Abstract
Introduction
Polypharmacy is common and is associated with higher risk of adverse drug event (ADE) among older adults. Knowledge on the ADE risk level of exposure to different drug combinations is critical for safe polypharmacy practice, while approaches for this type of knowledge discovery are limited. The objective of this study was to apply an innovative data mining approach to discover high-risk and alternative low-risk high-order drug combinations (e.g., three- and four-drug combinations).
Methods
A cohort of older adults (≥ 65 years) who visited an emergency department (ED) were identified from Medicare fee-for-service and MarketScan Medicare supplemental data. We used International Classification of Diseases (ICD) codes to identify ADE cases potentially induced by anticoagulants, antidiabetic drugs, and opioids from ED visit records. We assessed drug exposure data during a 30-day window prior to the ED visit dates. We investigated relationships between exposure of drug combinations and ADEs under the case–control setting. We applied the mixture drug-count response model to identify high-order drug combinations associated with an increased risk of ADE. We conducted therapeutic class-based mining to reveal low-risk alternative drug combinations for high-order drug combinations associated with an increased risk of ADE.
Results
We investigated frequent high-order drug combinations from 8.4 million ED visit records (5.1 million from Medicare data and 3.3 million from MarketScan data). We identified 5213 high-order drug combinations associated with an increased risk of ADE by controlling the false discovery rate at 0.01. We identified 1904 high-order, high-risk drug combinations had potential low-risk alternative drug combinations, where each high-order, high-risk drug combination and its corresponding low-risk alternative drug combination(s) have similar therapeutic classes.
Conclusions
We demonstrated the application of a data mining technique to discover high-order drug combinations associated with an increased risk of ADE. We identified high-risk, high-order drug combinations often have low-risk alternative drug combinations in similar therapeutic classes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Polypharmacy (i.e., the concurrent use of multiple drugs) is on the ascendancy among US older adults [1, 2]. Polypharmacy is a major cause of drug–drug interaction-induced (DDI-induced) serious adverse drug event (ADE) requiring an emergency department (ED) visit and/or hospitalization. Nearly 22% of ED visits and 9% of hospitalizations are caused by DDIs [3,4,5,6]. DDIs are most prevalent among older adults because of the disproportionately high prevalence of polypharmacy. The risk of DDI-induced ADE increases with age and is highest among older adults [7]. Several studies have identified two-drug combinations that interacted adversely to increase the risks of GI bleeding [8, 9], hypoglycemia [10,11,12], and opioid-induced ADEs [13]. However, emerging data, including our published data, have shown that the risk of ADE increases by the addition of each drug that is used concurrently with others [14,15,16,17].
The concurrent use of ≥ 3 drugs, hereby referred as high-order drug combination, has emerged as a major target for preventing serious ADE. A recent US nationwide survey has shown that 68% of US older adults used ≥ 3 drugs in the past 30 days [18]. Yet, the extant literature has been focused on the risk of ADE with respect to two-drug combinations. Currently, the literature on high-order drug combination is sparse, and drug knowledgebase and drug labeled ADEs are often limited to DDI involving two-drug combinations [19].
Recent developments of large-scale, real-world data and pharmacoinformatic data mining methods jointly facilitate the detection of high-order drug combinations associated with an increased risk of ADE. Computational methods for mining high-order drug combination-induced ADEs include association rule mining [20], closed itemset mining [21], graphic model [22], and the recently developed mixture drug-count response model (MDRM) [23]. The MDRM assumes the drug combinations following two ADE risk models: (1) the ADE risk maintains a constant rate as the number of drug ingredients increased (e.g., drug ingredients do not interact and increase risk of ADE), and (2) the ADE risk increases in a sigmoid function as the number of drug ingredients increased (e.g., high-order DDI-induced ADEs). Following the MDRM’s assumption, besides detecting drug combinations associated with a higher risk of ADE at a low false discovery rate (FDR), MDRM is able to characterize the risk patterns (e.g., constant risk and increased risk) of all drug combinations. Our primary objective is to apply the MDRM to discover high-order drug combination (e.g., three- and four-drug combinations) associated with an increased risk of ADE, as well as low-risk drug combination alternatives to the high-order drug combination associated with an increased risk of ADE.
