Abstract
Purpose of the review
Some individuals experience greater susceptibility to adverse health outcomes than others, which is known as frailty. There are two main approaches to operationalizing frailty—the phenotypic approach and the deficit accumulation approach. We review these approaches and discuss their respective strengths and limitations. Both approaches can advance our understanding of the unexplained heterogeneity in health outcomes observed among individuals with systemic lupus erythematosus (SLE).
Recent findings
A recent study using the frailty phenotype identified a higher than expected prevalence of frailty among women with SLE. Phenotypic frailty was associated with increased risk of subsequent functional decline and mortality. In a separate initiative, data from the Systemic Lupus International Collaborating Clinics (SLICC) inception cohort was used to construct a frailty index (FI) to measure deficit accumulation in SLE. FI scores in the SLICC inception cohort were higher than expected for similarly aged healthy individuals. Higher SLICC-FI values predicted increased risk of future organ damage accrual and mortality.
Summary
Emerging evidence demonstrates that frailty is a useful concept for improving our understanding of the variability in health outcomes observed among individuals with SLE. Preventing and treating frailty in SLE may lead to reduced morbidity and mortality in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune inflammatory disease with the potential to involve any organ system [1]. The clinical manifestations of SLE are diverse and highly variable between individuals [1]. Similarly, health outcomes in SLE are heterogeneous and challenging to predict. The clinical course of SLE can range from a relatively benign chronic illness to progressive organ damage and fulminant organ failure.
Given this variability in health trajectories, there is an unmet need to identify SLE patients, ideally early in their disease, who are at greatest risk for adverse outcomes. Although such information has the potential to alter patient management, tools for effective prognostication in SLE remain limited. This may reflect the inability of traditional SLE measures to accurately capture the complex interplay between the disease, adverse treatment effects, comorbidities, functional status, social vulnerability, and health protective factors in determining overall risk.
The concept of frailty initially emerged through the study of community-dwelling older adults as a means to describe the variability observed between aging individuals with respect to their susceptibility to adverse outcomes [2, 3]. Frailty has since become a topic of great interest across a wide range of medical disciplines [4,5,6]. One area of inquiry has been the evaluation of frailty in specific populations where accelerated aging is commonly observed, such as childhood cancer survivors [7] and individuals living with HIV/AIDS [8]. Frailty may be particularly relevant in a complex, multisystem disease like SLE, where the risk of morbidity and mortality is increased compared with similarly aged individuals in the general population [9,10,11], and where significant unexplained heterogeneity in health outcomes exists between patients [1].
Frailty: A clinical syndrome or a multidimensional risk state?
Individuals of the same age vary in their health status and life expectancy. Likewise, in non-human species, same-strain animals raised in controlled environments develop age-related diseases and die at variable rates [12]. This time-honored clinical observation of variability in the risk of death despite identical chronological age gave rise to the term “frailty” [13]. The term has subsequently been generalized to describe the predisposition for certain individuals to experience greater vulnerability to adverse health outcomes than others despite comparable exposures [3].
Frailty can be conceptualized as a diminished capacity to withstand and recover from health stressors due to a loss of physiologic reserve. Based on this definition, a definitive diagnosis of frailty can only be confirmed retrospectively through the observation of a disproportionately poor response to a stressful event, such as a serious infection or major surgery. In order for frailty to be clinically useful, it is necessary to detect it prior to an inciting event to allow opportunity for intervention. Thus, alternative strategies are needed to identify frailty prospectively.
How best to evaluate frailty remains a subject of ongoing debate [14]. While numerous methods have been proposed [15, 16], the two main approaches for operationalizing frailty are as follows: (1) The phenotypic approach, which views frailty as a clinical syndrome characterized by specific physical criteria; and (2) the deficit accumulation approach, which regards frailty as a multidimensional risk state that can be quantified using a frailty index [17]. Rather than determining the superiority of one approach over the other, we feel that each approach has strengths and limitations and both can provide valuable information when used to measure frailty among individuals with SLE [18, 19].
The phenotypic approach to frailty
The phenotypic approach regards frailty as a clinical syndrome that is characterized by a cluster of physical signs and symptoms commonly observed among vulnerable older adults. This clinical phenotype arises through progressive, age-related loss of muscle mass and strength, known as sarcopenia, which is accelerated in frail older adults [20]. The phenotypic approach views frailty as a biological syndrome of aging that can be multifactorial in etiology but leads to the common pathophysiologic pathway of sarcopenia [21, 22]. Clinically, this manifests as a cycle of physical decline with concomitant reductions in physical activity, gait speed, muscle strength, energy level, and nutritional status [20].
