Abstract
Introduction
The levonorgestrel oral emergency contraceptive is well tolerated and effective, however its use is still limited, mainly due to safety concerns.
Objective
This systematic review and meta-analysis aimed to summarize current evidence regarding the adverse events, and their prevalence, reported during the use of oral levonorgestrel emergency contraceptives.
Methods
Four electronic databases and the US FDA Adverse Event Reporting System (FAERS) Public Dashboard were searched. Studies that reported or investigated safety outcomes or adverse reactions during the use of levonorgestrel as an emergency oral contraceptive were included. Data on study design, demographics of levonorgestrel and the control cohort, and reported adverse effects were extracted.
Results
A total of 47 articles were included in this systematic review, from which it was shown that most of the adverse reactions were common and not serious. Uncommon adverse reactions identified included anorexia, ectopic pregnancy, exanthema, chloasma, miscarriage, and weight gain. Multiple serious adverse events, including convulsion, ectopic pregnancy, febrile neutropenia, stroke, abdominal hernia, anaphylaxis, cancer, ovarian cyst rupture, serious infections, and suicidal ideation, were reported. In addition, the prevalence of adverse events after a levonorgestrel 0.75 mg two-dose regimen and a levonorgestrel 1.5 mg single-dose regimen were not statistically different (p > 0.05).
Conclusions
The most common adverse effects of levonorgestrel were not serious. This systematic review shows that data regarding the adverse reactions of repeated use of levonorgestrel are scarce. Studies on the multiple uses of levonorgestrel emergency contraception are still required to ensure its safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most levonorgestrel emergency oral contraceptive adverse reactions were common and not serious. |
The prevalence of adverse events of a levonorgestrel 0.75 mg two-dose regimen and a levonorgestrel 1.5 mg single-dose regimen was not statistically different. |
The use of levonorgestrel emergency oral contraceptives should be promoted in populations that are in need but who also have safety concerns. |
1 Introduction
Levonorgestrel has been extensively used as emergency contraception and is available as intrauterine devices (IUDs) and oral contraceptives [1]. Oral levonorgestrel is most commonly administered as a 0.75 mg tablet within 72 h postcoital, while the second tablet, which also contains 0.75 mg of levonorgestrel, is administered 12 h after the first dose [2]. Other variations in the dosing regimen include taking the first tablet within 120 h postcoital, taking the second tablet 24 h after the first tablet, or taking two 0.75 mg tablets within 72 h postcoital [2]. Despite the fact that the levonorgestrel oral emergency contraceptive is well tolerated and effective as postcoital oral contraception [3], its use as an emergency contraceptive is still limited. One reason for this is that the efficacy of the levonorgestrel emergency oral contraceptive is less than the combined oral contraceptive. While the failure rate of the combined oral contraceptive ranges from 0.75 to 1.67% [4], the failure rate of the levonorgestrel emergency oral contraceptive ranges from 0.6 to 3.1%, which is higher than ulipristal acetate (failure rate 0.9–1.2%) and the copper IUD (failure rate: < 0.1%) [5]. In addition, there is evidence that repeated unprotected intercourse in the same menstrual cycle was associated with emergency contraceptive failure [6].
While efficacy is a concern for limiting use of the levonorgestrel oral contraceptive, safety is more concerning. Patients [7,8,9] and pharmacists [10] may feel that levonorgestrel oral emergency contraceptives are not well tolerated. In some women, minor common adverse effects such as nausea or headache can prevent them from using the product [11]. Moreover, special concerns that levonorgestrel oral emergency contraceptives can cause serious adverse effects, including abortion, infertility, blood clots, and even cancer, are common among women [7, 12]. Scientific evidence also shows conflicting evidence regarding the safety of oral levonorgestrel. For example, several observational studies showed that the use of oral levonorgestrel may cause ectopic pregnancy [13,14,15], but multiple systematic reviews suggested otherwise [3, 16, 17]. Another example is venous thromboembolism. Several studies suggested that levonorgestrel was associated with venous thromboembolism [18,19,20,21]; however, a review demonstrated that the effect of progestin on venous thromboembolism was inconclusive and the association between venous thromboembolism and levonorgestrel found in several observational studies might have been influenced by the effect of confounders, e.g. new use, older age, obesity, family history of venous thromboembolism, or prolonged immobilization [22]. In addition, several studies suggested that knowledge of oral emergency contraceptives was inadequate among healthcare professionals [23,24,25,26] and policymakers [27]. Therefore, this systematic review and meta-analysis aimed to summarize current evidence regarding adverse events and their prevalence reported during the use of oral levonorgestrel emergency contraceptives.
2 Methods
2.1 Data Sources and Search strategy
A systematic literature search was performed of the MEDLINE, Scopus, Science Direct, and CINAHL Complete databases from conception to October 2019, using the terms (‘postcoital oral contraceptive” [e.g. morning-after pills] OR ‘levonorgestrel’) AND (‘case report’ OR ‘adverse reaction’ [e.g. adverse drug reaction]) without applying language restrictions. Synonyms of search terms suggested by the search engines were used. The full search strategies are provided in Electronic Supplementary Material 1. References for related review articles, letters, and protocols were searched for potential pertinent studies.
Data from a spontaneous reporting system, the US FDA Adverse Event Reporting System (FAERS) Public Dashboard, were also retrieved to further capture the adverse events of levonorgestrel. The search term ‘levonorgestrel’ was used and an additional filter, ‘reason for use’ as oral contraception, was applied. The adverse event data of levonorgestrel in the FAERS Public Dashboard, available from 1971 to 2019, were retrieved. It should be noted the FDA does not require that a causal relationship between a drug and event be proven. Moreover, incidence, risk assessment, and risk ranking cannot be provided based on FAERS data.
2.1.1 Inclusion and Exclusion Criteria
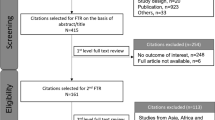
Studies were included in this meta-analysis if they were (1) human studies; (2) studies that explicitly indicate levonorgestrel as the exposure; and (3) studies that explicitly indicate safety outcomes or adverse reactions during the use of levonorgestrel. Studies were excluded if they were (1) not research articles; (2) studies whose participants used non-oral drug delivery systems for levonorgestrel; (3) studies that used levonorgestrel for purposes that were not emergency contraception (e.g. as progestin-only pills); (4) studies that used levonorgestrel as a combined oral contraceptive; or (5) conducted in males. In the case of case reports, case series, and studies that reported data that could not be used to calculate pooled data, these were included for the systematic review but not the meta-analysis. Figure 1 shows the preferred reporting items for systematic reviews and meta-analysis (PRISMA) diagram of the systematic literature review process.
