Abstract
Food addiction (FA) has recently emerged as a new field in the study of obesity. Previous studies have contributed to identifying psychological correlates of FA. However, few researchers have examined the cognitive profile related to this condition; up until now, attentional biases related to food cues and a poorer performance monitoring have been observed. The present study aimed to examine the psychological profile and executive functioning related to FA in individuals with severe obesity and awaiting bariatric surgery. Participants (N = 86) were split into two groups, according to their level of FA symptoms (low FA vs high FA). Groups were compared on questionnaires measuring binge eating, depression and anxiety symptoms, and impulsivity as well as on measures reflecting executive functioning (D-KEFS and BRIEF-A). The relationship between FA groups and patterns of errors during the D-KEFS’ Color-Word Interference Test was further analyzed. Individuals within the high FA group reported significantly more binge eating, depressive and anxiety symptoms, and more metacognitive difficulties. They also tended to show a poorer inhibition/cognitive flexibility score and a typical pattern of errors, characterized by an increased number of errors as the tasks’ difficulty rose as opposed to a decreased number of errors, which characterizes an atypical pattern of errors. The present results show that the inability to learn from errors or past experiences is related to the severity of FA and overall impairments.
Level of evidence Level V, descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is an important health issue all over the world. However, despite the efforts to reduce obesity rates, the prevalence is still high. Indeed, according to the World Health Organization, the worldwide prevalence of obesity is twice as high as it was in 1980: up to 600 million adults present obesity [1]. Obesity has been associated with a lot of health issues such as metabolic syndrome, type 2 diabetes, different types of cancers, cardiovascular diseases, Alzheimer’s disease, vascular dementia, and premature death [2,3,4,5,6,7]. Notwithstanding knowledge of these life-threatening consequences, many individuals do not lose weight and/or develop healthy habits [8]. To explain how obese individuals may struggle to modify eating behaviors, many experts have highlighted similarities between obesity and addiction to substances, arguing that these individuals could be addicted to food, just as others are addicted to substances like alcohol, tobacco or opiates [9,10,11].
Food addiction
Although there is no consensual definition of FA, it is generally referred to as “A chronic and relapsing condition caused by the interaction of many complex variables that increase craving for certain specific foods in order to achieve a state of high pleasure, energy or excitement, or to relieve negative emotional or physical states” [12]. In 2009, Gearhardt, Corbin, and Brownell have modeled the DSM-IV-TR substance dependence diagnostic criteria [13, 14] to food and eating and created the Yale Food Addiction Scale (YFAS). Since then, many authors have used this self-reported questionnaire to deepen the scientific knowledge on food addiction (FA) and characterize this condition. A FA diagnosis has been observed in 5–10% of healthy individuals [13, 15, 16], 15–25% of obese individuals [17,18,19,20,21], and 16–50% of individuals suffering from severe obesity and seeking bariatric surgery [22,23,24,25]. In addition to prevalence rates, studies have shown that FA was significantly related to binge eating disorder and that individuals with FA reported more depression, anxiety, PTSD and attention deficit hyperactivity disorder (ADHD) symptoms as well as more impulsivity when compared to individuals without FA [17, 18, 21, 23, 26,27,28]. With regards to impulsivity, FA has been associated to a stronger tendency to act rashly and irrationally while experiencing intense affects, a stronger tendency to give up on tasks, and a lower ability to keep focusing on a task [29,30,31,32]. Moreover, individuals with FA also tend to report more emotion dysregulation, more harm avoidance and less self-directedness than individuals without FA [17, 22].
However, few authors have examined the neurocognitive profile related to FA. Gearhardt et al. [33] compared the cerebral activity of specific brain regions using functional magnetic resonance imaging (fMRI) in healthy and obese women who endorsed a high level of FA symptoms (three criteria or more) and a low level of FA symptoms (one criterion or less) using the YFAS [33]. Their results showed positive correlations between FA scores and activation in many regions of the brain’s reward circuit when participants had to anticipate a highly palatable food intake (anterior cingulate cortex, medial orbitofrontal cortex, and amygdala). Their results also showed that participants with high FA levels showed a weaker activation in the lateral orbitofrontal cortex compared to those with low FA levels when they had to ingest highly palatable food, which is involved in inhibition processes. Those neurophysiological similarities between FA and other substance-related and addictive disorders were recently corroborated by Imperiatori et al. (2015) who compared individuals with high vs. low levels of FA symptoms on electroencephalographic (EED) power spectra and EEG connectivity [34].
Moreover, few studies have assessed cognitive status in individuals with high levels of FA symptoms. First, Frayn et al. [35] assessed the effect of an inducted sad mood on the attention attributed to unhealthy food in women with and without FA. Comparably to individuals with alcohol dependence, women with FA paid more attention to the unhealthy food cues after the induction of a sad mood, which was not the case for women without FA. These results suggest that for individuals with FA, unhealthy food cues involve more attention resources during an emotional experience, requiring the implication of executive functioning.
