Abstract
Background
Levetiracetam is widely used in post-stroke epilepsy. However, it is suspected to possess P-glycoprotein (P-gp) induction properties, and therefore, a potentially significant interaction with direct oral anticoagulants (DOACs). We aimed to search for ischemic stroke signals with levetiracetam and the DOACs.
Methods
In this retrospective pharmacovigilance study, we used the FAERS database to identify ischemic stroke events associated with DOACs and concomitant use of levetiracetam. We evaluated disproportionate reporting by the adjusted reporting odds ratio (adjROR) and the lower bound of the shrinkage 95% confidence interval. When shrinkage is positive, an increased risk of a specific adverse event occurrence is emphasized over the sum of the individual risks when these same drugs are used separately.
Results
We identified 1841 (1.5%), 3731 (5.3%), 338 (4.9%), and 1723 (1.3%) ischemic stroke reports with apixaban, dabigatran, edoxaban, and rivaroxaban, respectively. The adjROR of the interaction effect was 3.57 (95% CI 2.81–4.58) between DOACs and levetiracetam. The shrinkage analysis detected an interaction between each of the DOACs and levetiracetam. The logistic model and shrinkage analysis failed to detect an interaction when queried for hemorrhagic stroke. A significant signal in the classical enzyme inducer, carbamazepine, strengthened our results (adjROR; 8.47, 95% CI 5.37–13.36).
Conclusions
Our study shows a strong signal for the levetiracetam interaction with the DOACs. Our findings suggest implementation of a drug monitoring strategy.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Controversy exists regarding P-gp efflux protein induction with levetiracetam, an interaction that may decrease DOACs’ bioavailability. |
Clinical guidelines in atrial fibrillation stress the need for ‘real-world’ studies to investigate the safety of the levetiracetam–DOAC combination. |
We demonstrated a probable drug interaction resulting in a 3–5-fold increased reporting risk of ischemic stroke with a DOAC-levetiracetam combination. |
Our findings do not mean that DOACs should not be prescribed with levetiracetam, but suggest that pharmacodynamic monitoring might be helpful until more evidence accumulates. |
1 Introduction
Introducing direct oral anticoagulants (DOACs) has significantly altered the management of atrial fibrillation (AF) due to their improved safety profile and ease of use compared with warfarin. Contemporary guidelines prefer DOACs over warfarin for stroke prevention among patients with AF, excluding patients with mechanical valve replacement or significant mitral stenosis [1]. While there is no preference for one specific DOAC over another, in practice, DOACs are personalized according to patient age, gastrointestinal bleeding risk, chronic kidney disease, and drug interactions [2].
Since stroke is one of the most common structural etiologies of epilepsy, the concomitant use of DOACs and an anticonvulsant is not uncommon [3]. Post‐stroke seizures account for 11% of all epilepsy, 22% of all cases of status epilepticus, and 55% of newly diagnosed seizures amongst older people [4,5,6]. Since AF is a common cause of ischemic stroke, the rate of AF–stroke–epilepsy triplet, and thus DOAC-antiseizure medications (ASMs) combined, is not uncommon among older adults [7].
To date, the combination of DOAC and some anticonvulsants remains controversial. The European Heart Rhythm Association (EHRA) 2018 guide did not support using anticonvulsants (carbamazepine, levetiracetam, phenobarbital, phenytoin, topiramate, and valproic acid) in patients concurrently taking DOACs [8]. The 2021 EHRA guide states that after inquiry with the drug manufacturer, there is, unfortunately, no study that reliably investigated the effect of levetiracetam on DOAC plasma levels and clinical events in a sufficiently large ‘real-world’ cohort of concomitantly treated patients [9].
A recent registry from Sweden investigated whether mortality varies with specific ASMs among patients with post-stroke epilepsy. The study concluded that lamotrigine monotherapy had significantly lower mortality than carbamazepine, while levetiracetam showed lower cardiovascular mortality but did not differ in overall mortality from carbamazepine [10].
Levetiracetam is widely used for post-stroke epilepsy due to its favorable safety profile and fewer drug interactions. However, concerns regarding the interaction between levetiracetam and DOACs are dealt with in case reports and cohort studies in the literature. Paciullo et al. reported a case in 2020 of a 69-year-old man with AF who received rivaroxaban (20 mg/d) and developed a transient ischemic attack a few months after initiating levetiracetam for the indication of focal seizure prevention [11]. Specific anti-Xa activity for rivaroxaban found a zero-trough level immediately before rivaroxaban administration.
In 2020, Giustozzi et al. illustrated in a small prospective study (n = 91) that patients with non-valvular AF treated with DOACs and anticonvulsants appear to have a relatively high rate of thromboembolic events [12]. A similar conclusion was drawn in a nested case-control study supporting a diminished anticoagulant effect when combining DOACs with levetiracetam [13].
Therefore, our study aimed to investigate reports to the Federal Drug Agency (FDA) regarding ischemic and non-ischemic stroke with and without levetiracetam combination in patients with AF treated with DOACs.
