Abstract
Introduction
Bempedoic acid (ETC-1002) is a first-in-class lipid-lowering agent recently approved by the United States (US) Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for commercialization.
Objective
The aim was to assess, through a systematic review of the literature and a meta-analysis of the available phase 2 and phase 3 clinical studies, the effect of treatment with bempedoic acid on serum uric acid (SUA) concentration. Secondary outcomes were treatment-related variations in creatinine serum level and incidence of gout.
Methods
A systematic literature search in SCOPUS, PubMed Medline, ISI Web of Science and Google Scholar databases was conducted up to November 13th, 2019, in order to identify clinical trials potentially eligible for the meta-analysis. Effect sizes were expressed as absolute mean differences (MDs) and 95% confidence intervals (CIs).
Results
Data were pooled from four clinical studies comprising ten arms, which included overall 3369 subjects, with 2213 in the active-treatment arm and 1156 in the control one. Meta-analysis of data suggested that treatment with bempedoic acid is related to a significant increase in SUA (MD 0.73, 95% CI 0.54–0.91, P < 0.001), serum creatinine (MD 0.04, 95% CI 0.03–0.05, P < 0.001) and the incidence of gout (odds ratio 3.56, 95% CI 1.24–10.19, P = 0.018). The relatively small number of subjects involved in the studies and the exclusion of patients with renal impairment from the clinical trials are important limitations of the meta-analysis. However, our data indicate potential safety issues with bempedoic acid and suggest that further studies are performed both to elucidate the pathogenetic mechanisms underlying these associations and to verify the long-term safety of this treatment.
Conclusion
Bempedoic acid seems to have unfavourable effects on SUA, creatinine level and the incidence of gout. The ongoing Cardiovascular Outcomes Trial (CVOT) will explore the longer-term safety of treatment with bempedoic acid and clarify its effect on cardiovascular events and mortality.
PROSPERO database registration
CRD42019146126.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bempedoic acid is a first-in-class lipid-lowering agent recently approved by the United States Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for commercialization. |
This systematic review and meta-analysis showed that bempedoic acid seems to have unfavourable effects on serum uric acid, and increase creatinine serum levels and the incidence of gout. |
Further well-designed studies are needed to explore the longer-term safety of treatment with bempedoic acid. |
1 Introduction
Despite the availability of effective and overall safe lipid-lowering drugs, a large number of patients are not able to reach the ambitious low-density lipoprotein cholesterol (LDL-C) target suggested by the most recent guidelines for cardiovascular disease prevention [1]. In this context, the research for new drugs with innovative mechanisms of action that can be both effective and safe is still ongoing. The United States (US) Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have recently approved for commercialization bempedoic acid [2, 3], a first-in-class lipid-lowering agent and novel small molecule regulator of lipid and carbohydrate metabolism [4]. It is activated to the thioester with coenzyme A by the enzyme acyl-CoA synthetase, which in humans is encoded by the gene SLC27A2 and primarily expressed in liver and kidney [5]. The activated substance inhibits adenosine triphosphate (ATP) citrate lyase, which is involved in the liver's biosynthesis of cholesterol upstream of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase, the enzyme that is inhibited by statins [6]. Even if bempedoic acid acts on the same pathway as statins, the lack of the activating enzyme in skeletal muscle may prevent the muscular adverse effects associated with the HMG-CoA reductase inhibitors [7].
Bempedoic acid has shown a good efficacy and safety profile in the clinical studies carried out so far, with a mean percentage reduction in total cholesterol and LDL-C of − 17.12% and − 26.58%, respectively, and similar treatment-emergent signs and symptoms compared to placebo [8, 9]. However, some clinical trials reported a slight but significant increase in serum creatinine as well as a relevant increase in serum uric acid (SUA) levels [6, 10,11,12]. The molecular pathways underlying these effects are unknown, though several causal mechanisms might be hypothesized. At the same time, the clinical relevance and prognostic impact of these laboratory changes are yet to be clarified [13].
