Abstract
Background
While survival in overall pediatric malignancy has improved during recent decades, brain/central nervous system (CNS) tumors has not demonstrated comparable survival advantage. Incidence and mortality data in this malignancy continue to illustrate race and sex differences; however, there are few data in the pediatric setting. This study sought to characterize brain/CNS tumors by socio-demographic and assess racial and sex variances in both cumulative incidence and mortality.
Methods
A retrospective cohort design with Surveillance, Epidemiology and End Results (SEER) 1973–2014 was used for the assessment of children aged < 1–19 years diagnosed with brain/CNS tumors. The age-adjusted incidence rates were used for temporal trends, percent change, and annual percent change. We utilized binomial regression model to determine the exposure effect of race and sex on cancer mortality, adjusting for potential confounders.
Results
Childhood brain/CNS tumor cumulative incidence (CmI) continues to rise in annual percent change, and mortality varied by race, sex, and year of diagnosis. The CmI was highest among whites, intermediate among blacks, and lowest among Asians, as well as lower in females relative to that in males. Compared to whites, blacks were 21% more likely to die from brain/CNS tumors [risk ratio (RR) 1.21, 95% confidence interval (C.I.) 1.13–1.28], while males were 4% more likely to die relative to females (RR 1.04, 95% C.I. 1.00–1.08). After controlling for age, sex, and tumor grade, racial disparities persisted, with 16% increased risk of dying among blacks relative to whites [adjusted risk ratio 1.16, (99% C.I.) 1.08–1.25, p < 0.001].
Conclusion
The cumulative incidence of brain/CNS malignancy is higher among whites relative to that in blacks; however, blacks experienced survival disadvantage even after adjustment for potential tumor prognostic and predisposing factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system (CNS) tumors remain one of the most common types of pediatric cancers. Of this, low-grade gliomas as well as medulloblastoma are the most common. In children aged 15 years and younger, CNS cancers are the second highest in terms of incidence rate and are responsible for the highest percent of total cancer deaths [1]. Brain/CNS tumors occur most often in children 1–14 years of age, with the highest incidence among children < 4 years of age and highest mortality in children 5 to 9 years of age [2]. Between 2005 and 2009, there were a total of 311,202 new cases of CNS tumors reported by the United States Central Brain Tumor Registry [3]. In addition to brain tumors, spinal cord tumors constitute an estimated 1–2% of all CNS tumors in the USA [4].
A recent study by Mathew et al. [5] examined the survival rate of children with medulloblastoma and primitive neuroectodermal tumor (PNET) and high-grade gliomas. The survival rate was measured at 1, 5, and 10 years after the diagnosis of CNS tumors. In children, less than 3 years of age, the 10-year survival rate after diagnosis was 51.4%; and 10 years after diagnosis, children aged 3–14 years had a survival rate of 69%. These findings are indicative of survival advantage with advancing age.
Several epidemiologic data on brain/CNS tumors have included research mostly on adult population. Previous studies in this area indicate that there is a high rate of CNS tumors in the white male population [6,7,8]. A few other studies in adult settings in the past have focused on social adjustments after cancer diagnosis and treatment, health-related quality of life, and other socio-environmental factors affecting brain/CNS malignancy [9,10,11]. The primary central nervous system lymphoma (PCNSL) which is a rare subtype of extranodal non-Hodgkin lymphoma accounts for an estimated 4% of newly diagnosed CNS tumors. Data on sex and racial variability in incidence of PCNSL based on the SEER registry, 1980–2008, indicated higher incidence among whites and males, as well as survival disadvantage with advancing age and HIV infection [12]. However, this study and previous studies did not focus on pediatric age groups’ incidence characterization and survival, necessitating the current pediatric population-based investigation. Overall, additional studies on pediatric brain/CNS cancers are needed to characterize the social, neighborhood, and environmental factors that may affect incidence and mortality in childhood cancers.
Most available studies in brain/CNS tumors with children present with small sample sizes that tend to limit a clear assessment of clinically meaningful difference in terms of effect size as well as inference from the sample. To our knowledge, there are no cumulative incidence and mortality data on four-decade temporal trends or mortality, and neither are there are any recent findings on social determinants of pediatric brain/CNS cancer in a large sample as observed in Surveillance Epidemiology End Results (SEER) dataset. This study sought to characterize brain/CNS tumors by socio-demographics. Additionally, we aimed to assess racial and sex variances in both cumulative incidence and mortality.