2 Methods
An observational, retrospective pharmacovigilance study was carried out using the FDA Adverse Event Reporting System (FAERS) database, a global repository of voluntary reports by healthcare professionals and consumers, and mandatory reports from manufacturers [14]. The database was screened for reports containing the following terms in their brand or generic names: ‘rivaroxaban,’ ‘apixaban,’ ‘dabigatran,’ ‘dabigatran etexilate mesylate,’ ‘dabigatran etexilate,’ ‘edoxaban,’ ‘edoxaban mesylate,’ ‘edoxaban tosylate,’ ‘enoxaparin,’ ‘enoxaparin sodium,’ ‘heparin,’ ‘heparin sodium,’ ‘heparin calcium,’ ‘levetiracetam,’ ‘warfarin,’ ‘warfarin sodium,’ ‘warfarin potassium,’ ‘carbamazepine,’ and ‘omeprazole.’ Omeprazole and carbamazepine are, respectively, negative and positive controls in this study.
The study included patients reported as the primary suspects for a given adverse event (AE) when novel anticoagulants accessed the market (2012–2023). In case multiple reports of the same event were detected, only the latest case version of every event was retained, as recommended by the FDA. We further applied a population-linkage program to detect suspected duplicate reports of the same drug–event pair with different case numbers by screening for identical values in six key fields: age, sex, event date, country of occurrence, concomitant medications, and the same reasons for use. These suspected duplicate reports were excluded.
The database was then searched for the following adverse events in their Medical Dictionary for Regulatory Activities (MedDRA) preferred terms: ‘ischemic stroke,’ ‘hemorrhagic stroke,’ ‘cerebral hemorrhage,’ ‘intracranial hemorrhage,’ ‘cerebrovascular accident,’ ‘lacunar stroke,’ ‘cerebellar stroke,’ ‘cerebral artery occlusion,’ ‘basal ganglia stroke,’ ‘vertebrobasilar stroke,’ ‘brain stem stroke,’ ‘thrombotic stroke,’ and ‘embolic stroke.’ Those adverse events either denote a lack of effectiveness or toxicity. Detailed lists of terms included in our database query are available at http://bioportal.bioontology.org/.
The data were then filtered by the DOAC’s reason for use: embolic stroke in AF patient treatment and prevention. The dataset was then queried for cases with concomitant anticonvulsants used. Cases involving anticonvulsants were identified by a predefined list of anticonvulsant medications constructed using the FDA National Drug Code (NDC) file [15]. Only patients above the age of 12 years and cases with one reported anticonvulsant were included.
2.1 Study End Points
The predefined primary endpoint was any MedDRA-preferred term describing ischemic stroke. Additional information for each report in the database, including demographic information (country, reporter occupation, reporting year, age, and sex), concomitant anticonvulsant uses, and date of AE occurrence and its outcomes, were collected for the analysis. Cases were defined as serious medical events if one or more of the following outcomes were reported: death, life-threatening event, hospitalization, disability, or another serious medical event.
2.2 Statistical Analysis
Descriptive statistics were calculated for patient demographics. Means and standard deviations were generated for continuous variables. Frequencies and proportions were stated for categorical variables. A validated case–non-case method in drug safety research assessed whether ischemic and non-ischemic strokes were reported more frequently with the DOACs: apixaban, edoxaban, rivaroxaban, or dabigatran, compared with warfarin and enoxaparin/heparin. We further analyzed each of the DOACs compared with the other three for reported ischemic stroke. Each of the DOACs compared with all other DOACs aids in neutralizing confounding factors of the levetiracetam drug interaction, since cases with the combination of levetiracetam and a DOAC were compared with other cases of ischemic stroke with levetiracetam and other DOACs.
A logistic regression model obtained an adjusted reporting odds ratio (adj.ROR). The regression model included age, sex, and concomitant levetiracetam use. The ROR is a statistical model surrogate to the odds ratio and is an acceptable method to detect signals of adverse events and drug interactions [16, 17]. Missing sex data were coded as ‘Not Specified,’ and the median value imputed missing age data in each group of drug recipients. R-squared and adjusted R-squared were used to assess model fitness. The ROR for the variable levetiracetam was used to measure the strength of the association of the drug interaction.
Additionally, a refined model called the Ω shrinkage measure was used to calculate the observed-to-expected for detecting signals of potential drug–drug interactions (DDIs). Omega Ω is a robust observed-to-expected triplet measure of disproportionate reporting developed by the Uppsala Monitoring Centre [17, 18]. When Ω is positive, and two drugs are used together, an increased risk of a specific adverse event occurrence is emphasized over the sum of the individual risks when these same drugs are used separately [18]. Thus, Ω025 > 0, a positive lower bound of 95% CI, is used as a threshold for detecting the signals of the concomitant use of drug D1 and drug D2 [17]. In other words, it indicates the frequency of reporting specific drug–drug–event triplets in the dataset compared with what is expected on the basis of the relative reporting for each drug alone (see Eq. 1).
where \(\varnothing \left(0.975\right)\) is the standard normal distribution and n111 is the number of cases with the drug–drug–event triplet.
The logistic regression analyses were performed using SPSS version 27. Two-sided P < 0.05 indicated significance. Shrinkage calculation steps were inputted in Microsoft Excel version 2022. Noguchi et al. 2019 described the complete shrinkage calculation [17].
