Abstract
Introduction
The detection of paroxysmal atrial fibrillation (PAF) is crucial in the etiological study of an acute ischemic stroke (AIS), although this type of arrhythmia is often under-diagnosed. This prospective study aims to (1) evaluate the new-onset PAF detection rate among elderly patients with AIS in an acute setting, and (2) to assess the applicability of the STAF score (Score for the Targeting of Atrial Fibrillation) for such patients.
Methodology
An observational and prospective study was performed over a period of 11 months. Patients with acute ischemic stroke who had been admitted to the stroke unit were included. Exclusion criteria included prior AF, AF readings on ECG during admission, or stroke mimic. The patients were monitored with a bedside ECG monitor throughout the first 48 h, then simultaneously with an extended Holter recorder for a maximum of 6 days. The occurrence and duration of PAF events was evaluated. The STAF risk score for PAF was calculated and compared to the detection rate of PAF for each patient.
Results
The sample population consisted of 67 patients, whose median age was 76 years (IQR 71–84) and who were 57% males. The median duration of Holter recording was 3.5 days per patient (IQR 2–5). We detected new PAF cases in 16% of patients, and a total of 31% had supraventricular arrhythmia episodes lasting 10 s or longer. Among the patients in which this arrhythmia was detected, 10% had it detected by the bedside ECG monitor in the first 48 h. The median risk score was 5 (IQR 4–6). There was no association between the risk score used and PAF.
Conclusion
In elderly patients with AIS, the use of an extended Holter recorder led to the detection of more cases of PAF, offering them the chance to initiate hypocoagulant therapy. Among this population, the STAF score was non-discriminative and did not prove useful in predicting PAF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is a common cause of ischemic stroke, particularly in the elderly [1,2,3]. However, due to its characteristics (episodic, short duration and often asymptomatic presentation), paroxysmal atrial fibrillation (PAF) is underdiagnosed [1,2,3].
A subgroup of patients diagnosed with cryptogenic stroke will likely arise out of undiagnosed PAF patients [2, 4]. Moreover, it is known that the risk of stroke recurrence is about five times higher in patients with AF [1, 5].
On the other hand, different etiologies of ischemic stroke, namely macrovascular or microvascular disease, are easily detected through imaging and neck/brain examinations. In these cases, secondary prevention measures are indicated, which may include carotid endarterectomy or medical therapy with control of different vascular risk factors [1, 6, 7]. However, it is important to note that, particularly in elderly patients, there may be more than one possible cause for a patient with ischemic stroke. Accordingly, patients diagnosed with a non-cardioembolic etiology may have occult cardioembolism and benefit from anticoagulant agents [2, 8].
The clinical relevance of a PAF diagnosis is further increased by the availability of significantly effective hypocoagulation therapy to prevent ischemic events [1, 4,5,6].
Currently, there are several methods available for detecting PAF, both invasive and non-invasive. These may be grouped as intermittent, event-directed and continuous [1, 3]. The best method, the ideal duration of monitoring, and the population to be screened are still to be defined [5]. Although intermittent rhythm monitoring is inferior to continuous monitoring [9], these devices are not as available as Holter recorders in clinical practice.
The Holter recorder is a sensitive and specific method for detecting PAF, but its use usually has a relatively short duration (24 h) [3]. Other limitations stem from the need for patient compliance, the risk of skin irritation due to the electrodes, and the possibility of artefacts in the tracing due to muscle contraction [3, 10]. Even so, Holter recording is a cost-effective technique that is suitable to the clinical practice context [1, 3].
The hospitalization period after an AIS offers a good opportunity to investigate PAF: early monitoring might lead to a higher detection rate due to the possible higher frequency of cardiac arrhythmia during the acute phase [10], and it allows earlier secondary prophylaxis [8]. The continuous monitoring of the cardiac rhythm for 28h–72 h following hospital admission for stroke has detected PAF in 2–29% of patients [5]. Monitoring can be done in several ways, including continuous electrocardiographic monitoring for 24–48 h (according to European Stroke Organization and American Heart Association recommendations), telemetry, or through a cost-effective and non-invasive technique such as extended Holter, with durations greater than 24 h [6,7,8].
Different risk scores have been published to help identify stroke patients at greater risk for PAF. These are often based on age, clinical features and additional diagnostic tests, but the latter are not always available within the first few days after admission [4, 5, 11]. Suissa et al. proposed an easy-to-apply score based on four variables: age, left atrial size, National Institutes of Health Stroke Scale (NIHSS), and absence of small- or large-vessel vascular etiology [11].
