Abstract
Purpose
Even though the regeneration of periodontium tissue (PDT) around dental implants was of interest in recent years, this process was not investigated from a biomechanical point of view, to date. The purpose of this finite element study was to assess the impact of splinting technique on the initial stability and movement pattern of a tooth-shaped dental implant surrounded by periodontal ligament stem cells (PDLSCs) and was under occlusal forces.
Methods
A composite polymeric tooth-shaped dental implant, i.e., an artificial tooth model was constructed and connected to its adjacent teeth by two splints at the buccal and lingual sides. The displacement pattern of natural and artificial teeth under masticatory load, their center of rotation positions, and von Mises stresses for splints were calculated.
Results
Results of this study showed that splinting of a tooth-shaped dental implant can provide a tooth-like movement for the implant under masticatory loads, by up to 3.4 µm deviation in mesio-distal, 5.1 µm in bucco-lingual, and 9.5 µm in occluso-apical directions, compared with natural teeth. Also, it was shown that nickel-chrome splints have enough strength to provide the required initial stability for the artificial tooth under occlusal forces.
Conclusion
Based on this investigation, the splinting technique can provide enough stability and a tooth-like movement for a tooth-shaped dental implant under masticatory loads. It is speculated that by mimicking the shape and movement pattern of a natural tooth, the implant can transfer proper mechanical stimuli to the PDLSCs around its root, and consequently, would lead to proper regeneration of PDT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Osseointegrated dental implant is a well-accepted rehabilitation method for a lost tooth [1]. The mean survival rate of dental implants is reported to be 94.6%, with a mean follow-up time of 13.4 years [2]. The mechanical and biological characteristics of an implant interface with alveolar bone have a considerable impact on its performance and survival rate [3]. While a dental implant connects directly to the alveolar bone [4], a natural tooth connects to the bone via a periodontal ligament (PDL) [5]. This discrepancy in the interfaces between the tooth and implant with the alveolar bone causes different occlusal and sensory functions. Osseointegrated dental implants are ankylosed, and excessive stress concentration at their crestal region can lead to bone loss [6, 7]. Their use is impossible in children until the completion of dental and skeletal growth [8, 9] and challengeable in people with jaw bone defects [10]. Also, they lack a nervous system and proprioception [11, 12], and are more susceptible to infection and inflammation [13, 14]. Most difficulties associated with osseointegrated dental implants are related to the bony interface and lack of PDL between the implant and alveolar bone.
Seo et al. found that PDLSCs have the potential to differentiate into cementoblast-like and fibroblast-like cells in in-vitro condition, and to form cementum-like and PDL-like tissues in in-vivo condition [15]. Based on this finding, some studies conducted in-vivo tests to develop PDT around dental implants using PDLSCs and reported that with a high proportion of proliferated cells, a PDL-like tissue can be regenerated [16,17,18]. One of the main shortcomings of these kinds of studies was the lack of considering the biomechanical aspects of the regeneration process and not considering the important effects of mechanical stimuli on the PDLSC fate.
It is well-known that cells fate depends on various biological, physical, and chemical parameters [19]. It has been shown that stem cells are highly mechanosensitive and mechanoresponsive and that their growth and differentiation are affected by mechanical stimuli [20], and thus this may present an ideal method for controlling stem cell differentiation. Since PDL exists in a mechanically dynamic environment, mechanical stimuli relevant to the dynamic environment of PDL can differentiate PDLSCs into fibroblasts and cementoblasts cells, and consequently regenerate the PDT [21, 22].
It was shown that dental implants, surrounded by PDLSCs and inserted up-gingiva in the jaw bone, have a risk of failure due to their exposure to masticatory loads [16]. This could be due to a lack of proper initial implant stability during the PDT regeneration process. Like the primary stability in the osseointegration process, which is a key factor in the performance and survival rate of implants [23], periodontio-integrated dental implants need an initial stability before complete periodontium regeneration to bear the occlusal force and provide a proper dynamic environment for complete periodontium tissue regeneration.