2 Methods
2.1 Institutional Review Board (IRB)
This retrospective observational study was approved by the Institutional Review Board (IRB) at The Ohio State University.
2.2 Data Source
We used the US Medicare fee-for-service data (2018) and MarketScan Medicare Supplemental data (2012–2020). Medicare data included US Medicare beneficiaries. MarketScan data were derived from retirees with employer-paid Medicare supplemental insurance plans. Both datasets included enrollment records, medical claims (e.g., date of service, place of service, and diagnosis codes), and pharmacy claims (e.g., date of pharmacy claim and dates of supply). Please see Electronic Supplementary Material (ESM) #1 Appendix A for additional information of the data sources.
2.3 Data Preparation
2.3.1 Identification of ED Visits
We identified “new” emergency department (ED) visits from Medicare data and MarketScan data. Specifically, we used revenue codes (e.g., 0450, 0451, 0452, 0456, 0459, 0981, 0760, and 0762) to identify ED visits [24]. We included ED visits with ≥ 30 days enrolment history prior to the current ED visit. We adopted the inclusion criterion for better assessment of drug exposure data. We excluded ED visits that had ED visit(s) within 30 days prior to the current ED visit. We adopted the exclusion criterion to improve the specificity of adverse high-order drug combinations.
2.3.2 Assessment of Drug Exposure
We accessed drug exposure data within 30 days prior to the ED visit date (e.g., the drug exposure window). We obtained generic drug names from the Medicare data and the MarketScan data, and used the RxNorm [25] to process the generic drug names. We mapped all compound drugs to individual drug ingredient names. We defined each drug exposure window as an observation for computing frequencies. First, we computed the frequencies of all drug ingredient names. We included the top-200 frequent drug ingredient names based on the frequencies in Medicare data and MarketScan data (ESM #2, Table S1). Second, we computed the frequencies of drug combinations. We considered that an observation (e.g., a drug exposure window) was exposed to a drug combination if all individual drug ingredient names were presented in the drug exposure window. We computed total frequencies of two-drug combinations, three-drug combinations, and four-drug combinations that were derived from the top-200 frequent drug ingredient names. We included drug combinations that had total frequencies ≥ 200.
2.3.3 Measurement of ADEs
Because serious ADEs are of significant public health importance, the US Department of Health and Human Services (HHS) created the National Action Plan for Adverse Drug Event Prevention (NAPADEP) in 2014 to address ADEs [26]. Our analysis focused on three major ADE classes that were identified as priority ADEs by the HHS NAPADEP: (1) potential anticoagulant-induced ADE; (2) potential antidiabetic drug-induced ADE; and (3) potential opioid-induced ADE. We used the ADE phenotyping algorithm defined by Digmann et al. to identify these ADEs [27]. We focused on ADE diagnosis codes on the first diagnosis position during an ED visit to ensure the specificity of the ADE cases.
2.3.4 Creation of Analytic Datasets
We derived analytical datasets under the case-control setting according to the ADE status of ED visit records. We created three datasets from Medicare data for each of the aforementioned ADE class (e.g., anticoagulant-induced ADE, antidiabetic drug-induced ADE, opioid-induced ADE). We also created three datasets from MarketScan data for each of the aforementioned ADE class. We defined: (1) the total frequency as the frequency of a drug or a drug combination among all ED visit records; and (2) the outcome frequency as the frequency of a drug or a drug combination among ADE cases. Each of the six analytic datasets included total frequencies and outcome frequencies for the included frequent drug ingredient names and their two-way to four-way combinations.