2.2 Data Extraction
Articles retrieved from searching were stored in a citation manager (EndNote X7, Thomson Reuters, New York, NY, USA). After the removal of redundant articles, titles and abstracts of the remaining articles were reviewed by the first author by searching for specific words for the exclusion (e.g. to exclude intrauterine levonorgestrel, words such as intrauterine, devices, and IUD were searched). The remaining abstracts were reviewed. For non-English-language articles, English abstracts and Result sections in full texts were used to determine if further translation was necessary. For the abstraction process, the abstraction form was designed by the first author and reviewed by the coauthor. Data on study design, location, patient demographics, dosage regimens of levonorgestrel, timing after coitus, types of adverse reactions and their corresponding prevalence, and potential biases and confounders in every study were independently extracted by the first and second authors. Any disagreement was resolved by consensus. For the reporting system, the severity and duration of the adverse reactions were reported according to the definition of the frequency of adverse drug reactions developed by the Council for International Organizations of Medical Sciences [28]. Serious adverse reactions were “any untoward medical occurrence that at any dose results in death; is life-threatening; requires inpatient hospitalization or prolongation of existing hospitalization, or results in persistent or significant disability or incapacity”. Very common, common (or frequent), uncommon (or infrequent), rare, and very rare adverse reactions occur at a frequency higher than 1/10; less than 1/10 to higher than 1/100; less than 1/100 to higher than 1/1000; less than 1/1000 to higher than 1/10,000; and less than 1/10,000, respectively.
2.3 Risk of Bias
The risk of bias was determined using different tools according to the type of included studies. Clinical trials, observational studies, and cross-sectional studies were evaluated using the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials (CCRAB-RCT) [29], Newcastle–Ottawa Quality Assessment Scale (NOS) [30], and a modified Newcastle–Ottawa Quality Assessment Scale for cross-sectional studies [31], respectively. These tools were well-validated and recommended for use in systematic reviews and meta-analyses [32]. Case reports and case series were assessed using a tool modified from Pierson’s guide for evaluating the validity and educational value of a case report [33], Bradford Hills criteria [34], and Newcastle–Ottawa scale [30], which was proposed by Murad et al. [35]. Thresholds for converting CCARB-RCT and NOS results to the Agency for Healthcare Research and Quality (AHRQ) standard of ‘good’, ‘fair’, and ‘poor’ quality designations have been described by Likis et al. [36]. For the tool proposed by Murad et al., the questions with positive answers (e.g. yes or clear evidence, or no alternative explanation) were converted to 1. The total scores of 1–3, 4–5, and 6–8 were then converted to ‘good’, ‘fair’, and ‘poor’, respectively.
2.4 Statistical Methods
Only studies reporting the prevalence of adverse reactions were included in this meta-analysis. The binary random-effects model using the DerSimonian–Laird method was created using OpenMetaAnalyst for Windows 8 [37]. The I2 statistic was used to assess the heterogeneity of the underlying population. An I2 of < 25% was negligible heterogeneity, whereas I2 values > 75% were highly heterogeneous [38]. Stratification by levonorgestrel dose was planned prior to the analysis. The statistical significance of the data was considered at an α level of 0.05. Since the 95% confidence intervals (CIs) were aligned to detect the statistical difference in each data point, the exact p-values could not be reported.
3 Results
3.1 Study Characteristics
The systematic literature search retrieved 7314 non-redundant articles. According to the inclusion and exclusion criteria, 47 articles were included for the systematic review. There were 15 case reports or case series, 15 observational studies, and 17 clinical studies (Table 1). The quality of the included articles varied (a summary of the study quality is reported in Table 1). Of the 47 articles, 30, excluding case reports, were included in the meta-analysis (Table 2). Twenty-three studies had < 1000 participants (median 330 participants [range 25–4631]). The 30 articles were conducted in America (Brazil, USA, Peru), Europe (Italy, Norway, Poland, Spain, Sweden, UK), Asia (China, India, Iran, Japan, Thailand), Africa (Nigeria, Uganda), and Australia. The mean age median in the included studies was 27 years (range 13–48 years). Seventeen studies were conducted using a two-dose regimen of levonorgestrel 0.75 mg tablets [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55], with a median time between doses of 12 h (range 8–12 h). Eleven studies were conducted using a single-dose regimen of two tablets of levonorgestrel 0.75 mg [44, 53, 56,57,58,59,60,61,62,63,64]. Four studies did not report the dosing regimen used in their studies [65,66,67,68]. For the studies that reported the dosing regimen, participants used levonorgestrel within 3–72 h after unprotected sex (range 72 h). The median exposure frequency to levonorgestrel throughout the study was a single dose (range 1–13 times). The median study duration was 6 weeks (range 0.4–65.2 weeks). We inferred that the studies included in this meta-analysis represented a global population that used the clinically relevant levonorgestrel dosing regimen for emergency contraception. The duration of the included studies was sufficient to capture short-term uncommon adverse reactions. In addition, it was also possible that this meta-analysis might have captured very rare adverse reactions since the total number of patients in this meta-analysis was higher than 20,000.
3.2 Safety of Levonorgestrel Emergency Oral Contraceptives in Users
From the systematic review, adverse reactions that were found could be classified into gynecological adverse reactions, neurological adverse reactions, gastrointestinal adverse reactions, pregnancy and neonatal complications, and miscellaneous adverse reactions. Most adverse reactions were common and not serious. Uncommon adverse reactions identified included anorexia [58], ectopic pregnancy [68], exanthema [58], chloasma [64], miscarriage [68], and weight gain [64], while serious adverse reactions identified included convulsion, ectopic pregnancy, febrile neutropenia, and stroke [68]. In addition, three case reports regarding the adverse reaction of levonorgestrel were identified during the systematic search. The first reported a 23-year-old woman experiencing a stroke within 24 h after using levonorgestrel 1.5 mg [69]. Second, a case of venous thrombosis confirmed by a venous Doppler ultrasound and magnetic resonance venography was reported in a 22-year-old woman who used levonorgestrel 72 h prior to the occurrence of venous thrombosis [70]. The other case series presented a case of a patient in her 20 s who took a single tablet of levonorgestrel emergency contraception and had autoimmune progesterone dermatitis confirmed by skin prick and intradermal skin testing to progesterone [71].
