Abstract
Purpose of the Review
The purpose of this review is to describe current trends in e-cigarette use, provide an overview of the potential health risks and benefits, and discuss tobacco policy and regulatory considerations.
Recent Findings
E-cigarette use is popular among youth and adults, despite limited evidence about the long-term risks or benefits. Internationally, there is wide variability in how e-cigarettes are classified, which has also led to large differences in regulations on these products. Regulatory policies that strike a balance between the potential benefit of these devices for adult smokers who are trying to quit smoking with reducing the appeal and addictive potential for youth are critically needed.
Summary
Continued research on the health effects and consequences of e-cigarette use will be essential to inform e-cigarette product standards and tobacco regulatory policies as scientific research strives to keep pace with the ever-changing landscape of e-cigarette technology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
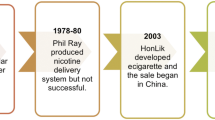
Electronic cigarettes (e-cigarettes) are battery-operated devices that are used to heat and inhale an aerosolized e-liquid solution that contains flavors, other chemical additives, and may contain nicotine. The current e-cigarette market contains many different types of devices (see Table 1). By 2014, there were over 466 different brands of e-cigarettes [1]. Early e-cigarette devices (e.g., “cig-a-likes”) closely resembled a traditional cigarette and were disposable or rechargeable and had a fixed amount of nicotine. Later generation devices such as vape pens, hookah pens, and advanced vaporizers were more customizable, allowing users to change the nicotine concentration, temperature, and voltage, and e-liquid constituents. More recent e-cigarette devices include “pod” devices, such as JUUL, which are often discreet and technologically advanced (e.g., shaped like a USB memory stick). These pod devices are now among the most popular e-cigarette products on the market [2, 3].
While e-cigarettes were initially introduced to the market as a potential cleaner form of nicotine for adult cigarette smokers, evidence on the efficacy of different e-cigarette devices to help smokers quit smoking, as well as on the health effects and long-term consequences of use, is still emerging as scientific research strives to keep pace with the ever-changing landscape of e-cigarette technology. In the meantime, youth use of these products has increased rapidly [4•], and a forecast report from 2017 indicates that the e-cigarette industry is expected to continue growing to over $26 billion in sales worldwide by 2023 [5]. There is also emerging use of e-cigarette devices to vaporize a variety of other substances like synthetic cannabinoids and methamphetamine [6, 7], raising concerns about exposure to other substances with these devices.
The purpose of this review is to describe current trends in e-cigarette use, provide an overview of what is currently known regarding potential health risks and benefits, and discuss tobacco policy and regulatory considerations.
Prevalence and Appeal
E-cigarette use is prevalent among both youth and adult populations. The appeal of e-cigarettes among youth and adults appears to be related to the presence of many appealing flavors (recently estimated as over 15,000 distinct flavors [8•]), and common perceptions that e-cigarettes are a safer alternative to cigarettes [8•, 9,10,11,12,13, –14].
E-cigarettes appear to be particularly appealing to youth and are now the most commonly used tobacco product among youth in the USA [15]. Recent national estimates indicate that in 2018, over 3.6 million middle and high-school students in the US reported using e-cigarettes in the past 30 days, corresponding to 20.8% of high-school students and 4.9% of middle-school students [4]. According to a recently published systematic review [16] of youth surveys from 13 countries (US, Korea, New Zealand, UK including Scotland and Wales, Poland, Canada, Hungary, China including Hong Kong, France, Ireland, Italy, Iceland and Greece) between 2013 and 2015, the prevalence of e-cigarette use among youth < 20 years was highest in Poland (62.1%) and lowest in Italy (5.9%). The review also observed that these rates appear to vary based on smoking status; specifically, among non-smoking youth, e-cigarette use rates varied from 4.2% in the US to 14.0% in New Zealand, and among tobacco smoking youth, the rates varied from 29.9% in Italy to 71.9% in Canada.
Furthermore, there is evidence that surveys assessing e-cigarette prevalence rates may actually underestimate the rate of use among youth [17], since some devices that are popular with youth are commonly known by unique terminology (e.g., “juuling” for the popular JUUL pod system [3]), and users of these devices may not endorse “e-cigarette use” because they do not consider these products to be e-cigarettes. Survey data indicate that youth seem to prefer more advanced generation e-cigarettes and use multiple types of devices [18, 19].
Further, results from the 2015 National Youth Tobacco Survey in the US indicate that among youth who had never tried e-cigarettes before, 32.1% of middle-school and 38.4% of high-school youth were susceptible to future use, reporting that they might experiment with e-cigarettes in the future or use an e-cigarette if offered by a friend [20••]. Longitudinal evidence indicates that susceptibility to future e-cigarette use is a significant predictor of e-cigarette initiation as soon as 6 months later [21]. Ongoing research is examining factors that influence susceptibility among youth [22,23,24], and these results are important for developing effective prevention campaigns. For example, results from a nationally representative sample of US youth indicated that perceptions of e-cigarettes as addictive and harmful are associated with decreased susceptibility to use [23]. However, about 80% of youth do not perceive great risk of harm from regular use of e-cigarettes [25].
Among adults, global estimates of current e-cigarette use vary across different countries, ranging from < 5% (e.g., Canada, UK) to 14% (e.g., Malaysia), reported in the International Tobacco Control Surveys from 2009 to 2013 [26]. Additionally, the prevalence of e-cigarette use among adults has increased over time across several countries [27,28,29]. Business reports from 2018 estimates of global sales indicate that the US is currently the largest market for e-cigarette products [30, 31]. National US estimates from 2017 indicated that while traditional combustible cigarettes remained the most commonly used tobacco product (14.0%, 34.3 million adults), 6.9 million adults (2.8%) reported e-cigarette use in the past 30 days [32].
