Abstract
Purpose of Review
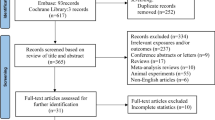
We reviewed and summarized the epidemiological evidence for the influence that pre- and postnatal exposures to perfluoroalkyl substances (PFASs) may have on health outcomes in offspring, with a particular focus on birth outcomes and postnatal growth, immunomodulatory effects and neurodevelopment.
Recent Findings
PFASs are persistent organic pollutants that have been widely produced and used in a range of commercial products since the 1950s. Human exposures to PFASs are nearly ubiquitous globally, but studies that addressed potential health effects of PFASs have only begun to accumulate in recent years. Animal studies suggest adverse effects resulting from developmental encompasses prenatal exposures to PFASs. In humans, the developing fetus is exposed to PFASs via active or passive placenta transfer, while newborns might be exposed via breastfeeding or PFAS in the home environment.
Summary
Overall, epidemiological findings are consistent and suggest possible associations with fetal and postnatal growth and immune function, while the findings on neurodevelopmental endpoints to date are rather inconclusive. Methodological challenges and future directions for PFASs-focused research are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perfluoroalkyl substances (PFASs) are a group of synthetic fluorine-containing compounds that exhibit unique surfactant properties and can be used as water and oil repellents. Large volumes of fluorinated organic compounds have been produced since the 1950s to treat paper, clothing, carpets, food packing material and kitchenware [1]. PFASs are resistant to environmental degradation and biotransformation with biological half-lives in humans estimated as 3–5 years for the most commonly used PFASs [1, 2]. Non-occupational PFASs exposures might occur from drinking contaminated water, ingestion of food or food packaging materials that contained PFASs, or from indoor air and household environments [3]. Also, some PFASs have been unfortunately exposed to high levels of PFAS due to point source pollutions, i.e. contamination of drinking water sources due to industrial releases [4] or use during military or firefighting training [5]. Fetuses in development are exposed to PFASs because these chemicals cross the placental barrier actively or passively [6]. Placental passage of PFASs depends on the carbon length, functional group (such as a sulfonate group), linear or branched isomers and their binding affinity to blood proteins like fatty acid binding protein [6, 7]. Young children have been found to have peak PFASs concentrations before 2 years of age [8] possibly due to cumulative exposure via breastfeeding [9] or ingestion of house dust from the home environment leading to high daily intakes [8]. In the U.S. general population, some PFASs have been detected in >99% of all serum samples from the 2009–2010 National Health and Nutrition Examination Survey (NHANES) [10]. Concentrations of perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA), the two most widely detected PFASs, have decreased in some countries following a drop in production since the year 2000 [11, 12], but exposure to other short-chain and also some long-chain PFASs are increasing in many countries [13]. In addition, some new fluorinated compounds that are used to replace PFOS have also recently been detected in biota [14,15,16].
Because they are so ubiquitously found in humans, these chemicals have caused tremendous concerns regarding potential health effects. Experimental studies have indicated rather strong effects during development for exposures to PFAS [17]. A goal of this short review is to provide an overview and summary of recent epidemiological findings for developmental and early childhood health effects from PFASs exposure. We focus on three outcomes of greatest interest, specifically fetal and postnatal growth, immunomodulatory effects and neurodevelopment, for which a sufficiently large number of studies has already been conducted. We also summarize the proposed biological mechanisms underlying findings, and discuss methodologic challenges that human studies face.
Fetal and Postnatal Growth
We reviewed findings from 24 studies that investigated the possible effects of prenatal PFASs exposure on fetal and postnatal growth, most of which were prospective cohort studies and five relied on cross-sectional data (see Table 1). We restricted this review to studies that utilized a sufficiently large sample to study adverse birth outcomes (i.e. more than 100 births).
In a cross-sectional study conducted in Baltimore, cord serum PFOS and PFOA were inversely associated with birth weight, ponderal index and head circumference [20]. In the Danish National Birth Cohort (DNBC), early pregnancy PFOA, but not PFOS, was inversely associated with birth weight in a large sub-sample (n = 1400) [24]. Also, in the same population, only PFOA was associated with birth length and abdominal circumference [25]. On the other hand, the Hokkaido study in Japan reported inverse associations for very low prenatal PFOS levels, but not for PFOA, and reduced birth weight was more apparent among female infants [32, 33]. A Chinese study reported associations for PFOA and reduced birth weight and length in a community with high environmental pollution from electronic waste recycling [30]. In the large Aarhus Birth Cohort in Denmark, 16 PFASs were examined in nulliparous women, but no association between PFASs and birth weight or other fetal growth indices were observed [27]. Interestingly, this Danish cohort recruited women much later (2008–2013) that the DNBC (1996–2002) and levels of PFOA and PFOS in maternal serum were much lower at this point in time. In a Colorado study, infants in the highest tertile of maternal PFOA, PFNA and PFHxS exposures had lower weight and adiposity (percent fat mass) at birth compared to infants in the lowest tertile of exposures. Additionally, the study reported inverse associations between maternal fasting glucose concentrations during pregnancy and PFASs, suggesting that reduced availability of maternal glucose reaching the fetus could be a potential mechanism linking PFAS exposure to reduced weight and adiposity at birth. [22]. In contrast, several studies did not find significant associations between PFASs and these birth outcomes [18, 19, 28, 29, 34]. Also, two studies from the C8 Health Project, utilizing modeled PFOA levels during pregnancy instead of measured biomarkers, did not show association between PFOA and birth weight [43, 44]. Participants in the C8 Health project had abnormally high PFOA level because of industrial PFOA releases that contaminated the drinking water. Few studies have reported on associations between PFASs and low birth weight (LBW) possibly due to insufficient sample size. Others did not report any associations [24, 29, 31, 44].
Considering postnatal in addition to prenatal growth, a study among British girls reported an inverse dose-response between prenatal exposure to PFOS, PFOA and PFHxS and birth weight; however, at 20 months of age, girls born to mothers in the upper tertile of PFOS concentrations were 580 g (95% CI: 301, 858 g) heavier than those in the lower tertile [41]. The Taiwan Birth Panel Study also reported inverse association of cord plasma PFOS with birth weight and head circumference and SGA [35], but in a follow up at 60–108 months of age, PFOS showed positive association with body mass index (BMI) among girls [42]. In contrast, a study from the DNBC observed that prenatal PFOS and PFOA reduced the weight of offspring at ages 5 and 12 months [38], but there was no association with anthropometry at 7 years of age [40]. The HOME birth cohort study in Cincinnati reported associations between maternal PFOA, but not PFOS, PFNA, and PFHxS, with higher BMI gains from 2 to 8 years and greater adiposity at age 8 years [36]. The Project Viva birth cohort in Massachusetts used anthropometric and dual X-ray absorptiometry to measure fat mass, fat-free mass and trunk fat mass indexes and associated maternal prenatal PFASs levels with higher BMI and a total fat mass index in mid-childhood among girls [37]. Also, they found associations of early-pregnancy PFOS and PFNA levels with reduced birth weight-for-gestational-age z scores, and adjusting for markers of pregnancy hemodynamics (glomerular filtration rate and plasma albumin) as potential confounders did not materially impact the associations observed [23]. A Danish study examined prenatal exposure to PFASs and risk of being overweight at 20 years of age and found that only maternal PFOA was positively associated with being overweight or obesity and higher waist circumference among female, but not male offspring [39]. The study also found that prenatal PFOA was positively correlated with serum insulin and negatively with leptin in girls [39].
