Abstract
Purpose of Review
E-cigarette use (vaping) among adults has increased, and various patterns of concurrent smoking and vaping (i.e., “dual use”) have emerged. Understanding dual use is important for mitigating tobacco-related harm. This narrative review summarizes recent research on dual use, including prevalence and types of dual use, sociodemographic and psychiatric characteristics, nicotine dependence, reasons for dual use, harm perceptions, toxicant exposure, trajectories of dual use, and emerging treatments for dual use.
Recent Findings
Nearly half of e-cigarette users concurrently use cigarettes, and many smoke more frequently than they use e-cigarettes. This is concerning because dual users are exposed to both cigarette and potential e-cigarette toxicants and the data are mixed regarding the ability of e-cigarettes to promote smoking cessation.
Summary
Further work is needed to identify ways to increase complete smoking abstinence and optimize harm reduction among dual users, including strategies to encourage e-cigarette cessation after stopping smoking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cigarette smoking remains a leading cause of preventable death worldwide [1]. Many people who smoke cigarettes are motivated to quit smoking and attempt to do so; however, evidence-based treatments (e.g., smoking cessation counseling, pharmacotherapies) are infrequently used, and most quit attempts are unsuccessful [2,3,4]. E-cigarettes (i.e., electronic cigarettes) may serve as a substitute for cigarettes and have the potential to reduce smoking-related harms among adults who are unwilling or unable to quit using tobacco [5].
E-cigarettes – also referred to as “vapes” or electronic nicotine delivery systems (ENDS) – are battery-operated devices that aerosolize a liquid solution that may contain nicotine, propylene glycol, glycerin, flavors, and other chemicals. Although adults who smoke cigarettes may use e-cigarettes in an attempt to quit smoking [6, 7], many continue to smoke while vaping and are thus considered “dual users” of both products [8, 9]. For some people, dual use may be an interim state as they transition away from cigarettes [10, 11••, 12••]. However, the process of fully transitioning from cigarettes to e-cigarettes (or complete abstinence from tobacco) may be a long-term phenomenon, and there are known harms of continued smoking, even at low levels [13, 14]. Additionally, it is unclear how differential dependence on e-cigarettes and cigarettes influences smoking cessation success for dual users. Thus, understanding dual use is important for identifying ways to mitigate harm from combustible cigarette use.
Notably, research on dual use has surged over the last decade. A PubMed search of “dual use” AND “smoking OR cigarette” AND “vaping OR e-cigarette OR ENDS OR electronic cigarette” in July 2022 yielded 580 journal articles published on this topic since 2011 (Fig. 1). There was a substantial increase in research on dual use in 2019, roughly coinciding with the increased popularity of Juul e-cigarettes and other nicotine-salt products in the USA, which deliver nicotine with high efficiency at levels comparable to combusted cigarettes [15]. As e-cigarette devices continue to evolve and adjust to changing regulatory environments (e.g., improving technology of ENDS, restricting the availability of e-cigarettes, e-cigarette brands, or flavors), regular review of the literature on dual use is necessary to help guide public health policy and inform treatment approaches.
Given the critical public health goal of reducing harm from combustible cigarette use and the growing interest in determining whether e-cigarettes may facilitate smoking cessation for adult smokers, this review focuses on understanding dual use among adults. Systematic reviews and meta-analyses have previously examined the effects of e-cigarettes on smoking cessation outcomes [11••, 12••]. To avoid duplicating these efforts, this narrative review provides a current summary of important topics within the dual use literature to help characterize individuals who are dual users, inform public messaging efforts, and highlight potential treatment methods. The topics reviewed include (1) prevalence and types of dual use, (2) sociodemographic and psychiatric characteristics of dual users, (3) nicotine dependence, (4) reasons for dual use, (5) beliefs about the relative harm of e-cigarettes, (6) toxicant exposure, (7) trajectories of dual use, and (8) emerging treatments for dual use. We also identify gaps in the literature and potential areas for future research. This broad narrative review of the dual use literature spans research from the introduction of e-cigarettes to the advent of pod-based systems and nicotine salt e-liquids. As such, readers should keep in mind the generations of e-cigarette products that were on the market at the time of each study [16].
Prevalence and Types of Dual Use
Prevalence and types of dual use can be affected by environmental factors such as what types of products are allowed to be sold and how products are allowed to be marketed. In 2016, an international sample of adults currently using cigarettes, recent quitters, and/or e-cigarette users who formerly smoked (i.e., the International Tobacco Control Four Country Tobacco and Vaping [ITC 4CV] survey) found that dual use rates were highest in Canada (13.0%), followed by England (12.4%), and the USA (10.2%), and lowest in Australia (2.6%) [17••]. The variability in prevalence is consistent with variability in regulatory environments (e.g., e-cigarettes are currently legal and approved for smoking cessation in England, but nicotine-containing e-cigarettes are illegal without a prescription in Australia). In the USA, where restrictions on e-cigarettes were minimal until recently, 2018–2020 national surveys suggest there are at least 2 million dual cigarette and e-cigarette users, representing about 1–2% of the US adult population [18, 19]. Dual use among current e-cigarette users is quite high: For example, data from the 2018–2019 US Tobacco Use Supplement to the Current Population survey found that 39% of current e-cigarette users were also current smokers [19].
Types of dual use can be studied by examining the frequency of using cigarettes versus e-cigarettes among dual users. Some researchers have suggested 4 major subgroups for characterizing dual use: (1) daily use of cigarettes and non-daily use of e-cigarettes (predominant smokers), (2) non-daily use of cigarettes and daily use of e-cigarettes (predominant vapers), (3) daily use of both products (dual daily users), and (4) non-daily use of both products (dual non-daily users) [17••]. According to data from the 2016 ITC 4CV survey, predominant smokers were the largest subgroup of dual users across countries (1.6% in Australia to 6.5% in England), whereas predominant vapers were typically the smallest subgroup (0.2% in Australia to 1.2% in England) [17••]. The observation that predominant smokers are more prevalent than predominant vapers regardless of differences in tobacco regulation may be due to a variety of pathways. One potential pathway is that some smokers may become dual users deliberately (e.g., vaping as a way to circumvent smoke-free policies or with the intent of reducing but not quitting smoking). Another potential pathway is that smokers who take up e-cigarettes intending to quit smoking may become stuck in the transition and instead become dual users.
