Abstract
Background
Psoriasis is a chronic, inflammatory, T-cell-mediated disease with a multifactorial pathogenesis. MicroRNA (miRNA) alteration in psoriasis has been identified within the last few years. In particular, miR-146a levels were altered. However, previous studies have equivocal or even contradictory findings.
Objective
The current study aimed to perform a systematic review and meta-analysis to evaluate the miRNA expression profile in different tissues in patients with psoriasis. Further, the correlation between miR-146a levels and psoriasis severity as well as the specific expression patterns of the miR-146a profile in patients with psoriasis after treatment were evaluated.
Methods
To retrieve studies investigating the correlation between miRNA and psoriasis, a comprehensive search of databases including PubMed, Cochrane Library, and Embase was performed from inception to 30 June 2023. Relevant journals and references of the included studies were also reviewed. A meta-analysis was conducted using the comprehensive meta-analysis version 3.
Results
The correlation between the miR-146a expression levels and psoriasis susceptibility in 14 studies was assessed. Results showed that the miR-146a expression level was upregulated in psoriasis samples [P = 0.001, standardized mean difference (SMD) = 1.489, 95% confidence interval (CI) = 0.618–2.360]. In a subgroup analysis based on sample type, the correlation between the peripheral blood mononuclear cell, blood, and tissue miR-146a expression level and psoriasis was significant (SMD = 1.293, 95% CI 0.310–2.276, P = 0.01; SMD = 2.526, 95% CI 1.710–3.342, P = 0.000; SMD = 3.153, 95% CI 1.432–4.874, P = 0.00, respectively). A positive correlation was observed between the miR-146a expression levels and Psoriasis Area and Severity Index (PASI) score. However, the result was not statistically significant (correlation coefficient = 0.29, 95% CI − 0.038 to 0.575, P = 0.081). Further, the miR-146a levels decreased after treatment (SMD = − 1.592, 95% CI − 2.067 to − 1.117, P = 0.000, I2 = 74.104).
Conclusions
The miR-146a expression level is positively correlated with and can contribute to the pathobiology of psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
miR-146a was upregulated in psoriasis samples including peripheral blood mononuclear cells (PBMCs), blood, and tissue. |
There was also a positive correlation between miR-146a levels and Psoriasis Area and Severity Index (PASI) score, although without statistical significance and decrease in miR-146a level after treatment. |
1 Introduction
Psoriasis is a chronic, inflammatory, T-cell-mediated skin disease associated with multifactorial immunologic, genetic, and environmental factors [1]. A previous study has shown genetic predisposition to psoriasis. Moreover, microRNAs (miRNAs) have been found to play a role in the pathogenesis of psoriasis [2].
MicroRNAs are small noncoding regulatory RNAs involved in RNA silencing at the post-transcriptional level [3]. Some miRNAs are produced at high concentrations within cells in a tissue-specific manner, and they are stable in the blood. Therefore, they can be promising biomarkers for diagnosis, prognosis, or treatment response [4, 5]. miRNAs control gene expression by targeting messenger RNAs. Hence, they can be potential targets via either miRNA replacement therapy or miRNA function inhibition [6].
Accumulating evidence has revealed that miRNAs have a major contribution in the pathogenesis of cancer and viral, neurodegenerative, and autoimmune diseases [7]. In skin, miRNAs have various effects on the differentiation of keratinocytes, apoptosis, and atypical immune activation [8]. The following miRNAs, either upregulated or downregulated, are associated with psoriasis: miR-21, miR-31, miR-146, miR-155, miR-203, miR-99, miR-125, miR-197, and miR-520 [2].
MiR-146a is a miRNA that negatively regulates innate immunity, inflammatory response, and antiviral pathways [9]. Previous studies established miR-146a as a key regulator in keratinocyte innate immunity through downregulation of the IRAK1/TRAF6/NF-κB pathway following TLR2 stimulation [10]. Also, miR-146a serves as a powerful inhibitor of IL-17-induced skin inflammation, and its diminished levels could potentially contribute to the early onset of disease in genetically predisposed individuals [11].
Several studies have investigated the miR-146a expression in psoriasis. However, the heterogeneity in specimens including PBMCs, blood, and tissue further increased the difficulty in evaluating the risk. Current studies on the miR-146a level in psoriasis have equivocal or even contradictory findings.