2.3 Sensitivity Analysis
First, we examined whether the drug interaction also manifests as hemorrhagic stroke. A model for hemorrhagic stroke comparing each of the DOACs, apixaban, rivaroxaban, and dabigatran, against the other two was performed. Edoxaban was not included in this analysis since there were no reports of hemorrhagic events with the levetiracetam–edoxaban combination.
A sensitivity analysis for the levetiracetam drug interaction included two drug combinations: apixaban–carbamazepine and apixaban–omeprazole. The former drug interaction is well established. Carbamazepine is known to induce P-glycoprotein and CYP3A4, thus reducing apixaban effectiveness (FDA and European Medical Agency physician guidance; [19, 20]). The EHRA guide recommends that strong inducers of P-gp and/or CYP3A4 (carbamazepine) will markedly reduce DOAC plasma levels; concomitant use with DOACs should be avoided or used with great caution and surveillance [9]. In contrast to carbamazepine, the combination of apixaban and omeprazole is widespread and considered safe without any known or potential drug interaction [21].
In an additional analysis, we further stratified DOACs by publication date up to 2020, aiming to mitigate reporting bias. We hypothesized that from 2020 onward, increased reports regarding DOACs and ischemic stroke may be expected, since the publication by Giustazzi et al. showed decreased effectiveness with concomitant DOAC–anticonvulsant use. Rivaroxaban was selected for further analysis since most patients in the Giustazzi et al. study were treated with rivaroxaban, and more case reports were published regarding rivaroxaban [12].
Further, we re-analyzed our results for the period 2015–2023 to account for the fact that during 2010–2014, a trial had been ongoing against Boehringer Ingelheim, dabigatran’s manufacturer [22]. Thus, to mitigate any additional negative reporting bias, we analyzed our data excluding 2012–2014.
2.4 Standard Protocol Approvals, Registrations, and Patient Consents
The FAERS Public Dashboard is a publicly available web-based tool containing mandatory data reports from drug manufacturers and voluntary ADR reports from consumers and healthcare professionals. Hence, an informed consent or ethical statement of approval by an ethical standards committee on human experimentation is not required for analysis.
3 Results
3.1 Demographics and Patient Characteristics
The FAERS database included 19,609,956 unique safety reports from January 2012 to January 2023. Of these reports, 125,799 were for apixaban, 69,993 for dabigatran, 6965 for edoxaban, and 136,710 for rivaroxaban. Among eligible patients in the FAERS database that reported any of the MedDRA preferred terms for ischemic stroke are 1841 (1.5%), 3731 (5.3%), 338 (4.9%), and 1723 (1.3%), treated with apixaban, dabigatran, edoxaban, and rivaroxaban, respectively. In contrast, reports that described hemorrhagic stroke included 3016 (2.2%), 1346 (1.1%), and 1256 (1.8%) for rivaroxaban, apixaban, and dabigatran, respectively. An additional 464 (0.53%) and 383 (6.9%) ischemic stroke cases were identified among warfarin and enoxaparin/heparin-treated patients, respectively.
The proportion of men was significantly higher in both adverse events. The mean age for apixaban-treated patients was 77 ± 10 years, substantially older than the other three DOACs. Warfarin and enoxaparin/heparin patients were younger with a mean age of 69 ± 10 years and 72 ± 13 years and did not differ by sex from the DOACs. Hemorrhagic stroke resulted in poorer outcomes and more mortality compared with ischemic stroke (Table 1).
Concomitant levetiracetam reports and percentages of the total in each anticoagulant were as follows: 122 (0.1%) in apixaban, 142 (0.2%) in dabigatran, 20 (0.3%) in edoxaban, 168 (0.1%) in rivaroxaban, 5 (0.9%) in warfarin, and 45 (0.8%) in enoxaparin/heparin. The number of reports with the DOAC–levetiracetam–adverse event triplet is listed in Table 1.
3.2 Ischemic Stroke
The DOACs did not differ from enoxaparin or heparin in the disproportionality analysis for ischemic stroke (adj.ROR; 1.14, 95% CI, 1.01–1.28). The adjusted ROR of the interaction effect was 3.57 (95% CI, 2.81–4.58) between DOACs and levetiracetam, supporting a significant interaction. When warfarin was chosen as the comparator, the adj.ROR of the interaction was like enoxaparin/heparin (adj.ROR; 4.07, 95% CI, 3.23–5.15). The DOACs demonstrated a higher adj.ROR for ischemic stroke than warfarin (adj.ROR; 16.7, 95% CI, 14.8–18.7).
When comparing each DOAC separately, apixaban and rivaroxaban demonstrated the least disproportionality for ischemic stroke (adj.ROR; 0.44, 95% CI, 0.41–0.47) and (adj.ROR; 0.35, 95% CI, 0.33–0.37), respectively. A significant disproportionality signal was identified for ischemic stroke in dabigatran (adj.ROR 3.69; 95% CI, 3.50–3.88) and in edoxaban (adj. ROR 1.85; 95% CI, 1.58–2.16) AF users (Table 2).