Sociodemographic and Psychiatric Characteristics
To the extent that dual use may help (or hinder) efforts to quit smoking, understanding which populations are likely to be dual users versus exclusive cigarette smokers is important for addressing tobacco-related health disparities. Dual use prevalence does not appear to differ by sex [19,20,21]; dual use rates are higher among women who are not pregnant (3.7%) than among pregnant women (1.4%) [22]. However, it should be noted that dual use is high among pregnant women who smoke (38.9%), possibly indicating an attempt to reduce risk by replacing smoking with vaping [23].
Regarding minoritized populations, dual use is especially low in the non-Hispanic Black population. For example, a comparison of dual use rates among current smokers observed rates of 3.8% for non-Hispanic Black compared to 8.8% for non-Hispanic White, 8.1% for Hispanic, 7.6% for American Indian/Alaskan Native, 8.2% for Asian, and 10.4% for multiracial individuals [19]. As with other patterns of tobacco use, dual use is more prevalent among US adults identifying as lesbian, gay, bisexual, or transgender (LGBT) [24,25,26]. One US study demonstrated that dual use prevalence was 4% among LGBT adults and 2% among non-LGBT adults between 2016 and 2019; after adjusting for other demographic factors, LGBT adults remained 69% more likely to report dual use than non-LGBT adults [24]. Conversely, in England, where tobacco use rates between LGBT and non-LGBT groups are less disparate, dual use rates among current smokers are similar among LGBT (15.9–22.5%) and non-LGBT adults (19.1–20.2%) [27].
In terms of education or income level, findings are mixed. Three studies found no differences in education or income level between dual or exclusive cigarette users; one study used data from the US Population Assessment of Tobacco and Health (PATH) study and analyzed education and income separately [28], the second study used ITC 4CV survey data and combined education and income level to form a composite socioeconomic status measure [17••], and the third study examined education and income level separately in a community sample of Canadian adults [20]. More recently, 2018–2019 US nationally representative data demonstrated that dual use prevalence was higher among current smokers with a college degree (9.6%) versus those with less than a high school education (5.7%) [19].
With respect to psychiatric characteristics, dual use appears to be more prevalent among adults with greater symptom severity. For example, among adults who participated in the US National Health Interview Survey (NHIS) (2014–2017), a higher percentage of those with versus without serious psychological distress (e.g., feelings of hopelessness, depression, nervousness) reported dual use (5.3% versus 1.3%, respectively) as well as exclusive cigarette use (39.5% versus 13.4%, respectively) [29]. According to the PATH study, compared to adults who report no tobacco use, adults who report dual or exclusive cigarette use are more likely to report internalizing (i.e., anxiety, depression, social withdrawal, and/or somatic complaints) and externalizing symptoms (i.e., opposition, aggression, and/or delinquent behavior) in the past 12 months (internalizing: dual users = 65.1%, smokers = 57.4%; externalizing: dual users = 61.8%, smokers = 54.1%); however, the study did not directly compare symptoms between the dual and exclusive cigarette use groups [30]. Similarly, in a sample of N = 422 smokers and dual users with no plans to quit smoking or vaping within the next 30 days recruited from a midwestern US state, a higher percentage of dual users (61.2%) versus exclusive smokers (43.4%) reported ever being diagnosed or treated for a psychiatric diagnosis [21].
Nicotine Dependence
Assessing nicotine dependence – a complex construct associated with neural adaptation, withdrawal symptoms, and chronic use despite a desire to quit [31] – can provide important insight into the potential risks of dual use as well as inform treatment approaches and predict cessation success. Nicotine dependence is assessed according to the product (e.g., cigarettes) [32,33,34,35]. Several cigarette dependence measures have been adapted for use with e-cigarette users, including the Fagerström Test of Cigarette Dependence (FTCD) and the Wisconsin Inventory of Smoking Dependence Motives (WISDM) [36, 37]. There are also new measures that have been specifically developed to assess e-cigarette dependence such as the Penn State E-cigarette Dependence Index (PS-ECDI) [38] and the E-cigarette Dependence Scale [39].
Research using these validated scales suggests that product-specific assessment of dependence is appropriate for dual users. For instance, one study found no correlation between the combustible and e-cigarette versions of the FTCD, WISDM, or PS-ECDI among dual users [40•]. Furthermore, among dual users, the cigarette and e-cigarette versions of these scales only predicted use and cessation rates of the product being assessed and were unrelated to the use or cessation of the other product (e.g., e-cigarette dependence was related to e-cigarette use and cessation but not cigarette use or cessation) [40•]. It should be noted that a 16-item measure of tobacco dependence developed in the PATH study using items from validated scales also assesses dependence by specific tobacco product. Items from this scale indicate a single underlying tobacco dependence construct with predictive validity that effectively measures dependence across products [41, 42]. However, the differential performance of e-cigarette and combustible cigarette items has not been examined among dual users.
Apart from full scales discussed above, nicotine dependence may be assessed with key product use behaviors such as the daily amount of nicotine consumed (e.g., number of cigarettes, mL of e-liquid) and time to first use in the morning (i.e., indicative of need to consume nicotine after overnight abstinence) [43]. Assessing dependence based on such behaviors may provide further insight into product-specific dependence among dual users. For example, a longitudinal observational study demonstrated that dual users who more frequently used e-cigarettes before cigarettes in the morning reported higher e-cigarette and lower cigarette dependence, and at 1-year follow-up were less likely to be smoking and more likely to be vaping [40•]. More research is needed to understand the development of dual dependence on combustible cigarettes and e-cigarettes and how such dual dependency might influence smoking and vaping cessation. Importantly, investigators should carefully consider variations in e-cigarette device characteristics (e.g., wattage, model) and components of e-liquids that can have a substantial impact on nicotine exposure and dependence [44].