In order to clarify investigate the relationship between bempedoic acid treatment and SUA levels in hyperlipidaemic patients, we carried out a systematic review and meta-analysis of the available phase 2 and phase 3 clinical trials, aiming to investigate this drug-related adverse event. Secondary outcomes were treatment-related variations in creatinine concentration and the incidence of gout.
2 Methods
The study was designed according to guidelines of the 2009 Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [14] and registered in the PROSPERO database (registration number CRD42019146126). Due to the study design (meta-analysis), neither institutional review board approval nor patient informed consent was required.
2.1 Search Strategy
PubMed, SCOPUS, Google Scholar and ISI Web of Science via Clarivate databases were searched, with no language restriction, using the following search terms: (“bempedoic acid” OR “ETC-1002”) AND (“serum uric acid” OR “SUA” OR “uric acid” OR “UA”). The authors of the studies were not contacted for additional information. Published data were only included in the meta-analysis. The wild-card term “*” was used to increase the sensitivity of the search strategy, which was limited to studies in humans. The reference lists of identified papers were manually checked for additional relevant articles. In particular, additional searches for potential trials included the references of review articles on that issue and the abstracts from selected congresses on the subject of the meta-analysis. Literature was searched from inception to November 13th, 2019 (corresponding to the last search date).
All paper abstracts were screened by two reviewers (FF and AFGC) in an initial process to remove ineligible articles and duplicates. The remaining articles were obtained in full-text and assessed again by the same two researchers, who evaluated each article independently and carried out data extraction and quality assessment. Disagreements were resolved by discussion with a third party (CB).
2.2 Study Selection Criteria
Original studies were included if they met the following criteria: (1) a phase 2 or 3 clinical trial with either a multicentre or single-centre design, (2) included adult patients and (3) investigated the effect of ETC-1002 on SUA levels. Studies not reporting any measure of dispersion around the central tendency for the considered outcomes were deemed inadequate to describe data and were excluded from the analysis. Studies that lacked a properly controlled design for ETC-1002 treatment were excluded also.
2.3 Data Extraction
Data abstracted from the eligible studies were (1) first author’s name; (2) year of publication; (3) study registration code; (4) study design; (5) treatment duration; (6) main inclusion criteria and underlying disease; (7) study groups; (8) number of participants in the active and control group; (9) age; (10) sex of study participants; and (11) average percentage change in LDL-C. All data extraction and database typing were reviewed by the principal investigator (AFGC) before the final analysis, and doubts were resolved by mutual agreement among the authors.
2.4 Quality Assessment
A systematic assessment of risk of bias in the included studies was performed using the Cochrane criteria [15]. The following items were used: adequacy of sequence generation, allocation concealment, blinding addressing of dropouts (incomplete outcome data), selective outcome reporting, and other probable sources of bias [16]. Risk-of-bias assessment was performed independently by two reviewers (FF and AFGC); disagreements were resolved by a consensus-based discussion.
2.5 Data Synthesis
Meta-analysis was entirely conducted using Comprehensive Meta-Analysis (CMA) V3 software (Biostat, NJ) [17].
Net changes in the investigated parameters (change scores) were calculated by subtracting the value at baseline from the one after intervention in the active-treatment group and in the control one. All values were collated as absolute change from baseline. Standard deviations (SDs) of the mean difference (MD) were obtained as reported by Follmann and colleagues: SD = square root [(SDpre-treatment)2 + (SDpost-treatment)2 − (2R × SDpre-treatment × SDpost-treatment)], assuming a correlation coefficient (R) = 0.5 [18]. Where the standard error of the mean (SEM) was only reported as a dispersion measure, SD was estimated using the following formula: SD = SEM × square root (n), n being the number of subjects. Study findings were combined using a fixed-effect model or a random-effect model (using the DerSimonian–Laird method) and the generic inverse variance method, based on the level of interstudy heterogeneity, which was quantitatively assessed using the Higgins index (I2) [19]. Effect sizes were expressed as absolute MDs or odds ratios (ORs) and 95% confidence intervals (CIs). In order to evaluate the influence of each study on the overall effect size, sensitivity analysis was conducted using the leave-one-out method (i.e. removing one study at a time and repeating the analysis) [20]. Two-sided P values ≤ 0.05 were considered as statistically significant for all tests.