This study aimed to perform a systematic review and meta-analysis to evaluate the miRNA expression profile in different tissues in patients with psoriasis. Further, the correlation between the miR-146a levels and psoriasis severity as well as the specific expression patterns of the miR-146a profile in patients with psoriasis after treatment were evaluated.
2 Materials and Methods
The current meta-analysis was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The systematic review and meta-analysis protocols were prospectively registered in PROSPERO (CRD42023456150).
2.1 Literature Search Strategy
To retrieve studies investigating the correlation between miRNA expression levels and psoriasis, a comprehensive search of databases including PubMed, Cochrane Library, and Embase was performed from inception to 30 June 2023. The search terms were: “psoriasis,” “microRNA-146a,” and “miR-146a.” The relevant journals and references of the included studies were also reviewed. Only English language publications and human subject studies were included.
2.2 Inclusion and Exclusion Criteria
The eligible studies included case-control studies on the miRNA-146a expression level of patients diagnosed with psoriasis (case group) and healthy people (control group); studies on the correlation between the miRNA-146a expression level and the Psoriasis Area and Severity Index (PASI) score in patients with psoriasis; and studies on the miRNA-146a expression level before and after psoriasis treatment. All studies provide detailed information about the miRNA expression level. Duplicate publications were excluded. The quality of the studies was evaluated by two investigators (Huang and Ho) using the Newcastle-Ottawa Quality Assessment Scale (NOS) for case-control studies and the Methodological Index for Nonrandomized Studies (MINORS) for case series (Online Supplementary Material (OSM) Tables S1 and S2).
2.3 Outcomes
The primary outcome was the miRNA-146a level between patients with psoriasis and those without (controls). The secondary outcome was the correlation between the miR-146a levels and psoriasis severity and the level of miR-146a alteration after treatment.
2.4 Data Extraction
Two researchers (Huang and Ho) independently conducted literature searches, article screening, data extraction, and quality assessment according to the inclusion and exclusion criteria. The data were compared, and discrepancies were resolved through discussion and consensus, with a third reviewer engaged if needed. The following data were retrieved: author list, year of publication, sample size, specimen origin, detection method, study design, ethnicity, psoriasis severity (Table 1), and miRNA expression level, including mean, standard deviation, and correlation coefficient (Table 2). ImageJ was used for the image processing of miRNA expression levels in articles for which original data were not provided.
2.5 Data Analysis
We produced a pooled estimate of the miRNA-146a level in patients with psoriasis and controls, the correlation between the miRNA-146a level and psoriasis severity, and the miRNA-146a level of patients with psoriasis before and after treatment. Subgroup analyses were stratified according to the different miRNA sample origins: blood (including the plasma and serum), peripheral blood mononuclear cells (PBMCs), and skin tissue.
Continuous data were analyzed using the standardized mean difference (SMD) corresponding to the 95% confidence interval (CI) to manage various and non-standardized outcomes across studies. Correlation analyses were performed using the correlation coefficient (r) with 95% CI. The heterogeneity between studies was examined using the Q test and I2 statistics. The random-effects model was adopted in all analyses because of the high degree of heterogeneity. Publication bias was evaluated using Egger’s test. All analyses were performed using the Comprehensive Meta-Analysis version 3 (Biostat, Inc., Englewood, NJ, USA) software.
3 Results
3.1 Characteristics of the Study
In total, 175 articles were identified from PubMed, Embase, and Cochrane Library. After reviewing the title and abstract, 24 studies were selected for full-text review. Finally, 14 studies [12,13,14,15,16,17,18,19,20,21,22,23,24,25] were included in the meta-analysis (Fig. 1). Table 1 shows the characteristics of the included studies. Of the 14 included studies, 11 were case-control studies and three were case series. Nine studies compared the miRNA-146a expression levels between patients with psoriasis and controls. Seven studies evaluated the miRNA-146a expression levels according to psoriasis severity. Seven studies assessed the miRNA-146a expression levels before and after psoriasis treatment. The miRNA-146a expression level in the PBMC, blood, and skin tissue samples was examined.
3.2 Quality Assessment
The NOS and MINORS scores ranged from 7 to 9 and from 11 to 13, respectively. Points were deducted in the items of comparability based on the design and nonresponse rate in NOS, inclusion of consecutive patients, prospective collection of data, unbiased assessment of the study endpoint, and loss to follow-up (< 5% in MINORS).
