Abstract
Mycophenolic acid is commonly prescribed in adult kidney transplant recipients for preventing graft rejection. A therapeutic target for total mycophenolic acid area under the concentration–time curve (30–60 mg h/L) has been established in adult kidney transplant recipients and widely referenced today. However, this specific target range does not adequately characterize mycophenolic acid-associated adverse effects. The primary objective of this qualitative and critical review was to characterize the exposure-toxicity relationships of mycophenolic acid in an attempt to determine whether exposure thresholds can be identified. The secondary objective was to determine the associations of clinical variables with specific adverse effects. The inclusion criteria consisted of all peer-reviewed papers in adult kidney transplant subjects (average study age > 18 years) with both exposure (area under the concentration–time curve) and toxicity data. The exclusion criteria were papers involving the pediatric population, studies lacking either area under the concentration–time curve or toxicity data, or studies with no apparent reported variations in area under the concentration–time curves. Of the 28 papers identified, inconsistent findings have been reported for the most frequently characterized adverse events of mycophenolic acid (gastrointestinal, infectious, and hematological), while promising exposure thresholds (i.e., > 40–60 mg h/L for total mycophenolic acid) have been suggested by a few studies. The roles of free mycophenolic acid exposure, mycophenolic acid metabolites, or clinical factors influencing the manifestation of the toxicities also remain to be clarified. Although it is not yet possible to define toxicity threshold(s) for the purpose of mycophenolic acid therapeutic drug monitoring, the information obtained and the limitations identified in this comprehensive literature body have provided a good foundation for future investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastrointestinal, infectious, and hematological adverse events are frequently associated with mycophenolate in adult kidney transplant recipients; however, the overall collective data are inconclusive to support a consistent relationship between mycophenolate exposure and the manifestation of these adverse events |
While promising exposure thresholds (i.e., > 40–60 mg h/L for total mycophenolate) can be hypothesized for the development of toxicity, further investigations using properly powered, controlled, randomized, or blinded trials with the primary aim to investigate specific toxicities are required |
1 Introduction
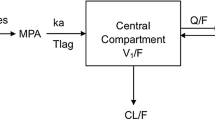
Mycophenolic acid (MPA) is commonly prescribed in combination with a calcineurin inhibitor and a corticosteroid in adult kidney transplant recipients as part of maintenance immunosuppression therapy for preventing graft rejection [1, 2]. Mycophenolic acid exerts its pharmacological action by inhibiting inosine-5′-monophosphate dehydrogenase, thereby reducing the production of guanosine nucleotides in both B and T lymphocytes [2]. The pharmacokinetics of MPA is highly variable between and within individuals, as evident by up to ten-fold variations often reported in the clinic. Sources of pharmacokinetic variability may involve absorption (e.g., formulation and gastric pH fluctuations), distribution (e.g., free fraction and enterohepatic recirculation), metabolism (e.g., genetic polymorphisms in UGT-glucuronosyltransferases and transporters [e.g., multidrug resistance-associated protein 2, solute carrier organic anion transporter family enzymes]), and excretion (e.g. renal function) [1, 3, 4]. Because of the large apparent pharmacokinetic variability, therapeutic drug monitoring of MPA has been recommended by many clinicians to optimize efficacy (e.g., [5]) and minimize toxicity (e.g., [6]). Moreover, the significant plasma protein binding of MPA leading to a low free fraction (1–3% under normal conditions) and the extensive metabolism of MPA in the production of glucuronidated metabolites can further complicate the therapeutic drug monitoring of MPA [1, 3]. These characteristics underscore the importance of considering free MPA concentrations and MPA metabolism while interpreting its pharmacokinetic–pharmacodynamic relationships.
Although there are both proponents and opponents to MPA therapeutic drug monitoring [2], a therapeutic target for the MPA area under the concentration–time curve (AUC; 30–60 mg h/L) has been established in adult kidney transplant recipients and widely referenced today. This specific target range was initially established in a patient population administered mycophenolate mofetil, cyclosporine, and corticosteroids where a significant correlation between total MPA exposure and biopsy-proven acute rejection was evident within 6 months post-transplant [5]. Moreover, it was determined that more subjects with lower MPA exposure (27.6 ± 12.3 mg h/L) had a biopsy-proven acute rejection (27.5%, n = 51) compared with sub-groups with higher MPA exposures (54.8 ± 15.3 mg h/L, 14.9%, n = 47; or 96.7 ± 32.2 mg h/L, 11.5%, n = 52) [5]. The resulting lower threshold of MPA (i.e., 30 mg h/L) for establishing efficacy has been subsequently verified in many other studies [4], supporting a robust pharmacokinetic–pharmacodynamic relationship. However, trends toward higher incidences of adverse events (e.g., gastrointestinal [GI] or hematological) in the high MPA exposure target group in comparison to those with lower exposures were observed in the same study, but the differences were not statistically significant and meaningful thresholds for toxicity were not established [5]. Therefore, this specific MPA upper therapeutic target (60 mg h/L) does not adequately characterize MPA-associated adverse effects and should not be interpreted as the threshold for the development of toxicity.