Only two studies aimed to examine inhibition control in individuals with FA. Meule et al. [16] studied inhibition control in female college students with high levels of FA symptoms, by asking them to perform a Go/No-go task while high-calorie food cues or neutral images were shown in the background. Comparatively to those with lower FA symptoms, women with a more important FA symptomatology showed faster reaction times when food cues were presented in the background and reported more attentional impulsivity than the other group. However, these differences between individuals with high and low FA levels, according to the Go/No-go task, were not recently found in a sample of 181 individuals, among which almost 35% endorsed three or more food addiction symptoms; in contrast to the previous study, no food cues were presented during the Go/No-go task [32]. Considering these results, it is possible to think that in individuals with FA, inhibition abilities are influenced by contextual cues.
More recently, Franken et al. [36] assessed performance monitoring in 34 individuals with a high level of FA symptoms, using behavioral (Eriksen flanker task) and electrophysiological (EEG) measures, and compared them to a control group of individuals with a low level of FA symptoms (n = 34). Taken together, their results indicated that participants from the high FA group exhibited a poorer performance monitoring, which is the ability to detect and monitor errors. Even if the aforementioned results are not sufficient to confirm that more severe executive functions deficits characterize FA, they certainly lay the basis for more studies on this topic. Furthermore, considering that participants from previous studies exploring cognitive profile of FA were mostly normal weight and undergraduate women, it would be interesting to explore this association among other samples.
The present study aimed to deepen the psychological and cognitive understanding of this condition in a sample of individuals with severe obesity seeking bariatric surgery. More precisely, the objective of the present study was to compare participants according to the severity of FA symptoms (high vs. low) in terms of body mass index (BMI), psychological variables (binge eating, depressive, anxiety, and impulsivity), and executive functions. With respect to literature on substance-related disorders and food addiction, it was hypothesized that participants with a more severe FA symptomatology would report more severe binge eating, depressive and anxiety symptoms, and more impulsivity, as well as a higher BMI. It was also hypothesized that participants with a more severe FA symptomatology report poorer performances on planning, inhibition, cognitive flexibility and error processing as well as more self-reported complaints pertaining to executive functioning.
Materials and methods
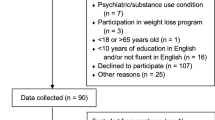
Participants and procedures
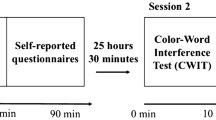
Participants were 20 men and 66 women (N = 86) suffering from severe obesity (BMI ≥ 40.0 kg/m2), recruited at the Heart and Lung Institute Research Center in Quebec City 3 months before their bariatric surgery, with support from the Research Chair in Bariatric and Metabolic Surgery. Participants were included if they were aged between 18 and 55 years old and met the criteria for bariatric surgery. Individuals who reached menopause, were pregnant/lactating, were suffering from type 2 diabetes for more than 10 years, had abnormal bowel habits, were excluded. Individuals who previously had a bariatric surgery, or presented an actual psychiatric condition that could affect the data collection (e.g., severe suicidal tendencies or psychosis) or a comorbid substance use disorder, were also excluded. During their preoperative visit, a staff member evaluated the participants’ substance use to verify whether they were eligible for the study. After giving their informed consent, participants were invited to complete two of the Delis–Kaplan Executive Function System’s subtests (D-KEFS) [37], namely the Color-Word Interference test (CWIT) and the Tower test (TT), measuring specific executive functions. Participants also received a series of questionnaires (see Measures section), which had to be filled within the following weeks and brought back upon their next hospital visit. Participants’ height and weight were measured to calculate BMI (kg/m²). The Heart and Lung Institute Research Center research ethics committee approved the study.
Participants’ average BMI was 47.68 kg/m2 (SD = 5.64). Mean age was 39.51 years (SD = 7.27) and all participants were Caucasian. Among participants, 17.4% have Type 2 diabetes, 17.4% have dyslipidemia, 43% have sleep apnea, and 31.4% have arterial hypertension. Between 76 and 89% of the participants with those conditions were receiving a treatment. Moreover, many participants reported at least one previous weight loss attempt. During their lifetime, 70.2% have subscribed to commercial diet plans, 57% have received nutrition counseling, 18% have received counseling by another health practitioner, 60.7% reported a supervised workout program, and 18% reported at least taking one prescription drug to lose weight.
Measures
Food addiction
The Yale Food Addiction Scale (YFAS) [13] was used to assess FA symptoms over the last year. It consists in a self-reported questionnaire covering FA criteria, based on the DSM-IV-TR seven diagnostic criteria for substance dependence [14]. For the present study, a 16-item version of the French YFAS that was best suited for clinical samples was used [38]. Most of the questions are answered on a five-point Likert scale, from zero (never) to four (more than four times a week or everyday), and the remaining questions are answered by yes or no. To fulfill a criterion, at least one item related to the criterion must be endorsed. Two methods have been developed to analyze the answers: it is possible to assess FA severity by summing up the endorsed criteria or to assess the presence or absence of the “FA diagnosis” if the patient has endorsed at least three criteria and reported functional impairment or clinical distress. In the present study, only the patient’s severity score was used. The 16-item version of the French YFAS yielded good internal consistency (Cronbach’s alpha of 0.85).
