Abstract
Background
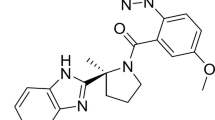
Daridorexant (ACT-541468) is a potent dual orexin receptor antagonist under development for the treatment of sleep disorders. Concomitant intake of ethanol and hypnotics has been shown to result in additive/supra-additive depression of the central nervous system, resulting in pronounced sedation.
Objective
The aim of this study was to evaluate the pharmacokinetic (PK) and pharmacodynamic (PD) interactions between ethanol and daridorexant.
Method
This was a single-center, double-blind, placebo-controlled, randomized, four-way crossover study conducted in 19 healthy male/female subjects. Subjects received the following four treatments: ethanol with daridorexant, daridorexant alone, ethanol alone, and placebo. Daridorexant 50 mg and the matching placebo were administered as single oral tablets. Ethanol was infused intravenously and clamped at a level of 0.6 g/L for 5 h. The PK of ethanol and daridorexant were assessed and a battery of PD tests performed.
Results
Concomitant administration of ethanol prolonged the time to reach maximum plasma concentrations (tmax) of daridorexant (median difference 1.25 h). No other relevant PK interactions were observed. Coadministration with ethanol produced a numerically greater impairment on saccadic peak velocity, body sway, visual analog scale (VAS) alertness, VAS alcohol intoxication, smooth pursuit, and adaptive tracking compared with daridorexant alone. All treatments were generally well tolerated without serious adverse events (AEs). The most commonly reported treatment-emergent AEs following coadministration of daridorexant and ethanol included somnolence, headache, fatigue, sudden onset of sleep, and dizziness.
Conclusions
Apart from a shift in tmax, no relevant changes in PK parameters were observed following coadministration of daridorexant and ethanol. The coadministration led to reinforced drug actions that were, at most, indicative of infra-additive effects on certain PD markers. Patients will be advised not to consume ethanol with daridorexant.
Clinical Trials Registration number:
NCT03609775 (ClinicalTrials.gov Identifier)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The pharmacokinetics of daridorexant were not affected following coadministration with ethanol (and vice versa), apart from a prolonged time to reach maximum plasma concentration (tmax) of daridorexant (by approximately 75 min). |
Administration of daridorexant as well as of ethanol alone showed their respective characteristic effects on the central nervous system. |
Compared with being administered alone, coadministration of daridorexant and ethanol led to an amplification of drug effects on several of the performed pharmacodynamic tests; however, these were less pronounced than the sum of the effects of each individual agent. Patients will be advised not to consume ethanol while being treated with daridorexant. |
All adverse events of moderate intensity occurred following ethanol infusion (i.e., alone or following coadministration with daridorexant). |
1 Introduction
Daridorexant (ACT-541468) is a new potent and selective compound being evaluated for the treatment of insomnia that blocks the actions of the orexin neuropeptides at both orexin-1 and orexin-2 receptors, i.e., a dual-orexin receptor antagonist (DORA) [1, 9, 10]. Across the dose range of 5–50 mg, the pharmacokinetic (PK) profile of daridorexant is characterized by quick absorption and elimination, with a median time to reach maximum concentration (tmax) of 1–2 h and a geometric mean (GM) terminal half-life (t½) of approximately 6 h. Daridorexant is extensively metabolized, with only traces of parent drug excreted unchanged in feces and urine, and most observed metabolic reactions were cytochrome P450 (CYP) 3A4-mediated oxidative transformations [2, 3]. With respect to drug–drug interactions, daridorexant has been determined as a CYP3A4 substrate, lacking any perpetrator interaction potential towards CYP3A4 or breast cancer resistance protein (BCRP) in humans [4, 5]. By selectively targeting wake-promoting regions in the brain not projecting into cerebral fine control regions such as the cerebellum or vestibular nuclei, DORAs are thought to reduce the impairment of cognitive performance, locomotor skills, and balance, commonly observed with γ-aminobutyric acid (GABA)A receptor modulators [6,7,8]. Based on the accumulated data from the comprehensive phase I program, daridorexant has further advanced in development following two phase II studies that showed a desired effect on sleep onset and sleep maintenance as well as a significant dose–response relationship, and is currently being further explored clinically in the phase III program (ClinicalTrials.gov identifiers: NCT03545191, NCT03575104, NCT03679884) [2, 3, 5, 9,10,11,12].
Ethanol is one of the most widely used central nervous system (CNS) active substances in Western society and causes impairment of a wide range of CNS functions, including alertness, motor stability, and hand–eye coordination [13, 14]. Previous studies have shown that ethanol intake enhances the function of the GABAA receptor, which is the same ionotropic receptor protein complex targeted by benzodiazepines and non-benzodiazepines (e.g. zolpidem, zopiclone), whereby they unfold their hypnotic/sedative properties [15,16,17,18,19,20]. It is well known that insomnia, which affects approximately 30% or more of the general population, is associated with increased use of ethanol as self-prescribed medication [21,22,23,24,25]. Although the sedating effects of ethanol may promote the shortening of sleep onset latency, this form of self-medication is rarely successful as it leads to a deterioration of sleep quality and thereby exacerbates the issue [26]. A systematic review of prevalence of concomitant use of ethanol and sedative-hypnotic drugs in middle-and older-aged persons has shown that up to 88% of men and 79% of women who used sedative hypnotics also consumed ethanol, and that 28% thereof were concomitant users of sedative hypnotics [27]. Studies with GABAA receptor agonists showed that the concomitant intake of ethanol can result in additive pharmacodynamic (PD) effects, i.e., enhanced sedative effects and/or psychomotor impairment (as measured in performance skills and greater self-rated sleepiness) [15,16,17,18, 28,29,30,31,32]. Moreover, there is also evidence for the co-occurrence of ethanol and benzodiazepine consumption with accident-related injuries (e.g. traffic accidents, falls, work- or sports-related injuries) [33,34,35]. Consequently, the effects of coadministration with ethanol need to be studied during the development of a new drug to treat insomnia in order to understand the clinical significance of the potential PD interactions with ethanol [26, 36, 37].
Although most ethanol interaction studies are performed after oral administration, herein a 10% w/v ethanol solution in 5% glucose was administered intravenously for 5 h and fixed (clamped) to a blood level of 0.6 g/L. The intravenous clamping method allows for precise control of ethanol blood levels and also eliminates the complex absorption PK of ethanol associated with oral administration, as ethanol absorption can be highly variable [14, 38]. Another advantage is the absence of smell and taste associated with oral ethanol ingestion, which can lead to unblinding of subjects. A constant ethanol blood level of 0.6 g/L has been shown to be associated with significant CNS effects without causing too many inadvertent events, leaving enough room for further CNS impairment without compromising safety, in case of an additive or supra-additive drug–ethanol interaction [38,39,40]. An ethanol level of 0.6 g/L is just above the legal driving limit in many European countries and just below the legal driving limit of 0.8 g/L in the United States, and is habitually achieved during social drinking [41, 42]. An interaction study utilizing such a clamping model that assures accurate target concentrations in all subjects has strong clinical relevance and has previously been used to evaluate the combined effects with ethanol of a variety of different compounds [16, 43].
