Abstract
Introduction
Intrauterine devices are implantable contraceptives of which some brands steadily release levonorgestrel over an extended time period. Exposure to a levonorgestrel-releasing intrauterine device has been associated with depression and, more recently, a connection to anxiety, panic attacks, sleep problems and restlessness has been suggested. This study uses data from the THIN database of UK general practice to investigate these suggestions.
Methods
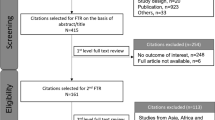
A cohort study was performed to compare the incidence of psychiatric adverse events between groups of women who were new users of levonorgestrel-releasing and non-hormonal intrauterine devices. Hazard ratios for the first occurrence of psychiatric symptoms or prescriptions of disease-specific treatments were calculated on an intention-to-treat basis using a proportional hazards model.
Results
Significant associations were found between levonorgestrel exposure and records of anxiety (hazard ratio = 1.18; 95% confidence interval 1.08–1.29) and sleep problems (hazard ratio = 1.22; 95% confidence interval 1.08–1.38) in women without a prior record of these events. No significant associations were found for panic attacks or restlessness. Clear baseline differences in clinical characteristics and age between the groups were present. These were included in the model as potential confounding factors.
Conclusion
Statistically significant associations of levonorgestrel exposure with anxiety and sleep problems were observed. Substantive differences in baseline characteristics of the treated groups make robust conclusions difficult but the results strongly suggest that additional studies are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This cohort study compares levonorgestrel-releasing intrauterine devices (IUDs) with non-medicated IUDs using UK general practice data in the THIN database |
Exposure to a levonorgestrel-releasing IUD is known to increase the risk of depression |
This study suggests that anxiety and sleeplessness may be associated with levonorgestrel-releasing IUDs |
1 Introduction
Intrauterine devices (IUDs) are implantable, long-acting reversible contraceptive methods. Intrauterine devices can be non-hormonal, such as the copper IUDs, or include a progestogen, such as levonorgestrel (LNG), when they may also be referred to as intrauterine systems. Levonorgestrel-intrauterine devices (LNG-IUDs) are indicated in contraception, including the treatment of menorrhagia in women who choose intrauterine contraception.
Administered locally, LNG-IUDs have been associated with systemic adverse effects. A European multicentre randomised clinical trial including 1821 women comparing LNG-IUD with a non-LNG-containing IUD showed that the removal rate after 5 years was significantly higher in the LNG-IUD group because of depression, with an increased number of cases of acne (five-fold), headaches (seven-fold) and weight gain reported [1].
A literature review of published evidence investigating the high discontinuation rate of up to 60% in women with LNG-IUDs found that, in women using LNG, by any route, for either contraception, heavy menstrual bleeding or oestrogen replacement therapy, the most commonly reported reasons for discontinuation were unscheduled bleeding (15–71%), progestogenic adverse effects (including depression and mood changes) and pelvic-abdominal pain [2]. A questionnaire sent to 212 women using LNG-IUD reported a continuation rate of 85%; 70, 59, 56, 50 and 50% at 6 months, 1, 2, 3, 4, and 5 years, respectively. The most common reasons for early removal were unscheduled bleeding, progestogenic adverse effects and abdominal pain [3].
In a randomised trial investigating the effect of a hysterectomy or levonorgestrel-releasing intrauterine system on sexual functioning in women with menorrhagia, only 48.7% of women randomised to LNG-IUDs still had their IUD after 5 years of follow-up, 42.7% underwent a hysterectomy and in 8.5% of women it was removed prematurely. A LNG-IUD was associated with worse sexual satisfaction and increased sexual problems among women with menorrhagia [4].
In addition to formal studies, case reports of mood disturbances, not restricted to depression, associated with levonorgestrel are quite common on Internet fora [5, 6]. The current UK product information for Mirena® lists both depression and nervousness as common side effects. There is sparse literature explicitly investigating other psychiatric effects and nervous system disorders affecting women using Mirena® or comparable IUDs. However, concerns with respect to potential psychiatric adverse effects have been voiced by the German Medical Association committee for drug-related matters since 2009. Online guidance [7] notes that ‘In the German spontaneous reporting system (joint database of BfArM and AkdÄ, as of January 15, 2009), 2129 suspected cases of ADRs to Mirena® are recorded, most reports are of uterine perforation (n = 455) or migration of the IUD (n = 170). There are also reports of psychiatric ADRs, such as: Depression and depressive moods (n = 52), panic attacks and anxiety (n = 35), sleep disorders (n = 14) and restlessness (n = 15)’.