The Fried frailty phenotype
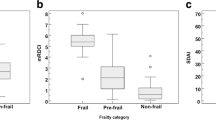
In 2001, Fried and colleagues [20] published the original frailty phenotype, which identified physical frailty based on five clinical criteria (Table 1). Individuals meeting three or more criteria were classified as frail, while those fulfilling one or two criteria were considered pre-frail, and those without any criteria were said to be non-frail or robust [20]. The Fried phenotype was first evaluated using observational data from over 5000 community-dwelling older adults in the USA enrolled in the Cardiovascular Health Study [20]. Seven percent of participants were classified as frail and were at increased risk for functional disability, hospitalizations, and mortality when compared with those who were non-frail [20]. Pre-frailty status showed intermediate risk for these outcomes and was associated with increased risk of progression to phenotypic frailty over time [20]. These findings have since been replicated in numerous cohort studies [23,24,25,26].
Chronic medical conditions are associated with many risk factors for sarcopenia, including poor nutrition, malabsorption, disuse atrophy, and elevated levels of pro-inflammatory cytokines [22]. Thus, it is not surprising that the prevalence of phenotypic frailty is increased among individuals with chronic conditions such as congestive heart failure [27], chronic obstructive pulmonary disease [28], and end-stage renal disease [6]. Similar to older adults, the presence of phenotypic frailty in these disease-specific cohorts is associated with increased risk of adverse health outcomes, including hospitalizations and mortality [6, 27,28,29].
Phenotypic frailty in SLE
The development of sarcopenia and phenotypic frailty may be accelerated in SLE. Several individual elements of the frailty phenotype have been observed with increased frequency in SLE, including muscle weakness [30, 31], exhaustion [30, 32, 33], and physical inactivity [34, 35]. Higher prevalence of objectively measured sarcopenia is reported among SLE patients compared with healthy controls, with the greatest risk in individuals with more active SLE [36]. Applying the Fried frailty phenotype in a prevalent cohort of 152 adult women with SLE, 20.4% were classified as frail, while 50.7% were considered pre-frail. This is a high prevalence of frailty compared with that of similarly aged women in the general population, in whom the expected prevalence of frailty is < 10% [37]. Women with SLE who were classified as frail at baseline were at increased risk of functional decline and cognitive impairment during follow-up. Furthermore, compared with non-frail SLE patients, the presence of phenotypic frailty at baseline was associated with a nearly sixfold increase in the risk of death during follow-up. These findings suggest that phenotypic frailty is a relevant concept in SLE that warrants further investigation.
The deficit accumulation approach to frailty
Frailty may also be considered a multidimensional risk state defined by accelerated deficit accumulation [38, 39]. As individuals age, their susceptibility to adverse outcomes is determined by the number of health problems they accumulate over time. The accrual of health deficits impairs the individual’s ability to respond and recover from future health challenges [38, 39]. Individuals with few deficits are considered relatively fit or robust, while those with an increasing number of health problems are considered increasingly frail and at greater risk for adverse outcomes (Fig. 1).
The impact of deficit accumulation on recovery from health challenges, using a hypothetical frailty index (FI) constructed from a total of 50 health deficits. The black arrows represent the occurrence of an inciting health event (e.g., serious infection or major surgery). a This individual possesses only 4 of the 50 health deficits for an FI score of 0.08, and is therefore considered non-frail or robust. A new insult may only cause a minor disruption in their overall health status, with rapid recovery back to their previous baseline. b With 14 of the 50 total deficits and an FI score of 0.28, this individual would be considered frail. When faced with a new health challenge, they will become more unwell. Recovery will be slower, and they may never fully recovery back to their previous baseline. c An individual possessing 24 of the 50 health deficits would be considered severely frail, based on an FI score of 0.48. They may not have enough physiologic reserve to withstand an additional health insult, and may die as a result
That many small effects can aggregate to produce larger ones is well-recognized in other disciplines. Applying this principle in medicine allows us to capture the cumulative effect of numerous small deficits, which individually may lack statistical significance, but once combined will have meaningful impact. In this approach, the total number of health problems is the critical factor, with less emphasis placed on the effects of specific, individual risk factors.
