Abstract
Gestational diabetes mellitus (GDM), defined as glucose intolerance with onset or first recognition during pregnancy, is the most common pregnancy complication worldwide. Recent data have shown a substantial rise in the prevalence of GDM among women of various ethnic/racial backgrounds and in different geographic regions. The purpose of the current review is to summarize recent studies about GDM diagnosis, prevalence, and long-term impact on women’s later life and their offspring’s health, and to provide an updated review to guide future research. Currently, available evidence indicates that GDM presents a significant risk factor for development of type II diabetes (T2D) and cardiovascular disease in women. Children whose mothers had diabetes during pregnancy are at increased risk of having obesity and T2D at a young age. Future research will be needed to address how to determine whether better glucose control during pregnancy would prevent long-term consequences for both women and their children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
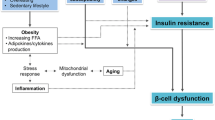
Gestational diabetes mellitus (GDM) is defined as glucose intolerance with onset or first recognition during pregnancy. GDM is characterized by pancreatic beta cell function being insufficient to meet the body’s insulin need, usually as a result of insulin resistance (IR) during pregnancy [1]. The established risk factors for GDM are high maternal age and parity, pre-pregnancy overweight/obese, previous delivery of macrocosmic newborns, and family history of diabetes [2]. Research in the past decade has identified a few lifestyle factors that are associated with GDM risk, including a Western dietary pattern, high consumption of red meat and sugary drinks, low consumption of dietary fiber, low glycemic index diet, and physical inactivity before pregnancy [3]. Although GDM has been recognized as one of the most common pregnancy complications, its epidemiology has not been well investigated. One of the reasons is the lack of global consensus on the diagnosis of GDM. Recent data have shown a substantial rise in the prevalence of GDM among women of various ethnic/racial backgrounds [4–8], and would likely further increase as the obesity rate is continually increasing globally. The purpose of the current study is to summarize recent studies about GDM diagnosis, prevalence, and long-term impact on women’s later life and their offspring’s health, and to provide an updated review to guide future research.
Diagnosis of GDM
Diagnosis of GDM is commonly based on the results of an oral glucose tolerance test (OGTT) during pregnancy; however, there is currently no global consensus on the diagnostic criteria. A variety of diagnostic criteria have been used in different studies over time and across regions, including criteria from the National Diabetes Data Group (1997) [9], Carpenter and Coustan (1982, also recommended by the fourth international workshop-conference of GDM, 1998) [10], the World Health Organization (WHO 1985 and 1999) [11, 12], the European Association for the Study of Diabetes (EASD, 1991) [13], American Diabetes Association (ADA 2004, 2011, and 2014) [14, 15, 16•], the International Association of Diabetes and Pregnancy Study Groups (IADPSG, 2010) [17•], and the US National Institutes of Health (NIH, 2013) [18]. There is a general agreement that the OGTT tests should be conducted at gestational weeks 24–28; however, the disagreement is whether to use the 100-g 3-h OGTT or 75-g 2-h OGTT, and different groups propose different cut-offs for the positive results. Table 1 provides descriptions of the diagnostic criteria that have been applied in different time periods and studies. It is important to know these diagnostic criteria because they have significant impact on the prevalence estimates at different times and in different countries. In a 2005 study of the agreement between several international diagnostic criteria, the prevalence of GDM in the same population ranged from 8 to 25 % depending on the criteria used (Fig. 1) [19], and the ADA and WHO criteria showed only a moderate correlation (kappa statistic = 0.51). In the current review, these inconsistencies are important to consider when comparing prevalence data across studies that used different diagnostic criteria.
The Different Diagnostic Criteria on GDM Prevalence in One Population of Pregnant Women. CDA Canadian Diabetes Association, EASD European Association for the Study of Diabetes, ADA American Diabetes Association, NZSSD New Zealand Society for the Study of Diabetes, WHO World Health Organization, ADIPS Australian Diabetes Pregnancy Society. Reference [19]
In 2004, the ADA proposed that GDM can be detected with either of two strategies: (1) “one-step” approach of 75-g OGTT or (2) “two-step” approach with a 50-g screen followed by one 100-g OGTT for those who screened positive. The same cut-off points are used in both tests (fasting ≥ 5.3 mmol/l; 1-h ≥ 10 mmol/l; and 2-h ≥ 7.8 mmol/l). However, it is required that two of three abnormal values are needed for diagnosis [14]. After deliberations in 2008 to2009, the IADPSG recommended testing women with risk factors for undiagnosed type II diabetes (T2D) at their initial prenatal visit. Women who are diagnosed with diabetes in the first trimester would be classified as T2D. GDM is diabetes diagnosed based on 75-g 2-h OGTT in the second or third trimester of pregnancy. This recommendation has been made based on findings from the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study and other works that examined associations of maternal glycemia with perinatal and long-term outcomes in offspring, and has been endorsed by multiple obstetrical and diabetes organizations [17•]. In 2011 Standard of Care, the ADA for the for the first time recommended that all pregnant women not known have prior diabetes undergo a 75-g OGTT at 24–28 weeks of gestation based on the recommendation of the IDAPSG [15]. In 2013, the NIH called a panel with 15 representatives from multiple fields (i.e., obstetrics/gynecology, maternal-fetal medicine, pediatrics, diabetes research, and biostatistics) to discuss the diagnostic criteria of GDM [18]. The panel recommended the two-step approach. These approaches differed on whether a 1-h sample should be included, whether two abnormal values are required, and the diagnostic cut-off values that were used. Given the fact that there are data to support both approaches, ADA recommended both two options for the diagnosis of GDM in 2014 [16•].