3.3 DOAC–Levetiracetam Drug–Drug Interactions
Apixaban, dabigatran, edoxaban, and rivaroxaban illustrated a significant signal for the drug interaction in the regression model. The strength of association seems higher in edoxaban (adj.ROR 5.59; 95% CI, 4.23–7.39). In comparison, the strength of association was slightly lower with rivaroxaban (adj.ROR 3.69; 95% CI, 2.92–4.67).
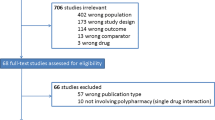
When queried for ischemic stroke, Ω0.25 was greater than zero for apixaban, dabigatran, and rivaroxaban, demonstrating an interaction with levetiracetam (Fig. 1). The magnitude of Ω0.25 was similar for the three DOACs. An interaction between levetiracetam and enoxaparin/heparin was not detected, with Ω0.25 < 0.
Shrinkage Analysis for the Anticoagulants–Levetiracetam Interaction. Ω025 > 0, a positive lower bound of 95% CI, is used as a threshold for detecting the signals of the concomitant use of the direct oral anticoagulants and levetiracetam. A positive shrinkage was noticed for ischemic in the concomitant use of either apixaban, dabigatran, and rivaroxaban with levetiracetam. A negative shrinkage was detected for hemorrhagic stroke and the concomitant use of apixaban or rivaroxaban with levetiracetam
3.4 Non-Ischemic Stroke–Hemorrhage
A significant disproportionality signal was identified for hemorrhagic stroke in rivaroxaban AF patients compared with apixaban and dabigatran (adj.ROR 1.46; 95% CI, 1.38–1.55) (Table 3). Dabigatran demonstrated a significantly lower adj.ROR for hemorrhagic stroke than the other DOACs, (adj.ROR 0.75; 95% CI, 0.70–0.78). Apixaban did not differ significantly from rivaroxaban and dabigatran.
The regression model queried for hemorrhagic stroke did not detect an interaction with levetiracetam. Likewise, the shrinkage analysis was negative for apixaban and rivaroxaban, detecting no interaction. The concomitant use of levetiracetam and the two DOACs does not seem to increase the risk of intracerebral bleeding reports. The shrinkage analysis tested positive for dabigatran (Fig. 1).
Contrary to the shrinkage analysis, the regression model did not detect signals for dabigatran–levetiracetam–hemorrhagic stroke triplet (adj.ROR 1.07; 95% CI, 0.90–1.28).
3.5 Sensitivity Analysis
In sensitivity analysis, we could not detect changes in disproportionality by publication date. The model detected signals in the positive control carbamazepine but not in the negative control omeprazole (Table 4).
4 Discussion
The current analysis is an expansion of a FAERS analysis by Perlman et al., concluding that enzyme-inducing ASMs were associated with an 86% increase in the odds of reporting thromboembolic and ischemic adverse events (ROR; 1.86, 95% CI 1.61–2.15) [23]. Here, we show a 3–5-fold increased risk of ischemic stroke reporting with the DOAC–levetiracetam combination. The interaction was confirmed using two methods accepted by regulators worldwide, suggesting a robust and significant finding.
The mechanism of the DDI is still not elucidated. There is controversy regarding cytochrome P450 or P-gp-inducting properties of levetiracetam. Preclinical studies suggest that levetiracetam reduces DOAC levels via P-glycoprotein induction, an efflux protein that reduces the bioavailability of DOACs [8, 9]. However, levetiracetam is not considered a classical inducer [9].
Nevertheless, there has been extensive concern regarding the interaction between levetiracetam and the DOACs. The 2021 European Heart Rhythm Association (EHRA) guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation recommends caution in the use of the ASM levetiracetam due to potential P-glycoprotein-mediated drug–drug interaction [8, 9].
Apixaban, dabigatran, edoxaban, and rivaroxaban are all substrates of the efflux transporter P-gp. Our analysis demonstrated an interaction with all four DOACs, with a 3–5-fold increased risk of stroke with some variability among the DOACs. Rivaroxaban showed the weakest association, probably because of its high baseline bioavailability compared with other DOACs [24].
The results of our study are supported by a large Information System for Research in Primary Care (SIDIAP) database, which demonstrated a significant association of increased ischemic stroke with levetiracetam, OR 95% CI values 4.1 (3.3–5.2) [25].
Recent pharmacokinetic studies suggest there is no such potential drug interaction. In a case study published by Menichelli et al. a 54-year-old male patient with AF, cirrhosis, and seizures showed no significant reduction in dabigatran plasma concentration when used alongside levetiracetam [26]. Another recent small PK study by Mavri et al. analyzed 21 patients concurrently receiving levetiracetam and DOACs, with 19 having atrial fibrillation and 2 having venous thromboembolism [27]. Blood samples were collected to measure trough concentrations of DOACs and levetiracetam. The results showed that none of the patients experienced thromboembolic events during the observation period of 1388 ± 994 days. Furthermore, there was no reduction in DOAC plasma levels during levetiracetam treatment, suggesting that levetiracetam may not significantly affect DOAC concentrations.
