Abstract
Purpose
Body shame has been strongly associated with eating pathology. However, less is known about the predisposing factors linked to these feelings and how they interact with other variables in eating disorder development. Thus, the aim of the present study was to provide a preliminary understanding of the relationship between body shame and some of the major risk factors for eating disorder onset, identifying the possible mechanisms of action. Specifically, we tested a structural equation model in which perceived parental bonding, self-esteem, perfectionism, and body mass index are associated with eating disorder risk via body shame.
Methods
1156 high school students aged 13–20 were screened by means of self-report measures of parental behavior, self-esteem, perfectionism, body shame and eating disorder risk. The height and weight of each individual were measured.
Results
In predicting eating disorder risk, parental protectiveness (β = 0.09), body mass index (β = 0.18), self-esteem (β = − 0.14) and body shame (β = 0.58) had a direct effect on this variable and overall our model accounted for 58% of its variance. The experience of shame related to one’s body appeared to have a considerably significant influence on eating disturbances vulnerability and it also serves as a mediator between other risk factors and eating disturbance risk. A series of multi-group analyses indicated no significant difference between males and females.
Conclusion
The emotion of shame may enhance our understanding of eating disorders, as well as being a salient factor for the development of preventive programs and treatment approaches.
Level of evidence
Level V, cross-sectional descriptive study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Body shame is the shame one feels about one’s body or any part of it [1] and it can also relate to how one’s body functions [2]. Despite considerable evidence on the association between these feelings and eating disorders (EDs), there is little consensus regarding the specific role of body shame in the onset, development, and maintenance of these disorders.
Evidence shows that the feelings of shame regarding one’s body might be a strong predictor of eating pathology [3, 4], especially of binge eating symptoms [5, 6]. On the other hand, other authors consider body shame as a consequence of eating disturbances [7]. Shame may be described both as cause and consequence of EDs. In this regard, there is increased recognition of a bidirectional association between body shame and ED symptoms. Goss and Gilbert [2] offered a model process based on risk factors (i.e., genetic factors, personality, early attachment history, abuse or rejection experiences) that might predispose people to develop both shame proneness and ED proneness. To defend themselves against negative social outcomes depending on shame, individuals may focus their attention on body shape and weight. Then, they may feel proud of their ability to manage their weight, but when they are not able to do so, they feel further shame. This leads to a shame–pride circle that maintains the pathology.
Overall, the literature supports the suggestion that shame proneness is strongly associated with several psychological characteristics generally related to ED [8], such as self-esteem and perfectionism.
Self-esteem is defined as a person’s perception of his/her overall worth as a human being [9]. Eating disorders might be considered self-esteem disorders, to cure this low self-concept patients use illusory compensations, which gets displaced onto controlling eating, weight, and fat [10]. However, some studies do not support the existence of a direct relationship between low self-esteem and eating pathology, and future studies should further investigate how self-esteem interacts with other predictor variables [11]. In this regard, self-esteem has been suggested to predict disordered eating via body shame [12], also among obese youth [13]. It would seem that body mass index (BMI) plays a more important role in promoting the risk factors for EDs [14], and the relationship between obesity and shame feelings has also been suggested [15]. Body shame appears linked to higher BMI and to greater weight stigma [16]. For overweight adolescents girls, higher levels of mindfulness were associated with a better perception of quality of life through lower shame about body [17]. To answer the question of what causes a high BMI, in a study about the influence of parental care in childhood on the risk of obesity in young adulthood, parental neglect was found to significantly affect the risk of adult obesity, independently of age and body mass index in childhood, sex, and social background. Instead, receiving overprotective parental support had no effect [18].
Perfectionism is a personality trait that is characterized by setting excessively high personal standards of performance [19]. Overall, existing literature supports the relationship between perfectionism and eating pathologies. Perfectionism seems to predict ED onset and maintaining [20]. Individuals with high levels of perfectionism might be at risk for long disease duration and poor prognoses [21]. An experimental study has suggested that perfectionism is a causal risk factor for ED pathology [22]. Nonetheless, some studies have not found a direct relationship between perfectionism and eating problems [23] and the specific mechanism by which perfectionism uses its influence on eating psychopathology has up until now not been recognized. Recently, body image-related perfectionistic self-presentation appears to play a central role in the relationship between shame and eating pathology [24, 25].
Furthermore, there is also evidence showing the impact of body shame in mediating early life experiences and disordered eating attitudes. In an interesting study involving men from the Portuguese general community, Oliveira and colleagues [26] suggested that feelings of shame acted as a mediator between the lack of early positive emotional experiences with peers and negative body attitude. Similarly, body shame mediated the longitudinal relationship between bullying experiences and disordered eating in a sample of adolescent girls [27]. Body shame plays also an important mediator role on the association between experiences of childhood physical and sexual abuse and bulimic attitudes [28]. For the author, body shame, related to traumatic bodily experience, is a subjective feeling related to how others have treated one’s body, and cannot be accounted for body dissatisfaction. In both male and female adult survivors, the absence of well-defined body boundaries mediated the association between childhood sexual abuse and body shame [29].
