Abstract
Background
Treatment decision-making in pediatric oncology can be complex. Recent advances in genome sequencing and novel or ‘personalized’ therapies potentially increases the complexity of decision-making and treatment options.
Objectives
This study explored the views and experiences of healthcare providers (HCPs) and parents with respect to decision-making in difficult-to-treat cancers, including genomic decision-making.
Methods
A two-phase qualitative study was undertaken in which oncologists and nurses and parents of children with relapsed and refractory cancers were interviewed using a semi-structured interview guide. Data were analyzed thematically, with a focus on measurable themes relevant to the development of candidate attributes for a discrete choice experiment (DCE). Secondly, a review of studies that utilized stated preference experiments in the fields of genomics, medical decision-making, and pediatrics was undertaken and compared with the candidate attributes identified from interviews.
Results
Six candidate attributes were developed from the interview themes: clinical benefit, quality of life (QoL) including both treatment effects and functionality, likelihood of a target, cost (who pays), recommendation of HCP or extent family supported the decision, and whether a biopsy was needed. Two further candidate attributes were identified from the literature review: severity of illness and cost (dollar amount).
Conclusions
This study identified eight candidate attributes that will be further validated prior to developing a DCE aimed at better understanding factors influencing decision-making related to genomic sequencing and personalized medicine. This study and the proposed DCE will contribute to improving ethical and clinical practices in the application of novel genomic technology in pediatric oncology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Healthcare providers reported that level of scientific evidence, perceived benefit to the child, and family preferences were important in treatment decision-making for difficult-to-treat childhood cancers. |
Parents perceived no real choice in treatment decision-making but relied on oncologist expertise and valued increased survival and quality of life for their child with difficult-to-treat cancer. |
Eight candidate attributes were identified that will be used to investigate decision-making specifically related to use of genomics and personalized medicine in complex childhood cancers. |
1 Introduction
There have been significant improvements in survival outcomes for children with cancer over the past half century [1, 2]. Decision-making for frontline treatments of common childhood cancers is relatively straightforward when there is a well-established treatment protocol or clinical trial and where survival rates are high [3]. In cases of rare, relapsed or refractory cancers [hereafter referred to as difficult-to-treat cancers], where there may not be a recognized standard of care, decision-making becomes more complex and may involve trade-offs between survival and quality of life (QoL) [4]. In this context, greater sharing of decision-making between families and clinicians is recognized as an appropriate process [3].
A small number of qualitative and quantitative studies have examined complex treatment decision-making in childhood cancer. Differences in preferences between clinicians and parents in decision-making have been identified, including evidence that parents may favor continued attempts at curative treatment longer than their physician [5, 6]. Factors identified as important in decision-making include the child’s prognosis and increasing chance of survival [4, 7,8,9] and child QoL including physical factors such as pain, amount of hospitalization, cognitive impacts, and social functioning [4, 10]. Parent treatment preferences are important to physicians [4, 11,12,13], as are family factors such as the financial impacts of treatment decisions [4, 8].
Recent advances in genomic sequencing in pediatric oncology have added yet another layer of decision-making complexity [14, 15]. Genomic sequencing technology offers a pathway toward potentially finding a drug therapy targeted at a mutation in an individual’s cancer [16]. This approach, referred to as personalized medicine, means there are now more factors to be taken into account, including whether to offer genomic testing, accessibility and cost of new drugs that may be identified by testing, communication of additional genomic findings, and management of parent and patient expectations [14, 17,18,19,20]. Little is known about what factors influence decision-making to utilize genomic testing and the perceived role and utility value of genomics in treatment decision-making [19]. This is important information as genomics becomes a standard element of clinical care and also in developing consensus guidelines for clinical implementation of genomics programs [19].
We conducted a qualitative study to (Aim 1) explore the views and experiences of healthcare providers (HCPs) and parents regarding treatment decision-making for children with difficult-to-treat cancers, including their perspectives on genomic sequencing as a pathway to identifying novel treatment options; and (Aim 2) analyze this qualitative data in order to inform the development of candidate attributes for a future planned discrete choice experiment (DCE). Ultimately, the DCE will investigate which factors HCPs, parents, and community members give most weight to in decision-making about genomics and novel drug treatments. The focus of this paper is on the qualitative research undertaken for the development of the candidate attributes and levels to inform the subsequent DCE.
2 Methods
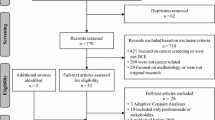
A two-step approach was utilized in this study. With institutional ethics approval, semi-structured interviews were conducted in Step 1 with oncology HCPs (Phase 1: HREC: 34104C) and with parents of children with refractory or relapsed cancer (Phase 2: HREC: 37008). In Step 2, a review of published stated-preference experiments in the fields of genomics, medical decision-making, and pediatrics was conducted and compared with the candidate attributes identified from the qualitative studies.