The aim of this study was to investigate potential PK and PD interactions, i.e., effects on alertness, motor coordination, and cognitive functions, between ethanol (clamped at a blood level of 0.6 g/L for 5 h) and daridorexant (50 mg), the highest clinically relevant dose assessed in the aforementioned phase III program for a suitable investigation of its potential interaction with ethanol.
2 Methods
2.1 Study Design
This was a single-center, double-blind, randomized, placebo-controlled, double-dummy, 2 × 2 factorial design, four-way crossover phase I study (ClinicalTrials.gov identifier: NCT03609775) conducted at the Centre for Human Drug Research (CHDR), Leiden, The Netherlands. The study was approved by the National Health Authority of The Netherlands (Centrale Commissie Mensgebonden Onderzoek [CCMO]) and by the local ethics committee (Stichting Beoordeling Ethiek Biomedisch Onderzoek [BEBO]). The study adhered to the Declaration of Helsinki and was conducted according to good clinical practice guidelines and applicable laws and regulations in The Netherlands. Prior to any study procedure, written informed consent was obtained from each participant after adequate explanation of the objectives, methods, and potential hazards of the study. The study was funded by Idorsia Pharmaceuticals Ltd, who also provided the study medication.
2.2 Study Population
The study population included eligible healthy female and male subjects aged 18–45 years, with a body mass index (BMI) of between 18 and 32 kg/m2 (inclusive) and non-smokers. Subjects were in good health, as determined on the basis of medical history, physical examination, clinical laboratory tests, and 12-lead electrocardiogram (ECG) at screening, as well as negative results from urine drug screen and breath ethanol test at screening and on day 1 predose. All study participants were familiar with the effects of ethanol. Subjects with a history of drug abuse or alcoholism, defined as an average ethanol consumption of more than 14 or 21 units of ethanol per week or an average daily intake of more than 2 or 3 units (1 ethanol unit = 8 g or 10 mL of pure ethanol, i.e., typical drinks may contain 1–3 units of ethanol), for female and male subjects, respectively, were excluded. Furthermore, subjects of Asian descent or other individuals reporting ethanol intolerance (e.g. flushing) were also excluded from the study. No concomitant medication was allowed during the course of the study, except for hormonal contraception in females and for the treatment of adverse events (AEs).
2.3 Treatments
Twenty-two healthy female and male subjects were enrolled and subsequently received four treatments, i.e., (A) ethanol with daridorexant; (B) daridorexant alone; (C) ethanol alone; and (D) placebo, in a blinded crossover fashion (Fig. 1). Each subject was randomized to one of the treatment sequences defined using a Williams design balanced for first-order carryover effects. Allocation of the treatments to the design square was randomized for every block of four subjects. Subjects were assigned to one of four sequences in accordance with the randomization schedule generated by an independent Contract Research Organization (Aixial s.r.o., Brno, Czech Republic) prior to the first study treatment administration, using SAS® software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Daridorexant 50 mg or matching placebo were administered orally as single dose tablets. Ethanol (10% w/v in 5% glucose) or matching placebo was infused intravenously through an indwelling catheter, started 30 min prior to daridorexant/placebo administration, and clamped for 5 h at a level of 0.6 g/L. Each treatment was followed by an observation period of 24 h. Ethanol clamping was performed as previously described [38, 39, 43]. Ethanol was administered intravenously using calibrated Graseby (model 3000, Watford, UK) volumetric infusion pumps. To prevent local pain, a parallel infusion with glucose 5% was administered for 10 min at the beginning of the infusion using calibrated Graseby (model 3200) syringe pumps. The infusion rate for the first and second 5-min interval was determined for each subject individually (before the start of the infusion) based on a level of ethanol clamping of 0.6 g/L and on the individual’s demographic data, i.e., weight, height, age, and sex, entered in the clamping spreadsheet according to the Watson estimate of body water [44]. The clamping spreadsheet was subsequently used online to set the infusion rate after each breath ethanol measurement during the ethanol infusion (based on the actual measured breath ethanol concentration (BrEC) at predetermined time intervals, as previously described [38, 45]. Thereby, after the loading phase, a constant ethanol blood level of 0.6 g/L was maintained during a 4.5 h plateau phase. For the matching placebo (5% glucose solution), a sham procedure was used, i.e., predefined results were entered into the clamping spreadsheet and the infusion rate was adapted accordingly. With this procedure, approximately 1 L of either treatment was infused over a 5-h time period.
Study design. Treatment A (daridorexant with ethanol); Treatment B (daridorexant alone); Treatment C (ethanol alone); Treatment D (placebo). * Screening took place between Day –28 and Day –10 for women of childbearing potential and between Day –21 and Day –3 for the other subjects. **There was a washout period of 6–14 days between study treatment administrations. EOT End-of Treatment, EOS End-of-Study, PD Pharmacodynamic, PK Pharmacokinetic
2.4 Pharmacokinetics
Blood samples (4 mL) for the measurement of daridorexant were collected in EDTA tubes and obtained immediately prior to the start of the ethanol/placebo infusion and at 10 and 20 min and 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 12, and 24 h after drug intake (Fig. 1). Plasma daridorexant concentrations were determined using a previously described validated liquid chromatography coupled with tandem mass spectrometry (LC–MS/MS) assay following protein precipitation (with acetonitrile containing the internal standard [IS], i.e., deuterated ACT-541468 [ACT-541468D]) with a limit of quantification (LOQ) of 0.5 ng/mL and covering a range up to 2000 ng/mL [3]. Mass spectrometric detection was performed using a triple quadrupole tandem mass spectrometer (API4000; AB Sciex, Concord, ON, Canada) operating in a positive electrospray ionization mode. Samples were quantified using peak area ratios. ACT-541468 and ACT-541468D transitions, i.e., parent m/z > fragment m/z were 451.2 > 202.0 amu and 455.2 > 206.0 amu, respectively. The inter- and intra-assay accuracy was between 2.3 and 4.0% and − 8.3 and 12.0%, respectively, and the inter- and intra-assay precision was ≤ 8.4% and ≤ 9.9%, respectively. Measurements of BrEC were performed at intervals of 5–30 min using calibrated hand-held Alco-Sensor VXL meters (Honac, Apeldoorn, The Netherlands). The range of the meter was from 0.01 to 4.0 g/L. The accuracy of the breath ethanol test is dependent on the relationship between the concentrations of ethanol in blood and deep lung breath; this ratio of 2300:1 is well established [46]. The Alco-Sensor VXL meter measures the BrEC and displays the derived ethanol blood level calculated with a ratio of 2300:1, which is reported herein.