Binge eating
The Binge Eating Scale (BES) [39], a 16-item self-reported scale, was used to measure symptoms related to behavioral, cognitive, and emotional manifestations of binge eating episodes. For each item, the participant is asked to choose, among four statements, the one that best describes his or her situation. Each item is allocated weight, representing severity (varying between zero and three), and subsequently summed up so that total scores vary from 0 to 46. A higher total score is associated with a more severe binge eating pathology. For the present study, the internal consistency was high, with a Cronbach’s alpha of 0.87.
Depressive symptoms
The Beck Depression Inventory-II (BDI-II) [40] was used to assess depressive symptoms. The 21 items of this questionnaire refer to the depressive symptoms experienced in the last 2 weeks and each symptom is rated on a 4-point scale from zero (the symptom is not associated to any suffering) to three (the symptom is associated to intense suffering). The total score ranges from 0 to 63: a score from 0 to 13 represents normal to minimal depressive symptoms, a score from 14 to 19 represents mild to moderate depressive symptoms, a score from 20 to 28 represents moderate depressive symptoms, and a score from 29 to 63 represents severe depressive symptoms. Cronbach’s alpha of the questionnaire as determined in the current study was 0.89.
Anxiety symptoms
The State-Trait Anxiety Inventory (STAI) [41] was used to assess anxiety symptoms. The STAI is a 40-item self-report questionnaire, divided into two 20-item scales to assess the state of anxiety, which refers to a transitory condition, and the trait anxiety, which is a persistent feeling of stress and worry. A score of 43 or more is considered as a high level of anxiety. In the present study, only the Trait Anxiety subscale was used and showed a good internal consistency (α = 0.89).
Impulsivity
The Barratt Impulsiveness Scale-11 (BIS-11) [42] was used to assess impulsivity. It consists of a 34-item self-reported questionnaire, divided into three subscales: attentional, motor and non-planning impulsivity. The items are answered on a four-point scale, ranging from one (rarely/never) to four (almost always/always). A higher score on the BIS-11 is associated with a higher impulsivity level. For the present study, the unidimensional version of the BIS was used (BIS-Brief), which is composed of eight items from the previous version and was validated by Steinberg et al. [43]. The total score varies from 8 to 32, and a higher value is associated with more impulsivity. The actual internal consistency was α = 0.70 for the BIS-Brief.
Executive functioning
The executive functions were first assessed with a neuropsychological test, the Delis–Kaplan Executive Function System (D-KEFS) [37]. Two of the nine subtests of the battery were used in the present study to assess specific higher-level cognitive skills such as inhibition, planning and cognitive flexibility.
First, we used the Color-Word Interference test (CWIT) to assess inhibition and cognitive flexibility. This task is divided into four conditions: (1) color naming—the examinee must name the colors of a series of squares as fast as possible without error, (2) word reading—the examinee must read a series of black printed color words as fast as possible without error, (3) inhibition—the examinee must name the incongruous ink color in which the color words are printed, and (4) inhibition/switching—similar to condition 3, except that the examinee must read the word (instead of naming the color), when it is framed. The completion time of the first two conditions measures basic cognitive skills: word naming processing speed (condition 1) and word reading processing speed (condition 2). The completion time of the third and the fourth condition measures higher-level cognitive functions, namely inhibition and the combination of inhibition and cognitive flexibility, respectively. To provide a more isolated score of inhibition and cognitive flexibility and to control for the lower-level basic cognitive skills, the D-KEFS includes three different contrast scaled scores. In the present study, these scores are referred to as inhibition (condition 3 minus condition 1), inhibition/cognitive flexibility (condition 4 minus the sum of conditions 1 and 2), and cognitive flexibility (condition 4 minus condition 3). The scoring grid also includes the number of errors for each condition. In the present study, the number of errors for the third and the fourth conditions are referred to as errors inhibition and errors inhibition/cognitive flexibility. Initially, the fourth condition was designed to be more challenging in terms of completion time and number of errors. Recently, some authors have identified another pattern, an atypical one, in which individuals performed better in the inhibition/cognitive flexibility condition (condition 4) than in the inhibition condition (condition 3) for both CWIT outcomes (completion time and errors) [44, 45]. It means that for the latest condition (inhibition and cognitive flexibility), someone with an atypical pattern would report a shorter or the same completion time and/or number of errors than the precedent (inhibition). These authors argue that atypical patterns could be associated with positive outcomes, as a better learning ability, in comparison to typical patterns. In the present study, only the typical and atypical patterns of number of errors were assessed, considering literature on addictions showing a particular importance of error processing deficits in the maintenance of addictions [36, 46].