Reasons for Dual Use
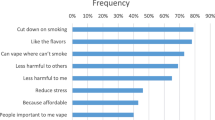
Adult dual users have reported a wide variety of reasons for e-cigarette use. Most dual users (over half) report using e-cigarettes to quit or cut down on cigarette smoking [19, 22, 45,46,47]. Other common reasons for e-cigarette use reported by dual users include coping with nicotine craving/withdrawal symptoms, evading smoke-free policies, and/or reducing secondhand smoke [45,46,47]. Additionally, appealing flavors and greater affordability of e-cigarettes relative to cigarettes are reasons that have been reported in multiple studies [45]. Older dual users (age 40 and older) may be more likely than younger dual users (18–24-year-olds) to use e-cigarettes to cut down on smoking and for affordability rather than enjoyment [47]. However, daily versus non-daily e-cigarette users may be more likely to report using e-cigarettes for enjoyment regardless of age [47].
Complementing survey studies, qualitative research has explored barriers to either completely switching to e-cigarettes or quitting both products. Interviews with 20 dual using adults in New Zealand found that common reasons for not fully switching from cigarettes to e-cigarettes included (1) “inauthenticity” of vaping compared to smoking (i.e., vaping failing to simulate smoking, thus resulting in an unsatisfying experience), (2) that smoking reduction without quitting was “success” enough, and (3) that when around other smokers, smoking was more socially acceptable than vaping, the latter of which sometimes had a derogated status [48]. Studies in the USA and England have produced similar findings (e.g., reports that e-cigarettes are an inadequate substitute for cigarettes when stressed, smoking is more acceptable than vaping in certain social contexts) [49,50,51,52].
Beliefs about Relative Harm
Examining dual users’ beliefs about cigarettes and e-cigarettes is essential for understanding their expectations and goals of use and how they may be encouraged to quit smoking. In alignment with the current scientific consensus [53, 54], many e-cigarette users and non-users believe e-cigarettes to be less harmful than cigarettes; however, multiyear analyses indicate a significant decrease in the proportion of US adults who hold this belief [55]. Data from a study of two national surveys found that 33.9–34.5% of US adults surveyed in 2017 rated e-cigarettes as less harmful than cigarettes, down from 39.4-50.7% in 2012 [55]. It may be that media coverage highlighting studies on the potential health risks of e-cigarettes (e.g., respiratory disease [56]) has broadly affected beliefs about the harms of e-cigarettes relative to cigarettes; research is needed to explore this possibility.
Importantly, harm perceptions of e-cigarettes relative to cigarettes may influence use behavior. According to the PATH study, dual users who perceived e-cigarettes to be less harmful than cigarettes were 40% less likely to later become exclusive cigarette smokers compared to dual users who perceived e-cigarettes to be equally or more harmful than cigarettes or were unsure about their relative harmfulness [57•]. Furthermore, dual users who perceived e-cigarettes to be less harmful than cigarettes (versus equally/more/unsure) were 3 times more likely to later become exclusive e-cigarette users and just as likely to become non-users of both products [57•]. In line with these findings, evidence from the ITC 4CV survey indicated that dual users who predominantly used e-cigarettes reported more positive attitudes toward vaping and more negative attitudes toward smoking compared to predominant smokers and dual daily users [17••].
Toxicant Exposure
Given the literature reviewed above, it is important for researchers, clinicians, and the public to understand current science regarding the absolute and relative risks of e-cigarettes and cigarettes. Harmful chemicals in cigarette smoke include tobacco-specific nitrosamines (TSNAs), heavy metals, polycyclic aromatic hydrocarbons (PAHs), and volatile organic compounds (VOCs) with known or suspected carcinogenic properties [58], and nicotine exposure during pregnancy is associated with impaired fetal brain and lung development [59, 60]. Cigarette smoke also contains chemicals that contribute to the development of cardiac (e.g., carbon monoxide, arsenic, cyanide) and pulmonary disease (e.g., acrolein, acetaldehyde), and smoking just one cigarette per day may be enough to reach exposure thresholds for adverse health effects [61, 62].
Exclusive use of e-cigarettes may reduce exposure to many of the toxicants described above (e.g., PAHs, VOCs) [22, 58]. However, evidence from the PATH study indicates that dual users and exclusive smokers have comparable levels of exposure to multiple toxicants [22, 58], and similar findings have been reported elsewhere [10, 21]. This suggests that typical dual use (e.g., predominant smoking [17••]) may be no safer than exclusive cigarette use. However, a recent randomized clinical trial demonstrated that dual use characterized by more frequent e-cigarette use and only intermittent cigarette use was associated with significant reductions in NNAL (a TSNA and potent lung carcinogen) and carbon monoxide [63•, 64]. Thus, dual use pattern (e.g., predominant smoking versus predominant vaping [17••]) may be an important predictor of overall toxicant exposure.
Despite the potential for (predominant or exclusive) e-cigarette use to reduce exposure to many of the toxicants found in cigarettes, e-cigarette use may involve novel risks. E-cigarettes work by aerosolizing e-liquid with heating components containing toxic metals (e.g., cadmium) [65]. Accordingly, heavy metal exposure may not be reduced by exclusive e-cigarette use [22, 58]. In addition, e-liquids contain chemicals such as propylene glycol, glycerin, and flavorings, some of which are associated with negative health outcomes when inhaled [66, 67]. Thus, on the continuum of harm reduction, evidence generally supports dual users minimizing harm by transitioning to exclusive e-cigarette use. As the long-term health consequences of e-cigarette use are still being investigated, stopping e-cigarette use after successfully quitting smoking may be important to eliminate harm.
