Abstract
Drug-induced liver injury (DILI), herbal-induced liver injury, and herbal and dietary supplement (HDS)-induced liver injury are an important aspect of drug safety. Knowledge regarding responsible drugs, mechanisms, risk factors, and the diagnostic tools to detect liver injury have continued to grow in the past year. This review highlights what we considered the most significant publications from among more than 1800 articles relating to liver injury from medications, herbal products, and dietary supplements in 2017 and 2018. The US Drug-Induced Liver Injury Network (DILIN) prospective study highlighted several areas of ongoing study, including the potential utility of human leukocyte antigens and microRNAs as DILI risk factors and new data on racial differences, the role of alcohol consumption, factors associated with prognosis, and updates on the clinical signatures of autoimmune DILI, thiopurines, and HDS agents. Novel data were also generated from the Spanish and Latin American DILI registries as well as from Chinese and Korean case series. A few new agents causing DILI were added to the growing list in the past 2 years, including sodium–glucose co-transporter-2 inhibitors, as were new aspects of chemotherapy-associated liver injury. A number of cases reported previously described hepatotoxins confirmed via the Roussel Uclaf Causality Assessment Method (RUCAM; e.g., norethisterone, methylprednisolone, glatiramer acetate) and/or the DILIN method (e.g., celecoxib, dimethyl fumarate). Additionally, much work centered on elucidating the pathophysiology of DILI, including the importance of bile salt export pumps and immune-mediated mechanisms. Finally, it must be noted that, while hundreds of new studies described DILI in 2017–2018, the quality of such reports must always be addressed. Björnsson reminds us to remain very critical of the data when addressing the future utility of a study, which is why it is so important to adhere to a standardized method such as RUCAM when determining DILI causality. While drug-induced hepatotoxicity remains a diagnosis of exclusion, the diverse array of publications that appeared in 2017 and 2018 provided important advances in our understanding of DILI, paving the way for our improved ability to make a more definitive diagnosis and risk assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
While studies regarding the diagnosis and risk assessment of drug-induced liver injury (DILI) and herbal-induced liver injury (HILI) continue to proliferate each year, the field still lacks a pathognomonic diagnostic biomarker. |
Many case reports and case series that report possible DILI still lack the requisite minimal number of elements needed to critically assess causality; more widespread use of the Roussel Uclaf Causality Assessment Method (RUCAM) or the methodologies employed by DILI registries, such as the US DILI Network (DILIN) are encouraged. |
Many new agents observed to cause hepatotoxicity were reported in 2017–2018, including fimasartan, everolimus, and obeticholic acid, among others. |
Interesting new studies of known hepatotoxins included protein adducts as a biomarker for acetaminophen toxicity, new evidence that direct oral anticoagulants may not be as hepatotoxic as previously thought, and a potential new DILI risk assessment tool for direct-acting antivirals for hepatitis C infection. |
New guidelines were created by the China Association of Chinese Medicine regarding the evaluation of HILI. An increasing number of articles in the last 2 years concerned Kratom, Garcinia cambogia, red yeast rice, and Ayurvedic compounds. |
1 Introduction
Drug-induced liver injury (DILI) and herbal and dietary supplement (HDS)-induced liver injury (HILI) are important aspects of drug safety, and knowledge regarding responsible drugs, mechanisms, risk factors, and diagnostic tools continued to grow in the last year, with more than 1800 publications. Many large registries were updated in the past 2 years, including the US DILI Network (DILIN) [1,2,3,4,5,6,7,8,9,10,11,12,13,14], Spanish DILI Registry [15, 16], and Latin American DILI Network. Contributions also came from populations in Iceland [17, 18], China [19], and Korea [20]. Additionally, recognition of HILI and HDS has been increasing and, in this past year, the list of herbal substances causing liver injury continued to increase [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37].
Much work has been undertaken to refine the diagnostic approach to DILI, as the diagnosis remains one of exclusion. This review briefly provides updates on the diagnosis of DILI, but a more thorough analysis of biomarkers and risk factors for DILI is beyond the scope of this review and is available elsewhere [12, 38,39,40,41,42,43,44,45,46,47,48,49,50,51].
The diagnosis of DILI is important not only in clinical practice but also in its potential broader impact. Reporting cases of possible DILI to the appropriate regulatory authorities is of great importance and has real-world consequences, as it can lead to termination of clinical trials or even force withdrawal of a drug from the market. Recently, a phase III trial of a type 2 diabetes mellitus medication, fasiglifam, was terminated because of an increased incidence of alanine transaminase (ALT) elevations greater than three times the upper limit of normal (ULN), which included several Hy’s law cases [52]. Biogen and AbbVie recently voluntarily withdrew the multiple sclerosis drug daclizumab after multiple reports of immune-related conditions, such as encephalitis and severe liver damage, in the postmarket setting, highlighting the importance of postapproval monitoring [53]. In addition, solithromycin, a potential antibiotic for treatment of community-acquired pneumonia did not receive US FDA approval because many patients experienced transaminase elevations, necessitating further investigation [54]. More details on solithromycin are provided later in the manuscript.
This past year, study of the specific mechanisms leading to DILI provided a better understanding for how and why this particular type of liver injury occurs. For example, publications dealing with mechanistic models to study bile salt export pumps and their role in cholestatic liver injury, and the link between the immune system and idiosyncratic DILI, were reviewed. The role of mitochondrial dysfunction and oxidative stress in DILI were also explored [55,56,57,58,59]. The aim of this review is to highlight publications in 2017 and 2018 that provide the clinician with new clinical and translational information regarding the recognition, identification, and mechanisms of DILI and HDS.
2 Methods
We performed an expansive search utilizing the PubMed search engine. We specifically searched for the following terms: DILI, hepatotoxins, mechanisms of DILI, herbal hepatotoxicity, and diagnosing DILI. We included articles that were published from January 2017 through September 2018. As more than 1800 articles appeared, we opted to focus on those specifically pertaining to new reports of established hepatotoxins, new reports of previously unknown hepatotoxins, mechanisms of DILI, and updates in international DILI registries. We limited our review to human studies unless we felt the specific article provided promising results at the forefront of DILI research. In addition, we only included studies written in English. Approximately 170 articles were used in the review process, across a variety of studies, including in vitro/ex vivo studies, case reports, and randomized controlled trials. Because of the large number of articles published in the last year on DILI, we tried to keep the review succinct, describing what we felt were the most innovative or informative for clinical practice. Articles not included should not be construed as lacking in importance or interest. A large portion of studies involved individual case reports as well as case series, which highlights the importance of the Roussel Uclaf Causality Assessment Method (RUCAM), our primary method of determining DILI due to a specific agent. We strove to only include cases that met a score of at least probable likelihood.
3 Drug-Induced Liver Injury (DILI) Registry Updates
3.1 US DILI Network
Authors from the US DILIN prospective study continued to publish new findings in several areas, including human leukocyte antigen (HLA) associations and other risk factors, differences among races, the effect of alcohol consumption, and updates in terms of diagnosis, prognosis, and several individual drug classes causing DILI, including autoimmune DILI.
De Boer et al. [1] characterized autoimmune hepatitis (AIH) in DILI by analyzing cases secondary to nitrofurantoin, minocycline, methyldopa, or hydralazine. They examined levels of immunoglobulin G (IgG) and titers of antinuclear antibodies (ANAs), smooth muscle antibody, and soluble liver antigen antibody, and derived an autoimmune score based on levels. This scoring system is summarized in Table 1. AIH-associated HLA antigens HLA-DRB1*03:01 and HLA-DRB1*04:01 allele frequencies in these cases were compared with controls. They defined an autoimmune phenotype as having an autoimmune score ≥ 2, which was present in the majority of cases with nitrofurantoin and minocycline (83 and 74%, respectively), whereas it was only seen in about one-half the cases with methyldopa and hydralazine (55 and 43%, respectively). Furthermore, the typical HLA alleles found in AIH (HLA-DRB1*03:01 and HLA-DRB1*04:01) were found at a rate in autoimmune DILI that was similar to that in the general population. In contrast to De Boer et al. [1], Urban et al. [3] found that HLA-B 35:02 was associated with an increased risk of liver injury from minocycline, thus providing a potential diagnostic tool for this type of liver injury.
Examining other HLA associations, Nicoletti et al. [2] performed a genome-wide association study to identify genetic risk factors for DILI from licensed drugs without previously reported genetic risk factors. They found an association between HLA-A*33:01 and DILI due to terbinafine and possibly fenofibrate and ticlopidine. They also identified the polymorphism rs116561224 on chromosome 18 associated with DILI from statins, along with two non-drug-specific risk factors including a single nucleotide polymorphism (SNP) on the LRBA gene and an intergenic SNP on chromosome 2, rs72631567 [2]. Fontana et al. [14] further discussed HLA associations with terbinafine-induced liver injury, which can be found in Sect. 5.2.
Whritenour et al. [4] attempted to incorporate the lymphocyte transformation test (LTT) into the DILIN framework. The LTT has been proposed as a way to assess hypersensitivity to a specific drug [4, 60]. Although it is not FDA approved, it is used elsewhere, especially in Japan [4, 61]. Suspect drugs are incubated with peripheral blood mononuclear cells (PBMCs), with a positive response seen when [3H]-thymidine is incorporated into new DNA. Using cytokine and granzyme B production, the authors developed a modified LTT (mLTT) and assessed PBMCs of donors with a history of drug hypersensitivity. Their results demonstrated that the mLTT was not a reliable test in diagnosing DILI for the majority of drugs: allopurinol, amoxicillin, carbamazepine, clavulanic acid, nitrofurantoin, isonicotinic acid, levofloxacin, metformin, minocycline, phenytoin, sulfamethoxazole, trimethoprim, and valproic acid. The only exception was isoniazid, where the authors observed that two of four samples elicited a positive mLTT response [4].
While not part of the US DILIN, we thought it was important to also note a similar study by Benesic et al. [62], who developed an in vitro test using monocyte-derived hepatocyte-like (MH) cells to help diagnose DILI in patients taking multiple medications. The premise of their test involved measuring the level of lactate dehydrogenase released from MH cells that had been isolated from a patient’s blood sample and incubated with each drug the patient was taking. Elevated levels of lactate dehydrogenase were considered to be positive for DILI. Their test demonstrated 92.3% sensitivity and 100% specificity. The drugs that tested positive for DILI with their method included amoxicillin–clavulanate, diclofenac, methylprednisolone, atorvastatin, metamizole, pembrolizumab, piperacillin/tazobactam, moxifloxacin, duloxetine, and sertraline. They also noted that a small subset of their patients were accidentally reintroduced to some of these medications, and the MH test correctly reidentified 92% of these drugs as being the culprit for liver injury [62].
US DILIN authors also continued to study microRNAs (miRNAs) for their potential utility as biomarkers for the diagnosis and prognosis of DILI. Russo et al. [5] examined sera from 78 subjects and showed that miRNA-122 combined with a low serum albumin (< 2.8 g/dL) accurately identified mortality within 6 months of acute DILI. If confirmed, this combination may prove useful in identifying patients who are at high risk of death and/or liver transplantation [5].
Bonkovsky et al. [6] examined the clinical presentation and prognosis of liver injury secondary to drugs associated with bile duct loss. By examining the US DILIN database for cases that included a liver biopsy, the authors identified 26 patients (7% of the total registry) with various degrees of bile duct loss (graded as mild, moderate, and severe) on histology. The most common clinical phenotype for these cases was a cholestatic pattern. Amoxicillin–clavulanate, HDS products, and temozolomide were associated with the most bile duct loss and were each implicated in three cases of bile duct loss, followed by azithromycin, fluoroquinolones, and lenalidomide/thalidomide, which were each implicated in two cases. Not surprisingly, patients with bile duct loss were more likely to develop chronic liver injury than were those without such injury (94 vs. 47%). The seriousness of the finding was demonstrated in that 5 of 26 patients died and another two required liver transplantation. The authors concluded that bile duct loss from DILI was indeed an indicator of vanishing bile duct syndrome, which currently has no cure or prevention [6].
Navarro et al. [7] summarized the work of a 2-day research symposium sponsored by the American Association for the Study of Liver Disease and the National Institutes of Health that focused on liver injury from HDS. In the USA, HDS now account for 20% of all hepatotoxicity cases. Challenges that emerged from this symposium included problems in diagnosis, identification of hepatotoxic constituents, regulation of nonprescription products, and developing strategic partnerships among physicians, chemists, toxicologists, and regulators [7]. Vega et al. [8] used the state of Delaware to look more closely at DILI, HILI, and HDS-induced liver injury. Using gastroenterologist-based surveillance data, the authors calculated an incidence of 2.7 cases per 100,000 adults in 2014, marking the first prospective estimate of DILI in the USA [8].
