Abstract
Purpose of Review
Global policy changes have increased access to products containing cannabidiol (CBD), a primary constituent of hemp and cannabis. The CBD product industry has experienced tremendous growth, in part, because CBD is widely touted as an effective therapeutic for myriad health conditions. However, only 1 CBD product (Epidiolex®) has been approved by the US Food and Drug Administration (FDA) to date. There is substantial interest among consumers and the medical and scientific communities regarding the therapeutic potential of CBD, including for indications that are not recognized by the FDA. The purpose of this review was to synthesize available evidence from clinical research regarding the efficacy of CBD as a therapeutic.
Recent Findings
Human laboratory studies and clinical trials (e.g., randomized controlled trials and single-arm, open-label trials) evaluating the efficacy of CBD as a therapeutic were identified for various medical conditions, including epilepsy, anxiety, pain/inflammation, schizophrenia, various substance use disorders, post-traumatic stress disorder, and others. There is clear evidence supporting the utility of CBD to treat epilepsy. For other health conditions reviewed, evidence was often mixed and/or there was a general lack of well-powered randomized, placebo-controlled studies to draw definitive conclusions.
Summary
Rigorous, controlled evidence for the therapeutic efficacy of CBD is lacking for many health conditions. Possible concerns with the use of CBD as a therapeutic include the potential for adverse effects (e.g., liver toxicity), drug-drug interactions, and lack of sufficient regulatory oversight of retail CBD products.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent global policy changes have increased access to medical cannabis or cannabinoid-based pharmacotherapeutics in over 50 countries. In the United States (USA) for example, medical cannabis use is legal in 33 states and the District of Columbia (D.C.), and non-medical use (i.e., “recreational”) is legal in 11 states. In addition to cannabis, the legalization of hemp (defined in the USA as cannabis with ≤ 0.3% of the psychoactive cannabis constituent Δ-9-tetrahydrocannabinol, THC) has expanded in many countries. Indeed, with the approval of the US Agriculture Improvement Act of 2018 (i.e., the “Farm Bill”), hemp and its derivative products are no longer considered controlled substances by the US Drug Enforcement Administration. These legislative changes have led to the emergence of a large and growing, retail market of cannabinoid-based products.
Cannabidiol (CBD) is a chief constituent of many cannabis and hemp plants. Hemp-derived CBD products have become ubiquitous because they are no longer considered controlled substances, meaning they are widely available in jurisdictions in which cannabis remains illegal. CBD products vary widely in regard to their formulation and intended route of administration. Oral CBD products make up the majority of the market, and these products may consist of CBD extracts suspended in a solution (e.g., tinctures), food products (e.g., chocolates, gummies), or beverages (e.g., sodas, teas). Beyond oral products, CBD products intended for inhalation (e.g., vape pens, CBD-dominant hemp or cannabis plant material), topical application (e.g., lotions, gels, balms), and other routes of administration (e.g., sublingual) abound; there are also burgeoning markets for other CBD products such as cosmetics, haircare products, and pet treats. The collective market for cannabis/hemp-based CBD products (including retail, dispensary, and pharmaceutical sales) is expected to exceed $20 billion in the USA by 2024 (BDS Analytics).
The CBD product industry has experienced this tremendous growth because CBD is widely touted as an effective therapeutic for myriad health conditions. In many US states, individuals can obtain a medical CBD license for well over a dozen indications, though to date, only 1 CBD product (Epidiolex®, GW Pharmaceuticals) is approved by the US Food and Drug Administration (FDA); this product is approved for the treatment of rare pediatric seizure disorders. Moreover, it is not uncommon for commercial CBD products to be marketed with specific health claims that are not recognized by the FDA. In the USA, this problem came to a head in 2019 when the FDA sent warning letters to 15 companies for making unsubstantiated therapeutic claims about CBD in violation of the US Federal Food, Drug, and Cosmetic Act. An additional concern with commercial CBD products is that they are often mislabeled with respect to their cannabinoid content (e.g., concentrations of THC and CBD) [1•, 2, 3].
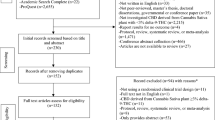
Despite the regulatory concerns with CBD products, there is substantial interest among consumers, as well as the medical and scientific communities, regarding the therapeutic potential of CBD, including the indications not yet approved by the FDA. The goal of this review was to synthesize available clinical evidence from human laboratory studies and clinical trials (e.g., randomized controlled trials and single-arm, open-label trials) regarding the efficacy of CBD as a therapeutic for various health conditions. We focus on studies which entailed administration of CBD alone and thus do not include studies featuring co-administration of CBD and THC (e.g., trials involving nabiximols/sativex). Additional important considerations concerning the use of CBD as a therapeutic including potential adverse effects, drug-drug interactions, and current lack of sufficient regulatory oversight of CBD products are discussed.
Seizure/Epilepsy
In 2018, Epidiolex® (an oral solution containing CBD as the principal constituent) became the first prescription, plant-derived cannabinoid therapeutic approved by the US FDA. Epidiolex® was approved for the treatment of seizures associated with Lennox-Gastaut and Dravet syndromes in patients ≥ 2 years of age. In the European Union, Epidiolex® is approved as an adjuvant to clobazam for the same indications. Several clinical trials were instrumental in the approval of Epidiolex® for these indications (for a systematic review, see [4]).
