Abstract
Gestational diabetes (GDM), defined as glucose intolerance with first recognition in pregnancy, is one of the most common medical conditions in pregnancy. It is well known that gestational diabetes is associated with a number of obstetric and neonatal complications; however, GDM is also an important risk factor for conditions that are diagnosed far past the postpartum period. One of these, which has become increasingly recognized, is the higher risk of cardiovascular disease among people who have been diagnosed with GDM. Evidence suggests that people with GDM have a twofold higher risk of cardiovascular disease and that this risk is evident within the first decade following pregnancy. As cardiovascular disease is the leading cause of death worldwide, it is imperative that the factors that contribute to cardiovascular disease in women are delineated to inform prevention and treatment strategies. A diagnosis of GDM offers women, clinicians, and policy makers a unique opportunity to implement effective screening and treatment strategies to reduce cardiovascular disease in this population. Much more research is needed to identify the best evidence-based practices for cardiovascular disease protection in this population. Nonetheless, it is essential that people with GDM and their healthcare providers recognize this risk and the importance of continued screening, treatment, and follow-up. This chapter will discuss the relationship between GDM and cardiovascular disease. Specifically, we will review: key highlights regarding GDM epidemiology, diagnosis, and outcomes; potential pathophysiologic mechanisms for the development of cardiovascular disease following GDM; the epidemiology of cardiovascular disease following GDM; and the screening for and prevention of cardiovascular disease following GDM.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Gestational Diabetes
Definitions and Epidemiology
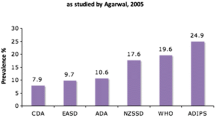
It is estimated that globally up to 17% of pregnancies are complicated by hyperglycemia in pregnancy [1]. Gestational diabetes (GDM), typically defined as glucose intolerance with first recognition in pregnancy, represents ~85% of hyperglycemic disorders in pregnancy. Its prevalence can vary significantly across populations based on the diagnostic criteria used and GDM risk factors present. However, it remains one of the commonest metabolic conditions affecting pregnant people. The prevalence of GDM continues to rise due to both person-level factors such as increasing obesity and advanced maternal age as well as diagnostic considerations such as screening practices and the glucose thresholds used in the diagnostic criteria.
Pathophysiology of Gestational Diabetes
Pregnancy is a time of substantial physiologic adaptation. The considerable hormonal changes that occur across pregnancy are essential to facilitate maternal–fetal nutrient transport and support fetal growth. The increase in a number of hormones such as human placental lactogen, progesterone, estrogen, prolactin, growth hormone, and corticotropin releasing hormone during pregnancy lead to a steep rise in insulin resistance typically beginning mid-gestation [2]. Additionally, excessive endogenous glucose production occurs as a result of hepatic gluconeogenesis and maternal glucose uptake inhibition. Gestational diabetes develops from the inability of pancreatic β-cells to meet the higher demands due to the combination of increased insulin resistance and excessive endogenous glucose production in the latter half of pregnancy.
Gestational Diabetes Diagnosis and Risk Factors
The diagnostic criteria debate is contentious and there remains no global consensus on the optimal diagnostic criteria for diagnosing GDM. Thus, international guidelines differ in terms of which criteria should be used. Likely the most commonly used diagnostic criteria are from the International Association of the Diabetes and Pregnancy Study Group (IADPSG), which diagnoses GDM based on a one-step 75 g 2-h oral glucose tolerance test (OGTT) [3]. While the screening and diagnostic criteria differ, almost all major international diagnostic criteria use dynamic glucose testing (e.g., 75 g OGTT, 50 g glucose challenge, 100 g OGTT) [4]. Most guidelines recommend screening for GDM occur at ~24–28 weeks’ gestation [5,6,7]. There remains controversy about the role for screening for GDM in early pregnancy as we currently lack published large randomized controlled trials to demonstrate the risks and/or benefits of early screening. Additionally, the recommendations for who should be screened for GDM also differ with some guidelines recommending risk factor-based screening and others recommending universal screening for GDM. Risk factors for GDM are summarized in Box 9.1.