2.6 Meta-regression Analyses
Random- or fixed-effect meta-regression analyses using the unrestricted maximum likelihood model and including age at baseline and treatment duration as potential independent moderator variables were planned to explore the heterogeneity. Two-sided P values ≤ 0.05 were considered as statistically significant for the tests.
2.7 Publication Biases
Potential publication biases were explored using visual inspection of Begg’s funnel plot asymmetry, Begg’s rank correlation test and Egger’s weighted regression test [21]. The Duval and Tweedie “trim and fill” method was used to adjust the analysis for the effects of publication biases [22]. Two-sided P values ≤ 0.05 were considered statistically significant, and in the case of a significant result, the Rosenthal fail-safe N test was applied in order to calculate the number of additional negative studies that would be needed to increase the P value for the meta-analysis to above 0.05 [23].
3 Results
3.1 Flow and Characteristics of the Included Studies
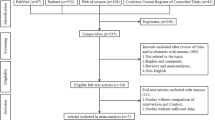
After database searches performed strictly according to inclusion and exclusion criteria, 253 published articles were identified and the abstracts reviewed. All the identified studies were written in English. Of these, 242 were excluded because they were non-original articles. Another seven were eliminated because they did not meet the inclusion criteria. Finally, four articles were carefully assessed and reviewed. On the basis of the established eligibility criteria, they were all included in the meta-analysis [6, 10,11,12]. The study selection process is shown in Fig. 1. Data were pooled from four clinical trials comprising ten treatment arms, which included 3369 subjects, with 2213 in the active-treatment arm and 1156 in the control one.
Eligible studies were published between 2014 and 2019. Follow-up periods ranged between 4 and 52 weeks, and several treatment schedules were tested. All selected trials were designed with parallel groups and were multicentre [6, 10, 12] or single-centre [11] clinical studies. Enrolled subjects were diabetics [11] or individuals at high risk for CVD [6, 10, 12]. Bempedoic acid was compared versus placebo [6, 10,11,12] or in association with ezetimibe versus ezetimibe alone [10]. However, all clinical trials had a double-blind design (i.e. trial participants and investigators were unaware of the treatment allocation). The main characteristics of the evaluated studies are summarized in Table 1.
3.2 Risk of Bias Assessment
All the included studies were characterized by sufficient information regarding sequence generation, allocation concealment, personal and outcome assessments. Details of the quality of bias assessment are reported in Table S1 (see the electronic supplementary material).
3.3 Effect of ETC-1002 on SUA
Meta-analysis of data showed that treatment with bempedoic acid significantly increased SUA levels (MD 0.73, 95% CI 0.54–0.91, P < 0.001; I2 = 74.9%) (Fig. 2). The effect size was robust in the leave-one-out sensitivity analysis (Figure S1; see the electronic supplementary material) and was not mainly driven by a single study.
Forest plot displaying mean difference and 95% confidence intervals for the impact of bempedoic acid on SUA. In the article by Ballantyne et al., bempedoic acid was compared versus placebo (Ballantyne II) or in a fixed-dose combination with ezetimibe versus ezetimibe alone (Ballantyne I). SUA serum uric acid
Visual inspection of Begg’s funnel plots did not reveal any asymmetry, suggesting no publication bias for the analysis (Figure S2). The absence of publication bias was supported by the Egger’s linear regression and the Begg’s rank correlation (P > 0.05 for all comparisons), and the Duval and Tweedie “trim and fill” method did not identify any aberrant study. The classic fail-safe N test suggested that 376 studies with negative results would be needed to bring the estimated effect size on SUA to a non-significant level (P > 0.05).