Measuring deficit accumulation using a frailty index
The deficit accumulation approach is operationalized using a frailty index (FI) [17], which can be developed from any existing health dataset by following a standard procedure for FI construction [40]. First, one must identify the health deficits to be included, using the criteria outlined in Table 2. In addition to comorbidities, a frailty index must also include variables that impact recovery and repair potential, including measures of function, resiliency, and other health protective factors [40]. By including these domains, FI scores have the potential to fluctuate either up or down, reflecting dynamic changes in frailty over time.
Once identified, each health deficit is assigned a scoring system from 0 to 1. The deficit will be coded as “0” when completely absent and coded as “1” when fully present. Intermediate values between 0 and 1 can be used to represent partial expression of deficits [40]. However, the benefit of a more graded scoring system versus dichotomization of individual deficits appears to be negligible [39••]. Finally, health deficits are combined to produce an FI score, calculated from the sum of individual health deficit scores divided by the total number of health deficits considered [40]. For example, using an FI with a total of 50 health deficits, an individual with 10 deficits fully expressed would have an FI score of 10/50 = 0.20. Because frailty may arise via multiple different pathways, an FI must include a large number of deficits in order to capture all aspects of frailty. Prior work suggests that at least 30–40 health deficits are required to produce stable and precise estimates of frailty [41].
Properties of the frailty index
While the FI was first developed to measure frailty among community-dwelling older adults [40,41,42,43], it has since been applied to several disease-specific clinical cohorts [44,45,46]. The generalizability of this approach even extends to animal models [47•]. Across these different settings, the properties of the FI have remained remarkably consistent. This reproducibility is particularly impressive given that each FI measure incorporates different types and numbers of health deficits based on data availability. With respect to the FI, it is not necessary to measure the same items, or even the same number of items, in order to obtain similar results.
There appears to be a biological limit to the number of health deficits one individual can accumulate, beyond which any further deficit accumulation will be incompatible with life. Among community-dwelling older adults, FI measures have consistently demonstrated a 99% submaximal limit of approximately 0.70, or 70% of the total number of deficits considered [40, 41, 48]. In other words, at FI values > 0.70, the risk of mortality is so great that < 1% of individuals would survive the accrual of an additional health deficit. Similar submaximal limit values have been reported in disease-specific cohorts [8, 44].
In the general population, as well as in clinical cohorts, a consistent relationship between sex, frailty, and mortality risk has been observed. Women tend to accumulate more deficits and exhibit higher FI scores than men at a given age [49]. However, women also tend to survive longer than men, with men demonstrating higher mortality risk than women at a given FI score [49]. Interestingly, these sex differences have also been observed between male and female C57BL/6 mice [50].
In the general population, FI scores follow a gamma distribution [40, 41]—most people exhibit relatively low FI scores resulting in positive skew, while a small number of more frail individuals are represented by the long, right-sided tail of the distribution. Among individuals with chronic diseases, deficit accumulation may be accelerated, as physiologic stressors are more frequent and recovery is slower compared with healthy individuals. In many disease-specific cohorts, FI scores are normally distributed [45], reflecting a higher degree of frailty among a greater number of individuals. Mean FI scores in disease-specific cohorts are also higher than expected for similarly aged healthy individuals [44,45,46], confirming that deficit accumulation is likely accelerated in chronic disease.
Among community-dwelling older individuals, there is a nonlinear rate of deficit accumulation with increasing age. On average, FI scores increase at a rate of 3.0–3.5% per year on a logarithmic scale [41, 51]. Similar rates of deficit accumulation have been observed in mice [47•]. The relationship between chronological age and FI scores tends to be less pronounced in disease-specific cohorts [44, 45], perhaps because individuals with chronic illnesses may demonstrate significant frailty at young ages. Finally, across all studies, higher FI values are associated with increased risk of adverse health outcomes, including mortality [25, 37, 41, 44, 45, 47]. This relationship between FI scores and mortality remains consistent across the life span [37], suggesting that frailty is not only an issue of the aged, but of the aging process itself.
Using a frailty index to measure deficit accumulation in SLE
Health issues rarely occur in isolation, and this is particularly true for a complex, multisystem disease like SLE. The deficit accumulation approach incorporates the totality of an individual’s health issues into a single outcome measure, regardless of whether the deficits represent manifestations of SLE, complications of its treatment, or unrelated comorbidities. Some SLE patients will accumulate health deficits more rapidly than others, leading to disproportionately poor health outcomes.
