Abstract
The use of direct oral anticoagulants (DOACs) is increasing because of their superior efficacy and safety compared with vitamin K antagonists. Pharmacokinetic drug interactions, particularly those involving cytochrome P450- mediated metabolism and P-glycoprotein transport, significantly affect the efficacy and safety of DOACs. In this article, we assess the effects of cytochrome P450- and P-glycoprotein-inducing antiseizure medications on DOAC pharmacokinetics in comparison to rifampicin. Rifampicin decreases to a varying extent the plasma exposure (area under the concentration–time curve) and peak concentration of each DOAC, consistent with its specific absorption and elimination pathways. For apixaban and rivaroxaban, rifampicin had a greater effect on the area under the concentration–time curve than on peak concentration. Therefore, using peak concentration to monitor DOAC concentrations may underestimate the effect of rifampicin on DOAC exposure. Antiseizure medications that are cytochrome P450 and P-glycoprotein inducers are commonly used with DOACs. Several studies have observed a correlation between the concomitant use of DOACs and enzyme-inducing antiseizure medications and DOAC treatment failure, for example, ischemic and thrombotic events. The European Society of Cardiology recommends avoiding this combination, as well as the combination of DOACs with levetiracetam and valproic acid, owing to a risk of low DOAC concentrations. However, levetiracetam and valproic acid are not cytochrome P450 or P-glycoprotein inducers, and the implications of their use with DOACs remain to be elucidated. Our comparative analysis suggests DOAC plasma concentration monitoring as a possible strategy to guide dosing owing to the predictable correlation between DOACs’ plasma concentration and effect. Patients taking concomitant enzyme-inducing antiseizure medications are at risk for low DOAC concentrations and subsequently, treatment failure and thus can benefit from DOAC concentration monitoring to prophylactically identify this risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Co-medication of direct oral anticoagulants (DOACs) and enzyme-inducing antiseizure medications is associated with low DOAC plasma concentrations and treatment failure. |
The effect of rifampicin on the area under the concentration–time curve of rivaroxaban and apixaban was greater than the effect on their peak concentration. Thus, DOACs’ peak concentration measurement is likely to underestimate the true impact of enzyme-inducing antiseizure medications on the exposure of DOACs. |
Co-medication of DOACs and levetiracetam or valproic acid has been associated with higher rates of thrombotic events despite the fact that these drugs are not enzyme-inducing antiseizure medications. Further studies are required to evaluate these interactions. |
Thresholds for DOAC plasma concentrations have yet to be determined to guide DOAC therapeutic drug monitoring in patients co-medicated with enzyme-inducing antiseizure medications and DOACs. We suggest that therapeutic drug monitoring-based dose adjustments can help in the safe and effective treatment of patients. |
1 Introduction
Direct oral anticoagulants (DOACs) have largely replaced vitamin K antagonists (VKAs) for the prevention of ischemic stroke in patients with atrial fibrillation and in the treatment and prevention of venous thromboembolism (VTE) [1, 2]. Compared with VKAs, DOACs have a more favorable safety profile (presumably because of a more predictable dose–response relationship), a smaller food effect, and fewer drug–drug interactions (DDIs), resulting in a lower risk of intracranial bleeding as compared with VKAs. Therefore, unlike VKAs that require routine coagulation monitoring (international normalized ratio), DOACs provide greater safety as well as convenience of treatment and an improved adherence to therapy [3, 4].
2 DOAC Pharmacokinetic (PK) Profiles
The following DOACs are approved by the US Food and Drug Administration and European Medicines Agency: dabigatran, rivaroxaban, apixaban, and edoxaban. Betrixaban is approved in the USA only for the prophylaxis of VTE in adult patients with a special risk for thromboembolic complications, and therefore, less data are available for comparison. Although DOACs have fewer DDIs than VKAs, they still have significant PK DDIs that may substantially impact their plasma concentrations and effects. As most of the clinically relevant DDIs are PK [5], a comparative analysis of the PK profile of each individual DOAC is critical for predicting its DDIs with other concomitantly administered medications (Table 1).
There are considerable differences in the reported oral bioavailability of the individual DOACs: dabigatran: 3–7%, rivaroxaban: 66–100%, apixaban: 50%, edoxaban: 62% and betrixaban: 32%. While the bioavailability of a drug is affected by numerous factors, P-glycoprotein (P-gp) transport has a significant influence on DOAC bioavailability. In addition, the elimination pathways of the individual DOACs vary as follows.
2.1 Dabigatran
Dabigatran per se is not orally absorbed. Consequently, it is marketed as a prodrug (dabigatran etexilate) that is metabolically hydrolyzed by hepatic non-specific esterases to the parent compound. Twenty percent of the absorbed dose is metabolized through non-cytochrome P450 (CYP)-mediated pathways, while more than 80% is excreted, mostly unchanged in the urine [6].
2.2 Rivaroxaban
About 50% of the absorbed rivaroxaban dose is metabolized in the liver, primarily by CYP2J2 and CYP3A4/5 and the formed metabolites are excreted in urine (30%) and feces (21%), while about 35% is excreted unchanged in urine by transporter-mediated processes [7].
2.3 Apixaban
About 50% of the absorbed apixaban dose is metabolized in the liver, primarily by CYP3A4, while the rest is excreted (unchanged) in urine. Apixaban metabolites are then excreted mostly in feces with a small percentage of metabolites excreted in urine [8].
2.4 Edoxaban
Approximately 24% of the absorbed edoxaban dose is metabolized in the liver, primarily by carboxylesterase 1-mediated hydrolysis, and to a lesser extent via CYP3A4. About 50% of the absorbed dose is excreted unchanged in urine [9].