Second, the Tower test was administered to assess the spatial planning abilities. It consists of a board with three vertical rods and five disks of different sizes. Overall, the Tower test contains nine items during which the examinee must reproduce a target tower presented on a picture, from a predetermined starting position. For each item, the examiner asks the examinee to build the tower in the fewest number of movements possible. Two rules must be followed during the test: (1) to move one disk at a time and to use one hand and (2) to never place a larger disk over a smaller disk. The difficulty level and the minimum number of moves required to complete each tower increases for each item. Overall, a total achievement score is based on the correctly completed items in the allowed time and the number of movements needed to reproduce them (0–30). In the present study, the total achievement and the move accuracy ratio scores were used. For both CWIT and the Tower test, scaled scores for each outcome were used (M = 10; SD = 3) [37].
To provide an assessment of executive functioning in the context of everyday behaviors, the Behavior Rating Inventory of Executive Functions was used (BRIEF-A) [47]. It is a 75-item self-reported questionnaire describing daily life situations, which require executive functions. The questions are answered on a three-point scale, ranging from one (never) to three (often), and target the frequency of some behaviors in the last month. It is possible to regroup items in a global score (Global Executive Composite; GEC) or in two indexes (Behavioral Regulation Index and Metacognition Index). The Behavioral Regulation Index (BRI) includes subscales for inhibition, flexibility, emotional control, and self-monitoring, while the Metacognition Index (MI) includes subscales for task initiation, working memory, task monitoring, and organization of materials. A higher score on one or more of the scales exhibits more difficulty with some aspects of executive function. Cronbach’s alphas in the present study were 0.77 for the BRI and 0.88 for the MI.
Data analysis
SPSS, version 24.0, was used for statistical analyses. Some of the variables of interest demonstrated non-normal distributions and were transformed using a logarithmic transformation (scaled scores for inhibition/cognitive flexibility, cognitive flexibility, errors inhibition, and errors inhibition/cognitive flexibility) [48]. As proposed by Gearhardt et al. [33], the sample was divided in two groups, according to the FA scores on the YFAS. Participants with three or more symptoms were placed into the high FA group (n = 37; 29 women and 8 men) and those with one or no symptoms were placed in the low FA group (n = 33; 25 women and 8 men). 16 participants endorsed two FA symptoms; they were ruled out of the analyses to ensure an appropriate division of the sample.
Associations between FA symptoms, age, BMI, psychological variables, and executive functioning measures were first tested using bivariate correlations on the entire group. One-way ANOVAS and descriptive analyses were performed to compare groups (high vs low FA) on psychological symptoms (binge eating symptoms, depressive symptoms, anxiety symptoms and impulsivity) and performance-based (D-KEFS’ CWIT and Tower test scores) and self-reported measurements of executive functioning (BRIEF-A’s BRI and MI). Considering the over-representation of women in the present sample, the gender was taken into account when we conducted all of the group comparisons.
To enhance the cognitive comprehension of FA regarding error processing, the relationship between CWIT’s error patterns and FA groups were examined with a Chi-square (χ2) test of independence.
Results
Correlations among BMI, age, psychological and cognitive outcomes, and YFAS scores are presented in Table 1.
Group comparisons
Results from the descriptive statistics and the one-way ANOVAS are presented in Tables 2 and 3. The high and low FA groups differed significantly on BMI, binge eating and depressive and anxiety symptoms, with effect sizes ranging from medium to large (0.12–0.39). More precisely, the high FA group reported significantly more binge eating as well as more depressive and anxiety symptoms than the low FA group. Surprisingly, the high FA group presented a lower mean BMI than the low FA group. No difference between groups was observed regarding impulsivity scores. According to the self-reported measures of executive functioning (BRIEF-A), both groups significantly differed on the Metacognition Index, but not on the Behavioral Regulation Index of the measure. More precisely, individuals from the high FA group reported more difficulties on the Working Memory, Planning and Organizing, and Task Monitoring subscales of the Metacognition Index, than individuals from the low FA group. Regarding the performance-based cognitive tasks (D-KEFS), none of the Tower test scaled scores were significantly different. Regarding the CWIT, the only significant difference was on the inhibition/cognitive flexibility scaled score. Effect sizes for all of the group comparisons are shown in Tables 2 and 3.
However, participants from the high FA group presented poorer performances on many of the D-KEFS scores. Specifically, they showed poorer scores on the total achievement and the move accuracy ratio scores of the Tower Test as well as on scores of inhibition, inhibition/cognitive flexibility, and cognitive flexibility of the CWIT. In addition, this visual inspection of the CWIT’s conditions scores allowed us to detect distinct performance patterns in both groups in terms of completion time as well as for the number of errors. Indeed, over the three first conditions, participants from the high FA group showed stable performances and tended to slow down and make more errors during the fourth condition, defined as the most complex condition. Conversely, participants from the low FA group showed a constant progression throughout the four conditions in terms of completion time as well as an important improvement between the third and the fourth conditions for the number of errors.