E-Cigarette Safety and Health Effects
E-cigarette use remains prevalent even though the safety and health effects of both acute and long-term use of e-cigarettes are still being determined. While e-cigarettes contain significantly fewer chemicals than those found in cigarettes, the aerosol generated from vaporizing e-liquids still contains many chemicals [33]. As detailed in a recent National Academies of Sciences report on e-cigarettes [34••], the following substances were identified in e-liquids and e-liquid aerosols: nicotine, propylene glycol, glycerin, tobacco-specific nitrosamines, aldehydes, volatile organic compounds, phenolic compounds, polycyclic aromatic hydrocarbons, a variety of flavoring chemicals (for example, acrolein and furfural), and tobacco alkaloids. While the levels of many of these compounds were lower than in combusted tobacco products, many of these agents are known respiratory toxins, inflammatory agents, and carcinogens, and it is unknown if the negative health effects are mitigated at lower exposure levels. However, a recent review suggests that e-cigarette use could be associated with pulmonary toxicity and increased incidence of asthma [35].
While the flavor chemicals in e-liquids and the solvents like propylene glycol and glycerin are generally recognized as safe for edible consumption, there is limited information on their safety following long-term exposure through inhalation. Recent evidence suggests that flavor chemicals can have toxic effects [36,37,38,39], and that e-liquid components can degrade into known toxicants when heated and vaporized [40,41,42]. Propylene glycol and glycerin have been identified as the source of many carbonyl compounds which have known toxicities [43, 44]. Many e-liquids may also contain alcohol as solvents, at levels high enough to influence psychomotor performance [45]. The aerosols can also contain metallic particles like chromium, cadmium, and lead, generated from the heating coils in the e-cigarette devices [46]. The levels of all these chemicals and their metabolites, as well as the metals, can be increased when e-liquids are vaporized at higher temperatures. Many e-cigarette devices allow users to modify the power and temperature in order to produce a better “throat hit” [47]. Thus, potential for high exposure to these chemicals exists, especially when e-cigarette devices are used for recreational behaviors that are popular among youth, like cloud chasing or vape tricks [48, 49] and “dripping” [50, 51], which involve vaporizing e-liquids at high temperatures to create thick vapor.
E-cigarettes can also expose users to high levels of nicotine. E-liquids are available in a wide variety of nicotine concentrations, with levels ranging from 0 ng/ml (i.e., no nicotine) to over 85 mg/ml [52], and a single e-liquid cartridge for some devices can contain the same amount of nicotine that is in a full pack of cigarettes [3]. Reports indicate many youth who use e-cigarettes do not know if they have used nicotine or not [53], which raises concerns about the potential for inadvertent exposure to nicotine. While most devices use a free-base nicotine solution, many of the newer pod devices contain a nicotine salt. Free-base nicotine is rapidly absorbed and produces rapid peaks in blood nicotine concentrations that can mimic combustible cigarettes, but it is also harsh and causes irritation [54]. In contrast, nicotine salt e-liquids contain free-base nicotine in combination with benzoic acid which lowers the pH of the e-liquid and allows for smoother delivery of higher doses of nicotine without throat irritation [54, 55]. While the higher levels of nicotine delivered in these nicotine salt solutions with pod devices (such as JUUL) may be beneficial to smokers who are trying to quit smoking combustible cigarettes, there is a lack of empirical evidence on this issue. It is also concerning that these pod-devices like JUUL are very popular among youth [3], and it was recently observed that youth who used JUUL had higher urine cotinine levels than a sample of youth who regularly smoked combustible cigarettes [56], indicating greater exposure to nicotine from these e-cigarettes and the potential for developing nicotine addiction.
It is important to remember that nicotine is not only addictive but influences many organ systems in the human body through its activity at the nicotinic acetylcholine receptor system. Acute effects of nicotine include a rapid increase in pulse rate and blood pressure, as well as an increase in the levels of catecholamines in the blood [57•, 58]. Nicotine also leads to increases in plasma-free fatty acids, hyperglycemia, an increased rate of respiration, endothelial dysfunction, and inflammation, and increases in blood viscosity [34, 59,60,61]. Chronic exposure to nicotine can change the functioning of all these systems. For example, nicotine use via e-cigarettes influences many cardiovascular markers [60,61,62], and there is evidence that e-cigarette use is associated with increased risk of myocardial infarction [63]. Importantly, nicotine is also a well-established neurotoxin in the adolescent brain [64]. The adolescent brain is highly susceptible to the effects of nicotine [65], and nicotine exposure during adolescence can interfere with development and cognitive functioning [66, 67•] and lead to nicotine addiction [66, 68].
Development of Nicotine Addiction and Progression to Other Substance Use Among Youth
In addition to potential toxicant exposure from e-cigarette constituents, e-cigarette use raises other concerns especially for youth. Data suggest that e-cigarettes are often the first tobacco product tried by youth [69, 70], and youth who are exposed to nicotine through these devices are at risk for nicotine addiction [71, 72] and progression to other substance use, including combustible tobacco products [73•, 74]. Nicotine is highly addictive, and nicotine dependence can develop quickly in adolescents [75]. Longitudinal studies indicate that even minimal exposure to nicotine only a few times puts youth at greater risk for later addiction [68].
Emerging evidence indicates youth e-cigarette users experience many symptoms of dependence, including craving or a strong urge to use e-cigarettes [71, 72]. Studies of high-school aged students indicate youth who first tried e-cigarettes at a younger age were at greater risk for e-cigarette dependence [72], and higher dependence is associated with lower odds of wanting to quit e-cigarettes [71]. Thus, there is evidence that some youth are progressing beyond initial experimentation with e-cigarettes and developing dependence. Recent reports indicate some youth are using e-cigarettes frequently; in 2018, over a quarter of US high-school students who used e-cigarettes reported using the product on more than 20 out of the past 30 days [4•].
E-cigarette use may also put youth at risk for other tobacco use. Youth who use e-cigarettes report greater intentions to smoke cigarettes [76, 77], and there is evidence from longitudinal studies that youth who use e-cigarettes are significantly more likely to transition to conventional cigarette use over time [73•, 78,79,80,81]. E-cigarette use predicts subsequent cigarette use even among youth who use e-cigarettes infrequently; one study showed that youth were significantly more likely to initiate conventional cigarette smoking whether they previously used e-cigarettes only 1–2 times (odds ratio OR = 2.88, 95% CI = 1.96–4.22) or as often as weekly/daily (OR = 4.09, 95% CI = 2.43–6.88) [82].
