Abstract
Congenital adrenal hyperplasia (CAH) comprises a group of autosomal recessive disorders caused by complete or partial defects in one of the several steroidogenic enzymes involved in the synthesis of cortisol from cholesterol in the adrenal glands. More than 95–99% of all cases of CAH are caused by deficiency of steroid 21-hydroxylase, an enzyme encoded by the CYP21A2 gene. Currently, CYP21A2 genotyping is considered a valuable complement to biochemical investigations in the diagnosis of 21-hydroxylase deficiency. More than 200 mutations have been described in literature reports, and much energy is still focused on the clinical classification of new variants. In this review, we focus on molecular genetic features of 21-hydroxylase deficiency, performing an extensive survey of all clinical pathogenic variants modifying the whole sequence of the CYP21A2 gene. Our aim is to offer a very useful tool for clinical and genetic specialists in order to ease clinical diagnosis and genetic counseling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An extensive effort was made in order to collect literature data reporting CYP21A2 pathogenic variants. |
We were able to provide 233 pathogenic CYP21A2 variants and their clinical classification. |
1 Introduction
Congenital adrenal hyperplasia (CAH) due to 21-hydroxylase (21-OH) deficiency represents 95–99% of all CAH cases [1,2,3]. The hallmark of the disease is the deficiency of enzyme activity, leading to poor cortisol production and the subsequent accumulation of precursor steroid hormones in the steroidogenic pathway, resulting in hyperandrogenism [4, 5]. This disorder has a broad spectrum of clinical forms, ranging from severe or classical (CL) to mild late-onset or non-classical (NC). CL CAH, affecting 1:13,000 to 1:15,000 live births, is represented by two phenotypes: simple virilizing (SV) and salt wasting (SW). SW CAH, the most severe among the two phenotypes, accounts for an estimated 75% of CL cases [4, 5]. The severe impairment of 21-hydroxylase enzyme (< 2% enzyme activity) leads to an inadequate production of aldosterone and cortisol to sustain life. The lack of aldosterone, required for sodium homeostasis, if left untreated, will lead to vomiting, lethargy, and failure to gain weight. In fact, severely affected newborns usually present at 1–4 weeks of age with hyponatremia, hyperkalemia, hyper-reninemia, and hypovolemic shock. These adrenal crises may prove fatal if proper medical care is not delivered [1, 4, 5].
An increase of about 1–2% in 21-hydroxylase activity, compared to SW CAH, leads to SV CAH (25% of all CL CAH patients) and in this case, aldosterone is produced in an adequate amount, preventing an SW crisis. The typical result in severely affected girls is ambiguous or male-appearing external genitalia with perineal hypospadias, chordee, and undescended testes [4]. Finally, NC CAH refers to a partial 21-hydroxylase enzyme deficiency, typically around 20–50% of normal enzyme function. Though not requiring therapy for survival, cortisol production by the adrenal glands is insufficient to adequately suppress adrenocorticotropic hormone (ACTH) over-secretion and the shunting of precursor steroids leads to hyperandrogenemia [6, 7].
CAH due to 21-hydroxylase deficiency is inherited in an autosomal recessive manner. About 65–70% of CAH patients are compound heterozygous, and the milder of the two affected alleles is usually expressed phenotypically [8, 9]. Many studies have addressed a strong correlation between genotype and phenotype. However, there is well-documented evidence that divergence between genotype and phenotype can occur in some cases [10,11,12,13]. Over the last few years, much progress has been made in mutation detection and various screening strategies have been reported. This has led to the identification of a large number of variants and their classification [14,15,16].
Depending on residual activity of mutant enzyme, CYP21A2 variants are classified in four groups (Null, A, B, and C). Variants of Null and A groups are both associated with the SW form of the disease. However, while Null variants show 0% enzyme activity during in vitro assay, group A variants, with the IVS2-13A/C>G mutation, preserve a minimal (< 1%) residual activity. Finally, group B (1–5% enzyme activity) and group C (20–50% enzyme activity) variants are related to the SV and the NC form, respectively [9].
In this review, we focus on molecular genetic features of the disease, performing an extensive survey of all clinically classified variants modifying the whole sequence of the CYP21A2 gene. Our aim is to offer a very useful tool for clinical and genetic specialists in order to make clinical diagnosis and genetic counseling of 21-hydroxylase deficiency easier.
2 Genetics of 21-Hydroxylase Deficiency
2.1 Structure of the CYP21A2 Gene and Gene Locus
The gene encoding 21-hydroxylase, CYP21A2, is located in the human leukocyte antigen (HLA) class III region on the short arm of chromosome 6p21.3 [17]. In this region, four tandemly arranged genes—serine/threonine kinase RP, complement C4, steroid 21-hydroxylase CYP21, and tenascin TNX—are organized as a genetic unit designated as an RCCX module. In an RCCX bimodular haplotype, duplication of the RCCX module occurs and the orientation of genes, from telomere to centromere, is RP1-C4A-CYP21A1P-TNXA-RP2-C4B-CYP21A2-TNXB. RP1 encodes a putative nuclear protein similar to DNA helicase, C4A and C4B genes encode the fourth component of complement, and TNXB encodes an extracellular matrix protein, tenascin X, which overlaps the CYP21A2 gene on the opposite strand. The three pseudogenes, CYP21A1P-TNXA and RP2, located between the two C4 loci, do not encode functional proteins [18,19,20]. Both the CYP21A2 gene and CYP21A1P pseudogene contain ten exons spaced over 3.1 kb. Their nucleotide sequences are 98% identical in exons and approximately 96% identical in introns [21]. In the Caucasian population, bimodular and monomodular RCCX organizations are present in about 69 and 17% of chromosome 6, respectively, while trimodular RCCX haplotypes have a frequency of about 14% [19]. A trimodular haplotype carrying one copy of the CYP21A1P pseudogene and two copies of the CYP21A2 gene has been described in different nationalities [22,23,24,25,26,27,28].