Adverse reactions included in the meta-analysis were very common and common adverse reactions. Very common adverse reactions during the use of levonorgestrel emergency contraception were gynecological adverse reactions, including alteration of menstrual flow (46.8%; 95% CI 38.5–55.1%; n = 1), bleeding (31.0%; 95% CI 29.3–32.7%; n = 2, I2 = 0.0%), hypomenorrhea (26.2%; 95% CI 21.9–30.6%; n = 2, I2 = 0.0%), intermenstruation spotting (23.5%; 95% CI 7.8–39.2%; n = 5, I2 = 98.5%), and early menstruation (18.5%; 95% CI 5.1–32.0%; n = 2, I2 = 88.0%). The detailed summary of the pooled frequency of adverse reactions is shown in Table 2. In brief, the most commonly reported gynecological safety outcomes with a sufficient number of publications for the stratification analysis were breast pain (8.3%; 95% CI 5.8–10.7%; n = 16, I2 = 98.0%) and late menstruation (6.5%; 95% CI 4.7–8.4%; n = 7, I2 = 85.4%). Neurological outcomes included headache (12.4%; 95% CI 9.8–14.9%; n = 24, I2 = 98.6%) and dizziness (10.8%; 95% CI 8.7–12.9%; n = 21%, I2 = 96.3%). Gastrointestinal outcomes included nausea (15.0%; 95% CI 11.9–18.1%; n = 25, I2 = 97.5%), vomiting (8.5%; 95% CI − 4.7 to 21.7%; n = 20, I2 = 99.9%), lower abdominal pain (11.4%; 95% CI 8.8–14.0%; n = 17, I2 = 98.9%), and diarrhea (4.4%; 95% CI 2.4–6.4%; n = 7, I2 = 97.5%), while miscellaneous outcomes included fatigue (14.0%; 95% CI 10.3–17.8%; n = 19, I2 = 99.1). After analysis by stratifying the data by the dose of levonorgestrel, the prevalence of these aforementioned outcomes in users receiving a levonorgestrel 0.75 mg two-dose regimen and users receiving a levonorgestrel 1.5 mg single-dose regimen were not statistically different (p > 0.05) [Table 3].
3.3 Levonorgestrel Emergency Oral Contraceptives and Pregnancy Outcomes
This systematic review found two studies that reported pregnancy outcomes after failure of the levonorgestrel contraceptive. De Santis et al. found that the rate of preterm delivery and congenital anomalies (e.g. gastroesophageal reflux and monolateral nasolacrimal duct obstruction) in levonorgestrel users and non-users was not significantly different [65]. In addition, Zhang et al. found that levonorgestrel had no effect on the physical and mental development of children born after failure of the contraceptive [67]. Levonorgestrel had no adverse effects on the feeding or behavior of breastfeeding infants [66]. Moreover, 11 case reports documented ectopic pregnancy after the use of levonorgestrel emergency oral contraceptives [72,73,74,75,76,77,78,79,80,81,82,83]. In every case report, ectopic pregnancy occurred after the use of levonorgestrel. Most of the studies did not report concomitant drug use in patients, except for the work of Cabar et al., which reported no concomitant drug use [73], and Tan et al., which reported that an IUD was inserted concomitantly with the use of oral levonorgestrel [82]. Only two studies reported on the previous abortion status of patients [79, 81], and four studies reported the status of the previous infection in the reproductive system [79,80,81, 83].
The pooled pregnancy rate after the use of levonorgestrel contraception from this meta-analysis was 1.7% (95% CI 1.3–2.1%; n = 26, I2 = 79.4%). The rate of pregnancy was not statistically different between the 0.75 mg two-dose regimen (1.5%, 95% CI 1.0–2.0%; n = 16, I2 = 73.0%) and the 1.50 mg single-dose regimen (1.9%, 95% CI 1.1–2.7%; n = 9, I2 = 83.3%). The prevalence of miscarriage, ectopic pregnancy, preterm delivery, congenital anomalies, and neonatal complications were not significantly different from zero (p > 0.05) [Table 3].
3.4 Descriptive Data from the US FDA Adverse Events Reporting System (FAERS) Database
As of 1 February 2020, 247 cases that reported adverse events during the use of levonorgestrel oral emergency contraception were retrieved from the FAERS database. Of these reports, 51 cases reported levonorgestrel use with other concurrent active ingredients or medication, and 16 cases reported problems with contraceptive devices, and hence were further excluded. From the remaining 180 cases, there were 66 serious adverse events, including one death from a pulmonary embolism and one unilateral blindness from retinal vein thrombosis, and 114 non-serious adverse events. An illustration of these cases is shown in Table 3. Ectopic pregnancy was the only serious adverse event that was both reported in the FAERS database and found during the systematic review. In other words, convulsion, febrile neutropenia, and stroke, which were found during the systematic review, were not found in the FAERS database. Other serious adverse events reported in the database included abdominal hernia, anaphylactic reaction, cancer ovarian, cyst rupture, embolism (retinal vein thromboembolism resulting in unilateral blindness, and pulmonary embolism resulting in death), serious infections, and suicidal ideation (Table 3).
4 Discussion
Despite the fact that levonorgestrel is effective and well tolerated as an emergency oral contraceptive, myths about its safety discourage the use of levonorgestrel in patients. The situation is complicated by the political and religious perspective of using oral contraceptives [84, 85]. This study is the first to summarize the evidence regarding the prevalence of adverse reactions related to levonorgestrel oral contraceptives. We aimed to emphasize the safety of the levonorgestrel method of contraception. The results from this meta-analysis showed that the most common, and common, adverse effects of levonorgestrel were not serious. The prescribing information of Plan B One-Step deposited in the US FDA database demonstrates that the most common adverse reactions (≥ 10%) of levonorgestrel emergency oral contraceptives in clinical trials included heavier menstrual bleeding (31%), nausea (14%), lower abdominal pain (13%), fatigue (13%), headache (10%), and dizziness (10%) [86]. This meta-analysis showed that the rate of nausea (15%), lower abdominal pain (11.4%), fatigue (14%), headache (12.4%), and dizziness (10.8%) approximated to the rate reported in the prescribing information; however, the meta-analysis was not able to show the rate of bleeding because of variation in the terminology that was used in each included article.
In this systematic review, multiple serious adverse events were found, including convulsion, ectopic pregnancy, febrile neutropenia, stroke, abdominal hernia, anaphylactic reaction, cancer, ovarian cyst rupture, serious infections, and suicidal ideation. The biological plausibility of each adverse event is discussed. Progesterone has antiseizure effects with an undefined mechanism of action [87]; however, it is possible the levonorgestrel induces seizure because the withdrawal of progesterone results in convulsion [88, 89]. For ectopic pregnancy, several observational studies support that the use of levonorgestrel is associated with it [13,14,15, 90]. A possible mechanism for levonorgestrel-induced ectopic pregnancy may be the reduction in ciliary beat frequency [91]. Next, a meta-analysis published in 2009 supports that progestogen-only contraceptives are not associated with the risk of stroke [92]. In addition, several studies confirmed that the risk of venous thrombosis in levonorgestrel users is lower than other progestogens [93,94,95,96]. However, some studies suggest an association between levonorgestrel and stroke [97, 98]. Together with the fact that levonorgestrel still involves the coagulation cascade, e.g. factors II, VII, X, and fibrinogen [99, 100], coagulation-relevant adverse reactions such as embolism and stroke are biologically plausible.
