Abstract
Lusutrombopag (Mulpleta®), an orally bioavailable, small molecule thrombopoietin receptor agonist, is approved for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. In placebo-controlled phase 3 clinical trials, lusutrombopag significantly increased the proportion of patients who did not require a platelet transfusion prior to the procedure or rescue therapy for bleeding up to 7 days after the scheduled procedure. Lusutrombopag also significantly increased the proportion of patients who were responders (i.e. had a platelet count ≥ 50 × 109/L and an increase of ≥ 20 × 109/L from baseline) compared with placebo. Lusutrombopag is well tolerated, with headache being the most common adverse reaction in lusutrombopag recipients in clinical trials. Thus, lusutrombopag represents a promising emerging therapeutic option for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A thrombopoietin receptor agonist; increases platelet counts by inducing the proliferation and differentiation of megakaryocytes |
Convenient 7-day oral regimen, with treatment starting 8–14 days prior to the scheduled procedure |
Reduces the need for platelet transfusion prior to, or rescue therapy after, a scheduled procedure |
Well tolerated; the most common adverse reaction in clinical trials was headache |
1 Introduction
Thrombocytopenia, defined as a platelet count of < 150 × 109/L [1], is a common haematological abnormality in patients with chronic liver disease, with a prevalence of up to 78% in patients with cirrhosis [2, 3]. The pathogenesis of thrombocytopenia in chronic liver disease is often multifactorial and may involve: decreased levels or activity of thrombopoietin (a growth factor that regulates platelet production); bone marrow suppression (e.g. caused by viruses, alcohol, medications or iron overload); and/or platelet destruction (e.g. by shear stress, immunologic destruction, infection, bacterial translocation or fibrinolysis) [2,3,4,5]. Of note, thrombopoietin regulates platelet production by binding to the extracellular cytokine receptor domains of the thrombopoietin receptor and activating numerous intracellular signal transduction pathways (e.g. JAK and STAT pathways), leading to the maturation of megakaryocytes and release of platelets into the peripheral circulation [2, 5].
Patients with thrombocytopenia and chronic liver disease frequently undergo invasive procedures, such as liver biopsies, large-volume paracentesis, thoracenteses and dental procedures [6]. In patients with thrombocytopenia, such procedures can be associated with an increased risk of bleeding (during or after the procedure) [7, 8], which can complicate routine patient care and may lead to procedure delays or cancellations [4, 6]. Additionally, there is evidence that preoperative thrombocytopenia may be associated with an increased risk of blood transfusion, major complications and death [9].
The standard therapy for thrombocytopenia prior to an invasive procedure is platelet transfusion [3, 10], which can increase platelet counts and reduce the risk of bleeding [10]. However, platelet transfusions are limited by a short duration of efficacy and are associated with possible complications, including the development of antiplatelet antibodies (alloimmunization), febrile non–haemolytic transfusion reactions, the need for hospitalization, iron overload and the risk of infection [3, 6, 10]. Given the limitations and possible complications of platelet transfusions, as well as recent advances in understanding the biology of thrombopoiesis in chronic liver disease, novel therapies are being researched and developed for thrombocytopenia prior to a procedure in patients with chronic liver disease [3, 10, 11]. These include pharmacological agents that target the thrombopoietic pathway in order to increase platelet counts by stimulating the endogenous production of platelets [3, 11].
Lusutrombopag (Mulpleta®) is an orally bioavailable, small molecule thrombopoietin receptor agonist which has been approved in the USA [12], the EU [13] and Japan [14] for the treatment of thrombocytopenia (severe thrombocytopenia in the EU [13]) in adult patients with chronic liver disease who are scheduled to undergo a procedure (invasive procedure in the EU [13]). This article reviews the efficacy and tolerability of lusutrombopag when used in the treatment of thrombocytopenia in patients with chronic liver disease, and summarizes its pharmacological properties.
2 Pharmacodynamic Properties of Lusutrombopag
As a thrombopoietin receptor agonist, lusutrombopag selectively interacts with the transmembrane domain of human thrombopoietin receptors expressed on megakaryocytes [12,13,14]. Through the same signal transduction system as that of endogenous thrombopoietin, lusutrombopag acts to increase platelet counts (and, in turn, correct thrombocytopenia) by inducing the proliferation and differentiation of megakaryocytes from bone marrow progenitor cells [12,13,14,15].