2.2 Mutations Causing 21-Hydroxylase Deficiency
Due to the high degree of sequence homology and the tandem repeating order of the RCCX module sequence, the CYP21A2 region seems to be the most likely area for misalignments to occur at meiosis, which would generate illegitimate genetic recombinations or unequal crossing over. In fact, intergenic recombinations are responsible for 95% of the mutations associated with 21-hydroxylase deficiency [5, 29, 30]. Mutations that are not apparently gene conversions account for 5–10% of 21-hydroxylase deficiency alleles in most populations [5]. Finally, about 1% of CYP21A2-inactivating mutations arise de novo [5].
2.2.1 Microconversion Events
Among the intergenic recombinations, approximately 75% are represented by mutations generally present in the CYP21A1P pseudogene and possibly transferred to the functional CYP21A2 gene by microconversion events [31]. The deleterious mutations in CYP21A1P include the following: a nucleotide substitution (g.5774A/C>G; IVS2-13A/C>G) before the end of intron 2 that results in aberrant splicing of RNA, an 8-bp deletion in exon 3 (g.5826_5833 delGAGACTAC, p.G110Vfs?), an insertion of one nucleotide in exon 7 (g.6882_6883insT, p.L307Ffs?), and a nonsense mutation in exon 8 (g.7114 C>T, p.Q318X). We also reported that the 238-amino acid deletion is present in the pseudogene, with a frequency of 4.5% [28], and as described, this pathogenic pseudogene deriving mutation can also be transferred to the active gene by a microconversion event [32]. Lastly there are also six missense mutations in CYP21A1P (p.P30L, p.I172N, p.I136N, p.V237E, p.M239K, and p.R356W), transferred to CYP21A2, that have all been observed in patients suffering from 21-hydroxylase deficiency, and each of these is related to a different clinical form of CAH [33].
We would like to underline that not all pseudogenes harbor these mutations. In fact, in the last few years, some studies investigating the existence of CYP21A2 wild-type loci in the CYP21A1P pseudogene reported specific allelic frequencies in the studied populations [28, 34,35,36]. In an Italian population, we reported frequencies of 3, 27, 16, and 57% for p.P30, p.V281, p.Q318, and p.R356 positions, respectively. No more wild-type loci have been detected [28]. This information should be considered during the planning of molecular testing for 21-hydroxylase deficiency [28, 37].
The remaining 20–25% of mutations are CYP21A2 whole gene deletions or CYP21A1P/CYP21A2 chimeric genes. Both events are the consequence of an unequal crossing over [5].
2.2.2 CYP21A2 Gene Deletion
Some reports have shown that complete deletion of CYP21A2 in Caucasians appears as a TNXA/TNXB hybrid gene, resulting in a recessive form of Ehlers–Danlos syndrome (EDS) caused by tenascin-X deficiency [38,39,40,41]. A total of nine types of EDS were outlined, and the form related to TNXB deficiency involves features of marked skin laxity, pronounced joint hypermobility, and severe bruising [39]. The complete deletion of the CYP21A2 gene changes the genomic organization in the RCCX module to the status of C4A-CYP21A1P-TNXA/TNXB. To date, at least nine kinds of chimeric TNXA/TNXB genes have been identified and associated with EDS as well as CAH [42].
2.2.3 Chimeric CYP21A1P/CYP21A2 Genes
A 26- or 32-kb deletion (depending on whether C4B is the short or long gene), involving the 3′ end of CYP21A1P, all of the C4B gene, and the 5′ end of CYP21A2, produces a single nonfunctional chimeric gene with its 5′ and 3′ ends corresponding to CYP21A1P and CYP21A2, respectively [43]. Several mutations within the CYP21A1P portion render such a gene incapable of encoding an active enzyme. To date, nine different chimeric CYP21A1P/CYP21A2 genes have been found and characterized in different studies [44]. Chimeric CYP21A1P/CYP21A2 genes have been classified into two categories, classic and attenuated, depending on the location of the junction sites relative to pseudogene mutation IVS2-13A/C>G within intron 2 [44]. Seven chimeras (CH-1, CH-2, CH-3, CH-5, CH-6, CH-7, and CH-8) carry the pseudogene specific mutation IVS2-13A/C>G in intron 2 and thus are associated with a severe SW phenotype [42,43,44,45,46,47,48,49,50,51]. This group of chimeras is common among CAH patients of Caucasian origin and has been referred to as the classic or common type of chimera [44].
In contrast, 21-hydroxylase enzyme activity is less severely impaired if the junction site occurs upstream of the IVS2-13A/C>G variant. By carrying a weak CYP21A1P promoter and an NC mutation, p.P30L, at exon 1 only, the chimera partially retains 21-hydroxylase activity, producing a milder clinical phenotype. In fact, CH-4 and CH-9, two uncommon chimeras, fall into the group of attenuated chimeras [44, 52].
2.2.4 CYP21A2 Gene Duplication
An unequal meiotic crossing-over event produces the duplication of CYP21A2 gene. In fact, a trimodular haplotype carrying one copy of the CYP21A1P pseudogene and two copies of the CYP21A2 gene has been described in different nationalities [22,23,24,25,26,27,28]. In most cases, the CYP21A2 copy downstream of the TNXA gene showed a wild-type sequence or the IVS-13A/C>G mutation, while the CYP21A2 gene next to TNXB carried the p.Q318X mutation [23,24,25,26,27]. Recently, the presence of this trimodular haplotype explained the lack of genotype–phenotype correlation in individuals of different families, suggesting the importance of trimodular haplotype assessment in CAH genetic diagnosis [53, 54]. In fact, the existence of rare trimodular haplotypes is a condition that should be strongly considered when CAH genetic analysis is offered at the prenatal level in order to define the real risk of the fetus and avoid further investigations at birth. It is very important to investigate this condition also when analysis is offered at the preconceptional level, in order to avoid unnecessary prenatal therapy.
We think that a robust assay for Copy Number Variation (CNV) assessment should be offered as an integral part of 21-hydroxylase deficiency genetic testing. Differently, most laboratories perform, as a sole investigation, CYP21A2 gene sequencing. However, because individuals carrying the p.Q318X variant frequently have a duplication of the CYP21A2 gene, when this mutation is detected, it is always recommended to established the correct number of copies. As reported above, providing this information is crucial in genetic counseling of couples as well as in prenatal diagnosis.