Despite recent research relating to periodontio-integrated dental implants, not enough attention was paid to its biomechanical aspects to date. The dynamic environment of the PDL and mechanical stimuli around the tooth root are in direct relationship to the shape and movement pattern of a tooth [24]. In this work, it was hypothesized that the splinting of a tooth-shaped dental implant, i.e., artificial tooth, which connects the crown of the implant to the crown of its adjacent natural teeth, can provide both the initial stability and a tooth-like movement pattern for an implant. Moreover, it was assumed that by mimicking the shape and movement pattern of a natural tooth, the implant can transfer suitable mechanical stimuli to the PDLSCs around its root, and consequently, lead to the proper regeneration of PDT around the implant. The finite element method, as an in-silico tool, offers a powerful means for discovering new aspects of biological systems [25,26,27,28]. So, to test the validity of the above-stated hypotheses, the finite element method was employed to biomechanically investigate the impact of splinting technique on the initial stability and movement pattern of an artificial tooth. In this regard, the displacement pattern of natural and artificial teeth under masticatory loads, their center of rotation positions, and von Mises stresses within the splints were investigated.
2 Materials and Methods
2.1 Construction of the CAD Model
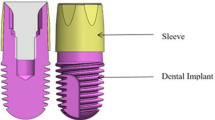
CAD models of the mandible and three teeth, including the 1st molar and the 1st and 2nd premolars, were created using the CT data of a 20 years old healthy male (Fig. 1a). The participant was provided informed consent, which was approved by the Institutional Review Board at TUMS. The point clouds were obtained by Mimics (V10.01, Materialise, Leuven, Belgium), and a 3D solid structure of the mandible and teeth was created by Catia (V5.R19, Dassault Systems, Paris, France). Alveolar bone was composed of a spongy core surrounded by cortical bone, and each tooth consisted of enamel, dentin, and PDT. Four distinct layers were constructed between the root dentin and alveolar bone. These layers, based on their proximity to the root dentin, were the cementum-dentin junction (CDJ), cementum, PDL-cementum junction (PCJ), and PDL (Fig. 1b) [29]. All four layers were considered to have uniform thicknesses. According to the mean values found in the literature, the following thicknesses: 50 µm, 150 µm, 20 µm, and 200 µm were considered for the CDJ, cementum, PCJ, and PDL, respectively [29,30,31,32,33].
3D models of natural and artificial teeth constructed for the finite element analysis: a The natural tooth model including cortical and spongy bones of the mandible, 1st molar, and 1st and 2nd premolars. b Cross-section of the 2nd premolar, which shows the four layers of the PDT, i.e., the CDJ, cementum, PCJ, and PDL. c The artificial tooth model, including the cortical and spongy bones of the mandible, 1st molar, 1st premolar, 2nd premolar artificial tooth, and splints. d Cross-section of the artificial tooth, which shows the empty space around its root. This space is empty because the PDLSCs were ignored due to their insignificant mechanical properties with respect to the splints. e Boundary conditions, including the area of applying distributed load over the crown of the natural and artificial teeth, and the restricted surfaces of the mandibular bones in all directions
Two models were constructed in this study. The first, i.e., the natural tooth model, was the model of a natural mandible and teeth where each tooth was connected to the alveolar bone via PDT (Fig. 1a, b). In the second model, i.e., the artificial tooth model, the PDT of the 2nd premolar was removed, and the material properties of 2nd premolar (its dentin and enamel) were replaced with the material properties of a composite polymer to simulate a tooth-shaped dental implant, the artificial tooth, which was surrounded by PDLSCs. Two nickel-chrome splints (plates with a thickness of 1 mm, width of 4 mm, and length of 17 mm) at the buccal and lingual sides, connected the artificial tooth to the 1st premolar and 1st molar (Fig. 1c). Since the elastic material properties of the splints are much greater than those of the stem cells and due to their insignificant role in the displacement pattern of the artificial tooth, and also in order to enhance the computational efficiency of the simulation, the stem cells were not considered in the model (Fig. 1d).
2.2 Material Properties
Under masticatory loads, the PDL experiences large deformation, and this causes the displacement of teeth [34]. A nonlinear elastic experimental model was employed to simulate the large strains of the PDL under masticatory loads, which was based on a quasi-static response of the PDL [35]. All other components and tissues were considered as linear, elastic, isotropic, and homogenous materials (Table 1).