In a preclinical study in knock-in thrombopoietin receptor-Ki/Shi mice, platelet increase ratios (platelet count divided by basal platelet count) were significantly (p < 0.01) higher in mice treated with oral lusutrombopag 10 mg/kg/day for 14 days than those treated with vehicle [16]. The platelet count increase ratio in lusutrombopag-treated mice reached 2.5 on day 14; after discontinuation of treatment at day 14 the platelet increase ratio decreased by day 21 and returned to near-basal levels by day 28. In a separate experiment using the same mouse model, mice treated for 21 days with oral lusutrombopag 10 mg/kg/day had significantly (p < 0.01) higher numbers of megakaryocytes in bone marrow and circulating platelets in the blood than those treated with vehicle [16].
In patients with thrombocytopenia and chronic liver disease, the effect of lusutrombopag on platelet count increase correlated with the area under the concentration-time curve (AUC) across a 0.25–4 mg dose range [12]. Further data on the effect of lusutrombopag on platelet counts in patients with thrombocytopenia and chronic liver disease are discussed in Sect. 4.
At eight times the recommended dosage (Sect. 6), lusutrombopag did not prolong the QT interval to any clinically relevant extent [12].
3 Pharmacokinetic Properties of Lusutrombopag
Lusutrombopag pharmacokinetics are similar between healthy subjects and patients with chronic liver disease [12]. Oral lusutrombopag exhibits dose-proportional pharmacokinetics after the administration of single doses across a dose range of 1–50 mg. In patients with chronic liver disease, lusutrombopag reached peak concentrations (Cmax) 6–8 h after administration [12]. Administration of lusutrombopag with a high-fat meal or calcium carbonate had no clinically significant effects on lusutrombopag pharmacokinetics [17]. Lusutrombopag is highly bound to plasma proteins (> 99.9%) [12]. In healthy subjects, lusutrombopag has a mean apparent volume of distribution of 39.5 L [12].
Lusutrombopag metabolism primarily occurs via CYP4 enzymes, including CYP4A11 [12]. In healthy subjects, the terminal elimination half-life of lusutrombopag was ≈ 27 h, and in patients with chronic liver disease, the mean estimated clearance of lusutrombopag was 1.1 L/h. Lusutrombopag is predominantly excreted in the faeces (83% of the administered dose, with 16% excreted as unchanged lusutrombopag); ≈ 1% of lusutrombopag is excreted in the urine [12].
Based on in vitro studies, lusutrombopag has a low potential to inhibit CYP enzymes, P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), organic anion transporting polypeptide (OATP)-1B1 and -1B3, organic cation transporter (OCT)-1 and -2, organic anion transporter (OAT)-1 and -3, multidrug and toxin extrusion (MATE) proteins MATE1 and MATE2-K and bile salt exporter pump (BSEP) [12]. It is a substrate of P-gp and BCRP. Lusutrombopag does not induce CYP1A2, CYP2C9, CYP3A4, UGT1A2, UGT1A6 or UGT2B7 enzymes in vitro [12]. In clinical drug interaction studies, co-administration of lusutrombopag with cyclosporin or an antacid containing a multivalent cation (calcium carbonate) had no clinically significant effect on lusutrombopag exposure. Similarly, co-administration of lusutrombopag with midazolam (a CYP3A substrate) had no clinically significant effect on midazolam exposure [12].
The pharmacokinetic properties of lusutrombopag are not altered to a clinically relevant extent by age, race/ethnicity, body weight, mild to moderate hepatic impairment (Child-Pugh class A and B), and mild to moderate renal impairment [creatinine clearance (CLCR) 30 to < 90 mL/min] [12]. There are limited data pertaining to the administration of the drug in patients with severe renal impairment (CLCR < 30 mL/min) [12].