Prevalence of GDM
Since there is no global consensus on the diagnostic criteria for GDM, the prevalence of GDM ranged from 1.0 to 14.2 % of all pregnancies depending on diagnostic criteria and the study population (based on our literature search of Medline publications with either population-based studies with sample size ≥500 or hospital-based studies with sample size ≥1000 and at least 70 % of population being screened for GDM) As shown in Table 2, the Southeast Asia region consistently reported the highest GDM prevalence with a median of 5.4 % (range of 3–14.2 %), followed by Eastern Mediterranean countries with a median of 4.75 % (range of 1.9–13.7 %). America, Africa, and Western Pacific appeared to have similar GDM prevalence with a median of 3.7 % across the three regions. Europe had the lowest GDM prevalence among all the WHO regions. The low prevalence was evident across all European countries (range 1.2–3.1 %) except for Italy. A population-based study in Sardinia, Italy, provided the largest GDM prevalence (22.3 %) of all the included studies [20]. A second large population-based study from a mainland Italian city, Pisa, also reported a GDM prevalence of 8.7 %.
The prevalence data in the USA over time are presented in Fig. 2. The study that had the largest time span, 15 years, showed the largest difference in prevalence, 2.6 % in 1990 and 7.5 % in 2005 [21]. A recent study using data from the Pregnancy Risk Assessment Monitoring System (PRAMS) reported that the GDM prevalence (included 21 states that participated in PRAMS from 2007–2010) was 8.1 % in 2007–2008 and 8.5 % in 2009–2010 [22•]. Another study using the Agency for Healthcare Research and Quality’s (AHRQ) National and State Inpatient Database (included 12 states) found that the GDM prevalence increased from 3.71 % in 2000 to 5.77 % in 2010 among all hospital deliveries [23]. Although other factors such as the diagnostic criteria, the geographic location, and the changing demographics of the study population must be acknowledged when comparing these studies and the actual numeric prevalence estimates, there was a clear trend on the increase in GDM prevalence in the USA from the 1990s to 2010s.
US prevalence data showed a clear difference across the races/ethnicities that was consistent throughout all the studies (Table 3). Whites had the lowest prevalence of GDM followed by Blacks, then Hispanics, and Asian Americans had the highest prevalence of GDM. This disparity was consistent across the almost 20-year time span of the studies included. As the data in Table 3 are displayed in ascending order by year of the study, we can see an increase in GDM prevalence for each race/ethnicity group over time and the highest increase was observed in Hispanics [23].
The geographic distribution of gestational diabetes in the USA is presented in a map as Fig. 3. Prevalence data was available for 21 states (with either population-based studies with sample size ≥500 or hospital-based studies with sample size ≥1000 and at least 70 % of population being screened for GDM). The states with the highest GDM prevalence, between 5.6 and 8.0 % of pregnancies, are Texas, California, Hawaii, and Alaska. This geographic difference of GDM may be largely explained by the racial/ethnic composition in each state. According to the 2000 census data, half of all Hispanics in the USA lived in just two states, Texas and California. California also had a substantial Asian population. Since Asian and Hispanic populations had a higher prevalence of GDM than other ethnicities, this may explain the high prevalence found in Texas and California. Hawaiian and Alaskan natives have also been implicated as high-risk ethnicities in several studies [24, 25]. Despite the agreement between the geographic and the ethnic disparity, more data should be collected for all of the states in order to further study regional trends and differences.
Long-Term Maternal Outcomes of GDM
Women with GDM are at greater risk for other pregnancy complications such as maternal hypertensive disorders and cesarean delivery [26]. Although most women with GDM regain normal glucose tolerance after delivery, many of them are featured with metabolic disorders in postpartum and later life. Women with GDM are at increased risk of developing impaired glucose tolerance (IGT) and T2D in their later life. On average, the risk of development of T2D is 7.4 times greater in GDM women than non-GDM women [27••]. Such increased risk of T2D among women with GDM has been documented in different populations and countries [28]. In a large Canadian population-based study, the probability of developing T2D among women with GDM was 3.7 % at 9 months and 18.9 % at 9 years after delivery. In contrast, the rate was only 2.0 % at 9 years for women who did not have GDM [29]. Another study in Australia also found risk of development of diabetes in GDM women increased with time from the index pregnancy: the cumulative incidence of diabetes is 2.6 % in 2 years, 8.1 % in 5 years, 17.3 % in 10 years, and 25.8 % in 15 years [30]. Moreover, recent data have indicated that women with a history of GDM might be at an increased risk of cardiovascular diseases (CVD) independent of T2D or obesity. Several studies have reported an association between GDM and CVD risk factors, including obesity, high blood pressure, abnormal plasma lipid levels, metabolic disorder, inflammation, and endothelial dysfunction [31–39]. In addition, other nontraditional CVD risk biomarkers, such as higher level of C-reactive protein (CRP), E-selectin, fibrinogen, plasminogen activator inhibitor (PAI)-1, and lower circulation level of adiponectin, have been fund in women with a history of GDM [37, 38, 40–43]. Moreover, recent studies have directly linked a history of GDM with a CVD clinical event. A US study reported that among women with a family history of T2D, those with GDM were more likely to have a CVD event (odds ratio (OR) = 1.85; P = 0.005), independent of T2D [44]. The higher risk of development of CVD among women with a history of GDM was also reported by a larger study in Canada with a median follow-up of 11.5 years [45]. A recent publication from CARDIA (The Coronary Artery Risk Development in Young Adults) study found that the history of GDM was associated with atherosclerosis (measured by common carotid intima-media thickness), independent of pre-pregnancy obesity [46]. Taken together, emerging evidence tends to suggest that women with GDM represent a population who are more likely to develop CVD at a relative younger age.