Materials and Methods
Study Design
A population-based retrospective cohort design was used to examine the aims of the study that form the basis of the hypotheses tested herein. This design is feasible given the preexisting data in SEER registry (1973–2014).
Data Source
Data from National Cancer Institute’s (NCI) Surveillance, Epidemiology and End Results (SEER) program was used in this study [13]. The SEER program is a cancer registry operated and managed by the NCI–National Institute of Health. The registry began in 1973 with nine SEER areas termed registries. In 1992, the registry expanded to include four additional registries; and in 2005, the registry was further expanded and included five additional registries rendering the current registry in SEER at 18. In the evolution of the database, the commonly identified registries include 9, 11, 13, 17, and 18. The information collected and stored in the SEER registry include cancer diagnosis, patient demographics, primary tumor site, tumor morphology and stage at diagnosis, prognostic factors, first course of treatment, and follow-up for vital status as well as some social determinants of health. This registry remains the most comprehensive source of population-based data which includes cancer stage at the time of diagnosis as well as patient survival. The approval of the registries into the SEER program is based on the ability of cancer centers to provide high-quality population-based information and other variables.
In the SEER registry, cancers are coded according to the International Classification of Disease 3rd edition (ICD-O-3) [14]. The SEER registries update their databases continuously, and they use the SEER Stat software to adjust for the delay in response rates. In this study, we presented incidence and mortality statistics for four racial and ethnic groups (White, Black, American Indian/Alaskan Native, and Asian/Pacific Islander). SEER cases are reported to NCI in the month of November each year and there is a completion rate of approximately 98% for all sites of cancer except for tumors such as melanoma, which are less complete.
Variable Ascertainment
The study cohort included cancer patients from SEER 18 registry and the age-adjusted incidence rates were obtained using data from SEER 9 to SEER 18. We categorized the cancer cases into five age groups: < 1 year, 1–4 years, 5–9 years, 10–14 years, and 15–19 years. The socio-demographic characteristics included in the study (age, race, sex, and insurance status) were self-reported and measured on a nominal scale. Insurance variable was classified as insured, any Medicaid, insured/no specifics, and uninsured. The outcome variable namely mortality is available in SEER as vital status and is coded as dead (1) and alive (0). This binary variable allowed for the use of binomial regression model in assessing the exposure effect of race and sex on the mortality outcome in brain/CNS tumors in children.
Race and Sex
Race and sex which are the main health disparity indicators in this study are available in SEER as nominal variables. The race data in SEER includes whites, blacks, and “other race” representing American Indian/Alaska Native (AI/AN), Asian/Pacific Islander (A/PI), and unknown race, while the sex variable includes male and female as a nominal scale; white was coded as 1, black as 2, and “other” as 3 (AI/AN, A/PI, and unknown) and sex was coded male as 1 and female as 2.
Sample Size and Power Estimations
The current study data involved preexisting cases of children with brain/CNS malignancy (n = 16,484). Implying the ability of our study to detect a clinically meaningful difference between the cumulative incidence or mortality, we estimated the power using the following parameters: (a) sample size (n = 16,484) by racial subgroups (whites, 13,379; blacks, 1882; other race, 1223); (b) effect size = 0.21—binomial regression risk ratio (21%); and (c) type I error tolerance and 95% C.I. (0.05) for the univariable model as well as 99% C.I. (0.01) for the multivariable model. With these parameters, we estimated the power to be 99% (type II error tolerance < 1%) which is a sufficient power to detect a minimum difference of 10% comparing the mortality experience of blacks relative to that of whites.
Statistical Analysis
Cumulative Incidence Rates and Trends Analysis
A weighted least squares (WLS) method was used to estimate the age-adjusted brain/CNS cancer trends in the age group of children from < 1 to 19 years (SEER Stat software) [15]. This method indicates the behavior of the random errors in the model and is applicable to regression functions that are either linear or non-linear in the parameter estimates of the sample statistic. Its application in model fitting incorporates extra non-negative constants, or weights, associated with each data point, into the fitting criterion. The size of the weight illustrates the precision of the information contained in the associated observation, implying the parameter value and parameter precision. Therefore, optimizing the weighted fitting criterion to identify or examine the parameter estimates allows the weights to determine the contribution of each observation to the final parameter estimates.