Taken together, despite some inconsistency, a preponderance of studies suggested that PFASs impact birth outcomes and pre- and postnatal growth. Further studies with larger sample sizes and longer follow-up for longitudinal observations are still needed to re-evaluate these findings.
Immunomodulatory Effects
Excluding studies conducted in occupational settings and in adults, 22 epidemiological studies remained that examined the potential immunomodulatory effects of exposure to PFASs in children and adolescents (Table 2). Most studies used a prospective design, and only five studies were cross-sectional. We reviewed the immune outcomes related to immunosuppression, hypersensitivity/autoimmunity and other measures of immune function.
Immunosuppression
Seven epidemiological studies have investigated associations between exposure to PFASs and vaccine antibody response, including studies relying on NHANES [48], and birth cohorts from the Faroe Islands [51, 53,54,55] and Norway [58, 59]. In the birth cohorts, higher maternal concentrations of PFASs during pregnancy were associated with lower anti-vaccine antibody levels for rubella [58], diphtheria [51] and tetanus [55] in their children at ages 3 to 5 years. No consistent associations were found however between prenatal concentrations of PFASs and vaccine antibody levels for influenza and measles among the children [58]. Childhood and infancy exposure to PFASs has also been shown to decrease vaccine antibody levels for diphtheria and tetanus in children aged 5 to 13 years in longitudinal studies from the Faroe Islands [51, 53,54,55]. Finally, cross-sectional measures of PFASs and rubella and mumps titers in adolescents aged 12 to 19 years in NHANES showed lower levels for these antibodies in relation to higher PFAS concentrations [48].
Five studies assessed infections as outcomes and markers of immunosuppression. A study of a subsample of children enrolled in the DNBC did not find associations between prenatal PFOS and PFOA and hospitalizations due to infections in early childhood [49], except when stratifying by the child’s gender. Higher hospitalization rates for infections among girls but lower rates among boys were observed with higher prenatal PFASs exposures. In a prospective birth cohort study in Japan, no associations were reported for infectious diseases, including pneumonia, bronchitis, chicken pox and other viral infections, during the first 18 months of life [61]. Three studies, however, did find PFASs to be related to infections. Higher maternal PFOA and PFOS concentrations were found to be associated with a greater proportion of days with fever and an increased number of episodes of fever and coughing and fever and nasal discharge in Danish children aged 1 to 3 years [50]. In Norway, positive associations between maternal PFOA and PFNA concentrations and the number of episodes of common cold and between PFOA and PFHxS and the number of episodes of gastroenteritis in offspring were reported [58], but this group did not see associations with otitis media. Finally, the Hokkaido study associated higher maternal PFASs concentrations with an increased prevalence of infectious diseases in children, including otitis media, pneumonia, varicella and respiratory virus infections, in children up to 4 years of age [64], specifically girls.
Hypersensitivity/Autoimmunity-Related Outcomes
Thirteen studies reported on autoimmunity/hypersensitivity endpoints in eight prospective birth cohorts from Canada [45], Japan [61, 62, 63], Taiwan [65], Faroe Islands [57], Greenland, Ukraine [60], Norway [58] and from four cross-sectional studies in Taiwan [66] and the USA (NHANES) [46,47,48]. Higher IgE levels in 2-year-old Taiwanese children were observed with higher cord blood PFOS and PFOA concentrations, but no associations were found for atopic dermatitis at the same age [65]. Contrary to this study, decreased IgE levels were reported with higher maternal PFOA concentrations in 18-month-old Japanese children, and no associations were observed between PFASs and food allergy, eczema or wheezing [61]. The Canadian MIREC birth cohort also found no association between 1st trimester pregnancy PFASs concentrations and cord-blood IgE levels [45]. Similarly, no associations were found between maternal prenatal PFASs concentrations and eczema/itchiness, wheeze, atopic eczema or asthma in a small sample (n = 99) of Norwegian children ages 1 to 3 years [58]. The Hokkaido birth cohort also observed lower odds of eczema and total allergic diseases in relation to higher prenatal PFASs concentrations in children aged 12 to 24 months; however, these effect estimates were only formally statistically significant in girls [62]. The same cohort reported inverse associations between prenatal PFASs concentrations (mainly long-chain PFASs) and total allergic diseases and eczema for the children at 4 years of age [63]. A Ukrainian study also found inverse associations between maternal PFASs concentrations and symptoms of wheeze in 5–9-year-old children [60]. Only one prospective study investigated both prenatal and childhood exposures to PFASs and hypersensitivity outcomes, and reported increased odds of asthma at ages 5 and 13 with higher levels of PFASs at age 5, but only among children not vaccinated for measles, mumps and rubella. The same study found no associations between maternal prenatal PFASs concentrations and IgE levels, childhood asthma or allergic diseases [57] at ages 5 and 13.
A cross-sectional NHANES based study reported that higher PFOA levels were associated with elevated odds of asthma, whereas for PFOS there were no associations with both asthma and wheezing [46]. In NHANES, another cross-sectional study found no associations between concurrent PFASs exposures and current allergic conditions [48]. However, concurrent PFNA concentrations were inversely associated with food sensitization (IgE ≥ 0.35 kU/L) in NHANES participants, and serum PFOA, PFOS and PFHxS concentrations were associated with higher odds of self-reported food allergies [47]. Positive associations between concurrent PFASs concentrations and asthma, asthma severity score and IgE concentrations were reported for children ages 10–15 years enrolled in the Taiwanese Genetic and Biomarker study for Childhood Asthma (GBCA) [66]. Finally, a very small study (n = 38) that investigated IgM and IgG autoantibodies specific to neural and non-neural antigens reported a negative association between prenatal PFOS concentrations and anti-actin IgG antibodies at 7 years of age [52].
Other measures of Immune Function
Five studies measured cytokines levels and white blood cell counts as markers of immune function. In the Taiwanese GBCA study positive associations between concurrent levels of PFASs and absolute eosinophil counts and eosinophilic cationic protein concentrations were seen in children 10–15 years of age [66]. However, this result was not reproduced in a small study of 54 children from the Faroe Islands where no association was found between prenatal and child 18-month PFASs concentrations and absolute eosinophil counts, nor with other white blood cell counts [56]. Only PFAS concentrations at 5 years were positively associated with basophil concentrations at the same age. No other associations were reported between PFAS levels and lymphocyte counts. Another investigation in the Taiwanese GBCA reported positive associations between concurrent serum PFAS concentrations and levels of T helper 2 cytokines [interleukin-4 (IL-4) and IL-5] and negative associations with T helper 1 cytokines (interferon-γ and IL-2) [67]. Finally, umbilical cord blood thymic stromal lymphopoietin and interleukin-33 levels were not associated with 1st trimester pregnancy PFASs concentrations [45] in the Canadian MIREC study, whereas transcriptomics profiling of neonatal cord blood identified a set of differentially expressed genes as being associated with both maternal PFASs concentrations and common cold episodes or rubella titers [59] in a Norwegian study.
