Abstract
Purpose of Review
To summarize the literature on the detection of atrial fibrillation (AF) in patients with “cryptogenic” stroke, a cohort including about 25% of all ischemic stroke patients and patients with embolic stroke of undetermined source (ESUS).
Recent Findings
A first episode of AF is detected in up to one third of cryptogenic stroke and in up to one fourth of ESUS patients during long-term monitoring. AF prevalence correlates to patient selection, duration, and quality of ECG monitoring. Higher rates of AF were reported in stroke patients with left atrial pathology, specific ECG alterations, or increased natriuretic peptides. While AF detection impacts on medical stroke prevention in the vast majority of patients, patient selection for prolonged monitoring is largely left at the physician’s discretion.
Summary
AF detection after cryptogenic stroke or ESUS is a frequent, potentially causal condition. Whether subsequent oral anticoagulation may improve outcome remains open.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is defined as one or more episode of at least 30 s of atrial arrhythmia with missing P-waves [1•]. AF is the most prevalent arrhythmia worldwide, affecting about 3% of the adult population, in particular older adults or those with co-existing cardiovascular risk factors. Individuals with paroxysmal, persistent, or permanent AF may suffer from AF-related symptoms including palpitations or dizziness (“symptomatic” AF). However, a relevant proportion of stroke patients with AF is asymptomatic (“silent” AF) at the time of AF detection (and later on) [2, 3]. AF increases the risk of ischemic stroke four- to five-fold on average, ranging from approximately 0.2 to 20% per year, corresponding to the presence of stroke risk factors [1•]. At the time of ischemic stroke or transient ischemic attack (TIA), AF is known in about 15–18% of all patients and stroke is related to AF in the vast majority of these patients [4,5,6]. While about 30% of all patients with known AF before stroke have documented AF during the in-hospital stay, a first episode of AF is detected in 4–13% of unselected acute stroke patients without known AF at the time of stroke [5, 7,8,9].
Overall, about 25% of all ischemic strokes presumed to be of cardioembolic origin, including strokes related to heart failure, patent foramen ovale, myocardial infarction, and endocarditis. Compared to non-cardioembolic strokes, cardioembolic strokes are associated with higher morbidity and mortality [10]. Another 25% of all ischemic strokes or transient ischemic attacks (TIAs) remain “cryptogenic” by definition [11], indicating that the etiology of stroke could not be clarified by (in)complete or (in)sufficient routine diagnostic care (in hospital). In the minority of these “cryptogenic” stroke patients, more than one probable (“competing”) cause of stroke is detected. Cryptogenic stroke patients have a 3–6% risk of recurrent ischemic stroke [12•], which is comparable to patients with other stroke causes.
To allow the conduction of clinical trials, the FDA requested a definition of the minimum diagnostic evaluation in patients with cryptogenic stroke. Subsequently, a group of leading stroke physicians defined the so-called “embolic stroke of undetermined source” (ESUS). By definition, an ESUS is a “non-lacunar brain infarct without proximal arterial stenosis or cardioembolic sources, with a clear indication for anticoagulation” [12•]. Based on the assumption that ESUS might be caused by so far undetected AF or other embolic sources, two large randomized secondary stroke prevention studies compared a non-vitamin K oral anticoagulant (NOAC) to acetylsalicylic acid, the present standard of care in patients with cryptogenic stroke or ESUS, respectively [13, 14••].