The deficit accumulation approach was used to construct a frailty index for patients with SLE [19••]. This FI was developed based on data from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort, which is an international, multicenter, prospective observational study of 1826 SLE patients enrolled within 15 months of SLE diagnosis and followed with annual clinical and laboratory assessments [19••]. There were 222 variables identified as potential health deficits from the SLICC database. A majority of these variables were derived from existing, well-validated SLE instruments, including the SLE Disease Activity Index 2000 (SLEDAI-2K) [52], SLICC/American College of Rheumatology (ACR) Damage Index (SDI) [53], and the Medical Outcomes Survey Short Form 36 (SF-36) [54].
Of the 222 candidate variables, there were 48 items that met all required criteria for inclusion as health deficits in the SLICC-FI [19••]. The 48 health deficits included 14 items related to organ damage (e.g., congestive heart failure and chronic kidney disease), 14 items reflecting active inflammatory disease (e.g., serositis and inflammatory arthritis), 6 items representing comorbid conditions (e.g., hypertension and obesity), and 14 other variables related to functional impairment, mobility, health attitude, and psychosocial factors [19••].
The properties of the SLICC-FI were initially evaluated in a baseline dataset of 1683 SLICC inception cohort patients who were mostly female (89%) with a mean age of 35.7 years and mean SLE disease duration of 18.8 months [19••]. Using a cut-point extrapolated from studies of older adults (FI > 0.21), 27.1% of SLE patients were classified as frail at baseline [19••], which is similar to the reported prevalence of phenotypic frailty in SLE [18••]. The mean baseline SLICC-FI score was 0.17 [19••], which is substantially higher than previously reported mean FI scores for similarly aged individuals in the general population, which are typically < 0.10 [37].
The measurement properties of the FI in the SLICC inception cohort were similar to those demonstrated in non-SLE populations. For example, there was a weak, positive correlation between chronological age and baseline SLICC-FI scores, with women exhibiting higher SLICC-FI scores than men at a given age [55••]. Baseline SLICC-FI values demonstrated weak, positive associations with SLEDAI-2K, SF-36, and SDI scores from the same assessment [55••], and these associations persisted even when overlapping items were omitted from the SLICC-FI. Importantly, these measurement properties were unchanged when SLICC-FI scores were recalculated using 80% of the total deficits, randomly selected [19••]. This demonstrates that SLICC-FI scores are not driven by a small number of influential variables, but instead reflect the global impact of deficit accumulation.
Similar measurement properties were observed for SLICC-FI scores at last follow-up in the SLICC inception cohort [55••]. Interestingly, the mean SLICC-FI score remained unchanged over a mean interval of 7.2 years [55••], which is uncommon in FI studies with such prolonged follow-up. When individual changes in SLICC-FI values during follow-up were evaluated, approximately two-thirds of patients had clinically meaningful changes (± 0.03) in their SLICC-FI scores over time, with 42% experiencing significant improvement in their SLICC-FI values [55••]. We hypothesize that these results may reflect the impact of treatment, or a trade-off between deficits related to active SLE versus those due to irreversible organ damage. Regardless, these findings provide important insights into the attenuated relationship between chronological age and frailty in chronic disease populations. Furthermore, the potential for SLICC-FI scores to decrease over time reinforces the notion that frailty is a potentially treatable, reversible process in SLE, distinct from the construct of organ damage.
Importantly, the SLICC-FI demonstrated predictive validity for future adverse health outcomes among SLE patients in the SLICC inception cohort. Higher baseline SLICC-FI values predicted increased risk of mortality [55••] and organ damage accrual [56•] during follow-up, and these associations persisted after adjusting for other important prognostic factors, including baseline SLEDAI-2K and SDI scores. In sensitivity analyses, the associations of baseline SLICC-FI values with adverse outcomes remained unchanged when items related to organ damage were omitted from the SLICC-FI, and when patients without baseline organ damage were considered, suggesting that the predictive validity of the SLICC-FI was not dependent on the impact of organ damage [55, 56]. Future work will evaluate the predictive validity of the SLICC-FI for other health outcomes such as functional disability, quality-of-life, and hospitalizations.
Comparing the phenotypic and deficit accumulation approaches
As phenotypic frailty arises as a consequence of underlying sarcopenia, a major strength of this approach is its physiologic basis, which positions frailty as a distinct and biologically plausible entity, independent from other constructs such as disability and comorbidity [57]. This approach may be most useful for studying the specific impact of sarcopenia and physical frailty on health outcomes in isolation from other prognostic factors. Because the phenotypic approach does not capture important non-physical domains that can contribute to health outcomes, separate evaluations of other constructs such as comorbidity, function, cognition, and social vulnerability are required for a comprehensive assessment of overall risk [57].