Another interesting area of study is the association of age, sex, and race with DILI. Suzuki et al. [9] examined 212 cases of DILI, studying differences between women aged < 50 years and others to assess the influence of menopause and sex on DILI. They noted that hepatocellular injury was significantly more prevalent in women aged < 50 years, with more severe interface hepatitis noted in these patients than in patients aged > 50 years from both sexes. Additionally, biopsies from female patients had greater plasma cell infiltrates, hepatocyte apoptosis, rosettes, and lobular disarray than those of males but less iron-positive hepatocytes and cholestatic features [9]. Chalasani et al. [10] examined racial differences between African Americans and Caucasians enrolled in the US DILIN prospective study. Drugs causing DILI differed among the two groups, with trimethoprim–sulfamethoxazole being the most common among African Americans and amoxicillin–clavulanate being much more common in Caucasians. More importantly, the authors noted a greater severity of illness in African American patients, defined by peak mean albumin, international normalized ratio (INR), and DILIN severity scores. They also observed higher rates of hospitalization, liver transplantation, and liver-related death at 6 months in acute DILI cases in African Americans compared with Caucasians (Table 2) [10].
Hayashi et al. [11] used the DILIN prospective study to analyze patients who had a fatal outcome within 2 years of acute DILI onset. The authors found that a higher peak bilirubin and the presence of coagulopathy, leukocytosis, and thrombocytopenia were all independently associated with death from DILI. Hayashi et al. [11] also studied a modified Hy’s law (nR Hy’s law criteria), defined as bilirubin ≥ 2.5 mg/dL and ([ALT/ULN] ÷ [alkaline phosphatase/ULN]) > 5, where aspartate transaminase (AST) is substituted for ALT if the AST yields a greater R ratio [11]. They noted that nR Hy’s law yielded a higher positive predictive value for fatality than the original Hy’s law (14 vs. 10%). Overall, their investigation found that DILI led to death in 7.6% of cases, either directly or indirectly, which continues to validate the observations of Hy Zimmerman [11]. The importance of this particular study by Hayashi et al. [11], specifically the creation of a modified Hy’s law, has been reinforced in a number of commentaries on their findings in the past year [63, 64].
Björnsson et al. [17] contributed to several areas of DILI in 2017, both within the US DILIN and in an Icelandic population. DILI induced by the antimetabolites azathioprine and 6-mercaptopurine was examined in 22 patients with injury from one of these two medications. Median time to onset of liver injury was 75 days. The most common symptoms were jaundice (73%), nausea (64%), and fatigue (50%) [17]. The authors noted that anicteric patients tended to present with a hepatocellular pattern of injury, whereas icteric patients generally had a mixed or cholestatic injury pattern. Median ALT was 210 U/L, alkaline phosphatase was 151 U/L, and bilirubin was 7.4 mg/dL with a peak of 13.4 mg/dL [17]. Most of the 22 patients recovered from their DILI within 3 months, usually by reducing the dose, as long as pre-existing liver disease was not present previously [17].
Björnsson et al. [18] also studied the response to corticosteroids in drug-induced AIH (DIAIH) in 14 Icelandic patients, 13 of whom were women. He noted the difficulties inherent in distinguishing DILI with autoimmune features from idiopathic AIH. In this cohort, 40% of patients had improvement in liver enzymes simply with drug cessation. The rest received corticosteroids at 30 or 40 mg/day for a mean of 4 months [18]. All patients had normalization of aminotransferases after a mean of 154 days [18]. Interestingly, none of the patients who required steroids experienced relapse, even after approximately 4 years of follow-up, which is not typically the case with idiopathic AIH [18].
Dakhoul et al. [12] examined the relationship between heavy alcohol consumption and DILI outcomes of patients enrolled in the US DILIN prospective study. The authors studied the characteristics of 348 patients with DILI (of 601 patients who reported alcohol consumption) who completed a questionnaire regarding alcohol use. They noted that anabolic steroids were the most common cause of DILI in those they defined as “heavy” alcohol drinkers (defined as an average of three drinks per day for men and two drinks per day for women). They did not find a significant difference in liver-associated deaths or need for transplant between heavy drinkers and nondrinkers [12]. However, outcomes were not reported for patients who may have far exceeded the two to three drinks per day minimum describing “heavy” alcohol consumption before or during acute DILI.
Another interesting area of study performed by the US DILIN was on sclerosing cholangitis (SC)-like changes seen on magnetic resonance cholangiopancreatography in patients with suspected DILI. A few studies have demonstrated this potential correlation, but they frequently included only a small number of cases. Ahmad et al. [13] looked at all patients within the US DILIN who underwent magnetic resonance imaging between 2004 and 2014. This initially yielded 233 patients, but imaging was available for only 83 of them. Among these 83, only 56 had imaging that was clear enough to be interpretable. In total, four patients had SC changes (7%). The authors noted they were unsure of why this happens in some cases of DILI, but they did discuss two important correlations, including that those with SC changes had not only more severe initial liver injury but also a higher incidence of chronic liver damage. While these conclusions are informative, their ultimate number of cases was small, despite looking at a 10-year period, so further study in this area is warranted.
3.2 Spanish DILI Registry
Several articles analyzed the Spanish DILI Registry and the Latin American DILI Registry, highlighting several important differences in drug hepatotoxicity outside of the USA. Zoubek et al. [15] examined ibuprofen-induced hepatotoxicity in 21 cases from the Spanish DILI Registry and five cases in the Latin American DILI Registry in comparison with both other nonsteroidal anti-inflammatory drug (NSAID)-induced DILI cases and non-NSAID DILI cases. The authors showed that ibuprofen was the most frequent NSAID known to cause DILI in Spain, but it was only the third-leading hepatotoxic drug in Latin America, behind nimesulide and diclofenac. A total of 29% of NSAID DILI cases were attributed to ibuprofen, and the authors postulated that the higher frequency in Spain compared with that in the USA might be secondary to the dose. In Spain, over-the-counter ibuprofen is available in both 200- and 400-mg formulations, whereas only the 200-mg dose is available in the USA [15].
Medina-Caliz et al. [16] characterized hepatotoxicity secondary to HDS recorded in the Spanish DILI registry. The authors found 32 patients from 1994 through 2016 with liver injury attributed to HDS. This group represented only 4% of the total registry, which is significantly lower than that found in the US DILIN. Of these 32 cases, 20 were secondary to anabolic steroids. The investigators noted a higher incidence of progression to acute liver failure in patients with HDS-induced liver injury (6%) than in either the anabolic steroid group (0%) or in the conventional drug group (4%) [16].
3.3 China
China has made significant strides to increase DILI awareness since 2014, with the establishment of the HepatoTox website, which is similar to the US LiverTox website and currently includes 400 drugs recorded in its database [19]. In addition, the Chinese Society of Hepatology drafted its own guidelines on the diagnosis and management of DILI [19]. These guidelines provided 16 evidence-based recommendations on the diagnosis, treatment, and prevention of DILI based on current practice in China. These recommendations share similarities to the 13 recommendations from the 2014 American College of Gastroenterology (ACG) clinical guidelines for diagnosing and managing idiosyncratic DILI [65] and incorporate some of the 2009 FDA guidelines for preventing hepatotoxicity in clinical trials (Tables 3, 4) [66].
3.4 Korea
Cho et al. [20] conducted a nationwide study specifically aimed at HILI in Korea. The authors prospectively collected data from April 2013 and January 2016 from 1001 inpatients from ten South Korean tertiary hospitals who were being treated with herbal medications. Of these patients, six were diagnosed with HILI based on RUCAM scores (four probable and two possible cases), although none of the cases had clinical symptoms. All of the patients were women who developed a hepatocellular pattern of HILI, and only one patient met the criteria for Hy’s law [20]. Based on these data, they calculated an incidence rate of just 0.6% over a span of nearly 3 years [20].
4 Newly Described Hepatotoxins
Only a few reports linked new drugs to DILI in 2017–2018. It is important to note that DILI is still much less common than other causes of acute liver injury [67]. Teschke and Danan [67] analyzed 22 DILI case series that included 13,335 cases and found that alternative causes were more likely than DILI in 34.2% of cases. Thus, although case reports are important in raising the possibility of DILI, they should not be seen as being conclusive for making a firm association.
Malnick et al. [68] described a case of denosumab-induced submassive hepatic necrosis that resulted from an immune reaction to the monoclonal antibody. Improvement in aminotransferases and gamma-glutamyl transferase (GGT) occurred following treatment with steroids. Namn et al. [69] reported what they described as the first case of acute liver failure from diphenhydramine without the concurrent use with acetaminophen, which developed in a 28-year-old man taking diphenhydramine 400 mg nightly for sleep. Unfortunately, no RUCAM or other causality score was applied in this case. Niijima et al. [70] described a 75-year-old patient with type 2 diabetes mellitus who switched to oral ipragliflozin, a sodium–glucose cotransporter-2 inhibitor, who then experienced cholestatic DILI, which improved after cessation of the medication. Conversely, this same drug is currently being studied to treat nonalcoholic fatty liver disease (NAFLD) and has recently been shown to exert equally beneficial effects as pioglitazone in NAFLD [71].
Patel et al. [72] discussed a case of everolimus-induced liver injury in a 56-year-old male who had received a liver transplant and was being maintained on this drug for immunosuppression. Their full analysis demonstrated a mixed hepatocellular and cholestatic type liver injury. They documented a RUCAM score of 8 (probable). Park et al. [73] reported a case of DILI in fimasartan, an angiotensin-receptor blocker (ARB). While they mentioned that hepatotoxicity was previously associated with other ARBs, there are currently no other published cases of fimasartan-induced liver injury. Workup included exclusion of other liver infections, trending of liver enzymes, and a liver biopsy demonstrating hepatocellular necrosis. The authors calculated a RUCAM score of 11 (highly probable) [73].
The FDA released a safety statement early in 2018 regarding the use of obeticholic acid in primary biliary cirrhosis, noting a significant number of incidences of inappropriate dosing of this particular medication, resulting in liver injury [74, 75]. Specifically, they noted that many patients were receiving supratherapeutic doses and that there were even some reports of liver injury with appropriate dosing of the drug. As a result, a safety statement was released to ensure that physicians pay close attention to the trending of liver enzymes when prescribing this drug [74].
Lugoboni et al. [76] studied the effect of high-dose benzodiazepines on the liver, as this class of drugs is primarily metabolized by the liver. They reviewed 201 cases of patients who had been admitted to an addiction treatment center for sole benzodiazepine misuse. They reviewed liver enzymes at admission and documented potential DILI if Hy’s law was met. They found that persistent high-dose benzodiazepine use did not result in significant hepatotoxicity despite its metabolic pathway [76].
4.1 Chemotherapy and DILI
There were several chemotherapeutic agents whose novel hepatotoxic profiles were noted for the first time. Honda et al. [77] described a case of rapidly developing hepatic fibrosis in a patient who received tegafur–uracil, even though administration was only short term. Edwards et al. [78] used multiple cancer center databases to find cases of vismodegib-associated hepatotoxicity. The authors found 94 reported cases in the FDA Adverse Event Reporting System, 35 of which were reported as severe adverse effects [78]. Sakumura et al. [79] described a case of sinusoidal obstruction syndrome (SOS) in a patient who received a non-hematopoietic-stem cell transplant. SOS has previously been described after hematopoietic-stem cell transplant from oxaliplatin-based neoadjuvant chemotherapy in metastatic colon cancer. The authors presented a 58-year-old Japanese man with lymphoma who was treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) and then switched to rituximab, cyclophosphamide, vincristine, doxorubicin, and methotrexate (R-CODOX-M) alternating with ifosfamide, etoposide, and high-dose cytarabine (IVAC) after two cycles. He experienced hepatocellular injury with a serum aminotransferase concentration ten times the ULN after the first cycle of R-CODOX-M. His clinical course deteriorated, and he died of cytomegalovirus pneumonia; on autopsy, he was diagnosed with hepatic SOS, likely secondary to R-CODOX-M [79].
Shah et al. [80] presented a case of an elderly woman who was thought to have developed DILI after receiving imatinib for the treatment of gastrointestinal stromal tumor. Initial laboratory testing showed significantly elevated AST (1450 U/L) and ALT (1632 U/L), with increased total bilirubin (4.9 mg/dL) and alkaline phosphatase (162 U/L). A liver biopsy demonstrated a histologic pattern of acute hepatitis consistent with DILI. Ultimately, discontinuation of imatinib led to recovery in the patient’s clinical condition along with normalization of her liver function tests over the next several weeks [80]. However, none of these case reports applied RUCAM or another causality assessment methodology to make the diagnosis of DILI.
SOS has also been linked to antibody–drug conjugates. In a study by McDonald et al. [81], a panel of hepatologists reviewed all subjects with liver abnormalities following inotuzumab ozogamicin (InO) therapy in patients with hematologic malignancy in two multicenter protocols. Patients (n = 638) were randomized to treatment with either InO or standard chemotherapy. The frequency of SOS was 5/328 (1.5%) compared with zero cases among the 310 controls. DILI developed in 26 (7.9%) of those in the treatment arm compared with three (1%) in the control arm. Overall, these data suggest that InO had a relatively low frequency of SOS but a relatively high frequency of DILI. However, for the most part, the manifestations of DILI were transient, with asymptomatic elevations of serum ALT, alkaline phosphatase, or total serum bilirubin. Unfortunately, it cannot be said with certainty whether DILI was related to InO exposure or toxicity from concomitant medications, as most patients in both arms of both protocols received antibiotics, antifungal drugs, and antiviral drugs [81].
