Abstract
Purpose
Aromatase inhibitors (AIs) represent the first-line adjuvant therapy for hormone receptor-positive breast cancer (BC) women. AIs have been associated with an increased rate of fractures. The aim of our study was to investigate trabecular bone score (TBS) and bone quantitative ultrasound (QUS) measurements as bone quality surrogates in AIs users.
Methods
Sixty postmenopausal BC women starting AIs and forty-two controls (mean age 61.64 ± 8.33 years) were considered. Bone mineral density (BMD) at lumbar spine and femoral neck and TBS were measured by DXA; QUS-derived Amplitude-Dependent Speed of Sound (AD-SoS), Bone Transmission Time (BTT), and Ultrasound Bone Profile Index (UBPI) were assessed at phalangeal site; morphometric vertebral fractures (Vfx) by X-ray, serum bone-specific alkaline phosphatase (BSAP), and C-telopeptide of type 1 collagen (CTX) were also evaluated.
Results
After 18 months, changes of TBS vs baseline were significantly different between AIs group and controls [Δ TBS − 2.2% vs − 0.4%, respectively, p = 0.001]. AD-SoS, BTT and UBPI values decreased only in AIs’ group (− 3.7%, − 6.45%, −8.5%, vs baseline, respectively, pall < 0.001). 3 Vfx occurred in AIs users and were associated with the greater TBS and AD-SoS modifications. In the AIs’ group, ΔTBS was associated with ΔAD-SoS (r = 0.58, p < 0.001) and ΔUBPI (r = 0.415, p = 0.001), but not with ΔBMD. Moreover, ΔTBS was independently predicted by ΔAD-SoS, after correcting for BMD, CTX and BSAP level changes (β = 0.37, SE = 2.44, p < 0.001).
Conclusions
TBS and phalangeal QUS provide useful information related to bone quality in AI-treated BC survivors and could be considered for fracture risk evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aromatase inhibitors (AIs) represent the first-line adjuvant therapy among patients with receptor-positive breast cancer (BC) leading to longer disease-free survival in comparison with tamoxifen (TAM) [1]. Their use is not always free from adverse events; some of them may threaten quality of life and adherence to treatment [2]. Due to suppression of estrogen levels caused by inhibition of the aromatase enzyme, AI-treated BC survivors often develop bone loss, which occurs at a rate at least twofold higher than those one observed in healthy, age-matched postmenopausal women, resulting in a significantly higher fracture incidence. In comparison with TAM, AIs lead to a 47% increased fracture risk [3].
Preventing fractures in BC survivors is mandatory, and concerns about AI-induced osteoporosis have led to several guidelines and recommendations [4].
Beyond bone mineral density (BMD) that is the stronger predictor of fragility fracture, bone strength is determined also by bone microarchitecture and materials’ properties that cannot be measured by the current golden standard investigation for osteoporosis dual-energy X-ray absorptiometry (DXA). As a consequence, Quantitative Computed Tomography (QCT), high-resolution (peripheral) QCT, but also the minimally invasive microindentation technique have been investigated to improve bone strength recognition [5,6,7,8].
Trabecular bone score (TBS) represents a new texture parameter coming from pixel gray-level variations in DXA images at lumbar spine. It has been proposed to reflect bone microarchitecture status and cumulating evidences suggest that it may contribute to fracture risk assessment [9,10,11].
Quantitative ultrasound (QUS) have been recently used in AI-treated BC women to detect bone health [12, 13], and the previous several studies showed correlations with DXA, prevalent vertebral fractures (Vfx), and risk of future fractures [14,15,16,17,18,19]. In particular, our group reported data on BMD, QUS, bone turnover markers, and morphometric Vfx after 18 months of AIs’ treatment [12]. Phalangeal QUS was proven to be able in identifying bone loss in BC postmenopausal women under AIs [12].
Such as TBS, QUS may detect information related to bone strength. QUS measurements are associated with physical properties of bone tissue (e.g., structure and elasticity affect ultrasound transmission) that contribute to bone strength and that are not recognized by DXA [20].
To date, there is no evidence of the association between TBS and QUS at phalangeal site in AI-treated BC women. Aim of this study was to explore bone health by phalangeal QUS and DXA including both BMD and TBS evaluations in BC survivors receiving AIs.