Regarding the risk of cancer, plenty of studies investigated the association between levonorgestrel and breast cancer. This is biologically plausible because in vitro studies show that progestogens play important roles in the proliferation of breast cancer [101,102,103]; however, such an association still requires investigation since observational studies in humans found conflicting results on the association between levonorgestrel and breast cancer [104, 105]. In this study, the incidence of lung and cervical cancer was identified. Although studies on the mechanism of levonorgestrel are not available, the study by Soini et al. shows a decrease in the risk of lung cancer in levonorgestrel users [104]. In addition, the study by Averbach et al. associates the risk of cervical cancer with levonorgestrel IUDs [106]; however, this association stems from the use of IUDs since the devices can disrupt the cervical cytology [107]. Together with several in vivo studies indicating that progestin has anticervical cancer effects [108,109,110], the positive association between cervical cancer and oral levonorgestrel is very unlikely.
This systematic review also found cases of infections during the use of levonorgestrel. The use of emergency contraception raises concerns about the increase in the rate of sexually transmitted disease (STD), but several studies have shown that the use of emergency contraceptive pills is not associated with the risk of STDs [111, 112]. However, evidence shows that progesterone-based compounds reduce the numbers of CD8 + T cells and lower secretion of proinflammatory cytokines [113, 114]. The effect of the compounds may alleviate or aggravate the infections, depending on the type of pathogens; therefore, there is a possibility that the use of levonorgestrel is associated with increased susceptibility in infections other than STDs.
Another incidence type identified as a result of this systematic review was psychiatric events. The use of progestins is associated with anxiety [115], depression [115,116,117], psychiatric disorders [118], and suicidal attempts [119]. Although the exact mechanism is unknown, it is possible that progesterone may cause such adverse effects because progesterone receptors are expressed wildly in the brain, including in the hippocampus and frontal cortex [120], i.e. the parts responsible for memory, emotion, cognition, and behavior [121, 122]. The possible mechanisms that explain the association between the use of levonorgestrel and abdominal hernia, febrile neutropenia, and ovarian cyst rupture are currently unavailable.
There were some limitations to this meta-analysis. First, the included studies were conducted in different countries around the globe and the methodology of the studies was varied. As a result, pooled statistics from the meta-analysis demonstrated high heterogeneity, which might have complicated the interpretation of the results. However, there was no attempt to categorize the study according to study location, design or quality because the number of publications per adverse reaction was small. The diversity in the dosing regimen, dosing schedule, and study design could be the reasons for heterogeneity. Second, this systematic review and meta-analysis included only studies that investigated the adverse reactions of levonorgestrel emergency contraceptives that are used orally. The rationale for the inclusion criteria was that there are studies showing that delivery systems such as IUDs [123] or transdermal delivery systems [124] are related to ectopic pregnancy and contact dermatitis, respectively. In addition, adverse reactions reported by studies using levonorgestrel as progestin-only pills can be long-term toxicities that are not related to the nature of the short-term sporadic use of levonorgestrel emergency contraceptives; however, because of this rationale, we decided to exclude multiple studies that may have included daily use of levonorgestrel [15, 125,126,127], or studies that included combined oral contraceptives that associated levonorgestrel with several adverse reactions e.g. cardiovascular death [128], depression [117], gallbladder disease [129], and venous thromboembolism [18, 21].
Next, most of the included studies were designed to study the contraceptive efficacy of levonorgestrel. Safety outcomes were mostly not the primary outcome; therefore, statistical analysis in the included studies might have had less power to detect the statistical difference among levonorgestrel users and non-users. This was overcome by pooling the data from each study and meta-analyzing the adverse reactions regardless of the differences in the comparators. In addition, the association between adverse effects and levonorgestrel reported in observational studies that were used in this meta-analysis does not equate to the causal relationship between levonorgestrel and the adverse effects.
Last, the results from the meta-analysis of the pregnancy rates was biased by the search criteria. Several studies recommended other contraception as back-up methods [44, 47, 53, 54, 59, 63]. Data from some studies could not be included in the meta-analysis because the studies were designed to capture the failure rate of contraception [65]. This was anticipated since the primary outcome of this systematic review was adverse reactions, not the efficacy of the oral contraceptives. Hence, the pregnancy rate from this meta-analysis must be interpreted with caution.
This study provides extensive safety data on levonorgestrel emergency oral contraception. For research perspectives, multiple signals for uncommon or serious adverse reactions, e.g. chloasma, convulsion, ectopic pregnancy, exanthema, febrile neutropenia, miscarriage, stroke, and venous thrombosis, were revealed from the literature search. This can be used as an hypothesis for further observational studies or systematic reviews and meta-analyses to prove whether the incidence was associated with the use of levonorgestrel. In fact, several observational studies have been conducted to find the association between ectopic pregnancy and levonorgestrel [13,14,15]. In addition, this systematic review shows that data on the adverse reactions of repeated use of levonorgestrel are scarce. Studies on the multiple uses of levonorgestrel emergency contraception are still required to ensure the safety of levonorgestrel emergency contraception.
The results of this systematic review and meta-analysis have several clinical meanings. First, the prevalence of the serious adverse reactions of levonorgestrel emergency contraception was not common and not statistically significant. Common adverse reactions were not serious and included menstruation disturbances, headache, dizziness, nausea, vomiting, abdominal pain, diarrhea, and fatigue. Therefore, the use of levonorgestrel emergency oral contraceptives should be promoted in populations that are in need but who also have safety concerns. The prevalence of adverse reactions in the levonorgestrel 0.75 mg two-dose regimen group and the levonorgestrel 1.5 mg single-dose regimen group were not statistically different. This finding reveals the possibility of flexible dosing schedules of levonorgestrel. However, the clinical implications of this study are confounded by the limitations based on the quality of the included studies. To improve the quality of the literature regarding adverse reactions from levonorgestrel, reporting guidelines should be compiled to enable the scientific community to clearly evaluate the study. The use of medical dictionary terminology for reporting adverse events during studies will greatly improve the feasibility of pooling data into a meta-analysis. Additional large observational studies with a low risk of selection bias, and postmarketing surveillance designed to detect the adverse effects of levonorgestrel, specifically used as emergency oral contraceptives, are needed to ascertain the safety of levonorgestrel used as an emergency oral contraceptive.
5 Conclusions
This systematic review and meta-analysis found that most of the adverse reactions of oral levonorgestrel for emergency contraception were common and not serious. Serious adverse reactions identified included convulsion, ectopic pregnancy, febrile neutropenia, and stroke. Ectopic pregnancy was the only serious adverse event identified from both systematic reviews and FAERS reports. The use of a 0.75 mg two-dose regimen and a 1.50 mg single-dose regimen showed no difference in the prevalence of adverse effects and the rate of pregnancy. To ascertain the safety of levonorgestrel used as an emergency oral contraceptive, both in the short- and long-term, additional large observational studies with a low risk of selection bias, and postmarketing surveillance designed to detect the adverse effects of levonorgestrel specifically used as an emergency oral contraceptive, are needed.