2.2.5 Novel CYP21A2 Variants
Variants that are not apparently gene conversions account for 5–10% of 21-hydroxylase deficiency alleles in most populations [5]. These novel mutations are easy to detect using automated sequencing technologies in specialized laboratories and thus have been reported at an increased rate over the past few years. The functional effects of a new mutation are generally assessed in vitro by recreating it in CYP21A2 complementary DNA (cDNA) and expressing the mutant cDNA using an appropriate expression vector in mammalian cells. A radioactive assay allows evaluation of the residual enzymatic activities of the mutant protein towards the two natural substrates of steroid 21-hydroxylase, 17-hydroxyprogesterone (17-OHP) and progesterone. Mutant enzyme activity is expressed as a percentage of the wild-type enzyme [55,56,57,58]. This approach allows correlation of each mutation to a different clinical form of CAH.
Over the last few years, much progress has been made towards predicting protein stabilities and correlating them to protein activities. Homology modeling and fast energetic calculations have emerged as useful tools to evaluate, through structure-based methods, the impairment of protein stability. Human 21-hydroxylase models have been built based on the available low homology CYP protein families. Structural features deduced from the models were in good correlation with clinical severity of mutations, confirming the applicability of a modeling approach in assessment of new CYP21A2 mutations [59,60,61,62,63,64,65,66,67].
3 CYP21A2 Variants Review
A list of some CYP21A2 variants can be found in the CYP21A2 database created by the Human Cytochrome P450 (CYP) Allele Nomenclature Committee (https://www.pharmvar.org/htdocs/archive/cyp21.htm) [68]. For each variant, the enzyme residual activity and the associated clinical phenotype is reported. The last update of this database was performed in 2011, after the release of our review [16]. However, over the last few years, many other novel CYP21A2 mutations have been described.
The aim of this work is to provide a complete focus on all pathogenic CYP21A2 variants reported to date in the literature. Our purpose is to offer very useful information for clinical and genetic specialists, making CAH diagnosis and genetic counseling easier. For this reason, we choose to consider only variants reported in literature papers where clinical and molecular information (genotype–phenotype correlation, functional characterization, structural study) are generally provided. So we exclude all those variants, reported in common databases, missing such data. We searched the National Center for Biotechnology Information (NCBI) PubMed literature database for articles in English, using the keywords “CYP21A2 new mutation/variant” and “CYP21A2 novel mutation/variant.” More than 100 articles, published from January 2011 to December 2017, were read and evaluated for the real presence of new variants. In our update, we decided to report all detected variants according to Locus Reference Genomic (LRG) CYP21A2 reference sequences: NG_007941.2 and NM_000500.6. Table 1 provides a list of all CYP21A2 exonic variants with an assessed pathogenic role; to each variant we associate molecular and clinical information, reporting in the reference section the papers providing the greatest contribution in classifying that specific variant. Similarly, Table 2 shows all CYP21A2 variants affecting the non-coding regions and their clinical significance. Finally, CYP21A2 exonic polymorphisms were also assessed in the present review and are reported in Table 3.
3.1 CYP21A2 Variants Distribution
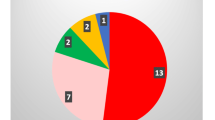
A total of 212 CYP21A2 disease-causing variants, affecting the coding region of the gene, are listed in Table 1, while 21 pathogenic variants within non-coding regions are reported in Table 2. According to our results, these 233 variants are scattered throughout the entire sequence of the CYP21A2 gene and consist of (a) 65.2% missense mutations, (b) 9.4% nonsense mutations, (c) 7.7% splicing affecting variants, (d) 13.3% frameshift mutations, (e) about 3% small in-frame deletions/insertions (del/ins), and, finally, (f) 1.3% variants involving untranslated regions (promoter and 3′UTR) (Fig. 1a). The exons harboring the major number of mutations were the 10, 8, and 7, respectively. On the contrary, exon 5 was the less affected region of the gene (Fig. 2).
a Percentages of missense, nonsense, frameshift, in-frame, splicing CYP21A2 variants reported to date. Percentage of nucleotide substitutions affecting UTRs is also shown. b Percentages of SW, SV, and NC variants. Percentage of variants with conflicting interpretation of significance is also shown. NC non-classical, SV simple virilizing, SW salt wasting, UTR untranslated region
Codons 1 and 483, in exon 1 and 10, respectively, were affected by the highest number of mutations. In particular, codon 1 is affected by four missense mutations all related to the SW form (p.M1I, p.M1L, p.M1V, and p.M1T), while three missense (p.R483W, p.R483Q, and p.R483P) and one frameshift variant (p.R483Pfs?) fall into codon 483 (Table 1).
The highest number of known variants affecting the splicing process is within intron 2 (27.8%) (Table 2); this is probably due to the fact that it is the most polymorphic region of the whole CYP21A2 gene.
3.2 Variant–Phenotype Association
As the aim of this work is to provide a useful tool for clinical and genetic specialists, we focused on associating a clinical, specific phenotype to each variant. For this purpose, diverse papers reporting a specific variant were carefully evaluated, considering the genotype and the phenotype of different described patients and analyzing all data from the performed structural and functional studies.
Regarding the 5′ and 3′ UTRs, only two disease-causing variants have been reported in addition to the cluster of four variants producing promoter conversion: the c.-126C>T (from the cluster that produces the promoter conversion c.-126C>T; c.-113G>A; -110T>C; -103A>G) and the c.*13C>T, both related to the NC form of the disease (Table 2) [69, 70]. Differently, 17 out of 18 splicing affecting variants are plausibly related to the most severe form of disease, the SW syndrome (Table 2). The IVS5-8T>A variant was detected in trans with the p.I172N in a patient affected by SV CAH. In this case, it is not possible to establish if the intronic variant is related to the SW or SV phenotype [71].