Materials and methods
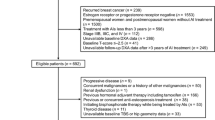
Early BC postmenopausal white women taking adjuvant endocrine therapy with AIs (i.e., anastrozole, letrozole, and exemestane) were considered. Inclusion and exclusion criteria were described in a previous research on the same population [12]. Briefly, women were recruited if they had completed surgical treatment, concluded chemotherapy and/or radiation therapy when prescribed, at least 3 months before the start of the study. Exclusion criteria were represented by: metastatic BC, other malignancies, chronic renal or liver failure, secondary causes of osteoporosis including hyperthyroidism, hyperparathyroidism, hypercortisolism, malabsorption, and diabetes mellitus, previous or current use of active bone agents (e.g., bisphosphonates, selective estrogen receptor modulators, strontium ranelate, teriparatide or PTH, calcitonin, and denosumab), but also drugs potentially involving bone metabolism in the previous 6 months (including corticosteroids, heparin, and anticonvulsant). Women with the previous fragility fractures were excluded. A control group of healthy age-matched postmenopausal women was also considered.
FRAX® algorithm (http://www.shef.ac.uk/FRAX) was used at baseline to estimate the 10-year probability of a major fracture (hip, clinical spine, humerus, or wrist fracture) and hip fracture too. FRAX score was calculated without considering BMD. Vitamin D (cholecalciferol 25,000 UI bimonthly) and calcium (calcium carbonate 500–1000 mg daily, when necessary to reach the recommended daily calcium intake) were administered over the 18-month observation period.
In our previous study, we investigated BMD, QUS, and bone turnover markers at baseline and after 18 months [12]. BMD was assessed by DXA densitometer (Hologic Discovery) at the lumbar spine (L1–L4) and femoral site, at baseline and after 18 months. DXA densitometer was calibrated daily according to the manufacturer’s instruction and its coefficient of variation (CV) was 0.5% at lumbar spine and femoral site. Phalangeal quantitative ultrasound (QUS) of bone was performed at the proximal phalangeal metaphysis of the last four fingers of the non-dominant hand using a DBM Sonic Bone Profiler (Igea, Carpi, Italy) as previously described [12, 21, 22], and several variables were considered (i.e., Amplitude-Dependent Speed of Sound (AD-SoS), Bone Transmission Time (BTT), Fast Wave Amplitude (FWA), Signal Dynamic (SDy), and Ultrasound Bone Profile Index (UBPI) automatically calculated [UBPI = − (0.0018 × SDy − 0.0560 × FWA 0.0560 − 1.1467 × BTT + 3.0300)]. To check for morphometric Vfx, a lateral X-ray scan of dorsal and lumbar spine was performed at baseline and at the end of the study, and a fracture was diagnosed if a vertebra body had at least a 20% height reduction in the anterior, middle, or posterior height compared with the same or adjacent vertebra according to the semiquantitative method proposed by Genant [23].
At baseline, and at after 18 months, C-telopeptide of type 1 collagen (CTX) (Roche, Basel, Switzerland) and Bone-Specific Alkaline Phosphatase (BSAP) (Beckman Coulter, Fullerton, California) were measured by enzyme-linked immunosorbent assay. High-performance liquid chromatography was used to explore 25-hydroxyvitamin D [25(OH)D] levels.
In addition to these preliminary variables, we further investigated TBS through DXA images. The TBS was obtained by iNsight software (version 3.0; Medimaps group, Geneva, Switzerland). TBS was evaluated considering the variogram of the trabecular bone projected image, calculated as the sum of the squared gray-level differences between pixels at a specific distance and angle. TBS was then calculated as the slope of the log–log transform of this variogram. TBS was reported as the mean value of the individual measurements for lumbar spine TBS. For longitudinal TBS comparison, if any vertebra was excluded at baseline, all subsequent TBS calculations were adjusted to ensure that identical vertebral bodies were analyzed [9, 24].
Statistical analysis was performed using MedCalc software (version 10.2.0.0; Mariakerke, 173 Belgium). The normal distribution of values was verified with the Kolmogorov–Smirnov test. Student’s t test for paired and unpaired observations or Wilcoxon test and Mann–Whitney test were used as appropriate. The degree of association between two variables was verified by Spearman’s coefficient. A multiple regression analysis was performed to analyze the relationship between a dependent variable and one or more explanatory variables. Values of p < 0.05 were considered to indicate statistical significance. All reported p values were two-sided.
The study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments, and written informed consent was obtained from all the participants.
