Abstract
Erythromycin resistance methylases (Erm) confer resistance to three classes of clinically important antibiotics, the macrolides, the lincosamides, and the streptogramins B (MLSB). Erm methylases are located on acquired genetic elements and are widespread in Staphylococcus and other bacterial species. The latest erm determinants have been identified predominantly in coagulase-negative staphylococci using whole-genome sequencing (WGS) and the subsequent search for sequence similarity to erm methylases and specific amino acid motifs. This review presents workflows facilitating the identification and characterization of novel methylase genes, as well as the current status of dissemination of erm genes and their associated genetic elements in staphylococci. Discovery of novel antibiotic resistance genes is necessary to give new insight into molecular epidemiology of antibiotic resistance, for the establishment of better identification and surveillance systems, as well as to continuously improve molecular diagnostic of antibiotic resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The erythromycin resistance methylase (Erm) ribosomal RNA methylases are a class of enzymes which confer resistance to macrolide, lincosamide, and streptogramin B (MLSB) antibiotics in bacteria. Macrolides are bacteriostatic agents, first introduced in the 1950s in the form of erythromycin, produced by the bacterium Saccharopolyspora erythrea [1]. Macrolides have a 12- to 16-membered macrolactone ring which targets the bacterial ribosome mainly through its sugar substitutions [2–4]. Binding of the antibiotic to the bacterial ribosome obstructs the elongation of the nascent peptide chain and subsequently inhibits protein translation. Inhibition of protein synthesis is a mechanism also used by the structurally distinct antibiotic classes lincosamides and streptogramin B [2]. All MLSB antibiotics possess overlapping binding sites and contact the adenine 2058 (A2058, Escherichia coli numbering) of the 23S rRNA, a key nucleotide for drug–ribosome interaction [2, 5]. Generally, MLSB antibiotics are used to treat Gram-positive bacterial infections in both humans and animals [6–8]. Newer semisynthetic macrolide compounds have a wider range of action also targeting Gram-negative species like Bartonella, Bordetella, Borrelia, Campylobacter, Chlamydia, Haemophilus, Helicobacter, Legionella, Neisseria, Moraxella, and Shigella and some species of the Gram-positive related Mycoplasma, Ureaplasma, and Mycobacterium [9]. In addition, macrolides are used for their prokinetic and anti-inflammatory properties in human and veterinary medicine [10–12]. Lincosamides such as clindamycin and lincomycin are used against Gram-positive infections, as well as in the treatment of anaerobes, while streptogramin B antibiotics like virginiamycin S1, quinupristin, or pristinamycin 1A have gained importance due to their activity against vancomycin-resistant Staphylococcus aureus (VRSA) and vancomycin-resistant Enterococcus (VRE) [6, 13]. In addition, individual MLSB compounds are extensively used as herd/flock medication to prevent or treat infectious diseases in food-producing animals [7, 13]. The World Health Organization (WHO) has classified macrolides as the highest-priority critically important antibiotics for human medicine and both lincosamides and streptogramins as highly important drug classes for human medicine [14]. The widespread use of MLSB antibiotics jeopardizes their effectiveness by increasing the risk of selecting bacteria with acquired resistance to these classes of drugs [15–17].
One of the most common mechanism of resistance to MLSB antibiotics is the chemical modification of the bacterial 23S rRNA by monomethylation or dimethylation of A2058 by Erm rRNA methylases [18]. Erm methylases add up to three methyl groups to nucleotides at positions 2057, 2058, and/or 2059 of the 23S rRNA [19, 20]. However, dimethylation of A2058 is the most common mechanism found in bacteria and efficiently prevents the binding of MLSB antibiotics, including the macrolide derivates ketolides (e.g., telithromycin) [16, 18, 20, 21]. Erm methylases are encoded by erm genes which are either constitutively expressed or induced in the presence of 14- and 15-membered macrolides [22]. Inducible MLSB resistance is regulated by a region upstream of the erm mRNA start codon. In staphylococci, this regulatory region consists of open reading frames (orfs) coding for either one or two leader peptides, of which one harbors the conserved IVFI or MRNVD amino acid motif [23–26]. The secondary structure of this leader mRNA embeds the ribosomal binding site and start codon of the erm gene in a hairpin structure, which prevents its expression. Binding of inducer macrolides such as erythromycin to the ribosome results in attenuated translation of the leader peptide mRNA, subsequently causing the ribosome to stall [26]. Translational attenuation causes a rearrangement of the mRNA hairpin secondary structure, releasing the ribosomal binding site and the start codon of the erm gene thus allowing translation of the methylase [27, 28]. As a result, isolates expressing an inducible phenotype can remain susceptible to lincosamides, streptogramin B, 16-membered macrolides, or ketolides if no macrolide is present [25]. However, selection of mutants constitutively expressing the erm gene may rapidly occur when lincosamides, streptogramin B, or ketolides are being used [9, 22]. Other mechanisms conferring resistance to all or individual classes of MLSB antibiotics are listed in Table 1 and were not taken into consideration in this review.
The genus Staphylococcus comprises more than 50 species which are subdivided into two groups depending on their ability to coagulate plasma [29, 30]. The coagulase-positive staphylococci include S. aureus, Staphylococcus argenteus, Staphylococcus delphini, Staphylococcus hyicus, Staphylococcus intermedius, Staphylococcus lutrae, Staphylococcus pseudintermedius, Staphylococcus schleiferi subsp. coagulans and Staphylococcus schweitzeri, while all other species belong to the group of the coagulase-negative staphylococci (CoNS). Staphylococci are naturally found on the skin and mucous membranes of mammals, as well as in diverse environmental sources [30, 31]. They can turn into major opportunistic pathogens in humans and animals and cause a wide variety of infections ranging from skin and soft tissue infections to bacteremia [30, 32, 33]. In general, S. aureus and other coagulase-positive staphylococci are the main staphylococcal pathogens [33]. However, during recent years, some of the CoNS have emerged as an important cause of nosocomial infections in human medicine as well as in veterinary medicine where they have been increasingly associated with bovine mastitis, as well as with several types of infections in companion animals [33–36]. Due to the acquisition of multiple resistance mechanisms, antimicrobial therapy became limited with some staphylococcal species representing a serious threat for human and animal health [23, 36–41]. As β-lactams and other critically important classes turned out to be increasingly ineffective in the treatment of staphylococcal infections, macrolide and lincosamide classes gained importance as alternative antimicrobial treatment options [42].