References
Black KI, Hussainy SY. Emergency contraception: oral and intrauterine options. Aust Fam Physician. 2017;46(10):722–6.
Hansen LB, Saseen JJ, Teal SB. Levonorgestrel-only dosing strategies for emergency contraception. Pharmacotherapy. 2007;27(2):278–84.
Shohel M, Rahman MM, Zaman A, Uddin MM, Al-Amin MM, Reza HM. A systematic review of effectiveness and safety of different regimens of levonorgestrel oral tablets for emergency contraception. BMC Womens Health. 2014;14:54.
Dinger JC, Cronin M, Mohner S, Schellschmidt I, Minh TD, Westhoff C. Oral contraceptive effectiveness according to body mass index, weight, age, and other factors. Am J Obstet Gynecol. 2009;201(3):263.e1–9.
Cleland K, Raymond EG, Westley E, Trussell J. Emergency contraception review: evidence-based recommendations for clinicians. Clin Obstet Gynecol. 2014;57(4):741–50.
Upadhya KK. Emergency contraception. Pediatrics. 2019;144(6):3149.
Doci F, Thaci J, Foster AM. Emergency contraception in Albania: a multimethods qualitative study of awareness, knowledge, attitudes and practices. Contraception. 2018;98(2):110–4.
Kongnyuy EJ, Ngassa P, Fomulu N, Wiysonge CS, Kouam L, Doh AS. A survey of knowledge, attitudes and practice of emergency contraception among university students in Cameroon. BMC Emerg Med. 2007;7:7.
Kgosiemang B, Blitz J. Emergency contraceptive knowledge, attitudes and practices among female students at the University of Botswana: a descriptive survey. Afr J Primary Health Care Family Med. 2018;10(1):e1–6.
Said A, Ganso M, Freudewald L, Schulz M. Trends in dispensing oral emergency contraceptives and safety issues: a survey of German community pharmacists. Int J Clin Pharm. 2019;41(6):1499–506.
Free C, Lee RM, Ogden J. Young women’s accounts of factors influencing their use and non-use of emergency contraception: in-depth interview study. BMJ. 2002;325(7377):1393.
Westley E, Glasier A. Emergency contraception: dispelling the myths and misperceptions. Bull WHO. 2010;88(4):243–4.
Zhang J, Li C, Zhao WH, Xi X, Cao SJ, Ping H, et al. Association between levonorgestrel emergency contraception and the risk of ectopic pregnancy: a multicenter case-control study. Sci Rep. 2015;5:8487.
Assouni Mindjah YA, Essiben F, Foumane P, Dohbit JS, Mboudou ET. Risk factors for ectopic pregnancy in a population of Cameroonian women: a case-control study. PLoS One. 2018;13(12):e0207699.
Kurian A, Kaushik K, Subeesh V, Maheswari E, Kunnavil R. Safety profile of levonorgestrel: a disproportionality analysis of food and drug administration adverse event reporting system (FAERS) database. J Reprod Infertil. 2018;19(3):152–6.
Jatlaoui TC, Riley H, Curtis KM. Safety data for levonorgestrel, ulipristal acetate and Yuzpe regimens for emergency contraception. Contraception. 2016;93(2):93–112.
Cleland K, Raymond E, Trussell J, Cheng L, Zhu H. Ectopic pregnancy and emergency contraceptive pills: a systematic review. Obstet Gynecol. 2010;115(6):1263–6.
van Hylckama Vlieg A, Helmerhorst FM, Vandenbroucke JP, Doggen CJM, Rosendaal FR. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case–control study. BMJ. 2009;339:b2921.
Farmer RDT, Lawrenson RA. Oral contraceptives and venous thromboembolic disease: the findings from database studies in the United Kingdom and Germany. Am J Obstet Gynecol. 1998;179(3):s78–86.
Wilks JF. Hormonal birth control and pregnancy: a comparative analysis of thromboembolic risk. Ann Pharmacother. 2003;37(6):912–6.
Lidegaard O, Nielsen LH, Skovlund CW, Skjeldestad FE, Lokkegaard E. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: danish cohort study, 2001–9. BMJ. 2011;343:d6423.
Combined hormonal contraception and the risk of venous thromboembolism: a guideline. Fertil Steril. 2017;107(1):43-51.
Najafi-Sharjabad F, Hajivandi A, Rayani M. Knowledge, attitude, and practice about emergency contraception among health staff in Bushehr state, south of Iran. Global J Health Sci. 2013;6(1):52–60.
Byamugisha JK, Mirembe FM, Faxelid E, Gemzell-Danielsson K. Knowledge, attitudes and prescribing pattern of emergency contraceptives by health care workers in Kampala, Uganda. Acta Obstet Gynecol Scand. 2007;86(9):1111–6.
Harrison A. Knowledge and attitude towards emergency contraception among medical doctors in Delta State. Afr J Med Health Sci. 2014;13(1):39–46.
Chung-Park M. Emergency contraception knowledge, attitudes, practices, and barriers among providers at a military treatment facility. Mil Med. 2008;173(3):305–12.
Sychareun V, Phongsavan K, Hansana V, Phengsavanh A. Policy maker and provider knowledge and attitudes regarding the provision of emergency contraceptive pills within Lao PDR. BMC Health Serv Res. 2010;10(1):212.
Reactions Reporting Adverse Drug. Definitions of terms and criteria for their use. Geneva: World Health Organization; 1999.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014 [cited 25 Nov 2019]. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? a systematic review. BMC Public Health. 2013;13(1):154.
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10.
Pierson DJ. How to read a case report (or teaching case of the month). Respir Care. 2009;54(10):1372–8.
Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300.
Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid-Based Med. 2018;23(2):60–3.
Likis FE, Andrews JC, Collins MR, Lewis RM, Seroogy JJ, Starr SA, et al. AHRQ comparative effectiveness reviews. nitrous oxide for the management of labor pain. Rockville: Agency for Healthcare Research and Quality; 2012.
Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009;9(1):80.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Bhattacharjee SK, Romeo J, Kononova ES, Pretnar-Darovec A, Saraya L, Shi YE, et al. Postcoital contraception with levonorgestrel during the peri-ovulatory phase of the menstrual cycle. Task force on post-ovulatory methods for fertility regulation. Contraception. 1987;36(3):275–86.
He CH, Shi YE, Xu JQ, Van Look PF. A multicenter clinical study on two types of levonorgestrel tablets administered for postcoital contraception. Int J Gynaecol Obstet. 1991;36(1):43–8.