In a 12-week open-label trial, oral CBD (2–5 mg/kg/day, increased to maximum dose of 25–50 mg/kg/day) reduced monthly motor seizures by 36.5% (median) among patients (ages 1–30 years) with severe, intractable, childhood-onset, treatment-resistant epilepsy [5•]. In subsequent double-blind, placebo-controlled trials, daily CBD treatment (10–20 mg/kg) over 14 weeks significantly reduced the frequency of convulsive seizures associated with Dravet and Lennox-Gastaut syndromes. Moreover, patients’ overall condition (assessed using the Caregiver Global Impression of Change scale) improved relative to placebo [6, 7].
GW Pharmaceuticals recently submitted a supplemental New Drug Application to the FDA to evaluate Epidiolex® for the treatment of seizures associated with tuberous sclerosis complex (TSC) in patients ages 1–65 years [8]. This was informed by a clinical trial which demonstrated that CBD treatment over 3 months (5 mg/kg/day; increased daily to a maximum dose of 50 mg/kg/day) significantly reduced weekly seizures relative to baseline (pretreatment) in a sample of patients (ages 2–31 years) diagnosed with both TSC and drug-resistant epilepsy [9]. Overall, there is high-quality evidence from clinical trials supporting CBD as an effective treatment to mitigate seizures associated with various disorders.
Anxiety
Many individuals report using CBD to alleviate anxiety. In a recent survey of young adults, 65% of respondents who were current CBD users cited stress/anxiety relief as a primary reason for use [10]. CBD’s anxiolytic properties have been examined in experimental settings using paradigms such as the simulated public speaking (SPS) task, which reliably increases self-reported anxiety levels in humans [11]. In studies with healthy volunteers (i.e., without clinical anxiety), oral administration of CBD prior to the SPS has decreased self-reported ratings of anxiety relative to placebo. For example, 300 mg oral CBD decreased post-stress anxiety ratings (i.e., those after the speech) relative to placebo [12]. In a similar study with multiple CBD doses, CBD exhibited an inverted U-shaped dose-response curve. That is, the middle dose (300 mg) reduced self-reported anxiety during the speech relative to placebo but the low (150 mg) and high doses (600 mg) did not [13]. In another study, healthy adults were given oral CBD (100, 300, or 900 mg) before completing a slightly different public speaking task (the test of public speaking in a real situation, TPSRS), and subjective anxiety and physiological indices of anxiety (i.e., heart rate or blood pressure) were evaluated. The same U-shaped dose-response curve was observed for post-speech subjective ratings of anxiety, but CBD did not have any appreciable effects on physiological indices of anxiety at any dose evaluated [14].
Some studies have examined the anxiolytic effects of CBD in populations with clinical anxiety. Bergamaschi and colleagues (2011) recruited patients with social anxiety disorder (SAD) to evaluate the efficacy of CBD (600 mg, oral) to decrease self-rated anxiety in the SPS test. Healthy controls were also recruited and used as a comparator to SAD patients, but did not receive CBD treatment. CBD significantly reduced anxiety (relative to placebo) during speech performance in SAD patients to a level that was similar to that of healthy controls, though anxiety during other time points (e.g., anticipatory phase, post-speech phase) did not differ from placebo [15•]. Orally administered CBD also reduced self-reported anxiety in patients with generalized anxiety disorder (N = 10, all males) before and after a neuroimaging procedure relative to when these individuals underwent the same procedure on a different day, but received placebo [16].
Several studies failed to demonstrate an anxiolytic effect of CBD following acute administration [17,18,19]. For example, healthy volunteers (preselected for paranoid traits) were immersed in a virtual reality session that increased salivary cortisol concentrations and elicited self-reported anxiety (measured by the Beck Anxiety Inventory, BAI). However, pretreatment with 600 mg oral CBD did not reverse these effects [20]. In another study, healthy volunteers ingested CBD (300, 600, or 900 mg) or placebo prior to being exposed to various visual stimuli, both positive and negative. CBD did not affect responses to negative emotional stimuli nor did it alter self-reported mood or anxiety [17].
Overall, evidence regarding the therapeutic efficacy of CBD to treat anxiety is mixed, with some studies showing that CBD acutely reduces self-reported anxiety levels during a stressful task and others failing to show differences between CBD and placebo on acute anxiety responses. CBD appears to have little influence on physiological responses to stress (e.g., cortisol, heart rate), though few studies have incorporated such outcomes and many have relied solely on subjective measures of anxiety. Most human laboratory studies in this area have included healthy adults and evaluated the anxiolytic effects of CBD following an acute stressor (e.g., public speaking task). To date, there are no completed randomized clinical trials that have evaluated a repeated CBD treatment regimen in patients with clinical anxiety disorders. The influence of route of administration on the efficacy of CBD as an anxiolytic is largely unelucidated, as almost all studies have administered CBD orally.
Pain and Inflammation
Though individuals commonly report using CBD products to treat pain/reduce inflammation [21•], few clinical studies have evaluated the efficacy of CBD alone for these indications. Indeed, almost all studies conducted in this area have co-administered CBD with THC. One randomized, placebo-controlled trial tested the efficacy of a transdermal CBD gel (ZYN002, 250 or 500 mg/day for 12 weeks) to treat knee pain associated with osteoarthritis. Patients receiving 250 mg/day ZYN002 exhibited qualitative reductions in knee pain scores, though these reductions did not differ significantly from those observed from placebo. A secondary analysis showed that treatment responders (defined as those with weekly improvement in worst pain score of > 30% and decrease in Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale of > 20%) who received CBD showed greater pain reductions compared with treatment responders who received placebo [22]. In another double-blind, randomized crossover trial of 24 patients with a neurological diagnosis, sublingual CBD (2.5–120 mg/day for 2 weeks, titrated against symptom relief/adverse effects) improved spasticity severity on a numerical symptom scale relative to placebo [23].