Due to the alarming increase of antibiotic resistance in bacteria over the last decades, the WHO has declared the current state of antimicrobial resistance a global health security threat [43]. Worldwide surveillance of antibiotic-resistant bacteria in humans, animals, and the food chain, and the reduction of inappropriate use of antimicrobial drugs are the essential proposed actions to control the spread of antimicrobial resistance [43]. To successfully monitor resistance, it is crucial to know all mediators and reservoirs of antibiotic resistance. In the last 5 years, novel MLSB resistance genes have been mostly detected in bacteria of animal origin [44–47]. These novel genes consisted of erm(43), erm(44), and erm(45) from different Staphylococcus species and erm(46) from Rhodococcus equi and were all detected using whole-genome sequencing (WGS) and subsequent sequence analysis.
Possible workflows useful for the discovery and characterization of novel erm genes using WGS are described in this review. Furthermore, the current state of distribution of erm genes in bacteria, as well as their location on different genetic elements in Staphylococcus sp., is presented, offering an updated baseline for future characterization of novel erm genes and of erm-containing genetic elements.
Search for Novel erm Methylases
Phenotypic Criteria
The likelihood of the presence of an erm gene can be evaluated by the phenotypic observation of either resistance to both erythromycin and clindamycin or resistance to erythromycin and inducible resistance to clindamycin. An inducible MLSB phenotype can be visualized in vitro by performing D-Test or by MIC determination of clindamycin in the presence of 4 μg/ml of erythromycin [48, 49]. In the presence of an inducible phenotype, it can be assumed that the strain contains an erm gene, whereas a constitutive resistance phenotype may also be associated with other resistance mechanisms (Table 1).
Genetic Approach to Identify an erm Determinant
Whole-genome sequencing has become more accessible during recent years due to increased user friendliness, efficiency, cost-effectiveness, and an increase in the number of facilities offering WGS services [50–52]. Compared to the classical shotgun cloning and subsequent phenotypic screening for the identification of candidate genes, WGS is significantly faster and therefore became the method of choice to identify novel MLSB candidate genes in bacterial genomes. However, rapid preliminary screening of bacteria for the presence of already known resistance mechanisms should still be considered. In general, the detection of acquired MLSB resistance is easier than that of resistance conferred by ribosomal mutations. Identification of ribosomal mutations calls for specific detection methods, since several operons of ribosomal genes are dispersed through the bacterial genome (Table 1)[53, 54]. Currently, microarrays represent an efficient and affordable tool to assign an acquired phenotype to known resistance genes [55, 56]. The recently described microarray of Strauss et al. is among the most suitable for allocating acquired resistance, as it can detect all currently known MLSB methylase genes in Staphylococcus as well as most other genes associated with MLSB resistance in Gram-positive bacteria [55]. If no association with a known resistance genotype can be made using such a microarray, there is a strong suspicion that the investigated strain contains a novel resistance mechanism and WGS becomes inevitable.
Nowadays, several WGS technologies for bacterial whole-genome sequencing are available including Illumina®MiSeq (Illumina, San Diego, CA), IonTorrentTM PGM (Life Technologies, Guilford, CT), PacBio® RSII (Pacific Biosciences, Menlo Park, CA), and MinIONTM (Oxford Nanopore Technologies, Oxford, UK) [57, 58]. In general, techniques generating long read lengths, such as IonTorrent and PacBio, are recommended for de novo sequencing of new erm determinants which can be located on genetic elements that may contain several copies of repeat elements, such as insertion sequences (IS) and extensive direct or tandem repeats [59].
Subsequent screening of the generated sequence contigs for putative erm genes using bioinformatic tools is straightforward. By current nomenclature, Erm methylases are defined novel if they have ≤79 % amino acid homology with any known methylase (http://faculty.washington.edu/marilynr/MLSnomenclatureCenter.pdf) [8]. Novel Erm methylases can be detected by BLAST alignment of either their amino acid or nucleotide sequence with known erm determinants [60]. Several freely available online tools, such as ResFinder and ARG-ANNOT, are also useful to detect novel resistance genes based on DNA/amino acid homology [61]. Searching for a specific conserved amino acid motif is an alternative to the detection of putative Erm homologies. The majority of the erm methylases contain the PROSITE rRNA adenine dimethylase signature pattern PS01131 (Fig. 1) [44]. Exceptions to this rule are Erm(I), Erm(N), Erm(Z), Erm(32), Erm(37), and Erm(41), which are found in Streptomyces and Mycobacteria and are suspected to be monomethylases, rather than dimethylases [20, 62]. To also include these additional erm methylases, a modified version of the PS01131 signature has been proposed by Schwendener and Perreten, allowing the detection of all known Erm methylases except Erm(32) (Fig. 1). Bioinformatic tools such as Scan Prosite (http://prosite.expasy.org/scanprosite/) or MOTIF (http://www.genome.jp/tools/motif/) can be used to search for such a specific Erm signature pattern. However, DNA sequences of entire contigs have to be first translated into all six amino acid reading frames and each frame must be screened individually.
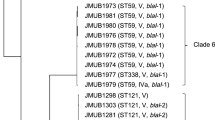
Phylogenetic relatedness and alignment of the ribosomal RNA adenine dimethylase signature (PROSITE pattern PS01131) of all 38 Erm methylases (modified from Schwendener et al. [44]). Complete amino acid sequence (Acc. no.) of Erm methylases were used for dendrogram construction and were chosen from the species for which the protein was initially described (species). Clustering of Erm amino acid sequences was performed by BioNumerics 7.5 (Applied Maths). The comparison settings were standard algorithm for pairwise alignment, open gap penalty 100 %, unit gap penalty 0 %, and the unweighted-pair group method using average linkages. The PS01131 signature pattern, with amino acids acceptable for one given position listed between square brackets and x for any amino acid followed by the possible repetition range between parentheses, is defined as [LIVMAC]-[LIVMFYWT]-[DE]-x-G-[STAPVLCG]-G-x-[GAS]-x-[LIVMF]-[ST]-x(2,3)-[LIVMA]-x(5,8)-[LIVMYF]-x-[STAGVLC]-[LIVMFYHCS]-E-x-D. In the figure, invariant amino acids are shaded black, highly conserved amino acids dark grey, and less conserved positions light grey. A modified PS0113 signature to recognize most Erm methylases would be [LIVMACT]-[LIVMFYWT]-[DE]-x-G-[STAPVLCG]-G-x-[GAS]-x-[LIVMF]-[ST]-x(2,3)-[LIVMA]-x(5,8)-[LIVMYF]-x-[STAGVLC]-[LIVMFYHCS]-E-x-[DH]. Erm(32) is listed but does not contain a complete PS01131 signature
Proof of Functionality
The function of MLSB resistance can only be attributed to a newly detected methylase gene after demonstration of an association between the gene and the phenotype. To demonstrate its expression in vitro, the gene can either be inactivated in the original strain generating a MLSB susceptible knockout mutant or transformed into a MLSB susceptible host generating a MLSB-resistant transformant. Replacement of genes in field strains of Staphylococcus can be impaired by a low transformation efficiency and/or the presence of restriction modification systems; therefore, expression in a laboratory strain like S. aureus RN4220 is more frequently used [63, 64]. Recently, S. aureus–E. coli shuttle vectors pBUS1-HC and pBUS1-P cap -HC have been shown to be suitable for expression of erm genes under control of their own promoter and the strong constitutive promoter of S. aureus type 1 capsule gene 1A [45, 46, 65]. Of note, inducibility will be kept only if the erm gene is still under control of its own regulatory sequence including the leader peptide region. On the other hand, the erm gene will be expressed constitutively in the absence of the leader peptide region [45, 46].