Relevance of AF Detection for Medical Stroke Prevention
The detection of AF after ischemic stroke is relevant for secondary stroke prevention, even if there is uncertainty regarding the most probable cause of stroke. Stroke patients with AF but without subsequent oral anticoagulation have a comparatively high risk of recurrent stroke [15]. Oral anticoagulation is highly effective by reducing the risk of recurrent ischemic stroke by approximately 70% compared to placebo in clinical trials [1•]. Irrespective of the fact that the total burden of AF may play a role regarding the magnitude of AF-related stroke risk [16, 17], oral anticoagulation is recommended by guidelines in all stroke patients independent of the type of AF (paroxysmal, persistent, or permanent) [1•, 18•]. Of note, effective oral anticoagulation at the time of ischemic stroke is associated with reduced stroke severity and mortality in AF patients [6]. Interestingly, there is only some data demonstrating that AF detected for the first time after acute ischemic stroke or TIA will be recurrent at later stages [19]. AF usually is a progressive disease and repeat episodes are very likely, in particular with increasing age. AF incidence during a condition of cardiac or systemic stress carries a high propensity of recurrence later on [20]. In these patients, the substrate for AF development exists and the arrhythmia is triggered by additional stress factors. Therefore, it can be assumed that individuals with a first episode of AF in context with TIA or stroke benefit from a close follow-up for recurrent AF and its sequelae.
Pathophysiology of AF-Related Stroke and Stroke-Related AF
The simplistic, unidirectional view is that AF and consecutive stasis in the atria lead to clot formation predominantly in the left atrial appendage and systemic embolization resulting in stroke needs refinement [21•]. A solid thrombus or highly thrombogenic conditions (e.g., spontaneous echo contrast) can be detected by standard methods such as transesophageal echocardiography in the minority of stroke patients with AF [4, 22]. Furthermore, it is known that AF per se does not necessarily carry an increased risk of stroke in the absence of additional stroke risk factors. Therefore, oral anticoagulation does not have a net clinical benefit in low-risk patients with a CHA2DS2-VASc (heart failure or left ventricular systolic dysfunction, hypertension, age ≥ 75 years (2 points), diabetes mellitus, prior stroke or TIA or thromboembolism (2 points), vascular disease, age 65–74 years and female sex) score of zero (points) [23].
In study of patients with implanted cardiac devices, there is a correlation of AF burden and subsequent stroke risk but the correlation between AF episodes and stroke onset is rather weak, as demonstrated in the Atrial Fibrillation and Stroke Evaluation in Pacemaker Patients and the Atrial Fibrillation Reduction Atrial Pacing Trial (ASSERT) [16, 24]. It has been suggested that not the arrhythmia itself but indirect mechanisms may be responsible for the increased stroke risk in AF [21•]. AF by itself may be a marker of this higher susceptibility of ischemic stroke. What AF and other atrial arrhythmias have in common is that they may be markers of a prothrombotic milieu in the atria [15, 21•]. The latter is enhanced by local cardiomyocyte, electrical and endothelial impairment, and augmented by systemic vascular changes. Therefore, AF alone may not be a sufficient cause to explain thromboembolic stroke in context with the arrhythmia.
Interestingly, there is a bidirectional relation between stroke and AF. It is well-established that strokes affecting the insular region, orbitofrontal and dorsal cingulate cortex, the hypothalamus, the amygdala, the periaqueductal gray, or the ventrolateral medulla may induce an autonomous imbalance [25], subsequently causing a first episode of AF in stroke patients without known AF. Therefore, in the individual patient with acute ischemic stroke, it may not be clarified whether AF is the cause or consequence of stroke [26•]. It also remains enigmatic, if the detection of a first episode of AF several months after cryptogenic stroke [27••, 28••] is related to the index stroke in a substantial number of patients. Recent subgroup analyses of the ASSERT trial indicated that stroke risk increase only increased with a higher AF burden, i.e., AF episodes of 24 h or longer [16]. Because of the fact that about 7% of all ASSERT patients had a previous stroke, these observations cannot directly be translated to post-stroke patients. Nevertheless, they call for caution to not attribute causality for ischemic stroke to every detected episode of AF. The clinical relevance of short atrial runs (lasing < 30 s)—a frequent finding after acute ischemic stroke [3, 8]—or atrial high rate episodes (AHRE)—detected in patients with implanted devices—remains to be established [15].