4.1.1 Immune-Checkpoint Inhibitors
Tanaka et al. [82] described a case of steroid-refractory ipilimumab hepatotoxicity, which is a well-described adverse effect of immune-checkpoint inhibitors. While this form of liver injury usually responds to steroids alone, these clinicians successfully treated a refractory case with the combination of mycophenolate mofetil along with corticosteroids, which offers an alternative regimen when steroids alone are insufficient—notably, this strategy was initially described by Eigentler et al. [83] in 2016.
With regard to other immune-checkpoint inhibitors, Gelsomino et al. [84] presented what may be the first thoroughly examined case of nivolumab-induced cholangitic liver disease. Prior to this case, nivolumab had only been associated with transient immune-related toxicity without cholestatic injury [84]. Matsubara et al. [85] also reported a case of nivolumab-induced persistent liver injury in a patient with malignant melanoma. This patient experienced grade 3 ALT elevation after the first cycle of nivolumab at week 3, with spontaneous recovery and subsequent recurrent grade 4 ALT elevation after 17 cycles of nivolumab; this contrasts with a prior pooled analysis in which the onset of liver toxicity in nivolumab-treated patients was found to typically occur after 2–6 cycles [86]. Interestingly, liver injury in this patient was sustained for more than 5 months after discontinuing nivolumab therapy [85].
Zarrabi et al. [87] conducted a meta-analysis of 27 clinical trials focusing on potential liver injury associated with nivolumab. They demonstrated a statistically significant increase in incidence of AST and ALT elevations due to nivolumab in a variety of cancers. The authors also found the incidence of DILI was markedly increased when nivolumab was implemented as part of combination therapy, specifically when in conjunction with ipilimumab.
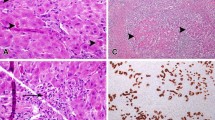
Zen et al. [88] presented a study that aimed to compare clinicopathologic features between checkpoint inhibitor-induced liver injury and acutely presenting AIH or idiosyncratic DILI. Seven patients treated with nivolumab or ipilimumab presented with liver dysfunction a median of 41 days after the initiation of immunotherapy. All patients had elevated liver enzymes; hyperbilirubinemia was less common. None of the patients had ANA or IgG elevations. Stopping the immunotherapy and increasing immunosuppression with additional corticosteroids normalized or decreased liver enzymes in all patients. Histologically, all biopsies showed predominantly lobular hepatitis with milder portal inflammation. Centrilobular confluent necrosis and plasmacytosis were observed in a single case and were less common and milder than those in AIH. One case each of bile duct injury, micro-abscesses, and extramedullary hematopoiesis was also found. Immunostaining revealed the presence of large numbers of cluster of differentiation (CD)-3+ and CD8+ lymphocytes, whereas CD20+ B cells and CD4+ T cells were fewer in checkpoint inhibitor-induced liver injury than in AIH or DILI. Overall, this histology study demonstrated that, although liver injury caused by cancer immunotherapy shares some features with injury of AIH, there are important differences between the two [88].
4.1.2 Chemotherapy-Associated Liver Injury
Vigano et al. [89] assessed the reversibility of chemotherapy-associated liver injury (CALI), notably in patients with colorectal cancer with liver metastases. CALI is important with regard to resection of liver metastases in metastatic colorectal cancer because of its association with increased postoperative morbidity and mortality [89]. The authors evaluated 429 patients undergoing liver resection for colorectal liver metastases who underwent neoadjuvant therapy with oxaliplatin and/or irinotecan. They noted that sinusoidal dilatation and nodular regenerative hyperplasia improved 9 months after chemotherapy and that an interval of > 270 days between chemotherapy and resection was an independent protective factor against grade 2–3 sinusoidal dilatation. However, steatosis and steatohepatitis were present even after 9 months, suggesting that CALI is only partially reversible [89].
Wakiya et al. [90] studied 64 patients undergoing oxaliplatin-based chemotherapy in three cohorts (< 65 years, 65–74 years, and > 75 years) to examine the effect of age in CALI. They observed no differences in sinusoidal injury or steatohepatitis and concluded that age alone did not play a role [90]. However, the three cohorts were unbalanced in terms of size, with 37 patients in the youngest cohort, compared with only ten in the oldest cohort and 17 in the middle age cohort [90].
4.2 Solithromycin
Solithromycin is a novel macrolide-ketolide specifically developed to combat the macrolide resistance seen in community-acquired bacterial pneumonia (CABP) [54]. It works similarly to other macrolides, binding to the large (50S) ribosomal subunit to inhibit protein synthesis; however, its longer alkyl-aryl side chains provide better anchoring [91].
Unfortunately, solithromycin was observed to cause a significant degree of transient aminotransferase elevations in its clinical trials [54, 92]. Specifically, Buege et al. [54] reported that elevations in ALT in the phase III trial were more than three, five and ten times the ULN in 7.2%, 2.4%, and 0.1%, respectively, of those treated with solithromycin versus 3.6%, 1.0%, and 0.2% of those treated with moxifloxacin as the comparator. Most solithromycin-treated patients had peak ALT values about 4 days after initiation of treatment, but up to 30% of patients developed peak levels following completion of treatment and up to 15 days later. Also noteworthy, the effect was more pronounced in those receiving the intravenous formulation as opposed to the oral formulation [54].
Given the hepatotoxicity risk, the FDA did not approve solithromycin for CABP, instead recommending a large safety study as they felt the risk of hepatotoxicity had not been adequately characterized [93]. The FDA asserted that, although a number of clinical trials were performed with this drug, not enough patients were included to fully understand the extent of the adverse side effects; they have requested a study including at least 9000 patients. In addition, the FDA noted that, if this future study finds no adverse effects, the availability of solithromycin to patients will still need to be limited, and it will not be used as a first-line option [92].
Of note, and although not the purpose of this paper, solithromycin is also being studied for its potential benefit in nonalcoholic steatohepatitis (NASH). One pilot study showed solithromycin improved NASH histologically, and these patients also saw a reduction in hepatic stiffness scores when measured by fibroscan [94]. We will continue to watch new developments with this agent to see how the difference between hepatotoxicity and hepatoprotection plays out and ultimately affects its approval and marketing.
5 New Reports of Established Hepatotoxins
5.1 Acetaminophen
While acetaminophen DILI is regularly studied, relatively few articles in the past 2 years provided significant advances in our understanding of intrinsic hepatotoxicity. Wong et al. [95] analyzed the accuracy of the paracetamol–aminotransferase multiplication product (APAP concentration [mg/L]) × ALT [IU/L]) as it pertains to modified-release paracetamol overdoses. The paracetamol–aminotransferase multiplication product has typically been studied and confirmed with immediate-release paracetamol [95,96,97]; this study used the modified-release formulation. They specifically noted that a multiplication product above 10,000 mg/L × IU/L was highly predictive of developing hepatotoxicity, whereas products < 1500 mg/L × IU/L were much less likely to cause acute liver injury [95].
Heard et al. [98, 99] studied acetaminophen protein adducts as a potential diagnostic biomarker of acetaminophen-induced liver injury in both children and adults. They performed a cross-sectional study in 100 children aged 1–12 years [98]. Of those whose caregivers confirmed they had received acetaminophen within the previous 2 weeks, 52% tested positive for the presence of the protein adduct, whereas 100% of those who denied acetaminophen use within the previous 2 weeks tested negative for the protein adduct [98]. Similarly, this same group of researchers studied the acetaminophen protein adduct in an adult population [99]. The study included 230 patients, with 42% of those who confirmed taking acetaminophen in the previous 2 weeks testing positive for the protein adduct and 99% of those who denied acetaminophen ingestion within the previous 2 weeks testing negative [99]. Both studies found a positive correlation between the serum level of the protein adduct and the time of ingestion and dose of the acetaminophen [98, 99]. For further information on the utility of acetaminophen protein adducts and the future of SNPs linked to acetaminophen-induced liver injury, the reader is directed to a thorough review by Heruth et al. [100].
On a similar note, Roberts et al. [101] developed a point-of-care test, called AcetaSTAT, for serum levels of the acetaminophen protein adduct and compared the results against those from a standard highly specific and sensitive quantitative assay. Their study included 19 patients with no exposure to acetaminophen, 29 patients with therapeutic dosing of acetaminophen, and 33 patients with acute liver injury due to acetaminophen. They observed a high level of concordance between the two assays. For patients with acute liver injury, the AcetaSTAT had 100% sensitivity, 86.2% sensitivity, 89.2% positive predictive value, and 100% negative predictive value [101].
5.2 Antifungals
Dob et al. [102] looked at the hepatotoxicity profiles of five major antimycotics used in invasive fungal disease, including caspofungin, liposomal amphotericin B, anidulafungin, fluconazole, and voriconazole. They used human hepatocytes with a previously established in vitro cytotoxicity screening model to analyze synthetic liver function at varying clinical doses of these antifungals. More specifically, they measured the following parameters: viability of cells, synthesis of albumin, cytochrome 1A2 activity, and cell death. They found that liposomal amphotericin B, caspofungin, and anidulafungin all demonstrated mild levels of hepatotoxicity. However, as drug concentrations increased, anidulafungin was associated with severe liver injury, and both fluconazole and voriconazole demonstrated dose-dependent liver injury. The mechanisms by which these drugs caused hepatotoxicity have not been fully delineated. This study confirmed that therapeutic drug monitoring is recommended for any patient who requires ‘azole’ therapy and already has some degree of hepatic dysfunction and that close monitoring is advised for any patient who requires treatment with anidulafungin [102].
In contrast to the findings of Dob et al. [102], Pettit et al. [103] specifically found that therapeutic drug monitoring may not be necessary for patients receiving posaconazole. However, their study was retrospective in nature, involving individuals who required therapy with posaconazole, such as those who underwent bone marrow transplant, and Pettit et al. [103] did not analyze varying doses. Their goal was therapeutic dosing, and while they did not observe any relationship between the posaconazole serum concentration and a linear change in liver enzymes, they did note that increases in the liver enzymes were seen predominantly in patients who were or had been receiving concomitant hepatotoxic medications.
Gayam et al. [104] reported a single case of DILI in an individual receiving intravenous fluconazole for sepsis due to inguinal candidiasis. After initiation of the antifungal, the patient subsequently had a rise in AST and ALT to 25,000 IU/L and 6500 IU/L, respectively, on day 3 of hospitalization [104]. The fluconazole was promptly discontinued, and the AST/ALT trended down within 3 days. This patient had no underlying kidney or liver impairment. The authors confirmed this was an adverse drug reaction (ADR) using the Naranjo algorithm, which yielded a score of 10, suggesting definite ADR. To establish causality, a RUCAM score of 11 was calculated, indicating highly probable. Notably, the patient did report having had elevated liver enzymes approximately 1 year prior after receiving oral fluconazole for candiduria. This case not only highlights the importance of a detailed history but also shows how a positive response when re-exposed to a particular medication can help establish causality through RUCAM [104].
As discussed, new genotypic polymorphisms continue to be identified as risk factors for DILI. Fontana et al. [14] discussed specific HLA polymorphisms in regard to the antifungal drug, terbinafine, that may predispose patients to liver injury. After reviewing a small population of patients with terbinafine-associated hepatotoxicity (determined by the DILIN causality committee), the authors found that HLA-A*33:01, HLA-B*14:02, and HLA-C*08:02 were significantly overrepresented in these particular patients. More specifically, these haplotypes were present in 91% of study patients with European ancestry but 1.6% of those in the control group with European ancestry. Molecular docking studies strengthened the association. In short, the authors obtained the sequences of HLA-A*33:01, HLA-A*33:03, HLA-B*14:02, and HLA-C*08:02 and generated atomic models. Their research found terbinafine had the potential to interact with all four haplotypes with moderate affinities. This highlights the increasing importance of identifying genetic risks factors for DILI [14].
5.3 Tolvaptan
Tolvaptan is a vasopressin receptor antagonist used for the short-term treatment of hyponatremia and long-term treatment of adult polycystic kidney disease (ADPKD) to reduce cyst burden. DILI has only been demonstrated in those with ADPKD taking the drug long term [105]. The mechanism by which DILI occurs is unknown, as the initial animal models in which tolvaptan was tested did not demonstrate any evidence of hepatotoxicity [106]. Mosedale et al. [107] utilized a collaborative cross mouse line to help delineate the mechanism of liver damage. This line is unique in that it has been found to be superior to the traditional mouse models [108, 109]. Indeed, Mosedale et al. [107] found that hepatotoxicity was induced by oxidative stress, with downstream immune system activation in addition to disruption of bile acid homeostasis. Moreover, they found that altering the bile acid composition actually led to the largest increase in ALT levels. Finally, they also found a potential biomarker linked to tolvaptan-induced liver injury in the form of elevated levels of secretory leukocyte peptidase inhibitor messenger RNA [107].