The PK parameters of daridorexant were obtained by non-compartmental analysis using Phoenix WinNonlin version 6.4 (Pharsight Corporation, Mountain View, CA, USA). The measured individual plasma concentration was used to directly obtain maximum plasma concentration (Cmax) and tmax. Area under the plasma concentration–time curve (AUC) from time zero to infinity (AUC∞) was calculated by combining AUC from zero to time t of the last measured concentration above the LOQ (AUCt) according to the linear trapezoidal rule and AUC representing an extrapolated value obtained by Ct/λz (AUCextra), where Ct was the last plasma concentration measured above the LOQ and λz represented the terminal elimination rate constant determined by log-linear regression analysis of the measured plasma concentrations of the terminal elimination phase. The t½ of daridorexant was calculated as follows: t½ = ln(2)/λz. Concentrations that were below the LOQ were entered as zero and included as such in the calculation of means.
2.5 Pharmacodynamics
PD were assessed on day 1 in all four treatment periods prior to the start of the ethanol/placebo infusion, and 0.5, 1, 2, 3, 4, 5, 6, 8, and 10 h after daridorexant/placebo administration using a battery of validated tests (NeuroCart®, CHDR, Leiden, The Netherlands), including the objective psychomotor performance tests saccadic peak velocity (SPV), adaptive tracking, the 2-min body sway test, and the subjective VAS Bond and Lader to evaluate alertness, mood, and calmness (Fig. 1). In addition, two further PD tests were performed that have previously been shown to be sensitive to ethanol administration, namely the smooth pursuit eye movement task and the VAS alcohol intoxication score [39, 43].
The SPV measurement was performed as previously described [3, 47, 48]. The recording of eye movements was performed in a quiet room with ambient lighting, while head movements were restrained using a fixed head support. The target consisted of a moving red dot that was displayed on a computer screen. For SPV, the target switched from left to right (15 degrees to either side), with interstimulus intervals varying randomly between 3 and 6 s, whereas the target drifted smoothly and sinusoidally to either side for the smooth pursuit assessment. The time in which the eyes were in smooth pursuit of the target was calculated for each frequency and was expressed as a percentage of stimulus duration.
The adaptive tracking test is a pursuit-tracking task in which a circle is moving randomly on a screen. The subject had to try to keep a dot inside the moving circle by operating a joystick [3, 43, 47,48,49,50,51].
Postural stability/body sway was assessed while subjects were asked to stand with a string attached to their waist, similar to the previously described Wright ataxia meter, keeping their eyes closed [3, 48, 52]. All body movements in the anteroposterior direction over a period of 2 min were recorded as millimeter sway.
The 16-item VAS of Bond and Lader was used to subjectively assess the effects of the different treatments on alertness, mood, and calmness, while the subjects regularly rated their current perceived ethanol effects on a 10 cm horizontal VAS, which asked the subjects how large the effect of ethanol was that they were feeling [39, 53,54,55].
All subjects were familiarized with the PD assessments during a training session, which took place within 3 weeks prior to the start of the first treatment phase to minimize learning effects.
2.6 Safety Variables
In addition to the broad range of CNS tests performed, safety and tolerability were evaluated based on supine vital sign measurement, 12-lead ECG, physical examination, assessing standard blood chemistry and hematology laboratory variables, and monitoring of AEs at predefined time points pre- and postdose.
2.7 Statistical Analyses
A sample size of 20 subjects was determined to provide 80% power to detect an ethanol effect in differences in means for the smooth pursuit test as well as an ethanol or daridorexant effect in differences in means for adaptive tracking, VAS alertness, body sway, and SPV. However, a study population of 19 was sufficient to observe the effects in question. SAS® software, version 9.4 (SAS Institute Inc.) was used for the statistical analysis and the reporting of clinical and PK data. The effects of ethanol on daridorexant PK were analyzed by mixed-effect models, with treatment and period as fixed effects and subject as random effect. The effects of ethanol on AUC∞, Cmax, and t½ of daridorexant were explored using the geometric means ratio (GMR) and its 90% confidence interval (CI), with daridorexant as the reference for the comparison of ethanol with daridorexant versus daridorexant alone. Differences between treatments for tmax were explored using the median differences and their 90% CI.
To assess a potential difference in mean ethanol blood levels between ethanol alone and ethanol with daridorexant over the infusion time, individual blood ethanol concentration–time data were analyzed by mixed-model analyses of variance (ANOVAs), with treatment, time, and treatment by time as fixed factors, and subject, subject by time, and subject by treatment as random factors. The difference in total ethanol dose between ethanol alone and ethanol with daridorexant was analyzed by mixed-model ANOVAs, with treatment as a fixed factor and subject as a random factor.
The PD endpoints were analyzed separately by mixed-model ANOVAs, with treatment, period, time, and treatment by time as fixed effects, with subject as a random effect, and with the (average) baseline value as a covariate. The mean of the four baselines (i.e., mean of the baselines of each treatment) was used as the average baseline. Missing PD values due to drug effect were imputed to the lowest/highest value of the respective treatment. Least square means (LSM) estimates over time, by treatment, were presented with 95% CIs. Treatment effects were analyzed as the contrasts between placebo and the different study treatments. Variables were initially analyzed without transformation, but if the data had suggested otherwise (data were not normally distributed), log-transformation would have been applied.
An additive drug–drug interaction is thought to be present if the combined effect of two independent agents corresponds to the expected sum of the effects of the two individual agents. Supra-additive effects (defined as effects, resulting from coadministration of two independent agents, being greater than the sum of effects of each individual agent) as well as infra-additive effects (defined as the combined effect of two independent agents being smaller than the expected sum of effects of each individual agent) were evaluated by analyzing the contrast of the effects of the coadministration of daridorexant and ethanol with subtraction of the effects of daridorexant alone versus the effects of ethanol alone with subtraction of the effects of placebo [40, 56]:
Thereby, if the difference in treatments was shown to be of statistical significance in the ANOVA linear mixed model for the contrast of treatments (A–B) vs. (C–D), then the absolute values of the contrast between treatments were used to evaluate whether a supra-additive effect, i.e., a value greater in magnitude for |(A–B)| compared with |(C–D)|, or an infra-additive effect, i.e., a value greater in magnitude for |(C–D)| compared with |(A–B)|, was evident. To adjust for multiple comparisons, a Bonferroni correction was applied to the ANOVA linear mixed model evaluating the contrast of treatments (A–B) versus (C–D) of the eight PD variables, resulting in a local significance level of 0.05/8 = 0.00625 for each single PD variable.
