Abstract
Purpose of Review
Ewing sarcoma is the second most common bone cancer seen in children and adolescents. Previous reports have demonstrated that the main driver of malignancy in this disease is an aberrant transcription factor that is expressed by gene fusions between the EWSR1 gene and an ETS family transcription factor such as FLI1 or ERG. Here we review recent preclinical and clinical advances in drug development for the treatment of Ewing sarcoma. We also discuss the rationale for promising combination therapies that have been considered in the interest of developing treatments for Ewing sarcoma.
Recent Findings
The main driver of malignancy in this disease is EWS-FLI1. There have been valiant efforts to develop targeted therapies targeting EWS-FLI1, epigenetic factors, factors that affect transcription and the repurposing of previously approved drugs has also been of interest.
Summary
The underlying mechanisms of how EWS-FLI1 contributes to malignancy in Ewing sarcoma have been extensively studied. Through these observations, EWS-FLI1 targeting and inhibition of aberrant transcription of downstream targets has been proposed as a potential pharmacologic treatment. Improved understanding of how newly developed compounds affect this disease, keeping associated toxicities in mind have led to structure activity relationship studies that have demonstrated improved efficacy and toxicity when treating at the preclinical level. Although there have been many challenges translating these promising results in the clinic, there are further studies ongoing to improve these efforts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ewing sarcoma (ES) is an aggressive malignant tumor that occurs in bones and soft tissue and is the second most common bone malignancy after osteosarcoma [1]. Primarily, this disease affects children and adolescents with about 200 patients being diagnosed annually in the USA. For patients with localized and metastatic disease the current standard chemotherapy for ES consists of four to six alternating cycles of VDC/IE (vincristine, doxorubicin, cyclophosphamide/ifosfamide and etoposide) [2, 3•]. The 5-year survival rate for patients with localized disease is about 83%. Unfortunately, patients with metastatic and/or recurrent disease have an overall survival rate of less than 20% [4]. Even those patients who do successfully recover and become long-term survivors often suffer from late effects of their therapy [5, 6, 7•, 8,9,10]. Many of these patients suffer from the development of secondary malignancies including hematopoietic cancers, carcinoma, and other sarcoma like cancers [11]. ES patients also suffer from reduced fertility, renal insufficiency, and cardiomyopathy [8]. Therefore, there is a need to develop treatments that specifically target the underlying biological drivers of this disease. The ES family of tumors (ESFT) is characterized by a unique chromosomal translocation that gives rise to specific gene fusions that involve the EWSR1 gene and ETS transcription factors with the end result being malignant transformation and disease progression. In 85% of ES cases, there is an associated t(11;22) (q24;q12) chromosomal translocation, which leads to the formation of the EWSR1-FLI1 fusion gene [12] whereas in 10–15% of ES cases, there is the EWSR1-ERG fusion gene arising from the t(21;12) (22;12) [12]. The remaining 1–5% of ES cases harbor one of several possible translocations resulting in a fusion gene that contains the EWSR1 gene and a member of the ETS family of transcription factors (Table 1) [1].
Structurally, the EWS and FLI1 components of the fusion protein EWS-FLI1 have unique activity. The c-terminus, comprised of a significant portion of the FLI1 protein, acts as the DNA-binding domain, while EWS, at the N terminus, acts as a transcriptional activator. In general, EWS-FLI1 localizes in the nucleus and binds DNA at GGAA microsatellite repeats to promote transcription of its downstream targets [13, 14]. Notably, the DNA-binding domain is conserved among all 28 members of the ETS family. The transcription program mediated by EWS-ETS leads to malignant transformation, allows cells to maintain a de-differentiated state, and affords them to circumvent toxicity associated with DNA damaging agents [15•, 16, 17]. Preclinical data aimed at understanding the role of EWS-FLI1 in ESFT viability has shown that silencing of EWS-FLI1 expression markedly impairs ES cell growth [18]. Many different approaches have been followed in efforts to develop therapeutic agents that target the biological drivers or malignant phenotype of ES. Here we highlight six classes of experimental agents: (i) DNA-binding agents targeting EWS-FLI1 and protein partners, (ii) agents that reverse transcriptional signature of EWS-FLI1, (iii) kinase inhibitors, (iv) inhibitors of LSD1 (lysine-specific demethylase 1), (v) inhibitors of poly ADP ribose polymerase-1 (PARP-1), and (vi) microtubule inhibitors.
Targeting EWS-FLI1
YK-4-279
The EWS-FLI1 transcriptional complex includes CREB-binding protein, RNA polymerase II, and RNA helicase A (RHA) [19, 20•]. It has been previously reported that RHA increases EWS-FLI1–mediated transcription, suggesting that these protein interactions are important for ES oncogenesis [20•]. EWS-FLI1 binds to RHA in a unique position where if inhibited it would not interfere with any other transcriptional or RNA metabolism proteins (Fig. 1a) [20•]. Based on these experimental discoveries, RHA inhibition is an attractive target for treating ES. Erkizan et al. developed the small molecule YK-4-279 as an inhibitor of RHA: EWS-FLI1 binding. YK-4-279 binds RHA inhibiting its ability to bind and interact with EWS-FLI1 at low micromolar concentrations [21]. They also demonstrated that YK-4-279 treatment inhibits EWS-FLI1 functionality. Luciferase reporter assays were conducted to demonstrate EWS-FLI1 activity at the NR0B1 promoter upon dose dependent YK-4-279 treatment in COS7 cells [21]. YK-4-279 was also shown to induce apoptosis and inhibit ES cell growth [21]. Efficacy studies in ES xenografts displayed significant decreases in tumor size compared with control showing potential use for YK-4-279 in the clinic [21]. Due to poor clinical activity, YK-4-279 is no longer being evaluated for the treatment of ES its clinical derivative TK216 which, is currently being evaluated in patients with relapsedor refractory ES [22•].
Mithramycin
In efforts to discover an EWS-FLI1 inhibitor a 50,000-compound high-throughput screen was conducted at the National Cancer Institute (NCI) in 2011. Cell-based luciferase reporter screens in TC32 ESFT cells identified mithramycin as a potent inhibitor of EWS-FLI1 (Fig. 1b) [23•]. Mithramycin is a tricyclic polyketide that was originally isolated from Streptomyces argillaceus for its antibiotic activity but was later found to have potent anti-tumor activity [24]. Mithramycin was characterized based on its ability to inhibit EWS-FLI1 activity in vitro using microarray expression profiling, qRT-PCR, and immunoblot analysis. In vitro assays displayed mithramycin ability to inhibit expression of downstream EWS-FLI1 targets at the mRNA and protein levels. In vivo studies included xenograft studies where mithramycin suppressed tumor growth in two different ESFT models [23•].
The success of this preclinical study prompted a phase I/II clinical study of mithramycin in children and adults with refractory ES [25•]. Results from the clinical trial showed that mithramycin has a very narrow therapeutic window. At doses relevant to treat and decrease tumor size in these patients, toxicity was prevalent [25•]. The average maximal mithramycin plasma concentration in patients was 17.8 ± 4.6 ng/mL. The average plasma concentrations of mithramycin measured were extremely low compared with the sustained mithramycin concentrations required to suppress EWS–FLI1 transcriptional activity in preclinical studies at ≥ 50 nmol/L [25•]. Patients displayed high levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), hallmarks of severe liver damage [25•]. It has been reported that mithramycin binds DNA specifically at GC sites, inhibiting the transcription factor Sp1 from binding and regulating expression of thousands of genes [26]. There is evidence that the inhibition of Sp1 by mithramycin is a substantial part of its associated toxicity [27]. This data has helped to guide the development of second generation mithramycin analogues that can confer potent inhibition of EWS-FLI1 while bypassing toxicities associated with mithramycin treatment.
Mechanistic studies based on the molecular mode of action of mithramycin have led to the development of novel mithramycin analogues (Fig. 1). MTMSA-Trp and MTMSA-Phe are semi synthetic analogues of mithramycin that have shown in vitro anti-cancer activity similar to mithramycin [28•]. It has also been reported that MTMSA-Trp and MTMSA-Phe bind DNA and physically interact with EWS-FLI1 [29•, 30•]. Further refinement of these mithramycin analogues has led to the development of MTMSA-Phe-Trp and MTMSA-Trp-Trp [31•]. Mitra et al. reported that both MTMSA-Phe-Trp and MTMSA-Trp-Trp have potency similar to mithramycin in ESFT cells [31•]. It was also reported that MTMSA-Phe-Trp and MTMSA-Trp-Trp are more selective for cell lines that express EWS-FLI1 than mithramycin and previously reported analogues [31•]. Further studies are currently ongoing to determine efficacy and pharmacokinetics of other analogues in xenograft mouse models of ES.
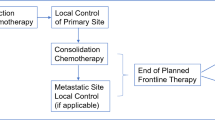
Depiction of the mechanism of action of novel treatment approaches for Ewing sarcoma. a YK-4-279 binds RHA inhibiting its interaction with EWS-FLI1 and transcription of target genes. b Mithramycin binds DNA and inhibits EWS-FLI1 mediated transcription. c Trabectedin-binding alkylates DNA distorting its structure and inhibits DNA repair protein activity and transcription factor activity. d LSD1 inhibitors bind LSD1 and prevent its interaction with EWS-FLI1. e, f CDK inhibitors bind cyclin/CDK complexes preventing phosphorylation. g PARP binds DNA and repairs DNA breaks, in the presence of olaparib PARP activity is inhibited rendering the cell vulnerable to consequences of DNA damage. h Eribulin inhibits microtubule growth causing nonproductive tubulin aggregates
Reversing the Transcriptional Signature of EWS-FLI1
Trabectedin
Trabectedin is a natural product that was originally isolated form the sea squirt Ecteinascidia turbinate [32]. Trabectedin binds DNA in the minor groove at GC-rich sequences and alkylates the amino group of guanine at position 2, bending DNA toward the major groove (Fig. 1c) [33]. A potent alkylator, its cytotoxicity comes from its ability to interact with DNA repair pathways. Trabectedin-DNA adducts can trap the transcription-coupled DNA nucleotide excision repair (TC-NER) system as it repairs DNA damage in transcribing cells, this then leads to lethal DNA breaks [34].