In contrast to phenotypic frailty, the deficit accumulation approach lacks a physiologic basis [14]. However, the remarkably consistent properties of the FI when applied in very different contexts, including in animal models, suggest an innate biological meaning [39••]. Unlike the Fried phenotype, the FI may include health deficits that overlap considerably with other constructs such as comorbidity and functional disability. This redundancy may become problematic when incorporating the FI into clinical prediction models [57, 58]. Alternatively, the holistic nature of the FI may be advantageous for prognostication, as this approach can combine information from many different domains into a single variable that accurately predicts the risk of future adverse outcomes.
Deficit accumulation may be a less suitable approach for investigating targeted therapeutic interventions for frailty, as the underlying factors driving high FI scores may differ between individuals, necessitating different treatment approaches [57, 58]. Operationalizing frailty as a specific clinical syndrome driven by sarcopenia may better facilitate its treatment. In sarcopenic individuals, physical activity programs and nutritional supplementation have been shown to increase muscle mass and improve strength [22]. A randomized trial of community-dwelling older adults confirmed that physical activity, nutritional, cognitive, and combined interventions were all effective for reducing the prevalence of phenotypic frailty when compared with usual care [59]. Future work should aim to determine whether similar interventions are capable of preventing and treating phenotypic frailty among individuals with SLE, and whether this will translate into improved clinical outcomes.
One disadvantage of the frailty phenotype is its lack of granularity, as individuals can only be classified into one of three risk categories. While this approach presents frailty as an all-or-none phenomenon, the FI method acknowledges that frailty can exist to varying degrees across a broad spectrum, and the degree of frailty present in a given individual is critically important in both determining their risk of adverse outcomes, as well as for making treatment decisions. A possible floor effect has also been identified when applying the Fried phenotype to community-dwelling older adults, as only a small percentage of individuals will be classified as frail [60]. Because subclinical health deficits, such as laboratory abnormalities, can be included in the FI, there is less risk of a floor effect with the deficit accumulation approach and greater potential for the early detection of individuals at risk for becoming frail [39••].
The generalizability of the deficit accumulation approach is one of its major strengths. The validity of the FI has been demonstrated not only in older adults [25, 40,41,42], but also in disease-specific cohorts [44,45,46, 55], and even in animal models [47•]. The flexibility afforded by the FI with respect to the number and type of included health deficits also means that an FI can be constructed from nearly any existing health dataset without additional data collection, facilitating the study of frailty using secondary health data sources.
Conversely, while the Fried phenotype has also been applied in many different contexts, the generalizability of the phenotypic criteria remains less clear. For example, in the study examining phenotypic frailty among women with SLE, exhaustion was far more common than expected, while slow gait speed was very rare [18••]. This suggests that some aspects of the frailty phenotype, as defined in geriatric medicine, may have limited utility in SLE. There is similar ongoing debate regarding the generalizability of the Fried phenotype to other diverse populations where the phenotypic expression of sarcopenia may differ significantly from community-dwelling older adults.
A practical limitation of the FI approach is the large number of included health deficits, which may be time consuming to assess in clinical practice. Electronic health records may make implementation of the FI more feasible [61]. Meanwhile, the Fried phenotype consists of only five criteria, which can be rapidly assessed in less than 10 min [16], allowing frailty to be identified in clinical settings with relative ease. However, the original frailty phenotype does include some physical performance measures, such as grip strength and gait speed, for which specialized equipment and trained evaluators are required for accurate assessment. This could be a barrier to implementation in certain settings. These items are also less likely to be captured in pre-existing health datasets. Researchers have addressed this issue by making adjustments to the original phenotypic criteria based on data availability, with a recent systematic review identifying 262 modifications in the literature [62]. However, such modifications have been shown to lack validity [62].
Ultimately, the two approaches to the measurement of frailty have different strengths and limitations and it is unlikely that a single approach can be deemed superior in all circumstances. Several factors should be considered when selecting an instrument to measure frailty, including its intended purpose, the domains of frailty captured, its measurement properties in prior studies, and its feasibility in a particular setting [15]. Although there is ongoing debate regarding the optimal method for measuring frailty, it seems that the preferred approach may differ, depending upon the above factors.