2.1 Qualitative Study
The qualitative study of HCPs and parents respectively were conducted within an interpretivist paradigm, utilizing interpretive description (ID) methodology specifically developed for practically oriented inquiry in healthcare settings [21, 22]. ID utilizes inductive analytic techniques in order to understand clinical phenomena, which ultimately is intended to inform disciplinary thought or understanding [21]. In keeping with ID, the focus of this study was on eliciting subjective accounts of decision-making arising from HCPs and parents making decisions in the context of difficult-to-treat cancers, including experiences related to genomic sequencing and targeted therapies. The conduct and reporting of the study was guided by the guidelines for reporting formative qualitative research to support the development of quantitative preference studies and the Consolidated Criteria for Reporting Qualitative Research criteria for qualitative research [23, 24].
2.1.1 Researcher Characteristics and Reflexivity
The first author and study PI (MM), an experienced oncology mental health clinician and researcher, conducted interviews. MM was known to some of the HCPs as an oncology and/or research colleague. The inclusion of an insider researcher [25] in the study design was deliberate as they may be perceived as trustworthy and knowledgeable by participants. None of the parents interviewed knew MM but were aware of her professional role. As an oncology mental healthcare clinician, MM is highly experienced in conducting interviews with oncology families and responding sensitively to parents’ emotional states and distress.
2.1.2 Sampling Strategy
Purposive sampling was utilized to recruit HCP participants. Consultant oncologists and specialist oncology nurses involved in the clinical care of patients were eligible to participate. HCPs were recruited from The Royal Children’s Hospital (RCH) in Melbourne, Australia and via the mailing list of the peak oncology professional body, the Australian and New Zealand Children’s Haematology and Oncology Group (ANZCHOG). Interested HCPs responded to study email invitations by directly contacting the study PI. Interview times were scheduled at a time convenient to participants. Participating in the interview was considered implied consent. A sample size of 20–25 HCPs was initially estimated to sufficiently approach saturation to identify key themes for attribute development. Data saturation, as described by Saunders et al. [26], was perceived by the research interviewer to be achieved after approximately 15 interviews. Recruitment was continued, however, to achieve input from the majority of pediatric oncology sites across Australia and New Zealand in order to enhance the validity and generalizability of the study findings.
The parent sample was recruited from the RCH. Parents of a child with a difficult-to-treat diagnosis (prognosis < 30%), who had consented to a pilot genomic sequencing study, were over 18 years, and had adequate English to participate in an interview were eligible. Thirty-one families were recruited to the pilot genomics study. Of these, four parents declined to be approached for interview, four children died before consent could be obtained, one child was deemed ineligible, and three families were not approached at the request of clinical staff. The remaining 19 families were approached for this interview study and all (100%) consented to participate. Parents of children who had agreed to be approached for this study were contacted by the study PI. Written and verbal information about the study was provided and written consent obtained. The recruitment strategy exhausted the eligible study population, and data saturation was deemed to be sufficiently achieved. Specifically, similar themes emerged from later interviews with little new information evident.
2.1.3 Data Collection
Individual semi-structured interview guides were used in order to provide participants with the safest possible environment to express any divergent views. Interview guides were developed using expert team opinion and guided by literature reviews examining HCP and parent perspectives on treatment decision-making in pediatric oncology. Interview questions were open-ended, with descriptions of challenging case scenarios utilized to elicit HCP examples of complex decision-making. For the HCPs, interview topics included factors and processes used in decision-making and experiences with decision-making related to genomics and personalized medicine. Demographic data were also collected. For the parent interviews, questions were designed to elicit the factors parents had considered in treatment decision-making for their child and specifically in consenting to genomic sequencing (see electronic supplementary material [ESM], Table 1). All interviews were audio-recorded and professionally transcribed verbatim.
2.1.4 Data Analysis
Interview data were analyzed thematically, using the approach described by Braun and Clarke [27]. De-identified interview transcripts were imported into QSR International’s NVivo 12 software for coding and analysis. For the HCP interviews, two members of the research team (MM and LM) independently coded the first seven interviews, using line-by-line coding. These initial codes were compared, consensus reached on differences, and a draft coding scheme was developed. This was discussed and finalized with members of the research team who have expertise in thematic analysis. The remaining interviews were coded using this schema by LM. Analysis of de-identified parent interviews was conducted in a similar manner.
For the purposes of this study, data analyses focused upon the extrinsic factors described by HCPs and parents as important in decision-making, as these were quantifiable and relevant to the development of DCE attributes. Additional themes that emerged from the data that were intrinsic to HCPs or parents, and thus not able to be actionable for development as attributes for a choice experiment, are not included in this paper. Examples of these themes included the nature of the oncologist–parent therapeutic relationship, the importance for parents of maintaining hope for their child, and clinician factors such as their level of clinical experience, communication style, and perceived caution or enthusiasm related to experimental treatments (see ESM, Table 3).