However, this study has two important limitations: DOAC trough levels are highly variable. Hence, the area under the curve must be analyzed to rule out the P-gp induction effect on plasma levels with and without levetiracetam. Second, the average trough levels of levetiracetam in that study (31.0 ± 34.5 mg/L) were higher than expected. Yet, the standard deviation may not ensure that all DOAC patients were adequately exposed to levetiracetam. In the literature, the lower bound confidence interval for levetiracetam concentrations is at least 15 mcg/mL [28].
Another retrospective cohort study published by Ip et al. evaluated the risk of thromboembolism in patients taking direct oral anticoagulants concurrently with antiseizure medications that modulate the cytochrome P450 or P-glycoprotein systems, including levetiracetam. While CYP/P-gp-modulating antiseizure medications were associated with an increased risk of ischemic stroke in the overall analysis, no difference in thromboembolism risk or death was observed in the epilepsy subgroup using levetiracetam [29].
Earlier studies on levetiracetam showed no alterations in plasma concentrations of other P-glycoprotein substrates such as digoxin [30, 31]. Therefore, it may also be reasonable to investigate pharmacodynamic interactions. Our shrinkage analysis did not detect an interaction with heparin/enoxaparin that resulted in bleeding or ischemic stroke, thus weakening the proposal of a pharmacodynamic interaction. We hypothesized that interactions involving protein coagulants would be revealed with heparin/enoxaprin.
Piracetam, a molecule similar in structure to levetiracetam, has been shown to have anticoagulant properties [32]. Our analysis did not show an increase in the reporting ratio of hemorrhagic stroke, defined as major bleeding, not supporting any levetiracetam anticoagulant properties, or increased bleeding.
It is worthwhile to note that dabigatran demonstrated a positive shrinkage signal for hemorrhagic stroke with the concomitant use of levetiracetam. However, the logistic regression failed to support any drug–drug interaction. A retrospective cohort of patients from Taiwan on DOACs and 11 different anticonvulsants reported an increased association of bleeding with concomitant prescription of phenytoin, valproic acid, or levetiracetam. The results were explained by an increased risk of renal failure with levetiracetam [33].
Although an interaction may exist between DOACs and levetiracetam, this does not mean physicians should stop prescribing the combination for post-stroke epilepsy. Levetiracetam is considered a newer and safer anticonvulsant [34]. We recommend implementing a drug monitoring strategy as a solution for this drug interaction.
Whether the interaction is pharmacokinetic or pharmacodynamic also has clinical implications for therapeutic drug monitoring. Naturally, a pharmacokinetic interaction is best monitored by plasma levels of DOACs. In contrast, anti-Xa for apixaban and rivaroxaban and the plasma diluted thrombin time for dabigatran would be more suitable for a pharmacodynamic interaction [22, 35].
Regarding evidence-based monitoring methods, Goldstein et al. examined the impact of cytochrome P450- and P-glycoprotein-inducing antiseizure medications on the pharmacokinetics of direct oral anticoagulants compared with rifampicin (a powerful inducer of DOACs elimination) [36]. They suggested monitoring DOAC plasma concentrations as a helpful strategy to guide dosing and identify patients at risk for low DOAC concentrations and treatment failure when taking enzyme-inducing antiseizure medications. In the event our findings are confirmed in further studies and the mechanism for the levetiracetam interaction is fully understood, pharmacodynamic monitoring would be preferred.
4.1 Strengths and Limitations
The major strengths of our study are utilizing a worldwide database, an analysis using two well-validated methods for signal detection, performing an extensive sensitivity analysis to challenge our model and mitigate reporting bias, and finally, suggesting pharmacological mechanisms that can explain the findings.
An essential limitation of the study is that patients treated with a DOAC and levetiracetam may be prone to a second stroke event. Thus, to minimize confounding by indication, our logistic regression model compared the effect of levetiracetam on one DOAC compared with the others; the comparator group for the interaction also reports that included DOAC–levetiracetam with probably similar risk factors, minimizing non-drug effects.
Another limitation is that some adverse events are likely not reported to national authorities for inclusion in the FAERS. This was mitigated by collecting data from all countries from 2012 to 2023. Although concomitant drug use was accounted for in our analysis, it is challenging to determine with certainty the sequence of medication use owing to missing data and temporality being associated with an adverse event rather than a drug.
Lamotrigine is an alternative medication to post-stroke epilepsy. Its use for that indication is seemingly low, probably due to potential cardiac sodium channel blockage [37]. Thus, we could not detect ischemic stroke reports in DOACs combined with lamotrigine. Therefore, we used omeprazole as our negative control, which is usually prescribed to prevent gastrointestinal bleeding with DOACs. The analysis could not detect a drug interaction with DOACs and omeprazole, but detected a significant signal in the classical enzyme inducer carbamazepine, which strengthened our results (adjROR; 8.47, 95% CI 5.37–13.36).
There were no reports of intracranial bleeding with the concomitant use of levetiracetam and edoxaban, limiting the directional analysis for edoxaban–levetiracetam interaction. Although the regression model and shrinkage analysis detected an interaction with edoxaban, a discrepancy in their magnitudes was noted. This could be explained by a high proportion of ischemic stroke reports and a low number of non-cases reporting concomitant levetiracetam use, which emphasized this variable in the regression model.