Overall, 126 (54.1%) out of 233 CYP21A2 mutations are associated with the SW form of the disease, 38 are associated with the SV form (16.3%), and 61 (26.2%) are related to the NC form (Fig. 1b). Seven exonic variants and one intronic variant (3.4%, variants marked with an asterisk in Tables 1, 2) are not definitively associated with a specific phenotype (SW, SV, NC) as there is missing or conflicting information in the literature (see next section) (Fig. 1b).
3.2.1 Variants with Conflicting Interpretation of Significance
We were not able to assign a definitive clinical phenotype to seven exonic variants. In the literature, we found several patients carrying the same variant, but showing different phenotypes; in most cases, the results of functional studies were not in agreement with the patient’s phenotype or with structural analysis. In addition, some variants have only been reported once by inconclusive papers.
3.2.1.1 p.P45L
This variant was detected in an SV CAH Norwegian patient carrying a complete CYP21A2 gene deletion on the second allele [72]. Subsequently, a functional study was performed; in vitro enzyme activity was normal, but the proline-to-leucine shift in position 45 was predicted as pathologic by computer modeling [73]. The p.P45 residue is located in the N-terminal region of the enzyme close to the hydrophobic domain that anchors the protein to the endoplasmic reticulum (ER) membrane [66]. As the functional characterization of the p.P45L mutant was carried out in the absence of membranes, the severely reduced in vivo activity compared to wild-type protein could be missed in the system used. In fact, the authors affirm that future studies should be performed using cell-free expression of 21-hydroxylase with the traditional use of transiently transfected COS7 cells including a wide range of known and well-characterized CYP21A2 variants [73]. Recently, Bruque et al. reported that, contrary to the in vitro assay results, the in silico-predicted p.P45L activity may correlate better with the SV form of the disease [67].
In our opinion, there is sufficient information for a definitive classification of this variant as SV. In fact, the discordance could be due to results obtained by functional studies performed using a different system from the conventional procedures.
3.2.1.2 E140K
The variant was detected in an SW patient carrying a complete CYP21A2 gene deletion on the second allele [73]. The residual enzyme activity was estimated by quantifying 11-deoxycortisol using 17-OHP as the substrate, and an in vitro assay showed a significant reduction in enzyme activity (11.3% ± 2.4). However, it was still much higher than expected for the SW phenotype. Structural analysis showed that the p.E140 residue forms a salt bridge with the R444 residue, and the shift from negatively charged glutamic acid to positively charged lysine breaks the salt bridge. This prediction could be in agreement with a severe form of disease, explaining the SW phenotype of the patient [73]. To date, there are no other papers in the literature reporting this variant in CAH patients.
We think that, despite the data obtained from the functional study, this rare variant is most likely related to the SW form. We recommend considering this possibility in genetic and prenatal counseling.
3.2.1.3 p.I171N
This variant was reported by Barbaro et al. [74] in an NC CAH Italian patient carrying the p.V281L mutation on the other allele. As it was impossible to classify this novel variant according to the clinical findings of this patient, a functional study was performed [74]. The results obtained showed that the variant was associated with the CL CAH phenotype [74]. However, 6 years later, a structural study classified this kind of variant as resulting in NC CAH [66]. The p.I171 residue is located in a predicted alpha helix structure (helix E) and the substitution of a polar asparagine to a hydrophobic non-polar isoleucine affects the hydrophobic property of this region [66]. To date, there are no other papers in the literature reporting this variant in CAH patients.
We think that further studies are needed in order to provide a definitive classification of this variant. To date, based on results from functional study, the possibility of a severe form of disease should be considered.
3.2.1.4 p.G178A
A Spanish patient, diagnosed as having SV CAH, carried both the p.G178A and the NC p.V281L mutation on the paternal allele and the IVS2-13A/C>G mutation on the maternal allele. The functional study was performed, and the p.G178A mutant was not able to metabolize progesterone at significant levels, while it retained significant activity (19%) for 17a-hydroxyprogesterone [75]. According to the authors, these results correlated well with the identification of the p.G178A in a patient with the SV form [75]. Subsequently, structural models showed that this variant could be related to a severe form of the disease (SW) [59, 66]. In fact, according to the authors, CYP21A2 protein inactivation can occur when conformational flexibility is impaired, mostly because of the introduction of bulkier residues. For example, the sharp fold between the E and F helices, where G178 is located, can only accommodate a small residue. The mutation of glycine to alanine will hinder the flexibility of this fold, impairing stability [66]. To date, there are no other papers in the literature reporting this variant in CAH patients. In our opinion, further studies would be needed for a final classification of this variant, because of the discrepancies in the currently available data.
3.2.1.5 p.E380D
The p.E380D variant was found in a homozygous patient suffering from the severe SW form of the disease [76]. A functional study, performed by Hsu et al. [77], indicated a 30% residual activity from the p.D380 mutant protein (17-OHP used as substrate) that does not correlate with the phenotypic presentation of the disease [77]. The structural study performed by Robins et al. [59] showed that there are only minor difference between a glutamate and an aspartate residue at the 380 position, while the structural model of Haider et al. classified the variant as related to the SW form [66]. To the best of our knowledge, there are no other reports in the literature of this variant in CAH patients.
The conflicting results do not allow a definitive classification of this variant. While waiting for further studies, we recommend considering the possibility of the SW form also in this case.
3.2.1.6 p.R483
The 483 codon harbors three rare variants that all seem to be related to the CL form of the disease. While data in the literature have definitively correlated p.R483Q to SV disease, contrasting information is reported for p.R483W and p.R483P variants [59, 66, 78,79,80,81,82]. We believe, based on the information reported above, that both these variants are reasonably related to the CL form of disease, with phenotypic manifestations associated with the SV or SW form.
3.2.1.7 p.R483W
This variant was first detected, in homozygous status, in a Tunisian patient who was diagnosed as having the SW phenotype [78]. Subsequently, p.R483W was reported in a Chinese girl carrying the E6 cluster mutation on the second allele. She was affected with the SV form [79]. The results obtained from the functional study were in accordance with the phenotype of the patient. So, authors classified the variant as related to the SV disease [79]. However, structural studies reported the p.R483W variant as being associated with SW [59, 66], showing that p.R483 residue makes a salt-bridge with p.D322, maintaining the structural elements in the correct position. The mutation interrupts this interaction, causing SW CAH [66].