Important areas for future research
While early research suggests that frailty may be a useful concept for better understanding the health outcomes of SLE patients, several unanswered questions remain. First, it must be acknowledged that the SLICC-FI has been developed and evaluated in a single cohort of relatively young SLE patients early in their disease course [19, 55]. External validation of the SLICC-FI is required to determine its generalizability to other SLE populations, including among older patients with longer standing SLE. Second, studies of older adults have shown that FI values greater than 0.21–0.25 are consistently associated with the presence of phenotypic frailty [63]. Future studies should aim to assess the agreement between the Fried phenotype and the SLICC-FI for identifying frailty among individuals with SLE. Third, additional studies are needed to confirm minimal clinically important differences in SLICC-FI scores.
Recent reports suggest that rapidly increasing frailty is associated with worse health outcomes when compared with arriving at the same level of frailty more slowly [64•]. Therefore, how past trajectories of FI scores influence their future predictive value is of great interest. Work is ongoing to better understand the trajectories of SLICC-FI scores over time and how these trajectories relate to adverse outcomes in SLE. Intervention studies will also be an important next step to determine how frailty can be prevented and treated among individuals with SLE and whether this will translate into improved health outcomes for SLE patients.
Conclusions
Frailty is a useful concept for understanding the unexplained variability in health outcomes observed among individuals with SLE. Both the deficit accumulation approach and the Fried frailty phenotype have been shown to be relevant in SLE. The SLICC-FI embraces the heterogeneity and complexity of SLE, by placing less emphasis on individual risk factors, and instead focusing on the cumulative impact of multiple interrelated health issues. Following additional validation studies, the SLICC-FI may be a valuable prognostic tool for identifying high-risk SLE patients who may require special interventions to prevent adverse health outcomes. Given that frailty is potentially reversible, the SLICC-FI may also be useful as an outcome measure for future intervention studies. Meanwhile, the Fried phenotype may be helpful for understanding the specific impact of sarcopenia and physical frailty in SLE, and will play an important role in the design and evaluation of interventions for the prevention and treatment of physical frailty among individuals with SLE.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365:2110–21.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62.
Fulop T, Larbi A, Witkowski JM, McElhaney J, Loeb M, Mitnitski A, et al. Aging, frailty and age-related diseases. Biogerontology. 2010;11:547–63.
Abel GA, Klepin HD. Frailty and the management of hematologic malignancies. Blood. 2018;131:515–24.
Partridge JSL, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41:142–7.
Chowdhury R, Peel NM, Krosch M, Hubbard RE. Frailty and chronic kidney disease: a systematic review. Arch Gerontol Geriatr. 2017;68:135–42.
Ness KK, Armstrong GT, Kundu M, Wilson CL, Tchkonia T, Kirkland JL. Frailty in childhood cancer survivors. Cancer. 2015;121:1540–7.
Brothers TD, Kirkland S, Guaraldi G, Falutz J, Theou O, Johnston BL, et al. Frailty in people aging with human immunodeficiency virus (HIV) infection. J Infect Dis. 2014;210:1170–9.
Yurkovich M, Vostretsova K, Chen W, Aviña-Zubieta JA. Overall and cause-specific mortality in patients with systemic lupus erythematosus: a meta-analysis of observational studies. Arthritis Care Res. 2014;66:608–16.
Bernatsky S, Ramsey-Goldman R, Labrecque J, Joseph L, Boivin J-F, Petri M, et al. Cancer risk in systemic lupus: an updated international multi-centre cohort study. J Autoimmun. 2013;42:130–5.
Manzi S, Meilahn EN, Rairie JE, Conte CG, Medsger TA, Jansen-McWilliams L, et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol. 1997;145:408–15.
Kirkwood TBL, Feder M, Finch CE, Franceschi C, Globerson A, Klingenberg CP, et al. What accounts for the wide variation in life span of genetically identical organisms reared in a constant environment? Mech Ageing Dev. 2005;126:439–43.
Vaupel JW, Manton KG, Stallard E. The impact of heterogeneity in individual frailty on the dynamics of mortality. Demography. 1979;16:439–54.
Walston JD, Bandeen-Roche K. Frailty: a tale of two concepts. BMC Med. 2015;13:185–3.
Buta BJ, Walston JD, Godino JG, Park M, Kalyani RR, Xue Q-L, et al. Frailty assessment instruments: systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev. 2016;26:53–61.
de Vries NM, Staal JB, van Ravensberg CD, Hobbelen JSM, Rikkert MGMO, Sanden der MWGN-V. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2011;10:104–14.
Theou O, Walston J, Rockwood K. Operationalizing frailty using the frailty phenotype and deficit accumulation approaches. Interdiscip Top Gerontol Geriatr. 2015;41:66–73.