Relationship between FA groups and CWIT error patterns
Considering the distinct patterns observed in the CWIT and the emphasis of error processing in the addiction literature, the relationship between patterns of number of errors on the CWIT and FA groups was examined. Results from the Chi-square (χ2) test of independence revealed that the relationship between these variables was significant, χ2 (2, N = 70) = 3.90, p < 0.05. Indeed, more participants in the low FA group demonstrated an atypical pattern of errors (37.7%), and thus more participants than expected within this group showed less than or an equal number of errors during the fourth condition compared with the third condition. Inversely, more participants than expected in the high FA group demonstrated a typical pattern of errors (24.6%), showing that belonging to the high FA group was significantly associated with an increased number of errors when the task became more challenging (between the third and the fourth conditions).
Discussion
The purpose of the current study was to expand knowledge on psychological and cognitive features of food addiction in a sample of severely obese individuals awaiting bariatric surgery. According to the scientific literature, participants from the high FA group were expected to exhibit a more impaired overall profile, including a higher BMI, more psychological symptoms and a poorer profile of executive functioning when compared with their low FA counterparts.
First, group comparisons confirmed the assumption of more psychological symptoms in the high FA group. Indeed, as found in previous studies, they reported significantly more binge eating and depressive and anxiety symptoms than their counterparts [17, 21, 26, 49]. According to the questionnaires scoring grids, results showed that individuals within the high FA group reported significant psychological symptoms. More precisely, their scores reflect mild to moderate levels of depressive symptoms and high levels of anxiety symptoms, in comparison to those from the low FA group, for whom average scores were below clinical thresholds. However, no significant difference was found according to their impulsivity scores. It is possible that the brief version of the BIS was not sufficiently sensitive to detect the facets of impulsivity that differentiate a high and a low level of FA symptomatology. In that sense, results from studies using the UPPS Impulsive Behavior Scale, a multifaceted scale to assess impulsivity, shown that mainly two facets tend to be more salient with FA, namely negative urgency (tendency to act rashly when experiencing negative affects) and lack of perseverance (inability to remain focused on a task) [29,30,31,32]. Surprisingly, BMI was significantly higher in the low FA group, which is contrary to what is generally observed of the relationship between body mass and FA. However, this result supports the non-linear relationship between FA symptoms and BMI described by Meule [50], who suggested, based on empirical data, the existence of a cubic relationship between BMI and FA. This result highlights the fact that positive correlations are observed for overweight and moderately obese individuals, while this relationship reaches its peak and decrease in severely obese individuals. It means that in the latter, the relationship between BMI and FA symptoms tends to be weak or non-existent. To explain this cubic relationship, Meule proposed that severely obese people might reach a physical limit to which the weight gain slows down or stops, regardless of FA severity. Thus, the relationship between these variables can become unpredictable in this population. Another possible explanation for this result could be the lack of sensitivity and specificity of BMI in the measurement of obesity, which does not take into account important factors such as differences in body composition between individuals [51]. Considering the obesity status of the present sample, this measurement may not be sensitive enough to determine the contribution of an addictive pattern of eating on body fat.
Second, the hypothesis of a more impaired self-reported profile of executive functioning was partially confirmed. Group comparisons showed that the high FA group reported higher scores and thus more difficulties than the low FA group on the Metacognition Index, but not on the Behavioral Regulation Index. More specifically, the significant differences were on three of the Metacognition subscales: working memory, planning/organizing, and task monitoring. It means that in everyday behaviors, it appears harder for individuals with more FA symptoms to keep information in mind to complete a task, plan and generate goals, to anticipate future events, set goals, and develop sequential steps to complete a task or an activity, and to remember problem-solving success or failure and correctly identify mistakes through a behavior [52]. These difficulties are suggesting a lack of reflection and anticipation in the decision-making process and behavioral choices, which is consistent with the neurocognitive conceptualization of addictions [53].
Third, the hypothesis that participants from the high FA group would show poorer scores on the performance-based cognitive tasks was also partially confirmed. The only significant difference observed was on the inhibition/cognitive flexibility scaled score of the CWIT. Because the inhibition and cognitive flexibility scaled scores were not significantly different, when taken separately, these scores do not allow us to conclude that performance is poorer on one of these specific functions. It rather points to a contribution from higher-level functions, by removing the contribution of the basic cognitive functions requested by the task. These results suggest that participants with a higher level of FA symptoms experienced greater difficulties in a more challenging context, where they must simultaneously keep in mind to inhibit a behavior and switch their mindset when the task required it. The absence of other significant differences on the CWIT could be explained by a more preserved executive functioning in FA than in other addictions. Actually, because food is widely considered as less harmful than many other substances, it is possible that when it comes to decision-making processes, the long-term consequences of addictive-like eating behaviors may seem less obvious than those related to abuse substances. Another hypothesis is that the D-KEFS, as other psychometric tests of executive functioning, does not capture the use of executive functions in a natural context. It could miss the whole affective system or « hot » executive functions, which is a central component of addictions, allowing to weigh the risks and benefits of an action [53,54,55]. It seems that a more contextualized measure of executive functioning would allow a clearer view of executive functioning difficulties accompanying FA symptoms.
