Abstract
Background
Psoriasis is an immune-mediated disease with interactions between genetic and environmental factors. An increasing number of studies are demonstrating the importance of microRNAs (miRNAs) in the pathogenesis of psoriasis. miR-146a, a dominant negative regulator of inflammation, has been consistently reported as overexpressed in the skin and peripheral blood mononuclear cells (PBMCs) of patients with psoriasis. Expression and/or function of this miRNA is highly influenced by genetic variations, some of which have already been associated with susceptibility to psoriasis.
Objective
We sought to study the importance of miR-146a in patients with moderate-to-severe psoriasis and to understand the impact of rs57095329 and rs2910164 polymorphisms in a psoriatic Portuguese population.
Methods
miR-146a circulating levels were quantified using molecular biology techniques in 99 patients with moderate-to-severe psoriasis (35 female, 64 male; age 47.4 ± 10.9 years) and 78 healthy individuals (52 female, 26 male; age 42.4 ± 10.1 years). miRNA expression was correlated with clinicopathological features as well as with genetic data such as the presence of human leukocyte antigen (HLA)-C*0602 allele and two miR-146a polymorphisms (rs2910164 and rs57095329).
Results
miR-146a serum levels were 3.7-fold higher in patients with psoriasis than in controls (p < 0.0001, area under the curve [AUC] 0.75; 95% confidence interval [CI] 0.66–0.83). Of note, miR-146a circulating levels positively correlated with Psoriasis Area and Severity Index (p < 0.05) and body surface area (p < 0.05) indexes. No variations in miR-146a levels were observed with rs2910164 and rs57095329 genotypes.
Conclusion
Circulating miR-146a levels were upregulated in patients with psoriasis, especially in those with active disease. To the best of our knowledge, this is the largest study with a homogenous psoriasis population, and our data could shed light on the pathogenesis of psoriasis, paving the way for new avenues for disease treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Circulating levels of microRNA (miR)-146a are upregulated in patients with psoriasis compared with controls. |
miR-146a circulating levels are positively correlated with Psoriasis Area and Severity Index and body surface area indexes. |
miR-146a levels did not vary with rs2910164 and rs57095329 polymorphisms, suggesting that the upregulation could be a reflex of the ongoing inflammatory process. |
1 Introduction
Psoriasis is a chronic inflammatory skin disease that is mediated by crosstalk between keratinocytes, dermal vascular cells, immune cells, and inflammatory mediators. Psoriasis affects 2–3% of the population worldwide [1] and is often associated with several comorbidities, such as obesity, atherosclerosis, and depression [2]. The disease impacts strongly on patients’ quality of life and places major direct and indirect costs on health systems [3, 4].
The pathogenesis of psoriasis is not yet fully understood. Evidence points towards an immune-mediated origin with complex interactions between genetic and environmental factors [5]. A strong genetic component has been highlighted by twin and family studies, demonstrating a 60–90% heritability rate [6,7,8]. It is now well-established that this heritability follows a multifactorial pattern, with concordance rates in monozygotic and dizygotic twins estimated to be 63–73% and 5%, respectively [6, 8]. Linkage, genome-wide, and candidate genes studies have found more than 80 loci linked to susceptibility to psoriasis, with many genes mainly associated with innate and adaptive immune system and skin barrier functions [8,9,10]. It is widely acknowledged that the human leukocyte antigen (HLA)-C*06:02 allele is the major risk factor for psoriasis [11]. Nevertheless, this allele accounts only for 35–50% of genetic susceptibility. Additional susceptibility factors remain to be identified, but gene–gene and, more importantly, gene–environment interactions highlight the role of epigenetic mechanisms in the aetiopathogenesis of psoriasis [12, 13].
Epigenetic mechanisms, such as DNA methylation, non-coding RNA molecules, or histone modification, can change gene expression without modification in the DNA sequence [14]. These mechanisms regulate multiple aspects of chromatin structure and function, allowing transcriptionally repressive or permissive configurations for gene expression [14]. This leads to a modified genome read, producing a different gene expression profile. An increasing number of studies have demonstrated the importance of epigenetics in the pathogenesis of psoriasis [15], with microRNAs (miRNAs) having a prominent role [16].
miRNAs are short non-coding RNA molecules (19–25 nucleotide length) that act as post-transcriptional regulators of gene expression [17]. This is accomplished through messenger RNA (mRNA) degradation or inhibition of its translation [17]. The net effect is the downregulation of protein synthesis, controlling the homeostasis of different biological processes with a significant impact in the immune system. One important feature of these molecules is the ability of one single miRNA to modulate distinct genes from the same or different pathways [18]. Additionally, one mRNA molecule can have several binding sites for different miRNAs [18].