Moreover, several studies have provided evidence associating the shame to negative experiences of parental care. A parenting style based on low care–high control, intrusiveness, and overprotectiveness has been shown to be the most frequent type amongst ED patients [30] and several variables have been considered as possible mediating factors on the association between parental bonding and eating problems. In this sense, parental bonding seems to have a relevant impact on the offspring’s self-concept and low self-esteem that, in turn, affects ED vulnerability [31, 32]. Furthermore, the perception of low parental care and high parental protectiveness in childhood has been found to be related to increased shame in the young adult [33]. Leung, Thomas, and Waller [34] identify perceived parental bonding as a risk factor for the later development of unhealthy core beliefs, including shame, in eating disordered patients, particularly anorexic women. Murray and colleagues [35] suggested that when individuals perceive their families as problematic, it might be clinically important to focus on shame as a psychological consequence of that experience. In their study, shame proneness acted as a moderator and internalized shame was a perfect mediator in the link between paternal overprotection and bulimic attitudes. Turner et al. [36] found that Young Schema Questionnaire scores relating to defectiveness/shame and dependence/incompetence were mediators in the relationship between parental bonding and eating disorder symptoms. On the other hand, it has been shown that parental bonding does not predict the vulnerability to body image shame, directly or indirectly. Body image esteem, global self-worth, appearance comparison and internalization of the thin ideal have been found to account for the 62% of the variance in body image shame [37].
The current study
In sum, body shame has been strongly associated with eating pathology and it may represent a vital step on the pathway to eating disturbances. However, less is known about the predisposing factors linked to these feelings and how they interact with other variables in eating disorder development. Thus, the aim of the present study was to explore the relationship between body shame and some of the major risk factors for eating disorder onset in a non-clinical sample of adolescents with structural equation modeling. Consistently with the findings of the research reviewed in the previous section, we hypothesized that perceived parental bonding, self-esteem, perfectionism and BMI did not have a direct effect on eating disorder risk. In our opinion, one potential mean by which these variables are related to ED vulnerability is through their effects on body shame. Furthermore, we tested the following set of direct relationships implied by our hypotheses: from parental care and parental protectiveness to self-esteem; from parental care and parental protectiveness to BMI; from parental care and parental protectiveness to body shame; from BMI to body shame; from self-esteem to maladaptive and adaptive perfectionism; from self-esteem to body shame; from maladaptive and adaptive perfectionism to body shame; from body shame to eating disorder risk. Understanding this mechanism could result in an enhanced conceptualization of some ways in which the variables reported above may lead to eating pathology.
A multi-group invariance analysis was also performed to state if the measurement and the structural models were equivalent across gender. Understanding that males and females share a similar process may support the choice of particular therapeutic strategies to improve the prevention/treatment of eating pathologies and its outcome.
Methods
Our study has been approved by the Ethics Board of the Department of Psychology and by the Ethics Committee of the University of Campania.
Participants and procedure
Italian adolescents 13–20 years old, still living at home, were considered eligible to participate in the present study. There were no exclusion criteria.
The study was presented to the participating schools’ students as a large survey about their feelings about themselves and their eating behaviors. It was explained that participation in the research was voluntary and that responses were anonymous and confidential. All of them agreed to participate and signed an informed consent form. Parental permission was requested and signed for subjects who were younger than 18.
Adolescents were given all the self-report questionnaires which were completed collectively during school time in the presence of the researcher. The height and weight of each individual were measured after the completion of questionnaires. After the procedure, the participants were debriefed.
Measures
Demographic data
Participants were asked to fill in a form with information about age, gender and parents’ education level.
Parental bonding
Parental bonding instrument (PBI) [38] is a 50-item self-report questionnaire to measure parental behavior as perceived by the offspring. Two principal areas of parental behaviors are investigated: parental care (behaviors indicating affection and warmth or coldness and rejection) and parental overprotection (behaviors indicating encouragement of autonomy/independence as opposed to strict control with regulations and intrusiveness). Participants were asked to rate how much they agreed with various statements (e.g., “Spoke to me in a warm and friendly voice”). Response options for items range from 3 (“very like”) to 0 (“very unlike”); however, not all items are scored in the same direction. The PBI was asked separately for each participant’s mother and father. In the study of Parker et al. [38], split-half reliability was 0.88 for the care scale and 0.74 for the protection scale in the non-clinical sample.
Self-esteem
The Rosenberg Self-Esteem Scale (RSES) [9] is a 10-item self-report measure that assesses global self-esteem. A sample item from the RSES is “I feel I do not have much to be proud of”. Participants answered each item using a four point scale from 0 (“Strongly agree”) to 3 (“Strongly disagree”). Scores range from 0 to 30, with lower scores indicating lower self-esteem. Rosenberg [9] reported test–restest correlations ranging from 0.82 to 0.88 and internal consistency values from 0.85 to 0.88.
Shame
The Experience of Shame Scale (ESS) [1] is a 25-item questionnaire to assess the frequency of shame experiences over the past year related to one’s character (e.g., “Have you felt ashamed of any of your personal habits?”), behavior (e.g., “Have you tried to hide or dissimulate things you feel ashamed to have done?”) and body (e.g., “Have you avoided to look at yourself in the mirror?”). Participants answered each item using a four point scale from 1 (“Not at all”) to 4 (“Very much”). In the original paper [1], the internal consistency was 0.92 for the total scale and 0.90, 0.87 and 0.86 for the subscales. Although participants completed the entire ESS, only Bodily Shame subscale was relevant to our hypothesis.