4 Therapeutic Efficacy of Lusutrombopag
4.1 In Clinical Trials
The efficacy of oral lusutrombopag in the treatment of thrombocytopenia in patients with chronic liver disease who were scheduled for a procedure was evaluated in two randomized, double-blind, placebo-controlled phase 3 trials, L-PLUS 1 (a multicentre study conducted in Japan; n = 97) [18] and L-PLUS 2 (a global study; n = 215) [19]. The lusutrombopag dosage (3 mg once daily) that was used in the phase 3 trials was earlier determined in a double-blind, placebo-controlled phase 2b dose-finding trial in Japanese patients with thrombocytopenia and chronic liver disease [20]; this trial is not discussed further.
Eligible patients were aged ≥ 20 years in L-PLUS 1 [18] and ≥ 18 years in L-PLUS 2 [19], had thrombocytopenia (baseline platelet count of < 50 × 109/L) associated with chronic liver disease and had an invasive procedure scheduled 9–14 days after initiation of study treatment [18, 19]. Patients undergoing specific invasive procedures (i.e. laparotomy, thoracotomy, craniotomy, open heart surgery or organ resection) were excluded. Other key exclusion criteria included a history of splenectomy or liver transplantation; Child-Pugh class C liver disease; and any other causes of thrombocytopenia or a prothrombotic condition other than chronic liver disease. Concomitant therapies that could influence platelet count (with the exception of rescue therapies and therapies related to the primary procedure) were prohibited in both trials [18, 19]. Baseline patient characteristics were generally similar between the lusutrombopag and placebo groups in each trial [18, 19]. Patients had a mean age of 68 years in L-PLUS 1 [18] and 55–56 years in L-PLUS 2 [19].
In the two trials, patients received lusutrombopag 3 mg or placebo once daily for up to 7 days, initiated 9–14 days before an invasive procedure [18, 19]. If a patient was a responder (defined as having a platelet count ≥ 50 × 109/L with an increase of ≥ 20 × 109/L from baseline) by day 5, 6 or 7, no additional study drug was administered. The most common invasive procedures were percutaneous radiofrequency ablation (RFA)/microwave coagulation therapy and transarterial chemoembolization (TACE) in L-PLUS 1 [18], and endoscopic variceal ligation, endoscopy with or without polypectomy or biopsy, dental extraction and TACE in L-PLUS 2 [19].
Lusutrombopag was superior to placebo with regard to the primary endpoint (defined in Table 1), significantly (p < 0.0001) increasing the proportion of patients not requiring a platelet transfusion before a scheduled procedure and/or with no rescue therapy for bleeding ≤ 7 days post-procedure [18, 19]. In L-PLUS 2, no patients in the lusutrombopag group and two patients (1.9%) in the placebo group required rescue therapy for bleeding ≤ 7 days post-procedure [19]. A sensitivity analysis in L-PLUS 2 using the per-protocol population supported the findings in the intent-to-treat population, with 72.5% (95% CI 62.2–81.4) of lusutrombopag recipients versus 20.2% (95% CI 12.4–30.1) of placebo recipients meeting the primary endpoint (p < 0.0001) [19].
In a key secondary endpoint of each trial, the proportion of patients who were responders was significantly (p < 0.0001) higher in the lusutrombopag group than in the placebo group (Table 1). Among lusutrombopag recipients without platelet transfusion, the median platelet count reached ≥ 50 × 109/L after ~ 5–7 days in both trials [18, 19]. Furthermore, the effect of lusutrombopag on platelet counts was durable. In both L-PLUS trials, the duration of sustained platelet count of ≥ 50 × 109/L was significantly (p < 0.0001) longer in the lusutrombopag group without platelet transfusion than in the placebo group with platelet transfusion (L-PLUS 1, n = 38 and 40, mean 21.09 vs. 6.05 days; L-PLUS 2, n = 74 and 73, median 19.2 vs. 0.0 days). Among lusutrombopag recipients without platelet transfusion in each trial, median platelet counts peaked at 85–87 × 109/L after a mean of 12–13 days [18, 19].