Several genome-wide and targeted studies have described more than 100 different miRNAs that are dysregulated in patients with psoriasis, and these are linked to various key disease-associated pathways, such as those that include the innate and adaptive immune system, angiogenesis, and the processes of cell proliferation, migration, and apoptosis [16, 19,20,21,22,23].
miR-146a, a dominant negative regulator of inflammation, has been consistently reported as overexpressed in skin and peripheral blood mononuclear cells (PBMCs) of patients with psoriasis [24,25,26,27]. Polymorphisms affecting expression and function of miR-146a have been described as susceptibility factors for several autoimmune diseases, including psoriasis [28,29,30]. rs2910164 and rs57095329 polymorphisms have been proven to affect miR-146a expression [31, 32] with a negative impact on the modulation of the immune response [31] and skin metabolism, explaining its association with psoriasis [29, 30].
These results suggest that miR-146a could be a potential psoriasis biomarker. miRNAs are very stable in biological fluids, where their concentration is thought to reflect tissue production.
In this context, our aim was to evaluate the role of miR-146a in patients with psoriasis, analyse its circulating levels, and assess the impact of rs2910164 and rs57095329 polymorphisms in a Portuguese population.
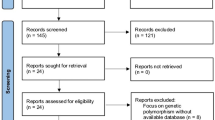
2 Material and Methods
2.1 Population Characteristics
Data from a cohort of 99 adult patients with moderate-to-severe plaque-type psoriasis followed in the Dermatology Centre of Centro Hospitalar Universitário do Porto (CHUP) were analysed. Exclusion criteria included the presence of psoriatic arthritis (previous/current signs and symptoms of joint involvement); the presence of other concomitant systemic inflammatory diseases, such as lupus erythematous, rheumatoid arthritis, or other spondyloarthropathies; or receiving treatment with systemic therapeutic options other than biologic agents. All subjects underwent a complete clinical evaluation that included a systematic physical examination and anamnesis. Individuals were asked about their demographics, disease characteristics, and comorbidities. Disease activity and severity were evaluated using the Psoriasis Area and Severity Index (PASI) score and body surface area (BSA).
The control population comprised 78 healthy individuals (52 female, 26 male; age 42.4 ± 10.1 years) voluntarily recruited among blood donors, ethnically matched, and from the same geographical area. This population was asked whether they had multiple diseases, and individuals with autoimmune diseases or a positive familial history of these pathologies were not included in our control cohort. The study was approved by the hospital Institutional Ethical Committee, and each subject’s written consent was obtained according to the Helsinki Declaration.
2.2 RNA Extraction from Serum
Peripheral blood samples were collected in Vacuette tubes, centrifuged at 490 g for 20 min, and serum aliquots were stored at − 20 °C. Samples that were processed more than 4 h post-collection were excluded. Haemolysis was visually evaluated based on the sample colour. Any sample with signs of haemolysis (with an orange to red tinge) was assessed via spectrophotometric analysis using a Nanodrop 2000 spectrophotometer. Samples with an absorbance at 414 nm ≥ 0.2 were excluded from the study because of the possibility of haemolysis. RNA was extracted using the miRNeasy® Serum/Plasma Kit (Qiagen, Germany), according to the manufacturer’s protocol.
2.3 MicroRNA Relative Quantification by Quantitative Real-Time Polymerase Chain Reaction
Five nanograms of RNA were converted to complementary DNA (cDNA) using the Taqman® MicroRNA Reverse Transcription kit (4366597; Applied Biosystems, Foster City, CA, USA) and Taqman® MicroRNA Assays (000468, Applied Biosystems). The reaction was performed in a Biometra Alfagene thermocycler according to the manufacturer’s instructions. The quantitative real-time polymerase chain reaction (qRT-PCR) amplification was run with an NzySpeedy qPCR mastermix (Nzytech, Portugal) in a Corbett Rotor Gene 600 real-time thermocycler (Corbett Research, Concorde, New South Wales, Australia). One µL of cDNA was used per reaction, and triplicates were run for each sample. miR-146a levels were evaluated in serum, a cell-free body fluid that has no known RNA species at constant levels that could be used as housekeeping genes for normalization [33]. Briefly, to overcome this issue, reaction conditions for miRNA expression analysis used serum sample volumes that were constant and uniform throughout all assays, and the same baseline and threshold cycle was set, so that expression levels could be comparable between samples. miRNAs levels are expressed as individual 50-Ct arbitrary units [33].
2.4 DNA Extraction and Genotyping
Peripheral blood samples (10 ml) were collected in 5% ethylenediaminetetraacetic acid (EDTA) tubes. Genomic DNA was obtained from proteinase-K-treated peripheral blood leukocytes using a salting-out procedure as previously described [21]. The rs2910164 and rs57095329 polymorphisms were genotyped using a pre-designed TaqMan allelic discrimination assay (C_15946974_10 and C_90078480_10, respectively; Applied Biosystems) and NzySpeedy qPCR mastermix (Nzytech) in a Rotor Gene 6000 RT-PCR machine (Corbett Life Science). HLA-C locus was genotyped using sequence-specific PCR based on previously described primer sequences [34]. PCR products were separated by electrophoresis on 1.5 % agarose gel containing ethidium bromide and visualized under ultraviolet light.