2.4 Statistical Analysis
2.4.1 Identification of High-Risk Drug Combinations
We used the mixture drug-count response model (MDRM) to mine drug combinations associated with an increased risk of ADE [23]. Under the MDRM, we defined the baseline risk as the ADE risk of using a single drug. We assumed the ADE risk of a high-order drug combination was either similar to the baseline risk (i.e., the null), or higher than the baseline risk (e.g., adverse drug combinations). Further, for the high-order adverse drug combinations, we assumed a sigmoid relationship between drug count (e.g., number of drug ingredients involved in the drug combination) and risk of ADE. We modeled the count of drug ingredients, as we assume drug ingredients were the bases of DDI-induced ADE. By clearly specifying the null distribution, we were able to identify adverse high-order drug combinations at a low false positive rate (FDR) under the empirical Bayesian framework.
We fitted the MDRM to each of the six analytical datasets. In the MDRM, we included five parameters characterizing constant risk (i.e., the null), drug-count response risk, and probabilities to follow drug-count risk for two-drug combinations, three-drug combinations, and four-drug combinations (ESM #1, Appendix B). We obtained the maximum likelihood estimators of the model parameters via the EM-algorithm. We defined FDR as the posterior probability of a drug combination to have a constant risk. We computed FDRs for all drug combinations. We used 0.01 as the threshold of FDR to identify high-order drug combinations (i.e., three-drug combinations and four-drug combinations) associated with an increased risk of ADE. All analyses were conducted in R (version 4.2).
2.4.2 Identification of Alternative Low-Risk Drug Combinations
We accessed the drug classes defined by the Anatomical Therapeutic Chemical (ATC) class system for high-order drug combinations associated with an increased risk of ADE. For each high-risk drug combination, we automatically searched all other drug combinations within the corresponding ATC level three class combination. We automatically performed multiple searches if a drug combination belonged to multiple drug class combinations. In each search, we used two proportion z-test to compare ADE risks between the high-risk drug combination and all other drug combinations within the drug class combination. We used P < 0.05 as a threshold of effect size to reveal low-risk drug combinations. All analyses were conducted in R (version 4.2).
3 Results
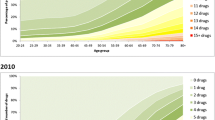
We identified 5.1 million ED visit records from Medicare data including 148,098 potential anticoagulant-induced ADE cases, 124,194 potential antidiabetic drug-induced ADE cases, and 146,245 potential opioid-induced ADE cases. We identified 3.3 million ED visits from MarketScan data including 113,531 potential anticoagulant-induced ADE cases, 108,523 potential diabetic drug-induced ADE cases, and 116,781 potential opioid-induced ADE cases. The demographic characteristics of the ED visits are presented in ESM #1 Table S1. Medicare data included 100,152 three-drug combinations and 103,490 four-drug combinations with frequencies ≥ 200. MarketScan data included 108,453 three-drug combinations and 109,448 four-drug combinations with frequencies ≥ 200. Distributions of ADE risk, constant risk curves, drug-count response risk curves, and portions of drug combinations to follow drug-count response risk curve are shown in Fig. 1. The fitted parameters are shown in ESM #1 Table S2. We identified a small portion of drug combinations to follow drug-count response risk curve (Fig. 1). Specifically, the percentages of drug combinations to follow a drug-count response risk curve for potential anticoagulant-induced ADE, potential antidiabetic drug-induced ADE, and potential opioid-induced ADE were: (1) 17%, 7% and 6% for three-drug combinations in Medicare data, respectively; (2) 11%, 2% and 1% for four-drug combinations in Medicare data, respectively; (3) 22%, 11% and 6% for three-drug combinations in MarketScan data, respectively; and (4) 18%, 3% and 1% for four-drug combinations in MarketScan data, respectively (Fig. 1). In other words, ≥ 78% three drug-combinations and ≥ 82% four-drug combinations had ADE risks followed a constant risk curve. Three-drug combinations and four-drug combinations to follow a drug-count response risk curve had on average 2.2-fold to 3.3-fold increased risks comparing to drug combinations to follow a constant risk curve.