2.5 Betrixaban
About 80% of the absorbed dose of betrixaban is eliminated from the body by hepatobiliary metabolic hydrolyses without CYP involvement, while 20% is excreted unchanged in urine [10]. In summary, all DOACs undergo P-gp-dependent absorption and renal excretion. Rivaroxaban, apixaban, and edoxaban undergo CYP-mediated metabolism. This P-gp-dependent absorption and/or their CYP-mediated metabolism provides the basis for many of their clinically relevant PK DDIs due to induction and/or inhibition of CYPs and/or P-gp-mediated processes.
3 DOAC DDIs
Drug interactions are common among elderly patients taking DOACs especially when polypharmacy is present, and the ramifications of toxicity or inefficacy are grave.
The DOAC PK drug interactions in the elderly include the interaction between DOACs and other substrates of P-gp and/or CYP3A4 such as statins. Specifically, simvastatin, atorvastatin, and lovastatin have been hypothesized to compete with DOAC metabolism, thereby possibly leading to increased DOAC concentrations. However, PK studies in healthy subjects did not find any changes in DOAC concentrations with these concurrent medications [11, 12]. Retrospective studies have analyzed the statin effect on DOAC concentrations [13, 14] and effects [14,15,16] with mixed findings. Thus, we conclude that no special precautions would seem necessary for the concurrent use of statins and DOACs.
In addition to PK interactions, DOACs have significant pharmacodynamic interactions that may be clinically relevant in the elderly. For example, a well-known pharmacodynamic mechanism of DDIs that may increase the bleeding risk in patients treated with DOACs is the antiplatelet activity of medications such as selective serotonin reuptake inhibitors and selective norepinephrine reuptake inhibitors as well as non-steroidal anti-inflammatory drugs [17,18,19]. In a retrospective cohort study, typical and atypical antipsychotics were also associated with an increased bleeding risk when co-administered with DOACs compared with patients taking DOACs without antipsychotics [20]. However, the cohorts compared were significantly different at baseline. Specifically, a considerable difference between mean HAS-BLED scores was reported, reflecting a baseline bleeding risk that was higher among patients taking antipsychotics as compared with patients who were not. The observed increased bleeding risk can be a result of differences in comorbidities between patients taking antipsychotics as compared with patients who were not, and not a result of DOAC-neuroleptic interactions.
4 Rifampicin and DOACs: PK Interaction
Cytochrome P450 and/or P-gp inducers increase the metabolism/transport of CYP and/or P-gp substrates, resulting in a variable reduction in DOAC plasma concentrations and clinical effect. Co-administration of rifampicin, a probe drug for CYP and P-gp induction, has been associated with a decrease in plasma exposures (area under the concentration–time curve [AUC]) of dabigatran, rivaroxaban, apixaban, and edoxaban [21,22,23,24,25]. The magnitude of the decline in DOACs’ AUC differs according to the CYP-mediated fraction metabolized and the extent of their P-gp-mediated transport as depicted in Table 2.
When rifampicin was concomitantly administered to healthy subjects, it reduced the AUC of dabigatran [21], apixaban [23], rivaroxaban [22], and edoxaban [24] by 67%, 54%, 49%, and 34%, respectively. The similar (about 50%) decrease in the AUC of rivaroxaban and apixaban is consistent with their similar metabolic and elimination pathways. Edoxaban exhibited the smallest decrease in AUC (34%), consistent with its relatively minor CYP-mediated metabolism. The decrease in AUC of these drugs was due to an increase in their oral clearance, while no effect was reported on their rates of absorption.
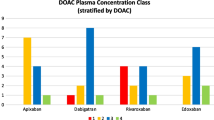
For apixaban and rivaroxaban and also for edoxaban, rifampicin had a greater effect on AUC than on Cmax. This can be explained by the dual induction of their P-gp-mediated transport and CYP-mediated metabolism [5] (Fig. 1).
Magnitude of the effect of rifampicin (expressed percentage change compared to baseline) on direct oral anticoagulants’ plasma exposure (area under the concentration–time curve [AUC]) and peak concentration (Cmax). The difference between the effect of rifampicin on direct oral anticoagulants’ AUC and Cmax varies according to the extent of the cytochrome P450-mediated fraction metabolized (fm) and, consequently, its largest effect is on rivaroxaban and apixaban and its smallest effect is on dabigatran. The whiskers depict the standard error (SE) in the magnitude of the effect of rifampicin on the various DOACs
For dabigatran, which undergoes extensive P-gp-mediated transport and no CYP-mediated metabolism, rifampicin reduced the AUC and Cmax of dabigatran in healthy subjects by 67% and 65.5%, respectively. Its poor oral bioavailability (3–7%) coupled with P-gp-dependent absorption resulted in similar reductions in AUC and Cmax after rifampicin administration. [21, 25].
5 Established ASMs and DOACs
Like rifampicin, the established antiseizure medications (ASMs) carbamazepine, phenytoin, phenobarbital, and primidone are potent inducers of CYPs and P-gp [26,27,28]. Therefore, these ASMs are likely to decrease DOAC plasma concentrations and exposure and, consequently, their clinical effect. While low DOAC concentrations likely contribute to a long-term stroke and VTE risk, other factors including epilepsy per se and enzyme-inducing ASM (EI-ASM) have also exhibited atherogenic effects even without a co-administered DOAC [29, 30].
In a retrospective study, concomitant treatment of DOAC and EI-ASMs was associated with low apixaban concentrations. In this study, the odds for subtherapeutic apixaban plasma concentrations were more than six-fold higher amongst patients co-treated with an EI-ASM compared with patients not treated with an EI-ASM. A similar trend was observed with rivaroxaban and dabigatran [31].