3.2.1.8 p.R483P
This rare variant was reported in 1998 in two compound heterozygote subjects, with the unique p.R483P mutation on one allele and the well-known p.I172N mutation on the other [80]. They had a moderate form of the disease, with early clitoral enlargement in the female sibling, but without SW. The R483P mutant retained 1–2% of the activity (both substrates) of the native enzyme, and this was in agreement with the clinical phenotypes of the patients [80]. Subsequently, Finkielstain et al. described an SW patient carrying the p.R483P variant in the hemizygous condition [81], while a few years later Krone et al. associated the mutation with SV CAH [82]. Finally, a structural study in 2006 reported the variant as associated with the CL form (SV/SW) of the disease [59], while a more recent paper classified it as an NC variant [66].
4 Conclusion
In the diagnosis of 21-hydroxylase deficiency, CYP21A2 genotyping is a valuable complement to biochemical investigations. Genotyping can confirm the diagnosis (or carrier state) and, at the same time, give prognostic information on disease severity. This is especially important in male newborns detected in neonatal screening, since they do not display genital malformations as a sign of CL disease [4]. In addition, the use of genetic testing is also helpful in prenatal counseling and prenatal diagnosis with the goal of preventing genital virilization of the female fetus [83]. To date, more than 200 mutations of the CYP21A2 gene have been reported in different studies, and although it is well-known that some exceptions exist, there is good agreement between clinical phenotype and patient genotype [1,2,3,4, 9]. For this reason, much effort is spent in the classification of new variants. Clinical classification of new variants should be clarified with clinical investigations on groups of patients carrying the same variant with a different genotype (being the phenotype defined by the milder of the two mutations present). In addition, in vitro enzyme activity assays and structural studies, although they are artificial systems that cannot provide absolute indications reflecting the in vivo situation, offer a means to investigate rare variants, comparing these to the more common mutations for which abundant clinical data are available.
Reference
El-Maouche D, Arlt W, Merke DP. Congenital adrenal hyperplasia. Lancet. 2017;17:31431–9.
Arlt W, Willis DS, Wild SH, Krone N, Doherty EJ, Hahner S, Han TS, Carroll PV, Conway GS, Rees DA, Stimson RH, Walker BR, Connell JM, Ross RJ, United Kingdom Congenital Adrenal Hyperplasia Adult Study Executive (CaHASE). Health status of adults with congenital adrenal hyperplasia: a cohort study of 203 patients. J Clin Endocrinol Metab. 2010;95:5110–21.
Gidlöf S, Falhammar H, Thilén A, von Döbeln U, Ritzén M, Wedell A, Nordenström A. One hundred years of congenital adrenal hyperplasia in Sweden: a retrospective, population-based cohort study. Lancet Diabetes Endocrinol. 2013;1:35–42.
Parsa AA, New MI. Steroid 21-hydroxylase deficiency in congenital adrenal hyperplasia. J Steroid Biochem Mol Biol. 2017;165:2–11.
White PC, Speiser PW. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr Rev. 2000;21:245–91.
Falhammar H, Nordenström A. Nonclassic congenital adrenal hyperplasia due to 21-hydroxylase deficiency: clinical presentation, diagnosis, treatment, and outcome. Endocrine. 2015;50:32–50.
Carmina E, Dewailly D, Escobar-Morreale HF, Kelestimur F, Moran C, Oberfield S, Witchel SF, Azziz R. Non-classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency revisited: an update with a special focus on adolescent and adult women. Hum Reprod Update. 2017;23:580–99.
Wedell A. Molecular genetics of 21-hydroxylase deficiency. Endocr Dev. 2011;20:80–7.
Krone N, Arlt W. Genetics of congenital adrenal hyperplasia. Best Pract Res Clin Endocrinol Metab. 2009;23:181–92.
New MI, Abraham M, Gonzalez B, Dumic M, Razzaghy-Azar M, Chitayat D, Sun L, Zaidi M, Wilson RC, Yuen T. Genotype-phenotype correlation in 1,507 families with congenital adrenal hyperplasia owing to 21-hydroxylase deficiency. Proc Natl Acad Sci USA. 2013;110:2611–6.
Krone N, Braun A, Roscher AA, Knorr D, Schwarz HP. Predicting phenotype in steroid 21-hydroxylase deficiency? Comprehensive genotyping in 155 unrelated, well defined patients from southern Germany. J Clin Endocrinol Metab. 2000;85:1059–65.
Marino R, Ramirez P, Galeano J, Perez Garrido N, Rocco C, Ciaccio M, Warman DM, Guercio G, Chaler E, Maceiras M, Bergadá I, Gryngarten M, Balbi V, Pardes E, Rivarola MA, Belgorosky A. Steroid 21-hydroxylase gene mutational spectrum in 454 Argentinean patients: genotype-phenotype correlation in a large cohort of patients with congenital adrenal hyperplasia. Clin Endocrinol (Oxf). 2011;75:427–35.
Khattab A, Yuen T, Malki AS, Yau M, Kazmi D, Sun L, Harbison M, Haider S, Zaidi M, New MI. A rare CYP21A2 mutation in a congenital adrenal hyperplasia kindred displaying genotype-phenotype nonconcordance. Ann N Y Acad Sci. 2016;1364:5–10.
Balsamo A, Baldazzi L, Menabò S, Cicognani A. Impact of molecular genetics on congenital adrenal hyperplasia management. Sex Dev. 2010;4:233–48.
Choi JH, Kim GH, Yoo HW. Recent advances in biochemical and molecular analysis of congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Ann Pediatr Endocrinol Metab. 2016;21(1):1–6.
Concolino P, Mello E, Zuppi C, Capoluongo E. Molecular diagnosis of congenital adrenal hyperplasia due to 21-hydroxylase deficiency: an update of new CYP21A2 mutations. Clin Chem Lab Med. 2010;48:1057–62.