Overall, PFAS exposures appear to modulate immune responses in children, with the evidence being most conclusive for an immunosuppressive effect, as indicated by decreased response to vaccines. Most studies investigating immunosuppressive effects reported reduced immune responses to vaccines and some studies reported increased rates of infection in early childhood. Both prenatal and childhood exposures to PFASs appear to modulate immune function. The strongest evidence comes from studies that took advantage of vaccination programs and measured the response to vaccine boosters. On the other hand, findings relating PFASs to outcomes related to hypersensitivity and autoimmunity were rather inconsistent. Other immune function-related outcome measures such as cytokine and chemokine levels, and white blood cell counts also did not produce consistent results. However, differences in studied endpoints, windows of exposure, age at outcomes evaluation and potential for outcome misclassification may explain some of the inconsistency in findings.
Neurodevelopmental Effects
The 21 epidemiological studies that examined the possible impacts of PFASs on neurodevelopment we reviewed (Table 3) were mostly prospective cohorts employing one-time measures of prenatal PFASs concentrations in maternal serum or plasma or in cord blood. Three cross-sectional studies evaluated associations between attention deficit/hyperactivity disorder (ADHD) and serum level of PFASs in children. The majority of studies were conducted in Northern Europe, USA and East Asia.
Studies that evaluated neurodevelopmental indicators in early infancy (below 2 years of age) reported inconsistent findings. The DNBC was the largest study that found no apparent associations between prenatal PFOS and PFOA concentrations and development milestones reported by the mothers for 1400 newborn at 6 and 18 months [26]. In the Hokkaido study, girls prenatally exposed to PFOA had lower mental developmental indices on the Bayley Scales (BSID II) reported by parents at 6 but not at 18 months [69]. This study also reported no associations for boys for any mental or psychomotor development measure in BSID II at both 6 and 18 months. The Taiwanese birth panel study found some indication for prenatal PFOS exposure affecting the gross motor development domain at 2 years of age, but no associations for PFOS and PFOA with cognitive, language, social and self-help domains [70]. A Cincinnati study conducted in areas with relatively high levels of PFOA pollutants in drinking water due to industrial contamination found a 10-fold increase in PFOA levels to be associated with elevated odds of hypotonic phenotypes characterized by presence of an increased muscle tone and higher scores of lethargy and non-optimal reflexes in young infants from the Neonatal Intensive Care Unit Network Scale (NNNS) [68]. In this cohort, infants with hypotonic phenotypes had lower psychomotor development and lower externalizing scores at 2–3 years of age [88]. A small Dutch cohort examined 76 children 18 months of age and found no associations between prenatal PFAS exposure and ADHD scores, but externalizing behavior in boys appeared to be related to prenatal PFOA level [86]. Lastly, the Norwegian birth cohort also found no associations between breastmilk levels of PFOS and PFOA and early neuropsychological development at 12 and 24 months [87].
A larger number of studies focused on neurobehavioral and neuropsychological endpoints in later childhood typically assessed at age 4 to 18. Three cross-sectional studies [83, 84, 85], including one using NHANES, reported higher serum levels of some PFASs to be positively correlated with impulsivity and ADHD in school-aged children. However, these findings were not corroborated in most longitudinal studies that evaluated prenatal PFASs exposures and an ADHD diagnosis [76, 81, 73], or parent- or teacher-reported ADHD symptoms or behavioral scores [72, 74•, 77] during childhood. Only in the INUENDO cohort that combined data from Greenland, Kharkiv (Ukraine) and Warsaw (Poland) found that prenatal exposure to PFOS and PFOA had a small to moderate size effect on hyperactive behavior in children ages 5–9 years; estimated effects were strongest in Greenland where exposure contrasts were the largest among these countries [75]. Two studies evaluating early exposure and ADHD symptoms later in childhood were conducted in the Faroe Islands and the USA. High serum PFAS levels at age 5 among Faroese children were associated with behavioral problems at age 7 [74•], and the C8 Health Study found PFASs levels in children aged 2 to 8 years to be related to improved executive function and ADHD-like problems among boys, but also saw adverse outcomes among girls assessed in the follow up about 3–4 years after exposure [71].
A Danish study reported no consistent association between six types of PFASs and childhood autism [73], while for a cohort in Cincinnati, high levels of PFOA were related with fewer autistic symptoms [79]. The Cincinnati cohort, however, also found that prenatal PFOS, but not PFOA, was associated with decreased executive functions at age 5 and 8 in the same population [80]. Two studies reported inconsistent findings regarding prenatal PFASs exposure and child IQ scores. The C8 Health Study examined 320 children aged 6–12 years and reported that geospatially estimated (not measured) in-utero PFOA levels were associated with higher full-scale IQ [78]. In Taiwan, prenatal perfluoroundecanoic acid (PFUnDA) was associated with lower performance IQ scores in children at age 5, and at further follow-up to age 8, seven types of prenatal PFASs appeared to be associated with a reduction of child IQ scores [82]. No apparent associations were found for high levels of PFOA exposure in childhood on math skills, language, memory and learning and visual-spatial processing reported in the C8 study [78]. A Danish study also found no association between prenatal exposure to PFOA and PFOS and the mean score of standardized written exams in 9th grade [81]. Two studies found no associations between prenatal PFOA and PFOS exposure and parent-reported child motor development [72, 75]. Another Danish study observed a dose-response increase in risks for cerebral palsy, a severe movement and posture disorder, with prenatal exposure to PFASs [73]. Finally, in yet another Danish cohort study, no association was seen between prenatal levels of PFOA and PFOS and subsequent diagnosis and treatment of depression up to 22 years of follow-up [81].
Overall, evidence is mixed regarding neurodevelopmental associations of PFASs exposures. Several key issues may explain the inconsistencies. First, various instruments and methods have been employed to evaluate neurodevelopmental endpoints at different ages. While this could be a strength because neurodevelopmental trajectories are complex and different measures provide comprehensive assessment of various neuropsychological functional domains in development, the importance of measurement error associated with various tools is difficult to assess. Secondly, exposure levels, ranges and PFAS mixture composition differed between study populations. Several reports from the C8 Health Study [71, 78, 84] relied on volunteers recruited from communities with PFOA levels about 10-fold higher than the values in other population-based cohorts; also, several long-chain PFASs were more frequently detected in samples from east Asia [82]. Results may vary across populations if there are dose or exposure level- and/or mixture-dependent effects of PFASs on neurodevelopment. Third, many studies had a relatively small sample size and insufficient statistical power may prevent researchers from being able to detect exposure effects, especially if these ubiquitous exposures have effects on a specific domains of neurodevelopment or affect small subgroups. Finally, most studies have focused on behavioral disorders or ADHD symptoms in childhood only. Endpoints that represent more severe neurological conditions, i.e. cerebral palsy [89] and long-term mental health conditions like depression [81], have only been evaluated once and additional studies are needed.