Concomitant administration of EI-ASMs with DOACs at the recommended dosage has been proposed as a potential cause of DOAC treatment failure, clinically manifested as stroke and recurrent VTE [32,33,34,35,36,37,38]. Several case reports describe clinical anticoagulant treatment failure in patients co-treated with an EI-ASM and with apixaban [32,33,34], rivaroxaban [35,36,37], and dabigatran [38]. Low DOAC plasma concentrations in these co-medicated patients were reported in some cases [32,33,34,35].
A study using the Food and Drug Administration Adverse Event Reporting System also found that concomitant use of EI-ASMs and DOACs was associated with a 86% increase in the proportion of reports involving failure of anticoagulation therapy, i.e., ischemic and thromboembolic events [39]. A large database study that included almost 90,000 patients co-treated with DOACs and ASMs confirmed earlier findings that phenytoin and carbamazepine were significantly associated with an increased risk of DOAC treatment failure with odds ratios (ORs) and 95% confidence intervals (95% CIs) of 4.46 (2.46–8.08), and 2.15 (1.07–4.30), respectively. Unexpectedly, this study found that levetiracetam and valproic acid, two ASMs that are not known to be CYP3A4/P-gp inducers, were significantly associated with the risk of DOAC treatment failure with OR (95% CI) values of 2.26 (1.13–4.54) and 2.38 (1.37–4.12), respectively [40]. Anticipated and reported clinical drug interactions between ASMs and DOACs are presented in Table 3.
6 Reports on Interactions Between DOACs and Non-EI-ASMs Levetiracetam and/or Valproic Acid
The explanation for the reported increased risk of DOAC treatment failure in patients co-medicated with DOACs and levetiracetam or DOACs and valproic acid is currently unknown [40]. This propensity score-matched, nested case-control study was limited by a few patients taking levetiracetam (83 patients), the possibility of an imbalance in baseline covariates, and the number of statistical comparisons performed. Levetiracetam is one of the well-tolerated drugs for post-stroke epilepsy [41], and such an indication may therefore be associated with an intrinsic recurrent stroke risk in these patients. In a stratified analysis of a recent population-based cohort study with a larger levetiracetam sample (398 patients), patients with epilepsy taking DOACs did not have an increased risk of thromboembolism with levetiracetam [42]. Previous animal studies have explored the possibility of P-gp induction by levetiracetam [43]; however, clinical studies did not confirm these findings [44, 45]. A recent case report suggested that levetiracetam initiation was associated with a reduction in rivaroxaban concentration, though a re-challenge was not performed [46]. A placebo-controlled DDI study in healthy subjects examined the effect of repeated administration of levetiracetam on the pharmacokinetics of the P-gp substrate, digoxin. Levetiracetam did not affect digoxin’s AUC, Cmax, and trough concentration, indicating that levetiracetam does not induce P-gp formation [45].
Other studies have measured the concentration of 4β-hydroxycholesterol, an endogenous marker of CYP3A4/5 activity, to examine the possibility of CYP3A4 induction by levetiracetam and valproic acid. 4β-Hydroxycholesterol concentrations were significantly increased, as much as ten-fold in one study, in patients treated with EI-ASMs as compared with patients treated with levetiracetam or valproic acid. Consequently, the authors concluded that levetiracetam and valproic acid are not likely to be significant inducers of CYP3A4/5 activity [47,48,49].
Pharmacodynamic mechanisms have also been explored to explain a possible interaction between levetiracetam and valproic acid use and DOAC failure. The association between levetiracetam and valproic acid use (irrespective of DOAC use) and the risk of ischemic stroke has been explored. A population-based matched case-control study including 22,271 patients treated with ASMs found no significant association between ischemic stroke and the use of ASMs when they were pooled together (OR = 1.06; 95% CI 0.998–1.128). However, the specific ASMs, levetiracetam and valproic acid were significantly associated with an increased ischemic stroke risk with the following OR (95% CI) values: levetiracetam 4.1 (3.3–5.2) and valproic acid 1.4 (1.1–1.9) [50]. Another large pharmaco-epidemiological study in a cohort of 252,407 patients treated with ASMs also did not find an independently increased risk of ischemic stroke with the use of EI-ASMs or valproic acid compared with all other ASMs including levetiracetam. This study did not differentiate between the various ASMs, thus the individual risk of ischemic stroke with each drug was not evaluated [51]. Whether the clinical use of levetiracetam or valproic acid per se increases the risk of stroke is yet to be determined.
7 Current Clinical Guidelines for the Management of DOAC-EI-ASM DDIs
Current recommendations warn against the concomitant use of apixaban, rivaroxaban, edoxaban, or dabigatran together with EI-ASMs. The European Society of Cardiology regards concomitant medication of valproic acid and DOACs as a contraindication and warns that the use of levetiracetam with DOACs may be associated with an increased risk for DOAC treatment failure, potentially because currently there are insufficient data on the concurrent use of levetiracetam with DOACs. [17]
Switching from a DOAC to a VKA or replacing the EI-ASM are two possible strategies to circumvent the clinically relevant DOAC-EI-ASM interaction. However, both may have considerable drawbacks. Switching from a DOAC to a VKA may be associated with foregoing DOACs’ main safety advantage, i.e., a lower risk of intracranial bleeding as compared with VKAs and foregoing their enhanced convenience [1, 3, 4]. As a result, many patients may be reluctant to switch from DOACs to VKAs, despite the above recommendations.