2.2 Comparison with Attributes in Published Stated-Preference Studies
The coding schema for the HCP and parent interviews provided the key source for the development of attributes to be used in our DCE study (see ESM, Table 3). In order to ensure, however, that we had not missed any potential attributes and to consider how previous studies had conceptualized attributes in common with our candidate attribute set, we reviewed studies that utilized stated preference experiments (DCEs and conjoint analyses) in the fields of genomics, medical decision-making, or pediatrics. Studies were sourced from a database, commenced in 2009 by the Centre for Health Economics Research and Evaluation, University of Technology Sydney, of publications of preference studies (e.g., conjoint analyses and DCEs; n = 1910). Studies were included if they were in the fields of interest and reported on the attributes and levels used. These attributes were then compared with the candidate attributes developed from the interview data in terms of the range of themes and conceptualization of attribute levels.
3 Results
3.1 Results of Qualitative Study
The HCP sample included 22 participants (15 oncologists, 7 nurses) from 11 oncology centers across Australia and New Zealand, with a mean length of experience of 15.73 years. Interviews were conducted in person at the RCH (n = 13) or via Skype or telephone (see Table 1). The parent sample (n = 20) consisted of 19 parents (including two parents from one family who both requested to be interviewed) and one young adult patient (19.3 years) who requested to be interviewed as she perceived herself as the primary decision-maker regarding her treatment and declined consent for her parents to be interviewed. Patients ranged in age from 1.8 to 19.3 years. Mean time since initial cancer diagnosis was 3.2 years (range 1–13.6 years) and 11 had experienced at least one relapse. Fourteen interviews were conducted in person; the remainder by telephone (see Table 2).
3.1.1 HCP Interviews
HCPs were asked to consider decision-making generally in the context of difficult-to-treat cancers and then more specifically genomic decision-making. Factors considered by HCPs fell broadly into three themes: (1) scientific evidence, (2) perceived benefit and QoL, and (3) family preferences. Direct quotations illustrating the themes and the candidate attribute to which they contribute are described below and in Table 3.
3.1.1.1 Scientific Evidence
A major theme for HCPs was the importance of evidence upon which to base estimations of whether and to what extent a child could benefit from a particular treatment pathway.
If there isn’t a standard of care that we would follow then they [oncologist] go looking for what’s available, evidence-based, always evidence-based. (Nurse 3)
All oncologists reported examining the level of evidence for possible treatments, describing a rigorous, deliberative process of evidence seeking and consultation.
I would see what clinical trials that we have currently open in this institution and then I would also search via the internet and look to see what other studies are available. I’d seek advice from other centers either in Australia but generally from other colleagues overseas where there may be newer approaches to treatment, particularly of the phase I studies around what we didn’t necessarily have access to, so really trying to identify other people’s experience and evidence around what may or may not be of benefit. (Oncologist 12)
Specifically related to genomically guided treatment, oncologists raised the issue of evidence, or lack of evidence, of targeted therapies involving novel drugs. A number of oncologists suggested that there should be a sound scientific rationale for any treatments offered. Although oncologists acknowledged the promise of personalized medicine, they identified the importance of such treatments being biologically plausible.
I would hope then that people are still making a decision based on excellent biology for those clinical trials where the evidence is lacking. (Oncologist 4)
3.1.1.2 Perceived Benefit and Child’s Overall Quality of Life
HCPs described considering patients’ overall prognosis and the potential benefit (or not) of further treatment for the patient. This included offering palliative care as an option where the perceived benefit of further treatment was minimal or uncertain. A number of oncologists expressed concern about offering families treatments that were of little or no perceived benefit.
If something is not going to work or it’s deemed relatively futile then I generally don’t think it’s fair to offer it to a family. (Oncologist 8)
Responses indicated that HCPs attempted to make decisions in the best interest of the child, and this frequently related to consideration of the child’s QoL, beyond benefit in terms of survival. QoL factors appeared to be both related to treatment side effects and drug toxicities, as well as functionally how the child may be affected in daily life.
How do you say, if you do this, you’re just going to make them miserable? Sick and miserable and they’re not going to have time to do the things they want to do. (Nurse 3)
Oncologists expressed similar views related to personalized medicine and child QoL. The likelihood of benefit to patients and the potential for side effects or toxicities of novel drugs were again identified as important factors when considering whether to offer or recommend a genomically guided treatment.
3.1.1.3 Family Preferences
Oncologists and nurses identified the importance of considering families’ preferences in treatment decision-making, which included providing families with information, assessing families’ level of understanding, and ascertaining whether families wanted to continue treatment or commence palliation. They frequently described a process of shared decision-making and, although child preferences were mentioned at times, more commonly they referred to consideration of parents’ wishes.