3 Results
3.1 Subjects
Nineteen subjects completed the study as per protocol. One subject withdrew from the study due to reasons unrelated to the study treatments, while two subjects were excluded from the PK/PD data sets due to major protocol deviations, i.e., one subject vomited 1 min after study drug administration and another subject was excluded due to implausible concentrations of daridorexant determined in plasma, i.e., after clinical conduct was completed. Treatment order was therefore not affected by the exclusion of subjects. Baseline demographics are summarized in Table 1.
3.2 Pharmacokinetics
3.2.1 Daridorexant
In the absence of ethanol, the plasma concentration–time profile of daridorexant was characterized by rapid absorption and disposition, with a GM Cmax of 1348 ng/mL (95% CI 1133–1604) attained at a median tmax of 1.5 h (Fig. 2a; Table 2). The GM of total exposure (AUC∞) was 10,287 ng·h/mL (95% CI 7810–13,550) and t½ was 7.94 h (95% CI 6.60–9.55). There were no relevant effects of ethanol on daridorexant exposure, with only the shift in tmax observed when daridorexant was administered together with ethanol (median difference 1.25 h, 90% CI 0.51–1.78) compared with the administration of daridorexant alone being of statistical significance (p <0.05).
a Arithmetic mean (± SD) plasma daridorexant concentration versus time profiles in healthy subjects (n = 19) after a single dose of 50 mg alone (Treatment B) or in combination with ethanol 0.6 g/L (Treatment A). b Arithmetic mean (± SD) blood ethanol concentration versus time profiles in healthy subjects (n = 19) after ethanol infusion for 5 h alone (Treatment C) and in combination with a single-dose administration of daridorexant 50 mg (Treatment A). SD standard deviation
3.2.2 Ethanol
Following intravenous infusion of ethanol to ascertain a blood level of 0.6 g/L, with or without daridorexant, BrEC increased rapidly and remained constant for the duration of the infusion. After infusion stop, BrEC declined rapidly following the characteristic zero-order kinetics of ethanol elimination (Fig. 2b). At 5.5 h after ending the ethanol infusion (10 h after daridorexant dosing), i.e., the last time point of measurement, BrEC was no longer measurable.
The ethanol dose (required to maintain the 0.6 g/L ethanol clamp), in the absence of daridorexant, for the 5 h duration of the infusion was 61.3 g (GM, 95% CI 56.7–66.3). Daridorexant did not alter the total dose of ethanol required to maintain the 0.6 g/L clamp compared with ethanol administered alone (GMR 1.00, 90% CI 0.97–1.02).
3.3 Pharmacodynamics
3.3.1 Saccadic Eye Movements
SPV was reduced following administration of both daridorexant alone (B–D: p < 0.0001 [LSM −14.3 degrees/s]) (Table 3) and ethanol alone (C–D: p < 0.0001 [LSM − 19.2 degrees/s]) compared with placebo. When ethanol and daridorexant were administered together, the overall effect on mean SPV values was slightly more pronounced compared with either treatment administered alone (A–D: p < 0.0001 [LSM −26.0 degrees/s]) (Table 3). Regardless of treatment, mean SPV values returned to baseline 8 h after administration of daridorexant/placebo (Fig. 3a).
Mean change from baseline (± SD) in objective pharmacodynamic tests, by treatment and time, in healthy subjects (n = 19) after ethanol 0.6 g/L, a single dose of daridorexant 50 mg, daridorexant 50 mg in combination with ethanol 0.6 g/L, and placebo. (a) Saccadic peak velocity (degrees/s); (b) adaptive tracking (%); (c) body sway (mm/2 min); and (d) smooth pursuit (%). SD standard deviation, orange circle represents Treatment A (daridorexant with ethanol), blue square represents Treatment B (daridorexant alone), black up-pointing triangle represents Treatment C (ethanol alone), white down pointing triangle represents Treatment D (placebo), ash square represents duration of ethanol/placebo infusion (5 h), asterisk indicates predose assessment performed within 2 h prior to the start of the ethanol/placebo infusion
3.3.2 Adaptive Tracking
Adaptive tracking performance was reduced with daridorexant alone compared with placebo (B–D: p < 0.0001 [LSM − 5.19%]) [Table 3], while the reduction in adaptive tracking performance following ethanol alone was less pronounced than the effect observed with daridorexant alone (C–D: p < 0.0001 [LSM − 4.46%]). Daridorexant administered together with ethanol showed a longer (Fig. 3b) and more pronounced impairing effect on adaptive tracking performance when compared with either treatment alone (A–D: p < 0.0001 [LSM − 6.51%]). However, unlike the effect observed with daridorexant alone, the maximum mean adaptive tracking performance remained relatively constant and returned slowly to baseline, i.e., 8 h after administration (Fig. 3b). Furthermore, the contrast between treatments (|A–B|) versus treatments (|C–D|) was statistically significant (p < 0.0001 [LSM 3.04%]), with the magnitude of the mean value to be greater for treatments (|C–D|), indicative of an infra-additive effect, i.e., the combined effect of the two drugs being smaller than the expected sum of the two actions, following the coadministration of daridorexant and ethanol (Table 3).
3.3.3 Body Sway
Daridorexant alone compared with placebo showed an increase in body sway, with a mean maximal increase observed 1 h after daridorexant administration (B–D: p =0.0003 [LSM 106 mm/2 min]) (Table 3). Body sway was more pronounced following administration of ethanol alone compared with placebo, as well as compared with daridorexant alone (C–D: p < 0.0001 [LSM 113 mm/2 min]). The increase induced by the combination of both active treatments on body sway performance exceeded the response of each treatment alone (A–D: p < 0.0001 [LSM 195 mm/2 min]), but the contrast in treatments ([A–B]–[C–D]) did not reach a level of statistical significance (Table 3).
3.3.4 Smooth Eye Pursuit
An effect on smooth pursuit was not observed following administration of daridorexant alone (Fig. 3d), whereas smooth pursuit was considerably reduced following administration of ethanol alone (C–D: p < 0.0001 [LSM − 4.17%]) (Table 3) compared with placebo. Combined administration of daridorexant and ethanol on smooth pursuit was comparable with the administration of ethanol alone (A–D: p < 0.0001 [LSM − 2.98%]) [Table 3].