Daily CBD dosing regimens have reduced pain in clinical populations in several small, single-arm open-label studies. In an open-label study of kidney transplant patients who requested CBD to treat their chronic pain, CBD (50 mg increased to 150 mg, twice daily) qualitatively reduced self-reported pain (either partially or completely) in 6/7 patients after 3 weeks; of note, the cause of chronic pain varied across these individuals (e.g., fibromyalgia, osteoarticular, neuropathic) [24]. In a second open-label study of 12 female participants with severe somatoform and dysautonomic syndrome following HPV vaccination, administration of sublingual CBD-rich hemp oil (titrated up to 150 mg/mL CBD per day over 3 months) improved physical component scores, vitality, and social role functioning on the short-form health survey questionnaire [25]. Without a proper control condition (i.e., placebo), it is difficult to determine the role that expectancy effects contributed to the observed reductions in pain in these open-label trials.
Controlled clinical research on CBD alone as a treatment for pain/inflammation is in its infancy, and it is thus difficult to make firm conclusions regarding CBD’s efficacy for such health conditions. Well-powered randomized, placebo-controlled clinical trials (with a range of doses) are needed in this area. Laboratory studies should also consider systematically exploring the acute analgesic effects of CBD using standardized measures (e.g., quantitative sensory testing, QST). Study populations of the highest interest for these research areas would likely include elderly individuals [26], as this group commonly uses CBD as a primary or adjunctive treatment for pain, as well as clinical pain populations.
Schizophrenia
Several studies have evaluated the efficacy of CBD to produce clinical improvements in patients with schizophrenia. In a 6-week, randomized placebo-controlled trial with antipsychotic-treated patients with schizophrenia, CBD treatment (600 mg/day) was not associated with improvement on cognitive performance or psychotic symptoms (Positive and Negative Syndrome Scale; PANSS) compared with placebo [27]. Other studies suggest that CBD treatment improves schizophrenia symptomatology. In a double-blind study of patients diagnosed with schizophrenia or schizophreniform psychosis, patients received either amisulpride or CBD over 4 weeks (doses began at 200 mg/day and were increased stepwise to 800 mg/day). Both CBD and amisulpride reduced total PANSS score and all subcategories of schizophrenia symptoms, consistent with significant clinical improvement. However, CBD displayed a more favorable side effect profile than amisulpride, including fewer extrapyramidal symptoms, less weight gain, and lower prolactin increases [28]. Another study found that, relative to placebo, 1000 mg/day oral CBD solution (administered for 6 weeks in conjunction with treatment as usual) decreased positive psychotic symptoms in patients with schizophrenia [29]. Overall, studies evaluating the efficacy of CBD to improve schizophrenia-related symptoms are mixed, and large, placebo-controlled trials are needed.
Substance Use Disorders and Withdrawal
Opioids
In a double-blind, placebo-controlled study, abstinent heroin users administered Epidiolex® (400 or 800 mg CBD) or placebo once daily for three consecutive days. Relative to placebo, CBD (400 and 800 mg) reduced cue-induced heroin craving and self-reported anxiety measures. Further, CBD reduced drug cue–induced physiological measures (i.e., heart rate and salivary cortisol). CBD also exhibited significant protracted effects on craving (800 mg) and anxiety (400 and 800 mg), 7 days after the drug was last administered [30, 31].
Nicotine
In a double-blind, placebo-controlled study, cigarette smokers used a CBD-containing inhaler (400 μg/inhaler) or an inhaler containing placebo aerosol for 7 days; they were instructed to use the inhaler if they felt an urge to smoke. CBD treatment did not alter cigarette craving relative to placebo. However, CBD significantly reduced the self-reported number of cigarettes on day 7 relative to day 1, although this effect did not appear to be maintained at a follow-up visit, 2 weeks after CBD administration [32].
In a double-blind crossover study, 30 non-treatment-seeking cigarette smokers were given placebo or an 800 mg oral CBD capsule during nicotine/tobacco abstinence. Attentional bias to cigarette-linked cues was increased during nicotine/tobacco abstinence, and this effect was reversed by CBD administration. CBD also reduced pleasantness of cigarette images relative to placebo and decreased systolic blood pressure during abstinence. However, craving and withdrawal questionnaire scores were unaffected by CBD treatment. Thus, studies supporting the efficacy of CBD to improve tobacco withdrawal and use disorder are mixed, and future studies are warranted [33].