I don’t think we need to treat it at any cost, and I think the families’ preferences come into it. And I think that it becomes more complex when families are very hungry for any kind of treatment at all. (Oncologist 9)
3.1.1.4 Issues Specific to Genomic Sequencing
At the time the interviews were conducted, the majority of the HCPs reported having limited experience with genomics. Some centers had recently commenced or were planning to commence participation in a genomic sequencing trial. The issue of the likelihood of genomic sequencing finding a mutation targetable by a drug was frequently mentioned as a factor that would influence whether it was likely to be recommended.
It’s not for every patient, and there’s not always a target. I think..that there’s probably a target 10% of the time, like a real target. (Oncologist 2)
A further concern frequently raised in the interviews related to the availability of drugs if an actionable target was identified and the costs associated with experimental drugs and who could or should pay for these.
And the question is should we be offering it to every single patient in that circumstance. Do we pay for it? You know, are we in a position to be doing that because it’s not a proven therapy or proven testing? (Oncologist 6)
The majority of oncologists referred to the need for a cautious approach in regard to managing expectations related to novel targeted therapies.
I feel like there’s a huge amount of enthusiasm, but I think that it relates more to the potential than the actuality at this point. I don’t know that we’ve really demonstrated major practice shifts in terms of actual therapies at this stage. (Oncologist 15)
3.1.2 Parent Interviews
With respect to treatment decision-making, parents perceived little choice and reported relying on the expertise of medical staff. Consideration of their child’s QoL was important for parents but their child’s survival was the predominant factor influencing their decisions. Direct quotations illustrating the themes and the candidate attribute to which they contribute are described below and in Table 4.
3.1.2.1 Recommendation from Oncologist
A major theme from parents related to treatment decision-making was that they relied heavily on the recommendation of their child’s oncologist. The majority of parents reported they had great faith in the expertise of the oncologist and treatment team. Particularly at the time of diagnosis, most parents felt they did not have the expertise to participate in decision-making.
They’re the professionals and they know what they’re doing. We’ve walked into this, especially first-time round knowing nothing about the disease or procedures or anything. This is a whole new world to us, so you’ve got to have a hundred percent faith in the hands that are looking after your children. (Mother 1)
The majority of parents examined the evidence for treatment options in a limited manner, and some not at all, particularly at the time of the initial diagnosis.
We did have a look [on the internet] but I found that a lot of the information that was given out to us was also good so the internet sort of kind of like just—what’s the word—confirmed, yeah what we were told sort of thing. (Mother 18)
3.1.2.2 Feeling of No Real Choice
Overall, parents perceived they had little choice with respect to treatment options.
That’s essentially what we’re doing; we’re handing over the care of our child to the treating team. And that’s the only choice you do have, whether you do that or not. (Father 19)
Following their child’s relapse, some parents perceived they were offered choices with respect to next treatments, but even in these circumstances, parents reported they relied heavily on the advice of their child’s oncologist. In these circumstances not accepting the treatment option offered would mean the only alternative for their child would be palliative care.
I do feel like it was [radiation] or nothing. The difference was, you know, like 6 to 12 months without radiation and 12 to 18 months with radiation, so it was almost like well we have to. It’s the only thing we can do at the moment, just to give us a bit more time with him. (Mother 1)
One family in the study had opted not to proceed with chemotherapy offered (which was not likely to be curative) on the basis that their child did not wish to have further treatment or be at the hospital and away from home.
3.1.2.3 Effects on Their Child
While most parents did not perceive a choice in treatment options, it was evident in their responses that they considered the risks (and benefit) to their child. Parents also demonstrated that they thought about their child’s QoL, particularly in the case of relapse and in undertaking second or third lines of treatment.
At that stage things were going really, really bad and [patient] was very, very sick. At one stage I wanted to stop treatment, but it has to be on both parents’ decision and [Husband] didn’t want to. (Mother 2)
3.1.2.4 Decision-Making and Genomics
All of the families interviewed had consented to having their child’s genome sequenced. When asked about this decision, all parents (and the young adult patient) described this as an easy decision to make.
If they can find something that gives you another treatment option, of course, yeah. (Young adult patient)
What if we do nothing? Oh she’ll die. Okay then where’s your pen? (Father 3)
The non-invasive nature of the sequencing was also a factor in parents’ willingness to consent. As all patients had fresh biopsy tissue stored, only a blood sample was required for the testing, so there was minimal impact on the child. A small number of parents indicated that they were unsure whether they would have consented if a new biopsy was required.
3.1.3 Development of Candidate Attributes
On the basis of the themes that emerged from the interviews, a draft list of candidate attributes was developed (see Table 5). These attributes reflect the themes from the HCP and parent interviews that are extrinsic to the individual in the context of decision-making for genomics and precision medicine. Moreover, they represent concepts that can be expressed in a quantifiable way, be it in terms of absolute magnitudes or relative rankings, to produce variation between scenarios.