Ho PC, Kwan MS. A prospective randomized comparison of levonorgestrel with the Yuzpe regimen in post-coital contraception. Hum Reprod. 1993;8(3):389–92.
Lerkiatbundit S, Reanmongkol W. Use of 0.75 mg Levonorgestrel for postcoital contraception in Thailand. J Clin Pharm Ther. 2000;25(3):185–90.
Efficacy and side effects of immediate postcoital levonorgestrel used repeatedly for contraception. United Nations Development Programme/United Nations Population Fund/World Health Organization/World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Task Force on Post-Ovulatory Methods of Fertility Regulation. Contraception. 2000;61(5):303-8.
von Hertzen H, Piaggio G, Ding J, Chen J, Song S, Bartfai G, et al. Low dose mifepristone and two regimens of levonorgestrel for emergency contraception: a WHO multicentre randomised trial. Lancet. 2002;360(9348):1803–10.
Hamoda H, Ashok PW, Stalder C, Flett GM, Kennedy E, Templeton A. A randomized trial of mifepristone (10 mg) and levonorgestrel for emergency contraception. Obstet Gynecol. 2004;104(6):1307–13.
Harper CC, Rocca CH, Darney PD, von Hertzen H, Raine TR. Tolerability of levonorgestrel emergency contraception in adolescents. Am J Obstet Gynecol. 2004;191(4):1158–63.
Ngai SW, Fan S, Li S, Cheng L, Ding J, Jing X, et al. A randomized trial to compare 24 h versus 12 h double dose regimen of levonorgestrel for emergency contraception. Hum Reprod. 2005;20(1):307–11.
Creinin MD, Schlaff W, Archer DF, Wan L, Frezieres R, Thomas M, et al. Progesterone receptor modulator for emergency contraception: a randomized controlled trial. Obstet Gynecol. 2006;108(5):1089–97.
Raymond EG, Goldberg A, Trussell J, Hays M, Roach E, Taylor D. Bleeding patterns after use of levonorgestrel emergency contraceptive pills. Contraception. 2006;73(4):376–81.
Tirelli A, Cagnacci A, Volpe A. Levonorgestrel administration in emergency contraception: bleeding pattern and pituitary-ovarian function. Contraception. 2008;77(5):328–32.
Farajkhoda T, Khoshbin A, Enjezab B, Bokaei M, Karimi Zarchi M. Assessment of two emergency contraceptive regimens in Iran: levonorgestrel versus the Yuzpe. Niger J Clin Pract. 2009;12(4):450–2.
Hoseini FS, Eslami M, Abbasi M, Noroozi Fashkhami F, Besharati S. A randomized, controlled trial of levonorgestrel vs. the yuzpe regimen as emergency contraception method among Iranian women. Iran J Public Health. 2013;42(10):1158–66.
Dada OA, Godfrey EM, Piaggio G, von Hertzen H. A randomized, double-blind, noninferiority study to compare two regimens of levonorgestrel for emergency contraception in Nigeria. Contraception. 2010;82(4):373–8.
Lech MM, Ostrowska L, Swiatek E. Emergency contraception in a country with restricted access to contraceptives and termination of pregnancy, a prospective follow-up study. Acta Obstet Gynecol Scand. 2013;92(10):1183–7.
Taylor DJ, Lendvay A, Halpern V, Bahamondes LG, Fine PM, Ginde SY, et al. A single-arm study to evaluate the efficacy, safety and acceptability of pericoital oral contraception with levonorgestrel. Contraception. 2014;89(3):215–21.
Arowojolu AO, Okewole IA. Vaginal bleeding following the use of a single dose of 1.5 mg levonorgestrel (LNG) for emergency contraception. West Afr J Med. 2004;23(3):191–3.
Byamugisha JK, Mirembe FM, Faxelid E, Tumwesigye NM, Gemzell-Danielsson K. A randomized clinical trial of two emergency contraceptive pill regimens in a Ugandan population. Acta Obstet Gynecol Scand. 2010;89(5):670–6.
Chen QJ, Xiang WP, Zhang DK, Wang RP, Luo YF, Kang JZ, et al. Efficacy and safety of a levonorgestrel enteric-coated tablet as an over-the-counter drug for emergency contraception: a Phase IV clinical trial. Hum Reprod. 2011;26(9):2316–21.
Festin MP, Bahamondes L, Nguyen TM, Habib N, Thamkhantho M, Singh K, et al. A prospective, open-label, single arm, multicentre study to evaluate efficacy, safety and acceptability of pericoital oral contraception using levonorgestrel 1.5 mg. Hum Reprod. 2016;31(3):530–40.
Glasier AF, Cameron ST, Fine PM, Logan SJ, Casale W, Van Horn J, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. Lancet. 2010;375(9714):555–62.
Mittal S, Sehgal R, Jindal VI, Sikka P, Kandpal S, Maiti L, et al. Single dose levonorgestrel and two regimens of centchroman for emergency contraception. J Turk Ger Gynecol Assoc. 2008;9:134–8.
Raine TR, Ricciotti N, Sokoloff A, Brown BA, Hummel A, Harper CC. An over-the-counter simulation study of a single-tablet emergency contraceptive in young females. Obstet Gynecol. 2012;119(4):772–9.
Shaaban OM, Hassen SG, Nour SA, Kames MA, Yones EM. Emergency contraceptive pills as a backup for lactational amenorrhea method (LAM) of contraception: a randomized controlled trial. Contraception. 2013;87(3):363–9.
Kesserü E, Larrañaga A, Parada J. Postcoital contraception with D-norgestrel. Contraception. 1973;7(5):367–79.
De Santis M, Cavaliere AF, Straface G, Carducci B, Caruso A. Failure of the emergency contraceptive levonorgestrel and the risk of adverse effects in pregnancy and on fetal development: an observational cohort study. Fertil Steril. 2005;84(2):296–9.
Polakow-Farkash S, Gilad O, Merlob P, Stahl B, Yogev Y, Klinger G. Levonorgestrel used for emergency contraception during lactation-a prospective observational cohort study on maternal and infant safety. J Matern Fetal Neonatal Med. 2013;26(3):219–21.
Zhang L, Ye W, Yu W, Cheng L, Shen L, Yang Z. Physical and mental development of children after levonorgestrel emergency contraception exposure: a follow-up prospective cohort study1. Biol Reprod. 2014;91(1):27.
Carvajal A, Sainz M, Velasco V, Garcia Ortega P, Treceno C, Martin Arias LH, et al. Emergency contraceptive pill safety profile. Comparison of the results of a follow-up study to those coming from spontaneous reporting. Pharmacoepidemiol Drug Saf. 2015;24(1):93–7.