In a different study, Mosedale et al. [110] used primary human hepatocytes for further study into the mechanism of tolvaptan-induced liver injury. They treated the hepatocytes with various doses of the drug and then measured the miRNA-122 levels. They found that the highest level of miRNA-122 correlated with increased incidence of cell death. Early increases of miRNA-122 correlated with increased apoptosis and oxidative stress. Notably, at each of these drug concentrations, there was no significant increase in alanine aminotransferase levels. The significance of this is that therapeutic levels of tolvaptan could potentially induce serious liver injury via the immune system before any significant change in liver transaminases occurs [110].
In addition, tolvaptan has been the subject of a number of studies utilizing quantitative systems pharmacology (QSP) over the last 2 years [111, 112]. An in silico model known as DILIsym® has been gaining more recognition as a diagnostic tool for idiosyncratic DILI and has previously been applied to tolvaptan. The reader is directed to a number of articles further addressing tolvaptan and QSP [111,112,113].
5.4 Enalapril
Enalapril is an angiotensin-converting enzyme (ACE) inhibitor most frequently used in cardiovascular disease. Overall, the incidence of DILI with ACE inhibitors is considered low, although the VigiBase (World Health Organization (WHO) individual case safety report database) contains reports of several hundred cases, although it must be noted that the quality of some of these reports is questionable [114, 115]. Table 5 demonstrates the number of reported cases of DILI associated with each ACE inhibitor. It is important to note that the number of DILI cases associated with each of the drugs listed in Table 5 may fluctuate according to how frequently it is prescribed [115]. Currently, the mechanism of DILI induced by enalapril is unknown. Shirai et al. [116] utilized a mouse model and hypothesized that the mechanism of DILI was centered on oxidative stress in livers with existing hepatic steatosis. While this has not yet been confirmed in humans, such information may be clinically useful when prescribing ACE inhibitors to a patient with pre-existing fatty liver disease.
5.5 Direct-Acting Oral Anticoagulants
Direct-acting oral anticoagulants (DOACs), also known as non-vitamin K antagonists, have become increasingly popular and are commonly used for prevention of stroke in patients with nonvalvular atrial fibrillation. The possibility of increased hepatotoxicity has been raised as a concern, with multiple cases of liver injury thought to be related to this class of drugs [117, 118]. To examine this further, Alonso et al. [119] analyzed 113,000 patients and found a decreased incidence of liver injury when directly comparing DOACs and warfarin. The results from this study were later confirmed by Douros et al. [120], who studied a population of 52,000 patients from the Canadian health database from 2011 to 2014. They found no association of increased liver injury in two populations, including those with and without a previous history of liver disease. Current European Heart Rhythm Association guidelines recommend checking liver enzymes once per year for patients receiving a DOAC [121]; however, the usefulness of such arbitrary monitoring can certainly be questioned. Douros et al. [120] emphasize that the status of any liver disease should not preclude the use of a DOAC if it would otherwise be the best available option for that patient.
5.6 Antivirals
In 2016, a number of studies warned of the potential hepatotoxic nature of direct-acting antivirals (DAAs) in regard to treatment of hepatitis C virus (HCV) infection and the potential risk of hepatic decompensation or reactivation of hepatitis B with this class of drugs [122]. Mishra et al. [123] provided an updated commentary on HCV DAAs. They reviewed the previously established ‘rule-of-2’ model (Ro2) [124] and its potential as a DILI risk assessment tool specifically with HCV DAAs. The Ro2 model states that increased lipophilicity (logP > 3) and high daily drug dose (> 100 mg/day) may result in an increased risk of DILI. In applying this model to the 12 DAAs currently available for HCV treatment, they found that the Ro2 model correctly identified those with known increased risk for hepatotoxicity (e.g., paritaprevir, dasabuvir, and simeprevir) when compared with each drug’s initial clinical trial results. The specificity of the Ro2 model was high (~ 95%), suggesting it may be a good screening tool for DAA selection. With that said, Mishra et al. [123] noted that further research is necessary to further confirm the potential utility of this model, including larger prospective studies.
Segamwenge et al. [125] presented a case series looking at the effects of antiretroviral therapy, specifically efavirenz, on the liver. They presented four patients with potential DILI secondary to efavirenz. All four were found to have a hepatocellular-type liver injury as evidenced by their R ratios being > 5, and a causality score was calculated for all patients using RUCAM. Three of the cases were found to be probable and one unlikely. See Table 6 for more details. The authors argued that hepatotoxicity as a result of efavirenz was not as rare as suggested in the literature and advocated for regular monitoring of liver enzymes while receiving this medication [125].
5.7 Antiarrhythmics
Although amiodarone-induced liver injury (AILI) has been extensively documented, less is known about patient-specific risk factors for this type of injury. Diab et al. [126] created a prospective case–control trial with 180 patients from intensive care units receiving intravenous amiodarone. The study found that the presence of the following factors were most predictive for the development of AILI: cardiomyopathy, congestive hepatomegaly, increasing baseline total bilirubin, direct current cardioversion, and increasing dose of amiodarone. These were all found to be independent predictors for AILI and all were statistically significant. Risk factors for severe AILI (AST or ALT more than five times the ULN) included the use of inotropic support, presence of congestive hepatomegaly, increasing baseline total bilirubin, and increasing dose of amiodarone. The authors recommend considering these risk factors before initiating intravenous amiodarone, especially for non-life-threatening conditions such as mild, uncomplicated atrial fibrillation [126].
Grimaldi-Bensouda et al. [127] also contributed to our understanding of the effects of amiodarone on the liver as part of their study examining the effects of all classes of antiarrhythmics on acute liver injury. They were inspired after the European Medicines Agency received several reports of acute liver injury following dronedarone administration a few years prior. To summarize, they found that only class III antiarrhythmics were statistically associated with an increased risk of acute liver injury (3.61; 95% confidence interval (CI) 1.56–8.35), of which amiodarone had the largest effect (odds ratio (OR) 5.90; 95% CI 1.74–20.00). Dronedarone also yielded an increased risk for acute liver injury, but the results were not statistically significant (OR 3.1; 95% CI 0.7–14.8). Classes I, II, and IV also did not show statistically meaningful associations. The authors acknowledged the wide CIs and attributed them to the overall low exposure of class III antiarrhythmics [127].
5.8 Antituberculosis Drugs
The typical therapeutic regimen for treating tuberculosis (rifampicin, isoniazid, pyrazinamide, and ethambutol) has been suggested to be associated with elevated liver enzymes in patients who possess a unique genotype of NAT2 [128]. However, when Zhang et al. [129] reviewed the literature, they noted inconsistent conclusions about the association between NAT2 polymorphisms and antituberculosis drug-induced liver injury (ATDILI). To better clarify the role of NAT2 polymorphisms in ATDILI, they performed a meta-analysis of 37 studies and found an overall OR of 3.15 (p < 0.005) for slow acetylators and risk of ATDILI. They also recognized this association was more or less pronounced depending on the patient population, with an OR of 6.42 for West Asian populations and 2.32 for European populations. The association between slow acetylators and ATDILI was further confirmed when results were consistent and independent of study design and genotyping methods [129].
Also new in 2018 was the identification of a subset of slow acetylators who are at even higher risk for liver injury, namely the ultra-slow acetylators. Using a meta-analysis, Suvichapanich et al. [128] identified that NAT2*6A and NAT2*7B genotypes were particularly susceptible to ATDILI. They found NAT2 ultra-slow acetylators and slow acetylators were at increased risk of ATDILI, with ORs of 3.6 and 2.80, respectively, when each were compared with fast acetylators. When directly comparing ultra-slow acetylators with slow acetylators, the increased risk of ATDILI continued, with an OR of 1.33 [128].
Zhang et al. [129] went on to propose the potential future implications of acetylator status on patient care and treatment of tuberculosis. They specifically discussed that physicians are given a unique opportunity to provide personalized medicine by tailoring dosing of medication according to the speed of specific NAT2 polymorphisms as a means to reducing overall adverse events, including ATDILI [129].
5.9 Steroids
Relapses and flares of many autoimmune conditions are often treated with high doses of corticosteroids. While most of the evidence for steroid-induced DILI is in the form of case reports, Nociti et al. [130] carried out a prospective study to further evaluate the incidence, severity, and risk factors for DILI, specifically in patients with multiple sclerosis treated with intravenous steroids. They included 175 patients who were treated with pulsed methylprednisolone during a 12-month period. Liver enzymes were checked 2 weeks after intravenous steroid therapy and were found to be elevated in 21 cases, six of which were regarded as severe elevations of ALT according to Hy’s law. The following causality assessment tools were used to determine the etiology of liver injury in these patients: the Naranjo scale, the WHO—Uppsala Monitoring Centre (UMC) causality assessment, RUCAM, and the Autoimmune Hepatitis Scoring System (IAHG). Ultimately, three patients received a diagnosis of possible, probable, or highly probable for DILI, and the other three were probable or definite AIH. This study highlighted the importance of deciphering between the toxic effects of steroids and novel presentations of AIH, as the difference has significant implications not only for treatment of the liver injury but also for subsequent management of the autoimmune condition [130].
Bresteau et al. [131] and Dumortier et al. [132] discussed similar cases. Both sets of authors demonstrated cases of DILI in patients receiving high-dose methylprednisolone for multiple sclerosis. Bresteau et al. [131] specifically discussed a 35-year-old woman whose ALT and AST peaked at 1512 IU/L and 778 IU/L, respectively. A RUCAM assessment was applied, with a result of 8, indicating probable DILI. The authors reviewed 12 previously published cases of methylprednisolone-induced liver injury in patients with multiple sclerosis. In all cases in which the appropriate information was available, R ratios were > 5 and RUCAM scores were suggestive of DILI [131]. Dumortier et al. [132] discussed a case of methylprednisolone-induced liver injury in addition to four other cases reported by the French pharmacovigilance center of Lyon. Their patient demonstrated evidence of acute hepatitis on liver biopsy. All five cases scored between 6 and 10 on the RUCAM scale, indicating probable to highly probable DILI. Three of the five patients had positive re-challenges to confirm causality [132].
5.10 Antidepressants
Billioti et al. [133] attempted to quantify the association between observed liver injury and antidepressants, specifically comparing risks between classes. Using data from the French National Health Insurance Database, the authors identified nearly 5 million patients who were initiated on an antidepressant from 2010 to 2015. Of these, 382 serious liver injuries were identified, all attributed to various classes of antidepressants and occurring with a mean of approximately 2 months after initiation of therapy. Age- and sex-adjusted incidence rates were 19.2, 22.2, 12.6, and 32.8 per 100,000 person-years for selective serotonin reuptake inhibitors (SSRIs), including venlafaxine, duloxetine, and mirtazapine, respectively. When compared specifically with SSRIs, no other classes of antidepressants were significantly associated with an increased risk of DILI. The authors did note that some antidepressants, namely duloxetine, have previously been identified in premarketing clinical trials as causing liver injury so are contraindicated in patients with liver disease, and as such could explain the lack of observed differences from this trial [133].
Ferrajolo et al. [134] presented a case–control series of 17 patients with liver injury due to antidepressants. The 17 exposed patients were matched to 99 controls. While the authors did not apply any specific causality scoring system to the cases, they did calculate a statistically significant OR of 1.84 (95% CI 1.02–3.32) for increased risk of liver injury associated with current use of antidepressants. Notably, citalopram, an SSRI, was observed to have an increased incidence of elevations in ALT compared with other antidepressants [134].
5.11 Antitumor Necrosis Factor-α Inhibitors
Kok et al. [135] reported a case series of anti-tumor necrosis factor (TNF)-α-associated acute liver failure; four cases were reported, with an additional five identified on literature review. The majority of individuals affected were female (eight of nine cases). The most common anti-TNF-α agent associated with acute liver failure was infliximab (n = 8). The latency between initial drug exposure and acute liver failure ranged from 3 days to over a year. Of the nine cases, six required emergency liver transplantation. Liver biopsy was obtained in seven cases; cholestatic–hepatic features were frequently found on pretransplant and explant histology; none of the biopsies showed clear autoimmune features, which is more typical of anti-TNF-α acute liver injury. Further, only three of the nine cases demonstrated hepatocellular injury, which is in contrast with previous literature documenting this as the more common anti-TNF-α-associated acute liver injury pathology. The authors concluded that anti-TNF-α-associated acute liver failure displays somewhat different characteristics than less serious acute liver injury. RUCAM scores were ascertained in four of the cases, and all four were deemed to have at least probable causality from the anti-TNF-α agent (RUCAM scores 6–7) [135].
Table 7 lists the other drugs reported to cause DILI in 2017 as well as in other recent summaries [136]. The causality assessment methodology used to diagnose DILI is provided when stated by the authors.
6 Herbal and Dietary Supplement (HDS)-Induced Liver Injury
A number of reports involving liver injury from HDS are discussed earlier in this review [7]. Alongside registry data, various individual case reports and other work appeared in 2017–2018 that add to the growing list of HILI and HDS-induced liver injury agents. Continued understanding of HDS that can cause liver damage is important, as the incidence is ever-increasing and has a significant impact on health. Wong et al. [137] discussed that, in the Asia-Pacific region especially, the incidence has been as high as 81% of DILI cases. Wang et al. [138] discovered that, in China, traditional Chinese medicine (TCM) accounted for almost 26% of DILI cases. In contrast, the incidence of HILI in the USA was significantly lower. In China, Liu et al. [139] attempted to create a database to organize the data on HILI into a format that could easily be used to study and evaluate and therefore prevent future cases of liver injury from herbal medications, which helps to fulfill the recommendations of Wong et al. [137].