Trajectories of Dual Use
To achieve the goal of maximizing harm reduction, it is important to understand product use patterns and transitions among dual users. Dual use may be an interim state for people attempting to quit cigarette smoking. While some studies indicate that e-cigarette use is associated with success quitting smoking [11••], findings are mixed in population studies [12••], and some evidence suggests that continued vaping may increase the risk of smoking relapse [68]. Examining trajectories of dual use can provide insight into what factors influence smoking cessation or continuation among dual users.
Observational studies generally do not support e-cigarette use for smoking cessation [12••]. For example, one longitudinal study demonstrated that dual users (versus exclusive cigarette users) had higher rates of biochemically confirmed seven-day point-prevalence smoking abstinence at a 1-year follow-up assessment [69]. However, very few initial dual users quit smoking at the 1-year assessment: 48.8% remained dual users, 43.9% were exclusive smokers, 5.9% were exclusive e-cigarette users, and only 1.4% quit using both products [69]. Interestingly, PATH data demonstrate that those with higher tobacco dependence (combined cigarette and e-cigarette) may be less likely to transition from dual use to exclusive cigarette or e-cigarette use, but those with higher e-cigarette dependence may be more likely to transition from dual use to exclusive e-cigarette use [70]: these findings align with evidence that more frequent use of e-cigarettes versus cigarettes among adult dual users is associated with greater smoking cessation success [12••, 70].
Although e-cigarettes are generally not associated with smoking cessation in observational studies, the use of e-cigarettes has been associated with greater smoking cessation success in randomized controlled trials (RCTs) [11••, 12••]. In a recent meta-analysis of 9 RCTs from 5 countries (USA, UK, New Zealand, Italy, and Korea), it was estimated that those using e-cigarettes were 55% more likely to quit smoking compared to those using conventional smoking cessation therapies [12••]. Similarly, a recent Cochrane review found some evidence that the use of nicotine-containing e-cigarettes increased smoking cessation rates compared to placebo e-cigarettes, and adverse events associated with e-cigarette use were generally minor (e.g., transient mouth or throat irritation) [11••]. In a large RCT conducted in the UK, 18.0% of participants using e-cigarettes plus behavioral support for smoking cessation exhibited sustained 1-year smoking abstinence compared to 9.9% of participants using NRT plus behavioral support [71]. This study also demonstrated that 80% of the participants in the e-cigarette condition continued using e-cigarettes one year later compared to only 9% of participants in the NRT condition who continued using NRT [71]. Although findings from RCTs generally indicate that e-cigarettes may promote smoking cessation, questions remain about possible long-term health effects of e-cigarette use, and whether factors such as regulatory environment (e.g., e-cigarette availability, public messaging), device type, nicotine formulation, and e-cigarette flavors influence smoking cessation [12••, 72••]. Thus, more research is needed to examine how e-cigarette regulations and product characteristics affect trajectories of dual use.
Emerging Treatments
Given the known health consequences of continued cigarette smoking, finding ways to enhance smoking cessation success among dual users is critical. Evidence suggests dual users are more likely to attempt to quit smoking than those who smoke exclusively [73]. Thus, engaging dual users in smoking treatment could represent an opportunity to facilitate smoking cessation as these individuals may already be motivated to quit and have taken initial steps toward cessation by using e-cigarettes. Emerging research in this area has focused on evaluating the effectiveness of treatments that address cigarette and e-cigarette cessation concurrently.
There are two published studies of behavioral interventions to help adult dual users quit smoking and vaping, both conducted in the USA [74••, 75]. In one study, evidence-based smoking-cessation self-help materials based on cognitive-behavioral theory [76] were adapted to target dual users by providing specific strategies for using an e-cigarette to facilitate smoking abstinence. Strategies included using e-cigarettes to reduce nicotine withdrawal and craving, only using e-cigarettes in places one would normally smoke, and gradually tapering nicotine levels in the e-cigarette to eventually stop vaping [77, 78]. In this manner, e-cigarettes functioned as a nicotine replacement strategy. Dual users who were not necessarily seeking treatment or motivated to quit smoking or vaping (N = 2896) were randomized to one of three conditions: (1) self-help materials targeting dual use, (2) generic smoking-cessation self-help materials [76], or (3) assessment only (i.e., control) [74••]. Over an 18-month treatment period, participants receiving self-help materials targeting dual use had smoking abstinence rates 5–10 percentage points higher than participants in the assessment-only control condition but comparable to participants receiving generic self-help materials. While abstinence rates were higher among participants with low versus high cigarette dependence, baseline cigarette dependence moderated treatment effects such that dual users with high cigarette dependence who received self-help materials targeting dual use achieved higher abstinence rates versus the control group [74••]. These findings indicate that dual users, particularly those with greater cigarette dependence struggling to quit, could benefit from specific smoking cessation strategies that capitalize on their e-cigarette use. Future research is needed to identify effective ways to encourage eventual e-cigarette cessation.
A second study (N = 96) recruited adults who were dual users from the Oklahoma Tobacco State quitline [75]. Participants were randomized to receive either (1) quitline treatment as usual (TAU) or (2) e-cigarette enhanced coaching (EEC). Everyone received 5 coaching calls and free nicotine replacement therapy. TAU coaching support focused on setting a quit date, coping with urges, and specified that participants stop both cigarettes and e-cigarettes on their quit date when they start NRT. EEC added e-cigarette education, discussing e-cigarettes as a quitting tool similar to NRT and an alternative form of NRT, and required coaches to assess and address e-cigarette use at each call. Although this pilot study was not powered to detect differences in quit rates, outcomes assessed at 3 months indicated high ratings of treatment satisfaction and 7-day point-prevalence abstinence in both groups, and a greater number of completed coaching calls in EEC (M [SE] = 3.4 [0.24]) vs. TAU (M [SE] = 2.7 [0.19]) [75]. Additional large-scale studies are needed to evaluate the effectiveness of this intervention that has the potential for wide dissemination as a treatment for dual use.