Regarding the distinct patterns of performances on the CWIT between the high and the low FA groups, the most important difference stands in patterns of errors between the third and the fourth conditions; the low FA group showed an improvement (fewer errors) and the high FA group showed a slight decline (more errors). Besides, the significant relationship between CWIT error patterns (typical and atypical) and FA groups (high and low) suggests that those with more FA symptoms tend to make more errors at the fourth condition than at the third and inversely so for the low FA group. This finding is consistent with the association between a more severe FA and greater difficulties to detect and monitor errors previously observed by Franken, Nijs, Toes and van der Veen [36]. This result also supports the idea that FA, just like other addictions, could be associated with a greater difficulty to detect and process errors.
Although the present study contributes to the expansion of the knowledge of the psychological and cognitive profiles of FA, it is important to underline its limitations. First, considering the cross-sectional design of the study, it is impossible to conclude to a causal relationship between psychological and cognitive features and FA. Second, a significant proportion of the participants presented medical comorbidities that might have an impact on results. However, our results showed that the proportion of those medical conditions were not statistically different according to the FA group’s belonging (high and low FA) (data not shown), thus allowing us to ascertain that the differences observed between our two groups were not attributable to those conditions. Third, even if the study population represents one of its strengths, participants of both groups suffered from severe obesity and were seeking bariatric surgery; at this point, they typically all experience daily challenges and a problematic relationship with food. Consequently, it becomes harder to detect a clear effect of addictive-like eating behaviors on their global symptomatology, even more when these behaviors are self-reported.
Conclusion
In summary, this study offers a more global comprehension of FA in a sample of individuals with severe obesity, in terms of both psychological features and executive functioning. Results from the present study first highlighted psychological and cognitive difficulties in individuals with higher levels of FA symptoms, in comparison to those with lower levels of FA symptoms. Consequently, they support the more severe psychological profile that tends to come with a higher FA symptomatology. Moreover, it reveals the difficulties to detect and to process errors that tend to show up with FA symptoms. It also provides a better understanding of the cognitive weaknesses associated with this condition, and in a more distal way, could represent a promising avenue in the understanding of the causal relationship between FA and executive functioning.
References
World Health Organization (2017) Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/
Engin A (2017) The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol 960:1–17. https://doi.org/10.1007/978-3-319-48382-5_1
Gustafson DR, Rothenberg E, Blennow K, Steen B, Skoog I (2003) An 18-year follow-up of overweight and risk of Alzheimer disease. Arch Intern Med 163(13):1524–1528. https://doi.org/10.1001/archinte.163.13.1524
Hassing LB, Dahl AK, Thorvaldsson V, Berg S, Gatz M, Pedersen NL, Johansson B (2009) Overweight in midlife and risk for dementia: a 40-year follow-up study. Int J Obes (Lond) 33(8):893–898. https://doi.org/10.1038/ijo.2009.104
Hruby A, Manson JE, Qi L, Malik VS, Rimm EB, Sun Q et al (2016) Determinants and consequences of obesity. Am J Public Health 106(9):1656–1662. https://doi.org/10.2105/AJPH.2016.303326
Kivipelto M, Ngandu T, Fratiglioni L, Viitanen M, Kåreholt I, Winblad B et al (2005) Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol 62(10):1556–1560. https://doi.org/10.1001/archneur.62.10.1556
Whitmer RA, Gunderson EP, Quesenberry CP, Zhou J, Yaffe K (2007) Body mass index in midlife and risk of Alzheimer disease and vascular dementia. Curr Alzheimer Res 4(2):103–109. https://doi.org/10.2174/156720507780362047
Shriner R, Gold M (2014) Food addiction: an evolving nonlinear science. Nutrients 6(11):5370–5391. https://doi.org/10.3390/nu6115370
Marks R (2016) Is the failure to lose weight among the obese partly because obesity is an addictive disease?. Adv Obes Weight Manag Control 4(3):00086. https://doi.org/10.15406/aowmc.2015.04.00086
Von Deneen KM, Liu Y (2011) Obesity as an addiction: Why do the obese eat more?. Maturitas 68(4):342–345. https://doi.org/10.1016/j.maturitas.2011.01.018