To help standardize the process of identifying HILI, another group of authors from the China Association of Chinese Medicine (CACM) created a set of nine recommendations, which are summarized in Table 8 [140].
Jing et al. [141] reiterate the importance of recommendation 1 in the proposed CACM guidelines for evaluation of HILI as Chinese medicine (CM)/herbal medicine (HM) are very different from synthetic drugs. Both sets of authors discuss that CM/HM are typically composed of multiple ingredients as opposed to synthetic drugs, which are made of a single agent [140, 141]. In addition, the actual incidence of HILI from CM is much lower than that of DILI. Further, Jing et al. [141] found that various analyses indicated other key features differentiated CM-HILI from DILI and as such, they should continue to be treated as separate entities.
Melchart and Teschke [21] reported on a large prospective, hospital-based study involving over 21,000 patients at the Hospital for TCM in Bad Kötzting, Germany, from 1994 to 2015. This study was the first to evaluate HILI at a single institution of such magnitude. They noted ALT increases of more than five times the ULN were seen in only 0.12% of patients, most being classified as “possible” HILI by RUCAM assessment, with the most common herbal medications implicated being Bupleuri radix and Scutellariae radix [21].
In addition to the herbal medications more well-known to cause liver injury, some newer agents are increasingly being reported, including Kratom (Mitragyna speciosa), Garcinia cambogia, red yeast rice, and Ayurvedic compounds.
Kratom, a tropical tree typically found in Southeast Asia and Africa, has been identified as an opiate receptor agonist, with a number of cases linking its abuse with cholestatic liver injury [26, 27]. Tayabali et al. [26] described a case of Kratom-induced HILI that scored an 8 via RUCAM (highly probable). For confirmation of their RUCAM scoring, they used liquid mass chromatography spectrometry [26]. The FDA has since made the use of Kratom illegal, as it appears to be fostering the opiate crisis with its similar physiologic effects, relatively easy accessibility, and lower cost than true opiates [26, 28].
Garcinia cambogia is an herbal supplement that is being used as a weight loss aid. Its active ingredient is hydroxycitric acid. No standard guidelines exist on how to safely take this supplement [29]. Initially, no concrete evidence existed to prove this supplement was directly causing hepatotoxicity, as it typically comes in a form combined with many other supplements. However, within the last 2 years, the number of people who have taken ‘purified’ G. cambogia and experienced associated hepatotoxicity has increased. In 2018, Sharma et al. [30] described a case of potential G. cambogia-induced liver injury. The authors used RUCAM to assess for causality, and the analysis yielded an 11, equating to highly probable. This supplement primarily causes hepatocellular liver injury with a wide range of observed clinical presentations, from acute hepatitis to acute liver failure requiring transplantation [29,30,31,32,33].
Red yeast rice is a Chinese herbal medication used as an adjunct for dyslipidemia that has been reported to cause liver injury [37]. Mazzanti et al. [37] used the Italian Surveillance System of Natural Products to review the incidence of liver injury associated with red yeast rice from 2002 to 2015 and found ten documented cases. The majority of these cases resulted in acute hepatitis requiring hospitalization. While the authors noted ten cases, RUCAM had only been applied to two, only one of which provided a significant association (7, probable). For seven of the other cases, the authors applied the WHO method for causality assessment, which yielded six “probable” case and one “unlikely” case. For the tenth case, not enough information was available to use any type of causality assessment. A more commonly seen side effect noted by the authors was an elevation of the creatine phosphokinase and general gastrointestinal reactions, including nausea and emesis [37].
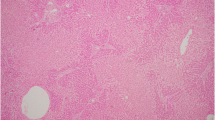
Finally, reports of Ayurvedic compounds causing various forms of liver injury have been increasing [22, 34, 35]. Phillips et al. [34] studied a population of patients from South India and attempted to characterize the histopathologic patterns of Ayurvedic-induced liver injury. Based on RUCAM scoring, they found 33 patients. Their results demonstrated that males had a higher incidence of liver injury, unlike the incidence of DILI in the Western world. Chronic hepatitis was the most common type of inflammation seen on histology. In addition, they found that heavy metals and hepatotoxic volatile organic compounds were present in > 70% of the compounds. Like many of the authors in the last year studying Chinese herbal medication-induced liver injury, Phillips et al. [34] and Devarbhavi [35] stressed that a larger governmental process regulating use and production of these compounds is necessary.
Table 9 lists other case reports of agents causing HILI in the last 1.5 years.
Wang et al. [36] further studied Polygonum multiflorum, a Chinese herbal medication used for anti-aging effects, in a case series of 29 patients in an attempt to discover more about the mechanism of liver injury. They noted that the majority of patients experienced severe hepatitis. After withdrawal from the herbal medication, most patients had resolution of liver injury, although the authors noted that some patients did progress to chronic disease.
7 Causality Assessment of DILI and HDS Cases
The RUCAM remains the most widely used assessment tool specifically developed for DILI. It was updated by Danan and Teschke [142] in 2016, and its value was reinforced by Teschke et al. [38] in their recent review on biomarkers and their role in causality assessment. While RUCAM has a significant number of advantages over other less liver-specific methodologies, including a stepwise, structured format that has been consistently validated and can be tailored to individual patients, a number of limitations remain. Björnsson and Hoofnagle [115] discussed the importance of knowing the quality of the data in published studies. DILI remains a diagnosis of exclusion [115]. As mentioned, RUCAM continues to be the most reliable method of determining causality, although numerous published reports of suspected or alleged DILI still appear without calculating a liver-specific causality assessment score such as RUCAM. In 2010, Agarwal et al. [143] found that most published studies fell far short of a true diagnosis of DILI. Björnsson et al. [115] analyzed reports of DILI listed on the LiverTox website and found that only 53% of 671 agents demonstrated enough evidence to make a diagnosis of DILI. More recently, Barnhill et al. [168] evaluated case reports and case series from the 2017 literature to see whether the use of causality assessment methodologies had improved since 2010. Perhaps not surprisingly, they found that many publications still did not contain the minimally necessary information to diagnose and accurately assess DILI.
As no specific diagnostic marker exists for DILI, we rely on the literature to provide us accurate reports as DILI is a diagnosis of exclusion and many other diseases can mimic it. Ganger et al. [135] found in the Acute Liver Failure Study Group (ALFSG) registry that 11% of the cases (303 patients) were listed as indeterminate etiology. The authors performed a more thorough investigation of each of these cases and found “highly likely” versus “probable” etiologies for 142 of the cases. Interestingly, they determined that 11 of the cases did not even meet the criteria for acute liver failure [144]. Such difficulties in proving causation have spurred the ongoing research efforts to identify a pathognomonic diagnostic blood (or other tissue) biomarker for DILI. In the meantime, as echoed by Björnsson and Hoofnagle [115], it is imperative that authors (and, we would add, reviewers and journal editors) follow a standardized method for diagnosing DILI to prevent poorly or undocumented cases from contaminating the literature.
In 2017, Scalfaro et al. [145] attempted to modify the RUCAM score and apply it to pharmacovigilance data (PV-RUCAM), which are often imperfectly documented. This new scoring system was developed from the original RUCAM, whose purpose was to standardize the process of confirming DILI in cases where it was suspected. This new system was found to have 100% sensitivity, and 91% specificity, with 25% positive predictive value and 100% negative predictive value. Although the authors acknowledged that more prospective research is necessary to confirm the utility of this modified scoring method, we would agree it represents an advance in how postmarketing surveillance for DILI is currently being performed.
Over the past 2 years, significant research has continued in the area of miRNAs and their potential to diagnose or predict the severity of DILI. The reader is directed to several sources for more in-depth reviews of the newly described miRNAs in 2017 and 2018 [113, 145,146,148]. Several studies confirmed the increased sensitivity and specificity of miRNA-122, specifically with DILI due to acetaminophen and amoxicillin–clavulanate [5, 148,149,151].
Similarly, DILI risk factors, particularly HLAs and other potential biomarkers where the continued focus of study in the past year, and the interested reader is referred to any number of recent reviews on this important topic [12, 39,40,41,42,43,44,45,46,47,48,49,50,51].
8 Updates in the Mechanisms of DILI
Much remains to be discovered in terms of the mechanisms of DILI, particularly that of idiosyncratic DILI. Mosedale et al. [42] and Cho et al. [152] reviewed the key components that lead to DILI, including changes within bile acid homeostasis, oxidative stress, and mitochondrial dysfunction. Similarly, Dakhoul et al. [153] provided a succinct review of various pathologic phenotypes of DILI with associated causative agents and histologic findings. Overall, many studies were published in 2017–2018 regarding DILI mechanisms—a select number of which have been selected for closer review as they provide important conclusions on this topic (Table 10).
8.1 Bile Salt Export Pumps
Bile salt export pumps have become an important area of study as they are a primary mechanism for cholestatic DILI. Multidrug-resistance-associated protein 3 (MRP3) is a specific type of bile salt export pump that is emerging as a primary constituent in cholestatic liver injury [154]. Ali et al. [155] created a model that specifically addressed cholestasis by predicting agents that would potentially inhibit this transporter. Using their model, they confirmed MRP3 inhibition at the cellular level, utilizing three MRP3 inhibitors: fidaxomicin, suramin, and dronedarone.
8.2 DILI and the Immune System
Ogese et al. [156] described a novel mechanism for DILI involving antigen-specific T cells, noting that these types of cells were found to be upregulated with DILI. Roth et al. [55] observed that cytokines are also upregulated with DILI, specifically, TNF-α and interferon (IFN)-γ, based on a model using human hepatocytes with the known hepatotoxic agents flucloxacillin, amoxicillin, and isoniazid. Based on these in vitro studies, they postulated that IFN-γ likely induces the formation of TNF-α, causing a cascade of cellular injury and eventuating in cell death. Their results suggest that these two molecules may be acting synergistically, but further data are needed. Similarly, Jian et al. [56] found that ceramide, an intracellular molecule, is upregulated when the immune system is activated and specifically induces hepatocyte apoptosis.
Kato and Uetrecht [57] expanded the knowledge that damage-associated molecular patterns (DAMPs) activate the immune system and are released by reactive metabolites, creating an inflammatory response within the liver and subsequently eliciting liver damage. These investigators hypothesized that drugs associated with idiosyncratic DILI could be tracked based on whether they released these DAMPs. They proved their theory by studying two drugs highly associated with idiosyncratic DILI (amodiaquine and nevirapine) and measuring high levels of DAMPs when either drug was given [57].
Mitochondrial dysfunction has also been linked to idiosyncratic DILI, specifically with acetaminophen toxicity [58]. Ramachandran and Jaeschke [59] reviewed that more progress has been made on the role of the innate immune system in acetaminophen toxicity, particularly regarding oxidative stress created by mitochondria. However, some controversy remains over the role of both neutrophils and some proinflammatory mediators, including interleukin (IL)-1β. They echo that more research is warranted on this topic [59].
Goda et al. [157] discovered that lipophilicity, an inherent pharmacologic property of drugs themselves, can be linked to mitochondrial dysfunction progressing to liver dysfunction. McEuen et al. [158] specifically looked at the DILIrank dataset with 1036 FDA-approved drugs to assess the relationship between lipophilicity and DILI. Their analysis confirmed that increased lipophilicity was associated with DILI. While this result was technically statistically significant, they did note it was not a strong association and requires further research. The authors also echoed results from previous studies that lipophilic drugs can be metabolized to toxic forms due to the extensive distribution within the body and that these toxic forms can cause oxidative stress via mitochondria and a subsequent inflammatory immune response [158].
9 Conclusions
Drug-induced liver injury and hepatic injury secondary to HDS continues to be a major area of study in the field of drug safety. Investigators continued to broaden our knowledge base of DILI, HILI, and HDS in the past year. This included work from the DILIN prospective study and other international registries. While only a few new cases of DILI and HILI were reported in the literature in 2017–2018, there were numerous publications concerning liver injury secondary to known agents, including a few important differences between DILI affecting Caucasians and African Americans, and the genetic and environmental risk factors affecting DILI. In addition, many authors reinforced the concept that herbal medications require more regulation as reports of associated liver injury are increasing. An analysis of alcohol intake in the US DILIN prospective study found no differences in outcome between nondrinkers and “heavy” drinkers who developed acute DILI, although anabolic steroid use was more likely to be the cause among those drinking the most, perhaps reflecting a lifestyle choice among these individuals. Whether or not alcoholics are at greater risk was not specifically addressed in their results, as “heavy drinking” was not further characterized. Acetaminophen protein adducts continue to demonstrate their utility with high positive and negative predictive values. Immune-checkpoint inhibitors in addition to antivirals for HCV and HIV treatments continue to pose an increasing risk of liver injury and require continuous liver enzyme monitoring. Finally, the roles of bile salt export pumps and the immune system as they relate to the pathophysiology of DILI continued to be a subject of interest this past year. As investigators continue to work on increasing our understanding of DILI and injury secondary to HDS, we look forward to the time when the clinician’s ability to diagnose and manage DILI will become a much more simplified task.