Perfectionism
The Multidimensional Perfectionism Scale (MPS) [19] identifies six dimensions of the perfectionism construct (excessive concern over making mistakes, high personal standards, the perception of high parental expectations, the perception of high parental criticism, the doubting of the quality of one’s actions and a preference for organization and order). Participants had to rate how much they agreed with 35 statements using a five point scale from “Strongly agree” to “Strongly disagree” (e.g., “Organization is very important to me”). Frost [14] reported an internal consistency value of 0.90 for the total perfectionism and values ranging from 0.77 to 0.93 for the six subscales.
Eating disturbance
Eating Disorders Inventory-3 (EDI-3) [39] is a self-report questionnaire used worldwide both in research and clinical work as a screener or as a tool to assess the level of symptomatology associated with eating disturbances. The present study evaluated only the Eating Disorder Risk Composite (EDRC) scale. The EDRC scale appears well suited for recognizing ED patients, including those with Binge Eating Disorder and Eating Disorder Not Otherwise Specified, and identifying subjects at risk for EDs [39, 40]. It is composed of three scales of eating disorder symptoms (i.e., drive for thinness, bulimia, and body dissatisfaction): the first scale measures the concerns about dieting, preoccupation of diet restrictions, and fear of weight gain; the second scale measures the tendency to think about or engage in uncontrollable overeating, purging to lose weight, and being emotionally upset in response to these behaviors; the last scale measures the overall feelings with the shape and size of one’s body. Participants were asked to rate how much they agreed with 25 statements (e.g., “I eat sweets and carbohydrates without feeling nervous”, “I feel extremely guilty after overeating”) with answers ranging over a scale from 0 (“always”) to 4 (“never”), with higher scores indicating a higher ED risk.
Body mass index
Each individual was weighed and measured in height.
A summary of the means, standard deviations and Cronbach’s alpha reliabilities for all variables under study are reported in Table 1.
Statistical analysis
Descriptive statistical analysis was carried out using SPSS 20 version.
Structural equation modeling (SEM) analysis were performed using LISREL 8.80 software [41]. As suggested by authors [42], we used a two-step approach to structural equation modeling, where the measurement model is tested before testing the structural model.
To account for non-normality of the data, asymptotic covariance matrices and maximum likelihood with robust standard errors (RML) were used as estimation methods. Consistent with Hoyle and Panter’s [43] recommendations, we considered multiple indices of fit from these different families: (a) the root mean square error of approximation (RMSEA; absolute fit index) [44]; (b) the standardized root mean square residual (SRMR; absolute fit index); (c) the comparative fit index (CFI; incremental fit index) [45]; (d) the non-normed fit index (NNFI; incremental fit index) [46].
Nested model fit differences were determined using a test on the difference between Chi square for the models. Given that our data departed evidently from multivariate normality, the Satorra–Bentler scaled Chi square statistic was preferred, according to the method developed by the authors [47].
Finally, a multi-group invariance analysis was performed to state if the measurement and the structural models were equivalent across gender. To test invariance, constrained and unconstrained models were compared using the CFI value. If a difference in CFI value > 0.01 [48] emerged, it indicated that the model fit was worse when parameters were fixed to be identical between groups and, therefore, that parameters were not invariant.
All path coefficients were considered statistically significant at p < 0.05.
Results
Preliminary analyses
A total of 1250 questionnaires were released, among which 1156 were included for the data analysis based on the number of returned valid questionnaires. Students who had completed less than 80% of the responses on any of the instruments in the research were omitted.
Preliminary screening data revealed that less than 1% of cases for each variable reported missing values. Missing values were dispersed randomly across items and participants, and were replaced with mean values.
Description of the sample
The sample included 1156 adolescents (640 females and 516 males) aged between 13 and 20 years (M 15.61, SD 1.56). Most participants (N = 591, 51.1%) fell into the high to the middle socio-economic category. About 80% of parents held a diploma of higher education or less. In the current sample, 26 (2.2%) adolescents were underweight, 829 (71.7%) adolescents had normal weight, 227 (19.6%) were overweight, and 74 (6.4%) were obese.
Examination of the structural model
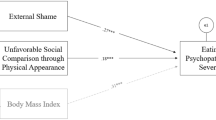
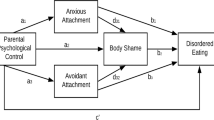
To establish an initial structural model, we first tested the hypothesized structural model A printed in Fig. 1. As shown in Table 2, the results indicated that the hypothesized model was a good fit to the data. All hypothesized paths were significant (except the path from maladaptive and adaptive perfectionism to body shame, the path from parental protection and parental care to body shame and the path from parental protection to BMI). The non-significant paths were eliminated and the model rerun. The fit did not improve and the difference in SBχ2 between the model A and the resulting model A2 was not significant; consequently, the model A2 that had fewer paths and was more parsimonious was accepted. Model A2 illustrating the relationship among measured variables via standardized regression coefficients and the percentage of variance explained is printed in Fig. 2.