3.4 Secondary Outcomes
Treatment with bempedoic acid was significantly associated with increased creatinine concentrations (MD 0.04, 95% CI 0.03–0.05, P < 0.001; I2 = 0%) and with an increase risk of developing gout (OR 3.56, 95% CI 1.24–10.19, P = 0.018; I2 = 0%) (Figs. 3, 4). Results were confirmed by the leave-one-out sensitivity analysis (Figure S3 and S4; see the electronic supplementary material).
Forest plot displaying mean difference and 95% confidence intervals for the impact of bempedoic acid on creatinine serum levels. In the article by Ballantyne et al., bempedoic acid was compared versus placebo (Ballantyne II) or in a fixed-dose combination with ezetimibe versus ezetimibe alone (Ballantyne I)
Forest plot displaying odds ratio and 95% confidence intervals for the impact of bempedoic acid on the incidence of gout. In the article by Ballantyne et al., bempedoic acid was compared versus placebo (Ballantyne II) or in a fixed-dose combination with ezetimibe versus ezetimibe alone (Ballantyne I)
3.5 Meta-regression Analysis
Meta-regression analyses did not suggest any significant association between change in SUA and age at baseline (slope − 0.03; 95% CI − 0.07 to 0.01; two-tailed P = 0.11) or treatment duration (slope − 0.004; 95% CI − 0.011 to 0.003; two-tailed P = 0.27) (Figure S5; see the electronic supplementary material).
4 Discussion
By analysing data from four phase 2 and phase 3 randomized controlled trials including a total of 3369 patients, our meta-analysis showed that treatment with bempedoic acid entails a significant increase in SUA concentration, also exerting a negative effect on creatinine levels and, finally, increasing the risk of developing gout. Based on current evidence, this effect appears to be independent of the duration of treatment and the age of treated patients.
Even if our study cannot address the pathogenetic mechanisms underlying the observed effects, it can be speculated that the observed increase in SUA may be consequent to abnormalities in renal tubular handling of both SUA and possibly creatinine, finally resulting in less urinary excretion of both these substances [24]. As a matter of fact, in animal models, renal proximal tubule urate secretion is inhibited by cellular stress-induced adenosine monophosphate (AMP)-activated protein kinase [25], suggesting that bempedoic acid may be directly related to reduced urate excretion and therefore increased serum urate concentration. Furthermore, mutations in ABCG2 transporter have been linked to statin toxicity [26]. It could therefore be speculated that, at least in statin-intolerant patients, genetic mutations in this transporter may influence SUA secretion at the renal tubule level [27].
Alternatively, the observed increase in SUA might be due to glomerular filtration rate reduction by bempedoic acid. Thus the observed increase in SUA could simply result from reduced urinary excretion by the kidney [28].
Finally, an additional and intriguing, although speculative explanation to account for the observed signs of renal damage may involve the exposure of glomerular and tubular structures to high SUA levels. As a matter of fact, both experimental [29, 30] and clinical studies [31] strongly support an unfavourable renal effect of hyperuricaemia.
Actually, among the traditional lipid-lowering drugs, rosuvastatin and fenofibrate have just been known to increase serum creatinine, but this effect is transient and fully reversible, even after long-term treatment [32, 33]. Moreover, these drugs have been shown to exert a positive or at most indifferent effect on SUA levels [34, 35], and have been proven to effectively reduce total cardiovascular events [36, 37]. On the contrary, data on decreased cardiovascular events and mortality are lacking for bempedoic acid so far. The increase in serum creatinine observed with bempedoic acid treatment could be prognostically negligible, but, assuming a life-time exposition, we have as yet no long-term data to know if this can have an impact on renal or cardiovascular health. On the other hand, based on the available data [38, 39], the observed SUA increase, in the context of a simultaneous reduction in glomerular filtration rate, could have a more rapid and negative impact on a number of cardiometabolic and renal outcomes.
The main limitation of this meta-analysis is related to the relatively small number of subjects involved in the studies, which were often short or medium term, as well as the exclusion of patients with renal impairment from the clinical trials. Furthermore, it was not possible to carry out a subgroup analysis to evaluate the synergistic effect of bempedoic acid as an add-on to other lipid-lowering drugs, since in most studies detailed information on the background treatment of the patients was lacking. The degree of heterogeneity for SUA change is another important limitation of the current analysis.