The FAERS database for dabigatran shows a peak, with high report rates between 2011 and 2014, which could be due to a trial against dabigatran’s manufacturer and negative publicity in those years [22, 38]. To account for this, we re-analyzed the data excluding 2010–2014, but the signal for ischemic events and the levetiracetam drug interaction did not significantly change.
Our results also show that dabigatran has the lowest adj.ROR for hemorrhagic stroke, a reciprocal image of the high reporting on ischemic stroke, which suggests the robustness of the model used. In the literature, dabigatran does not seem to differ in effectiveness from the other DOACs, but is associated with lower risk of major bleeding [39].
Although we could detect a signal for ischemic stroke in the DOACs compared with warfarin, a literature review does not support the results [40,41,42]. This could be explained by lead time bias, confounding by indication, and reporting bias. Moreover, patients being treated with warfarin have major comorbid conditions, which might constrict the use of DOACs, such as end-stage renal disease or valvular atrial fibrillation [42]. Overall, the comparator choice did not significantly affect the strength of association of the levetiracetam–DOAC interaction.
While the FAERS database includes a large amount of data on real-world adverse events with medications, it has limited information on patient characteristics, making it difficult to control for factors that may confound the relationship between medication and outcome occurrence and reporting, such as stroke risk factors. The results remained consistent regardless of comparator choice, following stratifications and head-to-head DOAC comparison, emphasizing the robustness of such real-world studies. Moreover, a retrospective cohort study by Perlman et al. illustrated a similar strength of association to the current research with enzyme-inducing ASMs. DOAC concentrations below the expected range were 5.82-fold higher than patients who did not use enzyme-inducing ASMs [43].
Another limitation of the study is that it cannot provide a direct estimate of the prevalence of the co-prescribing of FXa-DOACs and ASMs, as the FAERS database includes only cases reporting adverse events with treatment. In addition, reports lack dosage information.
Limitations to spontaneous reporting (e.g., underreporting) exist as well. However, despite its flaws, analyzing pharmacovigilance databases remains a cornerstone for studying adverse drug reactions and drug interactions by regulators and contributes majorly to drug labels.
4.2 Conclusions and Clinical Implications
We show a strong signal for the levetiracetam interaction with apixaban, dabigatran, edoxaban, and rivaroxaban. The interaction is demonstrated by a 3–5-fold increased reporting risk of ischemic stroke. Our findings do not mean that DOACs should not be prescribed levetiracetam, but suggest a need for pharmacodynamic monitoring until more evidence accumulates. Monitoring either anti-Xa for apixaban, edoxaban, and rivaroxaban or plasma diluted thrombin time for dabigatran while concomitantly prescribing levetiracetam with the DOACs when the two drugs are at a steady state could be helpful.
References
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan G-A, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau J-P, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL. ESC Scientific Document Group, 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612.
Chan N, Sobieraj-Teague M, Eikelboom JW. Direct oral anticoagulants: evidence and unresolved issues. Lancet. 2020;396(10264):1767–76. https://doi.org/10.1016/S0140-6736(20)32439-9.
Chang RS, Leung WC, Vassallo M, Sykes L, Battersby Wood E, Kwan J. Antiepileptic drugs for the primary and secondary prevention of seizures after stroke. Cochrane Database Syst Rev. 2022;2(2): CD005398. https://doi.org/10.1002/14651858.
Camilo O, Goldstein LB. Seizures and epilepsy after ischemic stroke. Stroke. 2004;35(7):1769–75. https://doi.org/10.1161/01.STR.0000130989.17100.96. (Epub 2004 May 27).
DeLorenzo RJ, Hauser WA, Towne AR, Boggs JG, Pellock JM, Penberthy L, Garnett L, Fortner CA, Ko D. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46(4):1029–35.
Herman ST. Epilepsy after brain insult: targeting epileptogenesis. Neurology. 2002;59(9 Suppl 5):S21–6. https://doi.org/10.1212/wnl.59.9_suppl_5.s21.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, Rowell N, Sinnaeve P, Collins R, Camm AJ, Heidbüchel H, ESC Scientific Document Group. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–93.
Jan Steffel and others. 2021 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. EP Europace. 2021;23(10):1612–76. https://doi.org/10.1093/europace/euab065.
Larsson D, Baftiu A, Johannessen Landmark C, von Euler M, Kumlien E, Åsberg S, Zelano J. Association between antiseizure drug monotherapy and mortality for patients with poststroke epilepsy. JAMA Neurol. 2022;79(2):169–75. https://doi.org/10.1001/jamaneurol.2021.4584.
Paciullo F, Costa C, Gresele P. Rivaroxaban plasma levels and levetiracetam. Ann Intern Med. 2020;173(9):772. https://doi.org/10.7326/L20-1066.
Giustozzi M, Mazzetti M, Paciaroni M, et al. Concomitant use of direct oral anticoagulants and antiepileptic drugs: a prospective cohort study in patients with atrial fibrillation. Clin Drug Investig. 2021;41:43–51. https://doi.org/10.1007/s40261-020-00982-8.