In a pooled post hoc analysis of per-protocol patients in the L-PLUS 1 and L-PLUS 2 trials, a significantly (p < 0.0001) greater proportion of lusutrombopag recipients than placebo recipients did not require a platelet transfusion prior to the invasive procedure or rescue therapy ≤ 7 days post-procedure regardless of whether they had hepatocellular carcinoma (n = 95; 68.0 vs. 8.9%) or other diagnoses of chronic liver disease (n = 175; 77.0 vs. 21.6%) [21]. Similar results in favour of lusutrombopag over placebo were observed across subgroups based on other underlying disease aetiologies, including chronic hepatitis B, chronic hepatitis C, alcoholic hepatitis, non-alcoholic hepatitis, autoimmune hepatitis or other hepatitis or mixed disease aetiology (significance not reported) [22].
4.2 Real-World Data
Interim results are available from an ongoing, multicentre, prospective postmarketing real-world surveillance study of patients (n = 338 at data cut-off) with chronic liver disease and thrombocytopenia undergoing invasive procedures in Japan [23]. At data cut-off (27 September 2018), 300 lusutrombopag recipients (excluding those with platelet transfusion refractoriness) had undergone an invasive procedure; of these, 282 (94.0%) did not require preoperative platelet transfusion. Among evaluable lusutrombopag recipients (n = 286), the mean maximum change from baseline in platelet count was 41.7 ± 31.4 × 109/L. Furthermore, no patients receiving second (n = 20) or third (n = 1) treatments with lusutrombopag required preoperative platelet transfusion [23].
5 Tolerability of Lusutrombopag
Oral lusutrombopag was well tolerated in clinical trials in adult patients with thrombocytopenia associated with chronic liver disease prior to a scheduled procedure [12, 13]. According to pooled data from the two phase 3 trials and the phase 2b trial (see Sect. 4.1), the only adverse reaction occurring in ≥ 3% of lusutrombopag recipients (n = 171 in total) and at a numerically higher rate than in placebo recipients (n = 170) was headache (in 4.7 and 3.5% of patients in the respective groups) [12, 13]. No patients discontinued lusutrombopag treatment due to an adverse reaction [12]. Four lusutrombopag recipients (three in L-PLUS 2 and one in the phase 2b trial) and no placebo recipients died during the trials; none of the deaths were considered to be related to the study drug [18,19,20]. Serious adverse events (SAEs) occurred in 5.3 and 7.1% of patients in the lusutrombopag and placebo groups in the pooled analysis [24]. The most common SAE in the lusutrombopag group was portal vein thrombosis (reported in 1.2% of lusutrombopag recipients and 1.2% of placebo recipients); observed events of portal vein thrombosis were not associated with a marked increase in platelet count [12, 13]. Thrombopoietin receptor agonists have been associated with thrombotic and thromboembolic complications in patients with chronic liver disease. The potential for increased thrombotic risk should be considered when administering lusutrombopag to patients with known risk factors for thromboembolism [12, 13]. Bleeding-related adverse events occurred in 8.8% of lusutrombopag recipients and 15.9% of placebo recipients in the pooled safety population [24].
The safety and tolerability profile of lusutrombopag in the real-world setting (based on available postmarketing surveillance data) is generally consistent with that observed in clinical trials [23]. Among the safety analysis set from the postmarketing real-world surveillance study discussed in Sect. 4.2 (n = 331), SAEs were reported in 8.8% of patients and adverse drug reactions were reported in 3.3% of patients. Six patients had an SAE of portal vein thrombosis, with four of the events considered possibly related to lusutrombopag treatment. There were five deaths reported, all of which were considered to be caused by an underlying disease or complication [23].
6 Dosage and Administration of Lusutrombopag
Lusutrombopag is approved in the USA [12], the EU [13] and Japan [14] for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. In the EU, the approved indication is restricted to patients with severe thrombocytopenia who are scheduled to undergo an invasive procedure [13]. In Japan, lusutrombopag should only be administered when the risk of bleeding is high with regard to clinical laboratory values (e.g. platelet count), clinical symptoms and the type of invasive procedure [14]; for example, the administration of lusutrombopag should be avoided if the procedure involves laparotomy, thoracotomy, craniotomy, open heart surgery or organ resection, as the efficacy and safety of the drug in these procedures has not been established [14].