Identification of Regions Flanking erm Genes
WGS provides further information on the regions flanking a novel gene and facilitates the characterization of the acquired genetic element carrying the new erm gene. For instance, plasmids can be identified by the presence of rep-genes, circularized sequence, or by a higher coverage [66]. Elements integrated into the bacterial chromosome can be identified by alignment of the erm-containing sequence region with that of a MLSB-susceptible strain of the same species. This allows identification of both the integrated element and the integration site, as well as the adjacent housekeeping genes. PCR with primers designed from the putative flanking housekeeping genes can be used to identify additional susceptible strains lacking the integrated element. Such PCR experiments will further assist the identification of the chromosomal integration site in MLSB-susceptible strains for which no whole-genome sequence is available. The presence of inverted and direct repeats, which are directly linked to transposases and integrases, is a further indication of foreign element integration.
Distribution of erm Genes and Their Association With Acquired Genetic Elements
The erm genes are widely distributed in Gram-positive, Gram-negative, aerobic, and anaerobic genera (Fig. 1) [8, 16]. Among the 38 currently described erm genes in bacteria, 12 have been identified in the genus Staphylococcus using PCR, hybridization, or sequence analysis. They consist of erm(A), erm(B), erm(C), erm(F), erm(G), erm(Q), erm(T), erm(Y), erm(33), erm(43), erm(44), and erm(45) [39, 45, 46] (Fig. 1 and Table 2). To date, the presence of all erm genes in Staphylococcus has been confirmed by sequence analysis, except for erm(F), erm(G), and erm(Q) [37, 67, 68]. Of note, the Erm determinants confirmed to be present in staphylococci by sequence analysis all clustered into the same branch of the Erm dendrogram (Fig. 1). Searching the GenBank and literature revealed that erm(A), erm(B), and erm(C) are the most widespread erm genes in the different staphylococcal species, as well as in a multitude of other bacterial genera (Table 2). The broad distribution of erm(A), erm(B), and erm(C) can be explained by their association with mobile genetic elements with a high potential for dissemination, like broad-host-range plasmids and transposons, whereas other erm genes are located on specific elements integrated into the chromosome. These integrated elements seem to be rather species specific or have lost their transfer machineries.
The erm(A) gene has been identified in a multitude of S. aureus strains and in CoNS (Table 2). The spread of erm(A) in Staphylococcus is mediated by transposon Tn554 and its relatives such as Tn6133, which belong to the high-frequency and site-specific transposable elements [69–71]. Tn554-like transposons integrate into a specific chromosomal attachment site but may also use alternative integration sites, such as those present on acquired genetic elements like SCCmec elements and plasmids [72, 73].
Erm(B) is the most widespread methylase in different bacterial genera and is also common in a multitude of staphylococcal species (Table 2). Spread of erm(B) is mediated by Tn917/Tn551 and Tn5405-like transposons [40, 74]. Those non-site-specific transposons easily conglomerate into larger transposal structures and promiscuously integrate into the chromosome and plasmids, offering further vessels for transportation and broad host distribution of erm(B) [75–78].
The erm(C) gene which is the most frequently annotated among staphylococcal species is commonly found on small plasmids (Table 2). Although these small plasmids are not self-transmissible, they contain mobilizing genes which contribute to their dissemination [79].
The remaining erm genes detected in Staphylococcus sp. have been mainly associated with single species. For instance, erm(T) and erm(Y) were found in S. aureus, erm(33) in Staphylococcus sciuri, erm(43) in Staphylococcus lentus, and erm(45) in Staphylococcus fleurettii (Table 2). The only exception is erm(44), which has been detected in Staphylococcus xylosus and Staphylococcus saprophyticus (Table 2). However, one erm(44) gene from a S. saprophyticus of human origin and one erm(44) from a S. saprophyticus isolated from sewage were found to share 77 % amino acid homology with each other and 81 and 84 % homology to the original erm(44), respectively. This suggests a different epidemiological origin [80]. The erm(T), erm(Y), and erm(33) genes are all located on plasmids between 12 and 20 kb in size, and erm(T) has also been found integrated into the chromosome (Table 2) [81]. The erm(33) is additionally linked to Tn554 located on a plasmid, most likely due to its relation to erm(A) [82].
The more recently described erm genes erm(43), erm(44), and erm(45) were found on so far unknown integrated elements. The erm(43) gene is located on an acquired fragment flanked by long direct repeats at a specific chromosomal site in S. lentus [44]. Structures like the erm(43)-carrying fragment arguably form a novel group of mobile genetic elements, which are also present in other species and associated with different resistance genes [83].
The recently discovered erm(44) was located in the genome of an integrated prophage in S. xylosus [45]. This prophage ΦJW4341-pro was the first to be fully sequenced and has been found to have naturally incorporated a resistance gene in Staphylococcus. The integration of bacterial DNA into phage genomes can lead to selective advantages for the phage host and was extensively described for virulence and other fitness-enhancing genes [84, 85]. With the detection of erm(44), the phenomenon of spreading genetic information via bacteriophages has gained in importance in the field of antimicrobial resistance dissemination. Although no active transduction of ΦJW4341-pro was observed, the occurrence of erm(44) in different S. xylosus from bovine mastitis suggests spreading of this gene by phage ΦJW4341-pro. Recently, erm(44) has also been identified on acquired chromosomal fragments in a human and environmental S. saprophyticus isolate using WGS (Table 2) [86]. The diverse flanking regions of the genetically distinct erm(44) genes support the suggested individual acquisition of those genes without direct transfer between S. xylosus and S. saprophyticus (Table 2) [86].
The erm(45) gene is another novel methylase gene detected on a phage related fragment [46]. It has been identified in a S. fleurettii strain isolated from bovine milk using WGS. This erm(45)-containing genetic island consists of open reading frames and a structure similar to those found in phage or the phage-associated S. aureus pathogenicity islands (SaPIs) [87]. Although capable of circularization, this island was not observed to be mobilized by either conjugation or transformation into S. aureus and its ability to disseminate is still unknown.