Hypothesized structural model A. BMI body mass index, RSES1 Rosenberg Self-Esteem Scale parcel 1, RSES2 Rosenberg Self-Esteem Scale parcel 2, CM MPS concern over mistakes, PE MPS parental expectations, PS MPS personal standards, DA MPS doubts about actions, ORG1 MPS organization parcel 1, ORG2 MPS organization parcel 2, BS1 ESS bodily shame parcel 1, BS2 ESS bodily shame parcel 2, DT EDI-3 drive for thinness, BU EDI-3 bulimia, BD EDI-3 body dissatisfaction. Red lines represent non significative paths
Model A2, standardized path coefficients and percentage of variance explained. BMI body mass index, RSES1 Rosenberg Self-Esteem Scale parcel 1, RSES2 Rosenberg Self-Esteem Scale parcel 2, CM MPS concern over mistakes, PE MPS parental expectations, PS MPS personal standards, DA MPS doubts about actions, ORG1 MPS organization parcel 1, ORG2 MPS organization parcel 2, BS1 ESS bodily shame parcel 1, BS2 ESS bodily shame parcel 2, DT EDI-3 drive for thinness, BU EDI-3 bulimia, BD EDI-3 body dissatisfaction. Correlations among residual variances are not reported for purpose of clarity
The model fit was high. However, we examined an alternative model to further provide evidence for our model and to let for the possibility of effects not captured by our proposed full mediating pathways. Thus, a partially mediated model (model B) was tested. Fit indices for all of these structural models are listed in Table 2.
While the paths from self-esteem, BMI, parental protectiveness to ED risk resulted to be significant, the paths from parental care, maladaptive and adaptive perfectionism to ED risk resulted to be not significative. Model difference testing, using the procedure described previously, indicated that this partially mediated model (model B) fits better than the fully mediated model (model A2). Subsequently, the non-significant paths were eliminated and the model was re-estimated resulting in the model B2. The difference in SBχ2 between the model B2 and the model B was not significative; thus, the more parsimonious model B2 was chosen as the final model in the present study.
The final model with standardized path coefficients and percentage of variance explained is printed in Fig. 3, without measured variables for purposes of clarity. Parental care and protectiveness were significantly related to self-esteem, suggesting that participants who reported higher parental care and lower parental protectiveness also reported higher self-esteem. Perceived parental bonding accounted for 30% of self-esteem variance. Self-esteem was negatively related to dysfunctional as well as positively to functional perfectionism. In predicting maladaptive perfectionism, self-esteem accounted for 44% of its variance; instead, regarding adaptive perfectionism, self-esteem accounted only for 3% of its variance. In predicting body shame, only self-esteem and BMI were significant predictors, explaining 40% of its variance. In predicting BMI, parental care was a significant and negative predictor (not parental protectiveness), even if it accounted just for 1% of BMI variance. In predicting eating disorder risk, parental protectiveness, BMI, self-esteem and, body shame had a direct effect on this variable and overall our model accounted for 58% of its variance. However, self-esteem (standardized indirect coefficient = − 0.35) and BMI (standardized indirect coefficient = 0.09) had also an indirect effect on ED risk via body shame, whereas parental protectiveness (standardized indirect coefficient = 0.10) and parental care (standardized indirect coefficient = − 0.24) had an indirect effect on ED risk via self-esteem.
Overall model cross-validation
The complete sample was randomly split in half, to test cross-validation of the final model. The results indicated that the overall final model tested on these two random groups (n = 578; n = 578) were cross-validated.
Gender differences in the model
As a prerequisite to testing for multi-group invariance, it is customary to consider a baseline model separately estimated for each group [49]. Then, we proceed to the formal test of invariance in three steps [50]: (1) configural invariance; (2) measurement invariance; (3) structural invariance. The history of the changes in fit is reported in Table 3.
As a first step, the hypothesized model was fitted for each group (baseline models) and it demonstrated a satisfactory fit to the data in both male and female participants. Successively, the same parameters that were estimated in the baseline model for each group separately were estimated again for all groups at the same time (configural invariance) [49], resulting in a good fit.
Then, a model in which factor loadings were constrained to be equal across groups (measurement invariance) was compared with the baseline model specifying no constraints and previously tested (configural invariance). Testing for invariant factor loadings has also been designated as tests for “metric invariance” [51]. The non-significant difference in the CFI values between the configural and the metric invariance models suggested that there was a full measurement invariance.
Successively, equality restrictions were imposed on the variance/covariance factors and on the regression paths. There was no significant change in fit between metric and structural invariance models; hence, there was evidence for a structural invariance between males and females.
Discussion
The purpose of this study is to test a structural equation model examining the potential mediating roles, in the link between perceived parental bonding, self-esteem, perfectionism, body mass index and eating disorder risk, of body shame. Data only partially supported the hypothesized model and several interesting findings emerged.
Regarding the determinants of body shame, the current data did not support our hypothesis that parental care and protectiveness were direct predictors of this variable. This agrees with findings from other researchers [37]. One reason for this may be that parental bonding had merely an indirect influence on body shame via self-esteem and BMI. Indeed, as predicted, self-esteem and BMI were each predictive of increased vulnerability of body shame. In particular, results highlight the importance of low self-esteem as a source of body shame. People who perceive themselves as inadequate or unworthy may be at greater risk of experiencing body shame [52].