2.3 Finite Element Model Generation and Analysis
All simulations were performed using ANSYS (ANSYS Inc., Canonsburg, Pennsylvania, United States). The natural and artificial teeth FE models (Fig. 1) contain 830,251 and 812,531 elements, respectively, and all the elements were of a 10-Node tetrahedral structural solid type. The convergence of the mesh for all models was successfully tested. The three Cartesian directions (X, Y, and Z) were coincided with the mesio-distal, bucco-lingual, and occluso-apical tooth orientations, respectively (Fig. 1). The mesial and distal surfaces of the alveolar bone were restricted in all directions (Fig. 1e). Bonded contacts were used for all interfaces in both models, including the connections between periodontium tissue layers, PDL to the bone, cortical bone to spongy bone, and CDJ to dentin [28, 38]. Occlusal pressure was assumed to be 3 MPa, which is equivalent to a 100 N concentrated force in occluso-apical direction, and was applied to the natural and artificial teeth on the uppermost surface of the crown with a total area of 33.4 mm2 (Fig. 1e), then the displacement of 2nd natural and artificial premolar teeth under loading and their center of rotation (CoR) positions were calculated. It should be noted that CoRs were calculated from a vertex at the apical region of the natural and artificial teeth. Moreover, von Mises stress, which can be used to predict the risk of failure in ductile materials [39], was used to check whether or not the splints construct will fail under load.
2.4 Validation of Finite Element Model
In order to compare the force–displacement pattern of 2nd premolar in the natural tooth model with results of other studies, and check the validity of its FE model, the occluso-apical displacement of the 2nd premolar tooth under the masticatory load was calculated. The predicted force–displacement pattern of the 2nd premolar in the natural tooth model at the center of crown, in comparison with other studies [40,41,42], is shown in Fig. 2. A maximum difference of 1.4 µm (mean difference = 1.2 µm) was found between the displacement of the 2nd premolar tooth in the present study with the results of Maceri et al. [41], for the same forces. The displacement pattern of the 2nd premolar under masticatory load in the natural tooth FE model showed reasonable agreement with experimental and numerical results of other studies (Fig. 2).
3 Results
This section encompasses results obtained for the displacement pattern of the natural and artificial teeth under masticatory load, their center of rotation positions, and von Mises stress in splints.
3.1 Displacements of Natural and Artificial Teeth Under Masticatory Load
The displacement of the natural and artificial teeth along the three Cartesian directions (X, Y, and Z) caused by a distributed load of 3 MPa are shown in Fig. 3. The displacements are shown along two paths on the root of the natural and artificial teeth, the first on the X–Z plane (Path A) and the second on the Y–Z plane (Path B). The maximum difference of displacements between the natural and artificial teeth models in X-, Y-, and Z directions, respectively, along path A were 3.4 μm (mean difference = 1.6 μm), 3.5 μm (mean difference = 1.9 μm), and 9.5 μm (mean difference = 5.4 μm), and along path B were 3.2 μm (mean difference = 1.6 μm), 5.1 μm (mean difference = 1.1 μm), and 4.5 μm (mean difference = 0.5 μm). As expected, due to the load direction, the largest displacements occurred along the long axis of the tooth, i.e., in the Z-direction. Bucco-lingual (Y) displacements in the natural and artificial teeth, respectively, were no more than 12%, and 7% of the displacement magnitude found in the Z-direction. In addition to the Z-direction, motion was also observed along the X-direction in both models.
Comparison of displacements of the natural and artificial teeth along Path A (on the X–Z plane) and Path B (on the Y–Z plane). a Representation of path A and path B at the root of the 2nd premolar tooth, b displacements of the natural and artificial tooth along path A (on X–Z plane), and c displacements of the natural and artificial tooth along path B (on the Y–Z plane). Displacements are shown for a distributed load of 3 MPa
3.2 Position of Center of Rotation of Natural and Artificial Teeth
The natural and artificial teeth both experience a rotation on the X–Z and Y–Z planes, under a 3 MPa occluso-apical distributed load. The results of this work showed that the artificial tooth’s CoR on the X–Z plane is close to that of the natural tooth, and their difference is 60 µm in the X and 120 µm in the Z directions, respectively. On the Y–Z plane, the artificial tooth’s CoR has 140 µm deviation in the Y and 300 µm deviation in the Z direction, as compared to the natural tooth's CoR (Table 2).