3.3 Meta-Analysis Results
Table 3 shows the meta-analyses results.
3.3.1 MiR-146a Expression Between Patients With Psoriasis and Controls
Overall, the meta-analysis of nine studies revealed that patients with psoriasis had an upregulated miR-146a expression level (P = 0.001, SMD = 1.489, 95% CI 0.618, 2.360) based on a pooled analysis using blood and PBMC samples. Tissue samples were excluded initially from the analysis due to the representativity of perilesional for controls. A subgroup analysis was performed on patients with psoriasis using blood, PBMC, and tissue samples. Stratification by adjustment for blood samples revealed that the blood and PBMC miR-146a levels were upregulated (SMD = 1.293, 95% CI 0.310–2.276, P = 0.01; SMD = 2.526, 95% CI 1.710–3.342, P = 0.000, respectively). Stratification by tissue samples showed that the miR-146a levels were upregulated (SMD = 3.153, 95% CI 1.432–4.874, P = 0.00) (Table 3, Fig. 2).
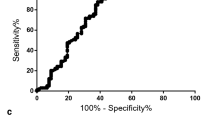
3.3.2 Correlation Between miR-146a Levels and Psoriasis Activity
A meta-analysis of seven studies showed a tendency toward a positive correlation between the miR-146a levels and PASI. However, it did not reach statistical significance (correlation coefficient = 0.29, 95% CI − 0.038 to 0.575, P = 0.081). A meta-analysis was performed on each subgroup using blood, PBMC, and tissue samples.
Stratification by adjustment revealed that the PBMC samples had a significantly higher miR-146a levels than the blood and tissue samples (correlation coefficient = 0.802, 95% CI 0.506–0.929, P = 0.000; correlation coefficient = − 0.002, 95% CI − 0.252 to 0.247, P = 0.986; correlation coefficient = 0.339, 95% CI − 0.048 to 0.638, P = 0.085; respectively) (Table 3, Fig. 3).
3.3.3 MiR-146a Expression Levels Before and After Treatment
A comprehensive meta-analysis of seven studies analyzed the miR-146a expression levels before and after psoriasis-related treatment. Results obtained using the whole data showed that the miR-146a levels decreased after treatment (SMD = − 1.592, 95% CI − 2.067 to − 1.117, P = 0.000, I2 = 74.104). We obtained similar pooled results in the subgroup analyses stratified by blood, PBMC, and tissue samples (SMD = − 1.969, 95% CI − 2.689 to − 1.249, P = 0.000, I2 = 71.160; SMD = − 1.392, 95% CI − 2.322 to − 0.461, P = 0.003, I2 = 84.307; SMD = − 2.338, 95% CI − 3.883 to − 0.792, P = 0.003, I2 = 0.000, respectively) (Table 3, Fig. 4).
3.3.4 Publication Bias
In this meta-analysis, only studies with seven or more articles were included for publication bias analysis. There was no publication bias noted (OSM Figs. S1–S3).
4 Discussion
This study evaluated the correlation between the miR-146a levels and psoriasis susceptibility in 14 studies. Results showed that the miR-146a expression was upregulated in patients with psoriasis. A subgroup analysis based on sample type showed that the correlation between the PBMCs, blood, and tissue miR-146a expression level and psoriasis was significant. A positive correlation was found between the miR-146a levels and PASI score. However, the results were not statistically significant. Further, the miR-146a levels decreased after treatment.
MiRNAs can be found in various human tissues [26]. Blood has been a useful resource in biomedical studies, and the major specimen types include PBMCs and whole blood. Whole blood, which is easy to process and store, is excellent for producing gene expression data with minimal variability and good sensitivity compared with PBMC samples [27]. Whole blood can also accurately reflect miRNA levels in PBMCs and detect changes in autoimmune diseases.
Increasing evidence has revealed that miRNAs play important roles in the development and pathogenesis of various diseases. MiR-146a is an important modulator of cell differentiation in innate and adaptive immunity [28], as well as a potential regulator involved in the pathogenesis of various diseases including cardiac dysfunction and type I /II diabetes [29, 30]. For autoimmune diseases, miR-146a blocked the autocrine IL-6- and IL-21-induced Th17 differentiation pathways in autoreactive CD4 T cells. Autoreactive CD4 T cells that differentiate into pathogenic Th17 cells trigger downstream autoimmunity [31] Moreover, miR-146a is expressed in Treg cells, and it regulates the suppressive function of Treg cells. The deficiency of miR-146a resulted in a breakdown of immunological tolerance [32].