Box 9.1: Risk Factors for Gestational Diabetes
≥ 35 years of age
From a high-risk group ethnic group (African, Arab, Asian, Hispanic, Indigenous, or South Asian)
Having a body mass index ≥ 30 kg/m2
Previous GDM
Previous birthweight > 4 kg
Family history of type 2 diabetes (first-degree relative)
Polycystic Ovary Syndrome
Acanthosis nigricans
Using corticosteroids
Having prediabetes
*Adapted from the 2018 Diabetes Canada Clinical Practice Guidelines [5]
Complications of Gestational Diabetes
The Hyperglycemia and Adverse Pregnancy Outcomes Study published in 2008 was a landmark study that established that lesser levels of hyperglycemia than overt diabetes were associated with an increased risk of complications [8]. Specifically, it demonstrated that the risk of large for gestational age (birthweight >90th centile), cord-blood C-peptide levels >90th centile, primary caesarean delivery, and neonatal hypoglycemia increased as glucose levels increased with no obvious threshold. While GDM is associated with a higher risk of pregnancy complications, large randomized controlled trials and high-quality meta-analyses have demonstrated treatment decreases the risk of a number of pregnancy complications such as primary caesarean delivery, shoulder dystocia, and large infant size (macrosomia and large for gestational age) [4, 9, 10].
While the pregnancy and neonatal complications associated with GDM are well-recognized, there are a number of metabolic long-term risks for people with GDM and their offspring associated with GDM. Type 2 diabetes is perhaps the most well recognized, with GDM being associated with a sevenfold increased risk of developing type 2 diabetes [11]. This is substantial for not only the large number of individuals being diagnosed with overt diabetes, but also in terms of the young age at diagnosis; within 10 years of delivery, about half of people with previous GDM will develop diabetes or pre-diabetes [12]. Increasingly recognized is the higher risk of future cardiovascular disease in people with GDM. A meta-analysis including over 5 million people demonstrated a twofold increased risk of cardiovascular events in people with previous GDM compared to those without GDM [13].
Pathogenesis of Gestational Diabetes as a Risk Factor for Cardiovascular Disease
The pathogenesis of GDM as a risk factor for cardiovascular disease is still being elucidated however, it is likely complex and multifactorial. This includes mechanisms such as the higher risk of type 2 diabetes, shared metabolic risk factors for GDM and cardiovascular disease, and other mechanisms such as subclinical inflammation, placental factors, and adipocyte dysfunction.
Risk of Type 2 Diabetes
Type 2 diabetes is a strong risk factor for cardiovascular disease. This may be particularly important in people with previous GDM given their young age at diagnosis. In fact, a younger age at diabetes diagnosis of type 2 diabetes confers an even stronger risk of all-cause mortality and macrovascular disease [14]. There are multiple pathogenic mechanisms that lead to diabetes causing cardiovascular disease. One important mechanism is that diabetes, a pro-inflammatory state, causes vascular inflammation and subsequent cardiovascular disease [15].
Shared Risk Factors
Gestational diabetes has many shared risk factors for the development of cardiovascular disease such as metabolic syndrome, obesity, dyslipidemia, hypertension, hypertensive disorders in pregnancy, polycystic ovary syndrome, and higher levels of deprivation. These shared risk factors likely explain part of risk of cardiovascular disease incurred with a diagnosis of GDM.
Other Mechanisms
There are a number of other postulated mechanisms that may further explain how GDM can lead to cardiovascular disease. These include subclinical inflammation, adipocyte dysfunction, placental factors, and subclinical alternations in cardiac structure or function. Interestingly, there is emerging evidence to suggest that a number of these mechanisms occur prior to pregnancy and/or persist after pregnancy [16,17,18,19]. Additional research is needed to further elucidate the pathophysiology of GDM leading to cardiovascular disease and determine the potential role for screening for biomarkers or subclinical disease may act as a risk factor for cardiovascular disease in people with previous GDM.
Epidemiology
The risk of cardiovascular disease is increased twofold in women affected by GDM compared with women without a history of GDM [13]. For women who subsequently develop type 2 diabetes, this risk is fourfold [20]. Some studies have reported that the risk of cardiovascular disease in women with GDM may be related to the development of type 2 diabetes [21], a known risk factor for cardiovascular disease, however, even without progression to type 2 diabetes, people with GDM have a higher risk of cardiovascular disease [13]. This increased risk is evident as early as the first decade after delivery [13, 22], and increases over time [22] (Fig. 9.1).
Cumulative incidence of cardiovascular hospitalization per 10,000 women over time*. (*Solid line, women with gestational diabetes, dotted, women without gestational diabetes. Results are shown for four outcomes that were representative of other cardiovascular disorders.) Reproduced from McKenzie-Sampson et al. [22] with permission from Springer Nature
Cardiovascular Disease Risk Factors
Gestational diabetes is one of many factors that may contribute to the development of cardiovascular disease among affected women. Not only do women with GDM have an almost eightfold increased risk of developing type 2 diabetes [11, 23], they are also more likely to be diagnosed with hypertension [24, 25] and dyslipidemia [26] following a pregnancy affected by GDM. Other cardiovascular risk factors that may contribute to their risk of developing cardiovascular disease include age, family history, smoking and having overweight or obesity.