3.3.5 Visual Analog Scale (VAS) Bond and Lader for Alertness, Mood, and Calmness
VAS alertness was reduced following the administration of daridorexant alone (B–D: p < 0.0001 [LSM − 2.34 mm]) [Table 3] and ethanol alone (C–D: p < 0.0001 [LSM − 2.06 mm]) when compared with placebo. For both daridorexant alone and ethanol alone, alertness subscores returned to baseline at around the same time as observed under placebo treatment, i.e., 5.5 h after ethanol infusion was started (Fig. 4a). When ethanol and daridorexant were administered together, the effect on alertness was more pronounced compared with the effect of daridorexant alone (A–D: p < 0.0001 [LSM − 3.81 mm]). The values remained constant until the end of the ethanol infusion, after which the values slowly returned to baseline 10 h post dose (Fig. 4a).
Mean change from baseline (± SD) in subjective pharmacodynamic tests, by treatment and time, in healthy subjects (n = 19) after ethanol 0.6 g/L, a single dose of daridorexant 50 mg, daridorexant 50 mg in combination with ethanol 0.6 g/L, and placebo. VAS according to Bond and Lader for (a) alertness (%), (b) mood (%), (c) calmness (%), and (d) VAS for alcohol intoxication (mm). SD standard deviation, VAS visual analog scale, orange circle represents Treatment A (daridorexant with ethanol), blue square represents Treatment B (daridorexant alone), black up-pointing triangle represents Treatment C (ethanol alone), white down pointing triangle represents Treatment D (placebo), ash square represents duration of ethanol/placebo infusion (5 h), asterisk indicates predose assessment performed within 2 h prior to the start of the ethanol/placebo infusion
No clear pattern in the time course of VAS mood and calmness was observed across all treatments (Figs. 4b, c; Table 3).
3.3.6 VAS for Alcohol Intoxication
No treatment effects were observed on the self-reported alcohol intoxication score following the administration of either placebo or daridorexant alone (Table 3). Following ethanol alone, values of the alcohol intoxication score increased rapidly, with the mean maximum effect occurring 1 h after ethanol infusion start, i.e., 30 min after administration of daridorexant/placebo (Fig. 4d). The effect of daridorexant administered together with ethanol on the alcohol intoxication score was less pronounced and delayed (A–D: p < 0.0001 [LSM − 7.21 mm]) [Fig. 4d; Table 3], with a mean maximum effect occurring 2.5 h after ethanol infusion start (Fig. 4d), compared with the administration of ethanol alone (C–D: p < 0.0001 [LSM 9.43 mm]). Furthermore, the contrast between treatments (|A–B|) versus Treatments (|C–D|) was statistically significant and indicative of an infra-additive effect ([A–B]–[C–D]: p = 0.0014 [LSM − 4.31 mm]) [Table 3].
3.4 Safety and Tolerability
All four treatments were well tolerated, with no serious AEs (SAEs). In total, at least one treatment-emergent AE (TEAE) of mild or moderate intensity was reported by 21 subjects (95.5%) during the study. All TEAEs of moderate intensity occurred following ethanol infusion. The most frequently reported TEAEs were somnolence, headache, fatigue, sudden onset of sleep, dizziness, and feeling drunk (Table 4). Except for headache, these TEAEs tended to be more frequently reported on active treatment, most frequently following coadministration of ethanol and daridorexant. The TEAEs of feeling drunk, nausea, and infusion site pain were only reported following ethanol infusion, while the TEAEs of headache, sudden onset of sleep, and dizziness were reported for both active treatments, but more frequently following ethanol infusion. No clinically relevant effects following the administration of study treatments were detected on vital signs, ECG, and laboratory variables.
4 Discussion
This was a single-center, double-blind, randomized, placebo-controlled, double-dummy, four-way crossover, phase I study with the objective to investigate the PD and PK interaction of a single-dose administration of daridorexant 50 mg and constant ethanol blood level of 0.6 g/L in healthy male and female subjects. The 50 mg dose of daridororexant (previously evaluated in PK/PD phase I studies), while also being the highest dose administered in the ongoing phase III trials, was chosen as it allowed an appropriate investigation of the potential interaction with ethanol. In light of the widespread (mis)use of ethanol, particularly in insomnia patients, it was considered to be of importance for the safety of patients to understand whether the combined administration would lead to infra-additive, additive, or supra-additive effects [21,22,23,24].
The PK of a single oral dose of daridorexant 50 mg was within the expected inherent variability when compared with the PK observed in previous studies in healthy adults [3, 12]. There were no statistically significant effects of ethanol on the exposure to daridorexant, apart from a shift in tmax that was reached later when daridorexant was coadministered with ethanol. This matches the finding of previously performed ethanol interaction studies with DORAs, in which no relevant PK interactions were observed between either almorexant or suvorexant and ethanol, except for a similar prolongation of almorexant tmax (median difference 1.22 h) observed by Hoch et al. [43, 57]. The shift in tmax might be explained by a prolongation of gastric emptying after the intake of ethanol, as previously reported [58,59,60,61]. This was also thought to be the explanation for a shift in tmax and lag time observed in an interaction study whereby erythromycin was administered together with ethanol [62].
While the Cmax and AUC of daridorexant were unchanged after concomitant administration with ethanol, lemborexant, a recently approved DORA for the treatment of insomnia in adults, showed an increase in Cmax and AUC by approximately 1.3- and 1.7-fold, respectively, following concomitant intake of ethanol [63]. There was no effect of daridorexant on the total dose of ethanol required to maintain ethanol levels at 0.6 g/L for 5 h, and it did also not change the ethanol concentration versus time profile.
The PD measurements were assessed by the same battery of validated, objective, and subjective tests used in previous DORA studies [43, 50, 64], including daridorexant studies [3, 11, 12], and have been shown to be sensitive to various aspects of sedation in early studies of CNS drugs. Objective and subjective PD variables measured after morning administration of daridorexant showed effects consistent with a sleep-promoting compound [65]. In line with the reported PK profile of daridorexant, the most prominent treatment effects of daridorexant were observed at approximately 2 h postdose [3]. Daridorexant alone, compared with placebo, showed a decrease in SPV, adaptive tracking performance, and subjective alertness as assessed by VAS Bond and Lader. In addition, an increase in body sway was observed. Mood subscores and the VAS for alcohol intoxication showed no treatment effect for daridorexant alone versus placebo.
During the administration of ethanol alone, objective and subjective PD variables measured over 10.5 h following the start of the infusion showed the expected effects of ethanol on the CNS. Similar to findings reported by Hoch et al., ethanol alone, compared with placebo, showed a decrease in SPV, smooth pursuit, adaptive tracking performance, and VAS alertness [43]. Furthermore, an increase in body sway and VAS for alcohol intoxication was measured. Mood and calmness subscores of the VAS showed no treatment effect for ethanol alone versus placebo. However, during the VAS alcohol intoxication assessment, the effects seemed to decrease during the plateau phase of the ethanol clamp, with and without concomitant administration of daridorexant, which might be due to a rapid tolerance development in the study population familiar with the effects of ethanol, as previously described [39].