Long-Term Outcomes in the Offspring of Women with GDM
Theoretically, exposure to a diabetic intrauterine environment results in excess fetal growth. Biologically, maternal glucose can cross the placenta but maternal insulin does not. To respond to this increase in glucose load, the fetal pancreas increases the insulin production, which in turn promotes fetal growth and adiposity development [47]. There is a growing in the literature that reports a positive association between maternal hyperglycemia and higher risk of development of obesity and diabetes in offspring. A few studies also found a direct link between maternal diabetes and offspring CVD risk factors, including blood pressure [48–51] and plasma lipids [49, 50]. One recent study by Kaiser Permanente South California found that exposure to GDM by 26 weeks’ gestation was associated with offspring autism [52]. Among those health outcomes, the strong evidence was found for offspring obesity and T2D.
Early evidence from Pima Indian data indicated that offspring of women with preexisting diabetes or GDM were heavier at birth and had an increased risk of obesity during childhood and young adulthood (5–19 years) [53–55]. These findings were confirmed by the Diabetes in Pregnancy Study at Chicago in which children born to women with diabetes during pregnancy (both pregestational diabetes and GDM) were on average 30 % heavier than expected for their height at age at 8 years [48]. While some studies did not find such a positive association between maternal diabetes and offspring obesity, a recent systematic review and meta-analysis of nine studies indicated that maternal diabetes was associated with increased offspring BMI [56]. Although most of the studies used the BMI to define overweight or obesity in the offspring, Catalano et al. showed that newborns of women with GDM had 20 % greater fat mass (measured by body electrical conductivity) compared with infants of women with normal glucose tolerance during pregnancy. Maternal fasting glucose was the strongest predictor of fat mass in newborns of women of GDM [57].
Several studies also found a positive association between maternal diabetes with insulin resistance, impaired glucose tolerance (IGT) and elevated risk of T2D in offspring. In the Diabetes in Pregnancy Study, the offspring of diabetic mothers had higher 2-h glucose and insulin concentrations when compared with the controls of nondiabetic mothers at age 10–16 years [58]. In the Pima Indian Study, there was a significantly higher prevalence of T2D in the offspring of diabetic mothers at all ages, ranging from 5 to 34 years, than in the offspring of prediabetic and nondiabetic mothers [59]. In addition, the insulin secretion was impaired in Pima adults whose mothers were diabetic during pregnancy than in those whose mothers developed diabetes after their births [60].
Although studies conducted from different populations consistently showed that maternal diabetes is associated with an increased risk of having obesity and T2D in offspring in both childhood and young adulthood, there are still questions and debates as to (1) whether such association is independent of the type of diabetes during pregnancy (i.e., pregestational type I or II diabetes or GDM), (2) whether the association of maternal diabetes and offspring diabetes is because of the exposure to a diabetic intrauterine environment during pregnancy in addition to genetic transmission of diabetes susceptibility between mother and their offspring, and (3) whether such associations are independent of maternal obesity (pre-pregnancy BMI or gestational weight gain). In the following sections, we review recent studies that provide data to answer these questions.
While most earlier studies did not differentiate the type of maternal diabetes in their analyses, recent evidence tends to suggest that the long-term consequence of exposure to maternal diabetes is not related to the type of diabetes during pregnancy. In the Diabetes in Pregnancy Study, the occurrence of IGT in offspring was associated with maternal hyperglycemic but not the type of diabetes in the mothers [58]. In German studies, the occurrences of IGT and obesity at 1–4 years and 5–9 years were similar in offspring of mothers with preexisting type I diabetes and in those of mothers with GDM [61, 62].
Studies that investigate the role of diabetic intrauterine environment on offspring obesity or diabetes are limited, but results are consistent from two studies in different populations. In the Pima Indians, the prevalence of T2D was compared between siblings born before and after their mother developed diabetes [59]. The risk of diabetes was significantly higher in siblings born after the mother developed diabetes as compared with those born before the mother’s diagnosis of diabetes (OR = 3.7, P = 0.02). Additionally, among 183 siblings without diabetes, the mean BMI was 2.6 kg/m [2] higher (P = 0.003) in the offspring of diabetic than in offspring of nondiabetic pregnancies. Since siblings are considered to have a similar risk of carrying genetic family environmental factors for diabetes, the different risks between siblings likely reflects the influence of intrauterine diabetes environments. A recent sibling study in Swedish men also found that maternal diabetes was associated with greater mean BMI of their son at age of 18 years [63••]. The BMI of men whose mother had GDM was 0.94 kg/m [2] greater than in their brothers born before their mothers were diagnosed with diabetes, suggesting this association is importantly driven by an intrauterine mechanism.