Conclusions
The recent discoveries of novel erm genes emphasize the role of staphylococci as a large reservoir of MLSB resistance genes. Staphylococci seem to have a particular ability to acquire new genes through multifaceted mechanisms, including plasmids, transposons, genomic islands, and bacteriophage or bacteriophage-related elements. WGS has already widely contributed to the detection of so far unknown and large mobile genetic elements in staphylococci and other bacteria. Considering the ability of bacteria to rapidly adapt to foreign environments such as antimicrobial selective pressure, it is crucial to have tools for the rapid identification of new emerging resistance genes. Rapid detection of novel resistance genes from different ecological and clinical niches is of major importance for the continuous improvement of antibiotic resistance surveillance programs and diagnostics, as well as for well-targeted and prudent use of antibiotics.
References
McGuire JM, Bunch RL, Anderson RC, Boaz HE, Flynn EH, Powell HM, et al. Ilotycin, a new antibiotic. Schweiz Med Wochenschr. 1952;82(41):1064–5.
Poehlsgaard J, Douthwaite S. The bacterial ribosome as a target for antibiotics. Nat Rev Microbiol. 2005;3(11):870–81.
Walsh C. Antibiotics: actions, origins, resistance. Washington: ASM Press; 2003.
Schlünzen F, Zarivach R, Harms J, Bashan A, Tocilj A, Albrecht R, et al. Structural basis for the interaction of antibiotics with the peptidyl transferase centre in eubacteria. Nature. 2001;413(6858):814–21.
Poehlsgaard J, Pfister P, Böttger EC, Douthwaite S. Molecular mechanisms by which rRNA mutations confer resistance to clindamycin. Antimicrob Agents Chemother. 2005;49(4):1553–5.
White DG, Alekshun MN, McDermott PF. Frontiers in antimicrobial resistance: a tribute to Stuart B. Levy. Washington: ASM Press; 2005.
Prescott JF, Baggot JD, Walker RD. Antimicrobial therapy in veterinary medicine. 3rd ed. Ames: Iowa State University Press; 2000.
Roberts MC. Update on macrolide-lincosamide-streptogramin, ketolide, and oxazolidinone resistance genes. FEMS Microbiol Lett. 2008;282(2):147–59.
Sivapalasingam S, Steigbigel NH. Macrolides, clindamycin, and ketolides. In: Bennet JE, Dolin R, Blaser MJ, editors. Mandell, Douglas and Bennett’s principles and practice of infectious diseases. 8th ed. St. Louis: Saunders Elsevier; 2015. p. 358–76.
Steel HC, Theron AJ, Cockeran R, Anderson R, Feldman C. Pathogen- and host-directed anti-inflammatory activities of macrolide antibiotics. Mediat Inflamm. 2012;2012:584262.
Nouri M, Constable PD. Effect of parenteral administration of erythromycin, tilmicosin, and tylosin on abomasal emptying rate in suckling calves. Am J Vet Res. 2007;68(12):1392–8.
Lester GD, Merritt AM, Neuwirth L, Vetro-Widenhouse T, Steible C, Rice B. Effect of erythromycin lactobionate on myoelectric activity of ileum, cecum, and right ventral colon, and cecal emptying of radiolabeled markers in clinically normal ponies. Am J Vet Res. 1998;59(3):328–34.
European Medicines Agency. Reflection paper on the use of macrolides, lincosamides and streptogramins (MLS) in food-producing animals in the European Union: development of resistance and impact on human and animal health. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2011/11/WC500118230.pdf. Accessed 8 Dec 2015.
The World Health Organization (WHO). Critically important antimicrobials for human medicine. 2011. http://apps.who.int/iris/bitstream/10665/77376/1/9789241504485_eng.pdf. Accessed 8 Dec 2015.
European Medicines Agency. Sales of veterinary antimicrobial agents in 26 EU/EEA countries in 2013. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/Report/2015/10/WC500195687.pdf. Accessed 8 Dec 2015.
Roberts MC, Sutcliffe J, Courvalin P, Jensen LB, Rood J, Seppälä H. Nomenclature for macrolide and macrolide-lincosamide-streptogramin B resistance determinants. Antimicrob Agents Chemother. 1999;43(12):2823–30.
English BK, Gaur AH. The use and abuse of antibiotics and the development of antibiotics resistance. Adv Exp Med Biol. 2010;659:73–82.
Weisblum B. Erythromycin resistance by ribosome modification. Antimicrob Agents Chemother. 1995;39(3):577–85.
Vester B, Douthwaite S. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob Agents Chemother. 2001;45(1):1–12.
Madsen CT, Jakobsen L, Buriánková K, Doucet-Populaire F, Pernodet JL, Douthwaite S. Methyltransferase Erm(37) slips on rRNA to confer atypical resistance in Mycobacterium tuberculosis. J Biol Chem. 2005;280(47):38942–7.
Liu M, Douthwaite S. Activity of the ketolide telithromycin is refractory to Erm monomethylation of bacterial rRNA. Antimicrob Agents Chemother. 2002;46(6):1629–33.
Leclercq R. Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002;34(4):482–92.
Chancey ST, Zähner D, Stephens DS. Acquired inducible antimicrobial resistance in Gram-positive bacteria. Future Microbiol. 2012;7(8):959–78.
Min YH, Kwon AR, Yoon EJ, Shim MJ, Choi EC. Translational attenuation and mRNA stabilization as mechanisms of erm(B) induction by erythromycin. Antimicrob Agents Chemother. 2008;52(5):1782–9.
Depardieu F, Podglajen I, Leclercq R, Collatz E, Courvalin P. Modes and modulations of antibiotic resistance gene expression. Clin Microbiol Rev. 2007;20(1):79–114.
Subramanian SL, Ramu H, Mankin AS. Inducible resistance to macrolide antibiotics. In: Dougherty TJ, Pucci MJ, editors. Antibiotic discovery and development. New York: Springer; 2012. p. 445–84.
Ramu H, Mankin A, Vazquez-Laslop N. Programmed drug-dependent ribosome stalling. Mol Microbiol. 2009;71(4):811–24.
Arenz S, Ramu H, Gupta P, Berninghausen O, Beckmann R, Vazquez-Laslop N, et al. Molecular basis for erythromycin-dependent ribosome stalling during translation of the ErmBL leader peptide. Nat Commun. 2014;5:3501.