3.2 Results of Literature Review
Twenty-eight papers met the inclusion criterion; these are summarized in the ESM, Table 2. Of the candidate attributes derived from the qualitative study, cost was included most often in those papers (18 occurrences), typically as the dollar cost of the diagnostic test, medicine, or genomic/treatment being investigated. Of the remaining candidate attributes, some conceptualization of benefit treatment or test availability, level of evidence, who made the recommendation/discussed results or the extent of support for the test/service, were identified in multiple papers. QoL was included specifically in one paper only. In addition, attributes presenting concepts of disease risk and severity occurred in 12 of the studies reviewed (see Table 5).
3.3 Refinement of Candidate Attributes
A set of candidate attributes and levels were developed for the proposed DCE and are presented in Table 6. The list includes six attributes arising from the qualitative research (note that for design purposes, the ‘Recommend’ and ‘Support’ attributes count as one since only one appears in the HCP and Parent versions, respectively). In describing QoL effects, it was noted that these might arise due to the occurrence of symptoms and side effects or to changes in a child’s functioning. However, it was considered implausible that these attributes could vary separately. Thus, while they have been described separately in Table 6, they are considered to be linked (one attribute). Two additional candidate attributes arising from the literature review were included; prognosis, reflecting aspects of disease severity, and cost specified in dollar amounts. It is likely that the attribute on severity did not emerge explicitly from the interviews because severity did not vary in the study context. HCPs were asked to consider decision-making related to relapsed and refractory cancers where prognosis was poor. Similarly, parents interviewed in this study had children who had already been identified as having a poor prognosis (i.e., < 30% chance of survival). The second candidate attribute added on the basis of the literature review was dollar cost (as distinct from ‘who pays’, which emerged as an important factor in the qualitative study). The inclusion of dollar values allows the choice relationship between attributes to be expressed as a marginal willingness to pay (e.g., how much would families be willing to pay for an additional month of survival). To facilitate development of realistic scenarios, the type of target ‘treatment’ was restricted to drug-based therapy, allowing a specific funding stream to be named and manipulated in the final DCE (e.g., the Pharmaceutical Benefits Scheme, the national public health funder for drugs in Australia).
Subsequently, levels for each candidate attribute were developed based on plausible ranges. For the attributes reflecting clinical outcomes (severity, target, and benefits), levels were developed based on clinical expert opinion and consultation with clinical oncologists and oncology researchers. The levels chosen reflect what is currently possible with regard to identification of targets for treatment, as well as the range of benefits (both in terms of the impact on survival and functioning) observed with a range of subsequent treatments (and were not treatment specific). The levels determined for the cost amounts were based on what has been observed in terms of annual costs of new targeted therapies on the Australian Pharmaceutical Benefits Scheme, with who pays reflecting the range of what is possible in the Australian institutional context. Finally, levels for the attributes recommendation/support and biopsy are dichotomous (yes/no), determined by what was observed in the interviews and is physically possible for these domains.
4 Discussion
The current study contributes to the existing small body of literature that has examined HCP and parent perspectives on treatment decision-making in childhood cancer. Previous studies have suggested that understanding factors influencing decision-making may facilitate improved communication between HCPs and parents, a factor that is likely to be particularly important in the context of new genomic technologies and targeted therapies. The importance of evidence-based decision-making was strongly endorsed by HCPs in this study and was perceived as a challenging aspect of genomic approaches. For parents, the importance of extending their child’s life was consistent with previous studies that have shown parents report prolonging life, spending more time with their child, and child QoL as key factors when considering further treatment during end-of-life care [12, 28, 29]. Child QoL was an important consideration for both HCPs and parents, a factor that has consistently been shown to be important in oncology decision-making, particularly where there are trade-offs between QoL and survival [4, 12].
In the context of difficult-to-treat cancers, HCPs reported understanding the families’ preferences was an important component of decision-making and this would include opting for no further treatment if that were the parents’ or child’s wishes, a finding consistent with previous studies examining end-of-life decision-making [8, 30]. Conversely, parents described a strong reliance and trust in the child’s medical team recommendations and expertise. These findings are consistent with previous literature which has identified recommendations received from HCPs [30, 31] as well as the importance of trust and high-quality communication as factors important to parents of children with cancer [7, 28, 31].
Consent to genomic testing was consistently described as a straightforward decision by parents, a finding that has been reported in recent studies examining the ethical implications of genomics in pediatric oncology [19, 32]. For a number of parents, the relatively non-invasive nature of genomic testing that did not require an additional biopsy was an influencing factor in consenting to testing. Re-biopsying has previously been identified as a limiting factor in oncologists’ willingness to refer patients for genomic testing but did not emerge as a theme for oncologists in this study [33].
Consistent with previous research, parents identified testing as offering new hope [19]. Hope, however, is another intrinsic factor not suitable for use as an attribute. HCPs were more likely to express concern over the low likelihood of finding a treatable target, particularly in relation to managing parents’ expectations; these factors have previously been identified as an ethical concern in the field of genomics [20, 34]. HCPs also raised concerns over who should pay for testing and expensive novel drug therapies, which has also previously been identified as an ethical and social issue in another interview study of clinicians and research scientists [14]. This was not raised by parents, most likely because the parents in this study were participating in a clinical trial and did not have any out-of-pocket expenses.