We expressed the incidence and mortality rates as the number of new primary cancer and deaths per 100,000 persons at risk. This study used the most recent SEER registry data available from 1973 to 2014. The percent change and annual percent change were also calculated using the SEER Stat Software. Percent changes were calculated using 1 year for each end point and annual percent changes were calculated using weighted least squares methods.
Proportionate Morbidity and Mortality Analyses
We also used “Proportionate Morbidity” to determine the proportion of a specific malignancy in relation to the overall malignancy diagnosed during the period of this study. Mathematically proportionate morbidity is given by:
This measure is represented as a percentage (%) or multiplier. For example. in our study, there was a total of 16,682 number of children with brain tumors implying the frequency of those with brain/CNS tumors divided by the total no. of cancer diagnosis in the entire study period. It is also expressed as the number of brain/CNS tumors per 1000 implying 1000 as a multiplier of the proportion.
Proportionate Morbidity for Brain/CNS Tumors
Similarly, we estimated Proportionate Mortality as the total number of children who died of brain/CNS tumors divided by the total number of children who died of pediatric malignancies during the study period.
Proportionate Mortality for Brain/CNS Tumors
Mortality Risk Marker: Hypothesis-Specific Analysis
The data were examined for missing variables and outliers using the tabulation method and visualization. The nominal and categorical variables such as sex and race respectively were summarized using descriptive statistics for frequencies and percentages.
Prior to hypothesis-specific analysis, we applied signal amplification and risk stratification modeling technique, which is a method used in assessing for potential confounders prior to model specification and multivariable modeling. A univariable binomial regression model was used to assess the single social determinants of health as a function of mortality. To determine the non-confounded exposure effect of race in childhood brain/CNS mortality, the Mantel-Haenszel stratification analysis was used in assessing for confounders. Where the magnitude of confounders, implying the comparison of the crude to the adjusted odds ratio, was > 10%, the potential confounding variable was confirmed as a confounder and introduced into the multivariable binomial regression model for simultaneous adjustment.
Mathematically, magnitude of confounding (MOC) = ORCrude – ORAdjusted/ORAdjusted.
All tests were two-tailed, and the type I error tolerance was set as 95% confidence interval (α = 0.05) for the univariable model and 99% C.I. (α = 0.01) for the multivariable model. STATA statistical software, version 14.0 (StataCorp, College Station, TX), was used to perform the mortality-related analysis.
Results
Study Characteristics
Race and Sex Distribution
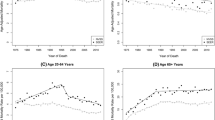
There were more whites, n = 13,379 (80.2%), diagnosed with CNS and brain tumors relative to blacks, n = 1882 (11.3%), during this period. American Indian/Alaska Native and Asian/Pacific Islander constituted 0.8% (n = 138) and 6.5% (n = 1085) respectively of the total sample (n = 16,682). Information on race was not available for 198 (1.2%) of the sample and was recorded as unknown and classifies as other race. Similarly, males had higher prevalence of tumors compared to females (54.3 vs. 45.6%). While the overall percent change (PC) was 50.6%, annual percent change (APC) was 0.8; however, there was a difference in PC and APC, comparing male to female. The PC for female was 70% and male 35%, while the APC for male was 0.7 and female 0.9. Additionally, the PC did differ comparing black (42.3%) to white (57%) as well as APC which was lower for blacks (0.3) relative to that for whites (0.9).
Temporal Trends by Age at Diagnosis and Race
The temporal trends by age at tumor’s diagnosis, stratified by race, are illustrated in Fig. 1a to e. Despite the observed fluctuations, the trends in all age groups are indicative of overall higher cumulative incidence of the tumors among whites (Fig. 1a–e).
a Age-adjusted temporal trends of incidence in pediatric brain/CNS. Malignancy by race (age < 1 year). b Age-adjusted temporal trends of incidence in pediatric brain/CNS. Malignancy by race (age 1–4 years). c Age-adjusted temporal trends of incidence in pediatric brain/CNS. Malignancy by race (age 5–9 years). d Age-adjusted temporal trends of incidence in pediatric brain/CNS. Malignancy by race (age 10–14 years). e Age-adjusted temporal trends of incidence in pediatric brain/CNS. Malignancy by race (age 15–19 years)
Proportionate Morbidity and Mortality
The proportionate morbidity was 0.18 per 1000, while proportionate mortality was 0.24 per 1000, implying that 18% of all pediatric tumors diagnosed were associated with brain/CNS tumor while 24% of all mortality from cancer were associated with brain/CNS malignancy.