Cannabis
In an open-label study of cannabis users (N = 8) admitted to an inpatient detoxification facility, participants received CBD (600 or 1200 mg) for 7 days and returned for a 28-day follow-up interview. Cannabis abstinence was maintained by 4/8 participants at follow-up (3 participants did not complete the full treatment period) [34]. In another open-label trial, 20 frequent cannabis users (defined as at least monthly use for 6 months) received CBD capsules (200 mg/day) while continuing to use cannabis as usual. Following CBD treatment, participants retrospectively reported decreased euphoria when using cannabis (Cannabis Experience Questionnaire), but cannabis use frequency and quantity did not change from baseline [35]. In a study of non-treatment-seeking healthy cannabis smokers, acute pretreatment with oral CBD (200, 400, or 800 mg) did not alter cannabis self-administration, cannabis-induced subjective drug effects including reinforcing effects (e.g., “high,” “good effect”), or cardiovascular effects relative to placebo [36•].
Overall, studies evaluating CBD for substance use disorders and withdrawal are limited, and data within drug classes are mixed, highlighting that continued research is needed.
Other Medical Conditions
Parkinson’s and Huntington’s Diseases
To our knowledge, there are two published clinical trials evaluating CBD in Parkinson’s disease patients. In one double-blind study of patients with Parkinson’s disease, 6 weeks of oral CBD (300 mg/day) improved self-reported functioning/well-being but did not alter clinically observed disease symptoms (assessed via the Unified Parkinson’s Disease Rating Scale, UPDRS) relative to placebo [37]. In an open-label trial, 13 Parkinson’s patients received CBD (Epidiolex®) titrated from 5 to 20 to 25 mg/kg/day, for 10–15 days. The ten participants who completed the study experienced improvements in total and motor UPDRS scores and self-reported emotional/behavioral dyscontrol scores [38]. Taken together, these two trials do not discount the efficacy of CBD to improve quality of life in Parkinson’s disease patients. However, it is difficult to draw firm conclusions on the efficacy of CBD to treat Parkinson’s disease from just two clinical trials, one of which was open-label.
One double-blind randomized controlled trial evaluated CBD’s effects on patients with Huntington’s disease. Patients received 10 mg/kg/day oral CBD (i.e., roughly 700 mg/day) or placebo (sesame oil) for 6 weeks. No clinically significant improvements were observed on Huntington’s disease-related symptoms (e.g., chorea sensitivity, sustained tongue protrusion, functional ability, or information recall and storage) compared with placebo [39].
Post-traumatic Stress Disorder
In one small, open-label trial, individuals (N = 11) with PTSD were given CBD capsules (22–28 mg) or a CBD spray (1.5 mg CBD/dose) for 8 weeks (the CBD formulation, dose, and dosing schedule were determined by provider and patient preference). Ten of the 11 participants displayed reduced PTSD symptoms (on the PTSD Checklist for the DSM-5, PCL-5) at 8 weeks relative to baseline [40]. The basis for CBD as a potentially effective treatment for PTSD comes predominantly from preclinical research as well as the limited clinical evidence that CBD may improve certain symptoms associated with PTSD such as anxiety and sleep (for review, see [41]). Published randomized controlled trials and human laboratory studies evaluating the efficacy of CBD to treat PTSD are lacking.
Sleep
The efficacy of CBD as a hypnotic was examined in one study with healthy individuals who reported difficulty falling or staying asleep. Participants received oral placebo or CBD capsules (40, 80, or 160 mg); those receiving 160 mg CBD had a longer duration of sleep, while all CBD doses decreased remembrance of dreams relative to placebo [42]. Despite these early findings and data from two case reports in which CBD improved sleep quality in a single pediatric patient with PTSD and four patients with Parkinson’s disease [43, 44], we identified only one randomized, double-blind, placebo-controlled study with sleep as the primary outcome measure. In this trial, 27 healthy volunteers received either oral CBD (300 mg dissolved in corn oil) or placebo. CBD did not alter any sleep measures (e.g., self-rated sleep quality or polysomnography examinations) relative to placebo. Additional controlled trials are needed to elucidate the efficacy of CBD as a sleep aid given that findings in this area appear to be mixed.
Chron’s Disease
The efficacy of CBD as a treatment for Chron’s disease was evaluated in patients with this condition. Participants received placebo or oral CBD (10 mg, twice daily) for 8 weeks; CBD treatment did not alter Chron’s disease symptoms compared with placebo, as assessed via the Chron’s disease activity index (CDAI) [45].
Type 2 Diabetes
Oral CBD (100 mg, twice daily for 16 weeks) or placebo was administered to 62 patients with type 2 diabetes (noninsulin treated). HDL-cholesterol concentrations (primary trial endpoint) did not differ following CBD treatment relative to baseline [46].
Intraocular Pressure
Sublingual CBD (20 or 40 mg CBD) or placebo was given to patients with ocular hypertension or early primary open angle glaucoma in a small trial (N = 6). The 40-mg CBD dose–elevated intraocular pressure relative to placebo and CBD had no impact on visual acuity, vital signs, and psychotropisms [47].
Concluding Remarks: Additional Considerations for CBD as a Therapeutic and Future Research Directions
In this review, we highlighted findings from human laboratory studies and clinical trials supporting or refuting CBD as a potential therapeutic for various indications. Overall, there is ample evidence to conclude that CBD is an efficacious treatment to alleviate seizures such as those associated with Lennox-Gastaut and Dravet syndromes (for a systematic review, see [4]). As such, the CBD therapeutic Epidiolex® is approved to treat these indications in the USA and European Union.