2.5 Statistical Analysis
Descriptive statistics are given as frequencies (n) and percentages for categorical variables and as means with standard deviations for continuous variables. Relative expression was calculated using the 2–ΔΔCT method [35]. Differences in ΔCt were evaluated using a two-tailed Student’s t-test or Mann–Whitney test as appropriate. Normal distribution was tested using the Kolmogorov–Smirnov method. Pearson’s correlation coefficients were used to evaluate interactions between disease duration, PASI, BSA, and miR-146a circulating levels. Differences between groups were tested using the one-way analysis of variance (ANOVA) test. Receiver operating characteristic (ROC) curves and area under the curve (AUC) were calculated to evaluate the diagnostic value of circulating miR-146a. Hardy–Weinberg equilibrium was tested. Statistical analysis was performed with SPSS (Statistical Package for the Social Sciences; IBM, Armonk, NY, USA) software version 26.0. Graphs were developed with GraphPad Prism 7.01. Significance levels were set at p < 0.05 for all statistical analysis.
3 Results
We analysed a cohort of 99 patients with active plaque psoriasis, with a mean age of 47.4 ± 10.9 years and a male predominance (n = 64). The mean disease duration was 22.5 ± 10.9 years. In total, 44% of the patients were positive for the susceptibility allele HLA-C*06:02 (HLA-C*06:02POS). Anthropometric measurements were evaluated, and the mean body mass index was 28.5 ± 5.4 kg/m2. Regarding disease severity, the mean PASI score was 13.3 ± 9.6 and the mean BSA was 13.0% ± 8.3%. Patients with psoriasis receiving biologic therapy (PsO-Bio) had very low disease activity, with PASI and BSA indexes of 2.42 ± 2.28 and 2.35% ± 2.21%, respectively. None of the PsO-Bio patients had diabetes, but 67% had hypertension and 50% dyslipidaemia. On the other hand, patients receiving no systemic therapeutics (PsO-NoSys) had more severe disease, with mean PASI and BSA values of 16.1 ± 10.3 and 16.9% ± 13.6%, respectively (Table 1). Hypertension and dyslipidaemia were reported in 47 and 61% of these patients, respectively (see Table 1 for further details).
Circulating miR-146a levels were 3.2-fold higher in patients with psoriasis than in controls (p < 0.0001; Fig. 1a). ROC curve analysis showed an AUC of 0.75 (95% confidence interval [CI] 0.68–0.83; p < 0.0001), with specificity and sensitivity of 76 and 60%, respectively (Fig. 1b). As the gender distribution in the control population and patient cohort was statistically significant, with a clear predominance of males in the psoriasis group (65 vs. 45%; p = 0.05), we wondered whether these could affect miR-146a levels. No differences in miR-146a levels were observed between males and females in the psoriasis and control populations (p = not significant; Fig. 1c). We also verified that the differences in miR-146a levels between patients and controls remained statistically significant even when the analysis was adjusted for gender (p < 0.0001).
miR-146a serum levels in patients with psoriasis and controls. a Circulating miR-146a levels are threefold higher in patients with psoriasis than in controls; b receiver operating characteristic curve analysis shows that miR-146a has a good diagnostic value in the comparison between patients and controls. c No differences are observed in miR-146a with gender. miR microRNA, PsO psoriasis
This difference was more pronounced in HLA-C*06:02POS patients, who had 3.8-fold higher miR-146a levels than controls (p < 0.05; Fig. 2a). In HLA-C*06:02-negative (HLA-C*06:02NEG) patients, miR-146a circulating levels were 3.0 higher than in controls (p < 0.05; Fig. 2a). No statistically significant differences were observed in miR-146 levels when comparing the two subgroups of patients (Fig. 2a).
miR-146a serum levels in controls and psoriasis subgroups. a HLA-C*06:02-positive patients have numerically higher miR-146a circulating levels than HLA-C*06:02-negative patients and controls; patients treated with biologic therapy have numerically lower miR-146a circulating levels than patients not receiving systemic therapeutics. b miR-146a levels are correlated with PASI index; c miR-146a is positively correlated with body surface area index. BSA body surface area, HLA human leukocyte antigen, miR microRNA, NEG negative, PASI Psoriasis Area and Severity Index, POS positive, PsO-Bio patients with psoriasis receiving biologic therapy, PsO-NoSys patients with psoriasis not receiving systemic therapeutics
Circulating miR-146a levels were positively correlated with the disease activity scores PASI (p < 0.05; r = 0.202; Table 2, Fig. 2b) and BSA (p < 0.05; r = 0.223; Table 2, Fig. 2c). No correlations were observed between circulating miR-146a levels and age at onset or disease duration (see Table 2 for further details). To further verify the correlation with disease activity, miR-146a levels were compared between PsO-Bio (with a lower disease activity) and PsO-NoSys patients (with a higher disease activity). miR-146a levels were 2.9-fold higher in Pso-Bio patients than in controls (p < 0.05; Fig. 2b), whereas PsO-NoSys patients had 3.3-fold higher miR-146a levels than controls (p < 0.0001; Fig. 2b). Although PsO-NoSys patients had higher circulating miR-146a levels than PsO-Bio patients, the difference did not reach statistical significance, probably because of the small number of individuals in each group (Fig. 2a).