This study was performed to investigate whether levonorgestrel delivered by an IUD increases the risk of anxiety, panic attacks, sleep disorders and restlessness and, if so, to quantify the size of these effects. These events could be of concern to patients and might affect the benefit-risk profile of the LNG-IUD.
2 Methods
2.1 Study Setting
The study used data from UK general practice electronic medical records collected in the THIN database between 1 January, 2000 and 31 December, 2016. At January 2017, the data contained records on 13.9 million patients considered to meet acceptable standards for research of whom 6.0 million were still under observation. The data for each patient form a record of visits and interactions with their general practitioner. In particular, all prescriptions issued by the general practitioner and clinical events discussed are routinely recorded using formal coding dictionaries together with the date of the consultation. This allows the temporal relationships between drug exposures and clinical events to be studied. Data are representative of the UK population in terms of age, deprivation and geographical distribution [8, 9], and have been used for analysis of contraceptive usage [10]. Diagnoses, symptoms and other relevant health information are recorded using the Read Code clinical classification system, a hierarchical classification system [11]. The study protocol was submitted to and approved by the THIN Scientific Review Committee.
2.2 Study Design
For each outcome of interest, a new user cohort study was carried out assessing the time to first manifestation of the disorder following insertion of an LNG-IUD. A comparison was made with a control group of new users of non-LNG IUDs. The primary study analysis followed the intention-to-treat (ITT) principle. Separate analyses were carried out in women with and without relevant psychiatric conditions recorded in their electronic medical record in the year prior to IUD prescription.
Study treatments were identified from seven codes for LNG-IUDs and 31 for non-hormonal IUDs in the THIN product dictionary. These codes were checked against trade names to ensure the product groups were correctly differentiated.
Cohort entry was defined by the date of an incident prescription for LNG-IUDs and non-LNG-releasing IUDs in women with at least 1 year of follow-up after registration in general practices with an acceptable mortality rate date (meaning their data had met quality standards recommended by the data provider). Women were excluded if codes were found for previous IUD usage or replacement indicating that this was not a new treatment episode. Cohort exit was defined as the earliest occurrence of the following: end of study follow-up (31 December, 2016), death, deregistration from the practice, date of an outcome event or 5 years from prescription of the IUD.
2.3 Validation Against Known Effect
A preliminary analysis was performed to determine the appropriateness both of the dataset and of the analytical methods to detect psychiatric adverse effects of this product. Depression is a labelled adverse drug reaction associated with levonorgestrel and thus we used the same methods in the same cohort of patients to analyse time to first records of depression or prescriptions of antidepressants.
2.4 Intention to Treat vs. As Treated
A secondary analysis was undertaken to evaluate the changes in treatment effects when the ITT (prescribe) model was replaced by one that censored women from the study at the earliest indication of possible treatment cessation. Thus, women only contributed study data when a high probability of current treatment exposure could be inferred. The cohort exit was the earliest occurrence of: end of study follow-up, death, deregistration from the practice, date of an outcome event, record of IUD removal or replacement without insertion of a new identical IUD, prescription of other methods of contraception or 5 years. This analysis is complementary to the ITT analysis, in that it assumes the minimum exposure time for each woman where the ITT assumes a likely maximum.
2.5 Outcome Variables
An outcome event was defined as the first Read Code or prescribed treatment for panic attacks, anxiety, sleep disorders or restlessness after prescription of the study IUD. Read Codes used in the study are available in the Electronic Supplementary Material. Anxiety was also identified through new prescriptions of anxiolytics (ATC N05B) and sleep problems through new prescriptions of hypnotics and sedatives (ATC N05C).
Depression was included as an outcome in the analysis as positive control. Depression was defined as new prescriptions of antidepressants (ATC N06A) in addition to Read Codes for depression.
2.6 Potential Confounding Variables
Potential confounders included in the model were age at IUD prescription, childbirth in the year prior to prescription of the study product, history of menorrhagia, other menstrual problems, anaemia, menopausal symptoms, endometriosis, dysmenorrhea and premenstrual symptoms. The clinical events were all evaluated on the basis of Read Codes recorded in the year prior to study entry.
Precise identification of childbirth is challenging in the THIN database but newborns registered into THIN practices can often be linked to mothers using a family number, the practice identifier and Read Codes related to childbirth. This process was used to identify women with probable live births in the year prior to the study.