One non-randomized study conducted in the UK used pharmacotherapy to treat dual use [79]. Dual users were enrolled and offered varenicline for up to 3 months plus phone-based smoking cessation support once weekly for 6 weeks [79]. Among the N = 204 enrolled, N = 124 (60.8%) were interested in trying varenicline and N = 80 started the medication. At the 3- and 6-month follow-up assessments, those who did (versus did not) use varenicline were more likely to be abstinent from smoking (RRs = 3.0–5.8, ps ≤ 0.006), vaping (RRs = 7.4–11.6, ps ≤ 0.007), and both products (RRs = 10.9–14.0, ps ≤ 0.02). It is sometimes assumed that adults using e-cigarettes to quit smoking are doing so because they are not interested in other methods including smoking cessation medications; however, this and other studies [80, 81] indicate that dual users are willing to use smoking cessation pharmacotherapy and that pharmacotherapy may improve their chances of quitting. This study also provides preliminary data suggesting that varenicline use among dual users may promote success in quitting smoking and vaping. Randomized trials are needed to permit causal inference.
Conclusions
In conclusion, concurrent use of cigarettes among e-cigarette users is common, and most dual users smoke more frequently than vape [17••]. This is noteworthy because although many adults report using e-cigarettes to quit or cut down on cigarette smoking [19, 22, 45,46,47], even low rates of smoking increase morbidity and mortality rates compared to not smoking [14, 61]. Thus, dual use without eventual smoking cessation poses health risks since individuals remain exposed to the toxicants contained in cigarette smoke [10, 21, 22, 58] as well as the potential toxicants contained in e-cigarette vapor.
There is evidence that e-cigarette use may facilitate smoking cessation and harm reduction among adults [11••, 12••, 71]; however, many remain dual users for extended periods and some return to exclusive cigarette smoking [68, 69, 82]. Further research is needed to identify ways to enhance smoking cessation success and optimize harm reduction among dual users, particularly among priority populations (e.g., minoritized groups, low socioeconomic status, psychiatric comorbidities) who are disproportionately burdened by tobacco-related harm. Receiving specific guidance on the use of e-cigarettes as a substitute for cigarettes [78] and using e-cigarettes more frequently (i.e., daily) [12••] may be useful strategies to help facilitate success in quitting smoking. However, little is known about how to advise those who smoke about what e-cigarette device, nicotine concentration, or flavors to use (or avoid) during a quit attempt. Additionally, research is needed to determine effective ways to educate dual users (and the general public) about e-cigarette use to stop smoking, known risks of e-cigarettes relative to cigarettes, and the importance of eventual e-cigarette cessation after quitting smoking. Currently, mass media messages about dual use are rare, and clear messaging to address dual use requires strong data.
The findings presented in this report should be interpreted considering key limitations. First, e-cigarettes represent myriad products and this may impact a variety of dual use outcomes (e.g., user behavior, nicotine exposure, dependence [44]). Unfortunately, it was not possible to partition out the findings presented in this review by specific e-cigarette characteristics. Future studies on dual use should carefully address e-cigarette product characteristics and/or clearly identify when data were collected so that readers will understand what products were available at that time. Second, as discussed, different countries have very different regulatory approaches which affect the availability of e-cigarettes, public messaging, and subsequently influence factors like dual use prevalence, reasons for dual use, and beliefs about the relative harm of e-cigarettes and cigarettes. Thus, systematic literature reviews and meta-analyses on dual use should also report the studies’ country of origin. We have identified a variety of critical research questions pertaining to dual use that need to be addressed to inform ways to reduce the public health harms of combustible tobacco. Of course, as the marketplace for e-cigarettes continues to evolve, ongoing review and synthesis of research on dual use will be critical to informing policy decisions, guiding clinical recommendations, and creating accurate and effective health messages targeting dual use.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Organization WH. WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. Geneva, Switzerland: World Health Organization. 2017. https://apps.who.int/iris/handle/10665/255874
Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38.
Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107(3):673–82.
Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000–2015. Morb Mortal Wkly Rep. 2017;65(52):1457–64.
Warner KE. How to think—not feel—about tobacco harm reduction. Nicotine Tob Res. 2019;21(10):1299–309.
Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P, et al. Reasons for current E-cigarette use among US adults. Prev Med. 2016;93:14–20.
Wackowski OA, Bover Manderski MT, Delnevo CD, Giovenco DP, Lewis MJ. Smokers’ early e-cigarette experiences, reasons for use, and use intentions. Tobacco Reg Sci. 2016;2(2):133–45.
King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010–2013. Nicotine Tob Res. 2015;17(2):219–27.
Owusu D, Huang J, Weaver SR, Pechacek TF, Ashley DL, Nayak P, et al. Patterns and trends of dual use of e-cigarettes and cigarettes among US adults, 2015–2018. Prev Med Rep. 2019;16: 101009.
Balfour DJ, Benowitz NL, Colby SM, Hatsukami DK, Lando HA, Leischow SJ, et al. Balancing consideration of the risks and benefits of e-cigarettes. Am J Public Health. 2021;111(9):1661–72.
•• Hartmann-Boyce J, McRobbie H, Butler AR, Lindson N, Bullen C, Begh R, et al. Electronic cigarettes for smoking cessation. Cochrane database of systematic reviews. 2021(9). This systematic review is very important as it provides an ongoing meta-analysis of studies examining e-cigarettes for smoking cessation. As more data on the topic emerges, it will be important to return to this review for updated evidence on what is known about using e-cigarettes for smoking cessation.
•• Wang RJ, Bhadriraju S, Glantz SA. E-cigarette use and adult cigarette smoking cessation: a meta-analysis. Am J Public Health. 2021;111(2):230–46. This meta-analysis of 64 studies (55 observational and 9 RCTs) is very important because it estimates the effect of e-cigarettes on smoking cessation among (1) all observational studies, (2) observational studies among people motivated to quit smoking, (3) people using e-cigarettes daily vs. less than daily, and (4) within randomized clinical trials. Overall, the effect sizes varied by study design and population studied, which is important for considering clinical and population-level effects.
Health UDo, Services H. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: S Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease and Health Promotion, Office on Smoking and Health. 2014.
Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health–AARP Diet and Health study. JAMA Intern Med. 2017;177(1):87–95.
Hajek P, Pittaccio K, Pesola F, Myers Smith K, Phillips-Waller A, Przulj D. Nicotine delivery and users’ reactions to Juul compared with cigarettes and other e-cigarette products. Addiction. 2020;115(6):1141–8.
Williams M, Talbot P. Design features in multiple generations of electronic cigarette atomizers. Int J Environ Res Public Health. 2019;16(16):2904.
•• Borland R, Murray K, Gravely S, Fong GT, Thompson ME, McNeill A, et al. A new classification system for describing concurrent use of nicotine vaping products alongside cigarettes (so-called ‘dual use’): findings from the ITC-4 Country Smoking and Vaping wave 1 survey. Addiction. 2019;114:24–34. Using a large, international sample, this study presented a new typology for characterizing dual use based on four product use patterns: predominant smokers (daily smoking, non-daily vaping), predominant vapers (daily vaping, non-daily smoking), dual daily users (daily smoking and vaping), and concurrent non-daily users (non-daily smoking and vaping). Importantly, this study demonstrated that dual users may differ on important characteristics, including product perceptions and attitudes and indicators of nicotine dependence.
Cornelius ME, Loretan CG, Wang TW, Jamal A, Homa DM. Tobacco product use among adults—United States, 2020. Morb Mortal Wkly Rep. 2022;71(11):397.
Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic characteristics, cigarette smoking, and e-cigarette use among US adults. JAMA Netw Open. 2020;3(10):e2020694-e.
González-Roz A, MacKillop J. No evidence of differences in smoking levels, nicotine dependence, carbon monoxide or motivational indices between cigarette smokers and cigarette+ e-cigarette dual users in two samples. Addict Behav. 2021;112: 106543.
Piper ME, Baker TB, Benowitz NL, Kobinsky KH, Jorenby DE. Dual users compared to smokers: demographics, dependence, and biomarkers. Nicotine Tob Res. 2019;21(9):1279–84.
Coleman SR, Bunn JY, Nighbor TD, Kurti AN, Bolívar HA, Tyndale RF, et al. Use of electronic nicotine delivery systems (ENDS) among US women of reproductive age: prevalence, reported reasons for use, and toxin exposure. Prev Med. 2021;152: 106582.
Liu B, Xu G, Rong S, Santillan DA, Santillan MK, Snetselaar LG, et al. National estimates of e-cigarette use among pregnant and nonpregnant women of reproductive age in the United States, 2014–2017. JAMA Pediatr. 2019;173(6):600–2. https://doi.org/10.1001/jamapediatrics.2019.0658.
Al Rifai M, Mirbolouk M, Jia X, Nasir K, Pickett JK, Nambi V, et al. E-cigarette use and risk behaviors among lesbian, gay, bisexual, and transgender adults: the Behavioral Risk Factor Surveillance System (BRFSS) survey. Kansas J Med. 2020;13:318.
Delahanty J, Ganz O, Hoffman L, Guillory J, Crankshaw E, Farrelly M. Tobacco use among lesbian, gay, bisexual and transgender young adults varies by sexual and gender identity. Drug Alcohol Depend. 2019;201:161–70.
Wheldon CW, Kaufman AR, Kasza KA, Moser RP. Tobacco use among adults by sexual orientation: findings from the population assessment of tobacco and health study. LGBT health. 2018;5(1):33–44.
Jackson SE, Brown J, Grabovac I, Cheeseman H, Osborne C, Shahab L. Smoking and quitting behavior by sexual orientation: a cross-sectional survey of adults in England. Nicotine Tob Res. 2021;23(1):124–34.
Harlow AF, Stokes A, Brooks DR. Socioeconomic and racial/ethnic differences in e-cigarette uptake among cigarette smokers: longitudinal analysis of the population assessment of tobacco and health (PATH) study. Nicotine Tob Res. 2019;21(10):1385–93.
Weinberger AH, Zhu J, Barrington-Trimis JL, Wyka K, Goodwin RD. Cigarette use, e-cigarette use, and dual product use are higher among adults with serious psychological distress in the United States: 2014–2017. Nicotine Tob Res. 2020;22(10):1875–82.
Kaplan B, Thrul J, Cohen JE. Association of cigarette and electronic nicotine delivery systems use with internalizing and externalizing problems among US adults: findings from wave 3 (2015–2016) of the PATH study. PLoS ONE. 2021;16(6): e0253061. https://doi.org/10.1371/journal.pone.0253061.
Markou A. Neurobiology of nicotine dependence. Phil Trans R Soc B: Biol Sci. 2008;363(1507):3159–68. https://doi.org/10.1098/rstb.2008.0095.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–27.
Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to tobacco dependence: the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68). J Consult Clin Psychol. 2004;72(2):139.
Piper ME, McCarthy DE, Baker TB. Assessing tobacco dependence: a guide to measure evaluation and selection. Nicotine Tob Res. 2006;8(3):339–51.
Shiffman S, Waters AJ, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327–48.
Piper ME, Baker TB, Benowitz NL, Smith SS, Jorenby DE. E-cigarette dependence measures in dual users: reliability and relations with dependence criteria and e-cigarette cessation. Nicotine Tob Res. 2020;22(5):756–63.
Rest EC, Mermelstein RJ, Hedeker D. Nicotine dependence in dual users of cigarettes and e-cigarettes: common and distinct elements. Nicotine Tob Res. 2021;23(4):662–8.
Foulds J, Veldheer S, Yingst J, Hrabovsky S, Wilson SJ, Nichols TT, et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking e-cigarette users. Nicotine Tob Res. 2015;17(2):186–92.
Morean ME, Krishnan-Sarin S, Sussman S, Foulds J, Fishbein H, Grana R, et al. Psychometric evaluation of the Patient-Reported Outcomes Measurement Information System (PROMIS) Nicotine Dependence Item Bankfor use with electronic cigarettes. Nicotine and Tobacco Res. 2020;22(11):2123.