Tong SY, Schaumburg F, Ellington MJ, Corander J, Pichon B, Leendertz F, et al. Novel staphylococcal species that form part of a Staphylococcus aureus-related complex: the non-pigmented Staphylococcus argenteus sp. nov. and the non-human primate-associated Staphylococcus schweitzeri sp. nov. Int J Syst Evol Microbiol. 2015;65(Pt 1):15–22.
Götz F, Bannerman T, Schleifer K-H. The genera Staphylococcus and Macrococcus. In: Dworkin M, Falkow S, Rosenberg E, Schleifer K-H, Stackebrandt E, editors. The Prokaryotes. New York: Springer; 2006. p. 5–75.
Kloos WE, Musselwhite MS. Distribution and persistence of Staphylococcus and Micrococcus species and other aerobic bacteria on human skin. Appl Microbiol. 1975;30(3):381–5.
Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339(8):520–32.
Casey AL, Lambert PA, Elliott TS. Staphylococci. Int J Antimicrob Agents. 2007;29 Suppl 3:S23–32.
Kern A, Perreten V. Clinical and molecular features of methicillin-resistant, coagulase-negative staphylococci of pets and horses. J Antimicrob Chemother. 2013;68(6):1256–66.
Pyörälä S, Taponen S. Coagulase-negative staphylococci emerging mastitis pathogens. Vet Microbiol. 2009;134(1–2):3–8.
Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870–926. doi:10.1128/CMR.00109-13.
van Hoek AH, Mevius D, Guerra B, Mullany P, Roberts AP, Aarts HJ. Acquired antibiotic resistance genes: an overview. Front Microbiol. 2011;2(203).
Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler Jr VG. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28(3):603–61.
Wendlandt S, Fessler AT, Monecke S, Ehricht R, Schwarz S, Kadlec K. The diversity of antimicrobial resistance genes among staphylococci of animal origin. Int J Med Microbiol. 2013;303(6–7):338–49.
Wendlandt S, Shen J, Kadlec K, Wang Y, Li B, Zhang WJ, et al. Multidrug resistance genes in staphylococci from animals that confer resistance to critically and highly important antimicrobial agents in human medicine. Trends Microbiol. 2015;23(1):44–54.
Gatermann SG, Koschinski T, Friedrich S. Distribution and expression of macrolide resistance genes in coagulase-negative staphylococci. Clin Microbiol Infect. 2007;13(8):777–81.
Chambers HF, De Leo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–41.
The World Health Organization (WHO). Antimicrobial resistance: global report on surveillance. 2014. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1. Accessed 8 Dec 2015.
Schwendener S, Perreten V. New macrolide-lincosamide-streptogramin B resistance gene erm(43) in Staphylococcus lentus. Antimicrob Agents Chemother. 2012;56(9):4746–52.
Wipf JRK, Schwendener S, Perreten V. The novel macrolide-lincosamide-streptogramin B resistance gene erm(44) is associated with a prophage in Staphylococcus xylosus. Antimicrob Agents Chemother. 2014;58:6133–8.
Wipf JRK, Schwendener S, Nielsen JB, Westh H, Perreten V. The new macrolide-lincosamide-streptogramin B resistance gene erm(45) is located within a genomic island in Staphylococcus fleurettii. Antimicrob Agents Chemother. 2015;59(6):3578–81.
Anastasi E, Giguère S, Berghaus LJ, Hondalus MK, Willingham-Lane JM, MacArthur I, et al. Novel transferable erm(46) determinant responsible for emerging macrolide resistance in Rhodococcus equi. J Antimicrob Chemother. 2015. doi:10.1093/jac/dkv279.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-fourth informational supplement M100–S24, 34(1). Wayne: Clinical and Laboratory Standards Institute; 2014.
Woods CR. Macrolide-inducible resistance to clindamycin and the D-test. Pediatr Infect Dis J. 2009;28(12):1115–8.
Fournier PE, Drancourt M, Colson P, Rolain JM, La Scola B, Raoult D. Modern clinical microbiology: new challenges and solutions. Nat Rev Microbiol. 2013;11(8):574–85.
Sibley CD, Peirano G, Church DL. Molecular methods for pathogen and microbial community detection and characterization: current and potential application in diagnostic microbiology. Infect Genet Evol. 2012;12(3):505–21.
Hasman H, Saputra D, Sicheritz-Ponten T, Lund O, Svendsen CA, Frimodt-Moller N, et al. Rapid whole-genome sequencing for detection and characterization of microorganisms directly from clinical samples. J Clin Microbiol. 2014;52(1):139–46.
Haanperä M, Huovinen P, Jalava J. Detection and quantification of macrolide resistance mutations at positions 2058 and 2059 of the 23S rRNA gene by pyrosequencing. Antimicrob Agents Chemother. 2005;49(1):457–60.
Canu A, Malbruny B, Coquemont M, Davies TA, Appelbaum PC, Leclercq R. Diversity of ribosomal mutations conferring resistance to macrolides, clindamycin, streptogramin, and telithromycin in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2002;46(1):125–31.
Strauss C, Endimiani A, Perreten V. A novel universal DNA labeling and amplification system for rapid microarray-based detection of 117 antibiotic resistance genes in Gram-positive bacteria. J Microbiol Methods. 2015;108:25–30.
Perreten V, Vorlet-Fawer L, Slickers P, Ehricht R, Kuhnert P, Frey J. Microarray-based detection of 90 antibiotic resistance genes of gram-positive bacteria. J Clin Microbiol. 2005;43(5):2291–302.
Miyamoto M, Motooka D, Gotoh K, Imai T, Yoshitake K, Goto N, et al. Performance comparison of second- and third-generation sequencers using a bacterial genome with two chromosomes. BMC Genomics. 2014;15:699.
Karlsson E, Lärkeryd A, Sjödin A, Forsman M, Stenberg P. Scaffolding of a bacterial genome using MinION nanopore sequencing. Sci Rep. 2015;5:11996.
Utturkar SM, Klingeman DM, Land ML, Schadt CW, Doktycz MJ, Pelletier DA, et al. Evaluation and validation of de novo and hybrid assembly techniques to derive high-quality genome sequences. Bioinformatics. 2014;30(19):2709–16.
Boratyn GM, Camacho C, Cooper PS, Coulouris G, Fong A, Ma N et al. BLAST: a more efficient report with usability improvements. Nucleic Acids Res. 2013;41(Web Server issue):W29-33.
Zankari E. Comparison of the web tools ARG-ANNOT and ResFinder for detection of resistance genes in bacteria. Antimicrob Agents Chemother. 2014;58(8):4986.
Nash KA, Brown-Elliott BA, Wallace Jr RJ. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob Agents Chemother. 2009;53(4):1367–76.