Tumor Grade and Histology
While unknown (ungraded) was n = 11,309 (68.6%), there were 1101 children with grade I malignancy (6.7%); grade II, n = 1536 (9.3%); grade III, n = 491 (3.0%); grade IV, n = 2047 (12.4%).
The most diagnosed brain/CNS tumor in this sample was astrocytoma, n = 5539 (41.4%), followed by gliomas, n = 3405 (25.4%); medulloblastoma consisted of n = 2637 (19.7%) and ependymomas n = 1115 (8.3%).
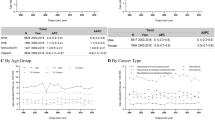
Study Characteristics by Race
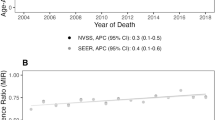
Table 1 illustrates the distribution of age group at diagnosis, sex, mortality, histology, insurance, SEER registry, tumor grade, and 5-year interval and year of diagnosis by race. The mortality prevalence was higher among blacks (40%) compared to that among whites (33%) (Fig. 2a). Likewise, relative to whites, mortality was higher among American Indian and Alaska Native (37.7%) as well as Asian/Pacific Islander (37.0%), χ2 (4) = 85.1, p < 0.0001. The overall brain/CNS tumor mortality prevalence was 33.9% (n = 5650), implying a survival proportion of 67.1% (n = 11,032) between 1973 and 2014 in the specified SEER registry.
a Cumulative mortality risk by race in childhood brain/CNS tumor, SEER (1973–2014). The error bars represent the parameter values and precision on the mortality experience by race from childhood brain/CNS tumors in the Surveillance Epidemiology and End Results (SEER) data, 1973–2014. AI/AN, American Indian and Alaska natives; A/PI, Asian and Pacific Islanders. b Childhood brain/CNS mortality by race, risk ratio (SEER, 1973–2014). The error bars represent the parameter values and precision on the mortality experience by race from childhood brain/CNS tumors in the Surveillance Epidemiology and End Results (SEER) data, 1973–2014. The white race is the reference group, with the risk ratio (RR) = 1.0. AI/AN, American Indian and Alaska natives; A/PI, Asian and Pacific Islanders
Mortality Prognostic Factors and Risk Modeling
Year and Age Cohort Effect
There was year of diagnosis cohort effect on mortality. The cohort effect showed a dose-response slope, with survival advantage associated with the later years of diagnosis compared to 1973–1977. From a 5-year interval, 1973–1977, there was a dose-response reduction in mortality, with 1973–1977 as the reference year group (risk ratio (RR) = 1.0); the risk ratio for 2008–2012 was 0.36 (RR = 0.36, 95% C.I. 0.33–0.39) while that for 2013–2014 was 0.18 (RR = 0.18, 95% C.I. 0.16–0.21).
The < 1 year at the age of diagnosis illustrated the worse mortality experience, implying the highest burden of the disease in this age group. Compared to < 1 year, 1–4, 5–9, 10–14, and 15–19 years at the age of diagnosis were 31, 27, 38, and 34% less likely to die from brain/CNS tumor.
Tumor Histology, Race, and Sex
The mortality prevalence by histology was the highest in gliomas (35.2%), medulloblastoma (26.1%), astrocytoma (22.5%), and ependymomas (9.3%). The mortality varied by race, with blacks demonstrating survival disadvantage compared to whites (Table 2). Relative to whites, blacks were 21% more likely to die [RR 1.21, 95% C.I. 1.13–1.28]. Similarly, relative to whites, there was a significant increased risk of mortality among Asians/Pacific Islanders (RR 1.12, 95%CI 1.03–1.42). Although statistically unstable in terms of parameter precision, but clinically meaningful in terms of difference or effect size, American Indian and Alaska Native were 14% more likely to die compared to whites (RR 1.14, 95% CI 0.92–1.42) (Fig. 2b). With respect to the survival experience by sex, the mortality prevalence was higher in males (55.4%) compared to that in females (44.6%), χ2 = 3.88 (1), p = 0.04. Compared to females, males were 4% more likely to die (RR = 1.04, CI 1.00–1.08).