A number of studies have documented an association between a bonding behavior pattern characterized by low care and high protectiveness and eating symptomatology [30, 53]. In a clinical sample of women with eating disorders, lower mother care was directly related to poorer body image, while low levels of father care have been shown to be indirectly associated with body dissatisfaction mediated by attachment anxiety and media internalization [54]. Our results pointed out a non-significant direct association between poor parental care and ED risk, but a significant indirect effect via low self-esteem. This datum is consistent with earlier empirical research [31].
Moreover, the association between parental care and ED risk was mediated through BMI. Thus, adolescents who are ignored or neglected by their parents may be at the greatest risk of developing obesity and eating problems. This finding concurs with evidence that only parental care, but not protectiveness, is predictive of high BMI [18]. There are several possible explanations for such a result. The existence of possible mediating variables, such as interoceptive awareness, in the relationship between parental protectiveness and BMI could be hypothesized. In this manner, parental protectiveness could not allow individuals to develop a sense of personal needs, altering interoceptive awareness and, consequently, eating behavior. Future empirical studies should investigate this suggestion.
In line with a previous study [32], our hypothesis that parental protectiveness had a direct effect on low self-esteem, and in turn on ED risk, was confirmed. However, parental protectiveness had also a direct effect on eating disturbance vulnerability. These findings add to the literature on psychological control documenting a direct relationship between parental protectiveness (but not care) and eating disorder proneness. As such, this finding suggests that overprotectiveness may be more directly relevant to eating disturbance development. Research should further explore this datum and examine the usefulness of differentiating the separate contribution of maternal and paternal bonding in the etiology of eating pathologies.
Furthermore, another hypothesis that did not receive empirical support was that perfectionism predicted body shame. However, the most striking finding was that both maladaptive and adaptive perfectionism had no influence on ED risk, directly or indirectly [55]. In our opinion, one possible interpretation of the present finding is that perfectionism could be considered as a correlate of low self-esteem and, therefore, as a mere psychological characteristic typically associated with eating disturbances. Several studies have associated to varying degrees eating disorder patterns, perfectionism and low self-esteem [56, 57]. Literature supports the hypothesis that a combination of a low perception of control and a low self-esteem moderates the effects of perfectionism on drive for thinness, bulimia and body dissatisfaction [10]. In our study, self-esteem emerged as a significant predictor of both maladaptive and adaptive perfectionism. Particularly, the linkage between low self-esteem and maladaptive perfectionism was particularly strong. This is in harmony with the hypothesis that striving to appear perfect is an attempt to compensate for low self-esteem. For eating disordered individuals, mistakes and failings may be interpreted as evidence of personal deficiencies [58]. In this perspective, to be flawless represents an obligation. However, future research is needed to better investigate further variables that may mediate the relationship between perfectionism and eating disorder risk.
Body shame was hypothesized to act as a mediator in the relationship between self-esteem and eating disorder risk. In line with previous studies [12, 13], our results corroborated this suggestion. Although 71% is the proportion of the effect that is mediated via body shame, self-esteem had also a direct influence on ED risk. Our data expand earlier studies which have described low self-esteem as a critical predictor of ED vulnerability [59].
Moreover, the association between BMI and eating disturbance vulnerability was partially mediated by body shame. Even after the mediating effects were taken into account, BMI had a positive direct effect on the variable under study and remained a strong predictor of eating disorder risk. Undeniably, a high BMI has even been considered as an ED risk factor [14].
Another important contribution of this research is to demonstrate that two different groups, males and females, emerge to share a similar process involving parental bonding, self-esteem, BMI, perfectionism, shame and eating disorder risk. Therefore, the present study represents a helpful first step suggesting that males and females could be subject to the same prevention programs and treatment approaches.
Conclusion
Most of the studies about the eating disorder onset have been focused on the risk factors unconnectedly, precluding understanding about interactive effects. This is the first study that conceptualizes how a number of risk factors may work together to create a pathway to eating pathologies. Collectively, perceived parental care and protectiveness, self-esteem, maladaptive and adaptive perfectionism, body shame and BMI account for 58% of the variance in eating disorder risk. Therefore, these initial findings suggest a promising model.
In our opinion, the perception of parental hyper-involvement and lack of sufficient caring may produce a feeling of ineffectiveness and impoverished self, which may be the root of eating psychopathologies. It would seem that for these individuals the body became responsible for the sense of general ineffectiveness, the stages of the illness and this would produce body shame: “I am not inadequate, but my body is”. From that perspective, eating disorders could be an attempt to change their unattractive and undesirable body shape. This suggestion goes in line with literature that has shown that body compassion attenuates the impact of general feelings of shame on body image shame and disordered eating [60]. The impact of body shame in mediating different dimensions of fears of compassion and disordered eating attitudes has also been reported [61].
Unfortunately, few studies have investigated the role of body shame in ED onset. In the current research, the experience of shame related to one’s body appeared to have a considerably significant influence on eating disturbances vulnerability. This finding supported results of other studies which have reported that body shame is a strong predictor of disordered eating [3] and of ED symptom severity [62].