3.3 Von Mises Stress Within Splints
For the artificial tooth, maximum von Mises stresses in the splints occurred at their connection regions to the implant, as shown in Fig. 4. The maximum stress observed in the splints under 3 MPa occluso-apical distributed load was much less than 500 MPa, which is the critical value of material failure for the material used for the splints (Table 1), i.e., nickel-chrome alloy.
4 Discussion
Even though investigations were recently conducted on the regeneration of PDT around dental implants using PDLSCs [16,17,18], the lack of biomechanical investigations on this topic is quite evident in the current literature. The main scope of this work was to biomechanically assess the impact of splinting technique on the initial stability and movement pattern of a tooth-shaped dental implant using the finite element method. This study was a part of another investigation still in progress that aims at making tooth-like composite dental implants, and testing it in animals, with the ultimate goal of coming up with a new generation of bio-mimicked dental implants. In this work, it was hypothesized that using a tooth-shaped dental implant, called an artificial tooth, and applying splinting technique, i.e., connecting the crown of the implant to the crowns of its adjacent natural teeth, can provide sufficient initial stability and tooth-like movement for the dental implant. Two types of models were considered in this study. The first, i.e., the natural tooth model, was a model of the natural mandible and teeth in which each tooth was connected to the alveolar bone via PDT (see Fig. 1a, b). In the second model, i.e., the artificial tooth model, the PDT of the 2nd premolar was removed, and the material properties of dentin and enamel were changed to the material properties of a composite polymer to simulate a tooth-shaped dental implant surrounded by PDLSCs (see Fig. 1c). Due to the negligible modulus of elasticity and material properties, and consequently insignificant effect of the stem cells on the displacement pattern of the artificial tooth, they were not considered in the artificial tooth model (see Fig. 1d). Two splints at the buccal and lingual sides of the artificial tooth connected its crown to the crowns of the 1st premolar and 1st molar (see Fig. 1c). The displacement of the 2nd premolar natural tooth and artificial tooth under distributed occluso-apical loading (see Fig. 1e), their position of the center of rotation (CoR), and von Mises stresses in the splints were investigated in this study.
After investigating the displacement pattern of the natural and artificial teeth under a 3 MPa occluso-apical distributed load, results showed that the artificial tooth fixed by splints followed the displacement pattern of the natural tooth, with a maximum of 3.4 µm deviation in the mesio-distal, 5.1 µm in the bucco-lingual, and 9.5 µm in the occluso-apical directions (see Fig. 3). Also, it was shown that the nickel-chrome splints have enough strength to avoid failure under 3 MPa occluso-apical distributed load (see Fig. 4).
PDLSCs are highly mechanosensitive and mechanoresponsive, and thus mechanical stimuli can affect their proliferation and differentiation [43,44,45]. Chen et al. showed that low-magnitude stretching of mesenchymal stem cells (MSCs) was possibly involved in the early osteoblastic differentiation of MSCs, whereas high-magnitude stretching upregulated the mRNA expressions of tendon/ligament-related genes [46]. After surrounding the root of the implant and being inserted into the jaw bone, PDLSCs experiences mechanical stimuli, which are in a direct relationship with the shape and movement pattern of the implant. Sub-gingiva insertion of an implant, covered by PDLSCs, eliminates the movement and dynamic environment of the implant root, and consequently, mechanical stimuli, which are essential to cause differentiation of PDLSCs into fibroblasts. Whereas, our study showed that a composite polymeric tooth-shaped dental implant splinted to its adjacent natural teeth could provide a tooth-like movement pattern, and due to its tooth-shaped geometry, it is speculated that proper mechanical stimuli can transfer to the PDLSCs around the implant’s root.