Race Exposure Effect as Function of Mortality: Multivariable Modeling
After controlling for tumor prognostic factors, racial disparities in brain/CNS tumors persisted and blacks were 16% more likely from brain/CNS tumors relative to whites [adjusted risk ratio (aRR) = 1.16, 99% CI (1.8–1.25)] (Table 3).
Discussion
The purpose of this study was to characterize brain/CNS tumors by socio-demographics. In addition, we aimed to assess racial and sex variances in both cumulative incidence and mortality. There are a few relevant findings based on the current study: First, racial differences were observed in incidence of brain/CNS tumors. Second, the temporal trend from 1973 to 2014 varied by race and year of diagnosis. Third, the cumulative incidence was higher among whites compared to that among blacks: a higher number of white children were diagnosed with brain/CNS tumors relative to blacks and other race. Fourth, mortality varied by race, with blacks observed with survival disadvantage relative to whites. Further, after controlling for the confounders, implying the removal of exposure effect heterogeneity, racial disparity in pediatric brain/CNS tumors persisted.
In this study, we illustrated that brain/CNS tumors’ cumulative incidence varied by race. Epidemiologic and clinical data on overall pediatric cancer supports this finding [16,17,18,19]. Surawicz et al. [16] illustrated the differences in the distribution of brain/CNS cancer by gender and race; males had a higher incidence rate compared to females, while whites had a higher incidence rate than any other race. The observation of an increased incidence in whites is not unexpected [20], given both individual and group heterogeneity in terms of exposure effect that might explain in part the observed excess of diagnosis among whites despite mortality disadvantage of blacks. It is also plausible that the excess cumulative incidence among whites might be attributed to gene-environment exposure. This explanation of exposure effect on cumulative incidence is due in part to the large amount of data on environmental carcinogen especially pesticides [18, 21, 22]. Likewise, parental exposure such as uterine exposure to alcohol and cigarette smoking as known carcinogens and mutagens may explain this variability [18, 23,24,25]. Additionally, the variances in the distribution of known or established risk factors in this malignancy mainly family history, genetics, sex, age, neurofibromatosis, Li-Fraumeni Syndrome (a rare autosomal dominant disease due to germline mutation of p53), and ionizing radiation by race remain a possible explanation of the racial variability in cumulative incidence herein. Further, the increasing and racially disproportionate use of electronic devices including though not limited to cell phones, iPods, iPads, e-books, and Kindle by children may account for these subpopulation variances in brain/CNS incidence since cumulative incidence of brain/CNS tumor is highest among whites, intermediate among blacks/AA, and lowest among Asians and Hispanics [26].
Survival disadvantage of blacks in overall pediatric malignancy have been previously observed [25, 27, 28]. In this study, we demonstrated the survival disadvantage of blacks in brain/CNS tumors. This observation from the current study is supported in part by previous epidemiologic and clinical data on mortality [20, 29, 30]. Early-stage diagnosis of malignancy is indicative of good prognosis, implying survival advantage [31]. Available data from our sample indicated poorly differentiated tumor among blacks relative to that among whites. Additionally, blacks had less access to both diagnosis and therapeutics, which tends to explain the survival disadvantage observed in these data. The insurance data though is limited due to inability of the SEER registries to collect data from the initiation of this registry in 1973. The current insurance data reflects malignancies diagnosed from 2011 to 2014. Despite these data insufficiencies, insurance still correlated with mortality.