In a cutaneous model, miR-146a targets the expression of the IRAK1 gene and suppresses the innate immune response in keratinocytes by decreasing Toll-like receptors-dependent epidermal inflammation and further reducing the activation of the nuclear factor kappa-light-chain-enhancer of activated B-cell pathway [33]. IRAK1 deletion decreased the interleukin-17 expression and suppressed inflammatory responses in acute and chronic inflammatory mouse models [34]. The expression of miR-146a is elevated in keratinocytes and chronic skin inflammation of atopic dermatitis, with a suppressive effect on allergic skin inflammation by directly targeting upstream nuclear factor kappa B signal transducers [35].
With regard to the genetics of psoriasis, there was a distinct miRNA expression profile in psoriatic skin compared to healthy skin, highlighting the overexpression of miR-146a that regulated inflammation and the proliferation of keratinocytes in psoriatic skin lesions [36]. miR-146a was ±twofold differentially expressed in psoriatic skin compared to normal skin according to microarray studies in human skin biopsies [37]. Hence, miR-146a can be a biomarker and therapeutic target in clinical settings.
Further research must be performed to evaluate whether miR-146a upregulation in psoriasis is a compensatory mechanism in response to exacerbated inflammatory response. Moreover, the upregulation of miR-146a enhanced immune suppression by increasing the regulatory T-cell population. Hence, further studies must be conducted to evaluate its role as a possible therapeutic target.
5 Limitations
This meta-analysis aimed to assess the correlation between the miR-146a level and psoriasis susceptibility using a larger sample size and higher statistical capacity. The current study had several limitations. First, the samples (blood, PBMC, and tissue) were diverse. We have already done subgroup analysis in the three different samples; however, it should be noted that due to the limited amount of data available, we were unable to further distinguish between serum and plasma samples within the blood category for statistical analysis. Secondly, although 14 studies were included, not all studies provided information on the severity of psoriasis, and the treatments were not standardized. These confounding factors led to significant statistical heterogeneity in our observations. Variations in miR-146a expression levels, influenced by factors such as age, sex, other medical conditions, or the presence of specific polymorphisms, may also contribute to this heterogeneity. However, due to limited information, we were unable to conduct further subgroup analysis or meta-regression. Due to the limited quantity and quality of the included studies, large, well-designed studies should be performed to further validate the conclusions of this study.
6 Conclusion
miR-146a upregulation is associated with psoriasis susceptibility. Furthermore, miR-146a is a potent marker for predicting the clinical severity and treatment outcome of psoriasis. Nevertheless, further clinical investigations with larger sample sizes should be performed to validate our results.
References
Vičić M, Kaštelan M, Brajac I, Sotošek V, Massari LP. Current concepts of psoriasis immunopathogenesis. Int J Mol Sci. 2021;22(21):11574. https://doi.org/10.3390/ijms222111574.
Timis TL, Orasan RI. Understanding psoriasis: role of miRNAs. Biomed Rep. 2018;9:367–74. https://doi.org/10.3892/br.2018.1146.
O’Brien J, Hayder H, Zayed Y, et al. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne). 2018;9:402. https://doi.org/10.3389/fendo.2018.00402.
Lagos-Quintana M, Rauhut R, Yalcin A, et al. Identification of tissue-specific microRNAs from mouse. Curr Biol. 2002;12:735–9. https://doi.org/10.1016/s0960-9822(02)00809-6.
Mitchell PS, Parkin RK, Kroh EM, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA. 2008;105:10513–8. https://doi.org/10.1073/pnas.0804549105.
Rupaimoole R, Slack FJ. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov. 2017;16:203–22. https://doi.org/10.1038/nrd.2016.246.
Li Y, Kowdley KV. MicroRNAs in common human diseases. Genom Proteom Bioinf. 2012;10:246–53. https://doi.org/10.1016/j.gpb.2012.07.005.
