989) A scientific methodology for mis case studies. MIS quarterly, 33–50
Melo C, Dantas J, Pereira P, Maciel P (2021) Distributed application provisioning over ethereum-based private and permissioned blockchain: availability modeling, capacity, and costs planning. J Supercomput 77(9):9615–9641
Azaron A, Katagiri H, Kato K, Sakawa M (2006) Reliability evaluation of multi-component cold-standby redundant systems. Appl Math Comput 173(1):137–149
Jasper A (2022) Servos Users manual. Available in: https://www.academia.edu/41870952/Manual_Operaç~ao_Servo_S?email_work_card=view-paper. Accessed Oct 10 2022
Maciel P, Matos R, Silva B, Figueiredo J, Oliveira D, Fé I, Maciel R, Dantas J (2017) Mercury: Performance and dependability evaluation of systems with exponential, expolynomial, and general distributions. In: 2017 IEEE 22nd Pacific Rim International Symposium on Dependable Computing (PRDC), 50–57. IEEE
Author information
Authors and Affiliations
Contributions
AM wrote the main text of the manuscript. DS contributed to the study design. AM and PM built the SPN model. PP participated in the construction and development of figures and the construction of the text. LL participated in the construction and development of the tables and model working. DCN participated in the construction of the text and translation into English. Both authors performed the revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare relevant to this article’s content. All the authors certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
This article contains no studies with human participants or animals performed by authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Monte, A.d., Pessoa, P., Silva, D. et al. Assessing the impact of battery charging and discharging times on the availability of mechanical ventilation service. J Reliable Intell Environ 10, 137–150 (2024). https://doi.org/10.1007/s40860-023-00213-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40860-023-00213-9