Replacing an effective EI-ASM with a non-EI-ASM is another potential strategy to avoid the DOAC-EI-ASM interaction; however, this may result in a considerable risk of recurrent seizures in an epileptic patient with previously controlled seizures. Levetiracetam, specifically, and valproic acid have been suggested as potentially safer combinations with DOACs for antiseizure treatment in patients requiring anticoagulation [44, 52, 53]; however, they were also significantly associated with the risk of DOAC treatment failure in a large retrospective cohort study [40]. Valproic acid was also associated with increased mortality with and without co-administered DOACs [42, 54].
8 DOAC Concentration Monitoring in Patients Co-Medicated with EI-ASM?
Direct oral anticoagulant plasma concentration monitoring is currently recommended in patients who require an urgent invasive procedure (e.g., following orthopedic trauma), in patients experiencing bleeding, or in patients with a suspected overdose [17]. DOAC concentration measurement (or calibrated AntiXa assay) may also be considered in patients with acute stroke who received a DOAC dose within 48 hours but would otherwise be candidates for tissue plasminogen activator treatment [55].
Previous studies are not consistent in determining a concentration–effect relationship for DOACs [56]. A correlation between low DOAC concentrations and DOAC treatment failure has been suggested in previous reports [57, 58]. A study with apixaban for the treatment or prevention of recurrent VTE observed that the predicted median steady-state peak and trough concentrations and their corresponding anti-Factor Xa activity were quantitatively higher in patients with bleeding and lower for those with thrombotic events compared with subjects without any event. Nevertheless, the range of plasma exposure in the patients with efficacy and safety endpoints was entirely contained within the range of plasma exposure of those without events [59].
In a study on VTE prevention in subjects undergoing orthopedic surgery, a significant association was observed between individual steady-state AUC and any bleeding endpoint. Additionally, in patients after a total knee replacement and total hip replacement surgery, a two-fold increase in apixaban daily AUC was associated with an increased predicted bleeding probability from 6.18 to 7.25% and from 9.32 to 10.9%, respectively [60].
In a post hoc analysis of the ENGAGE‐AF trial in which warfarin was compared with edoxaban at a standard dose (60 mg once daily) or a low dose (30 mg once daily), low edoxaban trough concentrations were associated with a higher risk of stroke and systemic embolism while high trough values were associated with a higher risk of major bleeding [61].
Various other factors can affect DOAC concentrations including adherence to therapy, extreme weight or body mass index, pharmacogenomics, and specific heart conditions that may predispose patients to DOAC failure. Thus, a possible strategy to reduce the risk of drug toxicity and DOAC treatment failure is the utilization of therapeutic drug monitoring (TDM), as clinical efficacy in general correlates better with drug plasma concentrations than with oral dosages [5]. Therapeutic drug monitoring has been advocated particularly in situations of suspected PK DDIs and other situations such as when a treatment is preventive, when there are no surrogate markers for a drug effect, and subsequently when therapeutic failure can have drastic consequences. [62,63,64,65].
The TDM approach has been successfully adopted for numerous medications to optimize their efficacy and safety when PK DDIs were clinically relevant. Monitoring the international normalized ratio with warfarin treatment is a prime example of a personalized dose adjustment when the dose–effect relationship is variable and unpredictable, as occurs in the presence of DDI or drug–food interactions. Similarly, monitoring DOAC plasma concentrations may allow patients taking concomitant EI-ASMs to be treated safely and effectively with DOACs.
Several challenges in adopting a TDM-based approach need to be addressed [63]. For most other drugs, trough concentrations are used for TDM because of less variability and likelihood to be influenced by absorption and distribution issues [66]. Furthermore, Cmax as an empirical single-point PK metric is susceptible to intra-subject variability and is influenced by the frequency of blood sampling [5]. In addition to other disadvantages, using Cmax to monitor DOAC concentrations in clinical practice may underestimate the effect of potent enzyme inducers on apixaban and rivaroxaban. Therapeutic drug monitoring of DOACs will stipulate determining appropriate sample timing and establishing a therapeutic concentration range for each individual DOAC.
In addition, several uncertainties may limit the practicality of the TDM approach and require further discussion. First, the degree of DOAC concentration reduction that may put a patient at risk for treatment failure is still unknown. While high concetrations correlate with higher rates of bleeding events and low concentrations with VTE and ischemic stroke, no cut-off values have been suggested. Second, reference ranges that have been published differ based on population differences including ethnicity, DOAC dose, and renal function, complicating the determination of a single therapeutic range for all patients. Last, a large observational study paradoxically found some EI-ASMs associated with bleeding when used concomittantly with DOACs [67]. Increased safety events may be explained by a higher bleeding baseline risk, though increasing the dosage based on TDM will need to address this issue as well.
9 Conclusions and Future Directions
Concomitant treatment of a DOAC with an EI-ASM can result in reduced DOAC concentrations [31], and potentially severe clinical consequences including systemic embolism, stroke, or recurrent VTE [39, 40]. In such cases, the lack of a monitoring practice becomes a shortcoming. Therapeutic drug monitoring-based dose adjustments in patients concomitantly treated with DOACs and EI-ASMs can reduce the risk of treatment failure associated with low DOAC concentrations.
The smaller effect of rifampicin on the Cmax of rivaroxaban and apixaban compared with the effect on their AUCs may have important clinical implications. In current practice, DOAC exposure is often measured by Cmax. In addition to other disadvantages, this practice may underestimate the effect of rifampicin on DOAC plasma exposure, especially on exposures of rivaroxaban and apixaban [21,22,23,24], and thus underestimate the effect of rifampicin on the efficacy and safety of DOACs. The difference between rifampicin effects on Cmax and AUC points towards a need to evaluate the usefulness of DOAC trough concentration as a measure for TDM, which is common practice in TDM [66, 68].