Ross K. Towards topical microRNA-directed therapy for epidermal disorders. J Control Rel. 2018;269:136–47. https://doi.org/10.1016/j.jconrel.2017.11.013.
Li L, Chen XP, Li YJ. MicroRNA-146a and human disease. Scand J Immunol. 2010;71:227–31. https://doi.org/10.1111/j.1365-3083.2010.02383.x.
Meisgen F, Xu Landén N, Wang A, et al. MiR-146a negatively regulates TLR2-induced inflammatory responses in keratinocytes. J Invest Dermatol. 2014;134(7):1931–40. https://doi.org/10.1038/jid.2014.89.
Srivastava A, Nikamo P, Lohcharoenkal W, et al. MicroRNA-146a suppresses IL-17-mediated skin inflammation and is genetically associated with psoriasis. J Allergy Clin Immunol. 2017;139(2):550–61. https://doi.org/10.1016/j.jaci.2016.07.025.
Xia P, Fang X, Zhang ZH, et al. Dysregulation of miRNA146a versus IRAK1 induces IL-17 persistence in the psoriatic skin lesions. Immunol Lett. 2012;148:151–62. https://doi.org/10.1016/j.imlet.2012.09.004.
Koga Y, Jinnin M, Ichihara A, et al. Analysis of expression pattern of serum microRNA levels in patients with psoriasis. J Dermatol Sci. 2014;74:170–1. https://doi.org/10.1016/j.jdermsci.2014.01.005.
Ele-Refaei AM, El-Esawy FM. Effect of narrow-band ultraviolet B phototherapy and methotrexate on MicroRNA (146a) levels in blood of psoriatic patients. Dermatol Res Pract. 2015;2015: 145769. https://doi.org/10.1155/2015/145769.
Raaby L, Langkilde A, Kjellerup RB, et al. Changes in mRNA expression precede changes in microRNA expression in lesional psoriatic skin during treatment with adalimumab. Br J Dermatol. 2015;173:436–47. https://doi.org/10.1111/bjd.13721.
Yang Z, Zeng B, Tang X, et al. MicroRNA-146a and miR-99a are potential biomarkers for disease activity and clinical efficacy assessment in psoriasis patients treated with traditional Chinese medicine. J Ethnopharmacol. 2016;194:727–32. https://doi.org/10.1016/j.jep.2016.08.028.
Hermann H, Runnel T, Aab A, et al. miR-146b probably assists miRNA-146a in the suppression of keratinocyte proliferation and inflammatory responses in psoriasis. J Invest Dermatol. 2017;137:1945–54. https://doi.org/10.1016/j.jid.2017.05.012.
Mensà E, Recchioni R, Marcheselli F, et al. MiR-146a-5p correlates with clinical efficacy in patients with psoriasis treated with the tumour necrosis factor-alpha inhibitor adalimumab. Br J Dermatol. 2018;179:787–9. https://doi.org/10.1111/bjd.16659.
Leal B, Carvalho C, Ferreira AM, et al. Serum levels of miR-146a in patients with psoriasis. Mol Diagn Ther. 2021;25:475–85. https://doi.org/10.1007/s40291-021-00531-9.
Chen L, Li J, Yao Y, et al. Circulating microRNA profile unveils mechanisms of action of acitretin for psoriasis vulgaris. Bioengineered. 2021;12:1838–50. https://doi.org/10.1080/21655979.2021.1925205.
Gu DC, Cheng MJ, Feng JR. Expression of miR-155 and miR-146a in skin tissue, peripheral blood mononuclear cells and serum of patients with psoriasis and its clinical significance. Adv Biosci Biotechnol. 2022;13:207–15.
Carreras-Badosa G, Maslovskaja J, Vaher H, et al. miRNA expression profiles of the perilesional skin of atopic dermatitis and psoriasis patients are highly similar. Sci Rep. 2022;12:22645. https://doi.org/10.1038/s41598-022-27235-2.
Shen H, Wang D, Zhan M, Ding H, et al. MicroRNA-146a and microRNA-146b deficiency correlates with exacerbated disease activity, and their longitude increment relates to etanercept response in psoriasis patients. J Clin Lab Anal. 2022;36: e24198. https://doi.org/10.1002/jcla.24198.