Discussion
This review of human epidemiological studies examining health effects of PFASs shows accumulated evidence that early-life exposure to PFASs affects fetal and postnatal growth and the immune system, while findings for neurodevelopmental endpoints are not conclusive yet. Next, we discuss potential mechanisms of action, challenges of PFASs research, and future directions for research that may strengthen the plausibility of findings regarding potential health effects of PFASs in humans.
Potential Mechanisms of Action
In terms of potential mechanisms of action for PFASs experimental studies have provided the first clues. For instance, many PFAS activate the peroxisome proliferator-activated receptor alpha and gamma (PPAR-α and γ) and activation of the PPAR-α modulates lipid and glucose homeostasis, cell proliferation and differentiation, and inflammation [90, 91]. PPAR-α knockout mice exposed to PFOA suggested that pathways other than PPAR-α can also be targeted, affecting hepatic peroxisome proliferation, lymphoid organ weight and antibody synthesis [92]. Rather compelling evidence from animal studies linked PFASs to suppression of the primary antibody response, i.e. the antigen-specific IgM antibody production to T-cell-specific antigens in mice [93,96,97,96]. Regarding metabolic effects, strong inverse associations between maternal PFOS with triglycerides, essential fatty acids and omega 3 and 6 fatty acids during pregnancy have been described [33]. Studies also found that prenatal exposure to PFASs is associated with glucocorticoids (cortisol and cortisone) and reproductive hormone (DHEA, progesterone, estradiol and testosterone) levels [97•, 98], suggesting that PFASs may reprogram the endocrine system and shift steroidogenesis. Mechanisms potentially involved in the neurobehavioral effects of PFASs exposures include influences on calcium homeostasis, protein kinase C, synaptic plasticity, cellular differentiation or via the thyroid hormone system [17, 24, 99]. PFASs affect neuronal plasticity and the exposed animals had increased levels of the proteins CaMKII, GAP-43, synaptophysin and Tau, all of which are involved in neuronal growth and synaptogenesis [100]. In vitro models suggested that PFASs can directly influence neuronal differentiation [101]. PFASs can compete with T4 for binding to transthyretin, a main carrier protein of TH in mammals [102], thus increasing thyroid-stimulating hormone (TSH) and decreasing free thyroxine (fT4) [103,104,105]. Thyroid hormones transferred from the mother to the embryo and fetuses are critical for normal brain development [106], and TH deficiency during gestation may cause cognitive and/or mental disorders [107,108,109,110,111].
General Methodological Challenges in PFAS Research
PFASs are nearly ubiquitously detected in humans, making comparisons challenging since no or few study participants are truly unexposed to these chemicals. Given the lack of an unexposed control group, reference exposure levels vary from study to study making the comparison of results across populations difficult. Additionally, non-monotonic relationships are likely with regard to endocrine-disrupting chemicals such as PFAS [112]. Thus, assessing non-linear exposure response is important and recommended when statistically modeling these associations; however, such analyses require sufficient sample size and exposure ranges.
Another limitation pertains to the lack of consideration of toxicity of PFASs in terms of a mixture of compounds. Very few of the previous studies considered this issue [51, 53, 54, 56, 60]; While some investigated health effects for summary measures of PFASs, this prevents us from investigating potential interactive effects of certain compounds within each mixture, and to assess marginal effects in the presence of mixtures of toxicants. Other persistent organic pollutants (POPs) like polybrominated diphenyl ethers (PBDE) and non-persistent pollutants such as phthalates and bisphenol A (BPA) have also been shown to influence immune, metabolic and cognitive or behavioral function [113, 114]. These compounds may exert their effects through mechanisms in common with PFASs and there is an urgent need to examine the potential effects of these chemical families simultaneously. The inception of new methodological approaches dealing with mixtures of chemicals is expected to improve future investigations [115, 116].
In the adult populations, the main exposure pathways to PFASs have been linked to the dietary intake of contaminated food and water [117]. Indoor exposures to PFAS are also a significant source of exposure, involving ingestion of dust, dirt particles and dermal contact with PFAS-treated products or their precursors [3, 118]. The half-lives of PFASs (PFOA 3.5 years; PFNA 1.5; PFDA 4.2; PFUnDA 4.4; PFHxS 7.1; PFOS 4.8) have considerable effects on the elimination rates of these compounds through the human body [119, 120]. Studies have also shown that shorter-carbon-chain PFAS such as PFBS were generally excreted more rapidly than long-chain PFASs [121]. In an experimental study that analyzed 21 PFASs in autopsy tissue samples (i.e. brain, liver, lung, bone and kidney), PFASs were detected in all human tissue samples (n = 99) in varying concentrations depending on the deposition site and the PFASs [122].
Prospective studies that evaluated effects of prenatal exposure to PFASs have utilized different pregnancy time-points, varying from the 1st trimester to delivery (cord blood). The timing of exposure can play an important role in the toxicity of PFASs given the different developmental timing for organ systems. Correlations for PFOA and PFOS measures between early- and late-pregnancy serum samples were found to be high [24], but other physiological factors such as maternal blood volume expansion and metabolic changes during pregnancy could add uncertainty to exposure measures [123]. Moreover, the transplacental transfer from the mother to the fetus might vary for different compounds [124]. All of these aspects can induce exposure misclassification or measurement errors in terms of the dose of PFASs received in utero. Other sources of measurement error might include differences in samples collection and processing as well as some related to the chemical analysis [125]. If measurement errors are random and non-differential, effect estimates might be biased towards the null. But, the bias could also go in either direction, especially in small sample sizes.
Except for studies conducted in communities exposed to known sources of pollutions, a majority of cohort studies included mothers and children from the general populations where exposures to PFASs occur via multiple and unknown sources. This leaves the possibility for uncontrolled confounding by some unmeasured factors related to some sources. When using biomarkers of PFASs, physiological factors that affect accumulation or excretions of PFASs should also be considered. Lower glomerular filtration rate (GFR) in mid- or late pregnancy have been suggested to be a possible confounding factor [126]; mothers with lower GFR might possibly have a lower rate of PFASs excretion, and a lower GFR in pregnancy has been linked with adverse birth outcomes [126]. Similarly, parity and breastfeeding duration has been shown to strongly impact early life concentrations of PFASs [127, 128], whereas breastfeeding is also known to influence measures of immune and metabolic function as well as behavioral and cognitive outcomes. Controlling for breastfeeding duration is recommended when investigating health effects of postnatal PFASs exposure, whereas parity should be considered when investigating both pre- and postnatal exposures.