In addition to increasing the risk for future cigarette smoking, e-cigarette use may also put youth at risk for other substance use. Longitudinal studies indicate e-cigarette users are at higher risk for initiating and using marijuana over time [74], and national survey studies in the US report that 10% of youth used e-cigarette devices to vape marijuana in 2017 [25]. Thus, e-cigarette use among youth poses risk for nicotine dependence and other substance use.
Effects on Smoking Cessation and Dual Use Among Smokers
On the one hand, e-cigarettes may be beneficial for public health if they serve as a smoking cessation aid, providing an alternative way to obtain nicotine with fewer harmful chemicals than combustible cigarettes. Some population survey studies support this notion, indicating greater rates of quit attempts or cessation success among adult cigarette smokers who use e-cigarettes [83,84,85,86], while other studies report lower rates of smoking cessation among e-cigarette users [87,88,89,90]. Systematic reviews conclude that there is currently very low-quality evidence supporting e-cigarettes for smoking cessation [91•, 92], in part because there is a need for more well-designed randomized controlled trials and longitudinal studies. Synthesizing equivocal results across studies is difficult because there is wide variability across studies in e-cigarette device characteristics (e.g., device type, nicotine level, flavor), use behavior (e.g., frequency and duration), and subject-related factors (e.g., quitting motivation, nicotine dependence) that may impact cessation outcomes. Preliminary evidence also suggests that the variability in the real-world effectiveness of e-cigarettes for smoking cessation may be related to the regulatory environment for these products, and that smokers in countries that have stricter regulations (e.g., Canada, Australia) are less likely to use these devices in unassisted quit attempts [93•].
Very few randomized controlled trials have been published that evaluate the efficacy of e-cigarettes for smoking cessation. In one trial, participants who were not intending to quit smoking in the next 30 days were randomized to one of two nicotine e-cigarettes or a placebo (no-nicotine) e-cigarette [94]. All participants significantly reduced their cigarette consumption throughout the study, and there were no statistically significant differences in median cigarettes per day or biochemically confirmed quit rates at 6-month and 1-year follow-ups among the three groups. A separate study that recruited smokers who were motivated to quit randomized participants to use a nicotine e-cigarette, placebo e-cigarette, or nicotine patch, and everyone received minimal behavioral support to quit smoking through telephone counseling [95]. Although those in the nicotine e-cigarette group reduced their cigarette consumption more than those in the nicotine patch group, the nicotine e-cigarette was not superior to the placebo e-cigarette, and there were no significant differences in biochemically confirmed continuous abstinence rates at 6 months between the three groups. A meta-analysis pooled the results of these two studies and concluded that there is some evidence that nicotine containing e-cigarettes are more effective than placebo (no-nicotine) e-cigarettes for reducing or stopping smoking [91•]. However, the combined effect size estimate was very small (5%) and the authors of the meta-analysis graded the evidence as low quality given the small number of studies analyzed. Additional studies are needed to understand the potential role of e-cigarettes for smoking cessation, especially as e-cigarette devices continue to evolve. Importantly, these two earlier studies evaluated the efficacy of first-generation e-cigarettes that have now been replaced by newer devices that are more efficient at delivering nicotine and therefore may be a more effective substitute for combustible cigarettes.
Other randomized trials have compared e-cigarettes to standard tobacco treatment. One study was a pragmatic trial offering smoking cessation interventions to employees who smoked regardless of their current interest in quitting [96]. Everyone received usual care (e.g., information on the benefits of quitting and access to a free text messaging service, SmokeFreeTXT from the National Cancer Institute), and some were randomized to one of several additional interventions. The primary outcome was biochemically confirmed sustained smoking abstinence 6 months later. Quit rates were low for all groups, and results indicated there were no differences between those randomized to receive free e-cigarettes, free cessation aids (e.g., nicotine replacement therapy or pharmacotherapy), or usual care alone.
A separate study recruited patients who were attending stop-smoking services in the UK and randomized them to receive either 3 months of nicotine replacement therapy (NRT) of their choice, including combinations of NRT products or an e-cigarette starter pack [97•]. Contrary to prior trials, all participants in this study also received weekly face-to-face behavioral support for at least 4 weeks. Results indicated significantly higher 1-year biochemically confirmed sustained abstinence rates among the e-cigarette group (18.0%) compared to the NRT group (9.9%). These data suggest e-cigarettes are effective for promoting abstinence from combustible cigarettes when combined with face-to-face behavioral support to quit smoking. However, of those who achieved abstinence at 1 year, 80% in the e-cigarette group were still using the device and remain exposed to nicotine and other chemicals from e-cigarette use, while only 9% were still using NRT.
These recent results show promise for the role of e-cigarettes in smoking cessation, although many questions still need to be answered in order to inform smokers about how to use these products to help them quit. For example, research is needed to identify what is the adequate dosage and duration of e-cigarette use to promote cessation, as well as how to combine e-cigarettes with other cessation aids or counseling, and how and when to discontinue e-cigarette use after quitting. A search of a trial registry (clinicaltrials.gov) shows there are multiple ongoing studies across various countries evaluating the use of e-cigarettes for smoking cessation, and we hope additional data will inform the use of these devices to optimize smoking cessation and reduce harm.
In general, e-cigarettes may be an effective harm reduction strategy if they substitute completely for smoked cigarettes. However, dual use of both cigarettes and e-cigarettes is common [26, 32], and longitudinal results from the US Population Assessment of Tobacco and Health study (PATH 2013–2015) indicate that over 44% of adult dual users of e-cigarettes and cigarettes maintained their dual use over time [98]. While dual use may be reducing harm exposure if e-cigarettes are replacing combustible cigarette use, there is the potential that e-cigarette use actually increases nicotine exposure if these devices are used in places where combustible smoking is not allowed (e.g., indoors), rather than as a substitution. Additionally, dual users continue to be exposed to the harmful effects of conventional cigarettes. Data on the health effects of cigarette smoking indicate that even light smoking (i.e., 1–4 cigarettes per day) significantly increases risk for cardiovascular problems and cancer [99, 100]. Furthermore, there is evidence that cigarette and e-cigarette use independently contribute to cardiovascular [63] and pulmonary risk [101], such that dual users of both products are at even greater risk compared to those using only cigarettes or e-cigarettes alone. Ultimately, there may be limited public health benefit if e-cigarette use reduces cigarette consumption but does not promote total abstinence from cigarettes; data on the long-term health effects are needed to address this question.