Notwithstanding these limitations, our data indicate potential safety issues with bempedoic acid and suggest that further studies are performed both to elucidate the pathogenetic mechanisms underlying these associations and to verify long-term safety of this treatment. In particular, it is necessary that any changes in kidney function during treatment with bempedoic acid are carefully evaluated, in particular in patients with moderate to severe chronic kidney disease.
The ongoing Cardiovascular Outcomes Trial (CVOT) (the CLEAR study), which in August 2019 completed the enrolment of 14,032 patients at over 1400 sites in 32 countries around the world, will answer the question (settle the issue) raised by our study and clarify the effect of bempedoic acid on cardiovascular events and mortality [9].
5 Conclusions
In conclusion, based on the results of this meta-analysis of double-blind, randomized clinical trials, bempedoic acid seems to have unfavourable effects on SUA and creatinine, with uncertain prognostic impact. The CVOT will explore the longer-term safety of the treatment and clarify its effect on cardiovascular events and mortality. However, further clinical studies are expected to evaluate the long-term effect of the treatment with bempedoic acid in patients with chronic kidney disease.
References
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al.; ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
European Medicine Agency. Committee for Medicinal Products for Human Use (CHMP). Nilemdo—Bempedoic acid. EMA/CHMP/44961/2020. 30 January 2020.
Food and Drug Administration. NEXLETOL (bempedoic acid) tablets, for oral use. Reference ID: 4564667. Initial U.S. Approval: 2020.
Honigberg MC, Natarajan P. Bempedoic acid for lowering LDL cholesterol. JAMA. 2019;322(18):1769–71.
Feng X, Zhang L, Xu S, Shen AZ. ATP-citrate lyase (ACLY) in lipid metabolism and atherosclerosis: an updated review. Prog Lipid Res. 2020;77:101006. https://doi.org/10.1016/j.plipres.2019.101006.
Ray KK, Bays HE, Catapano AL, Lalwani ND, Bloedon LT, Sterling LR, et al. CLEAR Harmony Trial. Safety and efficacy of bempedoic acid to reduce LDL cholesterol. N Engl J Med. 2019;380(11):1022–32. https://doi.org/10.1056/NEJMoa1803917.
Zagelbaum NK, Yandrapalli S, Nabors C, Frishman WH. Bempedoic acid (ETC-1002): ATP citrate lyase inhibitor: review of a first-in-class medication with potential benefit in statin-refractory cases. Cardiol Rev. 2019;27(1):49–56. https://doi.org/10.1097/CRD.0000000000000218.
Wang X, Luo S, Gan X, He C, Huang R. Safety and efficacy of ETC-1002 in hypercholesterolaemic patients: a meta-analysis of randomised controlled trials. Kardiol Pol. 2019;77(2):207–16. https://doi.org/10.5603/KP.a2019.0013.
Ray KK, Corral P, Morales E, Nicholls SJ. Pharmacological lipid-modification therapies for prevention of ischaemic heart disease: current and future options. Lancet. 2019;394(10199):697–708. https://doi.org/10.1016/S0140-6736(19)31950-6.
Ballantyne CM, Laufs U, Ray KK, Leiter LA, Bays HE, Goldberg AC, et al. Bempedoic acid plus ezetimibe fixed-dose combination in patients with hypercholesterolemia and high CVD risk treated with maximally tolerated statin therapy. Eur J Prev Cardiol. 2019;29:2047487319864671. https://doi.org/10.1177/2047487319864671(Epub ahead of print).
Gutierrez MJ, Rosenberg NL, Macdougall DE, Hanselman JC, Margulies JR, Strange P, et al. Efficacy and safety of ETC-1002, a novel investigational low-density lipoprotein-cholesterol-lowering therapy for the treatment of patients with hypercholesterolemia and type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2014;34(3):676–83. https://doi.org/10.1161/ATVBAHA.113.302677.