Clinically, trabectedin has shown activity in a wide range of malignancies, most notably in leiomyosarcoma and liposarcoma [35]. Previously it has been shown that sarcomas harboring chromosomal translocations are sensitive to trabectedin treatment [36]. Taamma et al. reported a 50% response rate in patients with myxoid liposarcoma which harbors a t(12:16) (q13;p11) chromosomal translocation FUS-CHOP, after treatment with trabectedin [36]. This finding has identified trabectedin as a potential drug of interest for the treatment of ES. Preclinical studies have shown that ES cells are sensitive to trabectedin treatment, and there is mechanistic evidence that trabectedin interferes with EWS-FLI1 activity in vitro, reversing the gene signature of the aberrant transcription factor [37, 38, 39•]. Trabectedin has not shown success in the clinic in ES patients, but there have been efforts to develop analogues that can better target the EWS-FLI1 translocation [40•]. Lurbinectedin, a trabectedin derivative, has shown evidence of activity against EWS-FLI1. This second generation trabectedin analogue causes nuclear redistribution of EWS-FLI1 from the nucleus to the nucleolus, similar to that of the parent compound trabectedin [41•]. Lurbinectedin is currently being tested in a phase 2 clinical trial in select advanced solid tumors [42•].
Inhibitors of LSD1
HCI-2509
Although there have been multiple efforts to target the transcription factor EWS-FLI1, the main oncogenic driver in ES, there has been little success in identifying a potent yet clinically acceptable small molecule inhibitor of the transcription factor. ES has one of the lowest mutation rates of any cancer, and it has emerged as a model system to investigate epigenetic aberrations resulting in oncogenesis [43•, 44, 45•]. Lysine specific demethylase 1 (LSD1) is an enzyme that functions as a histone demethylase and as a transcriptional activator and repressor [46]. LSD1 has been implicated in many malignancies including breast, prostate, bladder, lung, liver, neuroblastoma, amyloid leukemia and colorectal tumors [47,48,49,50,51,52]. In 2011, it was reported that ES expresses unusually high levels of LSD1 [53•, 54]. It has also been demonstrated that overexpression of LSD1 can drive transformation in cells [49, 54, 55]. Previous studies have demonstrated that LSD1 is required for chromosome segregation and downregulation of LSD1 can lead to abnormal centrosome duplication. This significantly impairs nuclear pore complex assembly, leading to an extended telophase [56, 57].
Initially LSD1 inhibition in ES was tested using tranylcypromine [53]. Tranylcypromine is currently prescribed as an anxiolytic and antidepressant. However, because of severe side effects associated with its treatment, its use is limited to treating patients with major depressive disorders [58]. It was shown that tranylcypromine inhibits LSD1 in a non-reversible manner, which translated to decreased cell proliferation at milli-molar concentrations in ES cells, thus supporting further exploration and development of a more potent and specific LSD1 inhibitor [53]. Sankar et al. have been investigating the therapeutic potential of HCI-2509, a non-competitive reversible small molecule inhibitor of LSD1, for the treatment of ES (Fig. 1d) [59•]. Their studies demonstrated that HCI-2509 can reverse the global oncogenic transcriptional program in ES with the use of cell viability assays and RNA-sequencing [59•]. They also demonstrated that HCI-2509 impairs tumorigenesis in vivo. As a single agent HCI-2509 decreased tumor size in comparison to the vehicle group, which led to improved survival of treated animals over 60 days, but these differences were not statistically significant [59•]. Despite this limited efficacy, an analogue of HCI-2509 known as SP-2577 is undergoing phase 1 clinical testing [60].
Kinase Inhibitors
CDK12/13 Inhibitors
One approach to treating ESFT is to target the basic transcriptional machinery with small molecule inhibitors such as THZ1, which is a covalent inhibitor of CDK7/12/13 [61]. The control of gene transcription involves a set of cyclin-dependent kinases (CDKs), including CDK7, CDK8, CDK9, CDK11, CDK12, CDK13, and CDK19 these kinases are essential to transcription, initiation and elongation. Specifically, CDKs phosphorylate RNA polymerase II (RNAPII) at its C-terminal domain (CTD) causing recruitment of transcriptional activators to the transcriptional complex [62]. THZ1 was implicated as a potential therapeutic for treating cancers defined by their high dependency on transcriptional programs for initiating transformation [63]. This was further demonstrated when 1081 cancer cell lines were screened, and ES cell lines were shown to be the most sensitive to THZ1 treatment [64]. Iniguez et al. reported that in ES cell lines THZ1 primarily targets CDK12, a kinase that regulates expression of DNA damage repair genes (Fig. 1e) [64, 65•]. Because of non-specific targeting, the THZ1 analogue THZ1531 was developed and tested in preclinical studies. These studies showed that THZ1531 was highly active in cells expressing EWS-FLI1, specifically showing an increase in proteins involved in double-stranded DNA damage repair. Considering this discovery, they then hypothesized that cells expressing EWS-FLI1 are more vulnerable to THZ1531 and other DNA damage repair inhibitors. ES cell lines have been reported to be highly sensitive to PARP inhibitors [66]. Preclinical combination study results showed strong synergy with THZ1531 and the PARP inhibitor olaparib.
Xenograft studies using THZ1 as a single agent did not cure mice of ES, suggesting that the combination of THZ1 and olaparib could be necessary to achieve complete efficacy [64]. Treatment of tumors with the combination of THZ1 and olaparib demonstrated a marked decrease in tumor size compared with control groups [64].
CDK4/6 Inhibitors
The ES genome is characterized by one of the lowest mutational rates among cancer types, implicating a possibility for epigenetic deregulation as a component for tumor development [44, 45•, 67]. Reports have shown that about 13 to 30% of ES tumors possess deletions in the gene CDKN2A, although these deletions do not appear to be associated with clinical outcome there is still some implication that this could be a target for pharmacological drug development [51, 68]. In ES, the tumor suppressors p16INK4a and p14arf arise from variant transcription start points of the CDKN2A gene, and p16 has been shown to inhibit CDK4 and CDK6–mediated phosphorylation of the RB protein, preventing cell cycle progression [69]. The alteration of p16INK4a in ES has sparked clinical interest in CDK4/6 inhibition. Cyclin D1, a regulatory subunit of CDK4 and CDK6, has also been shown to be a super enhancer in ES [70•] and consequently, in ES cells, the CyclinD1/CDK4 pathway is activated and is required for growth. Kennedy et al. conducted xenograft studies where they demonstrated that CDK4/6 inhibition decreased tumor growth [70•]. These results suggest yet another potential pathway to target oncogenic drivers of ES at the molecular level (Fig. 1f).
Currently, the CDK4/6 inhibitor, abemaciclib is being evaluated in a phase I clinical trial in children and adults with recurrent and refractory ES, neuroblastoma, rhabdomyosarcoma, and osteosarcoma [71]. The main toxicity associated with CDK4/6 inhibition is hematologic in nature, and there is growing interest in combining CDK4/6 inhibitors with cytotoxic chemotherapeutics that have non-overlapping toxicities [72]. There is also interest in combining CDK4/6 inhibitors with MEK, mTOR, and IGF-1R inhibitors, exploiting multiple pathways focusing on targets that can influence tumor growth in ES [73,74,75].
PARP-1 Inhibitors
Olaparib
Mechanistically, poly adenosine diphosphate ribose polymerase (PARP) is an enzyme that has been shown to both drive transcription and to accelerate base excision repair (Fig. 1g) [76,77,78]. Initial interest in PARP1 inhibitors have shown promising activity particularly in BRCA-mutant cancers defective in homologous repair (HR), in which they have demonstrated replication fork stalling and subsequent synthetic lethal cell death [79,80,81]. PARP inhibitors have also recently been of interest for the treatment of ES. It has been reported that ES cells express high levels of PARP mRNA and protein which translates to high PARP activity related to an increase in copy number compared with other cancers [82]. Increased PARP activity has led to the report that inhibition of PARP sensitizes ES cells to ionizing radiation [82]. In more recent studies Brenner et al. showed increased sensitivity of three ES cell lines to the PARP inhibitor olaparib, as opposed to an osteosarcoma and rhabdomyosarcoma cell line [83•]. In this study, however, olaparib was not effective as a single agent in xenograft experiments. They subsequently combined olaparib with temozolomide, a DNA alkylating agent, results displayed a marked decrease in tumor size of the xenograft models. These data represent the potential for elucidating synthetic lethality in ES cells in the presence of a PARP inhibitor and a DNA damaging agent [83•]. In 2014, a phase II clinical study was conducted evaluating the antitumor activity of olaparib, as a monotherapy in patients with refractory ES following failure of standard chemotherapy [84•]. This study concluded that olaparib administration was safe and well tolerated in patients. However, as a monotherapy, there were no significant responses or durable disease control [84•]. Currently a phase I study of olaparib and temozolomide for the treatment of ES is ongoing [85] .
Microtubule Inhibitors
Eribulin
Microtubules help support organelles, transport molecules, and give shape to the cell. The microtubule inhibitor eribulin inhibits polymerization of tubulin subunits by preventing lengthening and shortening of microtubules during cellular division (Fig. 1h) [86, 87]. When these unstable polymers of tubulin aggregate the result is apoptosis [88, 89]. Eribulin is approved by the FDA for treating metastatic breast cancer and may have promising activity in other cancers [90]. In ES, EWS-FLI1 drives expression of proteins that regulate microtubule stability, making this an attractive drug target. In pre-clinical studies, testing of eribulin in ES cell lines demonstrated Bcl-2 induced apoptosis [91]. Additionally, eribulin is FDA-approved for adult patients with liposarcoma who previously received an anthracycline [92]. An ongoing phase 2 trial is evaluating eribulin in patients with relapsed/refractory rhabdomyosarcoma and ES [93]. Another phase 1/2 clinical trial is evaluating the combination of eribulin with irinotecan in children with refractory and recurrent rhabdomyosarcoma and ES as well [94]. Overall, eribulin has shown strong preclinical and clinical results in ES, thus giving it great potential as either a monotherapy and in combination with another approved chemotherapeutic.