Further studies are required to determine whether DOACs’ TDM will allow patients taking EI-ASMs to be treated safely and effectively with DOACs. This approach requires adopting reliable and valid TDM assays and protocols as well as educating physicians on how to interpret the results. Currently, DOAC plasma concentration measurement is available for clinical practice in many institutions, but not in all. The most commonly used method for determination of DOAC concentration is based on a calibrated coagulation test (Factor Xa for apixaban, edoxaban, and rivaroxaban, diluted thrombin time for dabigatran) [68, 69]. The application of DOACs’ TDM in such cases depends on developing and applying validated methods for DOAC plasma concentration measurement [69].
Therapeutic drug monitoring-based clinical decisions require physicians to understand the mechanism of PK drug interactions. For example, an induction-based DDI is observed within 2–3 weeks of initiation of an EI-ASM. Similarly, enzyme de-induction following the discontinuation of an inducer is also gradual and can take about 2 weeks. If TDM of DOACs is performed before maximum induction is reached or before the induction completely wears off, it may give misleading results and consequently erroneous decisions on DOAC therapy [62, 70].
It may be reasonable to examine the clinical usefulness of potential plasma concentration thresholds to guide DOAC dosage adjustment in prospective studies. Such studies will also examine the magnitude of the DOAC dose increase required in these patients.
Prospective controlled studies are warranted to evaluate the possible interactions between levetiracetam or valproic acid and DOACs and their clinical implications. While DOACs concentration thresholds have not yet been determined, the efficacy and safety of DOACs have proven to be concentration dependent. Though DOAC doses are predefined, patients may benefit from a personalized dose adjustment based on individual PK variation.
References
Yao X, Abraham NS, Sangaralingham LR, Bellolio MF, McBane RD, Shah ND, et al. Effectiveness and safety of dabigatran, rivaroxaban, and apixaban versus warfarin in nonvalvular atrial fibrillation. J Am Heart Assoc. 2016;5:e003725. https://doi.org/10.1161/JAHA.116.003725.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST Guideline and Expert Panel report. Chest. 2016;149:315–52.
Pundi KN, Perino AC, Fan J, Schmitt S, Kothari M, Szummer K, et al. Direct oral anticoagulant adherence of patients with atrial fibrillation transitioned from warfarin. J Am Heart Assoc. 2021;10: e020904.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Derendorf H, Schmidt S, Rowland M, Tozer TN. Rowland and Tozer’s clinical pharmacokinetics and pharmacodynamics: concepts and applications. 5th ed. Philadelphia: Wolters Kluwer; 2020.
US Food and Drug Administration. Pradaxa prescribing information. 2010. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022512s000lbl.pdf. Accessed 20 Nov 2022.
US Food and Drug Administration. Xarelto prescribing information. 2011. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202439s000lbl.pdf. Accessed 20 Nov 2022.
US Food and Drug Administration. Eliquis prescribing information. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202155s000lbl.pdf. Accessed 20 Nov 2022.
US Food and Drug Administration. Savaysa prescribing information. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206316lbl.pdf. Accessed 20 Nov 2022.
Center for Drug Evaluation and Research. FDA betrixaban clinical pharmacology and biopharmaceutics review. DRUGS@FDA data files. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/208383Orig1s000ClinPharmR.pdf. Accessed 20 Nov 2022.
Kubitza D, Becka M, Roth A, Mueck W. Absence of clinically relevant interactions between rivaroxaban—an oral, direct Factor Xa inhibitor—and digoxin or atorvastatin in healthy subjects. J Int Med Res. 2012;40:1688–707.
Mendell J, Zahir H, Matsushima N, Noveck R, Lee F, Chen S, et al. Drug-drug interaction studies of cardiovascular drugs involving P-glycoprotein, an efflux transporter, on the pharmacokinetics of edoxaban, an oral factor Xa inhibitor. Am J Cardiovasc Drugs. 2013;13:331–42.
Škorňová I, Samoš M, Bolek T, Stančiaková L, Vádelová Ľ, Galajda P, et al. Does atorvastatin therapy change the anti-Xa activity in xabans-treated patients with atrial fibrillation? Pharmacol Res Perspect. 2021;9: e00730.
Soh XQ, Tan DS-Y, Chan ECY. Simvastatin, but not atorvastatin, is associated with higher peak rivaroxaban serum levels and bleeding: an Asian cohort study from Singapore. Cardiovasc Drugs Ther. 2022. https://doi.org/10.1007/s10557-022-07346-8.
Wu H-H, Chang S-H, Lee T-H, Tu H-T, Liu C-H, Chang T-Y. Concurrent use of statins decreases major bleeding and intracerebral hemorrhage in non-valvular atrial fibrillation patients taking direct oral anticoagulants: a nationwide cohort study. Front Cardiovasc Med. 2022;9: 969259.
Chang S-H, Chou I-J, Yeh Y-H, Chiou M-J, Wen M-S, Kuo C-T, et al. Association between use of non-vitamin K oral anticoagulants with and without concurrent medications and risk of major bleeding in nonvalvular atrial fibrillation. JAMA. 2017;318:1250.
Steffel J, Collins R, Antz M, Cornu P, Desteghe L, Haeusler KG, et al. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. EP Europace. 2021;23:1612–76.
Chang K-H, Chen C-M, Wang C-L, Tu H-T, Huang Y-T, Wu H-C, et al. Major bleeding risk in patients with non-valvular atrial fibrillation concurrently taking direct oral anticoagulants and antidepressants. Front Aging Neurosci. 2022;14: 791285.
Bellia A, Della-Morte D, Di Daniele N, Lauro D. Drug interactions of direct oral anticoagulants in elderly patients with cardiometabolic diseases. Curr Res Pharmacol Drug Discov. 2021;2: 100029.