3.1 Potential Anticoagulant-Induced ADE
We identified 4332 high-order drug combinations associated with an increased risk of ADE (e.g., FDRs < 0.01 in both Medicare data and MarketScan data). Of these, 2644 were three-drug combinations and 1688 were four-drug combinations. For these high-order drug combinations associated with an increased risk of ADE, 48.4% three-drug combinations and 73.9% four-drug combinations included warfarin [ATC code: B01AA (vitamin K antagonists)]; 18.9% three-drug combinations and 13.3 % four-drug combinations included direct factor Xa inhibitors (ATC code: B01AF; e.g., rivaroxaban and apixaban); and other frequent drug classes included HMG CoA reductase inhibitors (ATC code: C10AA; e.g., statins), plain sulfonamides (ATC code: C03CA; e.g., furosemide), selective beta blocking agents (ATC code: C07AB; e.g., metoprolol), proton pump inhibitors (ATC code: A02BC; e.g., omeprazole and pantoprazole), and platelet aggregation inhibitors excluding heparin (ATC code: B01AC; e.g., clopidogrel). The full list of high-risk drug combinations can be found in ESM #2 Table S2.
Out of the 2644 three-drug combinations associated with an increased risk of ADE, we identified 1104 drug combinations that had low-risk alternative drug combinations in both Medicare data and MarketScan data. Out of the 1688 high risk four-drug combinations associated with an increased risk of ADE, we identified 765 drug combinations that had low-risk alternative drug combinations in both Medicare data and MarketScan data. For high-risk drug combinations involving warfarin, 66.8% low-risk alternative drug combinations had warfarin been replaced by clopidogrel, 19.7% low-risk alternative drug combinations had warfarin been replaced by rivaroxaban or apixaban; 0.5% low-risk alternative drug combinations had warfarin not been replaced, and 12.2% had warfarin been replaced by dabigatran or cilostazol. For high-risk drug combinations involving direct factor Xa inhibitors (e.g., rivaroxaban and apixaban), 38.7% low-risk alternative drug combinations had direct factor Xa inhibitors been replaced by clopidogrel, 44.4% low-risk alternative drug combinations had direct factor Xa inhibitors not been replaced; 0.1% low-risk alternative drug combinations had direct factor Xa inhibitors been replaced by warfarin, and 17.2% had direct factor Xa inhibitors been replaced by dabigatran or cilostazol.
Table 1 presents exemplified high-order drug combinations associated with potential anticoagulant-induced ADE, as well as their low-risk alternative drug combinations. As presented in Table 1, low-risk alternative drug combinations were able to reduce the risks by 31.4–76.9%. For high-risk drug combinations involving antithrombotic agents, the risks were reduced by switching either antithrombotic agents or other concomitant drugs. For instance, risk of the drug combination involving digoxin, lisinopril and warfarin can be reduced by ≥ 44% by replacing warfarin [ATC class: B01A (antithrombotic agents)] with apixaban [ATC class: B01A (antithrombotic agents)] (Table 1). Full list of high-order drug combinations associated with an increased risk of ADE and their low-risk alternative combinations can be found in ESM #2 Table S3.
3.2 Potential Antidiabetic Drug-Induced ADE and Opioid-Induced ADE
We identified 519 and 362 high-order drug combinations for potential antidiabetic drug-induced ADE and potential opioid-induced ADE, respectively (e.g., FDRs < 0.01 in both Medicare data and MarketScan data). For potential antidiabetic drug-induced ADE, 443 were three-drug combinations and 76 were four-drug combinations. For potential opioid-induced ADE, 310 were three-drug combinations and 52 were four-drug combinations. The most frequent drug class in high-risk drug combinations for both potential antidiabetic drug-induced ADE and potential opioid-induced ADE included N06DA (anticholinesterases: donepezil, rivastigmine), N06DX (other anti-dementia drugs: memantine), C10AA (digitalis glycosides: simvastatin, pravastatin, atorvastatin, rosuvastatin), N06AB (selective serotonin reuptake inhibitors: citalopram, sertraline), and H03AA (thyroid hormones: levothyroxine). Full list of high-order drug combinations associated with an increased risk of ADE can be found in ESM #2 Table S4. For potential antidiabetic drug-induced ADE, we identified: (1) 19 drug combinations out of the 443 three-drug combinations associated with an increased risk of ADE had low-risk alternative drug combinations in both Medicare data and MarketScan data; and (2) none of the 76 four-drug combinations associated with an increased risk of ADE had low-risk alternative drug combinations in both Medicare data and MarketScan data. For potential opioid-induced ADE, we identified: (1) 15 drug combinations out of the 310 three-drug combinations associated with an increased risk of ADE had low-risk alternative drug combinations in both Medicare data and MarketScan data; and (2) only 1 drug combinations of the 52 four-drug combinations associated with an increased risk of ADE had low-risk alternative drug combinations in both Medicare data and MarketScan data. Table 2 presents exemplified drug combinations associated with potential antidiabetic drug-induced ADE and potential drug-induced ADE, as well as their low-risk alternative drug combinations. As Table 2 presents, the ADE risks can be reduced by 34.1–76.9% by the low-risk alternative drug combinations. Full list of high-order drug combinations associated with an increased risk of ADE and their low-risk alternative combinations can be found in ESM #2 Table S5.