rs2910164 (GG 59.4%, GC 33.7%, CC 7.0%; G 76.2%, C 23.8%) and rs57095329 (AA 91.1%, AG 8.9%, GG 0.0%, A 95.6%, G 4.4%) frequencies were in Hardy–Weinberg equilibrium. miR-146a serum levels were compared between the different genotypes with one-way ANOVA or the Mann–Whitney test as appropriate. No significant differences were observed between the different rs2910164 and rs57095329 genotypes in the psoriasis and control populations (p = not significant; Fig. 3a, b, respectively).
4 Discussion
Psoriasis is a prevalent skin disease associated with several comorbidities and decreased quality of life [7]. Affected patients are often subject to stigmatization, which contributes to the development of psychiatric disorders such as depression or suicidal behaviour [2, 4]. Diagnosis is mainly clinical, and its severity is measured using several tools, such as the PASI and BSA or Dermatology Life Quality Index, which evaluates the impact of the disease on patients’ quality of life. There is a high variability in the application of these scores, which makes it essential to identify reliable and stable biomarkers to be able to predict disease course and progression as well as response to different therapeutic options [2, 4]. The discovery of these biomarkers for psoriasis would allow a better understanding of the molecular mechanisms underlying its development and may eventually lead to the design of new treatment approaches.
miRNA are appealing candidates as psoriasis biomarkers because of their stability in serum and the speed, low cost, and non-invasiveness of the analytic process. In psoriasis, circulating miRNAs have only been analysed with small cohorts of patients [22, 24,25,26,27, 36, 37]. miR-146a is one of the most studied miRNAs in psoriasis and is generally found to be upregulated in skin lesions and PBMCs [24,25,26,27]. We also found higher circulating levels of miR-146a in patients with psoriasis. Taken together, these findings suggest that miR-146a could play a role in the development and progression of psoriasis. It has been argued that the miR-146a upregulation in psoriasis is a compensatory mechanism to overcome the exacerbated inflammatory response caused by upregulation of interleukin (IL)-17 [26]. In accordance with this hypothesis, it has been observed that miR-146a and IL-17 expression in psoriatic skin lesions are positively correlated [27]. An initial insult (environmental triggers, loss of tolerance) will lead to the activation of dendritic cells and IL-23-dependent production of IL-17, inducing keratinocyte proliferation [38,39,40]. Keratinocytes also produce several chemokines, such as IL-8, leading to the recruitment of IL-17-producing cells, such as neutrophils and other immune cells to lesion sites, further promoting both inflammation and epidermal hyperplasia [5]. In this way, a feed-forward loop in which exacerbated inflammation is driven by keratinocyte hyperproliferation is established [5]. miR-146a is a dominant regulator of inflammation that acts on a negative feedback loop [20, 41]. The activation of pro-inflammatory signalling pathways stimulates miR-146a expression that will inhibit inflammatory response downstream effectors, such as IL-1 receptor-associated kinase (IRAK1), IRAK2, and tumour necrosis factor (TNF) receptor-associated factor-6, dampening the inflammatory signalling pathway [42,43,44]. As a pleiotropic molecule, miR-146a also modulates other key players of psoriasis pathogenesis [4]. Experimental studies have shown that miR-146a modulates IL-8 expression, impacting on neutrophil migration to the lesion [26]. Cell transfection experiments have shown that miR-146a also regulates epidermal growth factor receptor expression, controlling keratinocyte proliferation [26, 28]. Studies in animal models have observed that miR-146a inhibition is associated with earlier psoriasis development [26]. Moreover, such animals developed a more severe and prolonged disease with exacerbated skin inflammation, epidermal hyperproliferation, and development of thicker lesions [26].
Despite the lower correlation coefficient, linked to high data variability and a lower number of patients in each group, we observed that higher PASI scores were correlated with higher circulating miR-146a levels, further supporting the compensatory role of this miRNA in psoriasis inflammation. Furthermore, HLA-C*06:02POS patients, who reportedly have more severe and active disease [45, 46], presented higher circulating miR-146a levels in our study. These findings are also supported by clinical studies demonstrating that therapeutic inhibition of inflammation is accompanied by a reduction in miR-146a expression in both plasma and PBMCs [24]. Interestingly, our study demonstrated that PsO-Bio patients had numerically lower circulating miR-146a levels. Although our results must be interpreted carefully, it can open new perspectives in the search for psoriasis diagnostic/prognostic biomarkers. To consolidate the data, further validation studies in larger and homogeneous cohorts are warranted. Also, to prove specificity, circulating miR-146a levels should be evaluated in a group of patients with other skin diseases such as atopic dermatitis.