Kreiswirth BN, Löfdahl S, Betley MJ, O’Reilly M, Schlievert PM, Bergdoll MS, et al. The toxic shock syndrome exotoxin structural gene is not detectably transmitted by a prophage. Nature. 1983;305(5936):709–12.
Corvaglia AR, Francois P, Hernandez D, Perron K, Linder P, Schrenzel J. A type III-like restriction endonuclease functions as a major barrier to horizontal gene transfer in clinical Staphylococcus aureus strains. Proc Natl Acad Sci U S A. 2010;107(26):11954–8.
Schwendener S, Perreten V. New shuttle vector-based expression system to generate polyhistidine-tagged fusion proteins in Staphylococcus aureus and Escherichia coli. Appl Environ Microbiol. 2015;81(9):3243–54.
Riley MC, Perreten V, Bemis DA, Kania SA. Discovering plasmids in MRSP using genome sequencing. 4th ASM-ESCMID conference on methicillin-resistant staphylococci in animals: Veterinary and Public Health Implications. Chicago, IL. 2-5th November 2015.
Chung WO, Werckenthin C, Schwarz S, Roberts MC. Host range of the ermF rRNA methylase gene in bacteria of human and animal origin. J Antimicrob Chemother. 1999;43(1):5–14.
Wang Y, Wang GR, Shoemaker NB, Whitehead TR, Salyers AA. Distribution of the ermG Gene among bacterial isolates from porcine intestinal contents. Appl Environ Microbiol. 2005;71(8):4930–4.
Bastos MC, Murphy E. Transposon Tn554 encodes three products required for transposition. EMBO J. 1988;7(9):2935–41.
Murphy E. Nucleotide sequence of ermA, a macrolide-lincosamide-streptogramin B determinant in Staphylococcus aureus. J Bacteriol. 1985;162(2):633–40.
Schwendener S, Perreten V. New transposon Tn6133 in methicillin-resistant Staphylococcus aureus ST398 contains vga(E), a novel streptogramin A, pleuromutilin, and lincosamide resistance gene. Antimicrob Agents Chemother. 2011;55(10):4900–4.
Chikramane SG, Matthews PR, Noble WC, Stewart PR, Dubin DT. Tn554 inserts in methicillin-resistant Staphylococcus aureus from Australia and England: comparison with an American methicillin-resistant group. J Gen Microbiol. 1991;137(6):1303–11.
Murphy E, Phillips S, Edelman I, Novick RP. Tn554: isolation and characterization of plasmid insertions. Plasmid. 1981;5(3):292–305.
Werner G, Hildebrandt B, Witte W. Linkage of erm(B) and aadE-sat4-aphA-3 in multiple-resistant Enterococcus faecium isolates of different ecological origins. Microb Drug Resist. 2003;9 Suppl 1:9–16.
Toh SM, Xiong L, Arias CA, Villegas MV, Lolans K, Quinn J, et al. Acquisition of a natural resistance gene renders a clinical strain of methicillin-resistant Staphylococcus aureus resistant to the synthetic antibiotic linezolid. Mol Microbiol. 2007;64(6):1506–14.
Gales AC, Deshpande LM, de Souza AG, Pignatari AC, Mendes RE. MSSA ST398/t034 carrying a plasmid-mediated cfr and erm(B) in Brazil. J Antimicrob Chemother. 2015;70(1):303–5.
Locke JB, Rahawi S, Lamarre J, Mankin AS, Shaw KJ. Genetic environment and stability of cfr in methicillin-resistant Staphylococcus aureus CM05. Antimicrob Agents Chemother. 2012;56(1):332–40.
Li B, Wendlandt S, Yao J, Liu Y, Zhang Q, Shi Z, et al. Detection and new genetic environment of the pleuromutilin-lincosamide-streptogramin A resistance gene lsa(E) in methicillin-resistant Staphylococcus aureus of swine origin. J Antimicrob Chemother. 2013;68(6):1251–5.
Projan SJ, Archer GL. Mobilization of the relaxable Staphylococcus aureus plasmid pC221 by the conjugative plasmid pGO1 involves three pC221 loci. J Bacteriol. 1989;171(4):1841–5.
Hall RM, Schwarz S. Resistance gene naming and numbering: is it a new gene or not? J Antimicrob Chemother. 2015. doi:10.1093/jac/dkv351.
Gómez-Sanz E, Zarazaga M, Kadlec K, Schwarz S, Torres C. Chromosomal integration of the novel plasmid pUR3912 from methicillin-susceptible Staphylococcus aureus ST398 of human origin. Clin Microbiol Infect. 2013;19(11):E519–22.
Kehrenberg C, Ojo KK, Schwarz S. Nucleotide sequence and organization of the multiresistance plasmid pSCFS1 from Staphylococcus sciuri. J Antimicrob Chemother. 2004;54(5):936–9.
Palmieri C, Mingoia M, Varaldo PE. Unconventional circularizable bacterial genetic structures carrying antibiotic resistance determinants. Antimicrob Agents Chemother. 2013;57(5):2440–1.
Fortier LC, Sekulovic O. Importance of prophages to evolution and virulence of bacterial pathogens. Virulence. 2013;4(5):354–65.
Brüssow H, Canchaya C, Hardt WD. Phages and the evolution of bacterial pathogens: from genomic rearrangements to lysogenic conversion. Microbiol Mol Biol Rev. 2004;68(3):560–602.
Wendlandt S, Hess S, Li J, Fessler AT, Wang Y, Kadlec K et al. Detection of the macrolide-lincosamide-streptogramin B resistance gene erm(44) and a novel erm(44) variant in staphylococci from aquatic environments. FEMS Microbiol Ecol. 2015;91(8):fiv090.
Novick RP, Christie GE, Penadés JR. The phage-related chromosomal islands of Gram-positive bacteria. Nat Rev Microbiol. 2010;8(8):541–51.
Wittmann HG, Stöffler G, Apirion D, Rosen L, Tanaka K, Tamaki M, et al. Biochemical and genetic studies on two different types of erythromycin resistant mutants of Escherichia coli with altered ribosomal proteins. Mol Gen Genet. 1973;127(2):175–89.
Schoner B, Geistlich M, Rosteck Jr P, Rao RN, Seno E, Reynolds P, et al. Sequence similarity between macrolide-resistance determinants and ATP-binding transport proteins. Gene. 1992;115(1–2):93–6.
Isnard C, Malbruny B, Leclercq R, Cattoir V. Genetic basis for in vitro and in vivo resistance to lincosamides, streptogramins A, and pleuromutilins (LSAP Phenotype) in Enterococcus faecium. Antimicrob Agents Chemother. 2013;57(9):4463–9.