Results
The baseline main clinical characteristics of all the participants are shown in Table 1. The percentages of patients with different grade of TBS deterioration (grade 1: TBS > 1.350, grade 2: 1.350-1200, grade 3: < 1.200) in AIs and control group are shown in Fig. 1. Comparing the BC women with controls, no significant differences were noticed as for the studied variables.
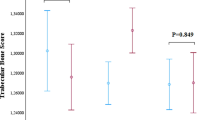
FRAX-derived 10-year probability of major fractures and hip fractures was significantly associated with TBS values (r = − 0.392, p < 0.001; r = − 0.363, p < 0.001; respectively) and with all the QUS measurements (p < 0.001 for all), but not with BMD values. TBS measurement were also negatively associated with age (r = − 0.39, p < 0.001) and positively related with T-score values at lumbar spine and femoral neck (r = 0.21, p = 0.04; r = 0.20, p = 0.04; respectively). After 18 months, variation of TBS was significantly different between AI-treated BC women and controls. In AI-treated BC women, TBS significantly changed from 1.310 (1.258–1351) to 1.298 (1.244–1.328) (p < 0.0001), while, in controls, TBS variation was not significant [1.315 (1.290–1354) to 1.312 (1.288–1.348) (p = 0.18)]. Change of TBS was, thus, significantly different between groups [Δ TBS (%) − 2.2 ± 3 vs − 0.4 ± 0.5, respectively, p = 0.0011 (Fig. 2)]. QUS values at phalangeal site changed over time too. After 18 months, AD-SoS, UBPI, and BTT values were significantly decreased in BC women receiving AIs (− 3.7%, − 6.45%, − 8.5%, respectively, p < 0.001 for all), but not in controls (− 0.7%, − 3.53%, − 2.97%, respectively) and, with the exception of UBPI, between-groups QUS differences were all statistically significant at the end of the study. In AIs’ users, a significant positive association was observed between change of TBS and change of AD-SoS values (r = 0.58; p < 0.0001) (Fig. 3), but also between change of TBS and change of UBPI (r = 0.41, p = 0.001),
Modification of BMD at lumbar spine was significantly different between AIs treated BC women and controls (− 2.94% vs − 0.69%, respectively, p = 0.001) and the same was observed for BMD at femoral neck (− 2.5% vs − 0.39%, p = 0.01). 25-OHD increased in both groups, and CTX and BSAP increased only in AI-treated women as previously reported [12]. At the end of the study, three incident morphometric mild Vfx occurred in three AIs’ users in comparison to one incident morphometric mild vertebral fracture in one woman from controls. After grouping AI-treated women in tertiles according to TBS variation [Δ TBS (%) − 5.8 ± 2, − 1.4 ± 0.8, 0.6 ± 0.6, respectively] and AD-SoS variation [Δ AD-SoS (%) − 6.8 ± 1.8, − 2.9 ± 1.3, 1 ± 1.8, respectively], a post hoc analysis indicated that incident Vfx occurred in the tertile of greater negative variation of TBS and AD-SoS.
In the AIs’ group, TBS variation over time was not significantly associated with BMD changes at lumbar spine and femoral neck (r = 0.16, p = 0.27 and r = 0.14, p = 0.36; respectively), but was significantly associated with AD-SoS (r = 0.58, p < 0.001) and UBPI (r = 0.415, p = 0.001) variations.
At a multiple regression analysis, change of TBS was independently predicted by change of AD-SoS, after correcting for BMD variation at lumbar spine and femoral neck and for modification of CTX and BSAP levels (β = 0.37, SE = 2.44, p < 0.001).
Discussion
AIs are the recommended standard of care for hormone receptor-positive BC postmenopausal women and the duration of adjuvant endocrine therapy is increasing beyond 5 years [1, 25].
Because of the predictable increased fracture risk, bone loss evaluation represents a challenge in the management of BC survivors assuming AIs [3, 4].
To our knowledge, this is the first time that DXA assessment including the TBS calculation was associated with QUS measurements of bone in postmenopausal women with early stage, hormone receptor-positive BC assuming AIs.
In accordance with the published data and in comparison with controls, we found increased bone loss in AIs’ users consistent with the more pronounced decrease of all DXA and QUS measurements and with a higher incidence of morphometric Vfx [2, 3].
We evaluated TBS as a surrogate assessment of bone quality. TBS is a novel gray-level texture measurement based on standard DXA images, which correlates with three-dimensional parameters of bone texture and that provides further information on bone strength additional to the standard BMD. Differently from BMD, it may be less affected by spinal degenerative changes [26].