However, the efficacy of CBD as a sole treatment for most of the other indications discussed in this review remains unclear due to various reasons. There have generally been few randomized, placebo-controlled clinical trials to evaluate the therapeutic efficacy of CBD for most indications discussed, and, in many instances, the data available from clinical trials or human laboratory studies were mixed with regard to the effectiveness of CBD versus placebo. Moreover, for many health conditions, a large percentage of available data came from open-label trials (these must be interpreted cautiously due to the absence of placebo control and potential for expectancy effects associated with CBD treatment). Further complicating matters, within many health conditions, CBD doses, formulations, dosing regimens, study populations, outcome measures, and methodologies varied considerably across studies. These differences make it difficult to conduct comparisons across studies and to draw firm conclusions on the therapeutic efficacy of CBD for a given condition. Thus, an important step needed to fully elucidate the therapeutic efficacy of CBD for many health conditions is determining how factors such as individual features of CBD products (e.g., doses, route of administration, dosing schedule), characteristics of participant populations, and research design influence study outcomes and contribute to variability across or within studies.
Beyond developing a more detailed understanding of the efficacy of CBD as a therapeutic treatment option, future research should continue to evaluate the safety of CBD. Several comprehensive reviews have concluded that CBD has low toxicity, no psychotomimetic effects, and very low abuse liability and is well tolerated by adults [15•, 48]. Moreover, CBD appears to have little influence on vital signs (e.g., heart rate, blood pressure) and does not produce respiratory depression, which further suggests it has a favorable safety profile. Adverse events were often a secondary endpoint in the clinical trials and laboratory studies reviewed in this manuscript. For example, the incidence of adverse events in patients with Dravet syndrome treated with CBD included somnolence (36%), diarrhea (31%), fatigue (20%), vomiting (15%), pyrexia (15%), and lethargy (13%) [6]; somnolence and diarrhea were observed in other studies where CBD was administered daily for several weeks or months [9, 38]. The incidence of severe adverse events resulting from CBD administration appears low based on review of these studies.
Despite this evidence pointing to the favorable safety profile of CBD, there are several noteworthy concerns associated with the use of CBD. First, as reviewed elsewhere (see [49]), daily CBD administration over a period of 12 weeks or greater has resulted in elevated liver function tests among participants in some trials. For example, GW Pharmaceuticals reported that 17% of epilepsy patients using 20 mg/kg/day CBD (Epidiolex®) exhibited over 3 times the upper limit of normal alanine transaminase elevations. At this same CBD dose, in epilepsy patients who were also using valproate and clobazam, 30% of these patients exhibited over 3 times the upper limit of normal alanine transaminase elevations [50]. The impact of CBD alone, and in combination with other medications, on liver function needs continued monitoring. A second concern with CBD surrounds the potential for drug-drug interactions (for reviews, see [51,52,53]). Specifically, CBD may inhibit metabolic activity for several cytochrome (CYP) P450 enzymes which are instrumental in the metabolism of many common prescription and OTC drugs. More specifically, administration of CBD in combination with drugs metabolized by certain CYP enzymes (e.g., CYP2C9, CYP2D6) may lead to delayed metabolism of these drugs. Recent case reports and small trials illustrate such drug-drug interactions [54, 55]. For example, a study of children with refractory epilepsy found that administration of Epidiolex® (5–25 mg/kg/day) in combination with clobazam (anti-seizure medication) elicited ~ 500% increase in plasma concentrations of the active metabolite of clobazam (norclobazam) [55]. Continued research is needed in this area, especially within disease states in which patients use concomitant medications (e.g., Parkinson’s disease, pain/inflammation, etc.) to determine the safety of CBD as a treatment option.
In sum, rigorous, controlled evidence for the therapeutic efficacy of CBD is lacking for many health conditions. Despite this, retail CBD products are often marketed for general health and wellness and/or make unsubstantiated claims about treating a disease condition (for review, see [56]). Given the widespread availability of CBD-containing products (e.g., vaporization liquids, oral capsules and solutions, topical skin products), consumer education and public health messaging are critical. Such educational efforts should accurately convey the state of CBD research as well as possible concerns associated with CBD use (e.g., potential for drug-drug interactions). Consumers should also be made aware that retail products are poorly regulated and thus may lack accurate labeling with respect to cannabinoid concentrations or may include constituents (e.g., THC, synthetic cannabinoids) that are not listed on the label [1, 3]. Further, it is possible that consumers mistakenly assume that evidence from controlled research with pharmaceutical-grade cannabinoid therapeutics (e.g., Epidiolex®) apply to all retail CBD products. As research continues to progress, it is important that consumers are able to disentangle which products are likely to have a therapeutic effect and which are not. To date, the consumer CBD market has far outpaced science, and well-designed, appropriately controlled, clinical trials and human laboratory studies are needed to definitively support or refute CBD’s therapeutic utility for many disease states.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Bonn-Miller MO, Loflin MJE, Thomas BF, Marcu JP, Hyke T, Vandrey R. Labeling accuracy of cannabidiol extracts sold online. Jama. 2017;318(17):1708–9. https://doi.org/10.1001/jama.2017.11909This study analyzed commercially-available CBD extracts. 69% were labeled inaccurately (43% underlabeled, 26% overlabeled for CBD concentrations) and 21% contained THC (up to 6.4 mg/mL).
Gurley BJ, Murphy TP, Gul W, Walker LA, ElSohly M. Content versus label claims in cannabidiol (CBD)-containing products obtained from commercial outlets in the state of Mississippi. J Diet Suppl. 2020:1–9. https://doi.org/10.1080/19390211.2020.1766634.