Recently, there is a debate as to whether the association between maternal diabetes and offspring obesity or glucose intolerance is independent of maternal obesity during pregnancy. Results from a birth cohort in Finland indicated that maternal pre-pregnancy overweight is associated with a higher risk of offspring obesity (OR = 2.56; P < 0.001) at age of 16 years, even among those mothers with a normal glucose during the pregnancy. However, in offspring with pre-pregnancy normal weight, the risk of obesity was not increased by prenatal exposure to GDM (OR = 0.73, P > 0.05) [64]. Data from the Avon Longitudinal Study of Parents and Children (ALSPAC) in the UK suggested GDM was associated with greater BMI and fat mass of offspring at 9–11 years of age. Although the association attenuated with adjustment of maternal early pregnancy BMI, the positive association remained [65]. This finding is also supported by two meta-analyses [56, 66]. A large population-based study in the USA using Kaiser Permanente data reported that the risk of offspring obesity was positively associated with hyperglycemia in pregnancy, independent of gestational weight gain [67]. A recent large prospective study in Swedish men also showed that maternal diabetes (both pregestational diabetes and GDM) was associated with greater offspring BMI in early adulthood, independent of maternal early pregnancy BMI [63]. Results from the SEARCH Case-Control study indicated that exposure to maternal diabetes (both pregestational diabetes and GDM: OR = 5.7) and exposure to maternal overweight/obesity (measured by pre-pregnancy BMI ≥25 kg/m [2]: OR = 2.8) were independently associated with T2D in youth (10–22 years) across different race/ethnicity groups (i.e., White, African-Americans, and Hispanics). For those youth who had intrauterine exposure to both maternal diabetes and obesity with the OR of T2D as 19.2 suggests an interactive effect [68]. Therefore, available evidence on the interrelationship of maternal diabetes, maternal obesity, and offspring risk of obesity/diabetes is inconsistent. One possible explanation for those studies failing to show the association is a possible attenuation of the risk due to the treatment of maternal diabetes during pregnancy. Another explanation could be that studies used different methods and criteria for the diagnosis of diabetes during pregnancy. Moreover, different studies have examined offspring obesity at various ages. Although most studies found a positive association between maternal diabetes and offspring obesity, it is still unclear at what age this association becomes apparent. Findings from Project Viva indicated that GDM predicted a slower weight gain in the first 6 months of life [69]. This finding was confirmed by longitudinal results from the Exploring Perinatal Outcomes among Children (EPOCH) Study in which the growth trajectory from birth through 13 years of age was compared between children with and without exposure to maternal diabetes. The overall BMI growth curve (adjusted for sex and race) was not significantly different for exposed and unexposed children from birth through 26 months of age (P = 0.48). However, the overall BMI curve from 27 months of age through 13 years differed significantly by exposure status (P = 0.008), indicating that exposure to maternal diabetes accelerates offspring BMI growth in late childhood thus increasing the long-term obesity risk [70].
In summary, current evidence indicates that maternal diabetes has long-term effects on the risk of diabetes and obesity in the offspring. The effects of exposure to maternal diabetes during pregnancy are similar regardless of the type of diabetes (i.e., preexisting type I or II diabetes or GDM). The higher risk of obesity and T2D in the offspring of diabetic mothers is likely due to the intrauterine environment which is independent of shared socioeconomic, lifestyle, and genetic factors within families. It is unclear how pre-pregnancy obesity and gestational weight gain interplay with maternal diabetes to influence the long-term health outcomes in offspring.
Conclusions
GDM presents a significant risk factor for development of T2D and CVD in women. Therefore, identifying women at high risk of GDM has important public health and clinical significances. The initial risk prevention approach for this population should be targeting a reduction in the risk of T2D. Additional efforts should include managing optimal body weight, blood pressure, blood lipids, and other CVD risk factors in this population. Ideally, such efforts will be considered and integrated into current clinical care in both prenatal and postpartum care. Future investigations will be needed to address how to do risk classification among women with GDM. Children whose mothers had diabetes during pregnancy are at increased risk of having obesity and T2D at a young age. Studies are needed to understand the relative contribution of maternal diabetes and obesity to the long-term effects on offspring risk for obesity and T2D. Future research is also needed to determine whether better glucose control during pregnancy would prevent the long-term consequences for both women and their children.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007;30 Suppl 2:S251–60.
Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes mellitus and its association with type 2 diabetes. Diabet Med. 2004;21:103–13.
Zhang C, Ning Y. Effect of dietary and lifestyle factors on the risk of gestational diabetes: review of epidemiologic evidence. Am J Clin Nutr. 2011;94:1975S–9S.
Ferrara A, Kahn HS, Quesenberry CP, Riley C, Hedderson MM. An increase in the incidence of gestational diabetes mellitus: Northern California, 1991–2000. Obstet Gynecol. 2004;103:526–33.
Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff K, Hamman R, McDuffie R. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care. 2005;28:579–84.
Zhang F, Dong L, Zhang CP, et al. Increasing prevalence of gestational diabetes mellitus in Chinese women from 1999 to 2008. Diabet Med. 2011;28:652–7.
Wang Y, Chen L, Xiao K, et al. Increasing incidence of gestational diabetes mellitus in Louisiana, 1997–2009. J Womens Health (Larchmt). 2012;21:319–25.
Leng J, Shao P, Zhang C, et al. Prevalence of gestational diabetes mellitus and its risk factors in Chinese pregnant women: a prospective population-based study in Tianjin. China PLoS One. 2015;10, e0121029.
Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. National Diabetes Data Group. Diabetes 1979;28:1039–57.
Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144:768–73.
WHO. Report of a WHO study group. WHO Technical Report Series 1985;727:106.
WHO. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications. Report of a WHO Consultation. Geneva: World Health Organization; 1999.
Lind T, Phillips PR. Influence of pregnancy on the 75-g OGTT. A prospective multicenter study. The Diabetic Pregnancy Study Group of the European Association for the Study of Diabetes. Diabetes. 1991;40 Suppl 2:8–13.
American Diabetes A. Gestational diabetes mellitus. Diabetes Care 2004;27 Suppl 1:S88–90.
American Diabetes A. Standards of medical care in diabetes--2011. Diabetes Care 2011;34 Suppl 1:S11–61.
American Diabetes A. Standards of medical care in diabetes--2014. Diabetes Care 2014;37 Suppl 1:S14–80. This paper is the most recent statement from ADA and inlcudes the current ADA recommendation for the diagnosis of GDM.
International Association of D, Pregnancy Study Groups Consensus P, Metzger BE, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–82. This paper is one of the most important international pannel discussion on recommendation for the diagnosis of GDM.
Vandorsten JP, Dodson WC, Espeland MA, et al. NIH consensus development conference: diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements. 2013;29:1–31.
Agarwal M, Dhatt G, Punnose J, Koster G. Gestational diabetes: dilemma caused by multiple international diagnostic criteria. Diabet Med. 2005;22:1731–6.
Murgia C, Berria R, Minerba L, et al. Gestational diabetes mellitus in Sardinia. Diabetes Care. 2006;29:1713.
Thorpe L, Berger D, Ellis J, et al. Trends and racial/ethnic disparities in gestational diabetes among pregnant women in New York City, 1990–2001. Am J Public Health. 2005;95:1536.
DeSisto CL, Kim SY, Sharma AJ. Prevalence estimates of gestational diabetes mellitus in the United States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2007-2010. Prev Chronic Dis. 2014;11:E104. This is the most recent national data on GDM prevalence use PRAMS across 4 years period.
Bardenheier BH, Imperatore G, Gilboa SM, et al. Trends in Gestational Diabetes Among Hospital Deliveries in 19 U.S. States, 2000-2010. Am J Prev Med. 2015;49:12–9.
Chu S, Abe K, Hall L, Kim S, Njoroge T, Qin C. Gestational diabetes mellitus: All Asians are not alike. Prev Med. 2009;49:265–8.
Murphy N, Bulkow L, Schraer C, Lanier A. Prevalence of diabetes mellitus in pregnancy among Yup'ik Eskimos, 1987-1988. Diabetes Care. 1993;16:315.
Group HSCR, Metzger BE, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002.
Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–9. This is a high quality systematic review and meta-analysis on the risk of development of type 2 diabetes in women with GDM as compared to women without GDM.
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25:1862–8.
Feig DS, Zinman B, Wang X, Hux JE. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. CMAJ. 2008;179:229–34.
Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M. Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 diabetes: a retrospective cohort study using survival analysis. Diabetes Care. 2007;30:878–83.
Meyers-Seifer CH, Vohr BR. Lipid levels in former gestational diabetic mothers. Diabetes Care. 1996;19:1351–6.
Osei K, Gaillard TR, Schuster DP. History of gestational diabetes leads to distinct metabolic alterations in nondiabetic African-American women with a parental history of type 2 diabetes. Diabetes Care. 1998;21:1250–7.
Ko GT, Chan JC, Tsang LW, Li CY, Cockram CS. Glucose intolerance and other cardiovascular risk factors in Chinese women with a history of gestational diabetes mellitus. Aust N Z J Obstet Gynaecol. 1999;39:478–83.
Hannemann MM, Liddell WG, Shore AC, Clark PM, Tooke JE. Vascular function in women with previous gestational diabetes mellitus. J Vasc Res. 2002;39:311–9.
Verma A, Boney CM, Tucker R, Vohr BR. Insulin resistance syndrome in women with prior history of gestational diabetes mellitus. J Clin Endocrinol Metab. 2002;87:3227–35.
Di Benedetto A, Russo GT, Corrado F, et al. Inflammatory markers in women with a recent history of gestational diabetes mellitus. J Endocrinol Invest. 2005;28:34–8.
Heitritter SM, Solomon CG, Mitchell GF, Skali-Ounis N, Seely EW. Subclinical inflammation and vascular dysfunction in women with previous gestational diabetes mellitus. J Clin Endocrinol Metab. 2005;90:3983–8.
Di Cianni G, Lencioni C, Volpe L, et al. C-reactive protein and metabolic syndrome in women with previous gestational diabetes. Diabetes Metab Res Rev. 2007;23:135–40.
Tobias DK, Hu FB, Forman JP, Chavarro J, Zhang C. Increased risk of hypertension after gestational diabetes mellitus: findings from a large prospective cohort study. Diabetes Care. 2011;34:1582–4.
Kautzky-Willer A, Fasching P, Jilma B, Waldhausl W, Wagner OF. Persistent elevation and metabolic dependence of circulating E-selectin after delivery in women with gestational diabetes mellitus. J Clin Endocrinol Metab. 1997;82:4117–21.
Lawrence NJ, Kousta E, Penny A, et al. Elevation of soluble E-selectin levels following gestational diabetes is restricted to women with persistent abnormalities of glucose regulation. Clin Endocrinol (Oxf). 2002;56:335–40.