Frequency of AF Detection in Cryptogenic Stroke or ESUS
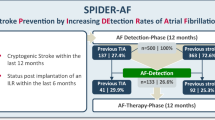
As demonstrated in Fig. 1, AF detection rate in stroke patients is correlated to the duration of (previous) ECG monitoring and the (cardiovascular) risk profile [29]. In patients with acute ischemic stroke or TIA, 12-lead resting ECG on hospital admission detects a first episode of AF in about 1.7–16% of all patients [30]. Additional (monitor-based) ECG monitoring for 24 h detects a first episode of AF in about 0.2–13% of all patients, while ECG monitoring for 72 h detects a first episode of AF in about 2.3–11% of all patients with acute ischemic stroke. Within a week after stroke, 1.7–14% of all patients were diagnosed to have AF [8, 30, 31]. Holter-ECG recording for 10 days in the intervention arm of the FIND-AF randomized study demonstrated that 18 out of 200 patients (9%) (aged ≥ 60 years; recruited within 7 days after stroke) had a first episode of AF [32]. Interestingly, a second 10-day Holter-ECG recording 3 months later detected a first episode of AF in additional 10 patients (5.5%), while another 10-day Holter-ECG recording further 3 months later was again feasible and well-tolerated but detected no AF in the remaining stroke patients without a history of AF. A 30-day event recorder detected a first episode of AF in 46 (16%) out of 286 patients (aged ≥ 55 years; recruited within 6 months after cryptogenic stroke) in the intervention arm of the EMBRACE study [28••]. Within 3 months, an implantable loop recorder (ILR) detected a first episode of AF in 19 (9%) out of 221 patients (aged ≥ 40 years; recruited within 3 months after cryptogenic stroke) in the intervention arm of the CRYSTAL-AF study. After 12 months or 36 months, ILR-based AF detection rate was 12% or 30%, respectively [27••]. In a German single-center observational study, an ILR detected a first episode of AF in 25 (33%) out of 75 patients with cryptogenic stroke and at least one additional clinical, electrocardiographic, or echocardiographic risk factor for AF (e.g., CHA2DS2-VASc ≥ 4, spontaneous echo contrast, or a previous atrial run) [3]. Of note, beside the presence of atrial runs during baseline ECG monitoring, a left atrial diameter of > 45 mm was predictive for AF. Within a year, a first episode of AF was detected by an ILR in 17–26% of all patients fulfilling the ESUS criteria [33,34,35], which is comparable to the reported detection rate in patients with cryptogenic stroke (Fig. 1).
Guideline Recommendations Regarding ECG Monitoring After Cryptogenic Stroke
Based on the results of the EMBRACE trial [28••], the US guideline recommends ECG monitoring for 30 days (Class IIa, Level C) in patients with a cryptogenic stroke within the last 6 months [18•]. The European Society of Cardiology (ESC) recommends ECG monitoring for at least 72 h in patients with stroke or transient ischemic attack (TIA) but without known AF (Class I, Level B) [1•]. The guidelines of the European Stroke Organization (ESO) recommend a long-term ECG registration in stroke patients with high suspicion of asymptomatic, paroxysmal AF. Specific information on the duration of ECG monitoring in the acute phase is not given [36].
How to Screen After Cryptogenic Stroke
A 12-lead resting ECG should be standard in diagnostic stroke work-up and is recommended by guidelines. However, limited resources are a major problem and even today, a standard ECG is not performed within the first 2 days in all patients with acute ischemic stroke cases [37]. The quality of further ECG evaluation impacts on the frequency of AF detection [38, 39]. Continuous ECG monitoring by automated arrhythmia detection is sensitive, but requires standardized manual evaluation [40, 41]. AF screening by intermittent handheld devices appears to be similarly effective as continuous monitoring and can also be operated by nurses [42]. Extended non-invasive ECG monitoring after hospital discharge increases the yield of AF detection [32]. As a step further, the implantation of ILR may help to optimize secondary prevention in selected patients with ischemic stroke. The insertion of ILRs should be considered carefully in the context of (present) costs of implantation and monitoring [29].