On the other hand, it was shown that up-gingiva insertion of a periodontio-integrated dental implant without the use of any fixation method or splinting technique has the risk of failure at the early stages of regeneration due to its exposure to masticatory loads [16]. This may be due to a lack of proper initial stability and fixation of the implant, and accordingly, its inability to bear occlusal forces in the initial stages of regeneration. During the first couple of days after implant insertion, its root is only surrounded by PDLSCs, which are mechanically weak and have a very low modulus of elasticity [47]. Thus, using a fixation method in the early stage of regeneration plays a crucial role in implant ability to bear the masticatory loads. By employing von Mises stress, as a well-known criterion for the failure of ductile materials, this study showed that an artificial tooth fixed with the splinting technique as a fixation method can tolerate occlusal forces, and can provide the load-bearing of normal mastication right after surgery (see Fig. 4).
Primary (mechanical) stability is associated with the macro-mechanical engagement of an implant with its surrounding bone [23]. After a while, the stability of the implant improves through bone regeneration and the remodeling phenomena, and a micro-mechanical engagement is achieved, which is called secondary (biological) stability [48, 49]. Secure primary stability is positively associated with secondary stability [50], and a dental implant needs both types of stability throughout its lifetime to securely engage with the alveolar bone and bear occlusal forces. In periodontio-integrated dental implants, the stability achieved through the application of splints, is temporary and can be useful until the regeneration of PDT is complete. After regeneration, the splints should be removed because the PDT is now sufficient to provide stability for the dental implant. Thus, the term initial stability was used in this study instead of primary stability to correctly identify the specific kind of stability used in the FE model.
There were some limitations in this study, which need to be stated here. First, the performance of the implanted constructs was investigated for just the early stage of the periodontium regeneration, i.e., when the implant was surrounded only by PDLSCs, and no other tissues were present around the implant. Secondly, in the modeling section, the periodontium tissue layers were considered to be uniform, and most tissues were modeled as a linear elastic material, which can lead to some errors in the predicted stress, as well as in the movement pattern. Lastly, no experimental tests were conducted for this research, and the validation of the models used here was done by comparing it with other studies reported in the literature.
5 Conclusion
The results of this study showed that splinting technique provides enough stability and a tooth-like movement for a tooth-shaped dental implant under masticatory loads (see Figs. 3 and 4), and thus it can be employed during the regeneration process of periodontio-integrated dental implants in the future. This work tried to shed some light on providing initial stability and tooth-like movement for a periodontio-integrated dental implant using the finite element analysis. It is hoped that this study can pave the way for other researchers to get involved in this field and improve currently used dental implants using mechanobiological perspectives and approaches.
Data Availability
The data supporting the results of this article are available.
Code Availability
No specific codes were written for this research.
References
Moy, P. K., Medina, D., Shetty, V., & Aghaloo, T. L. (2005). Dental implant failure rates and associated risk factors. International Journal of Oral & Maxillofacial Implants, 20(4), 569–577.
Moraschini, V., Poubel, L. A. D. C., Ferreira, V. F., & Barboza, E. D. S. P. (2015). Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. International Journal of Oral and Maxillofacial Surgery, 44(3), 377–388. https://doi.org/10.1016/j.ijom.2014.10.023.
Santander, S., Alcaine, C., Lyahyai, J., Perez, M. A., Rodellar, C., Doblare, M., et al. (2012). In vitro osteoinduction of human mesenchymal stem cells in biomimetic surface modified titanium alloy implants. Dental Materials Journal, 31(5), 843–850.
Albrektsson, T., Branemark, P. I., Hansson, H. A., & Lindstrom, J. (1981). Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthopaedica Scandinavica, 52(2), 155–170.
Nanci, A. (2013). Ten cate's oral histology: Development, structure, and function. Amsterdam: Elsevier.
Misch, C. E. (2007). A stress theorem for implant dentistry. In Contemporary implant dentistry (3rd ed.). St-Louis: Mosby Elsevier.
Sennerby, L., Rocci, A., Becker, W., Jonsson, L., Johansson, L. A., & Albrektsson, T. (2008). Short-term clinical results of Nobel Direct implants: a retrospective multicentre analysis. Clinical Oral Implants Research, 19(3), 219–226. https://doi.org/10.1111/j.1600-0501.2007.01410.x.
Op Heij, D. G., Opdebeeck, H., van Steenberghe, D., & Quirynen, M. (2003). Age as compromising factor for implant insertion. Periodontology, 2000(33), 172–184.