2.7 Data Analysis
For each outcome, crude hazard ratios (HRs) were calculated between the treatment and control groups. A Cox proportional hazards regression model was fitted estimating (1) age-adjusted and (2) fully adjusted HRs with 95% confidence intervals (CIs). Full adjustment made use of all baseline variables. No selection of confounders was made unless the model failed to converge. Apart from the analysis of restlessness, which had too few cases, all analyses were stratified by practice to increase the chance of balance in unknown demographic factors. The proportional hazards assumption was assessed using the Kolmogorov-type test implemented in the SAS PHREG procedure. Survival curves were estimated at specific values of the explanatory baseline variables [12].
The main comparison was LNG IUDs against non-LNG IUDs over the entire exposure period of 5 years. An exposure period of up to 5 years from the start of treatment was defined because of the duration of action of LNG-containing IUDs.
3 Results
3.1 Description of Study Population
The number of women with an incident prescription for LNG IUDs included in the cohort was 10,872 and the number with non-LNG IUDs was 6871. The mean study follow-up time for women in the ITT analysis was 4.2 years in the LNG IUD group and 4.4 years in the control group. In the ‘as-treated’ analysis, the follow-up was 3.3 and 3.1 years, respectively.
3.2 Baseline Characteristics
The mean age of women at first prescription was 36.9 years (standard deviation = 7.7) for LNG-IUDs and 33.1 years (standard deviation = 7.1) for non-medicated IUDs. Table 1 shows the demographic and clinical characteristics of the women in the study at the time of IUD prescription. All variables in Table 1 are assessed from 1 year of data prior to study entry. There are appreciable differences between the groups of women prescribed the LNG and non-LNG IUDs, notably in gynaecological conditions.
3.3 Validation Against Known Effect: Association with Depression
A positive association with depression and LNG-IUD exposure was observed in people without a prior history of depression (HR 1.17, 1.08–1.26). The large effects of age alone suggested that it should be included as a separate analysis against which to judge the adjustment for clinical variables. Several other factors were strongly statistically associated with the outcome but, as is clear from the comparison of age- and fully adjusted results, had little effect on the estimated association with LNG (Table 2).
3.4 Main Study Analysis
The observed overall 3-year event rates in this study for women without prior psychiatric conditions were 22% for depression, 13.5% for anxiety, 1.4% for panic attacks, 6.8% for sleep problems and 0.3% for restlessness. In all analyses, results in bold are statistically significant with p < 0.05.
The adjusted HRs in Table 3 suggest a similar association between the use of an LNG-IUD and anxiety and sleep problems to that estimated for depression in women without recent prior disease. Table 4 shows no fully adjusted significant effects in women with prior disease although the point estimates of HRs for anxiety and sleep problems are not very different from those in Table 3. No associations could be detected with panic attacks or restlessness. Figure 1 illustrates the evolution over time of the anxiety outcome by estimating the survival curves for a 35-year-old woman exposed and unexposed to LNG and without other risk factors.Footnote 1
Tests did not show significant departure from the proportional hazard assumption for the main treatment comparison or for age. Of the other variables, menopausal symptoms did show some departure. This is not unexpected as, in many cases, this will not be a long-lasting condition. However, removal of this variable from the models did not qualitatively change the treatment comparisons.
3.5 Effects of Adjusting Variables
Adding the full set of covariates to the age-adjusted model for the statistically significant associations resulted in a regression of the HR towards 1 but this was not large: 1.22 to 1.18 for anxiety and 1.24 to 1.22 for sleep problems. Removal of individual covariates from the model revealed that this change was mostly accounted for by a history of menorrhagia, which was a statistically significant predictor of increased hazard in all the analyses for women without prior disease.
3.6 Secondary Analysis
The secondary analysis that measured the association based on current exposure and censored women from the study when IUD removal codes were recorded or when other forms of contraception were prescribed, estimated similar HRs and CIs to the ITT analysis. In particular, no qualitative changes in statistical significance were found. This is despite considerably smaller numbers of outcomes resulting from the shorter follow-up period, for instance, the number of anxiety outcomes in LNG-exposed women free of prior disease fell from 1868 to 1438. Table 5 shows the results, including those for depression, in women without prior disease.
4 Discussion
The results of this study show a known positive association between prescription of an LNG-containing IUD and depression and an unestablished association with anxiety (HR increased by 18%) and sleep problems (HR increased by 22%) in women without these conditions prior to use of the IUD. Effects of a similar estimated size were seen in women with prior symptoms but these effects were not statistically significant.