Additionally, among youth and young adults, evidence indicates that e-cigarette use is not associated with smoking cessation or reduction. Results from surveys and observational cessation studies of youth and young adults indicate e-cigarette use is associated with lower motivation to quit smoking cigarettes [102] and a lower likelihood of stopping smoking [103]. Additionally, results from one study indicate that adolescents who are dual users of both e-cigarettes and cigarettes actually smoke more cigarettes, not fewer [104]. Dual use is especially concerning among youth because it increases the risk for developing nicotine dependence [105].
Ultimately, smokers need to be educated about the potential benefits and harms of e-cigarettes, and in the absence of strong evidence supporting e-cigarettes for cessation and guidance about how to use these devices to promote quitting, they should be encouraged to first consider other evidence-based methods to quit smoking, including available pharmacotherapies and behavioral counseling [106].
Regulatory Policy
The potential public health impact of e-cigarettes is complex. Regulatory policies that strike a balance between the potential benefit of these devices for adult smokers who are trying to quit smoking with reducing the appeal and addictive potential for youth are critically needed. But, establishing these regulatory policies is complex and challenging, and current regulations have not been able to keep up with the rapid market growth in e-cigarette devices and e-liquids.
Internationally, there is wide variability in how e-cigarettes are classified, which has also led to large differences in regulations of these products [107•]. According to evidence presented on a Global Tobacco Control website hosted by Johns Hopkins University [108•], which was extracted from the World Health Organization (WHO) report on electronic nicotine delivery systems [109•], of 98 countries examined, 70 classify e-cigarettes as vaping products, 57 as tobacco products, 24 as medicinal products, 18 as consumer products or devices, and 4 regulate these as poisons or hazardous substances because they contain nicotine with no medicinal purpose. The report further observed that the use of policies that has been standardly applied to combustible tobacco products like minimum age of purchase, restrictions on sales/marketing/packaging, product regulation, as well as inclusion in clean air and taxation laws, also vary widely around the world. Only 36 countries have minimal age of purchase/sales for these devices. With regard to sales, a large majority either ban sales of all types of e-cigarettes (29 countries) or regulate sales or require marketing authorization prior to sales (45 countries). The WHO report also indicates that 67 countries prohibit or regulate e-cigarette marketing, and 38 require health warnings on e-cigarette packaging. With regard to the product itself, 32 countries regulate the amount of nicotine in e-liquids, 32 do not permit the use of harmful ingredients other than nicotine, and 31 regulate the quality of e-liquid content. Finally, 49 countries prohibit or restrict use of e-cigarettes in public places, and only 13 countries tax e-cigarettes. The WHO report strongly encouraged countries that had not already banned e-cigarettes to consider applying some of the above regulatory policies, along with strong monitoring. Strong monitoring of these policies is critical for understanding the impact on public health. For example, although regulations in Australia prohibit the sale, possession, or use of nicotine-containing e-cigarettes, results from the 2013 International Tobacco Control Survey indicated 43% of current e-cigarette users surveyed in Australia reported using an e-cigarette with nicotine [29]. Changes in tobacco regulations and enforcement of these policies have the potential to greatly influence e-cigarette use. We provide below an example of how e-cigarette regulation has changed over time in the US.
Regulations in the US
In the US, e-cigarettes are regulated as tobacco products under the Family Smoking and Prevention Tobacco Control Act (FSPTCA) which passed in 2009 [110]. The original FSPTCA only covered cigarettes, cigarette tobacco, roll-your-own tobacco, and smokeless tobacco, and required that any tobacco product that appeared on the market after February 15, 2007, would need to get approval from the US Food and Drug Administration (FDA). The FSPTCA gave FDA the authority to enforce federal controls on sales of tobacco products to children; require that tobacco companies post ingredient lists for their products; require smokeless tobacco product–warning labels; preserve state, local, and tribal authority; and require that prior to making any claims of reduced harm (also known as modified risk) or no change in harm (also known as substantial equivalence) on any product, an application for that product would need to be submitted to the FDA and be approved. This law makes it clear that the FDA could not require prescriptions to purchase tobacco products, require the reduction of nicotine yields to zero in any product, or ban face-to-face sales of certain classes of tobacco products in retail outlets. The FDA’s regulation of tobacco products must be based on scientific evidence, and the evaluation of any new product is required to consider the risks and benefits of the product to the population as a whole, including users and non-users.
In 2016, the FDA extended its authority to cover “all products that meet the statutory definition of ‘tobacco products,’” including electronic nicotine delivery systems (ENDS: e-cigarettes, e-hookah, e-cigars, vape pens, advanced refillable personal vaporizers, and electronic pipes), and other products such as dissolvables, gels, waterpipe tobacco, cigars, and pipe tobacco [111•]. The FDA also required nicotine exposure warnings and child-resistant packaging on all products, including e-liquids. The FDA later announced that in order to ensure they had the appropriate scientific evidence to balance regulation while encouraging development of innovative tobacco products that may be less dangerous than cigarettes, they would delay the deadline for applications for cigars, pipe tobacco, and hookah tobacco to August 8, 2021, and for non-combustible products such as e-cigarettes to August 8, 2022. Manufacturers can continue to market products that have been on the market prior to August 2017 until the product applications are reviewed.
More recently, in November 2018, the FDA released an announcement [112] in response to the significant increase in youth use of e-cigarettes [4•], detailing planned regulatory policies that would restrict access to flavored e-liquids in common retail locations, like convenience stores and gas stations, and require stricter regulations on sales of these devices and e-liquids to minors over the internet. It is worth noting that the majority of sales of these devices come from non-traditional outlets like vape shops and online retailers [113], and many youth report obtaining their devices from online sales [114]. The FDA has also recently launched targeted youth prevention efforts; specifically, they have developed a national e-cigarette prevention campaign aiming to change youth attitudes and beliefs about e-cigarettes [115].