Percinoto, C., Vieira, A. E., Barbieri, C. M., Melhado, F. L., & Moreira, K. S. (2001). Use of dental implants in children: A literature review. Quintessence International, 32(5), 381–383.
Mittal, Y., Jindal, G., & Garg, S. (2016). Bone manipulation procedures in dental implants. Indian Journal of Dentistry, 7(2), 86–94. https://doi.org/10.4103/0975-962X.184650.
Bhatnagar, V. M., Karani, J. T., Khanna, A., Badwaik, P., & Pai, A. (2015). Osseoperception: An implant mediated sensory motor control—A review. Journal of Clinical and Diagnostic Research: JCDR, 9(9), ZE18–ZE20. https://doi.org/10.7860/JCDR/2015/14349.6532.
Mishra, S. K., Chowdhary, R., Chrcanovic, B. R., & Branemark, P. I. (2016). Osseoperception in dental implants: A systematic review. Journal of Prosthodontics, 25(3), 185–195. https://doi.org/10.1111/jopr.12310.
Giannobile, W. V. (2010). Getting to the root of dental implant tissue engineering. Journal of Clinical Periodontology, 37(8), 747–749. https://doi.org/10.1111/j.1600-051X.2010.01589.x.
Lindhe, J., Berglundh, T., Ericsson, I., Liljenberg, B., & Marinello, C. (1992). Experimental breakdown of peri-implant and periodontal tissues. A study in the beagle dog. Clinical Oral Implants Research, 3(1), 9–16.
Seo, B. M., Miura, M., Gronthos, S., Bartold, P. M., Batouli, S., Brahim, J., et al. (2004). Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet, 364(9429), 149–155. https://doi.org/10.1016/s0140-6736(04)16627-0.
Gault, P., Black, A., Romette, J. L., Fuente, F., Schroeder, K., Thillou, F., et al. (2010). Tissue-engineered ligament: Implant constructs for tooth replacement. Journal of Clinical Periodontology, 37(8), 750–758. https://doi.org/10.1111/j.1600-051X.2010.01588.x.
Lin, Y., Gallucci, G. O., Buser, D., Bosshardt, D., Belser, U. C., & Yelick, P. C. (2011). Bioengineered periodontal tissue formed on titanium dental implants. Journal of Dental Research, 90(2), 251–256. https://doi.org/10.1177/0022034510384872.
Oshima, M., Inoue, K., Nakajima, K., Tachikawa, T., Yamazaki, H., Isobe, T., et al. (2014). Functional tooth restoration by next-generation bio-hybrid implant as a bio-hybrid artificial organ replacement therapy. Scientific Reports, 4, 6044. https://doi.org/10.1038/srep06044.
Lutolf, M. P., Gilbert, P. M., & Blau, H. M. (2009). Designing materials to direct stem-cell fate. Nature, 462, 433. https://doi.org/10.1038/nature08602.
Goetzke, R., Sechi, A., De Laporte, L., Neuss, S., & Wagner, W. (2018). Why the impact of mechanical stimuli on stem cells remains a challenge. Cellular and Molecular Life Sciences, 75(18), 3297–3312. https://doi.org/10.1007/s00018-018-2830-z.
Oortgiesen, D. A., Yu, N., Bronckers, A. L., Yang, F., Walboomers, X. F., & Jansen, J. A. (2012). A three-dimensional cell culture model to study the mechano-biological behavior in periodontal ligament regeneration. Tissue Engineering Part C: Methods, 18(2), 81–89. https://doi.org/10.1089/ten.TEC.2011.0367.
Kim, J. H., Kang, M. S., Eltohamy, M., Kim, T. H., & Kim, H. W. (2016). Dynamic mechanical and nanofibrous topological combinatory cues designed for periodontal ligament engineering. PLoS ONE, 11(3), e0149967. https://doi.org/10.1371/journal.pone.0149967.
Javed, F., Ahmed, H. B., Crespi, R., & Romanos, G. E. (2013). Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interventional Medicine & Applied Science, 5(4), 162–167. https://doi.org/10.1556/IMAS.5.2013.4.3.