In this study, we intend to evaluate the PAF detection rate in elderly patients hospitalized for acute ischemic stroke (AIS)/transitory ischemic attacks (TIA) in a stroke unit, assessing the added value of extended Holter recording in the acute setting and the applicability of the Score for the targeting of atrial fibrillation (STAF) among this population.
Methodology
A prospective study was conducted on patients aged over 65 years with a diagnosis of AIS, over a period of 11 months, in a 6-bed stroke unit integrated into an internal medicine ward. Patients with AIS/TIA were admitted after evaluation and treatment at the emergency department.
According to unit protocol, the patients underwent continuous electrocardiographic monitoring for approximately 48 h, with the unit’s nurses and/or physicians detecting any dysrhythmias on the monitor; in addition, they also underwent a simultaneous extended Holter recording, for a maximum period of 6 days.
Two Holter devices (Burdick Vision Holter™) and four memory cards with 48 h recording capacity were used. The Holter recording was suspended early in any of the following scenarios: (1) AF detection in the cardiac monitor within the first 48 h; (2) patient intolerance to the Holter device; (3) skin irritation associated with the electrodes; (4) hospital discharge before 6 days; or (5) death.
The Holter registration was initiated for the majority of patients within 24–36 h following hospital admission to the emergency department. All patients with suspected AIS or TIA and previous history of < 3 mRs (modified Rankin scale) were included. Patients with previously known AF or with AF present on the admission electrocardiogram (ECG), other anticoagulated patients, patients with previous stroke mimics, with present or past hemorrhagic stroke, or wearing a cardiac pacemaker or other cardiac device were excluded. Patients with other possible causes of non-cardioembolic stroke (significant intra- or extracranial vascular disease with greater than 50% stenosis, lacunar etiology, etc.) were not excluded.
Patient characteristics were recorded—demographic data, clinical variables (severity (NIHSS) and type of stroke according to Oxfordshire Community Stroke Project (OCSP) classifications), brain computed tomography findings of cortical lesions, transthoracic echocardiogram (TTE) findings of left atrial dilatation, echocardiogram or transcranial Doppler findings of suspected right-to-left shunt, and ecodoppler findings of > 50% carotid stenosis using the North American Symptomatic Carotid Endarterectomy Trial (NASCET) method. The Holter reading was conducted by two technicians trained and experienced in reading Holter recordings, and suspicion was later validated by a cardiologist.
The presence of paroxysmal atrial fibrillation was defined by the occurrence of a period of at least 30 s of supraventricular arrhythmia (SVA) without detectable P waves. [1, 4] Supraventricular arrhythmia with clinical significance (defined by consensus, based on literature) was considered if one or more events occurred with a minimum duration of 10 s. [4, 6, 12] For the sake of simplification, PAF throughout the following text refers to a supraventricular arrhythmia greater than or equal to 30 s in duration. The supraventricular arrhythmia burden was calculated for each patient.
The PAF risk score proposed by Suissa et al. (STAF) was calculated for each patient. Scoring criteria are as follows: age > 62 years and left atrial dilatation (two points); NIHSS ≥ 8 (one point); absence of intra- or extra-cranial stenosis ≥ 50%, symptoms of arterial dissection, and lacunar syndrome (three points). A cut-off point of ≥ 5 was used, with a sensitivity of 89% and a specificity of 88% [4, 10]. The PAF detection rate was then compared with the risk score value.
Patients or family members were asked to provide their informed consent.
Data were analyzed using Statistical Package for the Social Sciences (SPSS) software version 21.0. A statistical analysis was performed using the Mann–Whitney test for continuous variables and Chi square test for categorical variables. The level of significance was set at 0.05, two-sided. The risk score was studied using linear regression with the maximum daily AF loading and logistic regression for the presence of supraventricular arrhythmia (≥ 10 s).
Results
A total of 144 patients were admitted to the stroke unit, of whom 20% (n = 29) had previously known AF symptoms. AF was detected in the admission ECG in 17% of patients (n = 25), and during the first 24–36 h of hospitalization in 1% (n = 2). Eighty-eight patients were candidates for Holter monitoring. Of these, 8 did not undergo Holter monitoring due to device unavailability and 13 were excluded due to mRs ≥ 3 at admission (Fig. 1).
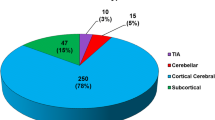
Sixty-seven patients fit the inclusion criteria and underwent extended Holter studies. These patients had an average age of 76 years (IQR 71–84), 57% were males, and average hospitalization time was 7 days (IQR 5–12). 10% were TIAs. Holter monitoring was performed for an average period of 3.5 days (IQR 2.0–5.0). Only one patient presented skin irritation that led to a shortening of the monitoring period.