It is expected that these and future regulatory policies will make strides towards decreasing access of e-cigarette devices to youth while maintaining access to individuals trying to quit smoking, but the path is not an easy one. For example, there is a significant concern that although limiting access to a variety of e-liquid flavors may reduce the appeal of e-cigarettes to youth, this regulation may also lead to decreases in smoking cessation efforts for adult smokers who are using these devices to quit smoking. Importantly, because e-cigarettes are regulated as a tobacco product in the US, rather than another product category, there are limits to the kinds of regulatory policies that can be implemented. For example, the FDA cannot require a prescription for e-cigarettes to encourage use only by adult smokers wanting to quit. Additional research on e-cigarette product characteristics, marketing, and access will be needed to inform US regulatory policies to reduce the appeal to youth and limit the potential toxicity for users.
Conclusions
E-cigarettes hold a lot of potential for use as part of a harm reduction strategy for smoking cessation in cigarette smokers. However, the current evidence to support the use of e-cigarettes to quit smoking is limited. Additional clinical research is needed to determine the optimal frequency and duration of use as well as the specific devices, constituents, and e-liquid features that may aid in smoking cessation. Utilization of these devices for smoking cessation should be accompanied by a strong behavioral counseling program and would likely involve a taper to wean subjects off nicotine to avoid the potential for returning to combustible product use.
Future efforts also need to focus on implementing regulatory policies as well as developing prevention and education programs to reduce e-cigarette use in youth to avoid new initiation of nicotine use and addiction, while supporting quitting efforts for current smokers. E-cigarette regulatory policies vary widely by country, and the range of classifications of e-cigarettes (e.g., tobacco product vs. medicinal product) influences the type of regulations that can be made. As the e-cigarette industry continues to evolve, the development of evidence-based regulatory policies and ongoing monitoring will be critical for establishing product standards and ensuring that e-cigarettes are available as part of a harm reduction approach to help smokers quit while restricting youth use and preventing renormalization of nicotine addiction.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zhu S-H, Sun JY, Bonnevie E, Cummins SE, Gamst A, Yin L, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(suppl 3):iii3–9.
Huang J, Duan Z, Kwok J, Binns S, Vera LE, Kim Y, et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2018;28(2):146-151.
Willett JG, Bennett M, Hair EC, Xiao H, Greenberg MS, Harvey E, et al. Recognition, use and perceptions of JUUL among youth and young adults. Tob Control. 2019;28(1):115-116. https://doi.org/10.1136/tobaccocontrol-2018-054273.
• Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students - United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2018;67:1276–7. https://doi.org/10.15585/mmwr.mm6745a5. Recent 2018 national rates and trends in e-cigarette use among U.S. youth.
Electronic cigarette market by product type, flavor, and distribution channel - global opportunity analysis and industry forecast, 2017-2023. In: Research and markets 2018. https://www.researchandmarkets.com/research/pjkd84/global_electronic?w=5.
Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611–6. https://doi.org/10.1542/peds.2015-1727.
Breitbarth AK, Morgan J, Jones AL. E-cigarettes-an unintended illicit drug delivery system. Drug Alcohol Depend. 2018;192:98–111.
• Hsu G, Sun JY, Zhu S-H. Evolution of electronic cigarette brands from 2013–2014 to 2016–2017: analysis of brand websites. J Med Internet Res. 8: 2018;20(3):e80. Reviews trends in e-cigarette devices, flavors, point-of-sale, and discusses regulation implications.
Ambrose BK, Rostron BL, Johnson SE, Portnoy DB, Apelberg BJ, Kaufman AR, et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2, Supplement 1):S53–60. https://doi.org/10.1016/j.amepre.2014.04.016.
Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P, et al. Reasons for current e-cigarette use among US adults. Prev Med. 2016;93:14–20.
Pepper JK, Ribisl KR, Emery SL, Brewer NT. Reasons for starting and stopping electronic cigarette use. Int J Environ Public Health. 2014;11:10345–61. https://doi.org/10.3390/ijerph111010345.
Tsai J, Walton K, Coleman BN, Sharapova SR, Johnson SE, Kennedy SM, et al. Reasons for electronic cigarette use among middle and high school students—National Youth Tobacco Survey, United States, 2016. MMWR. 2018;67(6):196–200.
Ambrose BK, Day HR, Rostron B, Conway KP, Borek N, Hyland A, et al. Flavored tobacco product use among US youth aged 12-17 years, 2013-2014. JAMA. 2015;314(17):1871–3.
Pepper JK, Brewer NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review. Tob Control. 2014;23:375–84. https://doi.org/10.1136/tobaccocontrol-2013-051122.
Wang TW, Gentzke A, Sharapova S, Cullen KA, Ambrose BK, Jamal A. Tobacco product use among middle and high school students—United States, 2011–2017. MMWR. 2018;67(22):629–33.
Yoong SL, Stockings E, Chai LK, Tzelepis F, Wiggers J, Oldmeadow C, et al. Prevalence of electronic nicotine delivery systems (ENDS) use among youth globally: a systematic review and meta-analysis of country level data. Aust N Z J Public Health. 2018;42:303–8.
Morean ME, Camenga DR, Bold KW, Kong G, Jackson A, Simon P, et al. Querying about the use of specific e-cigarette devices may enhance accurate measurement of e-cigarette prevalence rates among high school students. Nicotine Tob Res. 2018. https://doi.org/10.1093/ntr/nty240.
Barrington-Trimis JL, Gibson LA, Halpern-Felsher B, Harrell MB, Kong G, Krishnan-Sarin S, et al. Type of e-cigarette device used among adolescents and young adults: findings from a pooled analysis of eight studies of 2166 vapers. Nicotine Tob Res. 2017;20(2):271–4.