A cross-sectional study compared the cardiovascular disease risk profiles of women with GDM who did and did not develop type 2 diabetes using data from the Third National Health and Nutrition Examination Survey [27]. The authors found that while there were no differences in cardiovascular risk profiles between individuals with GDM without subsequent diabetes and those without a history of GDM, individuals who developed diabetes following GDM had a higher risk of metabolic syndrome and had more cardiovascular disease risk factors [27].
Participating in healthy lifestyle behaviours may play a mitigating role in the development of cardiovascular disease in this population. A prospective cohort study of women from the Nurse’s Health Study II reported that the risk of cardiovascular disease among women with GDM was not elevated among individuals who participated in healthy lifestyle behaviours including regular physical activity, not smoking, maintaining a healthy weight, and following a good quality diet [20].
Postpartum Screening
Cardiovascular risk factors including the development of type 2 diabetes are often identifiable in the first year postpartum [28]. Clinical practice guidelines recommend postpartum screening for diabetes in all women affected by GDM in pregnancy [6]. The reported proportion of women who complete postpartum screening for type 2 diabetes is highly variable with a systematic review reporting published estimates ranged from 5.7 to 57.9% in the first three years postpartum [29]. Although some studies have reported that the proportion of women completing postpartum screening tests for diabetes following a pregnancy affected by GDM has increased over time, less than half of women are being screened for this important cardiovascular disease risk factor [29, 30]. Postpartum screening rates for other cardiovascular disease risk factors is also poor.
Reasons for not screening for diabetes following a pregnancy affected by GDM are likely multifactorial with various health systems factors, healthcare provider factors, and patient factors contributing [31]. A survey of primary care providers and women affected by GDM in Ottawa, Ontario, Canada found that >95% of respondents believed that postpartum screening for diabetes was important, yet only 37% of primary care providers reported having their patients complete screening [32].
Women affected by GDM are asked to make many adaptations to treat the condition during pregnancy including monitoring blood glucose levels frequently, making lifestyle changes, and taking medication if required, and often have regular clinical follow-up with a diabetes team to navigate these changes. In the postpartum period, mothers experience competing demands and are less focused on their own health [33]. This may contribute to less adherence to postpartum recommendations regarding screening and lifestyle changes.
Preventing Cardiovascular Disease Following Gestational Diabetes
Despite the growing body of evidence demonstrating an association between GDM and risk of cardiovascular disease, there are a number of challenges when considering risk reduction in this population [13]. It is becoming increasingly noted that women have been historically excluded from or underrepresented in cardiovascular studies and trials. This may be particularly true for women of reproductive age who are at risk of pregnancy or who may be breastfeeding as these are common exclusion criteria for clinical trials. Thus, there remains a paucity of clinical trial evidence guiding the evaluation of cardiovascular risk and cardiovascular risk reduction strategies in this population [34]. Nonetheless, pregnancy and the postpartum period are a critical window of opportunity to reduce cardiovascular risk as this is often a time of engagement with the healthcare team.
As we await more clinical trials and studies to guide us, there are a number of strategies we can use to reduce the risk of cardiovascular disease following GDM. These include the prevention or delay of type 2 diabetes onset, the management of other cardiovascular risk factors as well as a variety of other considerations.
Preventing or Delaying Type 2 Diabetes Following Gestational Diabetes
While the risk of cardiovascular disease following GDM is not exclusively mediated through type 2 diabetes, preventing or delaying type 2 diabetes onset remains of paramount importance in cardiovascular risk reduction. It has been increasingly recognized that early onset type 2 diabetes (< 40 years) is an aggressive phenotype for the development of macro and microvascular complications [35, 36]. Given that half of people with GDM develop diabetes or prediabetes within 10 years postpartum, most people who develop type 2 diabetes following GDM will do so at a young age.
There is evidence for both lifestyle and pharmacotherapy for preventing or delaying type 2 diabetes onset. The landmark Diabetes Prevention Program (DPP) demonstrated that intensive lifestyle intervention and metformin reduced the risk of type 2 diabetes by 58% and 31% respectively in people at high risk for diabetes [37]. An analysis of the 10-year follow-up data examined the 350 women with a history of GDM who participated in the DPP [38]. This study demonstrated that both the intensive lifestyle intervention and metformin were effective in reducing progression to overt diabetes. Unlike the larger study population, metformin was found to be as efficacious as lifestyle therapy in the prevention of diabetes in this population.