Conclusion
ES treatment relies on combinations of surgery, radiation, and traditional chemotherapeutic regiments. In many ES patients, these conventional treatment approaches are not enough to remedy this aggressive cancer. Additionally, ES patients in remission must deal with considerable acute and long-term toxicities associated with these therapies. Improving the outcomes for patients with ES will require development of targeted therapies. Therefore, a thorough understanding of the activity, translation, and verification of novel agents is vital in targeting biologically relevant drivers of ES. This is important for clinical development of successful targeted therapies. In this review, we focused on several approaches targeting specific pathways that play a part in ESFT growth in patients. Targeting the EWS–FLI1 transcription factor directly is an approach that has shown promising results but has also been met with many challenges. A major challenge will be to discover a pharmacologic inhibitor that selectively acts to disrupt the function of EWS-FLI1. Alternatively, blocking important pathways, inhibiting the downstream gene signature of EWS-FLI1 and exploiting PARP inhibitor sensitivities have shown promising preclinical results that have yet to be translated in the clinic. Continued efforts toward developing novel therapeutics targeting specific molecular abnormalities in ES are currently ongoing in efforts to improve survival outcomes for these patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Riggi N, Stamenkovic I. The biology of Ewing sarcoma. Cancer Lett. 2007;254(1):1–10. https://doi.org/10.1016/j.canlet.2006.12.009.
Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med. 2003;348(8):694–701. https://doi.org/10.1056/NEJMoa020890.
• Mark C. Gebhardt MGD. MS. Treatment of the Ewing sarcoma family of tumors. UpToDate: MD; 2019. https://www.uptodate.com/contents/treatment-of-the-ewing-sarcoma-family-of-tumors#H21
Grohar PJ, Helman LJ. Prospects and challenges for the development of new therapies for Ewing sarcoma. Pharmacol Ther. 2013;137(2):216–24. https://doi.org/10.1016/j.pharmthera.2012.10.004.
Rodriguez-Galindo C, Liu T, Krasin MJ, Wu J, Billups CA, Daw NC, et al. Analysis of prognostic factors in Ewing sarcoma family of tumors: review of St. Jude Child Res Hosp Stud Cancer. 2007;110(2):375–84. https://doi.org/10.1002/cncr.22821.
Bacci G, Forni C, Longhi A, Ferrari S, Donati D, De Paolis M, et al. Long-term outcome for patients with non-metastatic Ewing’s sarcoma treated with adjuvant and neoadjuvant chemotherapies. 402 patients treated at Rizzoli between 1972 and 1992. European Journal of Cancer (Oxford, England : 1990). 2004;40(1):73–83.
• Marina NM, Liu Q, Donaldson SS, Sklar CA, Armstrong GT, Oeffinger KC, et al. Longitudinal follow-up of adult survivors of Ewing sarcoma: a report from the childhood cancer survivor study. Cancer. 2017;123(13):2551–60. BACKGROUND: Ewing sarcoma survivors (ESSs) are at increased risk for treatment-related complications. The incidence of treatment-related morbidity and late mortality with aging is unknown. METHODS: This study reports survival probabilities, estimated with the Kaplan-Meier method, and the cumulative incidence of cause-specific mortality and chronic conditions among ESSs in the Childhood Cancer Survivor Study who were treated between 1970 and 1986. Piecewise exponential models were used to estimate relative rates (RRs) and 95% confidence intervals (CIs) for these outcomes. Chronic conditions were graded with the Common Terminology Criteria for Adverse Events (version 4.03). RESULTS: Among 404 5-year ESSs (median age at last follow-up, 34.8 years; range, 9.1-54.8 years), the 35-year survival rate was 70% (95% CI, 66%-74%). Late recurrence (cumulative incidence at 35 years, 15.1%) was the most common cause of death, and it was followed by treatment-related causes (11.2%). There were 53 patients with subsequent neoplasms (SNs; cumulative incidence at 35 years, 24.0%), and 38 were malignant (14.3% at 35 years). The standardized incidence ratios were 377.1 (95% CI, 172.1-715.9) for osteosarcoma, 28.9 (95% CI, 3.2-104.2) for acute myeloid leukemia, 14.9 (95% CI, 7.9-25.5) for breast cancer, and 13.1 (95% CI, 4.8-28.5) for thyroid cancer. Rates of chronic conditions were highest for musculoskeletal (RR, 18.1; 95% CI, 12.8-25.7) and cardiac complications (RR, 1.8; 95% CI, 1.4-2.3). Thirty-five years after the diagnosis, the cumulative incidences of any chronic conditions and 2 or more chronic conditions were 84.6% (95% CI, 80.4%-88.8%) and 73.8% (95% CI, 67.8%-79.9%), respectively. CONCLUSIONS: With extended follow-up, ESSs’ risk for late mortality and SNs does not plateau. Treatment-related chronic conditions develop years after therapy, and this supports the need for lifelong follow-up. Cancer 2017;123:2551-60. (c) 2017 American Cancer Society.
Fuchs B, Valenzuela RG, Inwards C, Sim FH, Rock MG. Complications in long-term survivors of Ewing sarcoma. Cancer. 2003;98(12):2687–92. https://doi.org/10.1002/cncr.11891.
Navid F, Billups C, Liu T, Krasin MJ, Rodriguez-Galindo C. Second cancers in patients with the Ewing sarcoma family of tumours. Eur J Cancer (Oxford, England : 1990). 2008;44(7):983–91. https://doi.org/10.1016/j.ejca.2008.02.027.
Ginsberg JP, Goodman P, Leisenring W, Ness KK, Meyers PA, Wolden SL, et al. Long-term survivors of childhood Ewing sarcoma: report from the childhood cancer survivor study. J Natl Cancer Inst. 2010;102(16):1272–83. https://doi.org/10.1093/jnci/djq278.
Fuchs B, Valenzuela RG, Petersen IA, Arndt CA, Sim FH. Ewing's sarcoma and the development of secondary malignancies. Clin Orthop Relat Res. 2003;415:82–9. https://doi.org/10.1097/01.blo.0000093900.12372.e4.
Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M, et al. Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature. 1992;359(6391):162–5. https://doi.org/10.1038/359162a0.
May WA, Gishizky ML, Lessnick SL, Lunsford LB, Lewis BC, Delattre O, et al. Ewing sarcoma 11;22 translocation produces a chimeric transcription factor that requires the DNA-binding domain encoded by FLI1 for transformation. Proc Natl Acad Sci U S A. 1993;90(12):5752–6.
May WA, Lessnick SL, Braun BS, Klemsz M, Lewis BC, Lunsford LB, et al. The Ewing's sarcoma EWS/FLI-1 fusion gene encodes a more potent transcriptional activator and is a more powerful transforming gene than FLI-1. Mol Cell Biol. 1993;13(12):7393–8.
• Gorthi A, Romero JC, Loranc E, Cao L, Lawrence LA, Goodale E, et al. EWS-FLI1 increases transcription to cause R-loops and block BRCA1 repair in Ewing sarcoma. Nature. 2018;555(7696):387–91. https://doi.org/10.1038/nature25748. Ewing sarcoma is an aggressive paediatric cancer of the bone and soft tissue. It results from a chromosomal translocation, predominantly t(11;22)(q24:q12), that fuses the N-terminal transactivation domain of the constitutively expressed EWSR1 protein with the C-terminal DNA binding domain of the rarely expressed FLI1 protein. Ewing sarcoma is highly sensitive to genotoxic agents such as etoposide, but the underlying molecular basis of this sensitivity is unclear. Here we show that Ewing sarcoma cells display alterations in regulation of damageinduced transcription, accumulation of R-loops and increased replication stress. In addition, homologous recombination is impaired in Ewing sarcoma owing to an enriched interaction between BRCA1 and the elongating transcription machinery. Finally, we uncover a role for EWSR1 in the transcriptional response to damage, suppressing R-loops and promoting homologous recombination. Our findings improve the current understanding of EWSR1 function, elucidate the mechanistic basis of the sensitivity of Ewing sarcoma to chemotherapy (including PARP1 inhibitors) and highlight a class of BRCA-deficient-like tumours.
Ban J, Bennani-Baiti IM, Kauer M, Schaefer KL, Poremba C, Jug G, et al. EWS-FLI1 suppresses NOTCH-activated p53 in Ewing's sarcoma. Cancer Res. 2008;68(17):7100–9. https://doi.org/10.1158/0008-5472.can-07-6145.
Riggi N, Suvà M-L, Suvà D, Cironi L, Provero P, Tercier S, et al. EWS-FLI-1 expression triggers a Ewing’s sarcoma initiation program in primary human mesenchymal stem cells. Cancer Res. 2008;68(7):2176–85. https://doi.org/10.1158/0008-5472.Can-07-1761.
Maksimenko A, Malvy C. Oncogene-targeted antisense oligonucleotides for the treatment of Ewing sarcoma. Expert Opin Ther Targets. 2005;9(4):825–30. https://doi.org/10.1517/14728222.9.4.825.
Petermann R, Mossier BM, Aryee DN, Khazak V, Golemis EA, Kovar H. Oncogenic EWS-Fli1 interacts with hsRPB7, a subunit of human RNA polymerase II. Oncogene. 1998;17(5):603–10. https://doi.org/10.1038/sj.onc.1201964.
• Toretsky JA, Erkizan V, Levenson A, Abaan OD, Parvin JD, Cripe TP, et al. Oncoprotein EWS-FLI1 activity is enhanced by RNA helicase A. Cancer Res. 2006;66(11):5574–81. https://doi.org/10.1158/0008-5472.Can-05-3293. RNA helicase A (RHA), a member of the DEXH box helicase family of proteins, is an integral component of protein complexes that regulate transcription and splicing. The EWS-FLI1 oncoprotein is expressed as a result of the chromosomal translocation t(11;22) that occurs in patients with the Ewing's sarcoma family of tumors (ESFT). Using phage display library screening, we identified an EWS-FLI1 binding peptide containing homology to RHA. ESFT cell lines and patient tumors highly expressed RHA. GST pull-down and ELISA assays showed that EWS-FLI1 specifically bound RHA fragment amino acids 630 to 1020, which contains the peptide region discovered by phage display. Endogenous RHA was identified in a protein complex with EWS-FLI1 in ESFT cell lines. Chromatin immunoprecipitation experiments showed both EWS-FLI1 and RHA bound to EWS-FLI1 target gene promoters. RHA stimulated the transcriptional activity of EWS-FLI1 regulated promoters, including Id2, in ESFT cells. In addition, RHA expression in mouse embryonic fibroblast cells stably transfected with EWS-FLI1 enhanced the anchorage independent phenotype above that with EWS-FLI1 alone. These results suggest that RHA interacts with EWS-FLI1 as a transcriptional cofactor to enhance its function.