Current data indicate that ECG monitoring is most effective in the early phase after cryptogenic stroke [27••, 32]. Since published meta-analyses are of limited value due to substantial heterogeneity of cohorts, monitoring methods, or AF definition [9, 26•, 43], the optimal duration of ECG monitoring remains to be established.
Whom to Screen After Cryptogenic Stroke
In clinical practice, decision making on prolonged ECG monitoring after ischemic stroke is not based on scales or scores. According to the control arms of the randomized EMBRACE, FIND-AF randomized or CRYSTAL-AF study, prolonged ECG monitoring in the subacute phase of stroke is sparse in clinical practice. This may be caused by limited (personnel) resources, comparably low funding, and rather vague guideline recommendations.
Focusing on best practical use of present resources, a higher prevalence of AF will be found in cryptogenic stroke patients aged 60 years and older [44] or those with present “low-risk sources” of embolism (in particular heart failure or atherosclerosis with a stenosis < 50% of a brain supplying artery) [12•]. In addition, stroke patients with excessive supraventricular ectopic activity, detected atrial runs (lasing < 30 s), or prolonged PR interval should undergo prolonged ECG monitoring [3, 44, 45•]. While cardiac imaging (left atrial volume index in combination with atrial function, mitral valve stenosis, or left atrial enlargement) after stroke is proven to be helpful to identify stroke patients at high risk of AF [3, 46, 47], stroke lesion pattern(s) may not be solely used to guide prolonged ECG monitoring [48]. Finally, biomarkers (especially natriuretic peptides or troponin) may support optimized AF detection [29].
Open Questions Regarding AF Detection After Cryptogenic Stroke
First of all, it remains an open question whether a randomized clinical study will be able to demonstrate a reduction of relevant clinical endpoints in stroke patients undergoing prolonged ECG monitoring. So far, randomized trails like CRYSTAL-AF, EMBRACE, or FIND-AF randomized only demonstrated that prolonged ECG monitoring results in a significant higher proportion of AF detection and subsequent oral anticoagulation. The results of the randomized MonDAFIS study will add evidence in this regard [49]. This ongoing investigator-initiated study enrolled 3470 patients with acute ischemic stroke in 39 German stroke centers.
In the absence of a proven clinical benefit of prolonged ECG monitoring, optimal AF detection after cryptogenic stroke might lose relevance, if the ongoing randomized double-blind Dabigatran Etexilate for Secondary Stroke Prevention in Patients With Embolic Stroke of Undetermined Source (RE-SPECT ESUS) study will demonstrate a net clinical benefit of oral anticoagulation using dabigatran (150 or 110 mg TD) compared to acetylsalicylic acid (100 mg OD) [13]. However, the randomized double-blind Rivaroxaban versus Aspirin in Secondary Prevention of Stroke and Prevention of Systemic Embolism in Patients With Recent Embolic Stroke of Undetermined Source (NAVIGATE ESUS) study demonstrated a significantly higher bleeding risk in the rivaroxaban (15 mg OD) arm compared to acetylsalicylic acid (100 mg OD) [14••].
Second, it remains to be determined whether patients with a first episode of AF after stroke have a similar stroke risk compared to patients with known AF at the time of stroke. A retrospective analysis of the observational Ontario Stroke Registry revealed a similar annual stroke rate in stroke patients without known AF (8.0%) or stroke patients with a first episode of AF after the index stroke (7.0%), while patients with known AF at the time of the index stroke had a significantly higher rate (9.6%) [50•]. A similar observation was made in pacemaker patients with AHRE compared to patients with well-documented AF [15].