Rodriguez de Antonio LA, Fuentes B, Aguilar-Amat MJ, Diez-Tejedor E. Emergency contraception and stroke. A new case report. Med Clin (Barc). 2011;136(14):647–8.
Lomana AV, Aznar JMF, Cuenca VH. Venous thrombosis of the upper extremity following the ingestion of levonorgestrel as an emergency contraceptive. Anales de Patologia Vascular. 2010;4(4):204–6.
Foer D, Buchheit KM, Gargiulo AR, Lynch DM, Castells M, Wickner PG. Progestogen hypersensitivity in 24 cases: diagnosis, management, and proposed renaming and classification. J Allergy Clin Immunol Pract. 2016;4(4):723–9.
Basu A, Candelier C. Ectopic pregnancy with postcoital contraception–a case report. Eur J Contracept Reprod Health Care. 2005;10(1):6–8.
Cabar FR, Pereira PP, Zugaib M. Intrauterine pregnancy after salpingectomy for tubal pregnancy due to emergency contraception: a case report. Clinics (Sao Paulo). 2007;62(5):641–2.
Ghosh B, Dadhwal V, Deka D, Ramesan CK, Mittal S. Ectopic pregnancy following levonorgestrel emergency contraception: a case report. Contraception. 2009;79(2):155–7.
Jian Z, Linan C. Ectopic gestation following emergency contraception with levonorgestrel. Eur J Contracept Reprod Health Care. 2003;8(4):225–8.
Kaymak O, Simşek Y, Doğanay M, Yıldız Y, Mollamahmutoğlu L. Ectopic pregnancy following levonorgestrel emergency contraception: a case report. J Turk German Gynecol Assoc. 2010;11(3):168–9.
Kitani Y, Ishiguro T, Kobayashi A, Tamura R, Ueda H, Adachi S, et al. Ectopic pregnancy following oral levonorgestrel emergency contraception use. J Obstet Gynaecol Res. 2019;45(2):473–6.
Kozinszky Z, Bakken RT, Lieng M. Ectopic pregnancy after levonorgestrel emergency contraception. Contraception. 2011;83(3):281–3.
Pereira PP, Cabar FR, Raiza LC, Roncaglia MT, Zugaib M. Emergency contraception and ectopic pregnancy: report of 2 cases. Clinics (Sao Paulo). 2005;60(6):497–500.
Sheffer-Mimouni G, Pauzner D, Maslovitch S, Lessing JB, Gamzu R. Ectopic pregnancies following emergency levonorgestrel contraception. Contraception. 2003;67(4):267–9.
Steele BJ, Layman K. Ectopic pregnancy after plan b emergency contraceptive use. J Emerg Med. 2016;50(4):663–6.
Tan S, Bourke R, Roberts M, Chew M, Beilby R, Roach V. Heterotopic pregnancy after Postinor-2. Aust N Z J Obstet Gynaecol. 2004;44(5):460–1.
Sehgal A, Rani S, Singh A. Ectopic pregnancy following levonorgestrel postcoital contraceptive. J South Asian Feder Obst Gynae. 2017;9(2):131–2.
Cameron S, Li H, Gemzell-Danielsson K. Current controversies with oral emergency contraception. BJOG. 2017;124(13):1948–56.
Puig Borràs C, Álvarez Álvarez BI. The history of universal access to emergency contraception in Peru: a case of politics deepening inequalities. Reprod Health Matters. 2018;26(54):47–50.
Plan B One-Step (levonorgestrel) tablet, 1.5 mg, for oral use. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021998lbl.pdf.
Motta E, Golba A, Ostrowska Z, Steposz A, Huc M, Kotas-Rusnak J, et al. Progesterone therapy in women with epilepsy. Pharmacol Rep. 2013;65(1):89–98.
Moran MH, Smith SS. Progesterone withdrawal I: pro-convulsant effects. Brain Res. 1998;807(1–2):84–90.
Shiono S, Williamson J, Kapur J, Joshi S. Progesterone receptor activation regulates seizure susceptibility. Ann Clin Transl Neurol. 2019;6(7):1302–10.
Shurie S, Were E, Orang’o O, Keter A. Levonorgestrel only emergency contraceptive use and risk of ectopic pregnancy in Eldoret Kenya: a case-control study. Pan Afr Med J. 2018;31:214.
Li C, Zhang H-Y, Liang Y, Xia W, Zhu Q, Zhang D, et al. Effects of levonorgestrel and progesterone on oviductal physiology in mammals. Reprod Biol Endocrinol. 2018;16(1):59.
Chakhtoura Z, Canonico M, Gompel A, Thalabard JC, Scarabin PY, Plu-Bureau G. Progestogen-only contraceptives and the risk of stroke: a meta-analysis. Stroke. 2009;40(4):1059–62.
van Hylckama Vlieg A, Helmerhorst FM, Rosendaal FR. The risk of deep venous thrombosis associated with injectable depot-medroxyprogesterone acetate contraceptives or a levonorgestrel intrauterine device. Arterioscler Thromb Vasc Biol. 2010;30(11):2297–300.
de Bastos M, Stegeman BH, Rosendaal FR, Van Hylckama Vlieg A, Helmerhorst FM, Stijnen T, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014;(3):CD010813.
Weill A, Dalichampt M, Raguideau F, Ricordeau P, Blotière P-O, Rudant J, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
Dragoman MV, Tepper NK, Fu R, Curtis KM, Chou R, Gaffield ME. A systematic review and meta-analysis of venous thrombosis risk among users of combined oral contraception. Int J Gynaecol Obstet. 2018;141(3):287–94.
Cardiovascular disease and use of oral and injectable progestogen-only contraceptives and combined injectable contraceptives. Results of an international, multicenter, case-control study. World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Contraception. 1998;57(5):315–24.
Lidegaard O, Kreiner S. Contraceptives and cerebral thrombosis: a five-year national case-control study. Contraception. 2002;65(3):197–205.
Shaaban MM, Elwan SI, El-Kabsh MY, Farghaly SA, Thabet N. Effect of levonorgestrel contraceptive implants, Norplant, on blood coagulation. Contraception. 1984;30(5):421–30.
Middeldorp S, Meijers JC, van den Ende AE, van Enk A, Bouma BN, Tans G, et al. Effects on coagulation of levonorgestrel- and desogestrel-containing low dose oral contraceptives: a cross-over study. Thromb Haemost. 2000;84(1):4–8.
Ruan X, Neubauer H, Yang Y, Schneck H, Schultz S, Fehm T, et al. Progestogens and membrane-initiated effects on the proliferation of human breast cancer cells. Climacteric. 2012;15(5):467–72.
Sivik T, Jansson A. Progesterone and levonorgestrel regulate expression of 17betaHSD-enzymes in progesterone receptor positive breast cancer cell line T47D. Biochem Biophys Res Commun. 2012;422(1):109–13.