• Erkizan HV, Kong Y, Merchant M, Schlottmann S, Barber-Rotenberg JS, Yuan L, et al. A small molecule blocking oncogenic protein EWS-FLI1 interaction with RNA helicase A inhibits growth of Ewing’s sarcoma. Nat Med. 2009;15(7):750–6. https://doi.org/10.1038/nm.1983. Many sarcomas and leukemias carry nonrandom chromosomal translocations encoding tumor specific mutant fusion transcription factors that are essential to their molecular pathogenesis. Ewing's sarcoma family tumors (ESFTs) contain a characteristic t(11;22) translocation leading to expression of the oncogenic fusion protein EWS-FLI1. EWS-FLI1 is a disordered protein that precludes standard structure-based small-molecule inhibitor design. EWS-FLI1 binding to RNA helicase A (RHA) is important for its oncogenic function. We therefore used surface plasmon resonance screening to identify compounds that bind EWS-FLI1 and might block its interaction with RHA. YK-4-279, a derivative of the lead compound from the screen, blocks RHA binding to EWS-FLI1, induces apoptosis in ESFT cells and reduces the growth of ESFT orthotopic xenografts. These findings provide proof of principle that inhibiting the interaction of mutant cancer-specific transcription factors with the normal cellular binding partners required for their oncogenic activity provides a promising strategy for the development of uniquely effective, tumor-specific anticancer agents.
TK216 in patients with relapsed or refractory Ewing sarcoma. https://ClinicalTrials.gov/show/NCT02657005.
• Grohar PJ, Woldemichael GM, Griffin LB, Mendoza A, Chen QR, Yeung C, et al. Identification of an inhibitor of the EWS-FLI1 oncogenic transcription factor by high-throughput screening. J Natl Cancer Inst. 2011;103(12):962–78. https://doi.org/10.1093/jnci/djr156. BACKGROUND: Chromosomal translocations generating oncogenic transcription factors are the hallmark of a variety of tumors, including many sarcomas. Ewing sarcoma family of tumors (ESFTs) are characterized by the t(11;22)(q24;q12) translocation that generates the Ewing sarcoma breakpoint region 1 and Friend leukemia virus integration 1 (EWS-FLI1) fusion transcription factor responsible for the highly malignant phenotype of this tumor. Although continued expression of EWS-FLI1 is believed to be critical for ESFT cell survival, a clinically effective small-molecule inhibitor remains elusive likely because EWS-FLI1 is a transcription factor and therefore widely felt to be “undruggable.” METHODS: We developed a high throughput screen to evaluate more than 50 000 compounds for inhibition of EWS-FLI1 activity in TC32 ESFT cells. We used a TC32 cell-based luciferase reporter screen using the EWS-FLI1 downstream target NR0B1 promoter and a gene signature secondary screen to sort and prioritize the compounds. We characterized the lead compound, mithramycin, based on its ability to inhibit EWS-FLI1 activity in vitro using microarray expression profiling, quantitative reverse transcription-polymerase chain reaction, and immunoblot analysis, and in vivo using immunohistochemistry. We studied the impact of this inhibition on cell viability in vitro and on tumor growth in ESFT xenograft models in vivo (n = 15-20 mice per group). All statistical tests were two-sided. RESULTS: Mithramycin inhibited expression of EWS-FLI1 downstream targets at the mRNA and protein levels and decreased the growth of ESFT cells at half maximal inhibitory concentrations between 10 (95% confidence interval [CI] = 8 to 13 nM) and 15 nM (95% CI = 13 to 19 nM). Mithramycin suppressed the growth of two different ESFT xenograft tumors and prolonged the survival of ESFT xenograft-bearing mice by causing a decrease in mean tumor volume. For example, in the TC32 xenograft model, on day 15 of treatment, the mean tumor volume for the mithramycin-treated mice was approximately 3% of the tumor volume observed in the control mice (mithramycin vs control: 69 vs 2388 mm(3), difference = 2319 mm(3), 95% CI = 1766 to 2872 mm(3), P < .001). CONCLUSION: Mithramycin inhibits EWS-FLI1 activity and demonstrates ESFT antitumor activity both in vitro and in vivo.
Lombo F, Menendez N, Salas JA, Mendez C. The aureolic acid family of antitumor compounds: structure, mode of action, biosynthesis, and novel derivatives. Appl Microbiol Biotechnol. 2006;73(1):1–14. https://doi.org/10.1007/s00253-006-0511-6.
• Grohar PJ, Glod J, Peer CJ, Sissung TM, Arnaldez FI, Long L, et al. A phase I/II trial and pharmacokinetic study of mithramycin in children and adults with refractory Ewing sarcoma and EWS-FLI1 fusion transcript. Cancer Chemother Pharmacol. 2017;80(3):645–52. https://doi.org/10.1007/s00280-017-3382-x. PURPOSE: In a preclinical drug screen, mithramycin was identified as a potent inhibitor of the Ewing sarcoma EWS-FLI1 transcription factor. We conducted a phase I/II trial to determine the dose-limiting toxicities (DLT), maximum tolerated dose (MTD), and pharmacokinetics (PK) of mithramycin in children with refractory solid tumors, and the activity in children and adults with refractory Ewing sarcoma. PATIENTS AND METHODS: Mithramycin was administered intravenously over 6 h once daily for 7 days for 28 day cycles. Adult patients (phase II) initially received mithramycin at the previously determined recommended dose of 25 microg/kg/dose. The planned starting dose for children (phase I) was 17.5 microg/kg/dose. Plasma samples were obtained for mithramycin PK analysis. RESULTS: The first two adult patients experienced reversible grade 4 alanine aminotransferase (ALT)/aspartate aminotransferase (AST) elevation exceeding the MTD. Subsequent adult patients received mithramycin at 17.5 microg/kg/dose, and children at 13 microg/kg/dose with dexamethasone pretreatment. None of the four subsequent adult and two pediatric patients experienced cycle 1 DLT. No clinical responses were observed. The average maximal mithramycin plasma concentration in four patients was 17.8 +/- 4.6 ng/mL. This is substantially below the sustained mithramycin concentrations >/=50 nmol/L required to suppress EWS-FLI1 transcriptional activity in preclinical studies. Due to inability to safely achieve the desired mithramycin exposure, the trial was closed to enrollment. CONCLUSIONS: Hepatotoxicity precluded the administration of a mithramycin at a dose required to inhibit EWS-FLI1. Evaluation of mithramycin in patients selected for decreased susceptibility to elevated transaminases may allow for improved drug exposure.
Sleiman SF, Langley BC, Basso M, Berlin J, Xia L, Payappilly JB, et al. Mithramycin is a gene-selective Sp1 inhibitor that identifies a biological intersection between cancer and neurodegeneration. J Neurosci. 2011;31(18):6858–70. https://doi.org/10.1523/JNEUROSCI.0710-11.2011.
Chatterjee S, Zaman K, Ryu H, Conforto A, Ratan RR. Sequence-selective DNA binding drugs mithramycin a and chromomycin A3 are potent inhibitors of neuronal apoptosis induced by oxidative stress and DNA damage in cortical neurons. Ann Neurol. 2001;49(3):345–54.
• Scott D, Chen JM, Bae Y, Rohr J. Semi-synthetic mithramycin SA derivatives with improved anticancer activity. Chem Biol Drug Des. 2013;81(5):615–24.. Mithramycin (MTM) is a potent anti-cancer agent that has recently garnered renewed attention. This manuscript describes the design and development of mithramycin derivatives through a combinational approach of biosynthetic analogue generation followed by synthetic manipulation for further derivatization. Mithramycin SA is a previously discovered analogue produced by the M7W1 mutant strain alongside the improved mithramycin analogues mithramycin SK and mithramycin SDK. Mithramycin SA shows decreased anti-cancer activity compared to mithramycin and has a shorter, two carbon aglycon side chain that is terminated in a carboxylic acid. The aglycon side chain is responsible for an interaction with the DNA phosphate backbone as mithramycin interacts with its target DNA. It was therefore decided to further functionalize this side chain through reactions with the terminal carboxylic acid in an effort to enhance the interaction with the DNA phosphate backbone and improve the anticancer activity. This side chain was modified with a variety of molecules increasing the anticancer activity to a comparable level to mithramycin SK. This work shows the ability to transform the previously useless mithramycin SA into a valuable molecule and opens the door to further functionalization and semi-synthetic modification for the development of molecules with increased specificity and/or drug formulation.
• Hou C, Weidenbach S, Cano KE, Wang Z, Mitra P, Ivanov DN, et al. Structures of mithramycin analogues bound to DNA and implications for targeting transcription factor FLI1. Nucleic Acids Res. 2016;44(18):8990–9004. https://doi.org/10.1093/nar/gkw761. Transcription factors have been considered undruggable, but this paradigm has been recently challenged. DNA binding natural product mithramycin (MTM) is a potent antagonist of oncogenic transcription factor EWS-FLI1. Structural details of MTM recognition of DNA, including the FLI1 binding sequence GGA(A/T), are needed to understand how MTM interferes with EWS-FLI1. We report a crystal structure of an MTM analogue MTM SA-Trp bound to a DNA oligomer containing a site GGCC, and two structures of a novel analogue MTM SA-Phe in complex with DNA. MTM SA-Phe is bound to sites AGGG and GGGT on one DNA, and to AGGG and GGGA(T) (a FLI1 binding site) on the other, revealing how MTM recognizes different DNA sequences. Unexpectedly, at sub-micromolar concentrations MTMs stabilize FLI1-DNA complex on GGAA repeats, which are critical for the oncogenic function of EWS-FLI1. We also directly demonstrate by nuclear magnetic resonance formation of a ternary FLI1-DNA-MTM complex on a single GGAA FLI1/MTM binding site. These biochemical and structural data and a new FLI1-DNA structure suggest that MTM binds the minor groove and perturbs FLI1 bound nearby in the major groove. This ternary complex model may lead to development of novel MTM analogues that selectively target EWS-FLI1 or other oncogenic transcription factors, as anti-cancer therapeutics.