Bo S, Valpreda S, Menato G, et al. Should we consider gestational diabetes a vascular risk factor? Atherosclerosis. 2007;194:e72–9.
Ferraz TB, Motta RS, Ferraz CL, Capibaribe DM, Forti AC, Chacra AR. C-reactive protein and features of metabolic syndrome in Brazilian women with previous gestational diabetes. Diabetes Res Clin Pract. 2007;78:23–9.
Carr DB, Utzschneider KM, Hull RL, et al. Gestational diabetes mellitus increases the risk of cardiovascular disease in women with a family history of type 2 diabetes. Diabetes Care. 2006;29:2078–83.
Shah BR, Retnakaran R, Booth GL. Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care. 2008;31:1668–9.
Gunderson EP, Chiang V, Pletcher MJ, et al. History of gestational diabetes mellitus and future risk of atherosclerosis in mid-life: the Coronary Artery Risk Development in Young Adults study. J Am Heart Assoc. 2014;3:e000490.
Dabelea D. The predisposition to obesity and diabetes in offspring of diabetic mothers. Diabetes Care. 2007;30 Suppl 2:S169–74.
Silverman BL, Rizzo T, Green OC, et al. Long-term prospective evaluation of offspring of diabetic mothers. Diabetes. 1991;40 Suppl 2:121–5.
Bunt JC, Tataranni PA, Salbe AD. Intrauterine exposure to diabetes is a determinant of hemoglobin A(1)c and systolic blood pressure in pima Indian children. J Clin Endocrinol Metab. 2005;90:3225–9.
Tam WH, Ma RC, Yang X, et al. Glucose intolerance and cardiometabolic risk in children exposed to maternal gestational diabetes mellitus in utero. Pediatrics. 2008;122:1229–34.
Wright CS, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW, Oken E. Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. Am J Hypertens. 2009;22:215–20.
Xiang AH, Wang X, Martinez MP, et al. Association of maternal diabetes with autism in offspring. JAMA. 2015;313:1425–34.
Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC. Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med. 1983;308:242–5.
Pettitt DJ, Nelson RG, Saad MF, Bennett PH, Knowler WC. Diabetes and obesity in the offspring of Pima Indian women with diabetes during pregnancy. Diabetes Care. 1993;16:310–4.
Pettitt DJ, Knowler WC. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care. 1998;21 Suppl 2:B138–41.
Philipps LH, Santhakumaran S, Gale C, et al. The diabetic pregnancy and offspring BMI in childhood: a systematic review and meta-analysis. Diabetologia. 2011;54:1957–66.
Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003;189:1698–704.
Silverman BL, Metzger BE, Cho NH, Loeb CA. Impaired glucose tolerance in adolescent offspring of diabetic mothers. Relationship to fetal hyperinsulinism. Diabetes Care. 1995;18:611–7.
Dabelea D, Hanson RL, Lindsay RS, et al. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes. 2000;49:2208–11.
Gautier JF, Wilson C, Weyer C, et al. Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes. Diabetes. 2001;50:1828–33.
Plagemann A, Harder T, Kohlhoff R, Rohde W, Dorner G. Glucose tolerance and insulin secretion in children of mothers with pregestational IDDM or gestational diabetes. Diabetologia. 1997;40:1094–100.
Plagemann A, Harder T, Kohlhoff R, Rohde W, Dorner G. Overweight and obesity in infants of mothers with long-term insulin-dependent diabetes or gestational diabetes. Int J Obes Relat Metab Disord. 1997;21:451–6.
Lawlor DA, Lichtenstein P, Langstrom N. Association of maternal diabetes mellitus in pregnancy with offspring adiposity into early adulthood: sibling study in a prospective cohort of 280,866 men from 248,293 families. Circulation. 2011;123:258–65. This study is one of the few studies which applied the family design and sibiling comparision in the analyses. It provides the important edidence for the understadning the relative contribution of intraunterine environment vs. family environment and genetic factors on the risk of offspring obesity and diabetes.
Pirkola J, Pouta A, Bloigu A, et al. Risks of overweight and abdominal obesity at age 16 years associated with prenatal exposures to maternal prepregnancy overweight and gestational diabetes mellitus. Diabetes Care. 2010;33:1115–21.
Lawlor DA, Fraser A, Lindsay RS, et al. Association of existing diabetes, gestational diabetes and glycosuria in pregnancy with macrosomia and offspring body mass index, waist and fat mass in later childhood: findings from a prospective pregnancy cohort. Diabetologia. 2010;53:89–97.
Kim SY, England JL, Sharma JA, Njoroge T. Gestational diabetes mellitus and risk of childhood overweight and obesity in offspring: a systematic review. Exp Diabetes Res. 2011;2011:541308.
Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ. Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care. 2007;30:2287–92.
Dabelea D, Mayer-Davis EJ, Lamichhane AP, et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH Case-Control Study. Diabetes Care. 2008;31:1422–6.
Parker M, Rifas-Shiman SL, Belfort MB, et al. Gestational glucose tolerance and cord blood leptin levels predict slower weight gain in early infancy. J Pediatr. 2011;158:227–33.
Crume TL, Ogden L, Daniels S, Hamman RF, Norris JM, Dabelea D. The impact of in utero exposure to diabetes on childhood body mass index growth trajectories: the EPOCH study. J Pediatr. 2011;158:941–6.