Davis C, Carter JC (2009) Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite 53(1):1–8. https://doi.org/10.1016/j.appet.2009.05.018
Imperatori C, Fabbricatore M, Vumbaca V, Innamorati M, Contardi A, Farina B (2016) Food addiction: definition, measurement and prevalence in healthy subjects and in patients with eating disorders. Riv Psichiatr 51:60–65. https://doi.org/10.1708/2246.24196
Gearhardt AN, Corbin WR, Brownell KD (2009) Preliminary validation of the Yale Food Addiction Scale. Appetite 52(2):430–436. https://doi.org/10.1016/j.eatbeh.2013.07.002
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC (text revision)
Flint AJ, Gearhardt AN, Corbin WR, Brownell KD, Field AE, Rimm EB (2014) Food-addiction scale measurement in 2 cohorts of middle-aged older women. Am J Clin Nutr 99(3):578–586. https://doi.org/10.3945/ajcn.113.068965
Meule A, Lutz A, Vögele C, Kübler A (2012) Women with elevated food addiction symptoms show accelerated reactions, but no impaired inhibitory control, in response to pictures of high-calorie food-cues. Eat Behav 13(4):423–428. https://doi.org/10.1016/j.eatbeh.2012.08.001
Hardy R, Fani N, Jovanovic T et al (2018) Food addiction and substance addiction in women: common clinical characteristics. Appetite 120:367–373. https://doi.org/10.1016/j.appet.2017.09.026
Lent MR, Eichen DM, Goldbacher E, Wadden TA, Foster GD (2014) Relationship of food addiction to weight loss and attrition during obesity treatment. Obesity (Silver Spring) 22(1):52–55. https://doi.org/10.1002/oby.20512
Burmeister JM, Hinman N, Koball A, Hoffman DA, Carels RA (2013) Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite 60(1):103–110. https://doi.org/10.1016/j.appet.2012.09.013
Eichen DM, Lent MR, Goldbacher E, Foster GD (2013) Exploration of “Food Addiction” in overweight and obese treatment-seeking adults. Appetite 67:22. https://doi.org/10.1016/j.appet.2013.03.008
Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL (2011) Evidence that “food addiction” is a valid phenotype of obesity. Appetite 57(3):711–717. https://doi.org/10.1016/j.appet.2011.08.017
Ouellette A-S, Rodrigue C, Lemieux S, Tchernof A, Biertho L, Bégin C (2017) An examination of the mechanisms and personality traits underlying food addiction among individuals with severe obesity awaiting bariatric surgery. Eat Weight Disord 22(4):633–640. https://doi.org/10.1007/s40519-017-0440-7
Gearhardt AN, White MA, Masheb RM, Grilo CM (2013) An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry 54(5):500–505. https://doi.org/10.1016/j.comppsych.2012.12.009
Clark SM, Saules KK (2013) Validation of the Yale Food Addiction Scale among a weight-loss surgery population. Eat Behav 14(2):216–219. https://doi.org/10.1016/j.eatbeh.2013.01.002
Meule A, Heckel D, Kübler A (2012) Factor structure and item analysis of the Yale Food Addiction Scale in obese candidates for bariatric surgery. Eur Eat Disord Rev 20(5):419–422. https://doi.org/10.1002/erv.2189
Brewerton TD (2017) Food addiction as a proxy for eating disorder and obesity severity, trauma history, PTSD symptoms, and comorbidity. Eat Weight Disord 22(2):241–247. https://doi.org/10.1007/s40519-016-0355-8
Ahmed AY, Sayed AM, Mostafa MK, Abdelaziz EA (2016) Food addiction relations to depression and anxiety in Egyptian adolescents. Egypt Pediatr Assoc Gaz 64(4):149–153. https://doi.org/10.1016/j.epag.2016.09.002
Pivarunas B, Conner BT (2015) Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav 19:9–14. https://doi.org/10.1016/j.eatbeh.2015.06.007
Wolz I, Granero R, Fernández-Aranda F (2017) A comprehensive model of food addiction in patients with binge-eating symptomatology: the essential role of negative urgency. Compr Psychiatry 74:118–124. https://doi.org/10.1016/j.comppsych.2017.01.012
Wolz I, Hilker I, Granero R, Jiménez-Murcia S, Gearhardt AN, Dieguez C et al (2016) “Food Addiction” in patients with eating disorders is associated with negative urgency and difficulties to focus on long-term goals. Front Psychol 7(61):1–10. https://doi.org/10.3389/fpsyg.2016.00061
Murphy CM, Stojek MK, Mackillop J (2014) Interrelationships among impulsive personality traits, food addiction, and Body Mass Index. Appetite 73:45–50. https://doi.org/10.1016/j.appet.2013.10.008
VanderBroek-Stice L, Stojek MK, Beach SRH, vanDellen MR, MacKillop J (2017) Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite 112:59–68. https://doi.org/10.1016/j.appet.2017.01.009
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD (2011) Neural correlates of food addiction. Arch Gen Psychiatry 68(8):808–816. https://doi.org/10.1001/archgenpsychiatry.2011.32