Daridorexant administered together with ethanol did not lead to marked differences compared with the administration of either daridorexant alone or ethanol alone for VAS mood and calmness. Similarly, coadministration did not further decrease smooth pursuit compared with ethanol alone. An infra-additive effect was observed for the adaptive tracking assessment following coadministration. Statistical evaluation for the VAS alcohol intoxication questionnaire was indicative of an infra-additive effect even though a common pharmacological effect was not evident, as daridorexant administration alone led to subjects stating they felt sober, whereas other subjects reported the opposite, i.e., feeling drunk, following administration of ethanol alone [56]. Additionally, coadministration led to a prolonged effect on SPV and VAS alertness, while a longer, enduring, more pronounced effect was observed for body sway.
A previous study investigating the coadministration of the marketed DORA suvorexant with ethanol showed pronounced effects on psychomotor performance, such as sustained attention/vigilance, working memory, and postural stability, while the combination of ethanol and suvorexant also further decreased subjective alertness (as measured by VAS Bond and Lader) compared with suvorexant alone [57]. The effects of suvorexant and ethanol were generally consistent with additive rather than supra-additive effects. It must be highlighted that the design of the suvorexant–ethanol interaction study differed substantially from the present study in terms of administration of ethanol. In the present study, ethanol was administered intravenously and hence it was possible to clamp the ethanol concentrations precisely at a constant blood level of 0.6 g/L for a duration of 5 h, whereas in the suvorexant study, a 0.7 g/kg ethanol solution (to achieve a target blood concentration of 0.08%, i.e., 0.8 g/L) was administered orally in a drinking glass. Thereby, the effects of ethanol were most pronounced after 2 h and slowly diminished thereafter. As the effects of ethanol are concentration- and time-dependent, the interpretation of results is considered to be more complex if blood levels change over time, especially in a study population familiar with the effects of ethanol consumption and where adaptation and/or tolerance may play a role.
In the previous study by Hoch et al., concomitant administration of almorexant and ethanol was assessed with an almost identical clamping study design and the same PD assessments [43]. Coadministration of almorexant and ethanol was associated with similar effects on the measured PD variables as was observed in the present study, although some of the observed reinforced effects therein were additive in nature, e.g. adaptive tracking performance, body sway, SPV, subjective alertness, and, possibly, calmness. Supra-additive effects were not detected following coadministration. Recently, coadministration of lemborexant with ethanol was shown to produce a numerically greater negative impact on body sway and memory compared with ethanol alone, with no supra-additive effects observed either [63].
Studies with GABAA receptor agonists show that coadministration of ethanol results in additive or even supra-additive impairing effects on the CNS, thus leading to pronounced sedation [15,16,17,18, 20, 30]. In contrast, the absence of additive or supra-additive effects in the current study suggest that ethanol and daridorexant exert their sedative and impairing psychomotor and cognitive effects by not directly interacting in a manner that might potentiate the effects of either drug administered alone .
In this study, TEAEs were consistent with those reported in previous daridorexant studies and the known safety profile of ethanol [2,3,4, 11, 12, 14, 39]. Single morning administration of daridorexant alone and in combination with ethanol was well tolerated, with no severe or serious AEs reported and no observed effects on clinical laboratory or ECG variables.
The applied ethanol clamping method has limitations with regard to the generalizability of our study results. In our study, we administered ethanol intravenously, while the relevant situation for daridorexant coadministrated with an oral alcoholic beverage was not evaluated. In addition, we clamped ethanol at blood concentrations of 0.06%, while (much) higher intoxication concentrations may be achieved in real life.
5 Conclusions
No relevant or unexpected changes in PK parameters were observed, apart from a shift in daridorexant tmax, following coadministration of daridorexant and ethanol. The reinforced drug actions observed following coadministration of daridorexant and ethanol on the evaluated PD battery were less than additive in nature, i.e., showed, at most, an infra-additive effect on certain PD markers. All treatments were generally well tolerated, with TEAEs such as headache and sudden onset of sleep reported more frequently following coadministration of ethanol and daridorexant, while no SAEs were reported. Based on the observed psychomotor effects, daridorexant should not be administered with ethanol, as is the case for other sleep medications.
References
Treiber A, de Kanter R, Roch C, Gatfield J, Boss C, von Raumer M, et al. The use of physiology-based pharmacokinetic and pharmacodynamic modeling in the discovery of the dual orexin receptor antagonist ACT-541468. J Pharmacol Exp Ther. 2017;362(3):489–503.
Muehlan C, Fischer H, Zimmer D, Aissaoui H, Grimont J, Boss C, et al. Metabolism of the dual orexin receptor antagonist ACT-541468, based on microtracer/accelerator mass spectrometry. Curr Drug Metab. 2019;20(4):254–65.
Muehlan C, Heuberger J, Juif PE, Croft M, van Gerven J, Dingemanse J. Accelerated development of the dual orexin receptor antagonist ACT-541468: integration of a microtracer in a first-in-human study. Clin Pharmacol Ther. 2018;104(5):1022–9.
Zenklusen I, Muehlan C, Ulc I, Liska J, Dingemanse J. The dual orexin receptor antagonist daridorexant does not affect the pharmacokinetics of the BCRP substrate rosuvastatin. Clin Exp Pharmacol Physiol. 2020. https://doi.org/10.1111/1440-1681.13370.
Boof ML, Alatrach A, Ufer M, Dingemanse J. Interaction potential of the dual orexin receptor antagonist ACT-541468 with CYP3A4 and food: results from two interaction studies. Eur J Clin Pharmacol. 2019;75(2):195–205.
Sakurai T, Nagata R, Yamanaka A, Kawamura H, Tsujino N, Muraki Y, et al. Input of orexin/hypocretin neurons revealed by a genetically encoded tracer in mice. Neuron. 2005;46(2):297–308.
Tannenbaum PL, Tye SJ, Stevens J, Gotter AL, Fox SV, Savitz AT, et al. Inhibition of orexin signaling promotes sleep yet preserves salient arousability in monkeys. Sleep. 2016;39(3):603–12.
Otmani S, Demazieres A, Staner C, Jacob N, Nir T, Zisapel N, et al. Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers. Hum Psychopharmacol. 2008;23(8):693–705.
Dauvilliers Y, Zammit G, Fietze I, Mayleben D, Seboek Kinter D, Pain S, et al. Daridorexant, a new dual orexin receptor antagonist to treat insomnia disorder. Ann Neurol. 2020;87(3):347–56.
Zammit G, Dauvilliers Y, Pain S, Sebok Kinter D, Mansour Y, Kunz D. Daridorexant, a new dual orexin receptor antagonist, in elderly subjects with insomnia disorder. Neurology. 2020;94(21):e2222–32.