Poklis JL, Mulder HA, Peace MR. The unexpected identification of the cannabimimetic, 5F-ADB, and dextromethorphan in commercially available cannabidiol e-liquids. Forensic Sci Int. 2019;294:e25–e7. https://doi.org/10.1016/j.forsciint.2018.10.019.
Stockings E, Zagic D, Campbell G, Weier M, Hall WD, Nielsen S, et al. Evidence for cannabis and cannabinoids for epilepsy: a systematic review of controlled and observational evidence. J Neurol Neurosurg Psychiatry. 2018;89(7):741–53. https://doi.org/10.1136/jnnp-2017-317,168.
• Devinsky O, Marsh E, Friedman D, Thiele E, Laux L, Sullivan J, et al. Cannabidiol in patients with treatment-resistant epilepsy: an open-label interventional trial. Lancet Neurol. 2016;15(3):270–8. https://doi.org/10.1016/s1474-4422(15)00379-8In a 12-week open-label trial, oral CBD (2-5 mg/kg/day, increased to maximum dose of 25-50 mg/kg/day) reduced monthly motor seizures by 36.5% (median) among patients (ages 1-30 years) with severe, intractable, childhood-onset, treatment-resistant epilepsy. This study supported the FDA approval of CBD (i.e., Epidiolex®) to treat seizures associated with Lennox-Gastaut and Dravet syndromes.
Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. 2017;376(21):2011–20. https://doi.org/10.1056/NEJMoa1611618.
Devinsky O, Patel AD, Cross JH, Villanueva V, Wirrell EC, Privitera M, et al. Effect of cannabidiol on drop seizures in the Lennox-Gastaut syndrome. N Engl J Med. 2018;378(20):1888–97. https://doi.org/10.1056/NEJMoa1714631.
GW Pharmaceuticals and Greenwich Biosciences Announce FDA Acceptance of sNDA Filing with Priority Review for EPIDIOLEX® (cannabidiol) in the Treatment of Seizures Associated with Tuberous Sclerosis Complex. http://ir.gwpharm.com/node/11346/pdf: GW Pharmaceuticals; 2020. p. 1–2.
Hess EJ, Moody KA, Geffrey AL, Pollack SF, Skirvin LA, Bruno PL, et al. Cannabidiol as a new treatment for drug-resistant epilepsy in tuberous sclerosis complex. Epilepsia. 2016;57(10):1617–24. https://doi.org/10.1111/epi.13499.
Wheeler M, Merten JW, Gordon BT, Hamadi H. CBD (cannabidiol) product attitudes, knowledge, and use among young adults. Subst Use Misuse. 2020;55(7):1138–45. https://doi.org/10.1080/10826084.2020.1729201.
Graeff FG, Parente A, Del-Ben CM, Guimarães FS. Pharmacology of human experimental anxiety. Braz J Med Biol Res. 2003;36(4):421–32. https://doi.org/10.1590/s0100-879x2003000400003.
Zuardi AW, Cosme RA, Graeff FG, Guimaraes FS. Effects of ipsapirone and cannabidiol on human experimental anxiety. J Psychopharmacol. 1993;7(1 Suppl):82–8. https://doi.org/10.1177/026988119300700112.
Linares IM, Zuardi AW, Pereira LC, Queiroz RH, Mechoulam R, Guimaraes FS, et al. Cannabidiol presents an inverted U-shaped dose-response curve in a simulated public speaking test. Braz J Psychiatry. 2019;41(1):9–14. https://doi.org/10.1590/1516-4446-2017-0015.
Zuardi AW, Rodrigues NP, Silva AL, Bernardo SA, Hallak JEC, Guimarães FS, et al. Inverted U-shaped dose-response curve of the anxiolytic effect of cannabidiol during public speaking in real life. Front Pharmacol. 2017;8:259. https://doi.org/10.3389/fphar.2017.00259.
• Bergamaschi MM, Queiroz RH, Chagas MH, de Oliveira DC, De Martinis BS, Kapczinski F, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology. 2011;36(6):1219–26. https://doi.org/10.1038/npp.2011.6The efficacy of CBD (600 mg) to reduce anxiety in a simulated public speaking test was evaluated in patients with generalized social anxiety disorder. Pretreatment with CBD decreased anxiety, cognitive impairment, and discomfort in speech performance relative to placebo.
Crippa JA, Derenusson GN, Ferrari TB, Wichert-Ana L, Duran FL, Martin-Santos R, et al. Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: a preliminary report. J Psychopharmacol. 2011;25(1):121–30. https://doi.org/10.1177/0269881110379283.
Arndt DL, de Wit H. Cannabidiol does not dampen responses to emotional stimuli in healthy adults. Cannabis Cannabinoid Res. 2017;2(1):105–13. https://doi.org/10.1089/can.2017.0014.
Das RK, Kamboj SK, Ramadas M, Yogan K, Gupta V, Redman E, et al. Cannabidiol enhances consolidation of explicit fear extinction in humans. Psychopharmacology. 2013;226(4):781–92. https://doi.org/10.1007/s00213-012-2955-y.
Hindocha C, Freeman TP, Schafer G, Gardener C, Das RK, Morgan CJ, et al. Acute effects of delta-9-tetrahydrocannabinol, cannabidiol and their combination on facial emotion recognition: a randomised, double-blind, placebo-controlled study in cannabis users. Eur Neuropsychopharmacol. 2015;25(3):325–34. https://doi.org/10.1016/j.euroneuro.2014.11.014.