• Piper ME, Baker TB, Mermelstein R, Benowitz N, Jorenby DE. Relations among cigarette dependence, e-cigarette dependence, and key dependence criteria among dual users of combustible and e-cigarettes. Psychology of Addictive Behaviors. 2020. In this important longitudinal, 2-year observational study, it was demonstrated that most validated measures used to assess cigarette versus e-cigarette dependence tend to be uncorrelated, and these various measures predict product-specific outcomes. As such, product-specific assessment of nicotine dependence is warranted and may aid in selecting treatment approaches.
Strong DR, Pearson J, Ehlke S, Kirchner T, Abrams D, Taylor K, et al. Indicators of dependence for different types of tobacco product users: descriptive findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) study. Drug Alcohol Depend. 2017;178:257–66.
Strong DR, Leas E, Noble M, White M, Frissell KC, Glasser A, et al. Predictive validity of the adult tobacco dependence index: findings from waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) study. Drug Alcohol Depend. 2020;214: 108134.
Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–800.
DeVito EE, Krishnan-Sarin S. E-cigarettes: impact of e-liquid components and device characteristics on nicotine exposure. Curr Neuropharmacol. 2018;16(4):438–59.
Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med. 2017;52(2):e33–66.
Rutten LJF, Blake KD, Agunwamba AA, Grana RA, Wilson PM, Ebbert JO, et al. Use of e-cigarettes among current smokers: associations among reasons for use, quit intentions, and current tobacco use. Nicotine Tob Res. 2015;17(10):1228–34.
Yong HH, Borland R, Cummings KM, Gravely S, Thrasher JF, McNeill A, et al. Reasons for regular vaping and for its discontinuation among smokers and recent ex-smokers: findings from the 2016 ITC Four Country Smoking and Vaping survey. Addiction. 2019;114:35–48.
Robertson L, Hoek J, Blank M-L, Richards R, Ling P, Popova L. Dual use of electronic nicotine delivery systems (ENDS) and smoked tobacco: a qualitative analysis. Tob Control. 2019;28(1):13–9.
Goldberg RL, Cataldo JK. Using an e-cigarette is like eating tofu when you really want meat. Am J Health Behav. 2018;42(5):54–64.
Harrell PT, Brandon TH, England KJ, Barnett TE, Brockenberry LO, Simmons VN, et al. Vaping expectancies: a qualitative study among young adult nonusers, smokers, vapers, and dual users. Subst Abus: Res Treat. 2019;13:1178221819866210.
Loud EE, Duong HT, Henderson KC, Reynolds RM, Ashley DL, Thrasher JF, et al. Addicted to smoking or addicted to nicotine? A focus group study on perceptions of nicotine and addiction among US adult current smokers, former smokers, non-smokers and dual users of cigarettes and e-cigarettes. Addiction. 2022;117(2):472–81. https://doi.org/10.1111/add.15634.
Vandrevala T, Coyle A, Walker V, Cabrera Torres J, Ordoña I, Rahman P. ‘A good method of quitting smoking’or ‘just an alternative to smoking’? Comparative evaluations of e-cigarette and traditional cigarette usage by dual users. Health Psychol Open. 2017;4(1):2055102916684648.
Control CfD: About electronic cigarettes (e-cigarettes). https://www.cdc.gov/tobacco/basic_information/e-cigarettes/about-e-cigarettes.html (2021). Accessed 22 April 2022.
National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press. 2018. https://doi.org/10.17226/24952.
Huang J, Feng B, Weaver SR, Pechacek TF, Slovic P, Eriksen MP. Changing perceptions of harm of e-cigarette vs cigarette use among adults in 2 US national surveys from 2012 to 2017. JAMA network open. 2019;2(3):e191047-e.
Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med. 2020;58(2):182–90.
• Persoskie A, O’Brien EK, Poonai K. Perceived relative harm of using e-cigarettes predicts future product switching among US adult cigarette and e-cigarette dual users. Addiction. 2019;114(12):2197–205. In this longitudinal analysis of the US Population Assessment of Tobacco and Health (PATH) study, it was demonstrated that dual users who perceived e-cigarettes as less harmful than cigarettes were more likely to become exclusive e-cigarette users or remain dual users and less likely to become exclusive cigarette smokers 1 year later. These findings highlight the important potential associations between dual users’ relative perceptions of e-cigarettes and cigarettes and tobacco use trajectories.
Goniewicz ML, Smith DM, Edwards KC, Blount BC, Caldwell KL, Feng J, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes. JAMA network open. 2018;1(8):e185937-e.
Kuniyoshi KM, Rehan VK. The impact of perinatal nicotine exposure on fetal lung development and subsequent respiratory morbidity. Birth Defects Res. 2019;111(17):1270–83. https://doi.org/10.1002/bdr2.1595.
Wickstrom R. Effects of nicotine during pregnancy: human and experimental evidence. Curr Neuropharmacol. 2007;5(3):213–22.
Bjartveit K, Tverdal A. Health consequences of smoking 1–4 cigarettes per day. Tob Control. 2005;14(5):315–20.
Fowles J, Dybing E. Application of toxicological risk assessment principles to the chemical constituents of cigarette smoke. Tob Control. 2003;12(4):424–30.
• Arnold MJ, Nollen NL, Mayo MS, Ahluwalia JS, Leavens EL, Zhang G, et al. Harm reduction associated with dual use of cigarettes and e-cigarettes in Black and Latino smokers: secondary analyses from a randomized controlled e-cigarette switching trial. Nicotine Tob Res. 2021;23(11):1972–6. In this secondary analysis of data from a randomized clinical trial, it was demonstrated that greater substitution from cigarettes to e-cigarettes was associated with larger reductions in NNAL – a potent carcinogen. Substitution of cigarettes for e-cigarettes was also associated with reduces in carbon monoxide and self-reported respiratory symptoms, but was unrelated to blood pressure or spirometry. These findings suggest that e-cigarettes may function as a harm-reduction substitute for cigarettes, particularly with higher rates of substitution.