Krishnan-Sarin S, Jackson A, Morean M, Kong G, Bold KW, Camenga DR, et al. E-cigarette devices used by high-school youth. Drug Alcohol Depend. 2019;194:395–400.
•• USDHHS. E-cigarette use among youth and young adults. A report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health; 2016. Comprehensive summary of scientific research to date on e-cigarette use trends and health effects in youth and young adults.
Bold KW, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. E-cigarette susceptibility as a predictor of youth initiation of e-cigarettes. Nicotine Tob Res. 2016;20(1):140–4.
Carey FR, Rogers SM, Cohn EA, Harrell MB, Wilkinson AV, Perry CL. Understanding susceptibility to e-cigarettes: a comprehensive model of risk factors that influence the transition from non-susceptible to susceptible among e-cigarette naïve adolescents. Addict Behav. 2018.
Kwon E, Seo D-C, Lin H-C, Chen Z. Predictors of youth e-cigarette use susceptibility in a US nationally representative sample. Addict Behav. 2018;82:79–85.
Garrison KA, O'Malley SS, Gueorguieva R, Krishnan-Sarin S. A fMRI study on the impact of advertising for flavored e-cigarettes on susceptible young adults. Drug Alcohol Depend. 2018;186:233–41.
Johnston LD, Miech RA, O'Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future national survey results on drug use, 1975–2017: overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2018.
Gravely S, Fong GT, Cummings KM, Yan M, Quah AC, Borland R, et al. Awareness, trial, and current use of electronic cigarettes in 10 countries: findings from the ITC project. Int J Environ Res Public Health. 2014;11(11):11691–704.
Farsalinos KE, Poulas K, Voudris V, Le Houezec J. Electronic cigarette use in the European Union: analysis of a representative sample of 27 460 Europeans from 28 countries. Addiction. 2016;111(11):2032–40.
Hummel K, Hoving C, Nagelhout GE, de Vries H, van den Putte B, Candel MJ, et al. Prevalence and reasons for use of electronic cigarettes among smokers: findings from the International Tobacco Control (ITC) Netherlands Survey. Int J Drug Policy. 2015;26(6):601–8.
Yong H-H, Borland R, Balmford J, McNeill A, Hitchman S, Driezen P, et al. Trends in e-cigarette awareness, trial, and use under the different regulatory environments of Australia and the United Kingdom. Nicotine Tob Res. 2014;17(10):1203–11.
Jones L. Vaping - the rise in five charts. BBC News 2018. https://www.bbc.com/news/business-44295336.
BIS Research. Global e-cigarette and t-vapor market to reach $86.43 billion by 2025, Reports BIS Research. Minnesota: PRNewswire; 2018. https://www.prnewswire.com/news-releases/global-e-cigarette-and-t-vapor-market-to-reach-8643-billion-by-2025-reports-bis-research-675808803.html.
Wang TW, Asman K, Gentzke A, Cullen K, Holder-Hayes E, Reyes-Guzman C, et al. Tobacco product use among adults - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67:1225–32.
Goniewicz M, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–9.
•• National Academies of Sciences E, and Medicine. Public health consequences of e-cigarettes. Washington, DC: The National Academies Press; 2018. https://doi.org/10.17226/24952. Comprehensive summary of scientific research to date on e-cigarette toxicity and health effects
Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Phys Lung Cell Mol Phys. 2017;313(2):L193–206.
Behar RZ, Luo W, McWhirter KJ, Pankow JF, Talbot P. Analytical and toxicological evaluation of flavor chemicals in electronic cigarette refill fluids. Sci Rep. 2018;8(1):8288.
Bengalli R, Ferri E, Labra M, Mantecca P. Lung toxicity of condensed aerosol from e-CIG liquids: influence of the flavor and the in vitro model used. Int J Environ Res Public Health. 2017;14(10):1254.
Muthumalage T, Prinz M, Ansah KO, Gerloff J, Sundar IK, Rahman I. Inflammatory and oxidative responses induced by exposure to commonly used e-cigarette flavoring chemicals and flavored e-liquids without nicotine. Front Physiol. 2018;8:1130.
Rowell TR, Reeber SL, Lee SL, Harris RA, Nethery RC, Herring AH, et al. Flavored e-cigarette liquids reduce proliferation and viability in the CALU3 airway epithelial cell line. Am J Phys Lung Cell Mol Phys. 2017;313(1):L52–66.
Kamilari E, Farsalinos K, Poulas K, Kontoyannis CG, Orkoula MG. Detection and quantitative determination of heavy metals in electronic cigarette refill liquids using total reflection X-ray fluorescence spectrometry. Food Chem Toxicol. 2018;116:233–7.
Pankow JF, Kim K, McWhirter KJ, Luo W, Escobedo JO, Strongin RM, et al. Benzene formation in electronic cigarettes. PLoS One. 2017;12(3):e0173055.
Sleiman M, Logue JM, Montesinos VN, Russell ML, Litter MI, Gundel LA, et al. Emissions from electronic cigarettes: key parameters affecting the release of harmful chemicals. Environ Sci Technol. 2016;50(17):9644–51.
Jensen RP, Luo W, Pankow JF, Strongin RM, Peyton DH. Hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372(4):392–4.
Wang P, Chen W, Liao J, Matsuo T, Ito K, Fowles J, et al. A device-independent evaluation of carbonyl emissions from heated electronic cigarette solvents. PLoS One. 2017;12(1):e0169811.
Valentine GW, Jatlow PI, Coffman M, Nadim H, Gueorguieva R, Sofuoglu M. The effects of alcohol-containing e-cigarettes on young adult smokers. Drug Alcohol Depend. 2016;159:272–6.
Gaur S, Agnihotri R. Health effects of trace metals in electronic cigarette aerosols—a systematic review. Biol Trace Elem Res. 2019;188(2):295-315.
DeVito EE, Krishnan-Sarin S. E-cigarettes: impact of E-liquid components and device characteristics on nicotine exposure. Curr Neuropharmacol. 2018;16(4):438–59.
Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17:847–54. https://doi.org/10.1093/ntr/ntu257.