Goldberg AC, Leiter LA, Stroes ESG, Baum SJ, Hanselman JC, Bloedon LT, et al. Effect of bempedoic acid vs placebo added to maximally tolerated statins on low-density lipoprotein cholesterol in patients at high risk for cardiovascular disease: the CLEAR Wisdom randomized clinical trial. JAMA. 2019;322(18):1780–8. https://doi.org/10.1001/jama.2019.16585.
Bove M, Cicero AFG, Borghi C. Emerging drugs for the treatment of hypercholesterolemia. Expert Opin Emerg Drugs. 2019;24(1):63–9. https://doi.org/10.1080/14728214.2019.1591372.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Higgins J. Green S. Cochrane handbook for systematic reviews of interventions. Version 5.0. 2. 2009. Chichester: Wiley. Ref Type: Report; 2010.
Fogacci F, Ferri N, Toth PP, Ruscica M, Corsini A, Cicero AFG. Efficacy and safety of mipomersen: a systematic review and meta-analysis of randomized clinical trials. Drugs. 2019;79(7):751–66. https://doi.org/10.1007/s40265-019-01114-z.
Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis version 3. Englewood: Biostat; 2005. p. 104.
Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45(7):769–73.
Melsen WG, Bootsma MC, Rovers MM, Bonten MJ. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20:123–9. https://doi.org/10.1111/1469-0691.12494.
Fogacci F, Banach M, Cicero AFG. Resveratrol effect on patients with non-alcoholic fatty liver disease: a matter of dose and treatment length. Diabetes Obes Metab. 2018;20(7):1798–9. https://doi.org/10.1111/dom.13324.
Sahebkar A, Pirro M, Reiner Ž, Cicero A, Ferretti G, Simental-Mendía M, et al. A systematic review and meta-analysis of controlled trials on the effects of statin and fibrate therapies on plasma homocysteine levels. Curr Med Chem. 2016;23(39):4490–503.
Fogacci F, Grassi D, Rizzo M, Cicero AFG. Metabolic effect of berberine-silymarin association: a meta-analysis of randomized, double-blind, placebo-controlled clinical trials. Phytother Res. 2019;33(4):862–70. https://doi.org/10.1002/ptr.6282.
Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86:638–64. https://doi.org/10.1037/0033-2909.86.3.638.
Odden MC, Amadu AR, Smit E, Lo L, Peralta CA. Uric acid levels, kidney function, and cardiovascular mortality in US adults: National Health and Nutrition Examination Survey (NHANES) 1988–1994 and 1999–2002. Am J Kidney Dis. 2014;64(4):550–7. https://doi.org/10.1053/j.ajkd.2014.04.024.
Bataille AM, Maffeo CL, Renfro JL. Avian renal proximal tubule urate secretion is inhibited by cellular stress-induced AMP-activated protein kinase. Am J Physiol Ren Physiol. 2011;300(6):F1327–F13381338. https://doi.org/10.1152/ajprenal.00680.2010.
Niemi M. Transporter pharmacogenetics and statin toxicity. Clin Pharmacol Ther. 2010;87(1):130–3. https://doi.org/10.1038/clpt.2009.197.
Ward NC, Watts GF, Eckel RH. Statin toxicity. Circ Res. 2019;124(2):328–50. https://doi.org/10.1161/CIRCRESAHA.118.312782.
Benn CL, Dua P, Gurrell R, Loudon P, Pike A, Storer RI, et al. Physiology of hyperuricemia and urate-lowering treatments. Front Med. 2018;5:160. https://doi.org/10.3389/fmed.2018.00160.
Verzola D, Ratto E, Villaggio B, Parodi EL, Pontremoli R, Garibotto G, et al. Uric acid promotes apoptosis in human proximal tubule cells by oxidative stress and the activation of NADPH oxidase NOX 4. PLoS One. 2014;9(12):e115210. https://doi.org/10.1371/journal.pone.0115210.