Ross JI, Eady EA, Cove JH, Cunliffe WJ, Baumberg S, Wootton JC. Inducible erythromycin resistance in staphylococci is encoded by a member of the ATP-binding transport super-gene family. Mol Microbiol. 1990;4(7):1207–14.
Chesneau O, Ligeret H, Hosan-Aghaie N, Morvan A, Dassa E. Molecular analysis of resistance to streptogramin A compounds conferred by the Vga proteins of staphylococci. Antimicrob Agents Chemother. 2005;49(3):973–80.
Rodriguez AM, Olano C, Vilches C, Méndez C, Salas JA. Streptomyces antibioticus contains at least three oleandomycin-resistance determinants, one of which shows similarity with proteins of the ABC-transporter superfamily. Mol Microbiol. 1993;8(3):571–82.
Hot C, Berthet N, Chesneau O. Characterization of sal(A), a novel gene responsible for lincosamide and streptogramin A resistance in Staphylococcus sciuri. Antimicrob Agents Chemother. 2014;58(6):3335–41.
Geistlich M, Losick R, Turner JR, Rao RN. Characterization of a novel regulatory gene governing the expression of a polyketide synthase gene in Streptomyces ambofaciens. Mol Microbiol. 1992;6(14):2019–29.
Rosteck Jr PR, Reynolds PA, Hershberger CL. Homology between proteins controlling Streptomyces fradiae tylosin resistance and ATP-binding transport. Gene. 1991;102(1):27–32.
Allignet J, Loncle V, el Sohl N. Sequence of a staphylococcal plasmid gene, vga, encoding a putative ATP-binding protein involved in resistance to virginiamycin A-like antibiotics. Gene. 1992;117(1):45–51.
Jäger W, Kalinowski J, Pühler A. A Corynebacterium glutamicum gene conferring multidrug resistance in the heterologous host Escherichia coli. J Bacteriol. 1997;179(7):2449–51.
Zhang HZ, Schmidt H, Piepersberg W. Molecular cloning and characterization of two lincomycin-resistance genes, lmrA and lmrB, from Streptomyces lincolnensis 78–11. Mol Microbiol. 1992;6(15):2147–57.
Edgar R, Bibi E. MdfA, an Escherichia coli Multidrug resistance protein with an extraordinarily broad spectrum of drug recognition. J Bacteriol. 1997;179(7):2274–80.
Perreten V, Schwarz FV, Teuber M, Levy SB. Mdt(A), a new efflux protein conferring multiple antibiotic resistance in Lactococcus lactis and Escherichia coli. Antimicrob Agents Chemother. 2001;45(4):1109–14.
Clancy J, Petitpas J, Dib-Hajj F, Yuan W, Cronan M, Kamath AV, et al. Molecular cloning and functional analysis of a novel macrolide-resistance determinant, mefA, from Streptococcus pyogenes. Mol Microbiol. 1996;22(5):867–79.
Clancy J, Dib-Hajj F, Petitpas JW, Yuan W. Cloning and characterization of a novel macrolide efflux gene, mreA, from Streptococcus agalactiae. Antimicrob Agents Chemother. 1997;41(12):2719–23.
Ounissi H, Courvalin P. Nucleotide sequence of the gene ereA encoding the erythromycin esterase in Escherichia coli. Gene. 1985;35(3):271–8.
Allignet J, Loncle V, Mazodier P, el Solh N. Nucleotide sequence of a staphylococcal plasmid gene, vgb, encoding a hydrolase inactivating the B components of virginiamycin-like antibiotics. Plasmid. 1988;20(3):271–5.
Noguchi N, Tamura Y, Katayama J, Narui K. Expression of the mphB gene for macrolide 2′-phosphotransferase II from Escherichia coli in Staphylococcus aureus. FEMS Microbiol Lett. 1998;159(2):337–42.
Achard A, Villers C, Pichereau V, Leclercq R. New lnu(C) gene conferring resistance to lincomycin by nucleotidylation in Streptococcus agalactiae UCN36. Antimicrob Agents Chemother. 2005;49(7):2716–9.
Brisson-Noël A, Courvalin P. Nucleotide sequence of gene linA encoding resistance to lincosamides in Staphylococcus haemolyticus. Gene. 1986;43(3):247–53.
Jung YH, Shin ES, Kim O, Yoo JS, Lee KM, Yoo JI, et al. Characterization of two newly identified genes, vgaD and vatG, conferring resistance to streptogramin A in Enterococcus faecium. Antimicrob Agents Chemother. 2010;54(11):4744–9.
Allignet J, Loncle V, Simenel C, Delepierre M, el Solh N. Sequence of a staphylococcal gene, vat, encoding an acetyltransferase inactivating the A-type compounds of virginiamycin-like antibiotics. Gene. 1993;130(1):91–8.
Long KS, Poehlsgaard J, Kehrenberg C, Schwarz S, Vester B. The Cfr rRNA methyltransferase confers resistance to phenicols, lincosamides, oxazolidinones, pleuromutilins and streptogramin A antibiotics. Antimicrob Agents Chemother. 2006;50(7):2500–5.
Murphy E, Huwyler L. de Freire Bastos Mdo C. Transposon Tn554: complete nucleotide sequence and isolation of transposition-defective and antibiotic-sensitive mutants. EMBO J. 1985;4(12):3357–65.
Gill SR, Fouts DE, Archer GL, Mongodin EF, Deboy RT, Ravel J, et al. Insights on evolution of virulence and resistance from the complete genome analysis of an early methicillin-resistant Staphylococcus aureus strain and a biofilm-producing methicillin-resistant Staphylococcus epidermidis strain. J Bacteriol. 2005;187(7):2426–38.
Lüthje P, Schwarz S. Molecular basis of resistance to macrolides and lincosamides among staphylococci and streptococci from various animal sources collected in the resistance monitoring program BfT-GermVet. Int J Antimicrob Agents. 2007;29(5):528–35.
Szczuka E, Makowska N, Bosacka K, Slotwinska A, Kaznowski A. Molecular basis of resistance to macrolides, lincosamides and streptogramins in Staphylococcus hominis strains isolated from clinical specimens. Folia Microbiol (Praha). 2015. doi:10.1007/s12223-015-0419-6.
Ruzauskas M, Couto N, Kerziene S, Siugzdiniene R, Klimiene I, Virgailis M, et al. Prevalence, species distribution and antimicrobial resistance patterns of methicillin-resistant staphylococci in Lithuanian pet animals. Acta Vet Scand. 2015;57:27.
Kern A, Perreten V. Clinical and molecular features of methicillin-resistant, coagulase-negative staphylococci of pets and horses. J Antimicrob Chemother. 2013:1–11
Zmantar T, Kouidhi B, Miladi H, Bakhrouf A. Detection of macrolide and disinfectant resistance genes in clinical Staphylococcus aureus and coagulase-negative staphylococci. BMC Res Notes. 2011;4:453.