Pepper JK, Lee YO, Watson KA, Kim AE, Nonnemaker JM, Farrelly MC. Risk factors for youth E-cigarette “Vape trick” behavior. J Adolesc Health. 2017;61(5):599–605.
Talih S, Balhas Z, Salman R, Karaoghlanian N, Shihadeh A. “Direct dripping”: a high-temperature, high-formaldehyde emission electronic cigarette use method. Nicotine Tob Res. 2015:ntv080.
Krishnan-Sarin S, Morean ME, Kong G, Bold KW, Camenga DR, Cavallo D, et al. “Dripping” among youth using e-cigarettes. Pediatrics. 2017;139(3):e20163224.
Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23(suppl 2):ii11–i7.
Morean ME, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Nicotine concentration of e-cigarettes used by adolescents. Drug Alcohol Depend. 2016;167:224–7.
Duell AK, Pankow JF, Peyton DH. Free-base nicotine determination in electronic cigarette liquids by 1H NMR spectroscopy. Chem Res Toxicol. 2018;31:431–4.
Spindle TR, Eissenberg T. Pod mod electronic cigarettes—an emerging threat to public health. JAMA Netw Open. 2018;1(6):e183518-e.
Goniewicz ML, Boykan R, Messina CR, Eliscu A, Tolentino J. High exposure to nicotine among adolescents who use Juul and other vape pod systems (‘pods’). Tob Control. 2018:tobaccocontrol-2018-054565. https://doi.org/10.1136/tobaccocontrol-2018-054565.
• Bhatnagar A. E-cigarettes and cardiovascular disease risk: evaluation of evidence, policy implications, and recommendations. Curr Cardiovasc Risk Rep. 2016;10(7):24. Review of cardiovasular effects of nicotine and e-cigarettes.
Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nat Rev Cardiol. 2017;14(8):447.
US Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. Rockville: US Department of Health and Human Services; 2010.
Benowitz NL, Burbank AD. Cardiovascular toxicity of nicotine: implications for electronic cigarette use. Trends Cardiovasc Med. 2016;26(6):515–23.
Franzen KF, Willig J, Cayo Talavera S, Meusel M, Sayk F, Reppel M, et al. E-cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: a randomized, double-blinded pilot study. Vasc Med. 2018;23(5):419–25.
Nocella C, Biondi-Zoccai G, Sciarretta S, Peruzzi M, Pagano F, Loffredo L, et al. Impact of tobacco versus electronic cigarette smoking on platelet function. Am J Cardiol. 2018;122(9):1477–81.
Alzahrani T, Pena I, Temesgen N, Glantz SA. Association between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55(4):455–61.
Abreu-Villaça Y, Seidler FJ, Tate CA, Slotkin TA. Nicotine is a neurotoxin in the adolescent brain: critical periods, patterns of exposure, regional selectivity, and dose thresholds for macromolecular alterations. Brain Res. 2003;979(1–2):114–28.
Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–412.
Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122:125–39. https://doi.org/10.1016/j.pharmthera.2009.02.003.
• Smith RF, McDonald CG, Bergstrom HC, Ehlinger DG, Brielmaier JM. Adolescent nicotine induces persisting changes in development of neural connectivity. Neurosci Biobehav Rev. 2015;55:432–43. Reviews nicotine effects in adolescent brain development.
Sargent JD, Gabrielli J, Budney A, Soneji S, Wills TA. Adolescent smoking experimentation as a predictor of daily cigarette smoking. Drug Alcohol Depend. 2017;175:55–9.
Hines JZ, Fiala SC, Hedberg K. Electronic cigarettes as an introductory tobacco product among eighth and 11th grade tobacco users—Oregon, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(23):604–6.
Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. 2015;17:810–8. https://doi.org/10.1093/ntr/ntu243.
Case KR, Mantey DS, Creamer MR, Harrell MB, Kelder SH, Perry CL. E-cigarette-specific symptoms of nicotine dependence among Texas adolescents. Addict Behav. 2018;84:57–61.
Morean ME, Krishnan-Sarin S, O’Malley SS. Assessing nicotine dependence in adolescent e-cigarette users: the 4-item Patient-Reported Outcomes Measurement Information System (PROMIS) Nicotine Dependence Item Bank for electronic cigarettes. Drug Alcohol Depend. 2018;188:60–3.
• Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–97. Meta-analysis summarizing e-cigarette use as a significant predictor of future cigarette smoking among youth.
Audrain-McGovern J, Stone MD, Barrington-Trimis J, Unger JB, Leventhal AM. Adolescent E-cigarette, hookah, and conventional cigarette use and subsequent marijuana use. Pediatrics. 2018;142(3):e20173616.
DiFranza JR, Savageau JA, Fletcher K, O’Loughlin J, Pbert L, Ockene JK, et al. Symptoms of tobacco dependence after brief intermittent use: the development and assessment of nicotine dependence in youth–2 study. Arch Pediatr Adolesc Med. 2007;161(7):704–10.
McCabe SE, Veliz P, McCabe VV, Boyd CJ. Smoking behaviors and intentions among current e-cigarette users, cigarette smokers, and dual users: a national survey of US high school seniors. Prev Med. 2017;99:228–35.
Park J-Y, Seo D-C, Lin H-C. E-cigarette use and intention to initiate or quit smoking among US youths. Am J Public Health. 2016;106(4):672–8.
Miech R, Patrick ME, O'Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017:tobaccocontrol-2016-053291.
Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):e20160379.
Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–7. https://doi.org/10.1001/jama.2015.8950.
Bold KW, Kong G, Camenga DR, Simon P, Cavallo DA, Morean ME, et al. Trajectories of e-cigarette and conventional cigarette use among youth. Pediatrics. 2018;141(1):e20171832.
Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2017;26(1):34-39.
Adkison SE, O'Connor RJ, Bansal-Travers M, Hyland A, Borland R, Yong H-H, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44(3):207–15.
Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110(7):1160–8.
Zhu S-H, Zhuang Y-L, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358:j3262. https://doi.org/10.1136/bmj.j3262.