Table 1 presents the characteristics of patients both with and without ≥ 10 s supraventricular arrhythmia, with only gender (arrhythmia being more frequent in females) and treatment obtained at discharge (hypocoagulation in patients with supraventricular arrhythmia) being statistically significant.
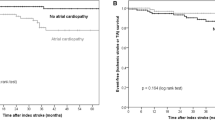
During the first 48 h of cardiac monitoring, PAF was detected in 7 of 67 patients (10%). The use of the Holter device allowed detection of PAF (SVA ≥ 30 s) in an additional 4 patients, for a total of 16% (11 of 67 patients) and SVA ≥ 10 s in an additional 10 patients, for a total of 31% (21 of 67 patients). In the 11 patients with PAF the median AF daily duration was 5.48 (IQR 0.023; 17.5) h. The 21 patients with SVA ≥ 10 s the arrythmia lasted for 0.142 (IQR 0.08; 0.25) min.
The detection rate for supraventricular arrhythmia was highest closer to the ischemic event (Figs. 2, 3), decreasing substantially over time. After the fourth day there was no new PAF detected.
At discharge, it was possible to change prophylactic therapy with onset of hypocoagulation in approximately one-third of patients (18 patients).
The population in this study had a mean 5-point risk score (IQR 4–6). No statistically significant association was observed between the value of patients’ STAF scores and the presence of paroxysmal atrial fibrillation (p > 0.05). For each unit of score, the risk of having PAF increases 25% (OR 1.25; CI 0.925–1.697).
Discussion
This study detected a very high rate of supraventricular arrhythmia in elderly patients with acute ischemic stroke/TIA. These results coincide with other with series in ischemic stroke patients (Table 2). The extended Holter monitoring increased the detection rate of ≥ 10 s supraventricular arrhythmia by 38% and ≥ 30 s by 19%, compared to the traditional 24-h Holter recording. The detection rate of arrhythmia was higher in the first 3 days of the ischemic event.
Among this population of elderly patients hospitalized with AIS the STAF score was non-discriminative and did not prove useful in predicting PAF. To the best of our knowledge this was the first study to apply this score in this specific population.
One of the still-unanswered questions in the literature is the PAF duration threshold above which clinical consequences arise. In the literature, there is no minimum duration for PAF classification, the most consensual being the arbitrary limit of 30 s [1, 4]. However, the clinical significance of < 30 s’ supraventricular arrhythmia remains to be clarified [1, 4], and is sometimes considered a precursor of PAF and associated with an increased risk of ischemic stroke [4, 6, 12]. Evidently, the PAF detection rate depends on the population studied and on the technique used [3, 5]. Several methods may be effective, but if the economic and clinical context of treatment centers is not considered in their choice, such methods might not be suitable for daily clinical practice and therefore have no clinical advantage.
Most PAF studies are conducted on patients with cryptogenic stroke [13,14,15]. However, because the elderly population has a higher risk of atheromatous disease of large vessels, small vessel disease and other major cardioembolic sources, there often is more than one possible cause for ischemic events in this population [16]. For this reason, even if another possible etiology for the ischemic event has already been identified, extended Holter remains important in elderly patients to avoid missing a PAF diagnosis.
Accordingly, 42% of the patients we studied exhibited symptomatic carotid stenosis greater than 50%, which could have been considered as the etiology of the event, and 15% had a concomitant supraventricular arrhythmia.
It is worth bearing in mind the special nature of the population we studied: being an elderly population in the acute phase of an ischemic event, we increased the chances of detecting this arrhythmia and of overvaluing short periods of supraventricular arrhythmia. As other authors have previously stated, in a patient who has already suffered the consequences of a stroke, it is difficult to ignore paroxysms of AF, even if short-lived [6]. The higher detection rate of supraventricular arrhythmia in the first days after the AIS event should be stressed, as suggested in other studies [8, 10].
The risk score used was not discriminatory in the detection of PAF in our population (OR 1.25). One possible explanation for this is the high STAF score of every elderly population. In our study, more than half of the patients had a score greater than or equal to 5 (cut-off proposed by the authors).
As previously mentioned, it would be useful to develop a risk score based on clinical features and findings detectable and available upon admission, which could help the physician assessing the benefit of extended Holter recording at this early stage.
This study has some limitations. First, the method used for detecting the supraventricular arrhythmia is based on the detection of fast supraventricular arrhythmia. Another limitation is the impossibility of proving causality between a detected arrhythmia, especially short SVA episodes, and AIS. However, knowing that the former is a major risk factor for cerebral ischemia and that it influences the secondary prophylactic therapy, detecting this arrhythmia remains clinically relevant. Third, a scarcity of resources might not allow performing these techniques in every treatment center or for every patient, making it more pertinent than ever to create an adequate risk score for selecting those who would benefit the most from extended Holter recording. Fourth, a bigger sample size and the presence of a control group without AIS would increase this study’s power.