The meaning of such effects requires some consideration. In those without prior symptoms in the preceding year, the analysis outcome is new psychiatric disease. By contrast, in a woman with recent prior symptoms, further symptoms would be expected. An association with quicker reoccurrence thus might be seen as either reflecting an exacerbation or a delay in resolution of the condition. It is not obvious that such effects should have the same HR as findings of new disease. Nevertheless, from a public health perspective, it is important to know about treatment effects in all women who might be exposed and hence we present both analyses. The interpretation of the non-significant analysis in women with prior disease is difficult. On the one hand, the population is smaller and the power to show associations is reduced. On the other hand, despite the differing interpretations discussed above, it would be incautious to consider the results for women with and without prior disease as entirely independent phenomena. If the association in women without prior disease is deemed likely to be causal, then that should have some bearing in interpreting the results in women with prior symptoms.
The question remains of whether the significant associations are causal. A fact tending to support this idea is that depression is a recognised psychiatric adverse effect of systemic exposure to LNG. It is therefore plausible that other adverse events such as anxiety and sleep problems, which are clinically associated effects [13], may occur through a common causal mechanism. Furthermore, our primary ITT analysis and the secondary analysis restricted to times of documented LNG exposure provided consistent results. On the other side of the argument, some characteristics of women prescribed LNG IUDs differed from those of women prescribed non-LNG IUDs. Adjusting out such differences relies on the assumptions that all such characteristics are reflected in the variables entered into the model and that those variables are measured with accuracy. With respect to this point, it is worth remarking that only events sufficiently concerning to merit discussion with a doctor will be present in the THIN data.
The question of the accuracy with which clinical details are recorded is also relevant to outcome measures. Psychiatric disease is poorly recorded in the THIN database as evidenced by the fact that many patients receive treatment for such disease but no specific clinical code is assigned. For this reason, where possible, we also used new prescribing of relevant medicines as a marker of psychiatric events. For anxiety, we only used anxiolytics although the first choice of treatment may also be an antidepressant. The similarity of results for depression and anxiety suggests that this is unlikely to have affected the estimated treatment effect. However, the poor recording of disease may have reduced the power for some outcomes.
The main limitation of the study is probably the difficulty of dealing with the imbalance in baseline factors between the groups. A major difference results from the indicated use in menorrhagia, which is specific to LNG IUDs. We tried to minimise this difficulty by not only using identifiable potential confounders but by stratifying on practice, a measure that might match some unknown confounders related to geographical or societal factors. It should be noted, however, that in adjusting for menorrhagia we may also risk obscuring a treatment effect, as menorrhagia is often a factor in opting for an LNG-IUD over a non-LNG IUD. It is worth noting that non-medicated IUDs also have specific indications for use as emergency contraception. A reviewer of the study noted that this usage may occur subsequent to rape or unwanted pregnancy, which may increase the likelihood of subsequent psychiatric events. This also would bias the results towards the null.
With regard to depression as an established effect of LNG exposure, it is worth noting that even this is debated. In a recent narrative review [14], the authors found the evidence from studies with validated measures of depression unconvincing. This judgement conflicts with regulatory assessment despite including a new large observational study [15] that supports the hypothesis. Hence, it is likely to provoke debate.
Information from the UK Office of National Statistics [16] shows that about 0.55 and 0.41% of women of reproductive age consulted sexual and reproductive health services about LNG IUDs and non-medicated LNGs in 2015. This suggests that we would detect at least 67 and 43% of women prescribed these devices via general practitioner prescribing. Although there is an imbalance in these detection rates, it is not clear how the differential ascertainment could result in a difference in psychiatric events.
We chose to conduct an ITT analysis as our primary method because attempting to model the true exposure of IUD products requires assumptions about the time scale over which an effect of LNG might persist even after removal and, perhaps more relevantly, a delay in reporting and recording of psychiatric effects cannot be excluded. Such models should be accompanied by evidence that risk windows have not been selected based on knowledge of the data and there is thus some advantage in using a model that simply does not require risk windows to be defined. These arguments are strong for this specific analysis because the relevant risk windows are particularly unclear and any model retains the possibility that treatment cessation might result from concerns about early psychiatric symptoms, which might only be included in patient notes if they eventually required treatment. Moreover, even if data were available to allow such effects to be realistically modelled, codes for the removal of IUDs appear to be used only sporadically in the THIN database. Whilst the entire dataset records prescriptions for around 280,000 IUDs, the code for removal is only recorded about 40,000 times.