A number of studies, trials, and systematic reviews have been published since the DPP examining strategies to reduce diabetes risk specifically following GDM. Overall, they suggest that both lifestyle and pharmacologic interventions are effective in delaying the onset of type 2 diabetes [39]. However, there are a number of things to highlight when translating this into clinical practice. The first is the presence of publication bias, with the presence of small positive trials and the absence small negative trials being noted in a recent high-quality review on lifestyle intervention trials [40]. The second is if clinical trial results can be effectively translated into real-world settings. The postpartum period is a busy and often stressful time in which many people find prioritizing their own health challenging. Intensive lifestyle therapy may not be a realistic or affordable option for many people in the postpartum period or the years to follow. Pharmacologic therapy may be a more feasible option for many people postpartum but evidence remains limited to metformin at this time. Ongoing studies in other classes of diabetes medication such as dipeptidyl peptidase 4 (DPP-4) inhibitors, sodium-glucose cotransporter 2 (SGLT-2) inhibitors, and glucagon-like peptide-1 (GLP-1) agonists may demonstrate other effective therapies.
There is a large body of evidence that has demonstrated that breastfeeding is associated with a lower risk of developing type 2 diabetes in both people with previous GDM and their offspring [41,42,43]. While we lack randomized controlled trial evidence to support causation, given the many benefits of breastfeeding, it is recommended in people who are able and willing to do so [5].
Treating Cardiovascular Disease Risk Factors—Postpartum Considerations
As GDM has been recognized as a pregnancy associated risk factor for cardiovascular disease, ongoing cardiovascular disease risk surveillance and treatment post-GDM is warranted. This includes but is not limited to screening for hypertension, dyslipidemia, microalbuminuria, obesity, and smoking [34]. Effective screening strategies and treatments for cardiovascular risk factors are detailed elsewhere however, there are a number special considerations to consider in the postpartum population.
Since the higher cardiovascular disease risk after GDM is evident within the first decade following pregnancy, screening for and treatment of cardiovascular risks should occur early and often [13, 34]. Studies examining postpartum screening for overt diabetes indicate that few people are being screened for diabetes alone postpartum. As few as 1 in 2 people with GDM are being screened for diabetes within the year after pregnancy and only 1 in 3 are receiving the guideline recommended screening test [44]. There remains much work to do to improve postpartum screening for diabetes in addition to screening for other cardiovascular risk factors. Ongoing studies of postpartum cardiovascular risk prevention strategies may offer more insight into the best strategy to manage cardiovascular risks in the postpartum period.
Risk prediction is an important tenet in the prevention of cardiovascular disease however, this may be especially challenging in women. Unfortunately, current risk prediction tools have low validity in young women. Additional research is need to develop and validate risk prediction tools in young females and consider pregnancy associated cardiovascular risk factors.
Safe Effective Contraception
Any discussion of risk management in the postpartum period must include safe effective contraception for those at risk of pregnancy. Many key cardiovascular risk reduction medications such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers, SGLT-2 inhibitors, and statins may be unsafe or lack adequate safety data for their use in the setting of pregnancy or lactation. A number of studies highlight the lack of safe effective contraception in people at risk of pregnancy with diabetes and misconceptions about contraception in people with cardiovascular disease or risk factors [45, 46]. While cardiovascular risk should always be considered and discussed with people when choosing a contraception method, there are a number of options still available. Lower risk yet effective options include the intrauterine device (copper or levonorgestrel), subdermal implant, progestin-only pills, and vasectomy where applicable [47,48,49,50]. While barrier methods are low risk, they have a high failure rate when used alone and therefore should be considered after or in addition to other options [47] (Table 9.1).
Future Directions
Gestational diabetes is a common endocrine disorder affecting pregnancy and is associated with an increased risk of developing cardiovascular risk factors and cardiovascular disease. Robust studies evaluating this association over time are needed along with evidence informed strategies to improve education about and prevention of the long-term cardiovascular sequelae of GDM. Until then, it is important to discuss screening and risk reduction strategies of type 2 diabetes and cardiovascular disease in all people with GDM.