The targeted literature review of DCE attributes conducted as part of this study showed strong support for the candidate attributes identified from the interview data. A total of eight candidate attributes were identified; six from interviews with HCPs and parents and a further two from the literature review. This number is consistent with a feasible sample size in the pediatric oncology setting, where there is a relatively small total population of HCPs and parents. While there is no absolute maximum as to the number of attributes in a DCE study, eight is within the range of what has been included in other DCEs [35].
4.1 Limitations
A limitation of the current study is that the parent sample was recruited from one institution. Furthermore, the sample included only parents who had already consented to genomic sequencing, which may be considered a selection bias. It is possible recruiting parents from different healthcare environments, or who had not consented to genomic sequencing, may have identified other attributes. Positively, however, the literature review examining attributes in studies looking more broadly at genomics and pediatrics indicated a high degree of concordance with the interview data. It is also important to note that the interviews revealed attributes that appeared to be of high importance to HCPs (e.g., who pays) or parents (e.g., biopsy), that were not widely identified in the literature. This highlights the importance of undertaking qualitative research to establish attributes and levels for choice experiments rather than relying only on existing literature or expert opinion.
5 Conclusions
Overall, this study was able to identify a set of measurable candidate attributes towards the development of a future choice experiment. The next step required is for the candidate attributes to undergo testing for respondent understanding and acceptability as part of piloting of the subsequent DCE. This study and the DCE will contribute novel data to better understand decision-making related to genomics and contribute to ethical and clinical practices in the application of this novel technology.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Forrest SJ, Geoerger B, Janeway KA. Precision medicine in pediatric oncology. Curr Opin Pediatr. 2018;30(1):17–24.
Saletta F, Seng M, Lau L. Advances in paediatric cancer treatment. Transl Pediatr. 2014;3(2):156–82.
Whitney S, Ethier A, Fruge E, Berg S, McCullough L, Hockenberry M. Decsion making in pediatric oncology: who should take the lead? The decisional priority in pediatric oncology model. J Clin Oncol. 2006;24(1):160–5.
Henrich N, Marra C, Gastonguay L, Mabbott D, Malkin D, Fryer C, et al. De-escalation of therapy for pediatric medulloblastoma: trade-offs between quality of life and survival. Pediatr Blood Cancer. 2014;2014(61):1300–4.
Rosenberg AR, Orellana L, Kang T, Geyer R, Feudtner C, Dussel V, et al. Differences in parent-provider concordance regarding prognosis and goals of care among children with advanced care. J Clin Oncol. 2014;32(27):3005–11.
Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: parental optimism and parent-physician interaction. J Clin Oncol. 2007;25(11):1357–62.
Coyne I, Amory A, Kiernan G, Givson F. Children’s participation in shared decision-making: children, adolescents, parents and healthcare professionals’ perspectives and experiences. Eur J Oncol Nurs. 2014;18:273–80.
Kang T, Hexem K, Localio R, Aplenc R, Feudtner C. The use of chemotherapy in pediatric oncology patients: a national survey of pediatric oncologists. Pediatr Blood Cancer. 2013;60:80–94.
Tomlinson D, Bartels U, Gammon J, Hinds PS, Volpe J, Bouffet E, et al. Chemotherapy versus supportive care alone in pediatric palliative care for cancer: comparing the preferences of parents and health care professionals. Can Med Assoc J. 2011;22:E1252–8.
Mack J, Hilden J, Watterson J, Moore C, Turner B, Grier H, et al. Parent and physician perspectives on quality of care the end of life in children with cancer. J Clin Oncol. 2005;23(36):9155–61.
Bartholdson C, Lutzen K, Blomgren K, Pergert P. Experiences of ethical issues when caring for children with cancer. Cancer Nurs. 2015;38(2):125–32.
Tomlinson D, Bartels U, Hendershot E, Maloney A, Ethier M, Sung L. Factors affecting treatment choices in pediatric palliative care: comparing parents and health professionals. Eur J Cancer. 2011;47:2182–7.
van Loenhout RB, van der Geest IM, Vrakking AM, van der Heide A, Pieters R, van den Heuvel-Eibrink MM. End-of-life decisions in pediatric cancer patients. J Palliat Med. 2015;18(8):697–702.
McGowan M, Settersten R, Juengst E, Fishman J. Integrating genomics into clinical oncology: ethical and social challenges from proponents of personalized medicine. Urol Oncol. 2014;32(2):187–92.
Devon KM, Lerner-Ellis JP, Ganai S, Angelos P. Ethics and genomic medicine, how to navigate decisions in surgical oncology. J Surg Oncol. 2015;2015(111):18–25.
Mody RJ, Prensner JR, Everett J, Parsons DW, Chinnaiyan AM. Precision medicine in pediatric oncology: lessons learned and next steps. Pediatr Blood Cancer. 2016;64:e26288.