White PC, Grossberger D, Onufer BJ, Chaplin DD, New MI, Dupont B, Strominger JL. Two genes encoding steroid 21-hydroxylase are located near the genes encoding the fourth component of complement in man. Proc Natl Acad Sci USA. 1985;82:1089–93.
Yang Z, Mendoza AR, Welch TR, Zipf WB, Yu CY. Modular variations of the human major histocompatibility complex class III genes for serine/threonine kinase RP, complement component C4, steroid 21-hydroxylase CYP21, and tenascin TNX (the RCCX module). A mechanism for gene deletions and disease associations. J Biol Chem. 1999;274:12147–56.
Haglund-Stengler B, Martin Ritzen E, Gustafsson J, Luthman H. Haplotypes of the steroid 21-hydroxylase gene region encoding mild steroid 21-hydroxylase deficiency. Proc Natl Acad Sci USA. 1991;88:8352–6.
Blanchong CA, Zhou B, Rupert KL, Chung EK, Jones KN, Sotos JF, Zipf WB, Rennebohm RM, Yung YuC. Deficiencies of human complement component C4A and C4B and heterozygosity in length variants of RP-C4-CYP21-TNX (RCCX) modules in caucasians. The load of RCCX genetic diversity on major histocompatibility complex-associated disease. J Exp Med. 2000;191:2183–96.
White PC, New MI, Dupont B. Structure of human steroid 21-hydroxylase genes. Proc Natl Acad Sci USA. 1986;83:5111–5.
Ezquieta B, Beneyto M, Muñoz-Pacheco R, Barrio R, Oyarzabal M, Lechuga JL, Luzuriaga C, Hermoso F, Quinteiro S, Martinez S. Gene duplications in 21-hydroxylase deficiency: the importance of accurate molecular diagnosis in carrier detection and prenatal diagnosis. Prenat Diagn. 2006;26:1172–8.
Kharrat M, Riahi A, Maazoul F, M’rad R, Chaabouni H. Detection of a frequent duplicated CYP21A2 gene carrying a Q318X mutation in a general population with quantitative PCR methods. Diagn Mol Pathol. 2011;20:123–7.
Parajes S, Quinteiro C, Domínguez F, Loidi L. High frequency of copy number variations and sequence variants at CYP21A2 locus: implication for the genetic diagnosis of 21-hydroxylase deficiency. PLoS One. 2008;3:e2138.
Wedell A, Stengler B, Luthman H. Characterization of mutations on the rare duplicated C4/CYP21 haplotype in steroid 21-hydroxylase deficiency. Hum Genet. 1994;94:50–4.
Kleinle S, Lang R, Fischer GF, Vierhapper H, Waldhauser F, Födinger M, Baumgartner-Parzer SM. Duplications of the functional CYP21A2 gene are primarily restricted to Q318X alleles: evidence for a founder effect. J Clin Endocrinol Metab. 2009;94:3954–8.
Koppens PF, Hoogenboezem T, Degenhart HJ. CYP21 and CYP21P variability in steroid 21-hydroxylase deficiency patients and in the general population in the Netherlands. Eur J Hum Genet. 2000;8:827–36.
Concolino P, Mello E, Minucci A, Giardina B, Capoluongo E. Genes, pseudogenes and like genes: the case of 21-hydroxylase in Italian population. Clin Chim Acta. 2013;424:85–9.
Werkmeister JW, New MI, Dupont B, White PC. Frequent deletion and duplication of the steroid 21-hydroxylase genes. Am J Hum Genet. 1986;39:461–9.
Lee HH. CYP21 mutations and congenital adrenal hyperplasia. Clin Genet. 2001;59:293–301.
Tusié-Luna MT, White PC. Gene conversions and unequal crossovers between CYP21 (steroid 21-hydroxylase gene) and CYP21P involve different mechanisms. Proc Natl Acad Sci USA. 1995;92:10796–800.
Concolino P, Mello E, Zuppi C, Toscano V, Capoluongo E. CYP21A2 p. E238 deletion as result of multiple microconversion events: a genetic study on an Italian congenital adrenal hyperplasia (CAH) family. Diagn Mol Pathol. 2013;22:48–51.
Lee HH. Variants of the CYP21A2 and CYP21A1P genes in congenital adrenal hyperplasia. Clin Chim Acta. 2013;418:37–44.
Tsai LP, Cheng CF, Chuang SH, Lee HH. Analysis of the CYP21A1P pseudogene: indication of mutational diversity and CYP21A2-like and duplicated CYP21A2 genes. Anal Biochem. 2011;413:133–41.
Tsai LP, Lee HH. Analysis of CYP21A1P and the duplicated CYP21A2 genes. Gene. 2012;506:261–2.
Cantürk C, Baade U, Salazar R, Storm N, Pörtner R, Höppner W. Sequence analysis of CYP21A1P in a German population to aid in the molecular biological diagnosis of congenital adrenal hyperplasia. Clin Chem. 2011;57:511–7.
Concolino P, Mello E, Minucci A, Zuppi C, Capoluongo E. Multiplex ligation-dependent probe amplification analysis is useful for diagnosing congenital adrenal hyperplasia but requires a deep knowledge of CYP21A2 genetics. Clin Chem. 2011;57:1079–80.
Koppens PF, Hoogenboezem T, Degenhart HJ. Carriership of a defective tenascin-X gene in steroid 21-hydroxylase deficiency patients: TNXB -TNXA hybrids in apparent large-scale gene conversions. Hum Mol Genet. 2002;11:2581–90.
Kaufman CS, Butler MG. Mutation in TNXB gene causes moderate to severe Ehlers–Danlos syndrome. World J Med Genet. 2016;6:17–21.
Schalkwijk J, Zweers MC, Steijlen PM, Dean WB, Taylor G, van Vlijmen IM, van Haren B, Miller WL, Bristow J. A recessive form of the Ehlers–Danlos syndrome caused by tenascin-X deficiency. N Engl J Med. 2001;345:1167–75.