• Hou C, Rohr J, Parkin S, Tsodikov OV. How mithramycin stereochemistry dictates its structure and DNA binding function. MedChemComm. 2019;10(5):735–41. https://doi.org/10.1039/c9md00100j. An aureolic acid natural product mithramycin (MTM) has been known for its potent antineoplastic properties. MTM inhibits cell growth by binding in the minor groove of double stranded DNA as a dimer, in which the two molecules of MTM are coordinated to each other through a divalent metal ion. A crystal structure of an MTM analogue, MTM SA-Phe, in the active metal ion-coordinated dimeric form demonstrates how the stereochemical features of MTM define the helicity of the dimeric scaffold for its binding to a right-handed DNA double helix. We also show crystallographically and biochemically that MTM, but not MTM SA-Phe, can be inactivated by boric acid through formation of a large macrocyclic species, in which two molecules of MTM are crosslinked to each other through 3-side chain-boron-sugar intermolecular bonds. We discuss these structural and biochemical properties in the context of MTM biosynthesis and the design of MTM analogues as anticancer therapeutics.
• Mitra P, Eckenrode JM, Mandal A, Jha AK, Salem SM, Leggas M, et al. Development of mithramycin analogues with increased selectivity toward ETS transcription factor expressing cancers. J Med Chem. 2018;61(17):8001–16. Mithramycin A (1) was identified as the top potential inhibitor of the aberrant ETS transcription factor EWS-FLI1, which causes Ewing sarcoma. Unfortunately, 1 has a narrow therapeutic window, compelling us to seek less toxic and more selective analogues. Here, we used MTMSA (2) to generate analogues via peptide coupling and fragment-based drug development strategies. Cytotoxicity assays in ETS and non-ETS dependent cell lines identified two dipeptide analogues, 60 and 61, with 19.1- and 15.6-fold selectivity, respectively, compared to 1.5-fold for 1. Importantly, the cytotoxicity of 60 and 61 is <100 nM in ETS cells. Molecular assays demonstrated the inhibitory capacity of these analogues against EWS-FLI1 mediated transcription in Ewing sarcoma. Structural analysis shows that positioning the tryptophan residue in a distal position improves selectivity, presumably via interaction with the ETS transcription factor. Thus, these analogues may present new ways to target transcription factors for clinical use.
Martinez EJ, Corey EJ. A new, more efficient, and effective process for the synthesis of a key pentacyclic intermediate for production of ecteinascidin and phthalascidin antitumor agents. Org Lett. 2000;2(7):993–6.
Pommier Y, Kohlhagen G, Bailly C, Waring M, Mazumder A, Kohn KW. DNA sequence- and structure-selective alkylation of guanine N2 in the DNA minor groove by ecteinascidin 743, a potent antitumor compound from the Caribbean tunicate Ecteinascidia turbinata. Biochemistry. 1996;35(41):13303–9. https://doi.org/10.1021/bi960306b.
Takebayashi Y, Pourquier P, Zimonjic DB, Nakayama K, Emmert S, Ueda T, et al. Antiproliferative activity of ecteinascidin 743 is dependent upon transcription-coupled nucleotide-excision repair. Nat Med. 2001;7(8):961–6. https://doi.org/10.1038/91008.
Demetri GD, Chawla SP, von Mehren M, Ritch P, Baker LH, Blay JY, et al. Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: results of a randomized phase II study of two different schedules. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2009;27(25):4188–96. https://doi.org/10.1200/jco.2008.21.0088.
Taamma A, Misset JL, Riofrio M, Guzman C, Brain E, Lopez Lazaro L, et al. Phase I and pharmacokinetic study of ecteinascidin-743, a new marine compound, administered as a 24-hour continuous infusion in patients with solid tumors. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2001;19(5):1256–65. https://doi.org/10.1200/jco.2001.19.5.1256.
Scotlandi K, Perdichizzi S, Manara MC, Serra M, Benini S, Cerisano V, et al. Effectiveness of Ecteinascidin-743 against drug-sensitive and -resistant bone tumor cells. Clin Cancer Res : an official journal of the American Association for Cancer Research. 2002;8(12):3893–903.
Aune GJ, Takagi K, Sordet O, Guirouilh-Barbat J, Antony S, Bohr VA, et al. Von Hippel-Lindau-coupled and transcription-coupled nucleotide excision repair-dependent degradation of RNA polymerase II in response to trabectedin. Clin Cancer Res : an official journal of the American Association for Cancer Research. 2008;14(20):6449–55. https://doi.org/10.1158/1078-0432.Ccr-08-0730.
• Grohar PJ, Griffin LB, Yeung C, Chen QR, Pommier Y, Khanna C, et al. Ecteinascidin 743 interferes with the activity of EWS-FLI1 in Ewing sarcoma cells. Neoplasia (New York, NY). 2011;13(2):145–53. ET-743 (trabectedin; Yondelis) is approved in Europe for the treatment of soft tissue sarcomas. Emerging phase 1 and 2 clinical data have shown high response rates in myxoid liposarcoma in part owing to the inhibition of the FUS-CHOP transcription factor. In this report, we show that modulation of specific oncogenic transcription factors by ET-743 may extend to other tumor types. We demonstrate that, among a panel of pediatric sarcomas, Ewing sarcoma family of tumors (ESFTs) cell lines bearing the EWS-FLI1 transcription factor are the most sensitive to treatment with ET-743 compared with osteosarcoma, rhabdomyosarcoma, and synovial sarcoma. We show that ET-743 reverses a gene signature of induced downstream targets of EWS-FLI1 in two different ESFT cell lines (P = .001). In addition, ET-743 directly suppresses the promoter activity of a known EWS-FLI1 downstream target NR0B1 luciferase reporter construct without changing the activity of a constitutively active control in ESFT cells. Furthermore, the effect is specific to EWS-FLI1, as forced expression of EWS-FLI1 in a cell type that normally lacks this fusion protein, HT1080 cells, induces the same NR0B1 promoter, but this activation is completely blocked by ET-743 treatment. Finally, we used gene set enrichment analysis to confirm that other mechanisms of ET-743 are active in ESFT cells. These results suggest a particular role for ET-743 in the treatment of translocation-positive tumors. In addition, the modulation of EWS-FLI1 makes it a novel targeting agent for ESFT and suggests that further development of this compound for the treatment of ESFT is warranted.
• Chuk MK, Aikin A, Whitcomb T, Widemann BC, Zannikos P, Bayever E, et al. A phase I trial and pharmacokinetic study of a 24-hour infusion of trabectedin (Yondelis(R), ET-743) in children and adolescents with relapsed or refractory solid tumors. Pediatr Blood Cancer. 2012;59(5):865–9. BACKGROUND: The objectives of this phase I study were to determine the maximum tolerated dose (MTD), toxicity profile, and pharmacokinetics of a 24-hour continuous intravenous infusion of trabectedin administered to children and adolescents with refractory or relapsed solid tumors. PROCEDURE: Patients between the ages of 4 and 16 years old with refractory solid tumors received trabectedin as a 24-hour infusion every 21 days. Dexamethasone and prophylactic growth factor support were administered with each cycle. Pharmacokinetic studies were conducted during cycle 1. RESULTS: Patients (n = 12) median (range) age 14.5 (8-16) years received trabectedin at 1.1 (n = 3), 1.5 (n = 6), or 1.7 (n = 3) mg/m(2). At the 1.5 mg/m(2) dose level, one patient had dose limiting anorexia and fatigue. At 1.7 mg/m(2), two patients experienced dose limiting toxicity, dehydration, and gamma glutamyl transpeptidase elevation. Non-dose limiting toxicities included elevated serum transaminases, myelosuppression, nausea, emesis, and fatigue. Plasma pharmacokinetic parameters were similar to historical data in adults. One partial response was observed in a patient with neuroendocrine carcinoma. Stable disease (>/=6 cycles) was achieved in three patients (osteosarcoma n = 2, desmoplastic small round cell tumor n = 1). CONCLUSIONS: The MTD of trabectedin in pediatric patients with refractory solid tumors is 1.5 mg/m(2) IV over 24 hours every 21 days. Dexamethasone to ameliorate hepatic toxicity and prophylactic growth factor support are required.
• Harlow ML, Maloney N, Roland J, Guillen Navarro MJ, Easton MK, Kitchen-Goosen SM, et al. Lurbinectedin inactivates the Ewing sarcoma oncoprotein EWS-FLI1 by redistributing it within the nucleus. Cancer Res. 2016;76(22):6657–68. There is a great need to develop novel approaches to target oncogenic transcription factors with small molecules. Ewing sarcoma is emblematic of this need, as it depends on the continued activity of the EWS-FLI1 transcription factor to maintain the malignant phenotype. We have previously shown that the small molecule trabectedin interferes with EWS-FLI1. Here, we report important mechanistic advances and a second-generation inhibitor to provide insight into the therapeutic targeting of EWS-FLI1. We discovered that trabectedin functionally inactivated EWSFLI1 by redistributing the protein within the nucleus to the nucleolus. This effect was rooted in the wild-type functions of the EWSR1, compromising the N-terminal half of the chimeric oncoprotein, which is known to be similarly redistributed within the nucleus in the presence of UV light damage. A second-generation trabectedin analogue lurbinectedin (PM01183) caused the same nuclear redistribution of EWS-FLI1, leading to a loss of activity at the promoter, mRNA, and protein levels of expression. Tumor xenograft studies confirmed this effect, and it was increased in combination with irinotecan, leading to tumor regression and replacement of Ewing sarcoma cells with benign fat cells. The net result of combined lurbinectedin and irinotecan treatment was a complete reversal of EWS-FLI1 activity and elimination of established tumors in 30% to 70% of mice after only 11 days of therapy. Our results illustrate the preclinical safety and efficacy of a disease-specific therapy targeting the central oncogenic driver in Ewing sarcoma. Cancer Res; 76(22); 6657-68. (c)2016 AACR.