Cardaropoli, D., & Gaveglio, L. (2007). The influence of orthodontic movement on periodontal tissues level. Seminars in Orthodontics, 13(4), 234–245. https://doi.org/10.1053/j.sodo.2007.08.005.
Dolgov, V. Y., Klyshnikov, K. Y., Ovcharenko, E. A., Glushkova, T. V., Batranin, A. V., Agienko, A. S., et al. (2019). Finite element analysis-based approach for prediction of aneurysm-prone arterial segments. Journal of Medical and Biological Engineering, 39(1), 102–108. https://doi.org/10.1007/s40846-018-0422-x.
Marinozzi, F., Bini, F., De Paolis, A., De Luca, R., & Marinozzi, A. (2015). Effects of hip osteoarthritis on mechanical stimulation of trabecular bone: A Finite Element Study. Journal of Medical and Biological Engineering, 35(4), 535–544. https://doi.org/10.1007/s40846-015-0061-4.
Rouhi, G., Tahani, M., Haghighi, B., & Herzog, W. (2015). Prediction of stress shielding around orthopedic screws: Time-dependent bone remodeling analysis using finite element approach. Journal of Medical and Biological Engineering, 35(4), 545–554. https://doi.org/10.1007/s40846-015-0066-z.
Zargham, A., Geramy, A., & Rouhi, G. (2016). Evaluation of long-term orthodontic tooth movement considering bone remodeling process and in the presence of alveolar bone loss using finite element method. Orthodontic Waves, 75(4), 85–96. https://doi.org/10.1016/j.odw.2016.09.001.
Ho, S. P., Marshall, S. J., Ryder, M. I., & Marshall, G. W. (2007). The tooth attachment mechanism defined by structure, chemical composition and mechanical properties of collagen fibers in the periodontium. Biomaterials, 28(35), 5238–5245. https://doi.org/10.1016/j.biomaterials.2007.08.031.
Natali, A. N., Pavan, P. G., & Scarpa, C. (2004). Numerical analysis of tooth mobility: Formulation of a non-linear constitutive law for the periodontal ligament. Dental Materials, 20(7), 623–629. https://doi.org/10.1016/j.dental.2003.08.003.
Pietrzak, G., Curnier, A., Botsis, J., Scherrer, S., Wiskott, A., & Belser, U. (2002). A nonlinear elastic model of the periodontal ligament and its numerical calibration for the study of tooth mobility. Computer Methods in Biomechanics & Biomedical Engineering, 5(2), 91–100. https://doi.org/10.1080/10255840290032117.
Kato, S., Nakagaki, H., Kunisaki, H., Sugihara, N., Noguchi, T., Ito, F., et al. (1992). The thickness of the sound and periodontally diseased human cementum. Archives of Oral Biology, 37(8), 675–676. https://doi.org/10.1016/0003-9969(92)90132-r.
Ho, S. P., Goodis, H., Balooch, M., Nonomura, G., Marshall, S. J., & Marshall, G. (2004). The effect of sample preparation technique on determination of structure and nanomechanical properties of human cementum hard tissue. Biomaterials, 25(19), 4847–4857. https://doi.org/10.1016/j.biomaterials.2003.11.047.
Naveh, G. R., Lev-Tov Chattah, N., Zaslansky, P., Shahar, R., & Weiner, S. (2012). Tooth-PDL-bone complex: Response to compressive loads encountered during mastication—A review. Archives of Oral Biology, 57(12), 1575–1584. https://doi.org/10.1016/j.archoralbio.2012.07.006.
Nishihira, M., Yamamoto, K., Sato, Y., Ishikawa, H., & Natali, A. N. (2003). Mechanics of periodontal ligament. In A. N. Natali (Ed.), Dental biomechanics. Bristol, PA: Taylor and Francis Inc.
Pegoretti, A., Fambri, L., Zappini, G., & Bianchetti, M. (2002). Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials, 23(13), 2667–2682. https://doi.org/10.1016/S0142-9612(01)00407-0.
Ho, S. P., Balooch, M., Goodis, H. E., Marshall, G. W., & Marshall, S. J. (2004). Ultrastructure and nanomechanical properties of cementum dentin junction. Journal of Biomedical Materials Research Part A: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials, 68(2), 343–351. https://doi.org/10.1002/jbm.a.20061.