On the other hand, one of the stronger points of this study is the increased PAF detection rate that enabled medical personnel to offer a more effective treatment with significant positive impact on secondary prevention. The STAF score was not discriminative in this population of elderly patients with AIS, stressing the need to continue the search for risk markers that may increase the degree of suspicion of this arrhythmia.
Conclusion
The supraventricular arrhythmia detection rate was high in the elderly population with acute ischemic stroke (those with ≥ 30 s duration comprised 16%, and those with ≥ 10 s 31%). The extended Holter duration increased the ≥ 10 s supraventricular arrhythmia detection rate by 38%, versus a standard Holter recording in this setting. This diagnostic technique is simple, easy to use, and well tolerated by most patients.
The STAF score does not seem to be useful in discerning which patients should be monitored.
References
Weber-Krüger M, Gelbrich G, Stahrenberg R et al (2014) Finding atrial fibrillation in stroke patients: randomized evaluation of enhanced and prolonged Holter monitoring–Find-AF(RANDOMISED)—rationale and design. Am Heart J 168:438–445
Kishore A, Vail A, Majid A et al (2014) Detection of atrial fibrillation after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Stroke 45:520–526
Rabinstein AA (2014) Prolonged cardiac monitoring for detection of paroxysmal atrial fibrillation after cerebral ischemia. Stroke 45:1208–1214
Gladstone DJ, Spring M, Dorian P et al (2014) Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med 370:2467–2477
Andrade JG, Field T, Khairy P (2015) Detection of occult atrial fibrillation in patients with embolic stroke of uncertain source: a work in progress. Front Physiol 6:100
Jauch EC, Saver JL, Adams HP Jr et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507
Grond M, Jauss M, Hamann G et al (2013) Improved detection of silent atrial fibrillation using 72-hour Holter ECG in patients with ischemic stroke: a prospective multicenter cohort study. Stroke 44:3357–3364
Charitos EI, Stierle U, Ziegler PD, Baldewig M, Robinson DR, Sievers HH, Hanke T (2012) A comprehensive evaluation of rhythm monitoring strategies for the detection of atrial fibrillation recurrence: insights from 647 continuously monitored patients and implications for monitoring after therapeutic interventions. Circulation 126:806–814
Stahrenberg R, Weber-Krüger M, Seegers J et al (2010) Enhanced detection of paroxysmal atrial fibrillation by early and prolonged continuous Holter monitoring in patients with cerebral ischemia presenting in sinus rhythm. Stroke 41:2884–2888
Suissa L, Bertora D, Lachaud S et al (2009) Score for the targeting of atrial fibrillation (STAF): a new approach to the detection of atrial fibrillation in the secondary prevention of ischemic stroke. Stroke 40:2866–2868
Glotzer TV, Daoud EG, Wyse DG et al (2009) The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: The TRENDS study. Circ Arrhythm Electrophysiol 2:474–480
Hariri E, Hachem A, Sarkis G et al (2016) Optimal duration of monitoring for atrial fibrillation in cryptogenic stroke: a nonsystematic review. Biomed Res Int 2016:5704963
Bridge F, Thijs V (2016) How and when to screen for atrial fibrillation after stroke: insights from insertable cardiac monitoring devices. J Stroke 18:121–128
Toyoda K, Okumura K, Hashimoto Y et al (2016) Identification of covert atrial fibrillation in cryptogenic ischemic stroke: current clinical practice in Japan. J Stroke Cerebrovasc Dis 25:1829–1837
Wachter R, Weber-Krüger M, Seegers J et al (2013) Age-dependent yield of screening for undetected atrial fibrillation in stroke patients: the Find-AF study. J Neurol 260:2042–2045
Acknowledgements
The authors would like to publicly thank nurses Sandra Gaspar and Cristina Morais for their collaboration in the collection of the data used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
This article does not contain any experimental procedure with human participants or animals. All exams performed were done in routine clinical practice.
Informed consent
All participants provided informed consent to do routine clinical exams during their stay in the hospital.
Rights and permissions
About this article
Cite this article
Alves, M., Narciso, M.R., Cruz, J. et al. Paroxysmal atrial fibrillation detection in patients with acute ischemic stroke through prolonged Holter: prospective study. Aging Clin Exp Res 31, 469–474 (2019). https://doi.org/10.1007/s40520-018-1014-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-1014-x