References
de Boer YS, Kosinski AS, Urban TJ, Zhao Z, Long N, Chalasani N, et al. Features of autoimmune hepatitis in patients with drug-induced liver injury. Clin Gastroenterol Hepatol. 2017;15(1):103–12.
Nicoletti P, Aithal GP, Bjornsson ES, Andrade R, Sawle A, Arrese M, International Drug-Induced Liver Injury Consortium, Drug-Induced Liver Injury Network Investigators, and International Serious Adverse Events Consortium, et al. Association of liver injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterology. 2017;152(5):1078–89.
Urban TJ, Nicoletti P, Chalasani N, Serrano J, Stolz A, Daly A, et al. Minocycline hepatotoxicity: clinical characterization and identification of HLA-B*35:02 as a risk factor. J Hepatol. 2017;67(1):137–44.
Whritenour J, Ko M, Zong Q, Wang J, Tartaro K, Schneider P, et al. Development of a modified lymphocyte transformation test for diagnosing drug-induced liver injury associated with an adaptive immune response. J Immunotoxicol. 2017;14(1):31–8.
Russo MW, Steuerwald N, Norton HJ, Anderson WE, Foureau D, Chalasani N, et al. Profiles of miRNAs in serum in severe acute drug induced liver injury and their prognostic significance. Liver Int. 2017;37(5):757–64.
Bonkovsky HL, Kleiner DE, Gu J, Odin JA, Russo MW, Navarro VM, et al. Clinical presentations and outcomes of bile duct loss caused by drugs and herbals and dietary supplements. Hepatology. 2017;65(4):1267–77.
Navarro VJ, Khan I, Björnsson E, Seeff LB, Serrano J, Hoofnagle JH. Liver injury from herbal and dietary supplements. Hepatology. 2017;65(1):363–73.
Vega M, Verma M, Beswick D, Bey S, Hossack J, Merriman N, et al. The incidence of drug- and herbal and dietary supplement-induced liver injury: preliminary findings from gastroenterologist-based surveillance in the population of the state of Delaware. Drug Saf. 2017;40(9):783–7.
Suzuki A, Barnhart H, Gu J, Bonkovsky HL, Tillmann HL, Fontana RJ, et al. Associations of gender and a proxy of female menopausal status with histological features of drug-induced liver injury. Liver Int. 2017;37:1723–30.
Chalasani N, Reddy KR, Fontana RJ, Barnhart H, Gu J, Hayashi PH, et al. Idiosyncratic drug induced liver injury in african-americans is associated with greater morbidity and mortality compared to Caucasians. Am J Gastroenterol. 2017;112(9):1382–8.
Hayashi PH, Rockey DC, Fontana RJ, Tillmann HL, Kaplowitz N, Barnhart HX, et al. Death and liver transplantation within 2 years of onset of drug-induced liver injury. Hepatology. 2017;66(4):1275–85.
Dakhoul L, Ghabril M, Gu J, Navarro V, Chalasani N, Serrano J, United States Drug Induced Liver Injury Network. Heavy consumption of alcohol is not associated with worse outcomes in patients with idiosyncratic drug-induced liver injury compared to non-drinkers. Clin Gastroenterol Hepatol. 2018;16(5):722–9.
Ahmad J, Rossi S, Rodgers SK, Ghabril M, Fontana RJ, Stolz A, et al. Sclerosing cholangitis-like changes on magnetic resonance cholangiography in patients with drug induced liver injury. Clin Gastroenterol Hepatol. 2018. https://doi.org/10.1016/j.cgh.2018.06.035.
Fontana RJ, et al. The role of HLA-A*33:01 in patients with cholestatic hepatitis attributed to terbinafine. J Hepatol. 2018. https://doi.org/10.1016/j.jhep.2018.08.004.
Zoubek ME, González-Jimenez A, Medina-Cáliz I, Robles-Díaz M, Hernandez N, Romero-Gómez M, et al. High prevalence of ibuprofen drug-induced liver injury in Spanish and Latin-American Registries. Clin Gastroenterol Hepatol. 2018;16(2):292–4.
Medina-Caliz I, Garcia-Cortes M, Gonzalez-Jimenez A, Cabello MR, Robles-Diaz M, Sanabria-Cabrera J, Spanish DILI Registry, et al. Herbal and dietary supplement-induced liver injuries in the Spanish DILI Registry. Clin Gastroenterol Hepatol. 2018;16(9):1495–502.
Bjornsson E, Jiezhun G, Kleiner D, Chalasani N, Hayashi P, Hoofnagle J. Azathioprine and 6-mercaptopurine-induced liver injury: clinical features and outcomes. J Clin Gastroenterol. 2017;51(1):63–9.
Björnsson ES, Bergmann O, Jonasson JG, Grondal G, Gudbjornsson B, Olafsson S. Drug-induced autoimmune hepatitis: response to corticosteroids and lack of relapse after cessation of steroids. Clin Gastroenterol Hepatol. 2017;15(10):1635–6.
Yu YC, Mao YM, Chen CW, Chen JJ, Chen J, Cong WM, et al. CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hepatol Int. 2017;11(3):221–41.
Cho JH, Oh DS, Hong SH, Ko H, Lee NH, Park SE, et al. A nationwide study of the incidence rate of herb-induced liver injury in Korea. Arch Toxicol. 2017;91(12):4009–15.
Melchart D, Hager S, Albrecht S, Dai J, Weidenhammer W, Teschke R. Herbal traditional Chinese medicine and suspected liver injury: a prospective study. World J Hepatol. 2017;9(29):1141–57.
Dalal KK, Holdbrook T, Peikin SR. Ayurvedic drug induced liver injury. World J Hepatol. 2017;9(31):1205–9.
Shaikh SA, Tischer S, Choi EK, Fontana RJ. Good for the lung but bad for the liver? Garlic-induced hepatotoxicity following liver transplantation. J Clin Pharm Ther. 2017;42(5):646–8.
Xiao A, He HY, Chen Q, Ma SW. Drug-induced liver injury due to Lepidium meyenii (Maca) medicinal liquor. Chin Med J (Engl). 2017;130(24):3005–6.
Li H, Wang X, Liu Y, Pan D, Wang Y, Yang N, et al. Hepatoprotection and hepatotoxicity of Heshouwu, a Chinese medicinal herb: context of the paradoxical effect. Food Chem Toxicol. 2017;108(Pt B):407–18.
Tayabali K, Bolzon C, Foster P, Patel J, Kalim MO. Kratom: a dangerous player in the opioid crisis. J Community Hosp Intern Med Perspect. 2018;8(3):107–10.
Fluyau D, Revadigar N. Biochemical benefits, diagnosis and clinical risks evaluation of Kratom. Front Psychiatry. 2017;8:62.
Chang-Chien G, Odonkor C, Amorapanth P. Is kratom the new ‘legal high’ on the block? The case of an emerging opioid receptor agonist with substance abuse potential. Pain Physician. 2017;20(1):E195–8.
Kothadia J, Kaminski M, Samant H, Olivera-Martinez M. Hepatotoxicity associated with use of the weight loss supplement Garcinia cambogia: a case report and review of the literature. Case Rep Hepatol. 2018;2018:6483605.
Sharma A, Akagi E, Njie A, Goyal S, Arsene C, Krishnamoorthy G, et al. Acute hepatitis due to Garcinia cambogia extract, an herbal weight loss supplement. Case Rep Gastrointest Med. 2018;2018:6360543.
Corey R, Werner K, Singer A, Moss A, Smith M, Noelting J, et al. Acute liver failure associated with Garcinia cambogia use. Ann Heptaol. 2016;15(1):123–6.
Lunsford K, Bodzin A, Reino D, Wang HL, Busuttil RW. Dangerous dietary supplements: Garcinia cambogia-associated hepatic failure requiring transplantation. World J Gastroenterol. 2016;22(45):10071–6.
Cescioli G, Lombardi N, Bettiol A, Marconi E, Risaliti F, Bertoni M, et al. Acute liver injury following Garcinia cambogia weight-loss supplementation: case series and literature review. Intern Emerg Med. 2018;13(6):857–72.
Phillips CA, Paramaguru R, Joy AK, Antony KL, Augustine P. Clinical outcomes, histopathological patterns, and chemical analysis of Ayurveda and herbal medicine associated with severe liver injury—a single center experience from southern india. Indian J Gastroenterol. 2018;37(1):9–17.
Devarbhavi H. Ayurvedic and herbal medicine-induced liver injury: it is time to wake up and take notice. Indian J Gastroenterol. 2018;37(1):5–7.
Wang Y, Wang L, Saxena R, Wee A, Yang R, Tian Q, et al. Clinicopathological features of He Shou Wu-induced liver injury: this ancient anti-aging therapy is not liver-friendly. Liver Int. 2018. https://doi.org/10.1111/liv.13939.
Mazzanti G, Moro P, Raschi E, Da Cas R, Menniti-Ippolito F. Adverse reactions to dietary supplements containing red yeast rice: assessment of cases from the Italian surveillance system. Br J Clin Pharmacol. 2017;83:894–908.
Teschke R, Schulze J, Eickhoff A. Drug induced liver injury: can biomarkers assist RUCAM in causality assessment? Int J Mol Sci. 2017;18:803.
Robles-Díaz M, Medina-Caliz I, Stephens C, Andrade RJ, Lucena MI. Biomarkers in DILI: one more step forward. Front Pharmacol. 2016;7:267.
Lin H, Ewing LE, Koturbash I, Gurley BJ, Miousse IR. MicroRNAs as biomarkers for liver injury: current knowledge, challenges and future prospects. Food Chem Toxicol. 2017;110:229–39.
Church RJ, Watkins PB. The transformation in biomarker detection and management of drug-induced liver injury. Liver Int. 2017;37(11):1582–90.
Mosedale M, Watkins P. Drug-induced liver injury: advances in mechanistic understanding that will inform risk management. Clin Pharmacol Ther. 2017;101(4):469–80.
Kullak-Ublick GA, Andrade RJ, Merz M, End P, Benesic A, Gerbes AL, et al. Drug-induced liver injury: recent advances in diagnosis and risk assessment. Gut. 2017;66:1154–64.
Araújo AM, Carvalho M, Carvalho F, Bastos ML, Gueses de Pinho P. Metabolomic approaches in the discovery of potential urinary biomarkers of drug-induced liver injury (DILI). Crit Rev Toxicol. 2017;47(8):633–49.
Gonzalez-Jimenez A, McEuen K, Chen M, Suzuki A, Robles-Diaz M, Medina-Caliz I, et al. The influence of drug properties and host factors on delayed onset of symptoms in drug-induced liver injury. Liver Int. 2018. https://doi.org/10.1111/liv.13952.
Fang WC, Adler NR, Graudins LV, Goldblatt C, Goh MS, Roberts SK, et al. Drug-induced liver injury is frequently associated with severe cutaneous adverse drug reactions: experience from two Australian tertiary hospitals. Intern Med J. 2018;48(5):549–55.
McGill MR, Jaeschke H. Biomarkers of drug-induced liver injury: progress and utility in research, medicine and regulation. Expert Rev Mol Diagn. 2018;18(9):797–807.
Osanlou O, Pirmohamed M, Daly AK. Pharmacogenetics of adverse drug reactions. Adv Pharmacol. 2018;83:155–90.
Kaliyaperumal K, Grove JI, Delahay RM, Giffiths WJ, Duckworth A, Aithal GP. Pharmacogenomics of drug-induced liver injury (DILI): molecular biology to clinical applications. J Hepatol. 2018. https://doi.org/10.1016/j.jhep.2018.05.013.
Bessone F, Dirchwolf M, Rodil MA, Razori MV, Roma MG. Review article: drug-induced liver injury in the context of nonalcoholic fatty liver disease—a physiopathological and clinical integrated view. Aliment Pharmacol Ther. 2018;1:1. https://doi.org/10.1111/apt.14952.
Kowalec K, Wright GE, Drogemoller BI, Aminkeng F, Bhavsar AP, Kingwell E, et al. Common variation near IRF6 is associated with IFN-beta-induced liver injury in multiple sclerosis. Nat Genet. 2018;50(8):1081–5.
Marcinak JF, Munsaka MS, Watkins PB, Ohira T, Smith N. Liver safety of fasiglifam (TAK-875) in patients with type 2 diabetes: review of the global clinical trial experience. Drug Saf. 2018;41(6):625–40.
The Lancet. End of the road for daclizumab in multiple sclerosis. Lancet. 2018;391(10125):1000. https://doi.org/10.1016/s0140-6736(18)30565-8.
Buege MJ, Brown JE, Aitken SL. Solithromycin: a novel ketolide antibiotic. Am J Health Syst Pharm. 2017;74(12):875–87.
Roth F, Maiuri A, Ganey P. Idiosyncratic drug-induced liver injury: is drug-cytokine interaction the linchpin? J Pharmacol Exp Ther. 2017;360(2):461–70.
Jian J, Mathijs K, Timmermans L. Omics-based identification of the combined effects of idiosyncratic drugs and inflammatory cytokines on the development of drug-induced liver injury. Toxicol Appl Pharmacol. 2017;332:100–8.