References
Guariguata L, Linnenkamp U, Beagley J, Whiting DR, Cho NH (2014) Global estimates of the prevalence of hyperglycaemia in pregnancy. Diabetes Res Clin Pract 103(2):176–185
Garcia-Patterson A, Gich I, Amini SB, Catalano PM, de Leiva A, Corcoy R (2010) Insulin requirements throughout pregnancy in women with type 1 diabetes mellitus: three changes of direction. Diabetologia 53(3):446–451
Metzger BE, Gabbe SG, Persson B, Buchanan TA et al (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682
Pillay J, Donovan L, Guitard S, Zakher B, Gates M, Gates A et al (2021) Screening for gestational diabetes: updated evidence report and systematic review for the us preventive services task force. JAMA 326(6):539–562
Diabetes Canada Clinical Practice Guidelines Expert Committee, Feig DS, Berger H, Donovan L, Godbout A, Kader T et al (2018) Diabetes and pregnancy. Can J Diabetes 42(Suppl 1):S255–S282
National Institute for Health and Care Excellence. Diabetes in pregnancy: management from preconception to the postnatal period UK2020. Available from: https://www.nice.org.uk/guidance/ng3
American Diabetes A. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 44(Suppl 1):S15–S33
Hapo Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B et al (2009) A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 361(14):1339–1348
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS et al (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352(24):2477–2486
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373(9677):1773–1779
Lowe WL Jr, Scholtens DM, Lowe LP, Kuang A, Nodzenski M, Talbot O et al (2018) Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA 320(10):1005–1016
Kramer CK, Campbell S, Retnakaran R (2019) Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia 62(6):905–914
Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T et al (2021) Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 64(2):275–287
Pickup JC (2004) Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care 27(3):813–823
Gunderson EP, Quesenberry CP Jr, Jacobs DR Jr, Feng J, Lewis CE, Sidney S (2010) Longitudinal study of prepregnancy cardiometabolic risk factors and subsequent risk of gestational diabetes mellitus: the CARDIA study. Am J Epidemiol 172(10):1131–1143
Quotah OF, Poston L, Flynn AC, White SL (2022) Metabolic profiling of pregnant women with obesity: an exploratory study in women at greater risk of gestational diabetes. Metabolites 12(10)
Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B (2010) Low adiponectin concentration during pregnancy predicts postpartum insulin resistance, beta cell dysfunction and fasting glycaemia. Diabetologia 53(2):268–276
Oliveira AP, Calderon IM, Costa RA, Roscani MG, Magalhaes CG, Borges VT (2015) Assessment of structural cardiac abnormalities and diastolic function in women with gestational diabetes mellitus. Diab Vasc Dis Res 12(3):175–180
Tobias DK, Stuart JJ, Li S, Chavarro J, Rimm EB, Rich-Edwards J et al (2017) Association of history of gestational diabetes with long-term cardiovascular disease risk in a large prospective cohort of US women. JAMA Intern Med 177(12):1735–1742
Shah BR, Retnakaran R, Booth GL (2008) Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care 31(8):1668–1669
McKenzie-Sampson S, Paradis G, Healy-Profitos J, St-Pierre F, Auger N (2018) Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: a retrospective cohort study. Acta Diabetol 55(4):315–322
You H, Hu J, Liu Y, Luo B, Lei A (2021) Risk of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis. Indian J Med Res 154(1):62–77
Tobias DK, Hu FB, Forman JP, Chavarro J, Zhang C (2011) Increased risk of hypertension after gestational diabetes mellitus: findings from a large prospective cohort study. Diabetes Care 34(7):1582–1584
Daly B, Toulis KA, Thomas N, Gokhale K, Martin J, Webber J et al (2018) Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. PLoS Med 15(1):e1002488
Retnakaran R, Shah BR (2022) Mediating effect of vascular risk factors underlying the link between gestational diabetes and cardiovascular disease. BMC Med 20(1):389
Kim C, Cheng YJ, Beckles GL (2008) Cardiovascular disease risk profiles in women with histories of gestational diabetes but without current diabetes. Obstet Gynecol 112(4):875–883
Smith G, Louis J, Saade G (2019) Pregnancy and the postpartum period as an opportunity for cardiovascular risk identification and management. Obstet Gynecol 134(4)