The recommended dosing regimen of lusutrombopag is 3 mg taken orally, once daily, with or without food, for 7 days [12, 14]. Dosing should be commenced 8–14 days (USA) [12], 8 or more days (EU) [13] or 8–13 days (Japan) [14] prior to a scheduled procedure. If a dose of lusutrombopag is missed, the missed dose should be taken as soon as possible [12, 13], and the normal schedule should be returned to the following day [12]. Platelet counts should be obtained prior to initiation of lusutrombopag therapy, and ≤ 2 days prior to the procedure [12].
There is no known antidote for an overdose of lusutrombopag [12, 13]. In the event of an overdose (in which thrombotic or thromboembolic complications may occur), closely monitor the patient and the patient’s platelet count [12,13,14], and treat any ensuing complications in accordance with the appropriate standard of care [12].
Lusutrombopag should not be administered to patients in an attempt to normalize platelet counts [12], or to patients who are breast-feeding (due to the potential for serious adverse reactions in a breastfed child) [12,13,14]. Consult local prescribing information for further details, including warnings and precautions and information regarding the use of lusutrombopag in special populations.
7 Current Status of Lusutrombopag
Standard therapy for thrombocytopenia prior to an invasive procedure has involved platelet transfusion [3, 10]. However, platelet transfusions are limited by a short duration of efficacy and are associated with several possible complications. Moreover, there is a lack of formal guidelines on the use of platelet transfusions in patients with chronic liver disease, such as regarding the platelet counts at which transfusions are indicated [10]. Other management strategies include splenic artery embolization, transjugular intrahepatic portosystemic shunts (TIPS) and splenectomies, which are invasive, associated with significant risks, costly and not always suitable for patients with advanced liver disease [10]. With recent advances in the understanding of the biology of thrombopoiesis in chronic liver disease, pharmacological agents have been developed that target the thrombopoietic pathway, with the small molecule thrombopoietin receptor agonists avatrombopag [25, 26] and lusutrombopag [12,13,14] now approved for use in the treatment of thrombocytopenia in patients with chronic liver disease prior to a procedure. In phase 3 clinical trials involving such patients, oral lusutrombopag reduced the need for platelet transfusions prior to the procedure or for rescue therapy for bleeding post-procedure (Sect. 4.1). Based on available data, lusutrombopag is well tolerated (Sect. 5). The tolerability profile of lusutrombopag observed in clinical trials was similar to that in placebo recipients; in pooled clinical trial data, the most common adverse reaction was headache. One important consideration in managing thrombocytopenia is balancing the risks of bleeding events and thrombotic events [3, 4]. Based on available evidence, lusutrombopag performs well in this regard; however, special consideration should be applied when administering lusutrombopag to patients with known risk factors for thromboembolism (Sect. 5).
Emerging real world data support the findings from clinical trials that lusutrombopag is efficacious and well tolerated in the treatment of thrombocytopenia in patients with chronic liver disease prior to a scheduled procedure (Sects. 4.2 and 5) [23, 27]. Further support is provided by a pharmacokinetic/pharmacodynamic analysis with a model developed using data from 78 healthy subjects and 349 patients with chronic liver disease [28]. In simulations based on the model, lusutrombopag 3 mg once daily for 7 days prior to a scheduled invasive procedure had an 85.2% probability of efficacy (i.e. achieving a platelet count of ≥ 50 × 109/L), with a low (1.2%) probability of platelet overshooting (platelet count of > 200 × 109/L) [28].
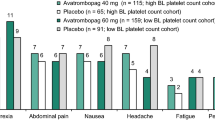
Lusutrombopag has a convenient 7-day oral administration regimen, with treatment starting 8–14 days prior to a scheduled procedure (Sect. 6). Lusutrombopag may offer some potential advantages over avatrombopag. While avatrombopag must be administered with food [25], lusutrombopag can be administered with or without food (Sect. 6). Moreover, the recommended dosage of avatrombopag differs according to the patient’s platelet count prior to the scheduled procedure [25]. To date, there are no direct head-to-head comparisons of lusutrombopag and avatrombopag for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. Comparative efficacy and tolerability trials would be of great interest.