• Clinical Trial of Lurbinectedin (PM01183) in Selected Advanced Solid Tumors. https://ClinicalTrials.gov/show/NCT02454972.
• Theisen ER, Pishas KI, Saund RS, Lessnick SL. Therapeutic opportunities in Ewing sarcoma: EWS-FLI inhibition via LSD1 targeting. Oncotarget. 2016;7(14):17616–30. https://doi.org/10.18632/oncotarget.7124. Ewing sarcoma is an aggressive primary pediatric bone tumor, often diagnosed in adolescents and young adults. A pathognomonic reciprocal chromosomal translocation results in a fusion gene coding for a protein which derives its N-terminus from a FUS/EWS/TAF15 (FET) protein family member, commonly EWS, and C-terminus containing the DNA-binding domain of an ETS transcription factor, commonly FLI1. Nearly 85% of cases express the EWS-FLI protein which functions as a transcription factor and drives oncogenesis. As the primary genomic lesion and a protein which is not expressed in normal cells, disrupting EWS-FLI function is an attractive therapeutic strategy for Ewing sarcoma. However, transcription factors are notoriously difficult targets for the development of small molecules. Improved understanding of the oncogenic mechanisms employed by EWS-FLI to hijack normal cellular programming has uncovered potential novel approaches to pharmacologically block EWS-FLI function. In this review we examine targeting the chromatin regulatory enzymes recruited to conspire in oncogenesis with a focus on the histone lysine specific demethylase 1 (LSD1). LSD1 inhibitors are being aggressively investigated in acute myeloid leukemia and the results of early clinical trials will help inform the future use of LSD1 inhibitors in sarcoma. High LSD1 expression is observed in Ewing sarcoma patient samples and mechanistic and preclinical data suggest LSD1 inhibition globally disrupts the function of EWS-ETS proteins.
Brohl AS, Solomon DA, Chang W, Wang J, Song Y, Sindiri S, et al. The genomic landscape of the Ewing sarcoma family of tumors reveals recurrent STAG2 mutation. PLoS Genet. 2014;10(7):e1004475. https://doi.org/10.1371/journal.pgen.1004475.
• Crompton BD, Stewart C, Taylor-Weiner A, Alexe G, Kurek KC, Calicchio ML, et al. The genomic landscape of pediatric Ewing sarcoma. Cancer Discov. 2014;4(11):1326–41. https://doi.org/10.1158/2159-8290.cd-13-1037. UNLABELLED: Pediatric Ewing sarcoma is characterized by the expression of chimeric fusions of EWS and ETS family transcription factors, representing a paradigm for studying cancers driven by transcription factor rearrangements. In this study, we describe the somatic landscape of pediatric Ewing sarcoma. These tumors are among the most genetically normal cancers characterized to date, with only EWS-ETS rearrangements identified in the majority of tumors. STAG2 loss, however, is present in more than 15% of Ewing sarcoma tumors; occurs by point mutation, rearrangement, and likely nongenetic mechanisms; and is associated with disease dissemination. Perhaps the most striking finding is the paucity of mutations in immediately targetable signal transduction pathways, highlighting the need for new therapeutic approaches to target EWS-ETS fusions in this disease. SIGNIFICANCE: We performed next-generation sequencing of Ewing sarcoma, a pediatric cancer involving bone, characterized by expression of EWS-ETS fusions. We found remarkably few mutations. However, we discovered that loss of STAG2 expression occurs in 15% of tumors and is associated with metastatic disease, suggesting a potential genetic vulnerability in Ewing sarcoma.
Shi Y, Lan F, Matson C, Mulligan P, Whetstine JR, Cole PA, et al. Histone demethylation mediated by the nuclear amine oxidase homolog LSD1. Cell. 2004;119(7):941–53. https://doi.org/10.1016/j.cell.2004.12.012.
Lim S, Janzer A, Becker A, Zimmer A, Schüle R, Buettner R, et al. Lysine-specific demethylase 1 (LSD1) is highly expressed in ER-negative breast cancers and a biomarker predicting aggressive biology. Carcinogenesis. 2009;31(3):512–20. https://doi.org/10.1093/carcin/bgp324.
Kahl P, Gullotti L, Heukamp LC, Wolf S, Friedrichs N, Vorreuther R, et al. Androgen receptor coactivators lysine-specific histone demethylase 1 and four and a half LIM domain protein 2 predict risk of prostate cancer recurrence. Cancer Res. 2006;66(23):11341–7. https://doi.org/10.1158/0008-5472.Can-06-1570.
Hayami S, Kelly JD, Cho HS, Yoshimatsu M, Unoki M, Tsunoda T, et al. Overexpression of LSD1 contributes to human carcinogenesis through chromatin regulation in various cancers. Int J Cancer. 2011;128(3):574–86. https://doi.org/10.1002/ijc.25349.
Schulte JH, Lim S, Schramm A, Friedrichs N, Koster J, Versteeg R, et al. Lysine-specific demethylase 1 is strongly expressed in poorly differentiated neuroblastoma: implications for therapy. Cancer Res. 2009;69(5):2065–71. https://doi.org/10.1158/0008-5472.Can-08-1735.
Harris WJ, Huang X, Lynch JT, Spencer GJ, Hitchin JR, Li Y, et al. The histone demethylase KDM1A sustains the oncogenic potential of MLL-AF9 leukemia stem cells. Cancer Cell. 2012;21(4):473–87. https://doi.org/10.1016/j.ccr.2012.03.014.
Zhao ZK, Yu HF, Wang DR, Dong P, Chen L, Wu WG, et al. Overexpression of lysine specific demethylase 1 predicts worse prognosis in primary hepatocellular carcinoma patients. World J Gastroenterol. 2012;18(45):6651–6. https://doi.org/10.3748/wjg.v18.i45.6651.
• Bennani-Baiti IM, Machado I, Llombart-Bosch A, Kovar H. Lysine-specific demethylase 1 (LSD1/KDM1A/AOF2/BHC110) is expressed and is an epigenetic drug target in chondrosarcoma, Ewing’s sarcoma, osteosarcoma, and rhabdomyosarcoma. Hum Pathol. 2012;43(8):1300–7. https://doi.org/10.1016/j.humpath.2011.10.010. Lysine-specific demethylase 1 (GeneID 23028), a flavin-dependent monoamine oxidoreductase and a histone demethylase, serves as an epigenetic coregulator of transcription. Lysine-specific demethylase 1 is up-regulated in neuroblastoma and in bladder, breast, colorectal, gastric, lung, and neuroendocrine cancers, and its overexpression drives the cell cycle of otherwise nontransformed human cells, suggesting oncogenic properties. Lysine-specific demethylase 1 was recently reported to be also overexpressed in several different mesenchymal tumors. We investigated lysine-specific demethylase 1 expression in over 500 sarcomas by gene expression profiling and tissue microarray-coupled immunohistochemical analyses and confirmed lysinespecific demethylase 1 overexpression in rhabdomyosarcoma and synovial sarcoma. We also show for the first time that lysine-specific demethylase 1 is also overexpressed in chondrosarcoma, Ewing's sarcoma, and osteosarcoma wherein it localizes in cell nuclei. We further show that a US Food and Drug Administration-approved drug that inhibits lysine-specific demethylase 1 also inhibits chondrosarcoma, Ewing's sarcoma, osteosarcoma, and rhabdomyosarcoma cell growth in vitro. These data suggest that lysine-specific demethylase 1 plays a role in sarcoma pathology and that lysine-specific demethylase 1 inhibition strategies might represent a novel means to inhibiting growth of lysine-specific demethylase 1-overexpressing sarcomas.
Schildhaus HU, Riegel R, Hartmann W, Steiner S, Wardelmann E, Merkelbach-Bruse S, et al. Lysine-specific demethylase 1 is highly expressed in solitary fibrous tumors, synovial sarcomas, rhabdomyosarcomas, desmoplastic small round cell tumors, and malignant peripheral nerve sheath tumors. Hum Pathol. 2011;42(11):1667–75. https://doi.org/10.1016/j.humpath.2010.12.025.
Cho HS, Suzuki T, Dohmae N, Hayami S, Unoki M, Yoshimatsu M, et al. Demethylation of RB regulator MYPT1 by histone demethylase LSD1 promotes cell cycle progression in cancer cells. Cancer Res. 2011;71(3):655–60. https://doi.org/10.1158/0008-5472.Can-10-2446.
Lv S, Bu W, Jiao H, Liu B, Zhu L, Zhao H, et al. LSD1 is required for chromosome segregation during mitosis. Eur J Cell Biol. 2010;89(7):557–63. https://doi.org/10.1016/j.ejcb.2010.01.004.
Schooley A, Moreno-Andres D, De Magistris P, Vollmer B, Antonin W. The lysine demethylase LSD1 is required for nuclear envelope formation at the end of mitosis. J Cell Sci. 2015;128(18):3466–77. https://doi.org/10.1242/jcs.173013.
Frieling H, Bleich S. Tranylcypromine: new perspectives on an "old" drug. Eur Arch Psychiatry Clin Neurosci. 2006;256(5):268–73. https://doi.org/10.1007/s00406-006-0660-8.