In the largest published study assessing TBS and considering 29,407 postmenopausal women in the Canadian province of Manitoba, there were 1668 incident major osteoporotic fractures, including 439 vertebral fractures and 293 hip fractures over the 5 years of follow-up. BMD at lumbar spine and TBS predicted fractures equally well, and the combination of both performed better than either individually [27, 28]. Moreover, TBS appeared to enhance fracture risk prediction in those women with BMD in the normal or osteopenic range, but not in those women in the osteoporotic BMD range [29].
At baseline, a strong positive association between lumbar BMD and TBS was detected, suggesting that women with preserved BMD were more likely to have well-maintained bone microarchitecture and vice versa. However, when investigating for correlations between TBS and BMD changes over the 18 months of AIs’ treatment, we found no significant associations. On the contrary, in the B-ABLE prospective cohort study, after 5 years of AIs, changes in spine BMD and TBS were weakly correlated [30]. It could be speculated that AIs’ treatment may differentially affect BMD and TBS within individual patients, thus, providing further evidence to the dramatic impact of AIs on bone health [31].
Bone QUS measurements reflect properties of bone not detected by DXA, and phalangeal QUS could represent a simple screening tool to improve fracture risk prediction [15]. QUS measurements were proven to distinguish between fractured and non-fractured patients and to be useful in different clinical settings, also in secondary osteoporosis [12, 13, 15, 21, 22]. In BC survivors treated with AIs, we previously explored bone health by phalangeal QUS and observed a significant bone loss over 18 months [12]. In the present study, we added data on TBS and reported significant changes of TBS values due to AIs’ treatment.
Interestingly, change of AD-SoS was associated with TBS variation over the observation period. This is a novel finding that supports the concept that phalangeal QUS and TBS measurements may be influenced by AIs’ treatment irrespectively from BMD variation.
In the study of Hans et al., strong significant correlations were obtained between TBS and three-dimensional parameters of bone microarchitecture such as connectivity density (connD), trabecular number (TbN), and trabecular spacing (TbSp) derived from micro-computed tomography acquisitions of human cadaver vertebrae. The highest degree of correlation was detected between TBS and connD, and TBS explained 67.2% of the variance in three-dimensional connectivity; therefore, low TBS was indicative of weak microarchitecture, associated with low connD, high TbSp, and a reduced TbN, whereas a high TBS reflected a stronger microarchitecture [10]. Furthermore, TBS was associated with trabecular microarchitecture and cortical width measured by bone biopsy in patients with chronic kidney disease [32].
Ultrasound is a mechanical wave and the QUS tools involve ultrasound impulses that are transmitted through the bone. Thus, the ultrasound wave may be differently transmitted according to the bone material properties and microarchitecture resulting in weak transmission when quality of bone is poor.
The phalangeal bone at the metaphyseal level which we considered for QUS investigation is a long bone consisting of both the trabecular and the cortical components, which are main determinants of the mechanical resistance [20].
It was previously reported that AD-SoS is mainly affected by cortical area, cortical bone density, and cortical porosity [33]. Consequently, because of AIs’ treatment impair both TBS and AD-SoS, we argue that BC survivors’ fracture risk could be increased due to quality derangement of trabecular and cortical components of bone, also beyond BMD variation. This is consistent with the reported increased rate of fractures in AI-treated BC survivors at sites where trabecular bone (e.g., vertebrae) or cortical bone (e.g., femur) is prevalent [2,3,4].
The positive association between TBS and AD-SoS was also indicative of concomitant disruption of trabecular and cortical bone, respectively, possibly explaining weaken bone in BC survivors assuming AIs.
Remarkably, the three morphometric Vfx in AIs group occurred all in those women with greater reduction of TBS. Change of AD-SoS values was also predictive of TBS modification; thus, QUS could serve to keep information on bone health (i.e., bone quality) regardless of BMD and bone turnover markers. Finally, in AIs’ users, we observed unbalanced bone turnover as suggested from modification of CTX and BSAP, indicative of bone loss. As well, vitamin D status improved in all the study participants due to cholecalciferol supplementation which could have preserved at least in part bone health and quality of life [34,35,36].
We acknowledge that this study has some limitations as the small sample size and the observation period not long enough to cover all the planned 5–10 year AIs’ treatment period. At the same time, this is the first observation of a significant positive association between QUS measurements at phalangeal site and DXA-derived TBS in BC survivors taking AIs.