Chen C-M, Chang K-H, Wang C-L, Tu H-T, Huang Y-T, Wu H-C, et al. Major bleeding risk in atrial fibrillation patients co-medicated with non-vitamin K oral anticoagulants and antipsychotics. Front Pharmacol. 2022;13: 819878.
Härtter S, Koenen-Bergmann M, Sharma A, Nehmiz G, Lemke U, Timmer W, et al. Decrease in the oral bioavailability of dabigatran etexilate after co-medication with rifampicin: rifampicin decreases oral bioavailability of dabigatran etexilate. Br J Clin Pharmacol. 2012;74:490–500.
Center for Drug Evaluation and Research. FDA rivaroxaban clinical pharmacology biopharmaceutics review. DRUGS@FDA data files. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/022406Orig1s000ClinPharmR.pdf. Accessed 19 Oct 2022.
Vakkalagadda B, Frost C, Byon W, Boyd RA, Wang J, Zhang D, et al. Effect of rifampin on the pharmacokinetics of apixaban, an oral direct inhibitor of Factor Xa. Am J Cardiovasc Drugs. 2016;16:119–27.
Mendell J, Chen S, He L, Desai M, Parasramupria DA. The effect of rifampin on the pharmacokinetics of edoxaban in healthy adults. Clin Drug Investig. 2015;35:447–53.
Foerster KI, Hermann S, Mikus G, Haefeli WE. Drug–drug interactions with direct oral anticoagulants. Clin Pharmacokinet. 2020;59:967–80.
US Food and Drug Administration, FDA. Drug development and drug interactions. Table of substrates, inhibitors and inducers. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers. Accessed 19 Oct 2022.
US Food and Drug Administration. Clinical drug interaction studies: cytochrome P450 enzyme- and transporter-mediated drug interactions guidance for industry. 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-drug-interaction-studies-cytochrome-p450-enzyme-and-transporter-mediated-drug-interactions. Accessed 19 Oct 2022.
Patsalos PN, Perucca E. Clinically important drug interactions in epilepsy: interactions between antiepileptic drugs and other drugs. Lancet Neurol. 2003;2:473–81.
Josephson CB, Wiebe S, Delgado-Garcia G, Gonzalez-Izquierdo A, Denaxas S, Sajobi TT, et al. Association of enzyme-inducing antiseizure drug use with long-term cardiovascular disease. JAMA Neurol. 2021;78:1367.
Chang C-S, Liao C-H, Lin C-C, Lane H-Y, Sung F-C, Kao C-H. Patients with epilepsy are at an increased risk of subsequent stroke: a population-based cohort study. Seizure. 2014;23:377–81.
Perlman A, Goldstein R, Choshen Cohen L, Hirsh-Raccah B, Hakimian D, Matok I, et al. Effect of enzyme-inducing antiseizure medications on the risk of sub-therapeutic concentrations of direct oral anticoagulants: a retrospective cohort study. CNS Drugs. 2021;35:305–16.
King PK, Stump TA, Walkama AM, Ash BM, Bowling SM. Management of phenobarbital and apixaban interaction in recurrent cardioembolic stroke. Ann Pharmacother. 2018;52:605–6.
Cole JL. Enzymatic deinduction phenomenon and clinical implications with a focus on direct-acting oral anticoagulants. Blood Coagul Fibrinolysis. 2020;31:283–6.
Di Gennaro L, Lancellotti S, De Cristofaro R, De Candia E. Carbamazepine interaction with direct oral anticoagulants: help from the laboratory for the personalized management of oral anticoagulant therapy. J Thromb Thrombolysis. 2019;48:528–31.
Stöllberger C, Finsterer J. Recurrent venous thrombosis under rivaroxaban and carbamazepine for symptomatic epilepsy. Neurol Neurochir Pol. 2017;51:194–6.
Burden T, Thompson C, Bonanos E, Medford AR. Lesson of the month 2: pulmonary embolism in a patient on rivaroxaban and concurrent carbamazepine. Clin Med. 2018;18:103–5.
Risselada AJ, Visser MJ, van Roon EN. Pulmonary embolism due to interaction between rivaroxaban and carbamazepine. Ned Tijdschr Geneeskd. 2013;157:A6568.
Hager N, Bolt J, Albers L, Wojcik W, Duffy P, Semchuk W. Development of left atrial thrombus after coadministration of dabigatran etexilate and phenytoin. Can J Cardiol. 2017;33:554.e13-554.e14.
Perlman A, Wanounou M, Goldstein R, Choshen Cohen L, Singer DE, Muszkat M. Ischemic and thrombotic events associated with concomitant Xa-inhibiting direct oral anticoagulants and antiepileptic drugs: analysis of the FDA Adverse Event Reporting System (FAERS). CNS Drugs. 2019;33:1223–8.
Gronich N, Stein N, Muszkat M. Association between use of pharmacokinetic-interacting drugs and effectiveness and safety of direct acting oral anticoagulants: nested case-control study. Clin Pharmacol Ther. 2021;110:1526–36.
Werhahn KJ, Trinka E, Dobesberger J, Unterberger I, Baum P, Deckert-Schmitz M, et al. A randomized, double-blind comparison of antiepileptic drug treatment in the elderly with new-onset focal epilepsy. Epilepsia. 2015;56:450–9.
Ip BY, Ko H, Wong GL, Yip TC, Lau LH, Lau AY, et al. Thromboembolic risks with concurrent direct oral anticoagulants and antiseizure medications: a population-based analysis. CNS Drugs. 2022;36:1313–24.
Moerman L, wyffels L, Slaets D, Raedt R, Boon P, De Vos F. Antiepileptic drugs modulate P-glycoproteins in the brain: a mice study with 11C-desmethylloperamide. Epilepsy Res. 2011;94:18–25.