• Sankar S, Theisen ER, Bearss J, Mulvihill T, Hoffman LM, Sorna V, et al. Reversible LSD1 inhibition interferes with global EWS/ETS transcriptional activity and impedes Ewing sarcoma tumor growth. Clin Cancer Res : an official journal of the American Association for Cancer Research. 2014;20(17):4584–97. PURPOSE: Ewing sarcoma is a pediatric bone tumor that absolutely relies on the transcriptional activity of the EWS/ETS family of fusion oncoproteins. While the most common fusion, EWS/FLI, utilizes lysine-specific demethylase 1 (LSD1) to repress critical tumor suppressors, small molecule blockade of LSD1 has not yet been thoroughly explored as a therapeutic approach for Ewing sarcoma. We therefore evaluated the translational potential of potent and specific LSD1 inhibition with HCI2509 on the transcriptional program of both EWS/FLI and EWS/ERG as well as the downstream oncogenic phenotypes driven by EWS/ETS fusions in both in vitro and in vivo models of Ewing sarcoma. EXPERIMENTAL DESIGN: RNA-seq was used to compare the transcriptional profiles of EWS/FLI, EWS/ERG, and treatment with HCI2509 in both EWS/FLI- and EWS/ERG-containing cell lines. We then evaluated morphologic phenotypes of treated cells with immunofluorescence. The induction of apoptosis was evaluated using caspase-3/7 activation and TUNEL staining. Colony forming assays were used to test oncogenic transformation and xenograft studies with patient-derived cell lines were used to evaluate the effects of HCI2509 on tumorigenesis. RESULTS: HCI2509 caused a dramatic reversal of both the up- and downregulated transcriptional profiles of EWS/FLI and EWS/ERG accompanied by the induction of apoptosis and disruption of morphologic and oncogenic phenotypes modulated by EWS/FLI. Importantly, HCI2509 displayed single-agent efficacy in multiple xenograft models. CONCLUSIONS: These data support epigenetic modulation with HCI2509 as a therapeutic strategy for Ewing sarcoma, and highlight a critical dual role for LSD1 in the oncogenic transcriptional activity of EWS/ETS proteins.
Clinical Trial of SP-2577 (Seclidemstat) in Patients With Relapsed or Refractory Ewing Sarcoma. https://ClinicalTrials.gov/show/NCT03600649.
Christensen Camilla L, Kwiatkowski N, Abraham Brian J, Carretero J, Al-Shahrour F, Zhang T, et al. Targeting transcriptional addictions in small cell lung cancer with a covalent CDK7 inhibitor. Cancer Cell. 2014;26(6):909–22. https://doi.org/10.1016/j.ccell.2014.10.019.
Chila R, Guffanti F, Damia G. Role and therapeutic potential of CDK12 in human cancers. Cancer Treat Rev. 2016;50:83–8. https://doi.org/10.1016/j.ctrv.2016.09.003.
Kwiatkowski N, Zhang T, Rahl PB, Abraham BJ, Reddy J, Ficarro SB, et al. Targeting transcription regulation in cancer with a covalent CDK7 inhibitor. Nature. 2014;511(7511):616–20. https://doi.org/10.1038/nature13393.
• Iniguez AB, Stolte B, Wang EJ, Conway AS, Alexe G, Dharia NV, et al. EWS/FLI confers tumor cell synthetic lethality to CDK12 inhibition in Ewing sarcoma. Cancer Cell. 2018;33(2):202–16.e6. Many cancer types are driven by oncogenic transcription factors that have been difficult to drug. Transcriptional inhibitors, however, may offer inroads into targeting these cancers. Through chemical genomics screening, we identified that Ewing sarcoma is a disease with preferential sensitivity to THZ1, a covalent small-molecule CDK7/12/13 inhibitor. The selective CDK12/13 inhibitor, THZ531, impairs DNA damage repair in an EWS/FLI-dependent manner, supporting a synthetic lethal relationship between response to THZ1/THZ531 and EWS/FLI expression. The combination of these molecules with PARP inhibitors showed striking synergy in cell viability and DNA damage assays in vitro and in multiple models of Ewing sarcoma, including a PDX, in vivo without hematopoietic toxicity.
• Blazek D, Kohoutek J, Bartholomeeusen K, Johansen E, Hulinkova P, Luo Z, et al. The Cyclin K/Cdk12 complex maintains genomic stability via regulation of expression of DNA damage response genes. Genes Dev. 2011;25(20):2158–72. https://doi.org/10.1101/gad.16962311. Various cyclin-dependent kinase (Cdk) complexes have been implicated in the regulation of transcription. In this study, we identified a 70-kDa Cyclin K (CycK) that binds Cdk12 and Cdk13 to form two different complexes (CycK/Cdk12 or CycK/Cdk13) in human cells. The CycK/Cdk12 complex regulates phosphorylation of Ser2 in the C-terminal domain of RNA polymerase II and expression of a small subset of human genes, as revealed in expression microarrays. Depletion of CycK/Cdk12 results in decreased expression of predominantly long genes with high numbers of exons. The most prominent group of down-regulated genes are the DNA damage response genes, including the critical regulators of genomic stability: BRCA1 (breast and ovarian cancer type 1 susceptibility protein 1), ATR (ataxia telangiectasia and Rad3-related), FANCI, and FANCD2. We show that CycK/Cdk12, rather than CycK/Cdk13, is necessary for their expression. Nuclear run-on assays and chromatin immunoprecipitations with RNA polymerase II on the BRCA1 and FANCI genes suggest a transcriptional defect in the absence of CycK/Cdk12. Consistent with these findings, cells without CycK/Cdk12 induce spontaneous DNA damage and are sensitive to a variety of DNA damage agents. We conclude that through regulation of expression of DNA damage response genes, CycK/Cdk12 protects cells from genomic instability. The essential role of CycK for organisms in vivo is further supported by the result that genetic inactivation of CycK in mice causes early embryonic lethality.
• Gill SJ, Travers J, Pshenichnaya I, Kogera FA, Barthorpe S, Mironenko T, et al. Combinations of PARP inhibitors with temozolomide drive PARP1 trapping and apoptosis in Ewing’s sarcoma. PLoS One. 2015;10(10):e0140988. Ewing’s sarcoma is a malignant pediatric bone tumor with a poor prognosis for patients with metastatic or recurrent disease. Ewing's sarcoma cells are acutely hypersensitive to poly (ADPribose) polymerase (PARP) inhibition and this is being evaluated in clinical trials, although the mechanism of hypersensitivity has not been directly addressed. PARP inhibitors have efficacy in tumors with BRCA1/2 mutations, which confer deficiency in DNA double-strand break (DSB) repair by homologous recombination (HR). This drives dependence on PARP1/2 due to their function in DNA single-strand break (SSB) repair. PARP inhibitors are also cytotoxic through inhibiting PARP1/2 auto-PARylation, blocking PARP1/2 release from substrate DNA. Here, we show that PARP inhibitor sensitivity in Ewing's sarcoma cells is not through an apparent defect in DNA repair by HR, but through hypersensitivity to trapped PARP1-DNA complexes. This drives accumulation of DNA damage during replication, ultimately leading to apoptosis. We also show that the activity of PARP inhibitors is potentiated by temozolomide in Ewing's sarcoma cells and is associated with enhanced trapping of PARP1-DNA complexes. Furthermore, through mining of large-scale drug sensitivity datasets, we identify a subset of glioma, neuroblastoma and melanoma cell lines as hypersensitive to the combination of temozolomide and PARP inhibition, potentially identifying new avenues for therapeutic intervention. These data provide insights into the anti-cancer activity of PARP inhibitors with implications for the design of treatment for Ewing's sarcoma patients with PARP inhibitors.
Sand LG, Szuhai K, Hogendoorn PC. Sequencing overview of Ewing sarcoma: a journey across genomic, epigenomic and transcriptomic landscapes. Int J Mol Sci. 2015;16(7):16176–215. https://doi.org/10.3390/ijms160716176.
• Huang HY, Illei PB, Zhao Z, Mazumdar M, Huvos AG, Healey JH, et al. Ewing sarcomas with p53 mutation or p16/p14ARF homozygous deletion: a highly lethal subset associated with poor chemoresponse. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2005;23(3):548–58. https://doi.org/10.1200/jco.2005.02.081. PURPOSE: EWS-FLI1 fusion type, p53 mutation, and homozygous deletion of p16/p14ARF have each been shown to be prognostically significant in Ewing sarcoma (ES). We provide the first combined prognostic analysis of these three molecular parameters in ES. PATIENTS AND METHODS: We studied 60 patients with ES (stage: localized in 54, metastatic in six). All cases were confirmed to contain the EWS-FLI1 (29 type 1, 12 type 2, 14 other types) or EWS-ERG fusions (five cases). Homozygous deletion of p16/p14ARF, and p53 mutations were determined by fluorescent in situ hybridization and Affymetrix (Santa Clara, CA) p53 GeneChip microarray hybridization, respectively. RESULTS: Eight cases (13.3%) contained point mutations of p53, and eight cases (13.3%) showed p16/p14ARF deletion, including one case with both alterations. Among 32 cases with data on histologic chemoresponse, all 10 with alterations in p53 or p16/p14ARF showed a poor chemoresponse (P = .03). Variables predicting poorer overall survival included p53 mutation alone (P < .001), either p53 or p16/p14ARF alteration (P < .001), and stage (P < .01). In multivariate analysis, alterations of p53 and/or p16/p14ARF as a single variable, was the most adverse prognostic factor (P < .001), followed by stage (P = .04). In a multivariate analysis with alterations of p53 and p16/p14ARF as separate variables, both were significant (P < .001 and P = .03, respectively). Six cases with p16/p14ARF deletion were also studied for co-deletion of the contiguous methylthioadenosine phosphorylase gene, and this was detected in four cases. CONCLUSION: Alterations in p53 or p16/p14ARF are found in a fourth of ES cases and define a subset with highly aggressive behavior and poor chemoresponse.
Serrano M, Hannon GJ, Beach D. A new regulatory motif in cell-cycle control causing specific inhibition of cyclin D/CDK4. Nature. 1993;366(6456):704–7. https://doi.org/10.1038/366704a0.