Uzun L, Kutlu R, Ataseven A, et al. Total oxidant capacity, total antioxidant capacity, ischemic modified albumin, microRNA levels, and their relationship with psoriasis area and severity index. Indian J Dermatol Venereol Leprol. 2023;89:501–9. https://doi.org/10.25259/IJDVL_111_2022.
Diotallevi F, Matacchione G, d’Agostino GM, et al. InflammamiR-146a and -155 plasma levels are associated with clinical efficacy of risankizumab treatment in psoriatic patients: pilot study. Dermatol Ther (Heidelb). 2023;13:1377–87.
Liang Y, Ridzon D, Wong L, et al. Characterization of microRNA expression profiles in normal human tissues. BMC Genom. 2007;8:166. https://doi.org/10.1186/1471-2164-8-166.
He D, Yang CX, Sahin B, et al. Whole blood vs PBMC: compartmental differences in gene expression profiling exemplified in asthma. Allergy Asthma Clin Immunol. 2019;15:67. https://doi.org/10.1186/s13223-019-0382.
Rusca N, Monticelli S. MiR-146a in immunity and disease. Mol Biol Int. 2011;2011: 437301. https://doi.org/10.4061/2011/437301.
Ghaffari M, Razi S, Zalpoor H, et al. Association of MicroRNA-146a with type 1 and 2 diabetes and their related complications. J Diabetes Res. 2023;2023:2587104. https://doi.org/10.1155/2023/2587104.
Heggermont WA, Papageorgiou AP, Quaegebeur A, et al. Inhibition of MicroRNA-146a and overexpression of its target dihydrolipoyl succinyltransferase protect against pressure overload-induced cardiac hypertrophy and dysfunction. Circulation. 2017;136:747–61. https://doi.org/10.1161/CIRCULATIONAHA.116.024171.
Li B, Wang X, Choi IY, et al. miR-146a modulates autoreactive Th17 cell differentiation and regulates organ-specific autoimmunity. J Clin Invest. 2017;127:3702–16. https://doi.org/10.1172/JCI94012.
Lu LF, Boldin MP, Chaudhry A, et al. Function of miR-146a in controlling Treg cell-mediated regulation of Th1 responses. Cell. 2010;142:914–29. https://doi.org/10.1016/j.cell.2010.08.012.
Guo Q, Zhang J, Li J, et al. Forced miR-146a expression causes autoimmune lymphoproliferative syndrome in mice via downregulation of Fas in germinal center B cells. Blood. 2013;121:4875–83. https://doi.org/10.1182/blood-2012-08-452425.
Maitra U, Davis S, Reilly CM, et al. Differential regulation of Foxp3 and IL-17 expression in CD4 T helper cells by IRAK-1. J Immunol. 2009;182:5763–9. https://doi.org/10.4049/jimmunol.0900124.
Rebane A, Runnel T, Aab A, et al. MicroRNA-146a alleviates chronic skin inflammation in atopic dermatitis through suppression of innate immune responses in keratinocytes. J Allergy Clin Immunol. 2014;134(4):836-847.e11. https://doi.org/10.1016/j.jaci.2014.05.022.
Sonkoly E, Wei T, Janson PC, et al. MicroRNAs: novel regulators involved in the pathogenesis of psoriasis? PLoS ONE. 2007;2(7):e610. https://doi.org/10.1371/journal.pone.0000610.
Joyce CE, Zhou X, Xia J, et al. Deep sequencing of small RNAs from human skin reveals major alterations in the psoriasis miRNAome. Hum Mol Genet. 2011;20:4025–40. https://doi.org/10.1093/hmg/ddr331.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No financial assistance was used to conduct the study described in the article or used to assist with the preparation of the manuscript. There was no sponsor for the open access fee.
Conflicts of interest
Pei-Yun Ho and Yu-Chen Huang declare that they have no conflicts of interest that might be relevant to the contents of this article.
Ethics approval
Not applicable.
Consent
Not applicable.
Author contributions
PYH and YCH were responsible for study design. PYH was responsible for assembly of data, data interpretation”, and manuscript draft preparation. YCH was responsible for the interpretation and final version of the manuscript.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ho, PY., Huang, YC. MicroRNA-146a Signature in Psoriasis: A Systematic Review and Meta-Analysis. Mol Diagn Ther 28, 379–388 (2024). https://doi.org/10.1007/s40291-024-00714-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-024-00714-0