Pulvers K, Nollen NL, Rice M, Schmid CH, Qu K, Benowitz NL, et al. Effect of pod e-cigarettes vs cigarettes on carcinogen exposure among African American and Latinx smokers: a randomized clinical trial. JAMA Netw Open. 2020;3(11):e2026324-e.
Hess CA, Olmedo P, Navas-Acien A, Goessler W, Cohen JE, Rule AM. E-cigarettes as a source of toxic and potentially carcinogenic metals. Environ Res. 2017;152:221–5.
Allen JG, Flanigan SS, LeBlanc M, Vallarino J, MacNaughton P, Stewart JH, et al. Flavoring chemicals in e-cigarettes: diacetyl, 2, 3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored e-cigarettes. Environ Health Perspect. 2016;124(6):733–9.
Muthumalage T, Lamb T, Friedman MR, Rahman I. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci Rep. 2019;9(1):1–11.
Barufaldi LA, Guerra RL, Rita de Cassia R, Nascimento A, Chanca RD, de Souza MC, et al. Risk of smoking relapse with the use of electronic cigarettes: a systematic review with metaanalysis of longitudinal studies. Tob Prev Cessation. 2021;29(29):1–10.
Piper ME, Baker TB, Benowitz NL, Jorenby DE. Changes in use patterns over 1 year among smokers and dual users of combustible and electronic cigarettes. Nicotine Tob Res. 2020;22(5):672–80.
Snell LM, Barnes AJ, Nicksic NE. A longitudinal analysis of nicotine dependence and transitions from dual use of cigarettes and electronic cigarettes: evidence from waves 1–3 of the PATH study. J Stud Alcohol Drugs. 2020;81(5):595–603.
Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–37.
•• Hung F, Wallach JD, O’Malley SS, Bold KW. Characteristics of registered clinical trials evaluating the role of e-cigarettes in cessation or reduction of cigarette smoking. JAMA Psychiat. 2021;78(11):1280–3. This study reviews completed and ongoing trials registered in the WHO clinical trial databases. Given the rapidly evolving marketplace for e-cigarettes, this review highlights very important evidence gaps in clinical trials evaluating whether e-cigarettes effectively promote smoking reduction/cessation.
Pasquereau A, Guignard R, Andler R, Nguyen-Thanh V. Electronic cigarettes, quit attempts and smoking cessation: a 6-month follow-up. Addiction. 2017;112(9):1620–8.
•• Martinez U, Simmons VN, Sutton SK, Drobes DJ, Meltzer LR, Brandon KO, et al. Targeted smoking cessation for dual users of combustible and electronic cigarettes: a randomised controlled trial. The Lancet Public Health. 2021;6(7):e500–9. https://doi.org/10.1016/S2468-2667(20)30307-8. This randomized controlled trial is one of the first to develop and test an intervention for dual users. The study presents results examining the efficacy of an 18-month self-help intervention in which e-cigarettes function as a nicotine replacement strategy.
Vickerman KA, Carpenter KM, Miles LN, Hsu JM, Watt KA, Brandon TH, et al. A randomized pilot of a tailored smoking cessation quitline intervention for individuals who smoke and vape. Nicotine Tob Res. 2022;XX:1–10. https://doi.org/10.1093/ntr/ntac129.
Brandon TH, Simmons VN, Sutton SK, Unrod M, Harrell PT, Meade CD, et al. Extended self-help for smoking cessation: a randomized controlled trial. Am J Prev Med. 2016;51(1):54–62.
Meltzer LR, Simmons VN, Sutton SK, Drobes DJ, Quinn GP, Meade CD, et al. A randomized controlled trial of a smoking cessation self-help intervention for dual users of tobacco cigarettes and e-cigarettes: intervention development and research design. Contemp Clin Trials. 2017;60:56–62. https://doi.org/10.1016/j.cct.2017.06.014.
Meltzer LR, Simmons VN, Piñeiro B, Drobes DJ, Quinn GP, Meade CD, et al. Development of a self-help smoking cessation intervention for dual users of tobacco cigarettes and e-cigarettes. Int J Environ Res Public Health. 2021;18(5):2328.
Hajek P, Peerbux S, Phillips-Waller A, Smith C, Pittaccio K, Przulj D. Are ‘dual users’ who smoke and use e-cigarettes interested in using varenicline to stop smoking altogether, and can they benefit from it? A cohort study of UK vapers. BMJ Open. 2019;9(3): e026642.
Çetinkaya PD, Turan A, Deniz PP. Effectiveness of behavioral and pharmacological smoking cessation treatment in patients with failed attempt at quitting with e-cigarettes. Turk Thorac J. 2020;21(6):404.
Rosen RL, Steinberg ML. Interest in quitting e-cigarettes among adults in the United States. Nicotine Tob Res. 2020;22(5):857–8.
Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) study, Waves 1 and 2 (2013–2015). Tob Control. 2019;28(1):50–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Section Editors for the topical collection Tobacco are Grace Kong and Krysten Bold. Please note that Dr. Bold was not involved in the editorial process of this article as she is a co-author.
Conflict of Interest
Research reported in this publication was supported by National Institute on Drug Abuse (NIDA) and Food and Drug Administration (FDA) Tobacco Centers of Regulatory Science (TCORS) Award U54DA036114 (SRMC) U54DA036151 (KWB), National Cancer Institute (NCI) R01CA239309 (MEP), NCI and FDA Center for Tobacco Products (CTP) grant number K01CA253234-01 (MJB), and NIDA K12DA000167 (KWB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA. The authors have no conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tobacco
The original online version of this article was revised: There was a missing text in the Ethics Declarations section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coleman, S.R.M., Piper, M.E., Byron, M.J. et al. Dual Use of Combustible Cigarettes and E-cigarettes: a Narrative Review of Current Evidence. Curr Addict Rep 9, 353–362 (2022). https://doi.org/10.1007/s40429-022-00448-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-022-00448-1