Finally, self-selection bias may occur if participants realized and were concerned about a source of PFASs exposure during study enrollment. This could be a possibility for the C8 health study which was established as part of a lawsuit settlement. Those community members who were affected or had concerns about their health associated with PFOA exposure might have been more likely to participate [4]. This is usually a minor concern in study of general populations since most are likely to be unaware of their exposure status. However, PFASs have been suggested to affect reproductive endpoints such as semen quality in men, reproductive hormones in both sexes and possibly also impair fertility [129–132]. Thus, those most highly exposed might possibly have a lower chance of being enrolled in a pregnancy cohort. Moreover, prenatal PFASs exposures may increase risk of miscarriages [133, 134]. A simulation study demonstrated that “live-birth selection bias” may occur in birth cohort analyses if PFASs cause fetal losses and only children who survive and are born alive are studied. In such a scenario, the true effect estimates might be biased towards the null or in a negative direction [135•].
Future Directions of Research
Widespread of PFASs have caused tremendous concerns regarding associated health effects. Biomonitoring of the exposures to understand the changes in exposure levels over time, and research that investigates potential health consequences of PFAS exposures should be continued. Several reproductive and childhood health consequences from PFAS exposure can be considered well-established. For instance, the National Toxicology Program issued a systematic review of human and experimental studies pointing out the immunotoxicity of PFOA and PFOS [136]. Future research that follows these offspring may be able to evaluate whether the effects observed on growth or immune system function persist into older ages. Incorporation of recent advances in causal inference methods to adjust for potential selection bias and time varying confounding is also a future area for methodologic advancement. Similar future studies focused on interactions between PFASs and other genetic or environmental stressors are needed. Mechanistic pathway studies that may explain the observed associations are of interest since mechanisms of action are still poorly understood. With the growing body of literature on PFAS health effects, pooled and meta-analyses might be possible and would increase statistical power to address the potential toxicity of these compounds. Finally, some fluorinated compounds that have recently replaced PFOS and PFOA in manufacturing processes and that are currently detected in humans and the biota [16] deserve attention and need to be considered in future studies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Houde M, et al. Biological monitoring of polyfluoroalkyl substances: a review. Environ Sci Technol. 2006;40(11):3463–73.
Lau C, et al. Perfluoroalkyl acids: a review of monitoring and toxicological findings. Toxicol Sci: Off J Soc Toxicol. 2007;99(2):366–94.
D'eon JC, Mabury SA. Is indirect exposure a significant contributor to the burden of perfluorinated acids observed in humans? Environ Sci Technol. 2011;45(19):7974–84.
Frisbee SJ, et al. The C8 health project: design, methods, and participants. Environ Health Perspect. 2009;117(12):1873–82.
Hu XC, et al. Detection of poly- and Perfluoroalkyl substances (PFASs) in U.S. drinking water linked to industrial sites, military fire training areas, and wastewater treatment plants. Environ Sci Technol Lett. 2016;3(10):344–50.
Gutzkow KB, et al. Placental transfer of perfluorinated compounds is selective–a Norwegian mother and child sub-cohort study. Int J Hyg Environ Health. 2012;215(2):216–9.
Kim S, et al. Trans-placental transfer of thirteen perfluorinated compounds and relationswith fetal thyroid hormones. Environ Sci Technol. 2011;45(17):7465–72.
Winkens K, Vestergren R, Berger U. Cousins IT early life exposure to per- and polyfluoroalkyl substances (PFASs): a critical review. Emerg Contam. 2017;3(2):55–68.
Brantsater AL, et al. Determinants of plasma concentrations of perfluoroalkyl substances in pregnant Norwegian women. Environ Int. 2013;54:74–84.
CDC. Centers for Disease Control and Prevention: National Health and Nutrition Examination Survey. 2009–2010 Data Documentation, Codebook, and Frequencies. Polyfluoroalkyl Chemicals (PFC_F). 2013. Available: http://wwwn.cdc.gov/nchs/nhanes/2009-2010/PFC_F.htm. Accessed 17 Oct 2017.
Kato K, et al. Trends in exposure to polyfluoroalkyl chemicals in the U.S. population: 1999-2008. Environ Sci Technol. 2011;45(19):8037–45.
Butenhoff JL, Olsen GW, Pfahles-Hutchens A. The applicability of biomonitoring data for perfluorooctanesulfonate to the environmental public health continuum. Environ Health Perspect. 2006;114(11):1776–82.
Glynn A, et al. Perfluorinated alkyl acids in blood serum from primiparous women in Sweden: serial sampling during pregnancy and nursing, and temporal trends 1996-2010. Environ Sci Technol. 2012;46(16):9071–9.
Wang Z, et al. Comparative assessment of the environmental hazards of and exposure to perfluoroalkyl phosphonic and phosphinic acids (PFPAs and PFPiAs): current knowledge, gaps, challenges and research needs. Environ Int. 2016;89-90:235–47.
Chu S, et al. A new fluorinated surfactant contaminant in biota: Perfluorobutane sulfonamide in several fish species. Environ Sci Technol. 2016;50(2):669–75.
Gebbink WA, van Asseldonk L, van Leeuwen SPJ. Presence of emerging per- and Polyfluoroalkyl substances (PFASs) in river and DrinkingWater near a Fluorochemical production Plant in the Netherlands. Environ Sci Technol. 2017;51(19):11057–65.
Lau C, Butenhoff JL, Rogers JM. The developmental toxicity of perfluoroalkyl acids and their derivatives. Toxicol Appl Pharmacol. 2004;198(2):231–41.
Monroy R, et al. Serum levels of perfluoroalkyl compounds in human maternal and umbilical cord blood samples. Environ Res. 2008;108(1):56–62.
Hamm MP, et al. Maternal exposure to perfluorinated acids and fetal growth. J Expo Sci Environ Epidemiol. 2010;20(7):589–97.
Apelberg BJ, et al. Cord serum concentrations of perfluorooctane sulfonate (PFOS) and perfluorooctanoate (PFOA) in relation to weight and size at birth. Environ Health Perspect. 2007;115(11):1670–6.
Stein CR, Savitz DA, Dougan M. Serum levels of perfluorooctanoic acid and perfluorooctane sulfonate and pregnancy outcome. Am J Epidemiol. 2009;170(7):837–46.
Starling AP, et al. Perfluoroalkyl substances during pregnancy and offspring weight and adiposity at birth: examining mediation by maternal fasting glucose in the healthy start study. Environ Health Perspect. 2017;125(6):067016.
Sagiv SK, Rifas-Shiman SL, Fleisch AF, Webster TF, Calafat AM, Ye X, et al. Early pregnancy perfluoroalkyl substance plasma concentrations and birth outcomes in project viva: confounded by pregnancy hemodynamics? Am J Epidemiol. 2017; https://doi.org/10.1093/aje/kwx332.
Fei C, et al. Perfluorinated chemicals and fetal growth: a study within the Danish national birth cohort. Environ Health Perspect. 2007;115(11):1677–82.
Fei C, et al. Fetal growth indicators and perfluorinated chemicals: a study in the Danish National Birth Cohort. Am J Epidemiol. 2008;168(1):66–72.
Fei C, et al. Prenatal exposure to perfluorooctanoate (PFOA) and perfluorooctanesulfonate (PFOS) and maternally reported developmental milestones in infancy. Environ Health Perspect. 2008;116(10):1391–5.