Additionally, body shame is not only a critical independent indicator of ED propensity, but it also serves as a mediator between other risk factors and eating disturbance risk. This is an important issue since it highlights the potential role of body shame as a key variable in explaining an increased eating pathology risk and as a core diagnostic feature of all eating disturbances. Further studies on this construct would be very useful.
The results of the present study have implications for EDs prevention and treatment. Our findings may help mental health professionals to identify which areas of the parent–child relationship and which personal factors are most relevant in the etiology of EDs and should therefore be the principal targets of preventive and/or intervention programs during adolescence. Clinicians should consider the routine assessment and treatment of these factors. First and foremost, intervention programs ought to be addressed to reduce subjective feelings of ineffectiveness and shame. Special attention should be paid to obese youth.
Limitations
The present research was limited by its use of self-report instruments and cross-sectional design. Exclusively southern Italian youths were included in the present study and further research is needed to assess the generalizability of the results. Then, our study neglected genetic and environmental variables such as specific phenotypes and sociocultural pressure for thinness. Race/ethnicity was not collected. Thus, added variables should be considered. Mean imputation is a widely used method and although not always shared, it has shown to perform equally well with low overall number of missing values [63]. However, future studies would benefit from a more sophisticated missing data approach. Since reciprocal causation among variables might occur, studies using non-recursive models should be realized. Finally, rather than focused on a measure of anorexic or bulimic psychopathology, this study used a generic measure of eating disorder vulnerability, that includes body dissatisfaction. Further research is needed to clarify the distinction between body shame and body dissatisfaction.
References
Andrews B, Qian M, Valentine JD (2002) Predicting depressive symptoms with a new measure of shame: the experience of shame scale. Br J Clin Psychol 41:29–42. https://doi.org/10.1348/014466502163778
Goss K, Gilbert P (2002) Eating disorders, shame and pride: a cognitive-behavioural functional analysis. In: Gilbert P, Miles J (eds) Body shame: conceptualisation, research and treatment. Brunner-Routledge, Hove, pp 219–255
Troop NA, Redshaw C (2012) General shame and bodily shame in eating disorders: a 2.5-year longitudinal study. Eur Eat Disord 20:373–378. https://doi.org/10.1002/erv.2160
Doran J, Lewis CA (2012) Components of shame and eating disturbance among clinical and non-clinical populations. Eur Eat Disord 20:265–270. https://doi.org/10.1002/erv.1142
Duarte C, Pinto-Gouveia J, Ferreira C (2014) Escaping from body image shame and harsh self-criticism: exploration of underlying mechanisms of binge eating. Eat Behav 15:638–643. https://doi.org/10.1016/j.eatbeh.2014.08.025
Higgins MK, Lin SL, Alvarez A, Bardone-Cone AM (2015) Examining impulsivity as a moderator of the relationship between body shame and bulimic symptoms in Black and White young women. Body Image 14:39–46. https://doi.org/10.1016/j.bodyim.2015.03.007
Skårderud F (2007) Shame and pride in anorexia nervosa: a qualitative descriptive study. Eur Eat Disord 15:81–97. https://doi.org/10.1002/erv.774
Cavalera C, Pagnini F, Zurloni V, Diana B, Realdon O, Castelnuovo G, Todisco P, Molinari E (2016) Shame proneness and eating disorders: a comparison between clinical and non-clinical samples. Eat Weight Disord 21:701–707. https://doi.org/10.1007/s40519-016-0328-y
Rosenberg M (1965) Society and the adolescent self-image. Princeton University Press, Princeton
Sassaroli S, Gallucci M, Ruggiero GM (2008) Low perception of control as a cognitive factor of eating disorders. Its independent effects on measures of eating disorders and its interactive effects with perfectionism and self-esteem. J Behav Ther Exp Psy 39:467–488. https://doi.org/10.1016/j.jbtep.2007.11.005
Shea ME, Pritchard ME (2007) Is self-esteem the primary predictor of disordered eating? Pers Individ Differ 42:1527–1537. https://doi.org/10.1016/j.paid.2006.10.026
Tylka TL, Subich LM (2004) Examining a multidimensional model of eating disorder symptomatology among college women. J Couns Psychol 51:314–328. https://doi.org/10.1037/0022-0167.51.3.314
Iannaccone M, D’Olimpio F, Cella S, Cotrufo P (2016) Self-esteem, body shame and eating disorder risk in obese and normal weight adolescents: a mediation model. Eat Behav 2:80–83. https://doi.org/10.1016/j.eatbeh.2015.12.010
Sim LA, Lebow J, Billings M (2013) Eating disorders in adolescents with a history of obesity. Pediatrics 132:e1026–e1030. http://www.pediatrics.org/. https://doi.org/10.1542/peds.2012-3940