The heterogeneity of exposure effect or treatment effect is expected to be addressed after controlling for the confounders and balancing the prognostic factors respectively. With race as a function of mortality in this study, we examined the other exposure effect heterogeneity as a confounder. After controlling for these confounders, the racial disparity in brain/CNS pediatric tumors persisted. Other studies have observed similar insufficiencies [20, 29, 32]. The observed inability to remove the variance or the differences by race with respect to brain/CNS malignancy may be due to unmeasured confounders such as parental education, income, disadvantaged neighborhood factors, and other unidentified exposures that might predispose to, or precipitate, cancer survival including brain/CNS malignancies in children. It is also biologically plausible that gene and environment interaction observed in mRNA transcription and gene expression may differ across subpopulations, which may tend to predispose black children to excess mortality coupled with early childhood adverse events that have been shown to affect gene expression [33]. Epigenetic change or alteration commences very early in life (gametogenesis) as a result of changes that do not affect DNA sequence but are epigenotypic (gene and environment interaction—diet, chemical exposure, hormones, etc.). For example, the subpopulation variation in the DNA methylation which is the transformation of the promoter region of the gene, where transcription occurs by a methyl group (CH3) to 5′-methylcytosine resulting in the inhibition of transcription, affecting protein synthesis involved in apoptotic and proliferative cellular processes, remains a feasible explanation of the observed survival disadvantage of blacks/AA relative to whites. These epigenomic alterations or modifications may predispose to brain/CNS aggressive variants in blacks, implying poorer prognosis. In effect, epigenomic studies present a collaborative opportunity to examine epigenetic alterations in the diseased or defective gene in black and white brain/CNS childhood cases, using DNA methylation for gene expression associated with hypo- and hypermethylation. With such initiatives, there remains an opportunity for specific risk characterization and preselection treatment with induction therapy.
Despite the strengths of this study, mainly large sample and accurate modeling, there are some limitations. First, we utilized retrospective design, which is prone to information and selection bias. Because we processed our data, examining missing variables and outliers, it is highly unlikely that these findings are driven solely by misclassification bias. Secondly, the retrospective nature of these data implies limited causal inference with respect to brain/CNS mortality and effect of race, given race as surrogate for health inequity, as well as other potential confounding variables with respect to exposure effect heterogeneity. Despite this observation on causal inference, the observed racial disparities in brain/CNS mortality do not appear to be influenced by causal inference limitation since race was identified or established before the tumor diagnosis. Thirdly, despite controlling for confounders, this study might be influenced in part by unmeasured and residual confounders. However, it is highly unlikely that the findings of temporal trends and mortality disadvantage of some subpopulations of children with brain/CNS tumors, mainly blacks, are driven solely by this unmeasured and residual confounder, since no matter how sophisticated the statistical software used, residual confounder persists [34]. The persistent failure of the multivariable model to remove disparities after controlling for confounders is due in greater part to the unavailability of the potential confounding variables in the SEER dataset, namely, health inequity variables (employment, income, access to care, transportation, and navigation). Further, the application of “other race” provides no meaningful approach to intervention mapping in brain/CNS cumulative incidence and mortality risk reduction. However, this study examined other races namely American Indian/Alaska Native and Asian/Pacific Islander. Nevertheless, since Hispanics constitute a substantial portion of the US population as well as SEER demographics, future studies on brain/CNS tumors in children should assess the cumulative incidence and survival in this subpopulation for intervention mapping.
Conclusion
In summary, there is a temporal trend in brain/CNS tumors with cumulative incidence higher among whites relative to that among blacks. The mortality experience from these malignancies varied by race, with blacks experiencing survival disadvantage which persisted after controlling for exposure effect heterogeneity. Despite the accuracy and validity of these data, caution should be exercised in their interpretation and application in clinical settings and public health arena due to the inability of NCI to provide reliable and relevant population data such as income and other social determinants of health variables, as exposure function of health inequity. Racial disparities in cumulative incidence and mortality existed and persisted after controlling for confounding variables. These findings are suggestive of future studies to examine the social determinants of health and their relationship with brain/CNS tumor incidence as well as mortality in order to assess and address for confounding factors, namely health inequity.
References
Fischer C, Petriccione M, Donzelli M, Pottenger E. Improving care in pediatric neuro-oncology patients: an overview of the unique needs of children with brain tumors. 2016;31(4):488–505. doi:https://doi.org/10.1177/0883073815597756.
Center for Disease Control & Prevention. Cancer among children: cancer prevention and care. https://www.cdc.gov/cancer/dcpc/data/children.htm. Published 2014.
Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. Neuro-Oncology. 2012;14(November):v1–v49. https://doi.org/10.1093/neuonc/nos218.