•• Katz PP, Andrews J, Yazdany J, Schmajuk G, Trupin L, Yelin E. Is frailty a relevant concept in SLE? Lupus Sci Med. 2017;4:e000186 The first study to estimate the prevalence of phenotypic frailty among individuals with SLE, and to show an association between phenotypic frailty and mortality in SLE.
•• Legge A, Kirkland S, Rockwood K, Andreou P, Bae S-C, Gordon C, et al. Construction of a frailty index as a novel health measure in systemic lupus erythematosus. J Rheumatol. 2020;47:72–81 A study outlining the development of the first frailty index to quantify deficit accumulation among individuals with SLE using data from the SLICC inception cohort.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol. 2001;56A:M146–56.
Landi F, Calvani R, Cesari M, Tosato M, Martone AM, Bernabei R, et al. Sarcopenia as the biological substrate of physical frailty. Clin Geriatr Med. 2015;31:367–74.
Walrand S, Guillet C, Salles J, Cano N, Boirie Y. Physiopathological mechanism of sarcopenia. Clin Geriatr Med. 2011;27:365–85.
Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, et al. Frailty in older adults: a nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci. 2015;70:1427–34.
Zaslavsky O, Zelber-Sagi S, Gray SL, LaCroix AZ, Brunner RL, Wallace RB, et al. Comparison of frailty phenotypes for prediction of mortality, incident falls, and hip fracture in older women. J Am Geriatr Soc. 2016;64:1858–62.
• Kojima G, Iliffe S, Walters K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. 2018;47:193–200 A recent systematic review and meta-analysis demonstrating the predictive validity of the frailty index for mortality risk.
Shamliyan T, Talley KMC, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. 2013;12:719–36.
Jha SR, Ha HSK, Hickman LD, Hannu M, Davidson PM, Macdonald PS, et al. Frailty in advanced heart failure: a systematic review. Heart Fail Rev. 2015;20:553–60.
Kennedy CC, Novotny PJ, LeBrasseur NK, Wise RA, Sciurba FC, Benzo RP. Frailty and clinical outcomes in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2019;16:217–24.
Maddocks M, Kon SSC, Canavan JL, Jones SE, Nolan CM, Labey A, et al. Physical frailty and pulmonary rehabilitation in COPD: a prospective cohort study. Thorax. 2016;71:988–95.
Stockton KA, Kandiah DA, Paratz JD, Bennell KL. Fatigue, muscle strength and vitamin D status in women with systemic lupus erythematosus compared with healthy controls. Lupus. 2012;21:271–8.
Andrews JS, Trupin L, Schmajuk G, Barton J, Margaretten M, Yazdany J, et al. Muscle strength, muscle mass, and physical disability in women with systemic lupus erythematosus. Arthritis Care Res. 2015;67:120–7.
Sterling K, Gallop K, Swinburn P, Flood E, French A, Sawah Al S, et al. Patient-reported fatigue and its impact on patients with systemic lupus erythematosus. Lupus. 2014;23:124–32.
Mahieu MA, Ahn GE, Chmiel JS, Dunlop DD, Helenowski IB, Semanik P, et al. Fatigue, patient reported outcomes, and objective measurement of physical activity in systemic lupus erythematosus. Lupus. 2016;25:1190–9.
Ahn GE, Chmiel JS, Dunlop DD, Helenowski IB, Semanik PA, Song J, et al. Self-reported and objectively measured physical activity in adults with systemic lupus erythematosus. Arthritis Care Res. 2015;67:701–7.
Legge A, Blanchard C, Hanly JG. Physical activity, sedentary behaviour and their associations with cardiovascular risk in systemic lupus erythematosus. Rheumatology (Oxford). 2019.
Santos MJ, Vinagre F, Canas da Silva J, Gil V, Fonseca JE. Body composition phenotypes in systemic lupus erythematosus and rheumatoid arthritis: a comparative study of Caucasian female patients. Clin Exp Rheumatol. 2011;29:470–6.
Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. Can Med Assoc J. 2011;183:E487–94.
Mitnitski A, Rockwood K. Aging as a process of deficit accumulation: its utility and origin. Interdiscip Top Gerontol Geriatr. 2015;40:85–98.
•• Rockwood K, Howlett SE. Age-related deficit accumulation and the diseases of ageing. Mech Ageing Dev. 2019;180:107–16 A recent narrative review that provides a comprehensive overview of the deficit accumulation approach to operationalizing frailty.