In conclusion, based on currently available data, lusutrombopag is efficacious and well tolerated in the treatment of thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a procedure. Although yet to be definitively demonstrated, lusutrombopag has the potential to reduce the risk of bleeding, improve post-procedural management and reduce the associated delays and cancellations of procedures. Ongoing experience in the clinical trial and/or real-world setting will assist in establishing the position of lusutrombopag for treating thrombocytopenia in patients with chronic liver disease prior to a scheduled procedure. In the meantime, given its convenient once-daily oral regimen and durable therapeutic effects, lusutrombopag is a promising emerging option for treating thrombocytopenia prior to a procedure in this patient population.
Data Selection Lusutrombopag: 118 records identified
Duplicates removed | 24 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 40 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase 1/2 trials) | 26 |
Cited efficacy/tolerability articles | 7 |
Cited articles not efficacy/tolerability | 21 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were lusutrombopag, Mulpleta, S-888711. Records were limited to those in English language. Searches last updated 12 August 2019. | |
References
National Heart Lung and Blood Institute. Thrombocytopenia. 2019. http://www.nhlbi.nih.gov/health-topics/thrombocytopenia. Accessed 22 Aug 2019.
Mitchell O, Feldman DM, Diakow M, et al. The pathophysiology of thrombocytopenia in chronic liver disease. Hepat Med. 2016;8:39–50.
Peck-Radosavljevic M. Thrombocytopenia in chronic liver disease. Liver Int. 2017;37(6):778–93.
Maan R, de Knegt RJ, Veldt BJ. Management of thrombocytopenia in chronic liver disease: focus on pharmacotherapeutic strategies. Drugs. 2015;75(17):1981–92.
Kuter DJ. The biology of thrombopoietin and thrombopoietin receptor agonists. Int J Hematol. 2013;98(1):10–23.
Afdhal N, McHutchison J, Brown R, et al. Thrombocytopenia associated with chronic liver disease. J Hepatol. 2008;48(6):1000–7.
Giannini EG, Greco A, Marenco S, et al. Incidence of bleeding following invasive procedures in patients with thrombocytopenia and advanced liver disease. Clin Gastroenterol Hepatol. 2010;8(10):899–902.
Seeff LB, Everson GT, Morgan TR, et al. Complication rate of percutaneous liver biopsies among persons with advanced chronic liver disease in the HALT-C trial. Clin Gastroenterol Hepatol. 2010;8(10):877–83.
Glance LG, Blumberg N, Eaton MP, et al. Preoperative thrombocytopenia and postoperative outcomes after noncardiac surgery. Anesthesiology. 2014;120(1):62–75.
Poordad F. Review article: thrombocytopenia in chronic liver disease. Aliment Pharmacol Ther. 2007;26(Suppl 1):5–11.
Miller JB, Figueroa EJ, Haug RM, et al. Thrombocytopenia in chronic liver disease and the role of thrombopoietin agonists. Gastroenterol Hepatol (N Y). 2019;15(6):326–32.
US FDA. Mulpleta® (lusutrombopag tablets) for oral use: US prescribing information. 2018. http://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Accessed 22 Aug 2019.
European Medicines Agency. Lusutrombopag Shionogi: summary of product characteristics. 2019. http://www.ema.europa.eu. Accessed 22 Aug 2019.
Japanese Pharmaceuticals and Medical Devices Agency. Lusutrombopag tablets 3 mg: Japanese prescribing information. 2015. http://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/340018_3399010F1022_1_02. Accessed 7 Jan 2019.
Katsube T, Ishibashi T, Kano T, et al. Population pharmacokinetic and pharmacodynamic modeling of lusutrombopag, a newly developed oral thrombopoietin receptor agonist, in healthy subjects. Clin Pharmacokinet. 2016;55(11):1423–33.
Yoshida H, Yamada H, Nogami W, et al. Development of a new knock-in mouse model and evaluation of pharmacological activities of lusutrombopag, a novel, nonpeptidyl small-molecule agonist of the human thrombopoietin receptor c-Mpl. Exp Hematol. 2018;59(30–9):e2.