Gronich N, Stein N, Muszkat M. Association between use of pharmacokinetic-interacting drugs and effectiveness and safety of direct acting oral anticoagulants: nested case-control study. Clin Pharmacol Ther. 2021;110(6):1526–36. https://doi.org/10.1002/cpt.2369.
FAERS database. https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-public-dashboard. Accessed Feb. 2023.
Center for Drug Evaluation and Research. National Drug Code Directory. U.S. Food and Drug Administration. 2022. https://www.fda.gov/drugs/drug-approvals-and-databases/national-drug-code-directory. Accessed Feb. 2023.
van Puijenbroek EP, Bate A, Leufkens HG, Lindquist M, Orre R, Egberts AC. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf. 2002;11(1):3–10. https://doi.org/10.1002/pds.668.
Noguchi Y, Tachi T, Teramachi H. Review of statistical methodologies for detecting drug–drug interactions using spontaneous reporting systems. Front Pharmacol. 2019;8(10):1319. https://doi.org/10.3389/fphar.2019.01319.
Norén GN, Sundberg R, Bate A, Edwards IR. A statistical methodology for drug–drug interaction surveillance. Stat Med. 2008;27(16):3057–70. https://doi.org/10.1002/sim.3247. (Erratum in: Stat Med. 2008 Dec 20;27(29):6271-2).
Apixaban Physician Guidance. https://www.medicines.org.uk/emc/product/2878/smpc#gref. Accessed Feb. 2023.
Apixaban Physician Guidance. FDA. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=095a08ac-cf0e-497e-a682-ddef38d6b29c#Section_5.3. Accessed, Feb. 2023.
Bolek T, Samoš M, Škorňová I, et al. Does proton pump inhibition change the on-treatment anti-Xa activity in xabans-treated patients with atrial fibrillation? A pilot study. J Thromb Thrombolysis. 2019;47:140–5. https://doi.org/10.1007/s11239-018-1748-5.
Kaba RA, Ara F, Ward DE, Emanuel S. The dabigatran debate. Glob Cardiol Sci Pract. 2014;2014(3):254–6. https://doi.org/10.5339/gcsp.2014.41.
Perlman A, Wanounou M, Goldstein R, Choshen Cohen L, Singer DE, Muszkat M. Ischemic and thrombotic events associated with concomitant xa-inhibiting direct oral anticoagulants and antiepileptic drugs: analysis of the FDA Adverse Event Reporting System (FAERS). CNS Drugs. 2019;33(12):1223–8. https://doi.org/10.1007/s40263-019-00677-5.
Rivaroxaban Physician Guidance: https://www.medicines.org.uk/emc/product/2793/smpc#gref. Accessed, Aug. 2023.
Giner-Soriano M, Marsal JR, Gomez-Lumbreras A, Morros R. Risk of ischaemic stroke associated with antiepileptic drugs: a population-based case-control study in Catalonia. BMC Neurol. 2021;21:208.
Menichelli D, Pastori D, Pignatelli P, Pani A. Minimizing drug-drug interactions between dabigatran and levetiracetam through clinical management: a case report. Eur Heart J Case Rep. 2023;7(1): ytad006. https://doi.org/10.1093/ehjcr/ytad006.
Mavri A, Ilc S. The efficacy of direct oral anticoagulants in patients on concomitant treatment with levetiracetam. Sci Rep. 2023;13(1):9257. https://doi.org/10.1038/s41598-023-33876-8.
Mendoza Aguilera M, Bellés Medall MD, Álvarez Martín T, Pascual Marmaneu Ó, LiñanaGranell C, Ferrando PR. Therapeutic drug monitoring of levetiracetam in daily clinical practice: high-performance liquid chromatography versus immunoassay. Eur J Hosp Pharm. 2020;27(e1):e2–6. https://doi.org/10.1136/ejhpharm-2018-001616.
Ip BY, Ko H, Wong GL, Yip TC, Lau LH, Lau AY, Leng X, Leung H, Chan HH, Chan HY, Mok VC, Soo YO, Leung TW. Thromboembolic risks with concurrent direct oral anticoagulants and antiseizure medications: a population-based analysis. CNS Drugs. 2022;36(12):1313–24. https://doi.org/10.1007/s40263-022-00971-9.
Mathy FX, Dohin E, Bonfitto F, Pelgrims B. Drug-drug interaction between levetiracetam and non-vitamin K antagonist anticoagulants. Eur Heart J. 2019;40(19):1571. https://doi.org/10.1093/eurheartj/ehy780.
Levy RH, Ragueneau-Majlessi I, Baltes E. Repeated administration of the novel antiepileptic agent levetiracetam does not alter digoxin pharmacokinetics and pharmacodynamics in healthy volunteers. Epilepsy Res. 2001;46(2):93–9. https://doi.org/10.1016/s0920-1211(01)00253-4.
Teng CM, Yeh HI, Lee LG. Anticoagulant and antiplatelet properties of piracetam. Taiwan Yi Xue Hui Za Zhi. 1983;82(11):1104–14.