Jones EJ, Hernandez TF, Edmonds JK, Edmonds JF, Ferranti EP, Ferranti EP (2019) Continued disparities in postpartum follow-up and screening among women with gestational diabetes and hypertensive disorders of pregnancy: a systematic review (1550-5073 (Electronic))
Carson MP, Frank MI, Keely E (2013) Original research: postpartum testing rates among women with a history of gestational diabetes–systematic review. Prim Care Diabetes 7(3):177–186
Nielsen KK, Kapur A, Damm P, de Courten M, Bygbjerg IC (2014) From screening to postpartum follow-up—the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth 14(1):41
Keely E, Clark H, Karovitch A, Graham I (2010) Screening for type 2 diabetes following gestational diabetes: family physician and patient perspectives. Can Fam Physician 56(6):558–563
Lie ML, Hayes L, Lewis-Barned NJ, May C, White M, Bell R (2013) Preventing type 2 diabetes after gestational diabetes: women’s experiences and implications for diabetes prevention interventions. Diabet Med 30(8):986–993
Nerenberg KA, Cooke CL, Smith GN, Davidge ST (2021) Optimising women’s cardiovascular health after hypertensive disorders of pregnancy: a translational approach to cardiovascular disease prevention. Can J Cardiol 37(12):2056–2066
Today Study Group, Bjornstad P, Drews KL, Caprio S, Gubitosi-Klug R, Nathan DM et al (2021) Long-term complications in youth-onset type 2 diabetes. N Engl J Med 385(5):416–426
Yamamoto JM, Murphy HR (2023) Treating to target glycaemia in type 2 diabetes pregnancy. Curr Diabetes Rev 19(2):e010222200742
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346(6):393–403
Aroda VR, Christophi CA, Edelstein SL, Zhang P, Herman WH, Barrett-Connor E et al (2015) The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab 100(4):1646–1653
Hedeager Momsen AM, Hotoft D, Ortenblad L, Friis Lauszus F, Krogh RHA, Lynggaard V et al (2021) Diabetes prevention interventions for women after gestational diabetes mellitus: an overview of reviews. Endocrinol Diabetes Metab 4(3):e00230
Retnakaran M, Viana LV, Kramer CK (2023) Lifestyle intervention for the prevention of type 2 diabetes in women with prior gestational diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 25(5):1196–1202
Martens PJ, Shafer LA, Dean HJ, Sellers EA, Yamamoto J, Ludwig S et al (2016) Breastfeeding initiation associated with reduced incidence of diabetes in mothers and offspring. Obstet Gynecol 128(5):1095–1104
Gunderson EP, Hurston SR, Ning X, Lo JC, Crites Y, Walton D et al (2015) Lactation and progression to type 2 diabetes mellitus after gestational diabetes mellitus: a prospective cohort study. Ann Intern Med 163(12):889–898
Jager S, Jacobs S, Kroger J, Fritsche A, Schienkiewitz A, Rubin D et al (2014) Breast-feeding and maternal risk of type 2 diabetes: a prospective study and meta-analysis. Diabetologia 57(7):1355–1365
Butalia S, Donovan L, Savu A, Johnson J, Edwards A, Kaul P (2017) Postpartum diabetes testing rates after gestational diabetes mellitus in Canadian women: a population-based study. Can J Diabetes 41(6):613–620
Forde R, Patelarou EE, Forbes A (2016) The experiences of prepregnancy care for women with type 2 diabetes mellitus: a meta-synthesis. Int J Womens Health 8:691–703
Murphy HR, Temple RC, Ball VE, Roland JM, Steel S, Zill EHR et al (2010) Personal experiences of women with diabetes who do not attend pre-pregnancy care. Diabet Med 27(1):92–100
O’Kelly AC, Michos ED, Shufelt CL, Vermunt JV, Minissian MB, Quesada O et al (2022) Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res 130(4):652–672
Trussell J (2011) Contraceptive failure in the United States. Contracept 83(5):397–404
Lindley KJ, Bairey Merz CN, Davis MB, Madden T, Park K, Bello NA et al (2021) Contraception and reproductive planning for women with cardiovascular disease: JACC focus seminar 5/5. J Am Coll Cardiol 77(14):1823–1834
World Health Organization (2015) Medical eligibility criteria for contraceptive use 5th ed. Available from: https://www.who.int/publications/i/item/9789241549158
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Benham, J.L., Yamamoto, J.M. (2023). Gestational Diabetes as a Risk Factor for Cardiovascular Disease. In: Kirshenbaum, L., Rabinovich-Nikitin, I. (eds) Biology of Women’s Heart Health. Advances in Biochemistry in Health and Disease, vol 26. Springer, Cham. https://doi.org/10.1007/978-3-031-39928-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-39928-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-39927-5
Online ISBN: 978-3-031-39928-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)