Sjöberg RL, Nilsson KW, Leppert J (2005) Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics 116:e389–e392. https://doi.org/10.1542/peds.2005-0170
Mensinger JL, Tylka TL, Calamari ME (2018) Mechanisms underlying weight status and healthcare avoidance in women: a study of weight stigma, body-related shame and guilt, and healthcare stress. Body Image 25:139–147. https://doi.org/10.1016/j.bodyim.2018.03.001
Moreira H, Canavarro MC (2017) Is body shame a significant mediator of the relationship between mindfulness skills and the quality of life of treatment-seeking children and adolescents with overweight and obesity? Body Image 20:49–57. https://doi.org/10.1016/j.bodyim.2016.11.004
Lissau I, Sørensen TI (1994) Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet 5:324–327. https://doi.org/10.1016/S0140-6736(94)91163-0
Frost RO, Marten P, Lahart CM, Rosenblate R (1990) The Dimensions of perfectionism. Cogn Ther Res 14:449–468. https://doi.org/10.1007/BF01172967
Holland LA, Bodell LP, Keel PK (2013) Psychological factors predict eating disorder onset and maintenance at 10-year follow-up. Eur Eat Disord 21:405–410. https://doi.org/10.1002/erv.2241
Egan SJ, Wade TD, Shafran R (2011) Perfectionism as a transdiagnostic process: a clinical review. Clin Psychol Rev 31:203–212. https://doi.org/10.1016/j.cpr.2010.04.009
Boone L, Soenens B, Vansteenkiste M, Braet C (2012) Is there a perfectionist in each of us? An experimental study on perfectionism and eating disorder symptoms. Appetite 59:531–540. https://doi.org/10.1016/j.appet.2012.06.015
Joyce F, Watson HJ, Egan SJ, Kane RT (2012) Mediators between perfectionism and eating disorder psychopathology in a community sample. Eat Behav 13:361–365. https://doi.org/10.1016/j.eatbeh.2012.07.002
Ferreira C, Trindade IA, Ornelas L (2015) Exploring drive for thinness as a perfectionistic strategy to escape from shame experiences. Span J Psychol 20:18:E29. https://doi.org/10.1017/sjp.2015.27
Marta-Simões J, Ferreira C (2016) Seeking a perfect body look: feeding the pathogenic impact of shame? Eat Weight Disord 21:477–485. https://doi.org/10.1007/s40519-015-0240-x
Oliveira S, Trindade IA, Ferreira C (2018) Explaining male body attitudes: the role of early peer emotional experiences and shame. Eat Weight Disord. https://doi.org/10.1007/s40519-018-0569-z
Duarte C, Pinto-Gouveia J, Stubbs RJ (2017) The prospective associations between bullying experiences, body image shame and disordered eating in a sample of adolescent girls. Pers Individ Differ 116:319–325. https://doi.org/10.1016/j.paid.2017.05.003
Andrews B (1997) Bodily shame in relation to abuse in childhood and bulimia: a preliminary investigation. Br J Clin Psychol 36:41–49. https://doi.org/10.1111/j.2044-8260.1997.tb01229.x
Talmon A, Ginzburg K (2018) “Body self” in the shadow of childhood sexual abuse: the long-term implications of sexual abuse for male and female adult survivors. Child Abuse Negl 76:416–425. https://doi.org/10.1016/j.chiabu.2017.12.004
Jáuregui Lobera I, Bolaños Ríos P, Garrido Casals O (2011) Parenting styles and eating disorders. J Psychiatr Ment Health Nurs 18:728–735. https://doi.org/10.1111/j.1365-2850.2011.01723.x
Perry JA, Silvera DH, Neilands TB, Rosenvinge JH, Hanssen T (2008) A study of the relationship between parental bonding, self-concept and eating disturbances in Norwegian and American college populations. Eat Behav 9:13–24. https://doi.org/10.1016/j.eatbeh.2007.01.007
Cella S, Iannaccone M, Cotrufo P (2014) How perceived parental bonding affects self-concept and drive for thinness: a community-based study. Eat Behav 15:110–115. https://doi.org/10.1016/j.eatbeh.2013.10.024
Lutwak N, Ferrari JR (1997) Understanding shame in adults: retrospective perceptions of parental bonding during childhood. J Nerv Ment Dis 185:595–598. https://doi.org/10.1097/00005053-199710000-00001
Leung N, Thomas G, Waller G (2000) The relationship between parental bonding and core beliefs in anorexic and bulimic women. Br J Clin Psychol 39:205–213. https://doi.org/10.1348/014466500163220
Murray C, Waller G, Legg C (2000) Family dysfunction and bulimic psychopathology: the mediating role of shame. Int J Eat Disord 28:84–89. https://doi.org/10.1002/(SICI)1098-108X(200007)28
Turner HM, Rose KS, Cooper MJ (2005) Parental bonding and eating disorder symptoms in adolescents: the meditating role of core beliefs. Eat Behav 6:113–118. https://doi.org/10.1016/j.eatbeh.2004.08.010
Markham A, Thompson T, Bowling A (2005) Determinants of body-image shame. Pers Individ Differ 38:1529–1541. https://doi.org/10.1016/j.paid.2004.08.018
Parker G, Tupling H, Brown LB (1979) A parental bonding instrument. Br J Med Psychol 52:1–10. https://doi.org/10.1111/j.2044-8341.1979.tb02487.x
Garner DM (2004) Eating Disorder Inventory-third edition (EDI-3). Psychological Assessment Resources, Lutz
Segura-García C, Aloi M, Rania M, Ciambrone P, Palmieri A, Pugliese V, Ruiz Moruno AJ, De Fazio P (2015) Ability of EDI-2 and EDI-3 to correctly identify patients and subjects at risk for eating disorders. Eat Behav 19:20–23. https://doi.org/10.1016/j.eatbeh.2015.06.010