Kato R, Uetrecht J. Supernatant from hepatocyte cultures with drugs that cause idiosynratic liver injury activates macrophage inflammasomes. Chem Res Toxicol. 2017;30(6):1327–32.
Hu J, Ramshesh V, McGill M, Jaeschke H, Lemasters JJ. Low dose acetaminophen induces reversible mitochondrial dysfunction associated with transient c-Jun N-terminal kinase activation in mouse liver. Toxicol Sci. 2016;150(1):204–15.
Ramachandran A, Jaeschke H. Acetaminophen toxicity novel insights into mechanisms and future perspectives. Gene Expr. 2018;18(1):19–30.
Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy. 2004;59(8):809–20.
Saito M, Yagi M, Uno K, Takanaka K. Comparative study of the usefulness of the drug-induced lymphocyte stimulation test and the leukocyte migration test in drug allergies. Biol Pharm Bull. 2008;31(2):299–304.
Benesic A, Rotter I, Dragoi D, Weber S, Buchholtz ML, Gerbes AL. Development and validation of a test to identify drugs that cause idiosyncratic drug-induced liver injury. Clin Gastroenterol Hepatol. 2018;16(9):1488–94.
Bessone F. Predicting fatalities in serious idiosyncratic drug-induced liver injury—a matter of choosing the best Hy’s law. Transl Gastroenterol Hepatol. 2017;2:112.
Bjornsson ES, Bjornsson HK. Mortality associated with drug-induced liver injury (DILI). Transl Gastroenterol Hepatol. 2017;2:114.
Chalasani NP, Hayashi PH, Bonkovsky HL, Navarro VJ, Lee WM, Fontana RJ, Practice Parameters Committee of the American College of Gastroenterology. ACG Clinical Guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol. 2014;109(7):950–66.
Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research, Food and Drug Administration. Guidance for industry. Drug-induced liver injury: premarketing clinical evaluation. Drug Saf. 2009. http://www.fda.gov/downloads/drugs/guidancescomplianceregulatoryinformation.guidances/ucm174090.pdf. Accessed 7 Feb 2018
Teschke R, Danan G. Drug induced liver injury with analysis of alternative causes as confounding variables. Br J Clin Pharmacol. 2018;84(7):1467–77.
Malnick S, Maor Y, Melzer E, Ziv-Sokolowskaia NN, Nueman MG. Severe hepatotoxicity linked to Denosumab. Eur Rev Med Pharmacol Sci. 2017;21(1 Suppl):78–85.
Namn Y, Scneider Y, Cui I, Jesudian A. Diphenhydramine as a cause of drug-induced liver injury. Case Reports Hepatol. 2017;2017:3864236.
Niijima K, Niijimia Y, Okada S. Drug-induced liver injury cause by ipragliflozin administration with causality established by a positive lymphocyte transformation test (LTT) and the RUCAM: a case report. Ann Hepatol. 2017;16(2):308–11.
Ito D, Shimizu S, Inoue K, Saito D, Yanagisawa M, Inukai K, et al. Comparison of ipragliflozin and pioglitazone effects on nonalcoholic fatty liver disease in patients with type 2 diabetes: a randomized, 24-week, open-label, active-controlled trial. Diabetes Care. 2017;40(10):1364–72.
Patel S, Mendler MH, Valasek MA, Tsunoda SM. Drug-induced liver injury associated with the use of everolimus in a liver transplant patient. Case Rep Transpl. 2018;2018:7410508.
Park DH, Yun GY, Eun HS, Joo JS, Kim JS, Kang SH, et al. Fimasartan-induced liver injury in a patient with no adverse reactions on other types of angiotensin II receptor blockers: a case report. Medicine (Baltimore). 2017;96(47):e8905.
FDA Drug Safety Communication: FDA warns about serious liver injury with Ocaliva (obeticholic acid) for rare chronic liver disease [Internet]. (2018). U.S. Food and Drug Administration. https://www.fda.gov/Drugs/DrugSafety/ucm576656.htm. Cited 12 Sept 2018.
Aschenbrenner DS. Excessive dosing of obeticholic acid may increase risk of liver damage. Am J Nurs. 2018;118(2):46.
Lugoboni F, Mirijello A, Morbioli L, Arzenton E, Leone R, Faccini M, et al. Does high-dose benzodiazepine abuse really produce liver toxicity? Results from a series of 201 benzodiazepine mono-abusers. Expert Opin Drug Saf. 2018;17(5):451–6.
Honda S, Sawada K, Hasebe T, Nakajima S, Fujiya M, Okumura T. Tegafur-uracil-induced rapid development of advanced hepatic fibrosis. World J Gastroenterol. 2017;23(31):5823–8.
Edwards B, Raisch D, Saraykar S, Sun M, Hammel J, Tran H, et al. Hepatotoxicity with vismodegib: an MD Anderson cancer center and research on adverse drug events and reports project. Drugs RD. 2017;17(1):211–8.
Sakumura M, Tajiri K, Miwa S, Nagata K, Kawai K, Miyazono T, et al. Hepatic sinusoidal obstruction syndrome induced by non-transplant chemotherapy for non-Hodgkin lymphoma. Intern Med. 2017;56(4):395–400.
Shah JM, Lin K, Etienne D, Reddy M, Liu Y. Imatinib-induced hepatitis in a patient treated for gastrointestinal stromal tumor: a rare adverse effect. Cureus. 2018;10(4):e2529.
McDonald GB, Freston JW, Boyer JL, DeLeve LD. Liver complications following treatment of hematologic malignancy with anti-cd22-calicheamicin (inotuzumab ozogamicin). Hepatology. 2018;1:1. https://doi.org/10.1002/hep.30222.
Tanaka R, Fujisawa Y, Sae I, Maruyama H, Ito S, Hasegawa N, et al. Severe hepatitis arising from ipilimumab administration, following melanoma treatment with nivolumab. Jpn J Clin Oncol. 2017;47(2):175–8.
Eigentler TK, Hassel JC, Verking C, Aberle J, Bachmann O, Grunwald V, et al. Diagnosis, monitoring and management of immune-related adverse drug reactions of anti-PD-1 antibody therapy. Cancer Treat Rev. 2016;45:7–18.
Gelsomino F, Vitale G, D’Errico A, Bertuzzi C, Andreone P, Ardizzoni A. Nivolumab-induced cholangitic liver disease: a novel form of serious liver injury. Ann Oncol. 2017;28(3):671–2.
Matsubara T, Nishida T, Higaki Y, Tomita R, Shimakoshi H, Shimoda A, Osugi N, Sugimoto A, Takahashi K, Nakamatsu D, Mukai K, Yamamoto M, Fukui K, Adachi S, Inada M. Nivolumab induces sustained liver injury in a patient with malignant melanoma. Intern Med. 2018;57(12):1789–92.
Abdel-Rahman O, ElHalawani H, Fouad M. Risk of elevated transaminases in cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Expert Opin Drug Saf. 2015;14:1507–18.
Zarrabi K, Wu S. Risk of liver toxicity with nivolumab immunotherapy in cancer patients. Oncology. 2018;94:259–73.
Zen Y, Yeh MM. Hepatotoxicity of immune checkpoint inhibitors: a histology study of seven cases in comparison with autoimmune hepatitis and idiosyncratic drug-induced liver injury. Mod Pathol. 2018;31:965–73.
Vigano L, De Rosa G, Toso C, Andres A, Ferrero A, Roth A, et al. Reversibility of chemotherapy-related liver injury. J Hepatol. 2017;67(1):84–91.
Wakiya T, Kudo D, Ishido K, Kimura N, Yakoshi Y, Toyoki Y, et al. Effect of age on the development of chemotherapy-associated liver injury in colorectal cancer liver metastasis. Mol Clin Oncol. 2017;7(2):200–4.
Zhanel GG, Hartel E, Adam H, Zelenitsky S, Zhanel MA, Golden A, et al. Solithromycin: a novel fluoroketolide for the treatment of community-acquired bacterial pneumonia. Drugs. 2016;76(18):1737–57.
Donald BJ, Surani S, Deol HS, Mbadugha UJ, Udeani G. Spotlight on solithromycin in the treatment of community-acquired bacterial pneumonia: design, development, and potential place in therapy. Drug Des Dev Ther. 2017;11:3559–66.
Meeting of the Antimicrobial Drugs Advisory Committee (AMDAC) [Internet]. FDA Briefing Document Solithromycin Oral Capsule and Injection; (2016). http://www.fda.gov. Cited 25 Sep 2018.
Dobbins R, Gholam P, Ertel S, Furey N, Baskaran GM, Goodman Z, Oldach D, Fernandes P. SAT-299—solithromycin treatment for 13 weeks improves histological parameters in nonalcoholic steatohepatitis: results of an ongoing pilot study. J. Hepatol. 2017;66(1):S586.
Wong A, Sivilotti M, Graudins A. Accuracy of the paracetamol-aminotransferase multiplication product to predict hepatotoxicity in modified-release paracetamol overdose. Clin Toxicol (Phila). 2017;55(5):346–51.
Sivilotti MLA, Green TJ, Langmann C, Yarema M, Juurlink D, Johnson D. Multiplying the serum aminotransferase by the acetaminophen concentration to predict toxicity following overdose. Clin Toxicol. 2010;48:793–9.
Chomchai S, Chomchai C. Predicting acute acetaminophen hepatotoxicity with acetaminophen-aminotransferase multiplication product and the Psi parameter. Clin Toxicol. 2014;52:506–11.
Heard K, Anderson V, Dart R. Serum acetaminophen protein adduct concentrations in pediatric emergency department patients. Hepatology. 2017;64(4):533–5.
Heard K, Anderson V, Lavonas E. Serum paracetamol-protein adducts in ambulatory subjects: relationship to recent reported paracetamol use. Biomarkers. 2018;23(3):288–92.
Heruth DP, Shortt K, Zhang N, Li DY, Zhang LQ, Ye SQ. Genetic association of single nucleotide polymorphisms with acetaminophen-induced hepatotoxicity. J Pharmacol Exp Ther. 2018. https://doi.org/10.1124/jpet.118.248583.
Roberts D, Lee W, Hinson J, Bai S, Swearingen CJ, Stravitz RT, et al. An immunoassay to rapidly measure acetaminophen protein adducts accurately identifies patients with acute liver injury or failure. Clin Gastroenterol Hepatol. 2017;15(4):555–62.
Dob S, Potschka H, Dob F, Mitzner S, Sauer M. Hepatotoxicity of antimycotics used for invasive fungal infections: in vitro results. Biomed Res Int. 2017;2017:9658018.
Pettit NN, Miceli MH, Rivera CG, Naraynanan PP, Perissinotti AJ, Hsu M, et al. Multicentre study of posaconazole delayed-release tablet serum level and association with hepatotoxicity and QTc prolongation. J Antimicrob Chemother. 2017;72(8):2355–8.
Gayam V, Khalid M, Dahal S, Garlapati P, Gill A. Hyperacute liver injury following intravenous fluconazole: a rare case of dose-independent hepatotoxicity. J Family Med Prim Care. 2018;7(2):451–4.
Watkins PB, Lewis JH, Kaplowitz N, Alpers DH, Blais JD, Smotzer DM, et al. Clinical pattern of tolvaptan-associated liver in- jury in subjects with autosomal dominant polycystic kidney disease: analysis of clinical trials database. Drug Saf. 2015;38:1103–13.
Oi A, Morishita K, Awogi T, Ozaki A, Umezato M, Fujita S, et al. Nonclinical safety profile of tolvaptan. Cardiovasc Drugs Ther. 2011;1:S91–9.
Mosedale M, Kim Y, Brock W, Roth SE, Wiltshire T, Eaddy JS, et al. Editor’s highlight: candidate risk factors and mechanisms for tolvaptan-induced liver injury are identified using a collaborative cross approach. Toxicol Sci. 2017;156(2):438–54.
Festing MFW. Inbred strains should replace outbred stocks in toxicology, safety testing, and drug development. Toxicol Pathol. 2010;38(5):681–90.
Harrill AH, DeSmet KD, Wolf KK, Bridges AS, Eaddy JS, Kurtz CL, et al. A mouse diversity panel approach reveals the potential for clinical kidney injury due to DB289 not predicted by classical rodent models. Toxicol Sci. 2012;130(2):416–26.
Mosedale M, Eaddy JS, Trask OJ, Holman NS, Wolf KK, LeCluyse E, et al. miR-122 release in exosomes precedes overt tolvaptan-induced necrosis in a primary human hepatocyte micropatterned coculture model. Toxicol Sci. 2018;161(1):149–58.
Woodhead JF, Watkins PB, Howell BA, Siler SQ, Shoda LK. The role of quantitative systems pharmacology modeling in the prediction and explanation of idiosyncratic drug-induced liver injury. Drug Metab Pharmacokinet. 2017;32(1):40–5.
Woodhead JF, Brock WJ, Roth SE, Shoaf SE, Brouwer KL, Church R, et al. Application of a mechanistic model to evaluate putative mechanisms of tolvaptan drug-induced liver injury and identify patient susceptibility factors. Toxicol Sci. 2017;155(1):61–74.