Our data suggest that miR-146a upregulation in psoriasis may be a physiological response to counteract the amplified epidermal activation and consequent exacerbated skin inflammation. The continuous inflammatory process in psoriatic skin indicates that miR-146a is not sufficient to totally suppress the triggers of psoriasis. One possible explanation is that other mediators override the miR-146a-suppressive effect. It is also possible that functional defects in target miRNAs could affect the inhibitory action of miR-146a. The tight regulation of a gene is the result of cooperation between several miRNAs, and its action may depend on the presence of other molecules. Accordingly, other miRNAs are described as cooperating with miR-146a to counteract keratinocyte-induced inflammation [47].
A recent meta-analysis described the rs2910164 polymorphism as a susceptibility factor for the development of psoriasis [29]. rs2910164 can also impact on miR-146a expression with different regulatory effects according to the cellular environments and the underlying complex interactions and regulatory mechanisms. A direct functional effect of this polymorphism has been proven as cells transfected with the rs2910164G allele showed a weaker inhibitory effect on human keratinocytes [28]. It has also been described that rs2910164CC patients have higher epidermal miR-146a expression than rs2910164GG patients [26]. Genetic association studies have presented contradictory results. The rs2910164C allele has been described as a susceptibility factor for psoriasis development in a South African Indian population [48]. On the other hand, in the largest association study performed so far, Srivastava et al. [26] observed that the rs2910164C allele was protective against early psoriasis development. In a Chinese population, rs2910164G carriers had a higher risk of psoriasis development [28]. Chatzikyriakidou et al. [49] and Maharaj et al. [48] did not observe an association between this polymorphism and psoriatic arthritis development in Caucasian populations. Discrepant results are very common in the study of complex diseases and can be explained by population differences in allele prevalence. Discrepancies may also be due to differences in phenotype definition with inclusion of different phenotypes, disease heterogeneity, and limited sample sizes and consequent lack of statistical power. In our cohort, the rs2910164 genetic and allelic frequencies were similar to the frequencies for Caucasian populations described in the literature (allelic frequency rs29101642C: 20–36%).
To the best of our knowledge, the link between psoriasis development and rs57095329 has not yet been addressed. It has been described that the rs57095329G risk allele has a very low frequency in Caucasian populations, as observed in our population. This polymorphism has been shown to decrease miR-146a expression levels, which could justify its association with the development of autoimmune diseases [39].
In this study, no variations in miR-146a circulating levels with the rs2910164 or rs57095329 genotypes were found, suggesting that it was not genetically determined.
5 Study Limitations and Conclusions
We have observed that serum miR-146a is upregulated in patients with psoriasis, especially in those with active disease. These results must be considered in light of some limitations. miR-146a is highly associated with inflammation, which is a common hallmark in diverse pathological states. Therefore, the specificity of miR-146a upregulation should be assessed in additional control populations and encompassing other skin diseases in which inflammation may also be relevant. Although the upregulation of miR-146a has been extensively described, especially in skin biopsies, this is, to the best of our knowledge, the largest study in serum (the most appealing biological source in the search for biomarkers). We also studied a homogeneous cohort of patients with psoriasis without evidence of articular/joint involvement, limiting the possible effects of confounding clinical/inflammatory factors.
It is thought that psoriasis medication significantly influences epigenetics. This has been mainly associated with chromatin-related epigenetic alterations, but some evidence has also indicated an effect on miRNAs. We have demonstrated that the beneficial effect of biologic therapy is accompanied by a reduction in circulating miR-146a levels. Nevertheless, these results should be interpreted carefully as the number of treated patients included was relatively small. The effect of therapy on miRNA levels in patients with psoriasis should be further analysed to understand the dynamics of these variations in larger psoriasis groups.
The link between miR-146a and the development of psoriasis has already been described, with studies showing that polymorphisms in the promoter region of miR-146a gene may be a genetic susceptibility factor for psoriasis development and clinical disease expression. We did not perform a genetic association study as we had a limited sample size with a consequent lack of statistical power to detect the small genetic effects common in complex diseases, such as psoriasis, that arise from the interaction of several genes with additional environmental factors. Nevertheless, we have shown that miR-146a circulating levels did not vary with rs2910164 or rs57095329 polymorphisms. This argues in favour of the hypothesis that miR-146a overexpression in psoriasis may not be genetically determined but instead a reflex of the ongoing inflammatory process. Further studies with larger cohorts would help increase understanding of the contribution of these genetic variations for psoriasis development.
miRNAs are extremely pleiotropic molecules, capable of regulating and being regulated by multiple mechanisms. Further studies to clarify the signalling pathways targeted by overexpressed miR-146a are warranted. The identification and characterization of these pathways would be a major advance in the understanding of the molecular mechanisms that drive psoriasis immune dysregulation. Ultimately, this would allow the identification of new drug targets and eventually the development of RNA-based therapies.