Mathy F-X, Dohin E, Bonfitto F, Pelgrims B. Drug-drug interaction between levetiracetam and non-vitamin K antagonist anticoagulants. Eur Heart J. 2019;40:1571.
Levy RH, Ragueneau-Majlessi I, Baltes E. Repeated administration of the novel antiepileptic agent levetiracetam does not alter digoxin pharmacokinetics and pharmacodynamics in healthy volunteers. Epilepsy Res. 2001;46:93–9.
Paciullo F, Costa C, Gresele P. Rivaroxaban plasma levels and levetiracetam: a case report. Ann Intern Med. 2020;173:71–2.
Hole K, Wollmann BM, Nguyen C, Haslemo T, Molden E. Comparison of CYP3A4-inducing capacity of enzyme-inducing antiepileptic drugs Using 4β-hydroxycholesterol as biomarker. Ther Drug Monit. 2018;40:463–8.
Gjestad C, Huynh DK, Haslemo T, Molden E. 4β-Hydroxycholesterol correlates with dose but not steady-state concentration of carbamazepine: indication of intestinal CYP3A in biomarker formation? Br J Clin Pharmacol. 2016;81:269–76.
Bodin K, Bretillon L, Aden Y, Bertilsson L, Broomé U, Einarsson C, et al. Antiepileptic drugs increase plasma levels of 4β-hydroxycholesterol in humans. J Biol Chem. 2001;276:38685–9.
Giner-Soriano M, Marsal JR, Gomez-Lumbreras A, Morros R. Risk of ischaemic stroke associated with antiepileptic drugs: a population-based case-control study in Catalonia. BMC Neurol. 2021;21:208.
Renoux C, Dell’Aniello S, Saarela O, Filion KB, Boivin J-F. Antiepileptic drugs and the risk of ischaemic stroke and myocardial infarction: a population-based cohort study. BMJ Open. 2015;5: e008365.
von Oertzen TJ, Trinka E, Bornstein NM. Levetiracetam and non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation and epilepsy: a reasonable combination. Eur Heart J. 2019;40:3800–1.
Kurt S, Sumbul O, Aksoy D. Combination of non-vitamin K antagonist oral anticoagulants and antiepileptic drugs. Eur Heart J. 2019;40:1572.
Sarycheva T, Lavikainen P, Taipale H, Tiihonen J, Tanskanen A, Hartikainen S, et al. Antiepileptic drug use and mortality among community-dwelling persons with Alzheimer disease. Neurology. 2020;94:e2099–108.
Hughes RE, Tadi P, Bollu PC. TPA therapy. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK482376/. Accessed 24 Oct 2022.
Toorop MMA, Lijfering WM, Scheres LJJ. The relationship between DOAC levels and clinical outcomes: the measures tell the tale. J Thromb Haemost. 2020;18:3163–8.
Macha K, Marsch A, Siedler G, Breuer L, Strasser EF, Engelhorn T, et al. Cerebral ischemia in patients on direct oral anticoagulants: plasma levels are associated with stroke severity. Stroke. 2019;50:873–9.
Testa S, Paoletti O, Legnani C, Dellanoce C, Antonucci E, Cosmi B, et al. Low drug levels and thrombotic complications in high-risk atrial fibrillation patients treated with direct oral anticoagulants. J Thromb Haemost. 2018;16:842–8.
Byon W, Sweeney K, Frost C, Boyd R. Population pharmacokinetics, pharmacodynamics, and exploratory exposure-response analyses of apixaban in subjects treated for venous thromboembolism: subjects treated for venous thromboembolism. CPT Pharmacometrics Syst Pharmacol. 2017;6:340–9.
Leil TA, Frost C, Wang X, Pfister M, LaCreta F. Model-based exposure-response analysis of apixaban to quantify bleeding risk in special populations of subjects undergoing orthopedic surgery. CPT Pharmacometrics Syst Pharmacol. 2014;3: e136.
Ruff CT, Giugliano RP, Braunwald E, Morrow DA, Murphy SA, Kuder JF, et al. Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes: an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 trial. Lancet. 2015;385:2288–95.
Johannessen Landmark C, Johannessen SI, Patsalos PN. Therapeutic drug monitoring of antiepileptic drugs: current status and future prospects. Expert Opin Drug Metab Toxicol. 2020;16:227–38.
Landmark CJ, Johannessen SI, Tomson T. Dosing strategies for antiepileptic drugs: from a standard dose for all to individualised treatment by implementation of therapeutic drug monitoring. Epileptic Disord. 2016;18:367–83.
Kahan BD, Keown P, Levy GA, Johnston A. Therapeutic drug monitoring of immunosuppressant drugs in clinical practice. Clin Ther. 2002;24:330–50.
Tod MM, Padoin C, Petitjean O. Individualising aminoglycoside dosage regimens after therapeutic drug monitoring: simple or complex pharmacokinetic methods? Clin Pharmacokinet. 2001;40:803–14.
Winter ME. Basic clinical pharmacokinetics. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2004.
Wang CL, Wu VC-C, Chang K-H, Tu H-T, Kuo C-F, Huang Y-T, et al. Assessing major bleeding risk in atrial fibrillation patients concurrently taking non-vitamin K antagonist oral anticoagulants and antiepileptic drugs. Eur Heart J Cardiovasc Pharmacother. 2020;6:147–54.
Van der Linden L, Hias J, Vanassche T. The value and limitations of new oral anticoagulant plasma level assessments. Eur Heart J Suppl. 2022;24:A32-41.
Drouet L, Bal dit Sollier C, Steiner T, Purrucker J. Measuring non-vitamin K antagonist oral anticoagulant levels: when is it appropriate and which methods should be used? Int J Stroke. 2016;11:748–58.