In conclusion, in hormone receptor-positive BC postmenopausal women, AIs could cause bone loss and enhance fracture risk. Beyond BMD, TBS at lumbar spine and phalangeal QUS measurements provide information about bone strength and could help physicians to identify women at higher fracture risk. Because QUS is a simple, inexpensive radiation-free tool, it might be considered in the follow-up of bone status in AI-treated BC women.
References
Rugo HS, Rumble RB, Macrae E et al (2016) Endocrine therapy for hormone receptor-positive metastatic breast cancer: American Society of Clinical Oncology Guideline. J Clin Oncol 34(25):3069–3103
Amir E, Seruga B, Niraula S, Carlsson L, Ocaña A (2011) Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst 103(17):1299–1309
Hadji P (2009) Aromatase inhibitor-associated bone loss in breast cancer patients is distinct from postmenopausal osteoporosis. Crit Rev Oncol Hematol 69:73–82
Hadji P, Aapro MS, Body JJ et al (2017) Management of Aromatase Inhibitor-Associated Bone Loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: joint position statement of the IOF, CABS, ECTS, IEG, ESCEO IMS, and SIOG. J Bone Oncol 23(7):1–12
Sakata S, Barkmann R, Lochmüller EM, Heller M, Glüer CC (2004) Assessing bone status beyond BMD: evaluation of bone geometry and porosity by quantitative ultrasound of human finger phalanges. J Bone Miner Res 19(6):924–930
Krause M, Museyko O, Breer S et al (2014) Accuracy of trabecular structure by HR-pQCT compared to gold standard μCT in the radius and tibia of patients with osteoporosis and long-term bisphosphonate therapy. Osteoporos Int 25(5):1595–1606
Shepherd JA, Schousboe JT, Broy SB, Engelke K, Leslie WD (2015) Executive summary of the 2015 ISCD position development conference on advanced measures from DXA and QCT: fracture prediction beyond BMD. J Clin Densitom 18(3):274–286
Malgo F, Hamdy NAT, Papapoulos SE, Appelman-Dijkstra NM (2017) Bone material strength index as measured by impact microindentation is low in patients with fractures irrespective of fracture site. Osteoporos Int 28(8):2433–2437
Harvey NC, Glüer CC, Binkley N et al (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone 78:216–224
Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14(3):302–312
Hans D, Šteňová E, Lamy O (2017) The Trabecular Bone Score (TBS) Complements DXA and the FRAX as a Fracture Risk Assessment Tool in Routine Clinical Practice. Curr Osteoporos Rep 15(6):521–531
Catalano A, Morabito N, Agostino RM et al (2017) Bone health assessment by quantitative ultrasound and dual-energy x-ray absorptiometry in postmenopausal women with breast cancer receiving aromatase inhibitors. Menopause 24(1):85–91
Catalano A, Gaudio A, Morabito N et al (2017) Quantitative ultrasound and DXA measurements in aromatase inhibitor-treated breast cancer women receiving denosumab. J Endocrinol Invest 40(8):851–857
Atteritano M, Lasco A, Mazzaferro S et al (2013) Bone mineral density, quantitative ultrasound parameters and bone metabolism in postmenopausal women with depression. Intern Emerg Med 8(6):485–491
Catalano A, Morabito N, Basile G et al (2013) Fracture risk assessment in postmenopausal women referred to an Italian center for osteoporosis: a single day experience in Messina. Clin Cases Miner Bone Metab 10(3):191–194
Guglielmi G, Njeh CF, de Terlizzi F (2003) Phalangeal quantitative ultrasound, phalangeal morphometricvariables, and vertebral fracture discrimination. Calcif Tissue Int 72(4):469–477
Guglielmi G, Rossini M, Nicolosi MG, Ragno A, Lentini G, de Terlizzi F (2013) Three-year prospective study on fracture risk in postmenopausal women by quantitative ultrasound at the phalanges. J Clin Densitom 16(3):341–346
Kanis JA, Johnell O, Oden A, De Laet C, De Terlizzi F (2005) Ten-year probabilities of clinical vertebral fractures according to phalangeal quantitative ultrasonography. Osteoporos Int 16(9):1065–1670