Muehlan C, Boehler M, Brooks S, Zuiker R, van Gerven J, Dingemanse J. Clinical pharmacology of the dual orexin receptor antagonist ACT-541468 in elderly subjects: exploration of pharmacokinetics, pharmacodynamics and tolerability following single-dose morning and repeated-dose evening administration. J Psychopharmacol. 2020;34(3):326–35.
Muehlan C, Brooks S, Zuiker R, van Gerven J, Dingemanse J. Multiple-dose clinical pharmacology of ACT-541468, a novel dual orexin receptor antagonist, following repeated-dose morning and evening administration. Eur Neuropsychopharmacol. 2019;29(7):847–57.
Jang GR, Harris RZ. Drug interactions involving ethanol and alcoholic beverages. Expert Opin Drug Metab Toxicol. 2007;3(5):719–31.
Zoethout RW, Delgado WL, Ippel AE, Dahan A, van Gerven JM. Functional biomarkers for the acute effects of alcohol on the central nervous system in healthy volunteers. Br J Clin Pharmacol. 2011;71(3):331–50.
Hesse LM, von Moltke LL, Greenblatt DJ. Clinically important drug interactions with zopiclone, zolpidem and zaleplon. CNS Drugs. 2003;17(7):513–32.
van Steveninck AL, Gieschke R, Schoemaker HC, Pieters MS, Kroon JM, Breimer DD, et al. Pharmacodynamic interactions of diazepam and intravenous alcohol at pseudo steady state. Psychopharmacology. 1993;110(4):471–8.
van Steveninck AL, Gieschke R, Schoemaker RC, Roncari G, Tuk B, Pieters MS, et al. Pharmacokinetic and pharmacodynamic interactions of bretazenil and diazepam with alcohol. Br J Clin Pharmacol. 1996;41(6):565–73.
Hollister LE. Interactions between alcohol and benzodiazepines. Recent Dev Alcohol. 1990;8:233–9.
Siggins GR, Roberto M, Nie Z. The tipsy terminal: presynaptic effects of ethanol. Pharmacol Ther. 2005;107(1):80–98.
Lovinger DM, Roberto M. Synaptic effects induced by alcohol. Curr Top Behav Neurosci. 2013;13:31–86.
Johnson EO, Roehrs T, Roth T, Breslau N. Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep. 1998;21(2):178–86.
Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22(Suppl 2):S347–53.
Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Subst Abuse. 2005;26(1):1–13.
Goodhines PA, Gellis LA, Kim J, Fucito LM, Park A. Self-medication for sleep in college students: concurrent and prospective associations with sleep and alcohol behavior. Behav Sleep Med. 2019;17(3):327–41.
Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7–10.
Roehrs T, Roth T. Sleep, sleepiness, and alcohol use. Alcohol Res Health. 2001;25(2):101–9.
Ilomaki J, Paljarvi T, Korhonen MJ, Enlund H, Alderman CP, Kauhanen J, et al. Prevalence of concomitant use of alcohol and sedative-hypnotic drugs in middle and older aged persons: a systematic review. Ann Pharmacother. 2013;47(2):257–68.
Wilkinson CJ. The acute effects of zolpidem, administered alone and with alcohol, on cognitive and psychomotor function. J Clin Psychiatry. 1995;56(7):309–18.
Kuitunen T, Mattila MJ, Seppala T. Actions and interactions of hypnotics on human performance: single doses of zopiclone, triazolam and alcohol. Int Clin Psychopharmacol. 1990;5(Suppl 2):115–30.
Linnoila M, Stapleon JM, Lister R, Moss H, Lane E, Granger A, et al. Effects of adinazolam and diazepam, alone and in combination with ethanol, on psychomotor and cognitive performance and on autonomic nervous system reactivity in healthy volunteers. Eur J Clin Pharmacol. 1990;38(4):371–7.
Scavone JM, Greenblatt DJ, Harmatz JS, Shader RI. Kinetic and dynamic interaction of brotizolam and ethanol. Br J Clin Pharmacol. 1986;21(2):197–204.
Dorian P, Sellers EM, Kaplan HL, Hamilton C, Greenblatt DJ, Abernethy D. Triazolam and ethanol interaction: kinetic and dynamic consequences. Clin Pharmacol Ther. 1985;37(5):558–62.
Kurzthaler I, Wambacher M, Golser K, Sperner G, Sperner-Unterweger B, Haidekker A, et al. Alcohol and benzodiazepines in falls: an epidemiological view. Drug Alcohol Depend. 2005;79(2):225–30.
Kurzthaler I, Wambacher M, Golser K, Sperner G, Sperner-Unterweger B, Haidekker A, et al. Alcohol and/or benzodiazepine use: different accidents—different impacts? Hum Psychopharmacol. 2005;20(8):583–9.
Orriols L, Philip P, Moore N, Castot A, Gadegbeku B, Delorme B, et al. Benzodiazepine-like hypnotics and the associated risk of road traffic accidents. Clin Pharmacol Ther. 2011;89(4):595–601.
Sullivan SS, Guilleminault C. Emerging drugs for insomnia: new frontiers for old and novel targets. Expert Opin Emerg Drugs. 2009;14(3):411–22.
Neubauer DN. New and emerging pharmacotherapeutic approaches for insomnia. Int Rev Psychiatry. 2014;26(2):214–24.
Zoethout RW, van Gerven JM, Dumont GJ, Paltansing S, van Burgel ND, van der Linden M, et al. A comparative study of two methods for attaining constant alcohol levels. Br J Clin Pharmacol. 2008;66(5):674–81.
Zoethout RW, Schoemaker RC, Zuurman L, van Pelt H, Dahan A, Cohen AF, et al. Central nervous system effects of alcohol at a pseudo-steady-state concentration using alcohol clamping in healthy volunteers. Br J Clin Pharmacol. 2009;68(4):524–34.
te Beek ET, Zoethout RW, Bani MS, Andorn A, Iavarone L, Klaassen ES, et al. Pharmacokinetics and central nervous system effects of the novel dopamine D3 receptor antagonist GSK598809 and intravenous alcohol infusion at pseudo-steady state. J Psychopharmacol. 2012;26(2):303–14.
European Transport Safety Council (ETSC). Blood Alcohol Content (BAC) Drink Driving Limits across Europe. https://etsc.eu/blood-alcohol-content-bac-drink-driving-limits-across-europe. Accessed 4 Dec 2019.
Anderson P, Baumberg B. Alcohol in Europe—public health perspective: report summary. Drugs Educ Prev Policy. 2009;13(6):483–8.