Conclusions
AF is a common comorbidity and frequently causal factor in ischemic stroke which may account for about 20% of all ischemic strokes. Furthermore, a first episode of AF is detected during long-term ECG monitoring using an ILR in up to one third of all patients with cryptogenic stroke and in about one fourth of all patients with ESUS. Future research needs to demonstrate whether treatment of AF detected by intensified ECG screening after ischemic stroke impacts on relevant outcome parameters like recurrent stroke or mortality. The selection of cryptogenic stroke patients who should undergo prolonged ECG monitoring is largely left at the physician’s discretion at present. Cardiac imaging, ECG alterations, or biomarkers may support the efficiency of post-stroke AF screening in patients with cryptogenic stroke.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962. https://doi.org/10.1093/eurheartj/ehw210. Present guidelines of the ESC/EACTS.
Brachmann J, Morillo CA, Sanna T, Di Lazzaro V, Diener H, Bernstein RA, et al. Uncovering atrial fibrillation beyond short-term monitoring in cryptogenic stroke patients: three-year results from the cryptogenic stroke and underlying atrial fibrillation trial. Circ Arrhythm Electrophysiol. 2016;9:e003333. https://doi.org/10.1161/CIRCEP.115.003333.
Poli S, Diedler J, Härtig F, Götz N, Bauer A, Sachse T, et al. Insertable cardiac monitors after cryptogenic stroke--a risk factor based approach to enhance the detection rate for paroxysmal atrial fibrillation. Eur J Neurol. 2016;23:375–81. https://doi.org/10.1111/ene.12843.
Herm J, Konieczny M, Jungehulsing GJ, Endres M, Villringer A, Malzahn U, et al. Should transesophageal echocardiography be performed in acute stroke patients with atrial fibrillation? J Clin Neurosci. 2013;20:554–9. https://doi.org/10.1016/j.jocn.2012.03.049.
Rizos T, Horstmann S, Dittgen F, Täger T, Jenetzky E, Heuschmann P, et al. Preexisting heart disease underlies newly diagnosed atrial fibrillation after acute ischemic stroke. Stroke. 2016;47:336–41. https://doi.org/10.1161/STROKEAHA.115.011465.
Hellwig S, Grittner U, Audebert H, Endres M, Haeusler KG. Non-vitamin K-dependent oral anticoagulants have a positive impact on ischaemic stroke severity in patients with atrial fibrillation. Europace. 2018;20:569–74. https://doi.org/10.1093/europace/eux087.
Grond M, Jauss M, Hamann G, Stark E, Veltkamp R, Nabavi D, et al. Improved detection of silent atrial fibrillation using 72-hour Holter ECG in patients with ischemic stroke: a prospective multicenter cohort study. Stroke. 2013;44:3357–64. https://doi.org/10.1161/STROKEAHA.113.001884.
Stahrenberg R, Weber-Krüger M, Seegers J, Edelmann F, Lahno R, Haase B, et al. Enhanced detection of paroxysmal atrial fibrillation by early and prolonged continuous holter monitoring in patients with cerebral ischemia presenting in sinus rhythm. Stroke. 2010;41:2884–8. https://doi.org/10.1161/STROKEAHA.110.591958.
Kishore A, Vail A, Majid A, Dawson J, Lees KR, Tyrrell PJ, et al. Detection of atrial fibrillation after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis. Stroke. 2014;45:520–6. https://doi.org/10.1161/STROKEAHA.113.003433.
Marini C, de Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005;36:1115–9. https://doi.org/10.1161/01.STR.0000166053.83476.4a.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon David L, et al. Classification of subtype of acute ischemic stroke.: definitions for use in a multicenter clinical trial. Stroke. 1993;24:35–41.
• Hart RG, Diener H, Coutts SB, Easton JD, Granger CB, O’Donnell MJ, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429–38. https://doi.org/10.1016/S1474-4422(13)70310-7. Position paper defining the term embolic stroke of undetermined source, further providing an excellent review of present knowledge.
Diener H, Bernstein R, Hart R. Secondary stroke prevention in cryptogenic stroke and embolic stroke of undetermined source (ESUS). Curr Neurol Neurosci Rep. 2017;17:64. https://doi.org/10.1007/s11910-017-0775-5.