Lee HH, Lee YJ, Lin CY. PCR-based detection of the CYP21 deletion and TNXA/TNXB hybrid in the RCCX module. Genomics. 2004;83:944–50.
Lee HH. Chimeric CYP21P/CYP21 and TNXA/TNXB genes in the RCCX module. Mol Genet Metab. 2005;84:4–8.
Lee HH. The chimeric CYP21P/CYP21 gene and 21-hydroxylase deficiency. J Hum Genet. 2004;49:65–72.
Chen W, Xu Z, Sullivan A, Finkielstain GP, Van Ryzin C, Merke DP, McDonnell NB. Junction site analysis of chimeric CYP21A1P/CYP21A2 genes in 21-hydroxylase deficiency. Clin Chem. 2012;58:421–30.
Concolino P, Mello E, Minucci A, Giardina E, Zuppi C, Toscano V, Capoluongo E. A new CYP21A1P/CYP21A2 chimeric gene identified in an Italian woman suffering from classical congenital adrenal hyperplasia form. BMC Med Genet. 2009;10:72.
Vrzalová Z, Hrubá Z, Hrabincová ES, Vrábelová S, Votava F, Koloušková S, Fajkusová L. Chimeric CYP21A1P/CYP21A2 genes identified in Czech patients with congenital adrenal hyperplasia. Eur J Med Genet. 2011;54:112–7.
Chu X, Braun-Heimer L, Rittner C, Schneider PM. Identification of the recombination site within the steroid 21-hydroxylase gene (CYP21) of the HLA-B47, DR7 haplotype. Exp Clin Immunogenet. 1992;9:80–5.
Helmberg A, Tabarelli M, Fuchs MA, Keller E, Dobler G, Schnegg I, Knorr D, Albert E, Kofler R. Identification of molecular defects causing congenital adrenal hyperplasia by cloning and differential hybridization of polymerase chain reaction-amplified 21-hydroxylase (CYP21) genes. DNA Cell Biol. 1992;11:359–68.
Lee HH, Lee YJ, Chan P, Lin CY. Use of PCR-based amplification analysis as a substitute for the Southern blot method for CYP21 deletion detection in congenital adrenal hyperplasia. Clin Chem. 2004;50:1074–6.
Lee HH, Chang SF, Lee YJ, Raskin S, Lin SJ, Chao MC, Lo FS, Lin CY. Deletion of the C4-CYP21 repeat module leading to the formation of a chimeric CYP21P/CYP21 gene in a 9.3-kb fragment as a cause of steroid 21-hydroxylase deficiency. Clin Chem. 2003;49:319–22.
White PC, New MI, Dupont B. HLA-linked congenital adrenal hyperplasia results from a defective gene encoding a cytochrome P-450 specific for steroid 21-hydroxylation. Proc Natl Acad Sci USA. 1984;81:7505–9.
L’Allemand D, Tardy V, Grüters A, Schnabel D, Krude H, Morel Y. How a patient homozygous for a 30-kb deletion of the C4-CYP 21 genomic region can have a nonclassic form of 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2000;85:4562–7.
Lekarev O, Tafuri K, Lane AH, Zhu G, Nakamoto JM, Buller-Burckle AM, Wilson TA, New MI. Erroneous prenatal diagnosis of congenital adrenal hyperplasia owing to a duplication of the CYP21A2 gene. J Perinatol. 2013;33:76–8.
Sani I, Rossodivita AN, Mariani M, Costella A, Molinario R, Concolino P, Capoluongo E. CYP21A2 genetics: When genotype does not fit phenotype. Clin Biochem. 2016;49:524–5.
Robins T, Bellanne-Chantelot C, Barbaro M, Cabrol S, Wedell A, Lajic S. Characterization of novel missense mutations in CYP21 causing congenital adrenal hyperplasia. J Mol Med (Berl). 2007;85:247–55.
Krone N, Riepe FG, Grötzinger J, Partsch CJ, Sippell WG. Functional characterization of two novel point mutations in the CYP21 gene causing simple virilizing forms of congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2005;90:445–54.
Concolino P, Vendittelli F, Mello E, Minucci A, Carrozza C, Rossodivita A, Giardina B, Zuppi C, Capoluongo E. Functional analysis of two rare CYP21A2 mutations detected in Italian patients with a mildest form of congenital adrenal hyperplasia. Clin Endocrinol (Oxf). 2009;71:470–6.
Concolino P, Vendittelli F, Mello E, Carelli Alinovi C, Minucci A, Carrozza C, Santini SA, Zuppi C, Capoluongo E. Two novel CYP21A2 missense mutations in Italian patients with 21-hydroxylase deficiency: Identification and functional characterisation. IUBMB Life. 2009;61:229–35.
Robins T, Carlsson J, Sunnerhagen M, Wedell A, Persson B. Molecular model of human CYP21 based on mammalian CYP2C5: structural features correlate with clinical severity of mutations causing congenital adrenal hyperplasia. Mol Endocrinol. 2006;20:2946–64.
Pey AL, Stricher F, Serrano L, Martinez A. Predicted effects of missense mutations on native-state stability account for phenotypic outcome in phenylketonuria, a paradigm of misfolding diseases. Am J Hum Genet. 2007;81:1006–24.
Alibés A, Nadra AD, De Masi F, Bulyk ML, Serrano L, Stricher F. Using protein design algorithms to understand the molecular basis of disease caused by protein-DNA interactions: the Pax6 example. Nucleic Acids Res. 2010;38:7422–31.
Minutolo C, Nadra AD, Fernández C, Taboas M, Buzzalino N, Casali B, Belli S, Charreau EH, Alba L, Dain L. Structure-based analysis of five novel disease-causing mutations in 21-hydroxylase-deficient patients. PLoS One. 2011;6:e15899.
Worth CL, Preissner R, Blundell TL. SDM—a server for predicting effects of mutations on protein stability and malfunction. Nucleic Acids Res. 2011;39:W215–22.
Zhao B, Lei L, Kagawa N, Sundaramoorthy M, Banerjee S, Nagy LD, Guengerich FP, Waterman MR. Three-dimensional structure of steroid 21-hydroxylase (cytochrome P450 21A2) with two substrates reveals locations of disease-associated variants. J Biol Chem. 2012;287:10613–22.