Jöreskog KG, Sörbom D (2006) LISREL 8.80 for Windows. Scientific Software International, Lincolnwood
Anderson JC, Gerbing DW (1988) Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull 103:411–423. https://doi.org/10.1037/0033-2909.103.3.411
Hoyle RH, Panter AT (1995) Writing about structural equation models. In: Hoyle RH (ed) Structural equation modeling: concepts, issues, and applications. Sage, Newbury Park
Steiger JH (1990) Structural model evaluation and modification: an interval estimation approach. Multivar Behav Res 25:173–180. https://doi.org/10.1207/s15327906mbr2502_4
Bentler PM (1990) Comparative fit indexes in structural models. Psychol Bull 107:238–246. https://doi.org/10.1037/0033-2909.107.2.238
Bentler PM, Bonnet DC (1980) Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull 88:588–606. https://doi.org/10.1037/0033-2909.88.3.588
Satorra A, Bentler PM (2001) A scaled difference Chi-square test statistic for moment structure analysis. Psychometrika 66:507–514. https://doi.org/10.1007/BF02296192
Cheung GW, Rensvold RB (2002) Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model 9:233–255. https://doi.org/10.1207/S15328007SEM0902_5
Byrne BM (1998) Structural equation modeling with LISREL, PRELIS and SIMPLIS: basic concepts, applications and programming. Lawrence Erlbaum Associates Publishers, Mahwah
Byrne BM (2006) Structural equation modeling with EQS: basic concepts, applications and programming, 2nd edn. Lawrence Erlbaum Associates Publishers, Mahwah
Horn JL, McArdle JJ (1992) A practical and theoretical guide to measurement invariance in aging research. Exp Aging Res 105:117–144. https://doi.org/10.1080/03610739208253916
Tangney JP (1992) Situational determinants of shame and guilt in young adulthood. Pers Soc Psychol Bull 18:199–206. https://doi.org/10.1177/0146167292182011
Swanson H, Power K, Collin P, Deas S, Paterson G, Grierson D, Yellowlees A, Park K, Taylor L (2010) The relationship between parental bonding, social problem solving and eating pathology in an anorexic inpatient sample. Eur Eat Disord 18:22–32. https://doi.org/10.1002/erv.967
Grenon R, Tasca GA, Maxwell H, Balfour L, Proulx G, Bissada H (2016) Parental bonds and body dissatisfaction in a clinical sample: the mediating roles of attachment anxiety and media internalization. Body Image 19:49–56. https://doi.org/10.1016/j.bodyim.2016.08.005
Levinson CA, Rodebaugh TL, White EK, Menatti AR, Weeks JW, Iacovino JM, Warren CS (2013) Social appearance anxiety, perfectionism, and fear of negative evaluation: distinct or shared risk factors for social anxiety and eating disorders? Appetite 67:125–133. https://doi.org/10.1016/j.appet.2013.04.002
Fairburn CG (1995) Overcoming binge eating. Guilford Press, New York
Wade TD, Wilksch SM, Paxton SJ, Byrne SM, Austin SB (2015) How perfectionism and ineffectiveness influence growth of eating disorder risk in young adolescent girls. Behav Res Ther 66:56–63. https://doi.org/10.1016/j.brat.2015.01.007
Hewitt PL, Flett GL, Ediger E (1995) Perfectionism traits and perfectionistic self-presentation in eating disorder attitudes, characteristics, and symptoms. Int J Eat Disord 18:317–326. https://doi.org/10.1002/1098-108X(199512)18:4%3C317
Button EJ, Loan P, Davies J, Sonuga-Barke EJ (1997) Self-esteem, eating problems, and psychological well-being in a cohort of schoolgirls aged 15–16: a questionnaire and interview study. Int J Eat Disord 21:39–47. https://doi.org/10.1002/(SICI)1098-108X(199701)21
Oliveira S, Trindade IA, Ferreira C (2018) The buffer effect of body compassion on the association between shame and body and eating difficulties. Appetite 125:118–123. https://doi.org/10.1016/j.appet.2018.01.031
Dias BS, Ferreira C, Trindade IA (2018) Influence of fears of compassion on body image shame and disordered eating. Eat Weight Disord. https://doi.org/10.1007/s40519-018-0523-0
Cella S, Cipriano A, Iannaccone M, Cotrufo P (2017) Identifying predictors associated with the severity of eating concerns in females with eating disorders. RIPPPO 20:91–99. https://doi.org/10.4081/ripppo.2017.19
Baker J, White N, Mengersen K (2014) Missing in space: an evaluation of imputation methods for missing data in spatial analysis of risk factors for type II diabetes. Int J Health Geogr 13:47. https://doi.org/10.1186/1476-072X-13-47
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
PC designed the study and wrote the protocol. SC and MI conducted literature searches and provided summaries of previous research studies. SC and MI conducted the statistical analysis and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cella, S., Iannaccone, M. & Cotrufo, P. Does body shame mediate the relationship between parental bonding, self-esteem, maladaptive perfectionism, body mass index and eating disorders? A structural equation model. Eat Weight Disord 25, 667–678 (2020). https://doi.org/10.1007/s40519-019-00670-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00670-3