4 Discussion
In this study, we demonstrate that the mixture drug-count response model (MDMR) is able to provide real-world evidence on drug safety among older adults with respect to use of multiple drugs. We identified certain high-order drug combinations (i.e., three-drug combinations and four-drug combinations) associated with an increased risk of adverse drug event (ADE) among older adults. Additionally, for some drug combinations associated with an increased risk of ADE, we identified alternative drug combinations that had a lower risk of ADE and similar therapeutic class combinations with the corresponding high-risk drug combinations.
First, the MDRM is able to characterize heterogeneous risk patterns of high-order drug combinations. For all ADE classes (e.g., potential anticoagulant-induced ADE, potential antidiabetic drug-induced ADE, and potential opioid-induced ADE), the majority of high-order drug combinations have risk of ADE remain similar as only using a single drug (e.g., the risk doesn’t increase as the number of drugs in the drug combination increases), and a portion of drug combinations have significantly higher risk of ADE than only using a single drug (e.g., the risk increases as the number of drugs in the drug combination increases). In other words, the majority of drug combinations have their risks similar to the risk of using a single drug, while a small portion of drug combinations have higher risk of ADE as number of drugs involved in the combination increases. It is important to distinguish these two types of drug combinations. Such a pattern reassures the safety for the majority of drug combinations and rises safety concerns for the remaining drug combinations.
Second, the Anatomical Therapeutic Chemical (ATC) Classification-based mining reveals that some high-order drug combinations associated with an increased risk of ADE have low-risk alternative drug combinations, where the low-risk drug combinations have similar drug classes as their corresponding high-risk combinations. Such a finding is naturally followed by the heterogeneous risk patterns of the drug combinations characterized by the MDRM. In this study, we searched low-risk alternative drug combinations with respect to ATC level three classes (e.g., chemical, pharmacological, or therapeutic subgroups). Certain high-order drug combinations associated with an increased risk of ADE often include a drug that may cause the ADE alone and concomitant drugs that are less likely to cause the ADE alone (Tables 1 and 2). Our search reveals that the risk of ADE can be reduced by either switching the drug that may cause the ADE alone, or substituting a drug that is less likely to cause the ADE alone (Tables 1 and 2). For instance, warfarin could cause GI bleeding alone. In our exemplified analysis, among all low-risk drug combinations of high-risk drug combinations involving warfarin, majority of the low-risk drug combinations have warfarin been replaced by other antithrombotic agents (e.g., clopidogrel, apixaban, rivaroxaban, cilostazol or dabigatran), while 0.5% of the low-risk drug combinations have other concomitant drugs been replaced and warfarin not been replaced. Interestingly, the aforementioned 0.5% of the low-risk drug combinations also have same five-digit ATC classes as the high-risk drug combinations. Such a finding provides real-world evidence for avoiding harmful high-order drug combinations without a significant change on the management of comorbidities. Full list of low-risk drug combinations with same drug classes (five-digit ATC codes) as the high-risk drug combinations are given in ESM #2 Table S6.