Milanesi S, Verzola D, Cappadona F, Bonino B, Murugavel A, Pontremoli R, et al. Uric acid and angiotensin II additively promote inflammation and oxidative stress in human proximal tubule cells by activation of toll-like receptor 4. J Cell Physiol. 2019;234(7):10868–76. https://doi.org/10.1002/jcp.27929.
De Cosmo S, Viazzi F, Pacilli A, Giorda C, Ceriello A, Gentile S, AMD-Annals Study Group, et al. Serum uric acid and risk of CKD in type 2 diabetes. Clin J Am Soc Nephrol. 2015;10(11):1921–9. https://doi.org/10.2215/CJN.03140315.
Newman CB, Preiss D, Tobert JA, Jacobson TA, Page RL 2nd, Goldstein LB, American Heart Association Clinical Lipidology, Lipoprotein, Metabolism, and Thrombosis Committee, a Joint Committee of the Council on Atherosclerosis, Thrombosis, and Vascular Biology, and Council on Lifestyle, and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology;, and Stroke Council, et al. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39(2):e38–e81. https://doi.org/10.1161/ATV.0000000000000073.
Mychaleckyj JC, Craven T, Nayak U, Buse J, Crouse JR, Elam M, et al. Reversibility of fenofibrate therapy-induced renal function impairment in ACCORD type 2 diabetic participants. Diabetes Care. 2012;35(5):1008–144. https://doi.org/10.2337/dc11-1811.
Derosa G, Maffioli P, Reiner Ž, Simental-Mendía LE, Sahebkar A. Impact of statin therapy on plasma uric acid concentrations: a systematic review and meta-analysis. Drugs. 2016;76(9):947–56. https://doi.org/10.1007/s40265-016-0591-2.
Derosa G, Maffioli P, Sahebkar A. Plasma uric acid concentrations are reduced by fenofibrate: a systematic review and meta-analysis of randomized placebo-controlled trials. Pharmacol Res. 2015;102:63–70. https://doi.org/10.1016/j.phrs.2015.09.012.
Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, HOPE-3 Investigators, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2021–31. https://doi.org/10.1056/NEJMoa1600176.
Ting RD, Keech AC, Drury PL, Donoghoe MW, Hedley J, Jenkins AJ, FIELD Study Investigators, et al. Benefits and safety of long-term fenofibrate therapy in people with type 2 diabetes and renal impairment: the FIELD Study. Diabetes Care. 2012;35(2):218–25. https://doi.org/10.2337/dc11-1109.
Casiglia E, Tikhonoff V, Virdis A, Masi S, Barbagallo CM, Bombelli M, Working Group on Uric Acid, and Cardiovascular Risk of the Italian Society of Hypertension (SIIA), et al. Serum uric acid and fatal myocardial infarction: detection of prognostic cut-off values: The URRAH (Uric Acid Right for Heart Health) study. J Hypertens. 2019. https://doi.org/10.1097/HJH.0000000000002287(Epub ahead of print).
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P. Is hyperuricemia an independent risk factor for new-onset chronic kidney disease? A systematic review and meta-analysis based on observational cohort studies. BMC Nephrol. 2014;15:122. https://doi.org/10.1186/1471-2369-15-122.
Acknowledgements
Authors wish to thank Claudia Cavicchi, librarian at the Clinical Library of the University of Bologna, for her support in finding the articles to prepare the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflict of interest
Claudio Borghi, Arrigo F.G. Cicero, Federica Fogacci, Roberto Pontremoli and Francesca Viazzi have no conflicts of interest that are directly relevant to the content of this study.
Data Sharing
Data are available from the corresponding author upon reasonable request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cicero, A.F.G., Pontremoli, R., Fogacci, F. et al. Effect of Bempedoic Acid on Serum Uric Acid and Related Outcomes: A Systematic Review and Meta-analysis of the available Phase 2 and Phase 3 Clinical Studies. Drug Saf 43, 727–736 (2020). https://doi.org/10.1007/s40264-020-00931-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-00931-6