Bach CC, et al. Perfluoroalkyl acids in maternal serum and indices of fetal growth: the Aarhus birth cohort. Environ Health Perspect. 2016;124(6):848–54.
Whitworth KW, et al. Perfluorinated compounds in relation to birth weight in the Norwegian mother and child cohort study. Am J Epidemiol. 2012;175(12):1209–16.
Manzano-Salgado CB, et al. Prenatal exposure to perfluoroalkyl substances and birth outcomes in a Spanish birth cohort. Environ Int. 2017;108:278–84.
Wu KS, et al. Association between maternal exposure to perfluorooctanoic acid (PFOA) from electronic waste recycling and neonatal health outcomes. Environ Int. 2012;48:1–8.
Li M, et al. Isomers of perfluorooctanesulfonate (PFOS) in cord serum and birth outcomes in China: Guangzhou birth cohort study. Environ Int. 2017;102:1–8.
Washino N, et al. Correlations between prenatal exposure to Perfluorinated chemicals and reduced fetal growth. Environ Health Perspect. 2009;117(4):660–7.
Kishi R, et al. The Association of Prenatal Exposure to Perfluorinated chemicals with maternal essential and long-chain polyunsaturated fatty acids during pregnancy and the birth weight of their offspring: the Hokkaido study. Environ Health Perspect. 2015;123(10):1038–45.
Lee ES, Han S, Oh JE. Association between perfluorinated compound concentrations in cord serum and birth weight using multiple regression models. Reprod Toxicol. 2016;59:53–9.
Chen MH, et al. Perfluorinated compounds in umbilical cord blood and adverse birth outcomes. PLoS One. 2012;7(8):e42474.
Braun JM, et al. Prenatal perfluoroalkyl substance exposure and child adiposity at 8 years of age: the HOME study. Obesity (Silver Spring). 2016;24(1):231–7.
Mora AM, et al. Prenatal exposure to Perfluoroalkyl substances and adiposity in early and mid-childhood. Environ Health Perspect. 2017;125(3):467–73.
Andersen CS, et al. Prenatal exposures to perfluorinated chemicals and anthropometric measures in infancy. Am J Epidemiol. 2010;172(11):1230–7.
Halldorsson TI, et al. Prenatal exposure to perfluorooctanoate and risk of overweight at 20 years of age: a prospective cohort study. Environ Health Perspect. 2012;120(5):668–73.
Andersen CS, et al. Prenatal exposures to perfluorinated chemicals and anthropometry at 7 years of age. Am J Epidemiol. 2013;178(6):921–7.
Maisonet M, et al. Maternal concentrations of polyfluoroalkyl compounds during pregnancy and fetal and postnatal growth in British girls. Environ Health Perspect. 2012;120(10):1432–7.
Chen MH, et al. The impact of prenatal perfluoroalkyl substances exposure on neonatal and child growth. Sci Total Environ. 2017;607-608:669–75.
Savitz DA, et al. Perfluorooctanoic acid exposure and pregnancy outcome in a highly exposed community. Epidemiology. 2012;23(3):386–92.
Savitz DA, et al. Relationship of perfluorooctanoic acid exposure to pregnancy outcome based on birth records in the mid-Ohio Valley. Environ Health Perspect. 2012;120(8):1201–7.
Ashley-Martin J, et al. Prenatal exposure to phthalates, bisphenol a and perfluoroalkyl substances and cord blood levels of IgE, TSLP and IL-33. Environ Res. 2015;140:360–8.
Humblet O, et al. Perfluoroalkyl chemicals and asthma among children 12-19 years of age: NHANES (1999-2008). Environ Health Perspect. 2014;122(10):1129–33.
Buser MC, Scinicariello F. Perfluoroalkyl substances and food allergies in adolescents. Environ Int. 2016;88:74–9.
Stein CR, et al. Perfluoroalkyl and polyfluoroalkyl substances and indicators of immune function in children aged 12-19 y: National Health and nutrition examination survey. Pediatr Res. 2016;79(2):348–57.
Fei C, et al. Prenatal exposure to PFOA and PFOS and risk of hospitalization for infectious diseases in early childhood. Environ Res. 2010;110(8):773–7.
Dalsager L, et al. Association between prenatal exposure to perfluorinated compounds and symptoms of infections at age 1-4years among 359 children in the Odense child cohort. Environ Int. 2016;96:58–64.
Grandjean P, et al. Serum vaccine antibody concentrations in children exposed to perfluorinated compounds. JAMA. 2012;307(4):391–7.
Osuna CE, et al. Autoantibodies associated with prenatal and childhood exposure to environmental chemicals in Faroese children. Toxicol Sci. 2014;142(1):158–66.
Mogensen UB, et al. Structural equation modeling of immunotoxicity associated with exposure to perfluorinated alkylates. Environ Health. 2015;14:47.
Grandjean P, et al. Serum vaccine antibody concentrations in adolescents exposed to Perfluorinated compounds. Environ Health Perspect. 2017;125(7):077018.
Grandjean P, et al. Estimated exposures to perfluorinated compounds in infancy predict attenuated vaccine antibody concentrations at age 5-years. J Immunotoxicol. 2017;14(1):188–95.
Oulhote Y, et al. Children's white blood cell counts in relation to developmental exposures to methylmercury and persistent organic pollutants. Reprod Toxicol. 2017;68:207–14.
Timmermann CA, et al. Association between perfluoroalkyl substance exposure and asthma and allergic disease in children as modified by MMR vaccination. J Immunotoxicol. 2017;14(1):39–49.
Granum B, et al. Pre-natal exposure to perfluoroalkyl substances may be associated with altered vaccine antibody levels and immune-related health outcomes in early childhood. J Immunotoxicol. 2013;10(4):373–9.
Pennings JL, et al. Cord blood gene expression supports that prenatal exposure to perfluoroalkyl substances causes depressed immune functionality in early childhood. J Immunotoxicol. 2016;13(2):173–80.
Smit LA, et al. Prenatal exposure to environmental chemical contaminants and asthma and eczema in school-age children. Allergy. 2015;70(6):653–60.
Okada E, et al. Prenatal exposure to perfluorinated chemicals and relationship with allergies and infectious diseases in infants. Environ Res. 2012;112:118–25.
Okada E, et al. Prenatal exposure to perfluoroalkyl acids and allergic diseases in early childhood. Environ Int. 2014;65(Supplement C):127–34.
Goudarzi H, et al. Effects of prenatal exposure to perfluoroalkyl acids on prevalence ofallergic diseases among 4-year-old children. Environ Int. 2016;94:124–32.
Goudarzi H, et al. Prenatal exposure to perfluoroalkyl acids and prevalence of infectious diseases up to 4years of age. Environ Int. 2017;104:132–8.
Wang IJ, et al. The effect of prenatal perfluorinated chemicals exposures on pediatric atopy. Environ Res. 2011;111(6):785–91.
Dong GH, et al. Serum polyfluoroalkyl concentrations, asthma outcomes, and immunological markers in a case-control study of Taiwanese children. Environ Health Perspect. 2013;121(4):507–13.