Seyoum B, Kiros K, Haileselase T, Leole A. Prevalence of gestational diabetes mellitus in rural pregnant mothers in northern Ethiopia. Diabetes Res Clin Pract. 1999;46:247–51.
Schmidt M, Matos M, Reichelt A, Forti A, de Lima L, Duncan B. Prevalence of gestational diabetes mellitusñdo the new WHO criteria make a difference? Diabet Med. 2000;17:376–80.
Aljohani N, Rempel B, Ludwig S, et al. Gestational diabetes in Manitoba during a twenty-year period. Clin Invest Med. 2008;31, E131.
Menacker F, Martin J. Expanded health data from the new birth certificate, 2005. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2008;56:1.
Jensen D, Molsted-Pedersen L, Beck-Nielsen H, Westergaard J, Ovesen P, Damm P. Screening for gestational diabetes mellitus by a model based on risk indicators: a prospective study. Am J Obstet Gynecol. 2003;189:1383–8.
Pöyhönen-Alho M, Teramo K, Kaaja R, Hiilesmaa V. 50 gram oral glucose challenge test combined with risk factor-based screening for gestational diabetes. Eur J Obstet Gynecol Reprod Biol. 2005;121:34–7.
Griffin M, Coffey M, Johnson H, et al. Universal vs. risk factor-based screening for gestational diabetes mellitus: detection rates, gestation at diagnosis and outcome. Diabet Med. 2000;17:26–32.
Di Cianni G, Volpe L, Lencioni C, et al. Prevalence and risk factors for gestational diabetes assessed by universal screening. Diabetes Res Clin Prac. 2003;62:131–7.
Weijers R, Bekedam D, Oosting H. The prevalence of type 2 diabetes and gestational diabetes mellitus in an inner city multi-ethnic population. Eur J Epidemiol. 1998;14:693–9.
Aberg A, Jˆnsson E, Eskilsson I, Landin-Olsson M, Frid A. Predictive factors of developing diabetes mellitus in women with gestational diabetes. Acta Obstet Gynecol Scand. 2002;81:11–6.
ÖStlund I, Hanson U. Repeated random blood glucose measurements as universal screening test for gestational diabetes mellitus. Acta Obstet Gynecol Scand. 2004;83:46–51.
Noussitou P, Monbaron D, Vial Y, Gaillard R, Ruiz J. Gestational diabetes mellitus and the risk of metabolic syndrome: a population-based study in Lausanne, Switzerland. Diabetes Metab. 2005;31:361–9.
Tanir H, Sener T, Gurer Kaya M H, Kaya M. A ten-year gestational diabetes mellitus cohort at a university clinic of the mid-Anatolian region of Turkey. Clin Exp Obstet Gynecol. 2005;32:241–4.
Erem C, Cihanyurdu N, Deger O, Karahan C, Can G, Telatar M. Screening for gestational diabetes mellitus in northeastern Turkey (Trabzon City). Eur J Epidemiol. 2003;18:39–43.
Dornhorst A, Paterson C, Nicholls J, et al. High prevalence of gestational diabetes in women from ethnic minority groups. Diabet Med. 1992;9:820–5.
Al Mahroos S, Nagalla D, Yousif W, Sanad H. A population-based screening for gestational diabetes mellitus in non-diabetic women in Bahrain. Ann Saudi Med. 2005;25:129.
Hossein-Nezhad A, Maghbooli Z, Vassigh A, Larijani B. Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwan J Obstet Gynecol. 2007;46:236–41.
Al-Shawaf T, Ariel A, MOGIIRABY S. Gestational diabetes and impaired glucose tolerance of pregnancy in Riyadh. BJOG Int J Obstet Gynaecol. 1988;95:84–90.
Lee C, Wang Z, Duthie S, et al. A multicentre study to investigate the prevalence of abnormal carbohydrate metabolism in Chinese pregnant women. Asia Oceania J Obstet Gynaecol. 1996;22:401–7.
Ko G, Tam W, Chan J, Rogers M. Prevalence of gestational diabetes mellitus in Hong Kong based on the 1998 WHO criteria. Diabet Med. 2002;19:80.
Zargar A, Sheikh M, Bashir M, et al. Prevalence of gestational diabetes mellitus in Kashmiri women from the Indian subcontinent. Diabetes Res Clin Prac. 2004;66:139–45.
Maegawa Y, Sugiyama T, Kusaka H, Mitao M, Toyoda N. Screening tests for gestational diabetes in Japan in the 1st and 2nd trimester of pregnancy. Diabetes Res Clin Pract. 2003;62:47–54.
Peng Chiong T, Liza Ping L, Siti Zawiah O. Screening for gestational diabetes at antenatal booking in a Malaysian university hospital: The role of risk factors and threshold value for the 50-g glucose challenge test. Aust N Z J Obstet Gynaecol. 2007;47:191–7.
Chandna A, Zuberi L, Munim S. Threshold values for the glucose challenge test in pregnancy. Int J Gynaecol Obstet. 2006;94:119–20.
Siribaddana S, Deshabandu R, Rajapakse D, Silva K, Fernando D. The prevalence of gestational diabetes in a Sri Lankan antenatal clinic. Ceylon Med J. 1998;43:88.