Wang CL, Wu VC, Chang KH, Tu HT, Kuo CF, Huang YT, Chu PH, Kuo CC, Chang SH. Assessing major bleeding risk in atrial fibrillation patients concurrently taking non-vitamin K antagonist oral anticoagulants and antiepileptic drugs. Eur Heart J Cardiovasc Pharmacother. 2020;6(3):147–54. https://doi.org/10.1093/ehjcvp/pvz035.
French JA, Gazzola DM. New generation antiepileptic drugs: what do they offer in terms of improved tolerability and safety? Ther Adv Drug Saf. 2011;2(4):141–58. https://doi.org/10.1177/2042098611411127.
Sarode R. Direct oral anticoagulant monitoring: what laboratory tests are available to guide us? Hematol Am Soc Hematol Educ Program. 2019;2019(1):194–7. https://doi.org/10.1182/hematology.2019000027.
Goldstein R, Jacobs AR, Zighan L, Gronich N, Bialer M, Muszkat M. Interactions between direct oral anticoagulants (DOACs) and antiseizure medications: potential implications on DOAC treatment. CNS Drugs. 2023;37(3):203–14. https://doi.org/10.1007/s40263-023-00990-0.
FDA: Studies show increased risk of heart rhythm problems with seizure and mental health medicine lamotrigine (Lamictal) in patients with heart disease. https://www.fda.gov/drugs/drug-safety-and-availability/studies-show-increased-risk-heart-rhythm-problems-seizure-and-mental-health-medicine-lamotrigine. Accessed Sep. 2022.
Pradaxa lawsuit. https://www.drugwatch.com/pradaxa/lawsuits/. Accessed Feb. 2023.
Lau WCY, Torre CO, Man KKC, Stewart HM, Seager S, Van Zandt M, Reich C, Li J, Brewster J, Lip GYH, Hingorani AD, Wei L, Wong ICK. Comparative effectiveness and safety between apixaban, dabigatran, edoxaban, and rivaroxaban among patients with atrial fibrillation: a multinational population-based cohort study. Ann Intern Med. 2022;175(11):1515–24. https://doi.org/10.7326/M22-0511.
Yao X, Abraham NS, Sangaralingham LR, Bellolio MF, McBane RD, Shah ND, Noseworthy PA. Effectiveness and safety of dabigatran, rivaroxaban, and apixaban versus warfarin in nonvalvular atrial fibrillation. J Am Heart Assoc. 2016;5(6): e003725. https://doi.org/10.1161/JAHA.116.003725.
Harrington J, Carnicelli AP, Hua K, Wallentin L, Patel MR, Hohnloser SH, Giugliano RP, Fox KAA, Hijazi Z, Lopes RD, Pokorney SD, Hong H, Granger CB. Direct oral anticoagulants versus warfarin across the spectrum of kidney function: patient-level network meta-analyses from COMBINE AF. Circulation. 2023;147(23):1748–57. https://doi.org/10.1161/CIRCULATIONAHA.122.062752.
Chen A, Stecker E, Warden BA. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc. 2020;9(13): e017559. https://doi.org/10.1161/JAHA.120.017559. (Epub 2020 Jun 15).
Perlman A, Goldstein R, Choshen Cohen L, Hirsh-Raccah B, Hakimian D, Matok I, Kalish Y, Singer DE, Muszkat M. Effect of enzyme-inducing antiseizure medications on the risk of sub-therapeutic concentrations of direct oral anticoagulants: a retrospective cohort study. CNS Drugs. 2021;35(3):305–16. https://doi.org/10.1007/s40263-021-00795-z.
Acknowledgments
We acknowledge the support of Professor Ilan Matok, Chairman of the Clinical Pharmacy Program, Faculty of Medicine, Hebrew University of Jerusalem. Preprints of this work have been posted in MedRxiv: www.medrxiv.org/content/10.1101/2023.08.21.23294397v1.full.pdf; https://www.medrxiv.org/content/10.1101/2023.08.21.23294397v1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of Interest
Mohammed Aboukaoud, Ran Nissan, Amitai Segev, Avi Sabbag, David Orion, and Elad Maor have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available in the FAERS repository. https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-public-dashboard.
Author Contributions
Mohammed Aboukaoud is responsible for the data collection, statistical analysis, and manuscript writing. Ran Nissan, expert in pharmacotherapy, participated in writing and reviewing the manuscript. Amitai Segev, Avi Sabbag, and Elad Maor, experts in Cardiology, participated in writing and reviewing the manuscript. David Orion is a Neurologist who reviewed the manuscript.
Ethics Approval
Not applicable. The FAERS Public Dashboard is a publicly available web-based tool containing mandatory data reports from drug manufacturers and voluntary ADR reports from consumers and healthcare professionals. Hence an informed consent or ethical statement of approval by an ethical standards committee on human experimentation is not required for analysis.
Code Availability
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abou Kaoud, M., Nissan, R., Segev, A. et al. Levetiracetam Interaction with Direct Oral Anticoagulants: A Pharmacovigilance Study. CNS Drugs 37, 1111–1121 (2023). https://doi.org/10.1007/s40263-023-01052-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01052-1