Zhu Y, et al. Associations of serum perfluoroalkyl acid levels with T-helper cell-specific cytokines in children: by gender and asthma status. Sci Total Environ. 2016;559:166–73.
Donauer S, et al. Prenatal exposure to polybrominated diphenyl ethers and polyfluoroalkyl chemicals and infant neurobehavior. J Pediatr. 2015;166(3):736–42.
Goudarzi H, et al. Prenatal exposure to perfluorinated chemicals and neurodevelopment in early infancy: the Hokkaido study. Sci Total Environ. 2016;541:1002–10.
Chen MH, et al. Perfluorinated compound levels in cord blood and neurodevelopment at 2 years of age. Epidemiology. 2013;24(6):800–8.
Stein CR, Savitz DA, Bellinger DC. Perfluorooctanoate exposure in a highly exposed community and parent and teacher reports of behaviour in 6-12-year-old children. Paediatr Perinat Epidemiol. 2014;28(2):146–56.
Fei C, Olsen J. Prenatal exposure to perfluorinated chemicals and behavioral or coordination problems at age 7 years. Environ Health Perspect. 2011;119(4):573–8.
Liew Z, et al. Attention deficit/hyperactivity disorder and childhood autism in association with prenatal exposure to Perfluoroalkyl substances: a nested case-control study in the Danish National Birth Cohort. Environ Health Perspect. 2015;123(4):367–73.
• Oulhote Y, et al. Behavioral difficulties in 7-year old children in relation to developmental exposure to perfluorinated alkyl substances. Environ Int. 2016;97:237–45. This study with several PFASs exposure assessment showed inverse association of postnatal exposure to PFASs and childhood behavioral problems in childhood.
Høyer BB, et al. Pregnancy serum concentrations of perfluorinated alkyl substances and offspring behaviour and motor development at age 5-9 years - a prospective study. Environ Health. 2015;14:2. https://doi.org/10.1186/1476-069X-14-2.
Ode A, et al. Fetal exposure to perfluorinated compounds and attention deficit hyperactivity disorder in childhood. PLoS One. 2014;9(4):e95891.
Lien GW, Huang CC, Shiu JS, Chen MH, Hsieh WS, Guo YL, et al. Perfluoroalkyl substances in cord blood and attention deficit/hyperactivity disorder symptoms in seven-year-old children. Chemosphere. 2016;156:118–27.
Stein CR, Savitz DA, Bellinger DC. Perfluorooctanoate and neuropsychological outcomes in children. Epidemiology. 2013;24(4):590–9.
Braun JM, et al. Gestational exposure to endocrine-disrupting chemicals and reciprocal social, repetitive, and stereotypic behaviors in 4- and 5-year-old children: the HOME study. Environ Health Perspect. 2014;122(5):513–20.
Vuong AM, et al. Prenatal polybrominated diphenyl ether and perfluoroalkyl substance exposures and executive function in school-age children. Environ Res. 2016;147:556–64.
Strom M, et al. Persistent organic pollutants measured in maternal serum and offspring neurodevelopmental outcomes–a prospective study with long-term follow-up. Environ Int. 2014;68:41–8.
Wang Y, et al. Prenatal exposure to perfluroalkyl substances and children's IQ: the Taiwan maternal and infant cohort study. Int J Hyg Environ Health. 2015;218(7):639–44.
Hoffman K, et al. Exposure to Polyfluoroalkyl chemicals and attention deficit/hyperactivity disorder in U.S. children 12-15 years of age. Environ Health Perspect. 2010;118(12):1762–7.
Stein CR, Savitz DA. Serum perfluorinated compound concentration and attention deficit/hyperactivity disorder in children 5-18 years of age. Environ Health Perspect. 2011;119(10):1466–71.
Gump BB, et al. Perfluorochemical (PFC) exposure in children: associations with impaired response inhibition. Environ Sci Technol. 2011;45(19):8151–9.
Quaak I, de Cock M, de Boer M, Lamoree M, Leonards P, van de Bor M, et al. Prenatal exposure to perfluoroalkyl substances and behavioral development in children. Int J Environ Res Public Health. 2016;13(5):511. https://doi.org/10.3390/ijerph13050511.
Forns J, et al. Perfluoroalkyl substances measured in breast milk and child neuropsychological development in a Norwegian birth cohort study. Environ Int. 2015;83:176–82.
Sucharew H, et al. NICU network neurobehavioral scale profiles predict developmental outcomes in a low-risk sample. Paediatr Perinat Epidemiol. 2012;26(4):344–52.
Liew Z, et al. Prenatal exposure to perfluoroalkyl substances and the risk of congenital cerebral palsy in children. Am J Epidemiol. 2014;180(6):574–81.
DeWitt JC, et al. Immunotoxicity of perfluorinated compounds: recent developments. Toxicol Pathol. 2012;40(2):300–11.
Corsini E, et al. Perfluorinated compounds: emerging POPs with potential immunotoxicity. Toxicol Lett. 2014;230(2):263–70.
DeWitt JC, et al. Immunotoxicity of perfluorooctanoic acid and perfluorooctane sulfonate and the role of peroxisome proliferatoractivated receptor alpha. Crit Rev Toxicol. 2009;39(1):76–94.
DeWitt JC, et al. Suppression of antigen-specific antibody responses in mice exposed to perfluorooctanoic acid: role of PPARalpha and T- and B-cell targeting. J Immunotoxicol. 2016;13(1):38–45.
DeWitt JC, Copeland CB, Luebke RW. Suppression of humoral immunity by perfluorooctanoic acid is independent of elevated serum corticosterone concentration in mice. Toxicol Sci. 2009;109(1):106–12.
Yang Q, et al. Potent suppression of the adaptive immune response in mice upon dietary exposure to the potent peroxisome proliferator, perfluorooctanoic acid. Int Immunopharmacol. 2002;2(2-3):389–97.
Loveless SE, et al. Evaluation of the immune system in rats and mice administered linear ammonium perfluorooctanoate. Toxicol Sci. 2008;105(1):86–96.
• Goudarzi H, et al. The Association of Prenatal Exposure to Perfluorinated chemicals with glucocorticoid and androgenic hormones in cord blood samples: the Hokkaido study. Environ Health Perspect. 2017;125(1):111–8. For the first time, the authors showed evidence regarding the effects of prenatal exposure to PFAS on glucocorticoids and androgenic hormones in the fetuses
Itoh S, et al. Association of perfluoroalkyl substances exposure in utero with reproductive hormone levels in cord blood in the Hokkaido study on environment and Children's health. Environ Int. 2016;94:51–9.
Mariussen E. Neurotoxic effects of perfluoroalkylated compounds: mechanisms of action and environmental relevance. Arch Toxicol. 2012;86(9):1349–67.
Johansson N, Eriksson P, Viberg H. Neonatal exposure to PFOS and PFOA in mice results in changes in proteins which are important for neuronal growth and synaptogenesis in the developing brain. Toxicol Sci. 2009;108(2):412–8.