Johnson L, Ma Y, Fisher SL, Ramsey AT, Chen L-S, Hartz SM, et al. E-cigarette usage is associated with increased past-12-month quit attempts and successful smoking cessation in two US population–based surveys. Nicotine Tob Res. 86: 2018:1-8. https://doi.org/10.1093/ntr/nty211
Kulik MC, Lisha NE, Glantz SA. E-cigarettes associated with depressed smoking cessation: a cross-sectional study of 28 European Union countries. Am J Prev Med. 2018;54(4):603–9.
Rigotti NA, Chang Y, Tindle HA, Kalkhoran SM, Levy DE, Regan S, et al. Association of E-cigarette use with smoking cessation among smokers who plan to quit after a hospitalization: a prospective study. Ann Intern Med. 2018;168(9):613–20.
Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4:116–28.
Weaver SR, Huang J, Pechacek TF, Heath JW, Ashley DL, Eriksen MP. Are electronic nicotine delivery systems helping cigarette smokers quit? Evidence from a prospective cohort study of US adult smokers, 2015–2016. PLoS One. 2018;13(7):e0198047.
• Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Libr. 2016;(9). https://doi.org/10.1002/14651858.CD010216.pub3. Meta-analysis indicating there is some evidence that nicotine containing e-cigarettes are more effective than placebo (no-nicotine) e-cigarettes for smoking cessation, although the quality of the evidence is low given the limited number of randomized controlled trials.
Malas M, van der Tempel J, Schwartz R, Minichiello A, Lightfoot C, Noormohamed A, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res. 2016;18(10):1926–36.
• Yong H-H, Hitchman SC, Cummings KM, Borland R, Gravely SM, McNeill A, et al. Does the regulatory environment for e-cigarettes influence the effectiveness of e-cigarettes for smoking cessation?: Longitudinal findings from the ITC Four Country Survey. Nicotine Tob Res. 2017;19(11):1268–76. Examines the influence of regulatory environment on real-world effectiveness of e-cigarettes across multiple countries.
Caponnetto P, Campagna D, Cibella F, Morjaria J, Caruso M, Russo C, et al. EffiCiency and safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8(6):e66317.
Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J et al. Electronic cigarettes for smoking cessation: a randomised controlled trial, in press. Published online. Lancet. 2013;382(9905):16-22.
Halpern SD, Harhay MO, Saulsgiver K, Brophy C, Troxel AB, Volpp KG. A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. N Engl J Med. 2018;378:2302-2310 .
• Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629-637.
Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) study, waves 1 and 2 (2013–2015). Tob Control. 2018:tobaccocontrol-2017-054174.
Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health–AARP diet and health study. JAMA Intern Med. 2017;177(1):87–95.
Pope CA, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke shape of the exposure-response relationship. Circulation. 2009;120(11):941–8.
Wills TA, Pagano I, Williams RJ, Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend. 2019;194:363–70.
Huang L-L, Kowitt SD, Sutfin EL, Patel T, Ranney LM, Goldstein AO. Electronic cigarette use among high school students and its association with cigarette use and smoking cessation, North Carolina Youth Tobacco Surveys, 2011 and 2013. Prev Chronic Dis. 2016;13:E103.
Gmel G, Baggio S, Mohler-Kuo M, Daeppen J-B, Studer J. E-cigarette use in young Swiss men: is vaping an effective way of reducing or quitting smoking? Swiss Med Wkly. 2015;146:w14271-w.
Goniewicz ML, Leigh NJ, Gawron M, Nadolska J, Balwicki L, McGuire C, et al. Dual use of electronic and tobacco cigarettes among adolescents: a cross-sectional study in Poland. Int J Public Health. 2016;61(2):189–97.
USDHHS. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. p. 17.
Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville: U.S. Department of Health and Human Services. Public Health Service; 2008.
• Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob Control. 2017;26(4):440–5. Describes e-cigarette product classifications and summarizes global e-cigarette regulatory policies.
•• Institute for Global Tobacco Control. Country laws regulating e-cigarettes: a policy scan. Baltimore: Johns Hopkins Bloomberg School of Public Health; 2018. http://globaltobaccocontrol.org/e-cigarette/country-laws-regulating-e-cigarettes. Summarizes global e-cigarette regulatory policies by country.
• World Health Organization. Electronic Nicotine Delivery Systems. WHO Framework Convention on Tobacco Control. 2014. http://apps.who.int/gb/fctc/pdf/cop6/fctc_cop6_10-en.pdf. Provides detailed policy suggestions for countries to regulate e-cigarettes.
Family Smoking Prevention and Tobacco Control, PUBLIC LAW 111–31 (2009).
• Food and Drug Administration. Deeming tobacco products to be subject to the federal food, drug, and cosmetic act, as amended by the family smoking prevention and tobacco control act; restrictions on the sale and distribution of tobacco products and required warning statements for tobacco products. Final rule. Fed Regist. 2016;81(90):28973. U.S. FDA plan to regulate e-cigarettes as a tobacco product.
FDA. Statement from FDA Commissioner Scott Gottlieb, MD, on proposed new steps to protect youth by preventing access to flavored tobacco products and banning menthol in cigarettes: U.S. Food & Drug Administration; 2018.
Nielsen HB. Tobacco “all channel” data through August 12, 2017. Charlotte: Wells Fargo Securities, LLC; 2017.
Kong G, Morean ME, Cavallo D, Camenga DR, Krishnan-Sarin S. Sources of electronic cigarette acquisition among adolescents in Connecticut. Tob Regul Sci. 2017;3(1):10–6.
US FDA. FDA launches new campaign: “the real cost” youth e-cigarette prevention campaign. 2018. https://www.fda.gov/TobaccoProducts/PublicHealthEducation/PublicEducationCampaigns/TheRealCostCampaign/ucm620783.htm.
Funding
Research reported in this publication was supported by grant number P50DA036151, U54DA036151 from the NIDA and FDA Center for Tobacco Products (CTP), and R01CA207229 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tobacco
Rights and permissions
About this article
Cite this article
Bold, K.W., Krishnan-Sarin, S. E-Cigarettes: Tobacco Policy and Regulation. Curr Addict Rep 6, 75–85 (2019). https://doi.org/10.1007/s40429-019-00243-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-019-00243-5