• Kennedy AL, Vallurupalli M, Chen L, Crompton B, Cowley G, Vazquez F, et al. Functional, chemical genomic, and super-enhancer screening identify sensitivity to cyclin D1/CDK4 pathway inhibition in Ewing sarcoma. Oncotarget. 2015;6(30):30178–93. https://doi.org/10.18632/oncotarget.4903. Ewing sarcoma is an aggressive bone and soft tissue tumor in children and adolescents, with treatment remaining a clinical challenge. This disease is mediated by somatic chromosomal translocations of the EWS gene and a gene encoding an ETS transcription factor, most commonly, FLI1. While direct targeting of aberrant transcription factors remains a pharmacological challenge, identification of dependencies incurred by EWS/FLI1 expression would offer a new therapeutic avenue. We used a combination of super-enhancer profiling, near-whole genome shRNA-based and smallmolecule screening to identify cyclin D1 and CDK4 as Ewing sarcoma-selective dependencies. We revealed that super-enhancers mark Ewing sarcoma specific expression signatures and EWS/FLI1 target genes in human Ewing sarcoma cell lines. Particularly, a super-enhancer regulates cyclin D1 and promotes its expression in Ewing sarcoma. We demonstrated that Ewing sarcoma cells require CDK4 and cyclin D1 for survival and anchorage-independent growth. Additionally, pharmacologic inhibition of CDK4 with selective CDK4/6 inhibitors led to cytostasis and cell death of Ewing sarcoma cell lines in vitro and growth delay in an in vivo Ewing sarcoma xenograft model. These results demonstrated a dependency in Ewing sarcoma on CDK4 and cyclin D1 and support exploration of CDK4/6 inhibitors as a therapeutic approach for patients with this disease.
Abemaciclib in children with DIPG or recurrent/refractory solid tumors. https://ClinicalTrials.gov/show/NCT02644460.
Geoerger B, Bourdeaut F, DuBois SG, Fischer M, Geller JI, Gottardo NG, et al. A phase I study of the CDK4/6 inhibitor Ribociclib (LEE011) in pediatric patients with malignant rhabdoid tumors, neuroblastoma, and other solid tumors. Clin Cancer Res : an official journal of the American Association for Cancer Research. 2017;23(10):2433–41. https://doi.org/10.1158/1078-0432.CCR-16-2898.
Study Of Palbociclib Combined With Chemotherapy In Pediatric Patients With Recurrent/Refractory Solid Tumors.
Ribociclib and Everolimus in Treating Children With Recurrent or Refractory Malignant Brain Tumors. https://ClinicalTrials.gov/show/NCT03387020.
Kolb EA, Gorlick R, Reynolds CP, Kang MH, Carol H, Lock R, et al. Initial testing (stage 1) of eribulin, a novel tubulin binding agent, by the pediatric preclinical testing program. Pediatr Blood Cancer. 2013;60(8):1325–32. https://doi.org/10.1002/pbc.24517.
Kim MY, Zhang T, Kraus WL. Poly (ADP-ribosyl) ation by PARP-1: 'PAR-laying' NAD+ into a nuclear signal. Genes Dev. 2005;19(17):1951–67. https://doi.org/10.1101/gad.1331805.
Krishnakumar R, Gamble MJ, Frizzell KM, Berrocal JG, Kininis M, Kraus WL. Reciprocal binding of PARP-1 and histone H1 at promoters specifies transcriptional outcomes. Science. 2008;319(5864):819–21. https://doi.org/10.1126/science.1149250.
Rouleau M, Patel A, Hendzel MJ, Kaufmann SH, Poirier GG. PARP inhibition: PARP1 and beyond. Nat Rev Cancer. 2010;10(4):293–301. https://doi.org/10.1038/nrc2812.
Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, et al. Inhibition of poly (ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361(2):123–34. https://doi.org/10.1056/NEJMoa0900212.
Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly (ADP-ribose) polymerase. Nature. 2005;434(7035):913–7. https://doi.org/10.1038/nature03443.
Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434(7035):917–21. https://doi.org/10.1038/nature03445.
Prasad SC, Thraves PJ, Bhatia KG, Smulson ME, Dritschilo A. Enhanced poly (adenosine diphosphate ribose) polymerase activity and gene expression in Ewing’s sarcoma cells. Cancer Res. 1990;50(1):38–43.
• Brenner JC, Feng FY, Han S, Patel S, Goyal SV, Bou-Maroun LM, et al. PARP-1 inhibition as a targeted strategy to treat Ewing’s sarcoma. Cancer Res. 2012;72(7):1608–13. https://doi.org/10.1158/0008-5472.can-11-3648. Ewing’s sarcoma family of tumors (ESFT) refers to aggressive malignancies which frequently harbor characteristic EWS-FLI1 or EWS-ERG genomic fusions. Here, we report that these fusion products interact with the DNA damage response protein and transcriptional coregulator PARP-1. ESFT cells, primary tumor xenografts, and tumor metastases were all highly sensitive to PARP1 inhibition. Addition of a PARP1 inhibitor to the second-line chemotherapeutic agent temozolamide resulted in complete responses of all treated tumors in an EWS-FLI1-driven mouse xenograft model of ESFT. Mechanistic investigations revealed that DNA damage induced by expression of EWS-FLI1 or EWS-ERG fusion genes was potentiated by PARP1 inhibition in ESFT cell lines. Notably, EWS-FLI1 fusion genes acted in a positive feedback loop to maintain the expression of PARP1, which was required for EWS-FLI-mediated transcription, thereby enforcing oncogene-dependent sensitivity to PARP-1 inhibition. Together, our findings offer a strong preclinical rationale to target the EWS-FLI1:PARP1 intersection as a therapeutic strategy to improve the treatment of ESFTs.
• Choy E, Butrynski JE, Harmon DC, Morgan JA, George S, Wagner AJ, et al. Phase II study of olaparib in patients with refractory Ewing sarcoma following failure of standard chemotherapy. BMC Cancer. 2014;14:813. https://doi.org/10.1186/1471-2407-14-813. BACKGROUND: Preclinical studies have documented antitumor activity of PARP inhibition both in vitro and in vivo, against Ewing sarcoma cells. This study aimed to translate that observation into a clinical trial to assess the efficacy and tolerability of olaparib, a PARP inhibitor, in patients with advanced Ewing sarcoma (EWS) progressing after prior chemotherapy. METHODS: In this nonrandomized phase II trial, adult participants with radiographically measureable metastatic EWS received olaparib tablets, 400 mg orally twice daily, until disease progression or drug intolerance. Tumor measurements were determined by CT or MRI at 6 and 12 weeks after starting olaparib administration, and then every 8 weeks thereafter. Tumor response determinations were made according to RECIST 1.1, and adverse event determinations were made according to CTCAE, version 4.0. A total of 22 participants were planned to be enrolled using a conventional 2-step phase II study design. If no objective responses were observed after 12 participants had been followed for at least 3 months, further accrual would be stopped. RESULTS: 12 participants were enrolled, and all were evaluable. There were no objective responses (PR/CR), 4 SD (duration 10.9, 11.4, 11.9, and 17.9 wks), and 8 PD as best response. Of the SD, 2 had minor responses (-9% and -11.7% by RECIST 1.1). The median time to disease progression was 5.7 weeks. Further enrollment was therefore discontinued. No significant or unexpected toxicities were observed with olaparib, with only a single case each of grade 3 anemia and grade 3 thrombocytopenia observed. CONCLUSIONS: This study is the first report of a prospective phase II trial to evaluate the safety and efficacy of a PARP inhibitor in patients with advanced Ewing sarcoma after failure of standard chemotherapy. Olaparib administration was safe and well tolerated when administered to this small heavily pre-treated cohort at the 400 mg BID dose, although the median duration of dosing was for only 5.7 weeks. No significant responses or durable disease control was seen, and the short average interval to disease progression underscores the aggressiveness of this disease. Other studies to combine cytotoxic chemotherapy with PARP inhibition in EWS are actively ongoing. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT01583543.
Phase I Study of Olaparib and Temozolomide for Ewings Sarcoma. https://ClinicalTrials.gov/show/NCT01858168.
Florian S, Mitchison TJ. Anti-microtubule drugs. Methods Mol Biol (Clifton, NJ). 2016;1413:403–21. https://doi.org/10.1007/978-1-4939-3542-0_25.
Garrone O, Miraglio E, Vandone AM, Vanella P, Lingua D, Merlano MC. Eribulin in advanced breast cancer: safety, efficacy and new perspectives. Future Oncol (London, England). 2017;13(30):2759–69. https://doi.org/10.2217/fon-2017-0283.
Jordan MA, Kamath K, Manna T, Okouneva T, Miller HP, Davis C, et al. The primary antimitotic mechanism of action of the synthetic halichondrin E7389 is suppression of microtubule growth. Mol Cancer Ther. 2005;4(7):1086–95. https://doi.org/10.1158/1535-7163.Mct-04-0345.
Kuznetsov G, Towle MJ, Cheng H, Kawamura T, TenDyke K, Liu D, et al. Induction of morphological and biochemical apoptosis following prolonged mitotic blockage by halichondrin B macrocyclic ketone analog E7389. Cancer Res. 2004;64(16):5760–6. https://doi.org/10.1158/0008-5472.Can-04-1169.
Hayashida T, Jinno H, Mori K, Sato H, Matsui A, Sakurai T, et al. Phase II trial of eribulin mesylate as a first- or second-line treatment for locally advanced or metastatic breast cancer: a multicenter, single-arm trial. BMC Cancer. 2018;18(1):701–7. https://doi.org/10.1186/s12885-018-4628-7.
WeiDelta LM, Hugle M, Fulda S. Eribulin alone or in combination with the PLK1 inhibitor BI 6727 triggers intrinsic apoptosis in Ewing sarcoma cell lines. Oncotarget. 2017;8(32):52445–56. https://doi.org/10.18632/oncotarget.17190.
Koliou P, Karavasilis V, Theochari M, Pollack SM, Jones RL, Thway K. Advances in the treatment of soft tissue sarcoma: focus on eribulin. Cancer Manag Res. 2018;10:207–16. https://doi.org/10.2147/cmar.S143019.
Study to assess safety and preliminary activity of eribulin mesylate in pediatric participants with relapsed/refractory rhabdomyosarcoma (RMS), non-rhabdomyosarcoma soft tissue sarcoma (NRSTS) and Ewing sarcoma (EWS). https://ClinicalTrials.gov/show/NCT03441360.
Study evaluating the safety and efficacy of eribulin mesilate in combination with irinotecan hydrochloride in children with refractory or recurrent solid tumors. https://ClinicalTrials.gov/show/NCT03245450.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Both authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Molecular Pathology of Skeletal Tumors
Rights and permissions
About this article
Cite this article
Hayden, R., Leggas, M. Novel Drug Treatments for Ewing Sarcoma. Curr Mol Bio Rep 5, 153–166 (2019). https://doi.org/10.1007/s40610-019-00125-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40610-019-00125-9