Wu SW, de Lencastre H, Tomasz A. The Staphylococcus aureus transposon Tn551: complete nucleotide sequence and transcriptional analysis of the expression of the erythromycin resistance gene. Microb Drug Resist. 1999;5(1):1–7.
Schwarz S, Cardoso M, Wegener HC. Nucleotide sequence and phylogeny of the tet(L) tetracycline resistance determinant encoded by plasmid pSTE1 from Staphylococcus hyicus. Antimicrob Agents Chemother. 1992;36(3):580–8.
Werckenthin C, Schwarz S, Dyke K. Macrolide-lincosamide-streptogramin B resistance in Staphylococcus lentus results from the integration of part of a transposon into a small plasmid. Antimicrob Agents Chemother. 1996;40(9):2224–5.
Boerlin P, Burnens AP, Frey J, Kuhnert P, Nicolet J. Molecular epidemiology and genetic linkage of macrolide and aminoglycoside resistance in Staphylococcus intermedius of canine origin. Vet Microbiol. 2001;79(2):155–69.
Wang Y, Zhang W, Wang J, Wu C, Shen Z, Fu X, et al. Distribution of the multidrug resistance gene cfr in Staphylococcus species isolates from swine farms in China. Antimicrob Agents Chemother. 2012;56(3):1485–90.
McManus BA, Coleman DC, Deasy EC, Brennan GI, O’Connel B, Monecke S, et al. Comparative genotypes, staphylococcal cassette chromosome mec (SCCmec) genes and antimicrobial resistance amongst Staphylococcus epidermidis and Staphylococcus haemolyticus isolates from infections in humans and companion animals. PLoS ONE. 2015;10(9):e0138079.
Li L, Feng W, Zhang Z, Xue H, Zhao X. Macrolide-lincosamide-streptogramin resistance phenotypes and genotypes of coagulase-positive Staphylococcus aureus and coagulase-negative staphylococcal isolates from bovine mastitis. BMC Vet Res. 2015;11:168.
Entorf M, Fessler AT, Kadlec K, Kaspar H, Mankertz J, Peters T, et al. Tylosin susceptibility of Staphylococci from bovine mastitis. Vet Microbiol. 2014;171(3–4):368–73.
Aslantas O, Oztürk F, Ceylan A. Prevalence and molecular mechanism of macrolide and lincosamide resistance in staphylococci isolated from subclinical bovine mastitis in Turkey. J Vet Med Sci. 2011;73(12):1645–8.
Stegmann R, Perreten V. Antibiotic resistance profile of Staphylococcus rostri, a new species isolated from healthy pigs. Vet Microbiol. 2010;145(1–2):165–71.
Frey Y, Rodriguez JP, Thomann A, Schwendener S, Perreten V. Genetic characterization of antimicrobial resistance in coagulase-negative staphylococci from bovine mastitis milk. J Dairy Sci. 2013;96(4):2247–57.
Horinouchi S, Weisblum B. Nucleotide sequence and functional map of pE194, a plasmid that specifies inducible resistance to macrolide, lincosamide, and streptogramin type B antibodies. J Bacteriol. 1982;150(2):804–14.
Somkuti GA, Solaiman DK, Steinberg DH. Molecular properties of the erythromycin resistance plasmid pPV141 from Staphylococcus chromogenes. Plasmid. 1997;37(2):119–27.
Lodder G, Werckenthin C, Schwarz S, Dyke K. Molecular analysis of naturally occuring ermC-encoding plasmids in staphylococci isolated from animals with and without previous contact with macrolide/lincosamide antibiotics. FEMS Immunol Med Microbiol. 1997;18(1):7–15.
Somkuti GA, Solaiman DK, Steinberg DH. Molecular characterization of the erythromycin resistance plasmid pPV142 from Staphylococcus simulans. FEMS Microbiol Lett. 1998;165(2):281–8.
Lampson BC, Parisi JT. Nucleotide sequence of the constitutive macrolide-lincosamide-streptogramin B resistance plasmid pNE131 from Staphylococcus epidermidis and homologies with Staphylococcus aureus plasmids pE194 and pSN2. J Bacteriol. 1986;167(3):888–92.
Hauschild T, Lüthje P, Schwarz S. Characterization of a novel type of MLSB resistance plasmid from Staphylococcus saprophyticus carrying a constitutively expressed erm(C) gene. VetMicrobiol. 2006;115(1–3):258–63.
de Vries LE, Christensen H, Agerso Y. The diversity of inducible and constitutively expressed erm(C) genes and association to different replicon types in staphylococci plasmids. Mob Genet Elements. 2012;2(2):72–80.
Hauschild T, Schwarz S. Macrolide resistance in Staphylococcus spp. from free living small mammals. Vet Microbiol. 2010;144:2.
Greene RT, Schwarz S. Small antibiotic resistance plasmids in Staphylococcus intermedius. Zentralbl Bakteriol. 1992;276(3):380–9.
Kadlec K, Schwarz S. Identification of a plasmid-borne resistance gene cluster comprising the resistance genes erm(T), dfrK, and tet(L) in a porcine methicillin-resistant Staphylococcus aureus ST398 strain. Antimicrob Agents Chemother. 2010;54(2):915–8.
Matsuoka M, Inoue M, Nakajima Y, Endo Y. New erm Gene in Staphylococcus aureus clinical isolates. Antimicrob Agents Chemother. 2002;46(1):211–5.
Schwarz S, Kehrenberg C, Ojo KK. Staphylococcus sciuri gene erm(33), encoding inducible resistance to macrolides, lincosamides, and streptogramin B antibiotics, is a product of recombination between erm(C) and erm(A). Antimicrob Agents Chemother. 2002;46(11):3621–3.
Bhargava K, Zhang Y. Multi-resistant coagulase-negative Staphylococci in food animals. J Appl Microbiol. 2012;113(5):1027–36.
Acknowledgments
We are grateful to Dr. Sybille Schwendener for helpful advice. This article was written as part of the PhD program of Juliette R.K. Wipf at the Graduate School for Cellular and Biomedical Sciences, University of Bern, Bern, Switzerland, and was financed by Grant 35–539 of the Institute of Veterinary Bacteriology, Bern, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Bacteriology
Rights and permissions
About this article
Cite this article
Wipf, J.R.K., Perreten, V. Discovery of Novel MLSB Resistance Methylase Genes and Their Associated Genetic Elements in Staphylococci. Curr Clin Micro Rpt 3, 42–52 (2016). https://doi.org/10.1007/s40588-016-0030-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-016-0030-x