The MDRM assumes the ADE risks to follow a constant curve (i.e., ADE risk remains same as the number of drugs in the combination increases) or a dose response curve (i.e., ADE risk increases as the number of drugs in the combination increases). The rationale of the MDRM is closely related to drug–drug interaction (DDI). The constant risk curve and the drug-count response curve may represent drug combinations with and without a DDI, respectively. Some of our findings are in agreement with existing knowledge on DDI. For instance, pharmacology study on warfarin and proton pump inhibitors (PPIs) suggested: (1) pantoprazole had no significant interaction with warfarin, and (2) omeprazole and esomeprazole could decrease the clearance of warfarin [28]. In our study, we identified certain high-order drug combinations including omeprazole and warfarin or including esomeprazole and warfarin had a higher risk of GI bleeding, while the GI bleeding risk for the aforementioned high-risk combinations can be reduced by replacing omeprazole or esomeprazole with pantoprazole (ESM #2, Table S3, Table S5). For all three potential ADEs, we identified the majority of high-order drug combinations to have risk of ADE following a constant curve (Fig. 1), which implies DDI occurs only in a small portion of high-order drug combinations. Additionally, our study identified more high-risk drug combinations for potential anticoagulant-induced ADEs than potential antidiabetic/opioid-induced ADEs. Such a finding could be contributed by: (1) more drugs are associated with increased risk of GI-bleeding; and (2) a higher likelihood of DDI to induce GI bleeding.
The primary limitation of this approach is the need to ensure clinically relevant replaceability rather than replacement simply based on drug class. For example, for the majority of clinical indications clopidogrel, an antiplatelet agent, is not an appropriate substitute for warfarin, a systemic anticoagulant. In some cases, the algorithm recommends a topical medication replace a systemic medication (e.g., betamethasone for prednisone). Nevertheless, these results demonstrate a large number of potential clinically relevant substitutions. A rigorous clinical review of all combinations will be to allow for clinical application will be conducted and will be reported in a subsequent manuscript.
Our study has a number of additional limitations. First, despite we used algorithms developed by subject matter experts to identify ADE cases [27], the cases and controls could be misclassified. However, we conservatively defined cases as an ED visit with an ADE-related ICD codes on the first diagnosis position to improve the specificity. We would like to point out that an improvement on specificity is associated with a compromise on sensitivity, as ADE cases without an ADE-related ICD codes on the first diagnosis position were misclassified under our ADE phenotyping approach. Second, the drug exposure data were derived from pharmacy claims, which may not represent the underlying drug consumption records. Pharmacy claims are also inadequate to capture drugs that have been administered in certain facilities (e.g., inpatient drug administration) and/or obtained without insurance claim. We largely assume the drug consumption records can be characterized by pharmacy claims. All the aforementioned limitations are associated with the intrinsic properties of insurance claim datasets. Third, the potential high-risk drug combinations are subjected to confounding bias. The purpose of this study is to generate signals of high-risk drug combinations and their low-risk alternative combinations. Our findings shall facilitate more rigorous pharmacoepidemiology studies. For instance, the comparative risk of a high-risk drug combination and its low-risk alternative combination can be tested naturally under the active comparator design [29, 30], as both drug combinations have similar drug-class combinations. Forth, our study doesn’t investigate the impact of strength of drug exposure (e.g., doses of drugs) on ADE and the potential pharmacologic mechanism of the high-risk drug combinations (e.g., pharmacokinetics or pharmacodynamics properties). These are both important future research directions. Both rigorous pharmacoepidemiology study and pharmacology study are warranted to validate the high-risk drug combinations, as polypharmacy will continue to be a reality of medical care for older adults. Last, the study datasets included Medicare beneficiaries and retirees with employer-paid Medicare supplemental insurance plans. Even if our datasets represent a geographically diverse US older adult population, the results may not be generalizable to other populations.