Slotkin TA, et al. Developmental neurotoxicity of perfluorinated chemicals modeled in vitro. Environ Health Perspect. 2008;116(6):716–22.
Weiss JM, et al. Competitive binding of poly- and perfluorinated compounds to the thyroid hormone transport protein transthyretin. Toxicol Sci: Off J Soc Toxicol. 2009;109(2):206–16.
Webster GM, et al. Associations between Perfluoroalkyl acids (PFASs) and maternal thyroid hormones in early pregnancy: a population-based cohort study. Environ Res. 2014;133:338–47.
Wang Y, et al. Association between maternal serum Perfluoroalkyl substances during pregnancy and maternal and cord thyroid hormones: Taiwan maternal and infant cohort study. Environ Health Perspect. 2014;122(5):529–34.
Wang Y, Starling AP, Haug LS, Eggesbo M, Becher G, Thomsen C, et al. Association between Perfluoroalkyl substances and thyroid stimulating hormone among pregnant women: a crosssectional study. Environ Health. 2013;12:76. https://doi.org/10.1186/1476-069X-12-76.
Lazarus JH. Thyroid hormone and intellectual development: a clinician's view. Thyroid: Off J Am Thyroid Assoc. 1999;9(7):659–60.
Koibuchi N, Chin MW. Thyroid hormone action and brain development. Trends Endocrinol Metab. 2000;11(4):123–8.
Oppenheimer JH, Schwartz HL. Molecular basis of thyroid hormone-dependent brain development. Endocr Rev. 1997;18(4):462–75.
Hong T, Paneth N. Maternal and infant thyroid disorders and cerebral palsy. Semin Perinatol. 2008;32(6):438–45.
Modesto T, et al. Maternal mild thyroid hormone insufficiency in early pregnancy and attention-deficit/hyperactivity disorder symptoms in children. JAMA Pediatr. 2015;169(9):838–45.
Andersen SL, et al. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG Int J Obstet Gynaecol. 2014;121(11):1365–74.
Vandenberg LN, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378–455.
Bellinger DC. Prenatal exposures to environmental chemicals and Children's neurodevelopment: an update. Saf Health Work. 2013;4(1):1–11.
Braun JM. Early-life exposure to EDCs: role in childhood obesity and neurodevelopment. Nat Rev Endocrinol. 2017;13(3):161–73.
Braun JM, et al. What can epidemiological studies tell us about the impact of chemical mixtures on human health? Environ Health Perspect. 2016;124(1):A6–9.
Bobb JF, et al. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics. 2015;16(3):493–508.
Mondal D, et al. Relationships of perfluorooctanoate and perfluorooctane sulfonate serum concentrations between mother-child pairs in a population with perfluorooctanoate exposure from drinking water. Environ Health Perspect. 2012;120(5):752–7.
Haug LS, et al. Diet and particularly seafood are major sources of perfluorinated compounds in humans. Environ Int. 2010;36(7):772–8.
Olsen GW, et al. Half-life of serum elimination of perfluorooctanesulfonate, perfluorohexanesulfonate, and perfluorooctanoate in retired fluorochemical production workers. Environ Health Perspect. 2007;115(9):1298–305.
Papadopoulou E, et al. Exposure of Norwegian toddlers to perfluoroalkyl substances (PFAS): the association with breastfeeding and maternal PFAS concentrations. Environ Int. 2016;94:687–94.
Zhang Y, et al. Biomonitoring of perfluoroalkyl acids in human urine and estimates of biological half-life. Environ Sci Technol. 2013;47(18):10619–27.
Perez F, et al. Accumulation of perfluoroalkyl substances in human tissues. Environ Int. 2013;59:354–62.
Rappazzo K, Coffman E, Hines E. Exposure to Perfluorinated alkyl substances and health outcomes in children: a systematic review of the epidemiologic literature. Int J Environ Res Public Health. 2017;14(7):691.
Winkens K, et al. Early life exposure to per- and polyfluoroalkyl substances (PFASs): a critical review. Emerg Contam. 2017;3(2):55–68.
Bach CC, et al. Perfluoroalkyl acid concentrations in blood samples subjected to transportation and processing delay. PLoS One. 2015;10(9):e0137768.
Verner MA, et al. Associations of Perfluoroalkyl substances (PFAS) with lower birth weight: an evaluation of potential confounding by glomerular filtration rate using a physiologically based pharmacokinetic model (PBPK). Environ Health Perspect. 2015;123(12):1317–24.
Sagiv SK, et al. Sociodemographic and perinatal predictors of early pregnancy per- and Polyfluoroalkyl substance (PFAS) concentrations. Environ Sci Technol. 2015;49(19):11849–58.
Harris MH, et al. Predictors of per- and Polyfluoroalkyl substance (PFAS) plasma concentrations in 6-10 year old American children. Environ Sci Technol. 2017;51(9):5193–204.
Bach CC, et al. Perfluoroalkyl and polyfluoroalkyl substances and measures of human fertility: a systematic review. Crit Rev Toxicol. 2016;46(9):735–55.
Joensen UN, et al. Do perfluoroalkyl compounds impair human semen quality? Environ Health Perspect. 2009;117(6):923–7.
Fei C, et al. Maternal levels of perfluorinated chemicals and subfecundity. Hum Reprod. 2009;24(5):1200–5.
Velez MP, Arbuckle TE, Fraser WD. Maternal exposure to perfluorinated chemicals and reduced fecundity: the MIREC study. Hum Reprod. 2015;30(3):701–9.
Darrow LA, et al. PFOA and PFOS serum levels and miscarriage risk. Epidemiology. 2014;25(4):505–12.
Jensen TK, et al. Association between perfluorinated compound exposure and miscarriage in Danish pregnant women. PLoSOne. 2015;10(4):e0123496.
• Liew Z, et al. Bias from conditioning on live birth in pregnancy cohorts: an illustration based on neurodevelopment in children after prenatal exposure to organic pollutants. Int J Epidemiol. 2015;44(1):345–54. This study provides extensive and detailed information regarding a common bias structure (leading to 'live-birth bias') that could arise when studying prenatal exposure effects to environmental factors on outcomes in the offspring in pregnancy cohorts
NTP. NTP Monograph. Immunotoxicity Associated with Exposure to Perfluorooctanoic Acid or Perfluorooctane Sulfonate. Research Triangle Park, NC: Office of Health Assessment and Translation, National Toxicology Program (NTP), National Institute of Environmental Health Sciences, National Institutes of Health, U.S. Department of Health and Human Services. 2016.
Acknowledgments
ZL was supported by the NIH/NIEHS Pathway to Independence Award (K99ES026729).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Zeyan Liew, Houman Goudarzi, and Youssef Oulhote declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Susceptibility Factors in Environmental Health
Rights and permissions
About this article
Cite this article
Liew, Z., Goudarzi, H. & Oulhote, Y. Developmental Exposures to Perfluoroalkyl Substances (PFASs): An Update of Associated Health Outcomes. Curr Envir Health Rpt 5, 1–19 (2018). https://doi.org/10.1007/s40572-018-0173-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-018-0173-4