References
Christophers E. Psoriasis—epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26(4):314–20. https://doi.org/10.1046/j.1365-2230.2001.00832.x.
Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: Psoriasis comorbidities and preferred systemic agents. J Am Acad Dermatol. 2019;80(1):27–40. https://doi.org/10.1016/j.jaad.2018.06.057.
Mustonen A, Mattila K, Leino M, Koulu L, Tuominen R. Psoriasis causes significant economic burden to patients. Dermatol Ther (Heidelb). 2014;4(1):115–24. https://doi.org/10.1007/s13555-014-0053-2.
Tampa M, Sarbu MI, Mitran MI, Mitran CI, Matei C, Georgescu SR. The pathophysiological mechanisms and the quest for biomarkers in psoriasis, a stress-related skin disease. Dis Mark. 2018;2018:5823684. https://doi.org/10.1155/2018/5823684.
Hawkes JE, Chan TC, Krueger JG. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017;140(3):645–53. https://doi.org/10.1016/j.jaci.2017.07.004.
Capon F. The genetic basis of psoriasis. Int J Mol Sci. 2017. https://doi.org/10.3390/ijms18122526.
Greb JE, Goldminz AM, Elder JT, Lebwohl MG, Gladman DD, Wu JJ, et al. Psoriasis. Nat Rev Dis Prim. 2016;2:16082. https://doi.org/10.1038/nrdp.2016.82.
Mahil SK, Capon F, Barker JN. Genetics of psoriasis. Dermatol Clin. 2015;33(1):1–11. https://doi.org/10.1016/j.det.2014.09.001.
Hwang ST, Nijsten T, Elder JT. Recent highlights in psoriasis research. J Investig Dermatol. 2017;137(3):550–6. https://doi.org/10.1016/j.jid.2016.11.007.
Ogawa K, Okada Y. The current landscape of psoriasis genetics in 2020. J Dermatol Sci. 2020;99(1):2–8. https://doi.org/10.1016/j.jdermsci.2020.05.008.
Alshobaili HA, Shahzad M, Al-Marshood A, Khalil A, Settin A, Barrimah I. Genetic background of psoriasis. Int J Health Sci (Qassim). 2010;4(1):23–9.
Hawkes JE, Nguyen GH, Fujita M, Florell SR, Callis Duffin K, Krueger GG, et al. microRNAs in psoriasis. J Investig Dermatol. 2016;136(2):365–71. https://doi.org/10.1038/JID.2015.409.
Reolid A, Munoz-Aceituno E, Abad-Santos F, Ovejero-Benito MC, Dauden E. Epigenetics in non-tumor immune-mediated skin diseases. Mol Diagn Ther. 2021;25(2):137–61. https://doi.org/10.1007/s40291-020-00507-1.
Goldberg AD, Allis CD, Bernstein E. Epigenetics: a landscape takes shape. Cell. 2007;128(4):635–8. https://doi.org/10.1016/j.cell.2007.02.006.
Frischknecht L, Vecellio M, Selmi C. The role of epigenetics and immunological imbalance in the etiopathogenesis of psoriasis and psoriatic arthritis. Ther Adv Musculoskelet Dis. 2019;11:1759720X19886505. https://doi.org/10.1177/1759720X19886505.
Liu Y, Liu Q. MicroRNAs as regulatory elements in psoriasis. Open Med (Wars). 2016;11(1):336–40. https://doi.org/10.1515/med-2016-0063.
Du T, Zamore PD. microPrimer: the biogenesis and function of microRNA. Development. 2005;132(21):4645–52. https://doi.org/10.1242/dev.02070.
Brennecke J, Stark A, Russell RB, Cohen SM. Principles of microRNA-target recognition. PLoS Biol. 2005;3(3):e85. https://doi.org/10.1371/journal.pbio.0030085.
Liu Q, Wu DH, Han L, Deng JW, Zhou L, He R, et al. Roles of microRNAs in psoriasis: immunological functions and potential biomarkers. Exp Dermatol. 2017;26(4):359–67. https://doi.org/10.1111/exd.13249.
O’Connell RM, Rao DS, Baltimore D. microRNA regulation of inflammatory responses. Annu Rev Immunol. 2012;30:295–312. https://doi.org/10.1146/annurev-immunol-020711-075013.
Singhvi G, Manchanda P, Krishna Rapalli V, Kumar Dubey S, Gupta G, Dua K. MicroRNAs as biological regulators in skin disorders. Biomed Pharmacother. 2018;108:996–1004. https://doi.org/10.1016/j.biopha.2018.09.090.
Xiao S, Liu X, Wang X, Lv H, Zhao J, Guo X, et al. Plasma microRNA expression profiles in psoriasis. J Immunol Res. 2020;2020:1561278. https://doi.org/10.1155/2020/1561278.