Imperatori C, Fabbricatore M, Innamorati M, Farina B, Quintiliani MI, Lamis DA et al (2015) Modification of EEG functional connectivity and EEG power spectra in overweight and obese patients with food addiction: An eLORETA study. Brain Imaging Behav 9(4):703–716. https://doi.org/10.1007/s11682-014-9324-x
Frayn M, Sears CR, von Ranson KM (2016) A sad mood increases attention to unhealthy food images in women with food addiction. Appetite 100:55–63. https://doi.org/10.1016/j.appet.2016.02.008
Franken IH, Nijs IMT, Toes A, Veen FM, van der Veen FM (2018) Food addiction is associated with impaired performance monitoring. Biol Psychol 131:49–53. https://doi.org/10.1016/j.biopsycho.2016.07.005
Delis DC. Kaplan E, Kramer JH (2001) The Delis-Kaplan executive function system: examiner’s manual. The Psychological Corporation, San Antonio
Ouellette A-S, Rodrigue C, Lemieux S, Tchernof A, Biertho L, Bégin C (2017) Yale Food Addiction Scale: examining the psychometric properties of the French version among Individuals with severe obesity awaiting bariatric surgery. Psychology 8(14):2547–2561. https://doi.org/10.4236/psych.2017.814161
Gormally J, Black S, Daston S, Rardin D (1982) The assessment of binge-eating severity among obese persons. Addict Behav 7(1):47–55
Beck AT, Steer RA, Brown GK (1996) BDI-II, Beck depression inventory: manual, 2d edn. The Psychological Corporation, San Antonio (TX)
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the state-trait anxiety inventory. Consulting Psychologist’s Press, Palo Alto
Patton JH, Stanford MS, Barratt ES (1995) Factor structure of the Barratt impulsiveness scale. J Clin Psychol 51(6):768–774. https://doi.org/10.1002/1097-4679(199511)51:6<768
Steinberg L, Sharp C, Stanford MS, Tharp AT (2013) New tricks for an old measure: the development of the Barratt Impulsiveness Scale–Brief (BIS-Brief). Psychol Assess 25(1):216–226. https://doi.org/10.1037/a0030550
Berg J, Swan NM, Banks SJ, Miller JB (2016) Atypical performance patterns on Delis–Kaplan executive functioning system Color–Word interference test: cognitive switching and learning ability in older adults. J Clin Exp Neuropsychol 38(7):745–751. https://doi.org/10.1080/13803395.2016.1161734
Lippa SM, Davis RN (2010) Inhibition/switching is not necessarily harder than inhibition: an analysis of the D-KEFS color-word interference test. Arch Clin Neuropsychol 25(2):146–152. https://doi.org/10.1093/arclin/acq001
Franken IH, van Strien JW, Franzek EJ, van de Wetering BJ (2007) Error-processing deficits in patients with cocaine dependence. Biol Psychol 75(1):45–51. https://doi.org/10.1016/j.biopsycho.2006.11.003
Roth RM, Isquith PK, Gioia GA (2005) BRIEF-A: Behavior Rating Inventory of Executive Function—adult Version: professional manual. Psychological Assessment Resources: Lutz, FL
Tabachnik BG, Fidell LS (2007) Using multivariate statistics, 5th edn. Pearson, New Yok
Ivezaj V, White MA, Grilo CM (2016) Examining binge-eating disorder and food addiction in adults with overweight and obesity. Obesity (Silver Spring) 24(10):2064–2069. https://doi.org/10.1002/oby.21607
Meule A (2012) Food addiction and body-mass-index: a non-linear relationship. Med Hypotheses 79(4):508–511. https://doi.org/10.1016/j.mehy.2012.07.005
Rothman KJ (2008) BMI-related errors in the measurement of obesity. Int J Obes (Lond) 32(Suppl 3):S56–S59. https://doi.org/10.1038/ijo.2008.87
Isquith PK, Roth RM, Gioia GA (2006) Behavior rating inventory of executive function—adult version. Psychological Assessment Resources, Florida
Noël X, Brevers D, Bechara A (2013) A neurocognitive approach to understanding the neurobiology of addiction. Curr Opin Neurobiol 23(4):632–638. https://doi.org/10.1016/j.conb.2013.01.018
Barkley RA (2012) Executive functions: what they are, how they work, and why they evolved. Guilford Press, New York
Damasio AR (1991) Toward a neurobiology of emotion and feeling: operational concepts and hypotheses. Neuroscientist 1(1):19–25. https://doi.org/10.1177/107385849500100104
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tchernof as well as Dr. Biertho report grants from Johnson & Jonhson Medical Companies, outside the submitted work. The other authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This article is part of the topical collection on Food Addiction.
Rights and permissions
About this article
Cite this article
Rodrigue, C., Ouellette, AS., Lemieux, S. et al. Executive functioning and psychological symptoms in food addiction: a study among individuals with severe obesity. Eat Weight Disord 23, 469–478 (2018). https://doi.org/10.1007/s40519-018-0530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0530-1