Hundal H, Lister R, Evans N, Antley A, Englund A, Murray RM, et al. The effects of cannabidiol on persecutory ideation and anxiety in a high trait paranoid group. J Psychopharmacol. 2018;32(3):276–82. https://doi.org/10.1177/0269881117737400.
• Corroon J, Phillips JA. A cross-sectional study of cannabidiol users. Cannabis Cannabinoid Res. 2018;3(1):152–61. https://doi.org/10.1089/can.2018.0006A self-selected convenience sample was recruited via an online survey designed to characterize whom, how, and why individuals are currently using CBD. Roughly 62% of respondents reported using CBD to treat a medical condition. The top three medical conditions were chronic pain, arthritis/joint pain, and anxiety.
Hunter D, Oldfield G, Tich N, Messenheimer J, Sebree T. Synthetic transdermal cannabidiol for the treatment of knee pain due to osteoarthritis. Osteoarthr Cartil. 2018;26:S26. https://doi.org/10.1016/j.joca.2018.02.067.
Wade DT, Robson P, House H, Makela P, Aram J. A preliminary controlled study to determine whether whole-plant cannabis extracts can improve intractable neurogenic symptoms. Clin Rehabil. 2003;17(1):21–9. https://doi.org/10.1191/0269215503cr581oa.
Cuñetti L, Manzo L, Peyraube R, Arnaiz J, Curi L, Orihuela S. Chronic pain treatment with cannabidiol in kidney transplant patients in Uruguay. Transplant Proc. 2018;50(2):461–4. https://doi.org/10.1016/j.transproceed.2017.12.042.
Palmieri B, Laurino C, Vadalà M. Short-term efficacy of CBD-enriched hemp oil in girls with dysautonomic syndrome after human papillomavirus vaccination. Isr Med Assoc J. 2017;19(2):79–84.
Brown JD, Costales B, van Boemmel-Wegmann S, Goodin AJ, Segal R, Winterstein AG. Characteristics of older adults who were early adopters of medical cannabis in the Florida Medical Marijuana Use Registry. J Clin Med. 2020;9(4). https://doi.org/10.3390/jcm9041166.
Boggs DL, Surti T, Gupta A, Gupta S, Niciu M, Pittman B, et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology. 2018;235(7):1923–32. https://doi.org/10.1007/s00213-018-4885-9.
Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94. https://doi.org/10.1038/tp.2012.15.
McGuire P, Robson P, Cubala WJ, Vasile D, Morrison PD, Barron R, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am J Psychiatry. 2018;175(3):225–31. https://doi.org/10.1176/appi.ajp.2017.17030325.
Hurd YL, Spriggs S, Alishayev J, Winkel G, Gurgov K, Kudrich C, et al. Cannabidiol for the reduction of cue-induced craving and anxiety in drug-abstinent individuals with heroin use disorder: a double-blind randomized placebo-controlled trial. Am J Psychiatry. 2019;176(11):911–22. https://doi.org/10.1176/appi.ajp.2019.18101191.
Hurd YL, Yoon M, Manini AF, Hernandez S, Olmedo R, Ostman M, et al. Early phase in the development of cannabidiol as a treatment for addiction: opioid relapse takes initial center stage. Neurotherapeutics. 2015;12(4):807–15. https://doi.org/10.1007/s13311-015-0373-7.
Morgan CJ, Das RK, Joye A, Curran HV, Kamboj SK. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict Behav. 2013;38(9):2433–6. https://doi.org/10.1016/j.addbeh.2013.03.011.
Hindocha C, Freeman TP, Grabski M, Stroud JB, Crudgington H, Davies AC, et al. Cannabidiol reverses attentional bias to cigarette cues in a human experimental model of tobacco withdrawal. Addiction. 2018. https://doi.org/10.1111/add.14243.
Pokorski I, Clement N, Phung N, Weltman M, Fu S, Copeland J. Cannabidiol in the management of in-patient cannabis withdrawal: clinical case series. Future Neurol. 2017;12(3):133–40. https://doi.org/10.2217/fnl-2016-0035.
Solowij N, Broyd SJ, Beale C, Prick JA, Greenwood LM, van Hell H, et al. Therapeutic effects of prolonged cannabidiol treatment on psychological symptoms and cognitive function in regular cannabis users: a pragmatic open-label clinical trial. Cannabis Cannabinoid Res. 2018;3(1):21–34. https://doi.org/10.1089/can.2017.0043.
• Haney M, Malcolm RJ, Babalonis S, Nuzzo PA, Cooper ZD, Bedi G, et al. Oral cannabidiol does not alter the subjective, reinforcing or cardiovascular effects of smoked cannabis. Neuropsychopharmacology. 2016;41(8):1974–82. https://doi.org/10.1038/npp.2015.367Healthy adults received placebo or oral CBD (200, 400, or 800 mg) prior to administration of high-THC smoked cannabis. CBD pretreatment did not alter self-reported subjective drug effects including reinforcing effects or cardiovascular outcomes relative to placebo.
Chagas MH, Zuardi AW, Tumas V, Pena-Pereira MA, Sobreira ET, Bergamaschi MM, et al. Effects of cannabidiol in the treatment of patients with Parkinson’s disease: an exploratory double-blind trial. J Psychopharmacol. 2014;28(11):1088–98. https://doi.org/10.1177/0269881114550355.