Neubauer H, Ma Q, Zhou J, Yu Q, Ruan X, Seeger H, et al. Possible role of PGRMC1 in breast cancer development. Climacteric. 2013;16(5):509–13.
Soini T, Hurskainen R, Grenman S, Maenpaa J, Paavonen J, Pukkala E. Cancer risk in women using the levonorgestrel-releasing intrauterine system in Finland. Obstet Gynecol. 2014;124(2 Pt 1):292–9.
Jareid M, Thalabard JC, Aarflot M, Bovelstad HM, Lund E, Braaten T. Levonorgestrel-releasing intrauterine system use is associated with a decreased risk of ovarian and endometrial cancer, without increased risk of breast cancer. Results from the NOWAC Study. Gynecol Oncol. 2018;149(1):127–32.
Averbach S, Silverberg MJ, Leyden W, Smith-McCune K, Raine-Bennett T, Sawaya GF. Recent intrauterine device use and the risk of precancerous cervical lesions and cervical cancer. Contraception. Epub 17 Apr 2018. https://doi.org/10.1016/j.contraception.2018.04.008.
Misra JS, Engineer AD, Tandon P. Cervical cytology associated with levonorgestrel contraception. Acta Cytol. 1995;39(1):45–9.
Yoo YA, Son J, Mehta FF, DeMayo FJ, Lydon JP, Chung S-H. Progesterone signaling inhibits cervical carcinogenesis in mice. Am J Pathol. 2013;183(5):1679–87.
Chung S-H. Targeting female hormone receptors as cervical cancer therapy. Trends Endocrinol Metab. 2015;26(8):399–401.
Mehta FF, Baik S, Chung S-H. Recurrence of cervical cancer and its resistance to progestin therapy in a mouse model. Oncotarget. 2017;8(2):2372–80.
Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA. Advance provision of emergency contraception for pregnancy prevention (full review). Cochrane Database Syst Rev. 2007;2:CD005497.
Sander PM, Raymond EG, Weaver MA. Emergency contraceptive use as a marker of future risky sex, pregnancy, and sexually transmitted infection. Am J Obstet Gynecol. 2009;201(2):146.
Hall OJ, Klein SL. Progesterone-based compounds affect immune responses and susceptibility to infections at diverse mucosal sites. Mucosal Immunol. 2017;10(5):1097–107.
Yao Y, Li H, Ding J, Xia Y, Wang L. Progesterone impairs antigen-non-specific immune protection by CD8 T memory cells via interferon-gamma gene hypermethylation. PLoS Pathog. 2017;13(11):e1006736.
Levonorgestrel-containing IUDs: psychiatric adverse events. React Week. 2018;1704(1):9.
Gingnell M, Engman J, Frick A, Moby L, Wikstrom J, Fredrikson M, et al. Oral contraceptive use changes brain activity and mood in women with previous negative affect on the pill–a double-blinded, placebo-controlled randomized trial of a levonorgestrel-containing combined oral contraceptive. Psychoneuroendocrinology. 2013;38(7):1133–44.
Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of Hormonal Contraception With Depression. JAMA Psychiatry. 2016;73(11):1154–62.
Glick ID, Bennett SE. Psychiatric complications of progesterone and oral contraceptives. J Clin Psychopharmacol. 1981;1(6):350–67.
Skovlund CW, Morch LS, Kessing LV, Lange T, Lidegaard O. Association of hormonal contraception with suicide attempts and suicides. Am J Psychiatry. 2018;175(4):336–42.
Brinton RD, Thompson RF, Foy MR, Baudry M, Wang J, Finch CE, et al. Progesterone receptors: form and function in brain. Front Neuroendocrinol. 2008;29(2):313–39.
Jin J, Maren S. Prefrontal–hippocampal interactions in memory and emotion. Front Syst Neurosci. 2015;9:170.
Sigurdsson T, Duvarci S. hippocampal–prefrontal interactions in cognition, behavior and psychiatric disease. Front Syst Neurosci. 2016;9:190.
Xiong X, Buekens P, Wollast E. IUD use and the risk of ectopic pregnancy: a meta-analysis of case–control studies. Contraception. 1995;52(1):23–34.
Romita P, Foti C, Calogiuri G, Cantore S, Ballini A, Dipalma G, et al. Contact dermatitis due to transdermal therapeutic systems: a clinical update. Acta bio-medica. 2018;90(1):5–10.
Bondon-Guitton E, Bagheri H, Montastruc JL. Drug-induced gingival overgrowth: a study in the French Pharmacovigilance Database. J Clin Periodontol. 2012;39(6):513–8.
Brinker A, Beitz J. Use of a spontaneous adverse drug events database for identification of unanticipated drug benefits. Clin Pharmacol Ther. 2002;71(1):99–102.
Buccellato E, Biagi C, Vaccheri A, Melis M, Montanaro N, Motola D. Possible occurrence of paraesthesia in patients taking norethisterone: an analysis on the WHO Global Individual Case Reports database (VigiBase). Expert Opin Drug Saf. 2013;12(5):615–9.
Jick H, Jick SS, Gurewich V, Myers MW, Vasilakis C. Risk of idiopathic cardiovascular death and nonfatal venous thromboembolism in women using oral contraceptives with differing progestagen components. Lancet. 1995;346(8990):1589–93.
Etminan M, Delaney JA, Bressler B, Brophy JM. Oral contraceptives and the risk of gallbladder disease: a comparative safety study. CMAJ. 2011;183(8):899–904.
Manzouri L, Parhizkar S, Mohammadi N. Comparison the effectiveness and side effects of two methods of emergency contraception: levonorgestrel versus LD, HD. Maturitas. 2015;81(1):194–5.
van Rooijen M, Silveira A, Thomassen S, Hansson LO, Rosing J, Hamsten A, et al. Rapid activation of haemostasis after hormonal emergency contraception. Thromb Haemost. 2007;97(1):15–20.
Task Force on Post-Ovulatory Methods for Fertility Regulation. Efficacy and side effects of immediate postcoital levonorgestrel used repeatedly for contraception. Contraception. 2000;61(5):303–8.
Author information
Authors and Affiliations
Contributions
NL and JM designed the research and conducted the systematic review and meta-analysis. NL wrote the paper and had primary responsibility for the final content. Both authors read and approved, and are in agreement with, the final version submitted for publication. The content has not been published elsewhere.
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Nattawut Leelakanok and Janthima Methaneethorn declare they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leelakanok, N., Methaneethorn, J. A Systematic Review and Meta-analysis of the Adverse Effects of Levonorgestrel Emergency Oral Contraceptive. Clin Drug Investig 40, 395–420 (2020). https://doi.org/10.1007/s40261-020-00901-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-020-00901-x