Xiong Y, Chen H, Liu L, Lu L, Wang Z, Tian F, et al. microRNA-130a promotes human keratinocyte viability and migration and inhibits apoptosis through direct regulation of STK40-mediated NF-kappaB pathway and indirect regulation of SOX9-meditated JNK/MAPK pathway: a potential role in psoriasis. DNA Cell Biol. 2017;36(3):219–26. https://doi.org/10.1089/dna.2016.3517.
Mensa E, Recchioni R, Marcheselli F, Giuliodori K, Consales V, Molinelli E, et al. MiR-146a-5p correlates with clinical efficacy in patients with psoriasis treated with the tumour necrosis factor-alpha inhibitor adalimumab. Br J Dermatol. 2018;179(3):787–9. https://doi.org/10.1111/bjd.16659.
Sonkoly E, Stahle M, Pivarcsi A. MicroRNAs: novel regulators in skin inflammation. Clin Exp Dermatol. 2008;33(3):312–5. https://doi.org/10.1111/j.1365-2230.2008.02804.x.
Srivastava A, Nikamo P, Lohcharoenkal W, Li D, Meisgen F, Xu Landen N, et al. MicroRNA-146a suppresses IL-17-mediated skin inflammation and is genetically associated with psoriasis. J Allergy Clin Immunol. 2017;139(2):550–61. https://doi.org/10.1016/j.jaci.2016.07.025.
Xia P, Fang X, Zhang ZH, Huang Q, Yan KX, Kang KF, et al. Dysregulation of miRNA146a versus IRAK1 induces IL-17 persistence in the psoriatic skin lesions. Immunol Lett. 2012;148(2):151–62. https://doi.org/10.1016/j.imlet.2012.09.004.
Zhang W, Yi X, Guo S, Shi Q, Wei C, Li X, et al. A single-nucleotide polymorphism of miR-146a and psoriasis: an association and functional study. J Cell Mol Med. 2014;18(11):2225–34. https://doi.org/10.1111/jcmm.12359.
Gong HB, Zhang SL, Wu XJ, Pu XM, Kang XJ. Association of rs2910164 polymorphism in MiR-146a gene with psoriasis susceptibility: a meta-analysis. Medicine (Baltimore). 2019;98(6):e14401. https://doi.org/10.1097/MD.0000000000014401.
Park R, Lee WJ, Ji JD. Association between the three functional miR-146a single-nucleotide polymorphisms, rs2910164, rs57095329, and rs2431697, and autoimmune disease susceptibility: a meta-analysis. Autoimmunity. 2016;49(7):451–8. https://doi.org/10.3109/08916934.2016.1171854.
Jazdzewski K, Murray EL, Franssila K, Jarzab B, Schoenberg DR, de la Chapelle A. Common SNP in pre-miR-146a decreases mature miR expression and predisposes to papillary thyroid carcinoma. Proc Natl Acad Sci USA. 2008;105(20):7269–74. https://doi.org/10.1073/pnas.0802682105.
Luo X, Yang W, Ye DQ, Cui H, Zhang Y, Hirankarn N, et al. A functional variant in microRNA-146a promoter modulates its expression and confers disease risk for systemic lupus erythematosus. PLoS Genet. 2011;7(6):e1002128. https://doi.org/10.1371/journal.pgen.1002128.
Wang G, Tam LS, Li EK, Kwan BC, Chow KM, Luk CC, et al. Serum and urinary cell-free MiR-146a and MiR-155 in patients with systemic lupus erythematosus. J Rheumatol. 2010;37(12):2516–22. https://doi.org/10.3899/jrheum.100308.
Bunce M, O’Neill CM, Barnardo MC, Krausa P, Browning MJ, Morris PJ, et al. Phototyping: comprehensive DNA typing for HLA-A, B, C, DRB1, DRB3, DRB4, DRB5 & DQB1 by PCR with 144 primer mixes utilizing sequence-specific primers (PCR-SSP). Tissue Antigens. 1995;46(5):355–67. https://doi.org/10.1111/j.1399-0039.1995.tb03127.x.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25(4):402–8. https://doi.org/10.1006/meth.2001.1262.
Chen XM, Zhao Y, Wu XD, Wang MJ, Yu H, Lu JJ, et al. Novel findings from determination of common expressed plasma exosomal microRNAs in patients with psoriatic arthritis, psoriasis vulgaris, rheumatoid arthritis, and gouty arthritis. Discov Med. 2019;28(151):47–68.
Lovendorf MB, Zibert JR, Gyldenlove M, Ropke MA, Skov L. MicroRNA-223 and miR-143 are important systemic biomarkers for disease activity in psoriasis. J Dermatol Sci. 2014;75(2):133–9. https://doi.org/10.1016/j.jdermsci.2014.05.005.
Chiricozzi A, Nograles KE, Johnson-Huang LM, Fuentes-Duculan J, Cardinale I, Bonifacio KM, et al. IL-17 induces an expanded range of downstream genes in reconstituted human epidermis model. PLoS ONE. 2014;9(2):e90284. https://doi.org/10.1371/journal.pone.0090284.