5 Conclusion
In this study, we highlighted the power of data mining methods on revealing real-world evidence for safe polypharmacy practice in older adults. We identified adverse high-order drug combinations (e.g., three-drug combinations and four-drug combinations) associated with a higher ADE risk. Additionally, we identified alternative low-risk drug combinations for the high-risk, high-order drug combinations without changing the therapeutic classes of the high-risk drug combinations. This work provides a more nuanced description of the risks of polypharmacy and potential strategies to test safer prescribing strategies.
References
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314(17):1818–31. https://doi.org/10.1001/jama.2015.13766.
Qato DM, Wilder J, Schumm P, Gillet V, Alexander GC. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473–82. https://doi.org/10.1001/jamainternmed.2015.8581.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. https://doi.org/10.1517/14740338.2013.827660.
Becker ML, Kallewaard M, Caspers PWJ, Visser LE, Leufkens HGM, Stricker BH. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf. 2007;16(6):641–51. https://doi.org/10.1002/pds.1351.
Dechanont S, Maphanta S, Butthum B, Kongkaew C. Hospital admissions/visits associated with drug-drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23(5):489–97. https://doi.org/10.1002/pds.3592.
Magro L, Moretti U, Leone R. Epidemiology and characteristics of adverse drug reactions caused by drug-drug interactions. Expert Opin Drug Saf. 2012;11(1):83–94. https://doi.org/10.1517/14740338.2012.631910.
Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA. 2016;316(20):2115–25. https://doi.org/10.1001/jama.2016.16201.
Leonard CE, Brensinger CM, Bilker WB, Kimmel SE, Han X, Nam YH, Gagne JJ, Mangaali MJ, Hennessy S. Gastrointestinal bleeding and intracranial hemorrhage in concomitant users of warfarin and antihyperlipidemics. Int J Cardiol. 2017;228:761–70. https://doi.org/10.1016/j.ijcard.2016.11.245.
Bykov K, Schneeweiss S, Glynn R, Mittleman MA, Gagne JJ. A case-crossover-based screening approach to identifying clinically relevant drug-drug interactions in electronic healthcare data. Clin Pharmacol Ther. 2019;106(1):238–44. https://doi.org/10.1002/cpt.1376.
Han X, Chiang CW, Leonard CE, Bilker WB, Brensinger CM, Li L, Hennessy S. Biomedical Informatics approaches to identifying drug-drug interactions application to insulin secretagogues. Epidemiology. 2017;28(3):459–68. https://doi.org/10.1097/Ede.0000000000000638.
Leonard CE, Bilker WB, Brensinger CM, Han X, Flory JH, Flockhart DA, Gagne JJ, Cardillo S, Hennessy S. Severe hypoglycemia in users of sulfonylurea antidiabetic agents and antihyperlipidemics. Clin Pharmacol Ther. 2016;99(5):538–47. https://doi.org/10.1002/cpt.297.
Nam YH, Brensinger CM, Bilker WB, Leonard CE, Han X, Hennessy S. Serious hypoglycemia and use of warfarin in combination with sulfonylureas or metformin. Clin Pharmacol Ther. 2019;105(1):210–8. https://doi.org/10.1002/cpt.1146.
Abrahamsson T, Berge J, Ojehagen A, Hakansson A. Benzodiazepine, z-drug and pregabalin prescriptions and mortality among patients in opioid maintenance treatment-A nation-wide register-based open cohort study. Drug Alcohol Depend. 2017;174:58–64. https://doi.org/10.1016/j.drugalcdep.2017.01.013.
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62(12):2261–72. https://doi.org/10.1111/jgs.13153.
Nobili A, Pasina L, Tettamanti M, Lucca U, Riva E, Marzona I, Monesi L, Cucchiani R, Bortolotti A, Fortino I, Merlino L, Locatelli GW, Giuliani G. Potentially severe drug interactions in elderly outpatients: results of an observational study of an administrative prescription database. J Clin Pharm Ther. 2009;34(4):377–86. https://doi.org/10.1111/j.1365-2710.2009.01021.x.
Qato DM, Ozenberger K, Olfson M. Prevalence of prescription medications with depression as a potential adverse effect among adults in the United States. JAMA. 2018;319(22):2289–98. https://doi.org/10.1001/jama.2018.6741.