•• Hart RG, Sharma M, Mundl H, Kasner SE, Bangdiwala SI, Berkowitz SD, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018;378:2191–201. https://doi.org/10.1056/NEJMoa1802686. Randomized double-blind study reporting the results of the NAVIGATE ESUS trial, comparing rivaroxaban to acetylsalicylic acid in ESUS patients.
Camm AJ, Simantirakis E, Goette A, Lip GYH, Vardas P, Calvert M, et al. Atrial high-rate episodes and stroke prevention. Europace. 2017;19:169–79. https://doi.org/10.1093/europace/euw279.
Gelder V, Isabelle C, Healey JS, Crijns HJGM, Wang J, Hohnloser SH, et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 2017;38:1339–44. https://doi.org/10.1093/eurheartj/ehx042.
Ganesan AN, Chew DP, Hartshorne T, Selvanayagam JB, Aylward PE, Sanders P, et al. The impact of atrial fibrillation type on the risk of thromboembolism, mortality, and bleeding: a systematic review and meta-analysis. Eur Heart J. 2016;37:1591–602. https://doi.org/10.1093/eurheartj/ehw007.
• Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–236. https://doi.org/10.1161/STR.0000000000000024. Present guidelines of the AHA/ASA.
Higgins P, Dawson J, MacFarlane PW, McArthur K, Langhorne P, Lees KR. Predictive value of newly detected atrial fibrillation paroxysms in patients with acute ischemic stroke, for atrial fibrillation after 90 days. Stroke. 2014;45:2134–6. https://doi.org/10.1161/STROKEAHA.114.005405.
Lubitz SA, Yin X, Rienstra M, Schnabel RB, Walkey AJ, Magnani JW, et al. Long-term outcomes of secondary atrial fibrillation in the community: the Framingham Heart Study. Circulation. 2015;131:1648–55. https://doi.org/10.1161/CIRCULATIONAHA.114.014058.
• Kamel H, Okin PM, Elkind MSV, Iadecola C. Atrial fibrillation and mechanisms of stroke: time for a new model. Stroke. 2016;47:895–900. https://doi.org/10.1161/STROKEAHA.115.012004. Review summarizing present knowledge.
Hur J, Kim YJ, Lee H, Nam JE, Hong YJ, Kim HY, et al. Cardioembolic stroke: dual-energy cardiac CT for differentiation of left atrial appendage thrombus and circulatory stasis. Radiology. 2012;263:688–95. https://doi.org/10.1148/radiol.12111691.
Friberg L, Rosenqvist M, Lip GYH. Net clinical benefit of warfarin in patients with atrial fibrillation: a report from the Swedish atrial fibrillation cohort study. Circulation. 2012;125:2298–307. https://doi.org/10.1161/CIRCULATIONAHA.111.055079.
Brambatti M, Connolly SJ, Gold MR, Morillo CA, Capucci A, Muto C, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation. 2014;129:2094–9. https://doi.org/10.1161/CIRCULATIONAHA.113.007825.
Tahsili-Fahadan P, Geocadin RG. Heart-brain axis: effects of neurologic injury on cardiovascular function. Circ Res. 2017;120:559–72. https://doi.org/10.1161/CIRCRESAHA.116.308446.
• Sposato LA, Riccio PM, Hachinski V. Poststroke atrial fibrillation: cause or consequence? Critical review of current views. Neurology. 2014;82:1180–6. https://doi.org/10.1212/WNL.0000000000000265. Review summarizing present knowledge.
•• Sanna T, Diener H, Passman RS, Di Lazzaro V, Bernstein RA, Morillo CA, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370:2478–86. https://doi.org/10.1056/NEJMoa1313600. Randomized study reporting the prevalence of AF detection in patients with cryptogenic stroke.
•• Gladstone DJ, Sharma M, Spence JD. Cryptogenic stroke and atrial fibrillation. N Engl J Med. 2014;371:1260. https://doi.org/10.1056/NEJMc1409495. Randomized study reporting the prevalence of AF detection in patients with cryptogenic stroke.