National Cancer Institute. Childhood brain and spinal cord tumors treatment overview—health professional version. https://www.cancer.gov/types/brain/hp/child-brain-treatment-pdq#section/_407. Published 2017.
Mathew RK, Kane RO, Parslow R, et al. Comparison of survival between the UK and US after surgery for most common pediatric CNS tumors. Neuro-Oncology. 2014;16(8):1137–45. https://doi.org/10.1093/neuonc/nou056.
Ostrom QT, Gittleman H, Farah P, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro-Oncology. 2013;15:1–56.
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro-Oncology. 2015;17(suppl 4):1–62. https://doi.org/10.1093/neuonc/nov189.
Abadin SS, Zoellner NL, Schaeffer M, Porcelli B, Gutmann DHJK. Racial/ethnic differences in pediatric brain tumor diagnoses in patients with neurofibromatosis type 1. J Pediatr. 2015;167(3):613–20. https://doi.org/10.1016/j.jpeds.2015.04.076.
Reimers TS, Mortensen EL, Nysom K, Schmiegelow K. Health-related quality of life in long-term survivors of childhood brain tumors. Pediatr Blood Cancer. 2009;53(April):1086–91. https://doi.org/10.1002/pbc.
Schulte F, Barrera M. Social competence in childhood brain tumor survivors: a comprehensive review. Support Care Cancer. 2010;18(12):1499–513. https://doi.org/10.1007/s00520-010-0963-1.
Rao AAN, Scafidi J, EM Wells RP. Biologically targeted therapeutics in pediatric brain tumors. Pediatr Neurol. 2012;46(4):203–11.
Villano JL, Koshy M, Shaikh H, Dolece TA, BJ MC. Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer. 2011;105(9):1414–8. https://doi.org/10.1038/bjc.2011.357.
Program SE and ER (SEER). SEER*Stat database: incidence-SEER 9 regs research datac(1973–2014) < Katrina/Rita Population Adjustment> − county attributes - total U.S., 1969–2015 counties. National Cancer Institute. https://seer.cancer.gov/data/citation.html. Published 2017. Accessed January 1, 2017.
Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International classification of childhood cancer, third edition. Cancer. 2005;103(7):1457–67. https://doi.org/10.1002/cncr.20910.
Surveillance Research Program, National Cance Institute SEER*Stat software version 8. 3.. SEER statistical software v 8.3.4. 2016. www.seer.cancer.gov/seerstat.
Surawicz TS, Mccarthy BJ, Kupelian V, Jukich PJ, Bruner JM, Davis FG. Descriptive epidemiology of primary brain and CNS tumors: results from the Central Brain Tumor Registry of the United States ,. Neuro Oncol. 1998;(October):14–25, 40, 2, 151, 160, DOI: https://doi.org/10.1023/A:1006091608586.
Klassen AF, Anthony SJ, Khan A, Sung L, Klaassen R. Identifying determinants of quality of life of children with cancer and childhood cancer survivors: a systematic review. Support Care Cancer. 2011;19(9):1275–87. https://doi.org/10.1007/s00520-011-1193-x.
Holmes L, Vandenberg J, McClarinl L, Dabney K. Epidemiologic, racial and healthographic mapping of Delaware pediatric cancer: 2004–2014. Int J Environ Res Public Health. 2015;13(1):2004–14. https://doi.org/10.3390/ijerph13010049.
Siegel DA, Singh L. Racial differences in survival of pediatric patients with brain and central nervous system cancer, United States, 2001–2012. Ann Epidemiol. 2017;27(8):505. https://doi.org/10.1016/j.annepidem.2017.07.040.
Patel S, Bhatnagar A, Wear C, Osiro S, Gabriel A, Kimball D, et al. Are pediatric brain tumors on the rise in the USA? Significant incidence and survival findings from the SEER database analysis. Childs Nervs Syst. 2014;30(1):147–54. https://doi.org/10.1007/s00381-013-2307-1.
George J, Shukla Y. Pesticides and cancer: insights into toxicoproteomic-based findings. J Proteome. 2011;74(12):2713–22. https://doi.org/10.1016/j.jprot.2011.09.024.