Barnhill M, Real M, Lewis J. Latest advances in diagnosing and predicting DILI: what was new in 2017. Expert Rev Gastroenterol Hepatol. 2018. https://doi.org/10.1080/17474124.2018.1512854.
Suzuki A, Andrade RJ, Bjornsson E, Lucena MI, Lee WM, Yuen NA, et al. Drugs associated with hepatotoxicity and their reporting frequency of liver adverse events in VigiBase: unified list based on international collaborative work. Drug Saf. 2010;33:503–22.
Bjornsson ES, Hoofnagle JH. Categorization of drugs implicated in causing liver injury: critical assessment based on published case reports. Hepatology. 2016;63:590–603.
Shirai Y, Oda S, Makino S. Establishment of a mouse model of enalapril-induced liver injury and investigation of the pathogenesis. Lab Investig. 2017;97(7):833–42.
Liakoni E, Ratz Bravo AE, Krahenbuhl S. Hepatotoxicity of new oral anticoagulants (NOACs). Drug Saf. 2015;38:711–20.
Glenn K, Chen P, Musleh M. A rare case of rivaroxaban causing delayed symptomatic hepatocellular injury and hyperbilirubinemia. Case Rep Gastrointest Med. 2017;2017:5678187.
Alonso A, MacLehose R, Chen L, Bengtson L, Chanberlain A, Norby F, et al. Prospective study of oral anticoagulants and risk of liver injury in atrial fibrillation patients. Heart. 2017;103(11):834–939.
Douros A, Azoulay L, Yin H, Suissa S, Renoux C. Non-vitamin K antagonist oral anticoagulants and risk of serious liver injury. JACC. 2018;71(10):1105–13.
Heidbuchel H, Verhamme P, Alings M, Antz M, Diener HC, Hacke W, et al. Updated European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist anticoagulants in patients with nonvalvular atrial fibrillation. Europace. 2015;17:1467–507.
Sarges P, Steinberg JM, Lewis JH. Drug-induced liver injury: highlights from a review of the 2015 literature. Drug Saf. 2016;2016:1–21.
Mishra P, Chen M. Direct-Acting antivirals for chronic hepatitis C: can drug properties signal potential for liver injury? Gastroenterol. 2017;152(6):1270–4.
Chen M, Borlak J, Tong W. High lipophilicity and high daily dose of oral medications are associated with significant risk for drug induced liver injury. Hepatology. 2013;58:388–96.
Segamwenge IL, Bernard MK. Acute liver failure among patients on efavirenz-based antiretroviral therapy. Case Rep Hepatol. 2018. https://doi.org/10.1155/2018/1270716.
Diab OA, Kamel J, Abd-Elhamid AA. Predictors of intravenous amiodarone induced liver injury. Egypt Heart J. 2017;69(1):45–54.
Grimaldi-Bensouda L, Matthias A, et al. Dronedarone, amiodarone and other antiarrhythmic drugs, and acute liver injuries: a case-referent study. Int J Cardiol. 2018;266:100–5.
Suvichapanich S, Fukunaga K, Zahroh H, Mushiroda T, Mahasirimongkol S, Toyo-oka L, et al. NAT2: ultra-slow acetylator and risk of anti-tuberculosis drug-induced liver injury: a genotype-based meta-analysis. Pharmacogenet Genom. 2018;28(7):167–76.
Zhang M, Wang S, Wilffert B, Tong R, van Soolingen D, van den Hof S, Alffenaar JW. The association between the NAT2 genetic polymorphisms and risk of DILI during anti-TB treatment: a systematic review and meta-analysis. Br J Clin Pharmacol. 2018. https://doi.org/10.1111/bcp.13722.
Nociti V, Biolato M, De Fino C, Bianco A, Losavio FA, Lucchini M, et al. Liver injury after pulsed methylprednisolone therapy in multiple sclerosis patients. Brain Behav. 2018;8(6):e00968. https://doi.org/10.1002/brb3.968.
Bresteau C, Prevot S, Perlemuter G, Voican C. Methylprednisolone-induced acute liver injury in a patient treated for multiple sclerosis relapse. BMJ Case Rep. 2018. https://doi.org/10.1136/bcr-2017-223670.
Dumortier J, Cottin J, Lavie C. Methylprednisolone liver toxicity: A new case and a French regional pharmacovigilance survey. Clin Res Hepatol Gastroenterol. 2017;41(4):497–501.
Billioti de Gage S, Collin C, Le-Tri T, Pariente A, Bégaud B, Verdoux H, Dray-Spira R, Zureik M. Antidepressants and hepatotoxicity: a cohort study among 5 million individuals registered in the French National Health Insurance Database. CNS Drugs. 2018;32(7):673–84.
Ferrajolo C, Scavone C, Donati M, Bortolami O, Stoppa G, Motola D, DILI-IT Study Group, et al. Antidepressant-induced acute liver injury: a case–control study in an Italian Inpatient Population. Drug Saf. 2017;41(1):95–102.
Kok B, Lester EL, Lee WM, Hanje AJ, Stravitz RT, Girgis S, United States Acute Liver Failure Study Group, et al. Acute liver failure from tumor necrosis factor-α antagonists: report of four cases and literature review. Dig Dis Sci. 2018;63(6):1654–66.
Barnhill M, Lewis JH. Are authors following the rules for causality assessment? Gastroenterology. 2018;154(6):S-1227 (abstract #2910244).
Wong MC, Huang JL, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol. 2018. https://doi.org/10.1038/s41575-018-0055.0.
Wang R, Qi X, Yoshida EM, Mendez-Sanchez N, Teschke R, Sun M, et al. Clinical characteristics and outcomes of traditional Chinese medicine-induced liver injury: a systematic review. Expert Rev Gastroenterol Hepatol. 2018;12(4):425–34.
Liu Z, He X, Wang L, Zhang Y, Hai Y, Gao R. Chinese herbal medicine hepatotoxicity: the evaluation and recognization based on large-scale evidence database. Curr Drug Metab. 2018. https://doi.org/10.2174/1389200219666180813144114.
Wang JB, Zhu Y, Bai ZF, Wang FS, Li XH, Xiao XH, et al. Guidelines for the diagnosis and management of herb-induced liver injury. Chin J Integr Med. 2018;24(9):696–706.
Jing J, Teschke R. Traditional Chinese medicine and herb-induced liver injury: comparison with drug-induced liver injury. J Clin Transl Hepatol. 2018;6(1):57–68.
Danan G, Teschke R. Review: RUCAM in drug and herb induced liver injury: the update. Int J Mol Sci. 2016;17(14):1–33.
Agarwal VK, McHutchinson JG, Hoofnagle JH. Important elements for the diagnosis of drug-induced liver injury. Clin Gastroenterol Hepatol. 2010;8(5):463–70.
Ganger DR, Rule J, Rakela J, Bass N, Reuben A, Stravitz RT, et al. Acute liver failure of indeterminate etiology: a comprehensive systematic approach by an expert committee to establish causality. Am J Gastroenterol. 2018. https://doi.org/10.1038/s41395-018-0160-2.
Scalfaro E, Streefkerk H, Merz M, Meier C, Lewis D. Preliminary results of a novel algorithmic method aiming to support initial causality assessment of routine pharmacovigilance case reports for medication-induced liver injury: the PV-RUCAM. Drug Saf. 2017;40(8):715–27.
Lauschke V. Dysregulation of miR-223 constitutes a promising biomarker that informs about clinical outcomes of acute liver failure. Clin Sci (Lond). 2017;131(15):2059–62.
Fang C, Li XP, Gong WJ, Wu NY, Tang J, Yin JY, et al. Age-related common miRNA polymorphism associated with severe toxicity in lung cancer patients treated with platinum-based chemotherapy. Clin Exp Pharmacol Physiol. 2017;44(Suppl 1):21–9.
Yang R, Yang F, Huang Z, Jin Y, Sheng Y, Ji L. Serum microRNA-122-3p, microRNA-194-5p and microRNA-5099 are potential toxicological biomarkers for the hepatotoxicity induced by Airpotato yam. Toxicol Lett. 2017;280:125–32.
Rissin D, Lopez-Longarela B, Pernagallo S. Poymerase-free measurement of microRNA-122 with single base specificity using single molecule arrays: detection of drug-induced liver injury. PLoS One. 2017;12(7):e0179669.
Vliegenthart A, Berends C, Potter C, Kersaudy-Kerhoas M, Dear JW. microRNA-122 can be measured in capillary blood which facilitates point-of-care testing for drug-induced liver injury. Br J Clin Pharmacol. 2017;83(9):2027–33.
Lee J, Ji SC, Kim B, Yi S, Shin KH, Cho JY, et al. Exploration of biomarkers for amoxicillin/clavulanate-induced liver injury: multi-omics approaches. Clin Transl Sci. 2017;10(3):163–71.
Cho T, Uetrecht J. How reactive metabolites induce an immune response that sometimes leads to an idiosyncratic drug reaction. Chem Res Toxicol. 2017;30(1):295–314.
Dakhoul L, Ghabril M, Chalasani N. Drug-induced chronic liver injury. J Hepatol. 2018;69(1):248–50.
Stieger B, Mahdi Z. Review: model systems for studying the role of canalicular efflux transporters in drug-induced cholestatic liver disease. J Pharm Sci. 2017;106(9):2295–301.
Ali I, Welch M, Lu Y, Swaan PW, Brouwer KL. Identification of novel MRP3 inhibitors based on computational models and validation using an in vitro membrane vesicle assay. Eur J Pharm Sci. 2017;103:52–9.
Ogese M, Faulkner L, Jenkins R, French NS, Copple IM, Antoine DJ, et al. Characterization of drug-specific signaling between primary human hepatocytes and immune cells. Toxicol Sci. 2017;158(1):76–89.
Goda K, Kobayashi A, Takahashi A. Evaluation of the potential risk of drugs to induce hepatotoxicity in human-relationships between hepatic steatosis observed in non-clinical toxicity study and hepatotoxicity in humans. Int J Mol Sci. 2017;18(4):810.
McEuen K, Borlak J, Tong W, Chen M. Associations of drug lipophilicity and extent of metabolism with drug-induced liver injury. Int J Mol Sci. 2017;18(7):1335.
Bilgic Y, Yilmaz C, Cagin YF, Atayan Y, Karadag N, Harputluoglu MM. Albendazole induced recurrent acute toxic hepatitis: a case report. Acta Gastroenterol Belg. 2017;80(2):309–11.
Bergland Ellingsen S, Nordmo E, Tore Lappegard K. Recurrence and severe worsening of hepatotoxicity after reintroduction of atorvastatin in combination with ezetimibe. Clin Med Insights Case Rep. 2017;10:1179547617731375.
Mukthinuthalapati PK, Fontana RJ, Vuppalanchi R, Chalasani N, Ghabril M. Celecoxib-induced liver injury: analysis of published case reports and cases reported to the Food and Drug Administration. J Clin Gastroenterol. 2017;52(2):114–22.
Muñoz MA, Kulick CG, Kortepeter CM, Levin RL, Avigan MI. Liver injury associated with dimethyl fumarate in multiple sclerosis patients. Mult Scler. 2017;23(14):1947–9.
Lévesque AM, Yang CD, Elchebly C, Doré M. Hepatotoxicity associated with iopamidol. Am J Health Syst Pharm. 2017;74(10):636–40.
Ahmad J, Odin JA, Hayashi PH, Chalasani N, Fontana R, Barnhart H, et al. Identification and characterization of fenofibrate-induced liver injury. Dig Dis Sci. 2017;62(12):3596–604.
Almeida J, Sola-Valls N, Pose E. Liver injury and glatiramer acetate, an uncommon association: case report and literature review. Ther Adv Neurol Disord. 2017;10(11):367–72.
Sako A, Bae S, Gushima T, Motoshita J, Bekki S, Abiru S, et al. Drug-induced liver injury associated with mosapride citrate: a report of two cases. Int Med. 2017;56:41–5.
Choudhary N, Bodh V, Chaudhari S. Norethisterone related drug induced liver injury: a series of 3 cases. J Clin Exp Hepatol. 2017;7(3):266–8.
Verma N, Kumar P, Mitra S, Taneja S, Dhooria S, Das A, et al. Drug idiosyncrasy due to pirfenidone presenting as acute liver failure: case report and mini-review of the literature. Hepatol Commun. 2017;2(2):142–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
There was no need for ethical approval.
Conflict of interest
Mark Real, Michele Barnhill, Cory Higley and Jessica Rosenberg have no conflicts of interest that are directly relevant to the content of this study. James Lewis has received fees for participation in review activities such as data monitoring boards, etc., for Otsuka, Allergan, GSK, Zydus, Shire, BMS but otherwise has no other conflicts of interest.
Funding
No sources of funding were used to assist in the preparation of this study.
Rights and permissions
About this article
Cite this article
Real, M., Barnhill, M.S., Higley, C. et al. Drug-Induced Liver Injury: Highlights of the Recent Literature. Drug Saf 42, 365–387 (2019). https://doi.org/10.1007/s40264-018-0743-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-018-0743-2