Boriboonhirunsarn D. Sunsaneevithayakul P, Nuchangrid M. Incidence of gestational diabetes mellitus diagnosed before 20 weeks of gestation. J Med Assoc Thai Chotmaihet Thangphaet. 2004;87:1017.
Yue D, Molyneaux L, Ross G, Constantino M, Child A, Turtle J. Why does ethnicity affect prevalence of gestational diabetes? The underwater volcano theory. Diabet Med. 1996;13:748–52.
Stone C, McLachlan K, Halliday J, Wein P, Tippett C. Gestational diabetes in Victoria in 1996: incidence, risk factors and outcomes. Diabetes Care. 1998;21:B33–42.
Yapa M, Simmons D. Screening for gestational diabetes mellitus in a multiethnic population in New Zealand. Diabetes Res Clin Prac. 2000;48:217–23.
Green J, Pawson I, Schumacher L, Perry J, Kretchmer N. Glucose tolerance in pregnancy: ethnic variation and influence of body habitus. Am J Obstet Gynecol. 1990;163:86.
Berkowitz G, Lapinski R, Wein R, Lee D. Race/ethnicity and other risk factors for gestational diabetes. Am J Epidemiol. 1992;135:965.
Shen J, Tymkow C, MacMullen N. Disparities in maternal outcomes among four ethnic populations. Ethn Dis. 2005;15:492–7.
Williams E, Kimpo L. A population-based cohort study of the relation between maternal birthweight and risk of gestational diabetes mellitus in four racial/ethnic groups. Paediatr Perinat Epidemiol. 1999;13:452–65.
Kieffer E, Carman W, Gillespie B, Nolan G, Worley S, Guzman J. Obesity and gestational diabetes among African-American women and Latinas in Detroit: implications for disparities in women's health. J Am Med Womens Assoc. 2001;56:181–7.
Rosenberg T, Garbers S, Lipkind H, Chiasson M. Maternal obesity and diabetes as risk factors for adverse pregnancy outcomes: differences among 4 racial/ethnic groups. Am J Public Health. 2005;95:1545.
Esakoff T, Cheng Y, Caughey A. Screening for gestational diabetes: Different cut-offs for different ethnicities? Am J Obstet Gynecol. 2005;193:1040–4.
Savitz D, Janevic T, Engel S, Kaufman J, Herring A. Ethnicity and gestational diabetes in New York City, 1995-2003. BJOG Int J Obstet Gynaecol. 2008;115:969–78.
Getahun D, Nath C, Ananth C, Chavez M, Smulian J. Gestational diabetes in the United States: temporal trends 1989 through 2004. Am J Obstet Gynecol. 2008;198:525.
Lawrence J, Contreras R, Chen W, Sacks D. Trends in the prevalence of pre-existing diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes Care 2008.
Baraban E, McCoy L, Simon P. Increasing prevalence of gestational diabetes and pregnancy-related hypertension in Los Angeles County, California, 1991ñ2003. Prev Chronic Dis. 2008;5:A77.
Jung B. Gestational Diabetes Mellitus Surveillance in Connecticut Issue Brief Connecticut Department of Health. 2008.
Cho P. Prevalence of Diabetes During Pregnancy in Georgia. Georgia Epidemiol Report. 2008;24.
Pedula K, Hillier T, Schmidt M, Mullen J, Charles M, Pettitt D. Ethnic differences in gestational oral glucose screening in a large US population. Ethn Dis. 2009;19:414.
Dooley S, Metzger B, Cho N. Gestational diabetes mellitus. Influence of race on disease prevalence and perinatal outcome in a US population. Diabetes. 1991;40:25–9.
Indiana Facts at a Glance. Indiana State Department of Health 2009.
Hall T. Diabetes: The Burden in Montana. Montana Diabetes Project 2008.
Rettig B. The Burden of Diabetes in Nebraska. Neb Diabetes Prev Control Program. 2003.
Page M. The Burden of Diabetes in the Sooner State. Oklahoma State Dep Health. 2003.
Lockwood C. Oregon Progress Report on Diabetes. Oregon Diabetes Coalition. 2008.
The Burden of Diabetes in Pennsylvania. Pennsylvania Department of Health 2007.
Ramadhani T, Canfield M, Waller D, Case A. Medical records vs. interview responses: A comparative analysis of selected variables for linked birth defect cases. Birth Defects Res A Clin Mol Teratol. 2004;70:592–6.
Barnard P. Bloebaum L. Utah Department of Health: An Overview of Gestational Diabetes in Utah; 2003.
Wise B. Taylor H. West Virgina Diabetes Control Program: The Burden of Diabetes in West Virginia; 2002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Liwei Chen, Rachel Mayo, and Adaire Chatry declare that they have no conflict of interest.
Gang Hu declares grant support from the National Institute of Diabetes and Digestive and Kidney Diseases.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding/Support
Dr. Chen is supported by grant from the National Institute of Child Health and Human Development under Award Number R01HD082311. Dr. Hu is supported by grant from the National Institute of Diabetes and Digestive and Kidney Diseases under Award Number R01DK100790.
Additional information
This article is part of the Topical Collection on Reproductive and Perinatal Epidemiology
Rights and permissions
About this article
Cite this article
Chen, L., Mayo, R., Chatry, A. et al. Gestational Diabetes Mellitus: Its Epidemiology and Implication beyond Pregnancy. Curr Epidemiol Rep 3, 1–11 (2016). https://doi.org/10.1007/s40471-016-0063-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-016-0063-y