Chiang CW, Zhang PY, Wang XY, Wang L, Zhang SJ, Ning X, Shen L, Quinney SK, Li L. Translational high-dimensional drug interaction discovery and validation using health record databases and pharmacokinetics models. Clin Pharmacol Ther. 2018;103(2):287–95. https://doi.org/10.1002/cpt.914.
CDC. Health, United States; 2018 [01/25/2020]. https://www.cdc.gov/nchs/data/hus/2018/038.pdf.
John R, Philip D. Although triple drug interactions are not well studied, available information points to some general principles that may be useful in managing such combination. Pharmacy Times; 2011 [01/25/2020]. https://www.pharmacytimes.com/publications/issue/2011/January2011/Interactions-0111.
Harpaz R, Chase HS, Friedman C. Mining multi-item drug adverse effect associations in spontaneous reporting systems. BMC Bioinform. 2010;11(Suppl 9):S7. https://doi.org/10.1186/1471-2105-11-S9-S7.
Xiang Y, Albin A, Ren K, Zhang P, Etter JP, Lin S, Li L. Efficiently mining Adverse Event Reporting System for multiple drug interactions. AMIA Jt Summits Transl Sci Proc. 2014;2014:120–5.
Chasioti D, Yao X, Zhang P, Lerner S, Quinney SK, Ning X, Li L, Shen L. Mining directional drug interaction effects on myopathy using the FAERS database. IEEE J Biomed Health Inform. 2019;23(5):2156–63. https://doi.org/10.1109/JBHI.2018.2874533.
Wang X, Zhang P, Chiang CW, Wu H, Shen L, Ning X, Zeng D, Wang L, Quinney SK, Feng W, Li L. Mixture drug-count response model for the high-dimensional drug combinatory effect on myopathy. Stat Med. 2018;37(4):673–86. https://doi.org/10.1002/sim.7545.
CMS. Medicare Claims Processing Manual 2019 [01/25/2020]. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1139CP.pdf.
RxNorm. https://www.nlm.nih.gov/research/umls/rxnorm/index.html.
U.S. Department of Health and Human Services OoDPaHP. National Action Plan for Adverse Drug Event Prevention. Washington, DC; 2014.
Digmann R, Thomas A, Peppercorn S, Ryan A, Zhang L, Irby K, Brock J. Use of medicare administrative claims to identify a population at high risk for adverse drug events and hospital use for quality improvement. J Manag Care Spec Pharm. 2019;25(3):402–10. https://doi.org/10.18553/jmcp.2019.25.3.402.
Wedemeyer RS, Blume H. Pharmacokinetic drug interaction profiles of proton pump inhibitors: an update. Drug Saf. 2014;37(4):201–11. https://doi.org/10.1007/s40264-014-0144-0.
Wintzell V, Svanstrom H, Pasternak B. Selection of comparator group in observational drug safety studies: alternatives to the active comparator new user design. Epidemiology. 2022;33(5):707–14. https://doi.org/10.1097/EDE.0000000000001521.
Yoshida K, Solomon DH, Kim SC. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol. 2015;11(7):437–41. https://doi.org/10.1038/nrrheum.2015.30.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work is supported by NIH under R01AG071018.
Conflicts of interest
All authors declare no conflict of interest.
Ethics approval
This retrospective observational study was approved by the Institutional Review Board (IRB) at The Ohio State University (ID: 2020H0546).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
MarketScan data is available from IBM, and Medicare data is available from Center of Medicare and Medicaid Services (CMS).
Code availability
Sample codes can be found in Appendix.
Author contributions
PZ conceived the study; YS and CW conducted data analysis; YS, CW, MD, and PZ drafted the manuscript; KH, KU, JC, AS, YY, LL, MD, and PZ interpreted the results; All authors critically revised and gave final approval of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, Y., Chiang, CW., Unroe, K.T. et al. Application of an Innovative Data Mining Approach Towards Safe Polypharmacy Practice in Older Adults. Drug Saf 47, 93–102 (2024). https://doi.org/10.1007/s40264-023-01370-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01370-9