Brodie MJ, Mintzer S, Pack AM, Gidal BE, Vecht CJ, Schmidt D. Enzyme induction with antiepileptic drugs: cause for concern? Enzyme induction with AEDs Epilepsia. 2013;54:11–27.
Stangier J. Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate. Clin Pharmacokinet. 2008;47:285–95.
European Medicines Agency. Eliquis: EPAR product Iiformation. https://www.ema.europa.eu/en/documents/product-information/eliquis-epar-product-information_en.pdf. Accessed 20 Nov 2022.
Candeloro M, Eikelboom JW, Chan N, Bhagirath V, Douketis JD, Schulman S. Carbamazepine, phenytoin, and oral anticoagulants: drug-drug interaction and clinical events in a retrospective cohort. Res Pract Thromb Haemost. 2022;6: e12650.
Laureano M, Crowther M, Eikelboom J, Boonyawat K. Measurement of dabigatran drug levels to manage patients taking interacting drugs: a case report. Am J Med. 2016;129:e247–8.
Perlman A, Hochberg-Klein S, Choshen Cohen L, Dagan G, Hirsh-Raccah B, Horwitz E, et al. Management strategies of the interaction between direct oral anticoagulant and drug-metabolizing enzyme inducers. J Thromb Thrombolysis. 2019;47:590–5.
Sennesael A-L, Larock A-S, Hainaut P, Lessire S, Hardy M, Douxfils J, et al. The impact of strong inducers on direct oral anticoagulant levels. Am J Med. 2021;134:1295–9.
Giustozzi M, Mazzetti M, Paciaroni M, Agnelli G, Becattini C, Vedovati MC. Concomitant use of direct oral anticoagulants and antiepileptic drugs: a prospective cohort study in patients with atrial fibrillation. Clin Drug Investig. 2021;41:43–51.
Chin PKL, Wright DFB, Zhang M, Wallace MC, Roberts RL, Patterson DM, et al. Correlation between trough plasma dabigatran concentrations and estimates of glomerular filtration rate based on creatinine and cystatin C. Drugs R D. 2014;14:113–23.
Dagan G, Perlman A, Hochberg-Klein S, Kalish Y, Muszkat M. Managing direct oral anticoagulants in patients with antiepileptic medication. Can J Cardiol. 2018;34(1534):e1-3.
Wiggins BS, Northup A, Johnson D, Senfield J. Reduced anticoagulant effect of dabigatran in a patient receiving concomitant phenytoin. Pharmacotherapy. 2016;36:e5-7.
Sáez-Torres de Vicente M, Martínez Puig P, Valverde Toresano L. Ischemic stroke due to possible interaction of rivaroxaban with primidone in a patient with atrial fibrillation. Med Clin (Barc). 2021;156:255–6.
Robinson ZS, Arvin JP, Madding KL. Rivaroxaban failure in a patient taking oxcarbazepine. Ann Pharmacother. 2021;55:1302–3.
Serra W, Li Calzi M, Coruzzi P. Left atrial appendage thrombosis during therapy with rivaroxaban in elective cardioversion for permanent atrial fibrillation. Clin Pract. 2015;5. http://www.clinicsandpractice.org/index.php/cp/article/view/788. Accessed 1 Oct 2020.
Barbar S, Simonetto M, De Bon E, Scarano L, Caneve G, Simioni N. Direct oral anticoagulants and antiepileptic drugs: is there room for concurrent treatment? [abstract]. Res Pract Thromb Haemost. 2020. https://abstracts.isth.org/abstract/direct-oral-anticoagulants-and-antiepileptic-drugs-is-there-room-for-concurrent-treatment. Accessed 17 Jan 2023.
Stöllberger C, Finsterer J. Prolonged anticoagulant activity of rivaroxaban in a polymorbid elderly female with non-convulsive epileptic state. Heart Lung. 2014;43:262–3.
Langenbruch L, Meuth SG, Wiendl H, Mesters R, Möddel G. Clinically relevant interaction of rivaroxaban and valproic acid: a case report. Seizure. 2020;80:46–7.
Acknowledgments
This work is abstracted from the Ph.D. thesis of Rachel Goldstein in partial fulfillment of the Ph.D. degree requirements for The Hebrew University of Jerusalem. Meir Bialer (meirb@ekmd.huji.ac.il) and Mordechai Muszkat (muszkatm@hadassah.org.il) are co-corresponding authors for the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was funded by a research grant from the Estates Committee, Israel Ministry of Justice (proposal submitted to the Chief Scientist, Ministry of Health) to Mordechai Muszkat 2021–2024.
Conflicts of Interest
Meir Bialer received speaker’s or consultancy fees from Alkaloid, Boehringer Ingelheim, Clexio Bioscines, Guidepoint, Pharma Two B, Rekah-Vitamed, USWorldMeds, and Xenon Pharma. Rachel Goldstein, Aviya R. Jacobs, Lana Zighan, Naomi Gronich, and Mordechai Muszkat have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
RG, ARJ, LZ, NG, and MM produced an initial draft of the manuscript and conducted a literature search under guidance and supervision from MB and MM. RG, MB, and MB contributed to a critical evaluation of the data and to the revision and finalization of the manuscript. All authors have read and approved the final version of the manuscript, and agree to be accountable for the work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goldstein, R., Jacobs, A.R., Zighan, L. et al. Interactions Between Direct Oral Anticoagulants (DOACs) and Antiseizure Medications: Potential Implications on DOAC Treatment. CNS Drugs 37, 203–214 (2023). https://doi.org/10.1007/s40263-023-00990-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-00990-0