Maele-Fabry GV, Hoet P, Lison D. Parental occupational exposure to pesticides as risk factor for brain tumors in children and young adults: a systematic review and meta-analysis. Environ Int. 2013;56:19–31. www.sciencedirect.com/science/article/pii/S0160412013000500. https://doi.org/10.1016/j.envint.2013.02.011.
Wang N, Tikellis G, Pezic A, Wang L, Wells JCK, Cochrane J, et al. The effect of maternal prenatal smoking and alcohol consumption on the placenta-to-birth weight ratio. J Placenta. 2014;35(7):437–41. www.sciencedirect.com/science/article/pii/S0143400414001581. https://doi.org/10.1016/j.placenta.2014.04.006.
Heck JE, Contreras ZA, Park AS, Davidson TB, Cockburn M, Ritz B. Smoking in pregnancy and risk of cancer among young children: a population-based study. Int J Cancer. 2016;139(3):613–6. https://doi.org/10.1002/ijc.30111.
Holmes L, Hossain J, Desvignes-Kendrick M, Opara F. Sex variability in pediatric leukemia survival: large cohort evidence. ISRN Oncol. 2012;2012:439070. https://doi.org/10.5402/2012/439070.
Von Behren J, Reynolds P. Birth characteristics and brain cancers in young children. Int J Epidemiol. 2003;32(2):248–56. https://doi.org/10.1093/ije/dyg057.
Ward E, Desantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):83–103. https://doi.org/10.3322/caac.21219.
Amin R, Bohnert A, Holmes L, Rajasekaran A, Assanasen C. Epidemiologic mapping of florida childhood cancer clusters. Pediatr Blood Cancer. 2010;54(4):511–8. https://doi.org/10.1002/pbc.22403.
Holmes Jr LNLDK. Survival variability in Delaware pediatric cancer: translational initiative. Vol 27.; 2017. http://www.sciencedirect.com/science/article/pii/S1047279717303642.
Bondy ML, Scheurer ME, Malmer B, Barnholtz-Sloan JS, Davis FG, Il'yasova D, et al. Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer. 2008;113(7):1953–68. https://doi.org/10.1002/cncr.23741.
Flores LE, Williams DL, Bell BA, O’Brein M, Delay RA. In the diagnosis of pediatric brain tumors. Am J Dis Child. 1986;140(7):684–6.
Bhatia S. Disparities in cancer outcomes: lessons learned from children with cancer. Pediatr Blood Cancer. 2011;56(6):994–1002. https://doi.org/10.1002/pbc.23078.
Spector LG, Street D, Pankratz N, Marcotte EL. Genetic and nongenetic risk factors for childhood cancer. Pediatr Clin N Am. 2015;62(1):11–25. https://doi.org/10.1016/j.pcl.2014.09.013.Genetic.
Holmes L, Chan W, Jiang ZDX. Effectiveness of androgen deprivation therapy in prolonging survival of older mean treated for locoregional prostate cancer. Prostate Cancer Prostatic Dis. 2007;10(4):388–95. https://doi.org/10.1038/sj.pcan.4500973.
Acknowledgements
The authors acknowledge the contribution of SEER in providing the data used in this study; however, SEER is not responsible for the assessment of these data, but the sole responsibility of the primary author LH. Secondly, the authors would like to acknowledge Patricia Oceanic and April Aguilera for coordinating the administrative aspect of this project.
Funding
This study received no external funding.
Author information
Authors and Affiliations
Contributions
LH conceptualized the study, acquired the data, performed the analysis, interpreted the data, prepared the manuscript, and reviewed and approved the final draft. PC extracted the data from the SEER database, processed the data, assisted in the analysis, tabulated the results, interpreted the data, prepared the manuscript, and reviewed and approved the final draft.
TB facilitated data processing and preparation of the manuscript and reviewed and approved the final draft. KB assisted in manuscript preparation and data interpretation, and reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic Supplementary Material
ESM 1
(DOCX 48 kb)
Rights and permissions
About this article
Cite this article
Holmes, L., Chavan, P., Blake, T. et al. Unequal Cumulative Incidence and Mortality Outcome in Childhood Brain and Central Nervous System Malignancy in the USA. J. Racial and Ethnic Health Disparities 5, 1131–1141 (2018). https://doi.org/10.1007/s40615-018-0462-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-018-0462-5