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:731–10.
Mitnitski A, Song X, Skoog I, Broe GA, Cox JL, Grunfeld E, et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc. 2005;53:2184–9.
Fang X, Shi J, Song X, Mitnitski A, Tang Z, Wang C, et al. Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing longitudinal study of aging. J Nutr Health Aging. 2012;16:903–7.
Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010;58:681–7.
Rockwood MR, MacDonald E, Sutton E, Rockwood K, Baron M. Frailty index to measure health status in people with systemic sclerosis. J Rheumatol. 2014;41:698–705.
Guaraldi G, Brothers TD, Zona S, Stentarelli C, Carli F, Malagoli A, et al. A frailty index predicts survival and incident multimorbidity independent of markers of HIV disease severity. AIDS. 2015;29:1633–41.
Hubbard RE, Peel NM, Smith M, Dawson B, Lambat Z, Bak M, et al. Feasibility and construct validity of a frailty index for patients with chronic kidney disease. Australas J Ageing. 2015;34:E9–12.
• Rockwood K, Blodgett JM, Theou O, Sun MH, Feridooni HA, Mitnitski A, et al. A frailty index based on deficit accumulation quantifies mortality risk in humans and in mice. Sci Rep. 2017;7:43068 A recent observational study demonstrating remarkably consistent properties of the frailty index in both humans and mice.
Rockwood K, Mitnitski A. Limits to deficit accumulation in elderly people. Mech Ageing Dev. 2006;127:494–6.
Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol. 2017;89:30–40.
Kane AE, Keller KM, Heinze-Milne S, Grandy SA, Howlett SE. A murine frailty index based on clinical and laboratory measurements: links between frailty and pro-inflammatory cytokines differ in a sex-specific manner. J Gerontol A Biol Sci Med Sci. 2019;74:275–82.
Mitnitski A, Rockwood K. The rate of aging: the rate of deficit accumulation does not change over the adult life span. Biogerontology. 2016;17:199–204.
Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29:288–91.
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39:363–9.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
•• Legge A, Kirkland S, Rockwood K, Andreou P, Bae S-C, Gordon C, et al. Evaluating the properties of a frailty index and its association with mortality risk among patients with systemic lupus erythematosus. Arthritis Rheumatol. 2019;11:455–11 A recent observational study demonstrating the properties of a frailty index in an inception cohort of SLE patients, including the association between higher frailty index values and increased mortality risk.
Legge A, Kirkland S, Rockwood K, Andreou P, Bae S-C, Gordon C, et al. Prediction of damage accrual in systemic lupus erythematosus using the Systemic Lupus International Collaborating Clinics Frailty Index (SLICC-FI). Arthritis Rheumatol. 2019. https://doi.org/10.1002/art.41144 An observational study using data from the SLICC inception cohort demonstrating an association between higher SLICC-FI values early in disease and increased organ damage accrual during follow-up.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–63.
Afilalo J. Conceptual models of frailty: the sarcopenia phenotype. Can J Cardiol. 2016;32:1051–5.
Fairhall N. Physical, nutritional, cognitive and combination interventions reduce frailty in community-dwelling prefrail and frail older people. Evid Based Med. 2016;21:142.
Kulminski AM, Ukraintseva SV, Kulminskaya IV, Arbeev KG, Land K, Yashin AI. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56:898–903.
Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45:353–60.
Theou O, Cann L, Blodgett J, Wallace LMK, Brothers TD, Rockwood K. Modifications to the frailty phenotype criteria: systematic review of the current literature and investigation of 262 frailty phenotypes in the Survey of Health, Ageing, and Retirement in Europe. Ageing Res Rev. 2015;21:78–94.
Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol. 2007;62A:738–43.
• Stow D, Matthews FE, Hanratty B. Frailty trajectories to identify end of life: a longitudinal population-based study. BMC Med. 2018;16:171–7 An interesting population-based study demonstrating how the past trajectory of an individual’s frailty index values can predict future adverse health outcomes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alexandra Legge declares that she has no conflict of interest. John G. Hanly declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other CTD: Inflammatory Myopathies and Sjogren’s
Rights and permissions
About this article
Cite this article
Legge, A., Hanly, J.G. Using the Concept of Frailty to Understand Variability in Health Outcomes Among Individuals with Systemic Lupus Erythematosus. Curr Treat Options in Rheum 6, 268–281 (2020). https://doi.org/10.1007/s40674-020-00150-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-020-00150-1