Zhao, Y., Wang, W., Xin, H., Zang, S., Zhang, Z., & Wu, Y. (2013). The remodeling of alveolar bone supporting the mandibular first molar with different levels of periodontal attachment. Medical & Biological Engineering & Computing, 51(9), 991–997. https://doi.org/10.1007/s11517-013-1078-x.
De Groot, R., Peters, M. C., De Haan, Y. M., Dop, G. J., & Plasschaert, A. J. (1987). Failure stress criteria for composite resin. Journal of Dental Research, 66(12), 1748–1752. https://doi.org/10.1177/00220345870660121001.
Brunski, J. B. (1992). Biomechanical factors affecting the bone-dental implant interface. Clinical Materials, 10(3), 153–201.
Maceri, F., Martignoni, M., & Vairo, G. (2007). Mechanical behaviour of endodontic restorations with multiple prefabricated posts: A finite-element approach. Journal of Biomechanics, 40(11), 2386–2398. https://doi.org/10.1016/j.jbiomech.2006.11.018.
Ren, L. M., Wang, W. X., Takao, Y., & Chen, Z. X. (2010). Effects of cementum-dentine junction and cementum on the mechanical response of tooth supporting structure. Journal of Dentistry, 38(11), 882–891. https://doi.org/10.1016/j.jdent.2010.07.013.
Huang, H., Yang, R., & Zhou, Y. H. (2018). Mechanobiology of periodontal ligament stem cells in orthodontic tooth movement. Stem Cells International, 2018, 6531216. https://doi.org/10.1155/2018/6531216.
Zhang, C., Li, J., Zhang, L., Zhou, Y., Hou, W., Quan, H., et al. (2012). Effects of mechanical vibration on proliferation and osteogenic differentiation of human periodontal ligament stem cells. Archives of Oral Biology, 57(10), 1395–1407. https://doi.org/10.1016/j.archoralbio.2012.04.010.
Shen, T., Qiu, L., Chang, H., Yang, Y., Jian, C., Xiong, J., et al. (2014). Cyclic tension promotes osteogenic differentiation in human periodontal ligament stem cells. International Journal of Clinical and Experimental Pathology, 7(11), 7872–7880.
Chen, Y. J., Huang, C. H., Lee, I. C., Lee, Y. T., Chen, M. H., & Young, T. H. (2008). Effects of cyclic mechanical stretching on the mRNA expression of tendon/ligament-related and osteoblast-specific genes in human mesenchymal stem cells. Connective Tissue Research, 49(1), 7–14. https://doi.org/10.1080/03008200701818561.
Khani, M. M., Tafazzoli-Shadpour, M., Rostami, M., Peirovi, H., & Janmaleki, M. (2014). Evaluation of mechanical properties of human mesenchymal stem cells during differentiation to smooth muscle cells. Annals of Biomedical Engineering, 42(7), 1373–1380. https://doi.org/10.1007/s10439-013-0889-0.
Natali, A. N., Carniel, E. L., & Pavan, P. G. (2009). Investigation of viscoelastoplastic response of bone tissue in oral implants press fit process. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 91(2), 868–875. https://doi.org/10.1002/jbm.b.31469.
Greenstein, G., Cavallaro, J., Romanos, G., & Tarnow, D. (2008). Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: A review. Journal of Periodontology, 79(8), 1317–1329. https://doi.org/10.1902/jop.2008.070067.
Davies, J. E. (1998). Mechanisms of endosseous integration. International Journal of Prosthodontics, 11(5), 391–401.
Acknowledgements
The authors would like to thank the Amirkabir University of Technology, Iran.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by HJ, GR, and NA. The first draft of the manuscript was written by HJ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Rights and permissions
About this article
Cite this article
Jokar, H., Rouhi, G. & Abolfathi, N. The Effects of Splinting on the Initial Stability and Displacement Pattern of Periodontio-Integrated Dental Implants: A Finite Element Investigation. J. Med. Biol. Eng. 40, 719–726 (2020). https://doi.org/10.1007/s40846-020-00544-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-020-00544-5