Johnson TM. Perspective on precision medicine in oncology. Pharmacotherapy. 2017;37(9):988–9.
Clarke AJ. Managing the ethical challenges of next-generation sequencing in genomic medicine. Br Med Bull. 2014;111:17–30.
Marron JM, DuBois SG, Glade Bender J, Kim A, Crompton BD, Meyer SC, et al. Patient/parent perspectives on genomic tumor profiling of pediatric solid tumors: the Individualized Cancer Therapy (iCat) experience. Pediatr Blood Cancer. 2016;63(11):1974–82.
Johnson L, Hamilton K, Valdez J, Knapp E, Baker J, Nichols K. Ethical considerations surrounding germline next-generation sequencing of children with cancer. Expert Rev Mol Diagn. 2017;17(5):523–34.
Thorne S, Kirkham SR, O’Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3(1):1–11.
Hunt M. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res. 2009;19(9):1284–92.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Hollin IL, Craig BM, Coast J, Beusterien K, Vass C, DiSantostefano R, et al. Reporting formative qualitative research to support the development of quantitative preference study protocols and corresponding survey instruments: guidelines for authors and reviewers. Patient. 2020;13(1):121–36.
Greene MJ. On the inside looking in: methodological insights and challenges in conducting qualitative insider research. Qual Rep. 2014;19(29):1–13.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Heinze KE, Nolan MT. Parental decision making for children with cancer at the end of life: a meta-ethnography. J Pediatr Onol Nurs. 2012;29(6):337–45.
Bluebond-Langner M, Belasco J, Goldman A, Belasco C. Understanding parents’ approaches to care and treatment of children with cancer when standard therapy has failed. J Clin Oncol. 2007;25(17):2414–9.
Hinds P, Oakes L, Furman W, Faoppiano P, Olsen M, Quargnenti A, et al. Decsion making by parents and healthcare professionals when considering continued care for pediatric patients with cancer. Oncol Nurs Forum. 1997;24(9):1523–8.
Robertson E, Wakefield C, Shaw J, Darlington A, McGill B, Cohn R, et al. Decision-making in childhood cancer: parents’ and adolescents’ views and perceptions. Support Care Cancer. 2019;27(11):4331–40.
McCullough LB, Slashinski MJ, McGuire AL, Street RL, Eng CM, Gibbs RA, et al. Is whole-exome sequencing an ethically disruptive technology? Perspectives of pediatric oncologists and parents of pediatric patients with solid tumors. Pediatr Blood Cancer. 2016;63(3):511–5.
Cohen B, Roth M, Marron JM, Gray SW, Geller D, Hoang BH, et al. Pediatric oncology provider views on biopsying solid tumors in children with relapsed or refractory disease for the purpose of genomic profiling. Annals Surg Oncology. 2016;23(Suppl 5):990–7.
Tomlinson AN, Skinner D, Perry DL, Scollon SR, Roche ML, Bernhardt BA. “Not tied up neatly with a bow”: Professionals’ challenging cases in informed consent for genomic sequencing. J Genet Couns. 2016;25:62–72.
Muhlbacher A, Johnson F. Choice experiments to quantify preferences for health and healthcare: state of the practice. Appl Health Econ Health Policy. 2016;14(3):253–66.
Bennette C, Trinidad S, Fullerton S, Patrick D, Amendola L, Burke W, et al. Return of incidental findings in genomic medicine: measuring what patients value-development of aninstrument to measure preferences for information from next-generation testing (IMPRINT). Genet Med. 2013;15:873–81.
Carlsen B, Hole A, Kolstad J, Norheim O. When you can’t have the cake and eat it too: a study of medical doctors’ priorities in complex choice situations. Soc Sci Med. 2012;75:1964–73.
Blumenschein P, Lilley M, Bakal J, Christian S. Evaluating stakeholder's perspective on referred out genetic testing in Canada: a discrete choice experiment. Clin Genet. 2016;89(1):133–8.
Severin F, Hess W, Schmidtke J, Mühlbacher A, Rogowski W. Value judgments for priority setting criteria in genetic testing: a discrete choice experiment. Health Policy. 2015;119:164–73.
Powell G, Holmes E, Plumpton C, Ring A, Baker G, Jacoby A, et al. Pharmacogenetic testing prior to carbamazepine treatment of epilepsy: patients' and physicians' preferences for testing and service delivery. Br J Clin Pharmacol. 2015;80(5):1149–59.
Herbild L, Gyrd-Hansen D, Bech M. Patient preferences for pharmacogenetic screening in depression. Int J Technol Assess Health Care. 2008;24(1):96–103.
Herbild L, Bech M, Gyrd-Hansen D. Estimating the Danish populations' preferences for pharmacogenetic testing using a discrete choice experiment. The case of treating depression. Value Health. 2009;12:560–7.