Glüer CC, Eastell R, Reid DM et al (2004) Association of five quantitative ultrasound devices and bone densitometry with osteoporotic vertebral fractures in a population-based sample: the OPUS Study. J Bone Miner Res 19(5):782–793
Guglielmi G, de Terlizzi F (2009) Quantitative ultrasound in the assessment of osteoporosis. Eur J Radiol 71(3):425–431
Catalano A, Morabito N, Di Vieste G, Pintaudi B, Cucinotta D, Lasco A, Di Benedetto A (2013) Phalangeal quantitative ultrasound and metabolic control in pre-menopausal women with type 1 diabetes mellitus. J Endocrinol Invest 36(5):347–351
Catalano A, Bellone F, Cicala G, Giandalia A, Morabito N, Cucinotta D, Russo GT (2017) Multiple fractures and impaired bone metabolism in Wolfram syndrome: a case report. Clin Cases Miner Bone Metab 14(2):254–257
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148
Muschitz C, Kocijan R, Haschka J et al (2015) TBS reflects trabecular microarchitecture in premenopausal women and men with idiopathic osteoporosis and low-traumatic fractures. Bone 79:259–266
van Hellemond IEG, Geurts SME, Tjan-Heijnen VCG (2018) Current Status of Extended Adjuvant Endocrine Therapy in Early Stage Breast Cancer. Curr Treat Options Oncol 19(5):26
Anderson KB, Holloway-Kew KL, Mohebbi M, Kotowicz MA, Hans D, Pasco JA (2018) Is trabecular bone score less affected by degenerative-changes at the spine thanlumbar spine BMD? Arch Osteoporos 13(1):127. https://doi.org/10.1007/s11657-018-0544-3
Leslie WD, Anderson WA, Metge CJ, Manness LJ (2007) Maximizing Osteoporosis Management in Manitoba Steering Committee. Clinical risk factors for fracture in postmenopausal Canadian women: a population-based prevalence study. Bone 40(4):991–996
Liu J, Curtis EM, Cooper C, Harvey NC (2019) State of the art in osteoporosis risk assessment and treatment. J Endocrinol Invest. https://doi.org/10.1007/s40618-019-01041-6
Boutroy S, Hans D, Sornay-Rendu E, Vilayphiou N, Winzenrieth R, Chapurlat R (2013) Trabecular bone score improves fracture risk prediction in non-osteoporotic women: the OFELY study. Osteoporos Int 24(1):77–85
María RS, Marta PM, Sonia S et al (2016) TBS and BMD at the end of AI-therapy: a prospective study of the B-ABLE cohort. Bone 92:1-8
Mariotti V, Page DB, Davydov O et al (2016) Assessing fracture risk in early stage breast cancer patients treated with aromatase-inhibitors: An enhanced screening approach incorporating trabecular bone score. J Bone Oncol 7:32–37
Ramalho J, Marques IDB, Hans D et al (2018) The trabecular bone score: relationships with trabecular and cortical microarchitecture measured by HR-pQCT and histomorphometry in patients with chronic kidney disease. Bone 116:215–220
Sakata S, Barkmann R, Lochmüller EM, Heller M, Glüer CC (2004) Assessing bone status beyond BMD: evaluation of bone geometry and porosity by quantitative ultrasound of human finger phalanges. J Bone Miner Res 19(6):924–930
Catalano A, Martino G, Morabito N, Scarcella C, Gaudio A, Basile G, Lasco A (2017) Pain in Osteoporosis: From Pathophysiology to Therapeutic Approach. Drugs Aging 34(10):755–765
Catalano A, Morabito N, Atteritano M, Basile G, Cucinotta D, Lasco A (2012) Vitamin D reduces musculoskeletal pain after infusion of zoledronic acid for postmenopausal osteoporosis. Calcif Tissue Int 90(4):279–285
Martino G, Catalano A, Bellone F et al (2018) Quality of life in postmenopausal women: which role for vitamin D? Mediterr J Clin Psychol 6(2):85. https://doi.org/10.6092/2282-1619/2018.6.1875
Funding
This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Antonino Catalano, Agostino Gaudio, Rita Maria Agostino, Nunziata Morabito, Federica Bellone, and Antonino Lasco declare that they have no conflicts of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Catalano, A., Gaudio, A., Agostino, R.M. et al. Trabecular bone score and quantitative ultrasound measurements in the assessment of bone health in breast cancer survivors assuming aromatase inhibitors. J Endocrinol Invest 42, 1337–1343 (2019). https://doi.org/10.1007/s40618-019-01063-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-019-01063-0