Hoch M, Hay JL, Hoever P, de Kam ML, te Beek ET, van Gerven JM, et al. Dual orexin receptor antagonism by almorexant does not potentiate impairing effects of alcohol in humans. Eur Neuropsychopharmacol. 2013;23(2):107–17.
Watson PE, Watson ID, Batt RD. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am J Clin Nutr. 1980;33(1):27–39.
O’Connor S, Morzorati S, Christian J, Li TK. Clamping breath alcohol concentration reduces experimental variance: application to the study of acute tolerance to alcohol and alcohol elimination rate. Alcohol Clin Exp Res. 1998;22(1):202–10.
Mulder JA, Neuteboom W, Wessel RM. Breath alcohol legislation in The Netherlands. Blutalkohol. 1991;28(2):94–107.
van Steveninck AL, van Berckel BN, Schoemaker RC, Breimer DD, van Gerven JM, Cohen AF. The sensitivity of pharmacodynamic tests for the central nervous system effects of drugs on the effects of sleep deprivation. J Psychopharmacol. 1999;13(1):10–7.
Zuurman L, Roy C, Schoemaker RC, Hazekamp A, den Hartigh J, Bender JC, et al. Effect of intrapulmonary tetrahydrocannabinol administration in humans. J Psychopharmacol. 2008;22(7):707–16.
Borland RG, Nicholson AN. Visual motor co-ordination and dynamic visual acuity. Br J Clin Pharmacol. 1984;18(Suppl 1):69S–72S.
Hoever P, de Haas S, Winkler J, Schoemaker RC, Chiossi E, van Gerven J, et al. Orexin receptor antagonism, a new sleep-promoting paradigm: an ascending single-dose study with almorexant. Clin Pharmacol Ther. 2010;87(5):593–600.
de Haas SL, Schoemaker RC, van Gerven JM, Hoever P, Cohen AF, Dingemanse J. Pharmacokinetics, pharmacodynamics and the pharmacokinetic/pharmacodynamic relationship of zolpidem in healthy subjects. J Psychopharmacol. 2010;24(11):1619–29.
Wright BM. A simple mechanical ataxia-meter. J Physiol. 1971;218(Suppl):27–28P.
Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br J Med Psychol. 1974;47(3):211–8.
de Visser SJ, van der Post J, Pieters MS, Cohen AF, van Gerven JM. Biomarkers for the effects of antipsychotic drugs in healthy volunteers. Br J Clin Pharmacol. 2001;51(2):119–32.
Norris H. The action of sedatives on brain stem oculomotor systems in man. Neuropharmacology. 1971;10(21):181–91.
Bourgeois BFD. Antiepileptic drugs: combination therapy and interactions. Cambridge: Cambridge University Press; 2005.
Sun H, Yee KL, Gill S, Liu W, Li X, Panebianco D, et al. Psychomotor effects, pharmacokinetics and safety of the orexin receptor antagonist suvorexant administered in combination with alcohol in healthy subjects. J Psychopharmacol. 2015;29(11):1159–69.
Pfeiffer A, Hogl B, Kaess H. Effect of ethanol and commonly ingested alcoholic beverages on gastric emptying and gastrointestinal transit. Clin Investig. 1992;70(6):487–91.
Kasicka-Jonderko A, Jonderko K, Bozek M, Kaminska M, Mglosiek P. Potent inhibitory effect of alcoholic beverages upon gastrointestinal passage of food and gallbladder emptying. J Gastroenterol. 2013;48(12):1311–23.
Beck IT, Dinda PK. Acute exposure of small intestine to ethanol: effects on morphology and function. Dig Dis Sci. 1981;26(9):817–38.
Greenblatt DJ, Sahder RI, Weinberger DR, Allen MD, MacLaughlin DS. Effect of a cocktail on diazepam absorption. Psychopharmacology. 1978;57(2):199–203.
Morasso MI, Chavez J, Gai MN, Arancibia A. Influence of alcohol consumption on erythromycin ethylsuccinate kinetics. Int J Clin Pharmacol Ther Toxicol. 1990;28(10):426–9.
The Medical Letter. Lemborexant (Dayvigo) for insomnia. Med Lett Drugs Ther. 2020;62(1601):97–100.
Hoever P, de Haas SL, Dorffner G, Chiossi E, van Gerven JM, Dingemanse J. Orexin receptor antagonism: an ascending multiple-dose study with almorexant. J Psychopharmacol. 2012;26(8):1071–80.
Groeneveld GJ, Hay JL, Van Gerven JM. Measuring blood-brain barrier penetration using the NeuroCart, a CNS test battery. Drug Discov Today Technol. 2016;20:27–34.
Acknowledgments
The authors thank the study team at the CHDR (Leiden, The Netherlands) for the clinical conduct of this study; Radka Štěpánová (Aixial s.r.o., Brno, Czech Republic) for statistical analysis of the clinical data; and Susanne Globig (Department of Preclinical Pharmacokinetics and Metabolism, Idorsia Pharmaceuticals Ltd) for the bioanalytical conduct of daridorexant. Last but not least, the authors thank the clinical research team, i.e., Alexandre Mathis, István Kerekes, Pascale Gasser, and Marie Stoffel (Department of Clinical Pharmacology, Idorsia Pharmaceuticals Ltd).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Idorsia Pharmaceuticals Ltd.
Conflicts of Interest
Benjamin Berger, Muriel Richard, Clemens Muehlan, and Jasper Dingemanse were full-time employees of Idorsia Pharmaceuticals Ltd at the time of study conduct. Muriel Richard, Clemens Muehlan, and Jasper Dingemanse own stocks in Idorsia Pharmaceuticals Ltd, and Clemens Muehlan and Jasper Dingemanse own stock options in Idorsia Pharmaceuticals Ltd. Sander Brooks and Rob Zuiker were employees of CHDR at the time of study conduct. There are no other relationships or activities that could appear to have influenced the submitted work. CHDR received financial compensation for conducting the study from Idorsia Pharmaceuticals Ltd.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study prior to any study-mandated procedure.
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author Contributions
MR and JD designed the study. BB and SB wrote the manuscript. SB and RZ performed the assessments and collected the data. Data were analyzed by BB, CM, SB, and RZ. All authors reviewed and approved the final manuscript.
Additional information
The authors confirm that the Principal Investigator for this study is Rob Zuiker and that he had direct clinical responsibility for the subjects.
Rights and permissions
About this article
Cite this article
Berger, B., Brooks, S., Zuiker, R. et al. Pharmacological Interactions between the Dual Orexin Receptor Antagonist Daridorexant and Ethanol in a Double-Blind, Randomized, Placebo-Controlled, Double-Dummy, Four-Way Crossover Phase I Study in Healthy Subjects. CNS Drugs 34, 1253–1266 (2020). https://doi.org/10.1007/s40263-020-00768-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00768-8