Katsube T, Wajima T, Fukuhara T, et al. Effects of food and calcium carbonate on the pharmacokinetics of lusutrombopag, a novel thrombopoietin receptor agonist. Clin Ther. 2019. https://doi.org/10.1016/j.clinthera.2019.06.004.
Hidaka H, Kurosaki M, Tanaka H, et al. Lusutrombopag reduces need for platelet transfusion in patients with thrombocytopenia undergoing invasive procedures. Clin Gastroenterol Hepatol. 2019;17(6):1192–200.
Peck-Radosavljevic M, Simon K, Iacobellis A, et al. Lusutrombopag for the treatment of thrombocytopenia in patients with chronic liver disease undergoing invasive procedures (L-PLUS 2). Hepatology. 2019. https://doi.org/10.1002/hep.30561.
Tateishi R, Seike M, Kudo M, et al. A randomized controlled trial of lusutrombopag in Japanese patients with chronic liver disease undergoing radiofrequency ablation. J Gastroenterol. 2019;54(2):171–81.
Alkhouri N, Imawari M, Izumi N, et al. Safety and efficacy of lusutrombopag for treatment of thrombocytopenia in subjects with HCC undergoing planned invasive procedures: combined analysis of L-PLUS 1 and L-PLUS 2 trials [abstract no. 0949 plus poster]. In: AASLD—The Liver Meeting®. 2018.
Alkhouri N, Imawari M, Izumi N, et al. Efficacy of oral thrombopoietin receptor agonist lusutrombopag in chronic liver disease by underlying disease aetiology [abstract no. SAT-006]. J Hepatol. 2019;70(Suppl 1):e627.
Sasaki R, Shiino C, Imawari M, et al. Safety and effectiveness of lusutrombopag in Japanese chronic liver disease patients with thrombocytopenia undergoing invasive procedures: interim results of a postmarketing surveillance. Hepatol Res. 2019. https://doi.org/10.1111/hepr.13392.
Afdhal N, Brown R, Izumi N, et al. Lusutrombopag is a safe treatment option for thrombocytopenia in patients with chronic liver disease undergoing an invasive procedure: pooled safety analysis from 3 studies [abstract no. SAT-002]. J Hepatol. 2019;70(Suppl 1):e625.
US FDA. Doptelet® (avatrombopag) tablets, for oral use: US prescribing information. 2019. http://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Accessed 22 Aug 2019.
European Medicines Agency. Doptelet (avatrombopag): summary of product characteristics. 2019. http://www.ema.europa.eu. Accessed 30 Aug 2019.
Takada H, Kurosaki M, Nakanishi H, et al. Real-life experience of lusutrombopag for cirrhotic patients with low platelet counts being prepared for invasive procedures. PLoS One. 2019;14(2):e0211122.
Katsube T, Shimizu R, Fukuhara T, et al. Pharmacokinetic/pharmacodynamic modelling and simulation of lusutrombopag, a novel thrombopoietin receptor agonist, for the treatment of thrombocytopenia in patients with chronic liver disease undergoing invasive procedures. Clin Pharmacokinet. 2019. https://doi.org/10.1007/s40262-019-00770-4.
Acknowledgements
During the peer review process, the manufacturer of lusutrombopag was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Matt Shirley, Emma McCafferty and Hannah Blair are salaried employees of Adis International Ltd/Springer Nature, are responsible for the article content and declare no relevant conflicts of interest.
Additional information
Additional information for this Adis Drug Evaluation can be found at: https://doi.org/10.6084/m9.figshare.9764948.
The manuscript was reviewed by:A. Ascione, Department of Internal Medicine, Centre for Liver Disease, Fatebenefratelli Hospital, Naples, Italy; R. Maan, Department of Gastroenterology and Hepatology, Erasmus MC University Medical Center Rotterdam, Rotterdam, Netherlands.
Rights and permissions
About this article
Cite this article
Shirley, M., McCafferty, E.H. & Blair, H.A. Lusutrombopag: A Review in Thrombocytopenia in Patients with Chronic Liver Disease Prior to a Scheduled Procedure. Drugs 79, 1689–1695 (2019). https://doi.org/10.1007/s40265-019-01197-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01197-8