A limitation of this study from a clinical viewpoint is that it only considers exposure to LNG via an IUD. Inclusion of a comparison with long-term oral use was considered but rejected because of limited power in the THIN dataset. Additional studies in independent observational datasets would help to resolve the more general question regarding systemic exposure to LNG by any route and provide clarification regarding the effects of exposure from IUDs.
The preliminary analysis of depression revealed that the dataset and methods were capable of detecting known associations with psychiatric adverse effects. Such information is probably more useful in interpreting a lack of association in other outcomes than a positive association because it implies that if a positive association with similar amounts of evidence had existed it would have been detected. However, it is clear that the much lower frequencies of outcomes for restlessness and panic attacks than for depression mean that power was lacking to investigate these outcomes.
5 Conclusions
Associations consistent with a causal effect of levonorgestrel exposure on anxiety and sleep problems were observed. Substantive differences in baseline characteristics of the treated groups make robust conclusions difficult but the results strongly suggest that additional studies are warranted.
Notes
Note that the HR for LNG exposure illustrated in the figure is as estimated for all women but that absolute levels of anxiety as shown apply only to the specified values of the covariates.
References
Andersson K, Odlind V, Rybo G. Levonorgestrel-releasing and copper-releasing (Nova-T) IUDs during five years of use: a randomized clinical trial. Contraception. 1994;49:56–72.
Ayman A, Ewies A. Levonorgestrel-releasing intrauterine system: the discontinuing story. Gynecol Endocrinol. 2009;25(10):668–73.
Daud S, Ewies A. Levonorgestrel-releasing intrauterine system: why do some women dislike it? Gynecol Endocrinol. 2008;24(12):686–90.
Halmesmäki K, Hurskainen R, Teperi J, et al. The effect of hysterectomy or levonorgestrel-releasing intrauterine system on sexual functioning in women with menorrhagia: a 5 year randomized controlled trial. BJOG. 2007;114:563–8.
Patient Info. Anxiety and Mirena® (IUD). https://patient.info/forums/discuss/anxiety-and-mirena-iud–587345. Accessed 4 Apr 2018.
FBDC. Mirena® ruined my life: a public service announcement. https://fueledbydietcoke.com/2012/12/10/mirena-iud-ruined-my-life-a-public-service-announcement/. Accessed 4 Apr 2018.
AkdÄ. Psychiatrische Erkrankungen als unerwünschte Arzneimittelwirkung von Mirena® (Aus der UAW-Datenbank). https://www.akdae.de/Arzneimittelsicherheit/Bekanntgaben/Archiv/2009/20090501.html. Accessed 4 Apr 2018.
Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12:171–7.
Maguire A, Blak B, Thompson M. The importance of defining periods of complete mortality reporting for research using automated data from primary care. Pharmacoepidemiol Drug Saf. 2009;18:76–83.
Soriano LC, Wallander MA, Andersson SW, Requena G, García-Rodríguez LA. Study of long-acting reversible contraceptive use in a UK primary care database: validation of methodology. Eur J Contracept Reprod Health Care. 2013;19(1):22–8.
Booth N. What are the Read Codes? Health Libr Rev. 1994;11(3):177–82.
Cox DR, Oakes D. Analysis of survival data. London: Chapman and Hall; 1984.
Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329–36.
Worly B, Gur T, Schaffir J. The relationship between progestin hormonal contraception and depression: a systematic review. Contraception. 2018. https://doi.org/10.1016/j.contraception.2018.01.010 (Epub ahead of print).
Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of hormonal contraception with depression. JAMA Psychiatry. 2016;73:1154–62.
Office of National Statistics. Sexual and reproductive health services, England 2015–16. London: Office of National Statistics; 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was conducted using European Medicines Agency resources and no additional funding source.
Conflict of interest
Jim Slattery, Daniel Morales, Luis Pinheiro and Xavier Kurz have no direct or indirect financial or personal interest in the products included in this study or in competitor products.
Data availability
This study uses de-identified data from UK general practice collected in the THIN database.
Ethics approval
The study protocol was approved by the THIN Scientific Review Committee.
Disclaimer
The views expressed in this article are those of the authors and should not be understood or quoted as being made on behalf of or reflecting the position of the European Medicines Agency.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Slattery, J., Morales, D., Pinheiro, L. et al. Cohort Study of Psychiatric Adverse Events Following Exposure to Levonorgestrel-Containing Intrauterine Devices in UK General Practice. Drug Saf 41, 951–958 (2018). https://doi.org/10.1007/s40264-018-0683-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-018-0683-x