Haeusler KG, Gröschel K, Köhrmann M, Anker SD, Brachmann J, Böhm M, et al. Expert opinion paper on atrial fibrillation detection after ischemic stroke. Clin Res Cardiol. 2018; https://doi.org/10.1007/s00392-018-1256-9.
Sposato LA, Cipriano LE, Saposnik G, Ruíz Vargas E, Riccio PM, Hachinski V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2015;14:377–87. https://doi.org/10.1016/S1474-4422(15)70027-X.
Wallmann D, Tüller D, Wustmann K, Meier P, Isenegger J, Arnold M, et al. Frequent atrial premature beats predict paroxysmal atrial fibrillation in stroke patients: an opportunity for a new diagnostic strategy. Stroke. 2007;38:2292–4. https://doi.org/10.1161/STROKEAHA.107.485110.
Wachter R, Gröschel K, Gelbrich G, Hamann GF, Kermer P, Liman J, et al. Holter-electrocardiogram-monitoring in patients with acute ischaemic stroke (Find-AFRANDOMISED): an open-label randomised controlled trial. Lancet Neurol. 2017;16:282–90. https://doi.org/10.1016/S1474-4422(17)30002-9.
Israel C, Kitsiou A, Kalyani M, Deelawar S, Ejangue LE, Rogalewski A, et al. Detection of atrial fibrillation in patients with embolic stroke of undetermined source by prolonged monitoring with implantable loop recorders. Thromb Haemost. 2017;117:1962–9. https://doi.org/10.1160/TH17-02-0072.
Cotter PE, Martin PJ, Ring L, Warburton EA, Belham M, Pugh PJ. Incidence of atrial fibrillation detected by implantable loop recorders in unexplained stroke. Neurology. 2013;80:1546–50. https://doi.org/10.1212/WNL.0b013e31828f1828.
Ritter MA, Kochhäuser S, Duning T, Reinke F, Pott C, Dechering DG, et al. Occult atrial fibrillation in cryptogenic stroke: detection by 7-day electrocardiogram versus implantable cardiac monitors. Stroke. 2013;44:1449–52. https://doi.org/10.1161/STROKEAHA.111.676189.
The European Stroke Organization (ESO) Executive Committee and the ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25:457–507. https://doi.org/10.1159/000131083.
Bravata DM, Myers LJ, Arling G, Miech EJ, Damush T, Sico JJ, et al. Quality of care for veterans with transient ischemic attack and minor stroke. JAMA Neurol. 2018;75:419–27. https://doi.org/10.1001/jamaneurol.2017.4648.
Kallmünzer B, Breuer L, Hering C, Raaz-Schrauder D, Kollmar R, Huttner HB, et al. A structured reading algorithm improves telemetric detection of atrial fibrillation after acute ischemic stroke. Stroke. 2012;43:994–9. https://doi.org/10.1161/STROKEAHA.111.642199.
Rizos T, Güntner J, Jenetzky E, Marquardt L, Reichardt C, Becker R, et al. Continuous stroke unit electrocardiographic monitoring versus 24-hour Holter electrocardiography for detection of paroxysmal atrial fibrillation after stroke. Stroke. 2012;43:2689–94. https://doi.org/10.1161/STROKEAHA.112.654954.
Kurka N, Bobinger T, Kallmünzer B, Koehn J, Schellinger PD, Schwab S, et al. Reliability and limitations of automated arrhythmia detection in telemetric monitoring after stroke. Stroke. 2015;46:560–3. https://doi.org/10.1161/STROKEAHA.114.007892.
Uphaus T, Grings A, Gröschel S, Müller A, Weber-Krüger M, Wachter R, et al. Automatic detection of paroxysmal atrial fibrillation in patients with ischaemic stroke: better than routine diagnostic workup? Eur J Neurol. 2017;24:990–4. https://doi.org/10.1111/ene.13326.