Pallan PS, Wang C, Lei L, Yoshimoto FK, Auchus RJ, Waterman MR, Guengerich FP, Egli M. Human Cytochrome P450 21A2, the major steroid 21-hydroxylase: structure of the enzyme progesterone substrate complex and rate-limiting C-H bond cleavage. J Biol Chem. 2015;290:13128–43.
Haider S, Islam B, D’Atri V, Sgobba M, Poojari C, Sun L, Yuen T, Zaidi M, New MI. Structure-phenotype correlations of human CYP21A2 mutations in congenital adrenal hyperplasia. Proc Natl Acad Sci USA. 2013;110:2605–10.
Bruque CD, Delea M, Fernández CS, Orza JV, Taboas M, Buzzalino N, Espeche LD, Solari A, Luccerini V, Alba L, Nadra AD, Dain L. Structure-based activity prediction of CYP21A2 stability variants: a survey of available gene variations. Sci Rep. 2016;6:39082.
Database of CY21A2 by the Human Cytochrome P450 (CYP) Allele Nomenclature Committee: https://www.pharmvar.org/htdocs/archive/cyp21.htm. Accessed 14 Feb 2018.
Araújo RS, Mendonca BB, Barbosa AS, Lin CJ, Marcondes JA, Billerbeck AE, Bachega TA. Microconversion between CYP21A2 and CYP21A1P promoter regions causes the nonclassical form of 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2007;92:4028–34.
Menabò S, Balsamo A, Baldazzi L, Barbaro M, Nicoletti A, Conti V, Pirazzoli P, Wedell A, Cicognani A. A sequence variation in 3′UTR of CYP21A2 gene correlates with a mild form of congenital adrenal hyperplasia. J Endocrinol Investig. 2012;35:298–305.
Concolino P, Rizza R, Costella A, Carrozza C, Zuppi C, Capoluongo E. CYP21A2 intronic variants causing 21-hydroxylase deficiency. Metabolism. 2017;71:46–51.
Nermoen I, Brønstad I, Fougner KJ, Svartberg J, Øksnes M, Husebye ES, et al. Genetic, anthropometric and metabolic features of adult Norwegian patients with 21-hydroxylase deficiency. Eur J Endocrinol. 2012;167:507–16.
Brønstad I, Breivik L, Methlie P, Wolff AS, Bratland E, Nermoen I, Løvås K, Husebye ES. Functional studies of novel CYP21A2 mutations detected in Norwegian patients with congenital adrenal hyperplasia. Endocr Connect. 2014;3:67–74.
Barbaro M, Baldazzi L, Balsamo A, Lajic S, Robins T, Barp L, Pirazzoli P, Cacciari E, Cicognani A, Wedell A. Functional studies of two novel and two rare mutations in the 21-hydroxylase gene. J Mol Med (Berl). 2006;84:521–8.
Nunez BS, Lobato MN, White PC, Meseguer A. Functional analysis of four CYP21 mutations from spanish patients with congenital adrenal hyperplasia. Biochem Biophys Res Commun. 1999;262:635–7.
Kirby-Keyser L, Porter CC, Donohoue PA. E380D: a novel point mutation of CYP21 in an HLA-homozygous patient with salt-losing congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Mutat. 1997;9:181–2.
Hsu NC, Guzov VM, Hsu LC, Chung BC. Characterization of the consequence of a novel Glu-380 to Asp mutation by expression of functional P450c21 in Escherichia coli. Biochim Biophys Acta. 1999;1430:95–102.
Kharrat M, Tardy V, M’Rad R, Maazoul F, Jemaa LB, Refaï M, Morel Y, Chaabouni H. Molecular genetic analysis of Tunisian patients with a classic form of 21-hydroxylase deficiency: identification of four novel mutations and high prevalence of Q318X mutation. J Clin Endocrinol Metab. 2004;89:368–74.
Jiang L, Song LL, Wang H, Wang JL, Wang PP, Zhou HB, Zhang XL. Identification and functional characterization of a novel mutation P459H and a rare mutation R483W in the CYP21A2 gene in two Chinese patients with simple virilizing form of congenital adrenal hyperplasia. J Endocrinol Invest. 2012;35:485–9.
Nikoshkov A, Lajic S, Vlamis-Gardikas A, Tranebjaerg L, Holst M, Wedell A, Luthman H. Naturally occurring mutants of human steroid 21-hydroxylase (P450c21) pinpoint residues important for enzyme activity and stability. J Biol Chem. 1998;273:6163–5.
Finkielstain GP, Chen W, Mehta SP, Fujimura FK, Hanna RM, Van Ryzin C, McDonnell NB, Merke DP. Comprehensive genetic analysis of 182 unrelated families with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2011;96:E161–72.
Krone N, Rose IT, Willis DS, Hodson J, Wild SH, Doherty EJ, Hahner S, Parajes S, Stimson RH, Han TS, Carroll PV, Conway GS, Walker BR, MacDonald F, Ross RJ, Arlt W, United Kingdom Congenital adrenal Hyperplasia Adult Study Executive (CaHASE). Genotype-phenotype correlation in 153 adult patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency: analysis of the United Kingdom Congenital adrenal Hyperplasia Adult Study Executive (CaHASE) cohort. J Clin Endocrinol Metab. 2013;98:E346–54.
Kazmi D, Bailey J, Yau M, Abu-Amer W, Kumar A, Low M, Yuen T. New developments in prenatal diagnosis of congenital adrenal hyperplasia. J Steroid Biochem Mol Biol. 2017;165:121–3.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors (PC and AC) declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Concolino, P., Costella, A. Congenital Adrenal Hyperplasia (CAH) due to 21-Hydroxylase Deficiency: A Comprehensive Focus on 233 Pathogenic Variants of CYP21A2 Gene. Mol Diagn Ther 22, 261–280 (2018). https://doi.org/10.1007/s40291-018-0319-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-018-0319-y