Harden JL, Krueger JG, Bowcock AM. The immunogenetics of psoriasis: a comprehensive review. J Autoimmun. 2015;64:66–73. https://doi.org/10.1016/j.jaut.2015.07.008.
Martin DA, Towne JE, Kricorian G, Klekotka P, Gudjonsson JE, Krueger JG, et al. The emerging role of IL-17 in the pathogenesis of psoriasis: preclinical and clinical findings. J Invest Dermatol. 2013;133(1):17–26. https://doi.org/10.1038/jid.2012.194.
Saba R, Sorensen DL, Booth SA. MicroRNA-146a: a dominant, negative regulator of the innate immune response. Front Immunol. 2014;5:578. https://doi.org/10.3389/fimmu.2014.00578.
Meisgen F, Xu Landen N, Wang A, Rethi B, Bouez C, Zuccolo M, et al. MiR-146a negatively regulates TLR2-induced inflammatory responses in keratinocytes. J Investig Dermatol. 2014;134(7):1931–40. https://doi.org/10.1038/jid.2014.89.
Niimoto T, Nakasa T, Ishikawa M, Okuhara A, Izumi B, Deie M, et al. MicroRNA-146a expresses in interleukin-17 producing T cells in rheumatoid arthritis patients. BMC Musculoskelet Disord. 2010;11:209. https://doi.org/10.1186/1471-2474-11-209.
Yang L, Boldin MP, Yu Y, Liu CS, Ea CK, Ramakrishnan P, et al. miR-146a controls the resolution of T cell responses in mice. J Exp Med. 2012;209(9):1655–70. https://doi.org/10.1084/jem.20112218.
Fan X, Yang S, Sun LD, Liang YH, Gao M, Zhang KY, et al. Comparison of clinical features of HLA-Cw*0602-positive and -negative psoriasis patients in a Han Chinese population. Acta Derm Venereol. 2007;87(4):335–40. https://doi.org/10.2340/00015555-0253.
Gudjonsson JE, Karason A, Runarsdottir EH, Antonsdottir AA, Hauksson VB, Jonsson HH, et al. Distinct clinical differences between HLA-Cw*0602 positive and negative psoriasis patients—an analysis of 1019 HLA-C- and HLA-B-typed patients. J Investig Dermatol. 2006;126(4):740–5. https://doi.org/10.1038/sj.jid.5700118.
Hermann H, Runnel T, Aab A, Baurecht H, Rodriguez E, Magilnick N, et al. miR-146b probably assists miRNA-146a in the suppression of keratinocyte proliferation and inflammatory responses in psoriasis. J Investig Dermatol. 2017;137(9):1945–54. https://doi.org/10.1016/j.jid.2017.05.012.
Maharaj AB, Naidoo P, Ghazi T, Abdul NS, Dhani S, Docrat TF, et al. MiR-146a G/C rs2910164 variation in South African Indian and Caucasian patients with psoriatic arthritis. BMC Med Genet. 2018;19(1):48. https://doi.org/10.1186/s12881-018-0565-1.
Chatzikyriakidou A, Voulgari PV, Georgiou I, Drosos AA. The role of microRNA-146a (miR-146a) and its target IL-1R-associated kinase (IRAK1) in psoriatic arthritis susceptibility. Scand J Immunol. 2010;71(5):382–5. https://doi.org/10.1111/j.1365-3083.2010.02381.x.
Acknowledgements
The authors acknowledge the patients followed at HSA-CHUP. We also acknowledge the nurses from the Dermatology outpatient clinic and Mrs Dina Lopes for collaboration in sample collection and Ms. Maria Rebelo for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflict of interest
Bárbara Leal, Cláudia Carvalho, Ana Marta Ferreira, Miguel Nogueira, Sandra Brás, Berta M. Silva, Manuela Selores, Paulo P. Costa, and Tiago Torres have no conflicts of interest that are directly relevant to the content of this article.
Availability of Data and Material
Not applicable.
Ethics approval
The study was approved by the hospital Institutional Ethical Committee.
Consent
Written informed consent was obtained from every participant in the study in accordance with Helsinki Declaration.
Author contributions
The study was conceived and designed by Bárbara Leal, Cláudia Carvalho, and Tiago Torres. Material preparation and data collection and analysis were performed by Bárbara Leal, Cláudia Carvalho, Ana Marta, Miguel Nogueira, and Sandra Brás. The first draft of the manuscript was written by Bárbara Leal and Cláudia Carvalho. Miguel Nogueira, Berta M. Silva, Manuela Selores, Paulo Pinho e Costa, and Tiago Torres critically revised the manuscript, and the final version was read and approved by all authors.
Rights and permissions
About this article
Cite this article
Leal, B., Carvalho, C., Ferreira, A.M. et al. Serum Levels of miR-146a in Patients with Psoriasis. Mol Diagn Ther 25, 475–485 (2021). https://doi.org/10.1007/s40291-021-00531-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-021-00531-9