Tu HT, Chen Z, Swift C, Churilov L, Guo R, Liu X, et al. Smartphone electrographic monitoring for atrial fibrillation in acute ischemic stroke and transient ischemic attack. Int J Stroke. 2017;12:786–9. https://doi.org/10.1177/1747493017696097.
Dussault C, Toeg H, Nathan M, Wang ZJ, Roux J, Secemsky E. Electrocardiographic monitoring for detecting atrial fibrillation after ischemic stroke or transient ischemic attack: systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2015;8:263–9. https://doi.org/10.1161/CIRCEP.114.002521.
Thijs VN, Brachmann J, Morillo CA, Passman RS, Sanna T, Bernstein RA, et al. Predictors for atrial fibrillation detection after cryptogenic stroke: results from CRYSTAL AF. Neurology. 2016;86:261–9. https://doi.org/10.1212/WNL.0000000000002282.
• Gladstone DJ, Dorian P, Spring M, Panzov V, Mamdani M, Healey JS, et al. Atrial premature beats predict atrial fibrillation in cryptogenic stroke: results from the EMBRACE trial. Stroke. 2015;46:936–41. https://doi.org/10.1161/STROKEAHA.115.008714. Substudy of a randomized study reporting the importance of atrial premature beats to detect AF in patients with cryptogenic stroke.
Broughton ST, O’Neal WT, Salahuddin T, Soliman EZ. The influence of left atrial enlargement on the relationship between atrial fibrillation and stroke. J Stroke Cerebrovasc Dis. 2016;25:1396–402. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.02.004.
Waldenhjort D, Sobocinski Doliwa P, Alam M, Frykman-Kull V, Engdahl J, Rosenqvist M, et al. Echocardiographic measures of atrial function may predict atrial fibrillation in stroke patients. Scand Cardiovasc J. 2016;50:236–42. https://doi.org/10.1080/14017431.2016.1175657.
Bernstein RA, Di Lazzaro V, Rymer MM, Passman RS, Brachmann J, Morillo CA, et al. Infarct topography and detection of atrial fibrillation in cryptogenic stroke: results from CRYSTAL AF. Cerebrovasc Dis. 2015;40:91–6. https://doi.org/10.1159/000437018.
Haeusler KG, Kirchhof P, Heuschmann PU, Laufs U, Busse O, Kunze C, et al. Impact of standardized MONitoring for Detection of Atrial Fibrillation in Ischemic Stroke (MonDAFIS): rationale and design of a prospective randomized multicenter study. Am Heart J. 2016;172:19–25. https://doi.org/10.1016/j.ahj.2015.10.010.
• Sposato LA, Cerasuolo JO, Cipriano LE, Fang J, Fridman S, Paquet M, et al. Atrial fibrillation detected after stroke is related to a low risk of ischemic stroke recurrence. Neurology. 2018;90:e924–31. https://doi.org/10.1212/WNL.0000000000005126. Retrospective analysis of a large registry reporting the recurrent stroke rate in stroke patients with sinus rhythm, a first episode of AF after stroke, or known AF before stroke.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Karl Georg Haeusler has received grants and personal fees from Bayer and Sanofi, personal fees from Boehringer Ingelheim, Daiichi-Sankyo, Pfizer, BMS, Medtronic, EIP Pharma, Edwards Lifesciences, and non-financial support from Getemed.
Serdar Tütüncü has received lecture fees from DTN-Kompakt (meeting/conference).
Renate B. Schnabel has received a grant from the European Research Council, and personal fees from BMS/Pfizer and the German Cardiac Society.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Haeusler, K.G., Tütüncü, S. & Schnabel, R.B. Detection of Atrial Fibrillation in Cryptogenic Stroke. Curr Neurol Neurosci Rep 18, 66 (2018). https://doi.org/10.1007/s11910-018-0871-1
Published:
DOI: https://doi.org/10.1007/s11910-018-0871-1