Marshall D, Deal K, Bombard Y, Leighl N, MacDonald K, Trudeau M. How do women trade-off benefits and risks in chemotherapy treatment decisions based on gene expression profiling for early-stage breast cancer? A discrete choice experiment. BMJ Open. 2016;6:e010981.
Torbica A, Fattore G. Understanding the impact of economic evidence on clinical decision making: a discrete choice experiment in cardiology. Soc Sci Med. 2010;70(10):1536–43.
Veldwijk J, Lambooij M, Kallenberg F, van Kranen H, Bredenoord A, Dekker E, et al. Preferences for genetic testing for colorectal cancer within a population-based screening program: a discrete choice experiment. Eur J Hum Genet. 2016;24(3):361–6.
Vermeulen H, Ubbink DT, de Zwart F, Goossens A, de Vos R. Preferences of patients, doctors, and nurses regarding wound dressing characteristics: a conjoint analysis. Wound Repair Regen. 2007;15(3):302–7.
Huang MY, Huston SA, Perri M. Consumer preferences for the predictive genetic test fo rAlzheimer disease. J Genet Couns. 2014;23(2):172–8.
Kilambi V, Johnson F, Gonzalez J, Mohamed A. Valuations of genetic test information for treatable conditions: the case of colorectal cancer screening. Value Health. 2014;17(8):838–45.
Knight S, Mohamed A, Marshall D, Ladabaum U, Phillips K, Walsh J. Value of genetic testing for hereditary colorectal cancer in a probability-based US online sample. Medical Decsion Making 2015.
Hall J, Fiebig D, King M, Hossain I, Louviere JJ. What influences participation in geneti ccarrier testing?: Results from a discrete choice experiment. J Health Econ. 2006;25(3):520–37.
De Abreu Lourenco R, Viney J, M, Haas M, King M, Kenny P. Economic evaluation of genetic screening using choice modelling. 22nd Australian Conference of Health Economics 2001.
Griffith GL, Edwards RT, Williams JM, Gray J, Morrison V, Wilkinson C, et al. Patient preferences and National Health Service costs: a cost-consequences analysis of cancer genetic services. Fam Cancer. 2009;8(4):265–75.
Payne K, Fargher E, Roberts S. Valuing pharmacogenetic testing services: a comparison of patients' and health care professionals' preferences. Value Health. 2011;14(1):121–34.
Regier D, Friedman J, Makela N, Ryan M, Marra CA. Valuing the benefit of diagnostic testing for genetic causes of idiopathic developmental disability: willingness to pay from families of affected children. Clin Genet. 2009;75:514–21.
Dong D, Ozdemir S, Mong Bee Y, Toh S, Bilger M, Finkelstein E. Measuring high-risk patients' preferences for pharmacogenetic testing to reduce severe adverse drug reaction: a discrete choice experiment. Value Health. 2016;19(7):67–75.
Peacock S, Apicella C, Andrews L, Tucker K, Daly M, Hopper J. A discrete choice experiment of preferences for genetic counselling among Jewish women seeking cancer genetics services. Br J Cancer. 2006;95(10):1448–53.
Gray E, Eden M, Vass C, McAllister M, Louviere J, Payne K. Valuing preferences for the process and outcomes of clinical genetics services: a pilot study. Patient. 2016;9:135–47.
Severin F, Schmidtke J, Mühlbacher A, Rogowski WH. Eliciting preferences for priority setting in genetic testing: a pilot study comparing best-worst scaling and discrete-choice experiments. Eur J Hum Genet. 2013;21(11):1202–8.
Turbitt E, Wiest M, Halliday J, Amor D, Metcalfe S. Availability of treatment drives decisions of genetic health professionals about disclosure of incidental findings. Eur J Human Genet. 2014;22(10):1225–8.
Acknowledgements
We acknowledge the funding support for this project from the Victorian Cancer Agency (HSR15034) and the Victorian Governments’ Operational Infrastructure Support Program. We acknowledge the generosity of the families and healthcare providers who participated in this research.
Author information
Authors and Affiliations
Contributions
MM coordinated the study and contributed to the study design, conducted the interviews, undertook data analysis and attribute development, and drafted and revised the manuscript. RL and LG contributed to the study design, data analysis, and attribute development and drafted and revised the manuscript. LM assisted with study coordination, conducted the qualitative data analyses, and revised the paper. EM conducted the DCE literature review, contributed to candidate attribute development, and revised the paper. AC conducted literature reviews, assisted with study coordination, and contributed to revising the paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to report.
Additional information
This article is part of the topical collection “Formative qualitative evidence for health preference and outcomes research”.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McCarthy, M.C., De Abreu Lourenco, R., McMillan, L.J. et al. Finding Out What Matters in Decision-Making Related to Genomics and Personalized Medicine in Pediatric Oncology: Developing Attributes to Include in a Discrete Choice Experiment. Patient 13, 347–361 (2020). https://doi.org/10.1007/s40271-020-00411-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-020-00411-0