Leehey MA, Liu Y, Hart F, Epstein C, Cook M, Sillau S, et al. Safety and tolerability of cannabidiol in Parkinson disease: an open label, dose-escalation study. Cannabis Cannabinoid Research. 2020. https://doi.org/10.1089/can.2019.0068.
Consroe P, Laguna J, Allender J, Snider S, Stern L, Sandyk R, et al. Controlled clinical trial of cannabidiol in Huntington’s disease. Pharmacol Biochem Behav. 1991;40(3):701–8. https://doi.org/10.1016/0091-3057(91)90386-g.
Elms L, Shannon S, Hughes S, Lewis N. Cannabidiol in the treatment of post-traumatic stress disorder: a case series. J Altern Complement Med. 2019;25(4):392–7. https://doi.org/10.1089/acm.2018.0437.
Loflin MJ, Babson KA, Bonn-Miller MO. Cannabinoids as therapeutic for PTSD. Curr Opin Psychol. 2017;14:78–83. https://doi.org/10.1016/j.copsyc.2016.12.001.
Carlini EA, Cunha JM. Hypnotic and antiepileptic effects of cannabidiol. J Clin Pharmacol. 1981;21(S1):417 s–27 s. https://doi.org/10.1002/j.1552-4604.1981.tb02622.x.
Shannon S, Opila-Lehman J. Effectiveness of cannabidiol oil for pediatric anxiety and insomnia as part of posttraumatic stress disorder: a case report. Perm J. 2016;20(4):16–005. https://doi.org/10.7812/tpp/16-005.
Chagas MH, Eckeli AL, Zuardi AW, Pena-Pereira MA, Sobreira-Neto MA, Sobreira ET, et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson’s disease patients: a case series. J Clin Pharm Ther. 2014;39(5):564–6. https://doi.org/10.1111/jcpt.12179.
Naftali T, Mechulam R, Marii A, Gabay G, Stein A, Bronshtain M, et al. Low-dose cannabidiol is safe but not effective in the treatment for Crohn’s disease, a randomized controlled trial. Dig Dis Sci. 2017;62(6):1615–20. https://doi.org/10.1007/s10620-017-4540-z.
Jadoon KA, Ratcliffe SH, Barrett DA, Thomas EL, Stott C, Bell JD, et al. Efficacy and safety of cannabidiol and tetrahydrocannabivarin on glycemic and lipid parameters in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel group pilot study. Diabetes Care. 2016;39(10):1777–86. https://doi.org/10.2337/dc16-0650.
Tomida I, Azuara-Blanco A, House H, Flint M, Pertwee RG, Robson PJ. Effect of sublingual application of cannabinoids on intraocular pressure: a pilot study. J Glaucoma. 2006;15(5):349–53. https://doi.org/10.1097/01.ijg.0000212260.04488.60.
Iffland K, Grotenhermen F. An update on safety and side effects of cannabidiol: a review of clinical data and relevant animal studies. Cannabis Cannabinoid Res. 2017;2(1):139–54. https://doi.org/10.1089/can.2016.0034.
White CM. A review of human studies assessing cannabidiol’s (CBD) therapeutic actions and potential. J Clin Pharmacol. 2019;59(7):923–34. https://doi.org/10.1002/jcph.1387.
Epidiolex (Cannabidiol) prescribing information. In: Greenwich Biosciences I, editor. Carlsbad, CA; 2018.
Stout SM, Cimino NM. Exogenous cannabinoids as substrates, inhibitors, and inducers of human drug metabolizing enzymes: a systematic review. Drug Metab Rev. 2014;46(1):86–95. https://doi.org/10.3109/03602532.2013.849268.
Brown JD, Winterstein AG. Potential adverse drug events and drug-drug interactions with medical and consumer cannabidiol (CBD) use. J Clin Med. 2019;8(7). https://doi.org/10.3390/jcm8070989.
Anderson GD, Chan LN. Pharmacokinetic drug interactions with tobacco, cannabinoids and smoking cessation products. Clin Pharmacokinet. 2016;55(11):1353–68. https://doi.org/10.1007/s40262-016-0400-9.
Madden K, Tanco K, Bruera E. Clinically significant drug-drug interaction between methadone and cannabidiol. Pediatrics. 2020;145(6). https://doi.org/10.1542/peds.2019-3256.
Geffrey AL, Pollack SF, Bruno PL, Thiele EA. Drug-drug interaction between clobazam and cannabidiol in children with refractory epilepsy. Epilepsia. 2015;56(8):1246–51. https://doi.org/10.1111/epi.13060.
Corroon J, Kight R. Regulatory status of cannabidiol in the United States: a perspective. Cannabis Cannabinoid Res. 2018;3(1):190–4. https://doi.org/10.1089/can.2018.0030.
Funding
This work was supported by the National Institute on Drug Abuse (NIDA) Training Grant T32DA07209.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cannabis
Rights and permissions
About this article
Cite this article
Sholler, D.J., Schoene, L. & Spindle, T.R. Therapeutic Efficacy of Cannabidiol (CBD): a Review of the Evidence From Clinical Trials and Human Laboratory Studies. Curr Addict Rep 7, 405–412 (2020). https://doi.org/10.1007/s40429-020-00326-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-020-00326-8