Mycophenolic acid is associated with many adverse effects [1, 3]. The most common side effects are GI in nature, manifesting in the clinic as nausea, vomiting, stomach cramps, and sometimes bothersome diarrhea [7, 8], which can significantly affect quality of life and lead to high rates of mycophenolate discontinuation [9]. Clinical management of GI side effects usually involves reducing the dose, increasing the dosing frequency, or switching to a potentially gastro-protective enteric-coated formulation to mitigate the hypothesized localized insult to GI mucosa by mycophenolate mofetil [7, 8]. However, complicated side effects such as infections or hematological complications (anemia, leukopenia, neutropenia) can also occur relatively frequently but require more resources for management. More importantly, these severe complications may lead to unwanted complications that may threaten graft survival and significantly reduce the patient’s quality of life. For example, a common clinical approach in the absence of MPA exposure data in a neutropenic/leukopenic patient is the empiric reduction of MPA dosage [7, 8], which can result in an increased incidence of graft rejection [10]. A leukopenic patient with infection is also more likely to be admitted to the hospital, requiring significant expenditures in human (nursing, clinical pharmacy) and drug (e.g., broad-spectrum antibiotics, granulocyte-colony stimulating factor) resources. Having clinical tools (i.e., therapeutic thresholds) that can assist clinicians identify the likelihood of developing MPA-associated toxicity would help mitigate these complications and reduce costs associated with their care.
The exposure-toxicity relationships of MPA have been summarized in the solid organ transplant population (e.g., [1, 3]), but a focused and updated critical summary in the adult kidney transplant population is warranted. As it is widely accepted that MPA exposure (i.e., AUC) but not individual concentrations (e.g., trough) best correlates with efficacy and potentially toxicity [4], this review focuses only on exposure data. Furthermore, because of significant differences in pharmacokinetic characteristics in pediatric subjects [11], only adult data, where the majority of the information is available, are presented. The primary objective of this review was to characterize the exposure-toxicity relationships of MPA for individual MPA-associated adverse effects in an attempt to determine whether an exposure threshold can be identified. The secondary objective was to determine the associations of clinical variables (e.g., patient demographical information, type of graft) with specific adverse effects.
2 Data Selection
This was a qualitative and critical review of the peer-evaluated literature. PubMed, MEDLINE, and EMBASE were searched, with no time limits, using combinations of the following terms: mycophenolic acid, mycophenolate, Cellcept, Myfortic, pharmacokinetics, pharmacodynamics, exposure, toxicity, adverse effects, gastrointestinal, hematologic, infection, anemia, leukopenia, neutropenia, and kidney transplant. The reference sections of all identified papers were further screened manually. The inclusion criteria consisted of all papers in adult kidney transplant subjects (average study age > 18 years) with both exposure (AUC) and toxicity data. The exclusion criteria were papers involving the pediatric population, studies lacking either AUC or toxicity data, or studies with no apparent reported variations in AUCs. All included studies are summarized chronologically in Table 1, incorporating information on the patient population, experimental design, dosing, analytical assay, and exposure-toxicity relationships. For the text discussion, data are presented based on adverse-effect categories: GI, infections, and hematological.
3 Important Mycophenolic Acid-Associated Adverse Events
3.1 Gastrointestinal Adverse Effects
Of the 28 identified papers, 21 have characterized GI adverse events either independently or as a composite of adverse outcomes (Table 1). The most common adverse events characterized were diarrhea, abdominal pain, constipation, dyspepsia, flatulence, nausea, and vomiting. The frequencies of GI side effects are highly variable between and within studies (Table 1). Overall, the relationships between independently characterized GI side effects and MPA exposures have proven to be mixed, with only a limited number of studies supporting an association. In a double-blinded, concentration-controlled study with primarily Caucasian subjects taking mycophenolate mofetil, van Gelder et al. [5] reported trends toward higher incidences of diarrhea (19.2%), vomiting (9.6%), and abdominal pain (13.5%) in their high MPA exposure group (AUC 96.7 ± 32.2 mg h/L) compared with other subjects with lower MPA AUCs (medium 54.8 ± 15.3 mg h/L or low exposure 27.6 ± 12.3 mg h/L) within 6 months of transplant. Despite not reaching statistical thresholds, these findings seemed to suggest an exposure-dependent effect, especially in the case of diarrhea where the incidence increased more than two fold (from 8.5% to 19.2%) with an increase in exposure between the two AUC groups (Table 1). Likewise, in a German population taking enteric-coated mycophenolate, Sommerer et al. [12] reported higher MPA AUCs in individuals with GI side effects (n = 6, AUC of 51 mg h/L) compared with subjects with no GI adverse events (AUC of 38 mg h/L) within 2 months post-transplant; however, a subsequent multiple regression analysis failed to identify MPA AUC as a predictor of GI effects. The findings from these two studies suggested that an AUC of 50–60 mg h/L might be the threshold limit for the escalation of diarrhea, but additional analysis (i.e., using receiver-operating characteristic curve) is needed to confirm this hypothesis.
However, in contrast to the findings of van Gelder et al. [5] and Sommerer et al. [12], an inverse relationship has also been reported between MPA exposure and GI toxicity. This was evident in a Japanese population where Kagaya et al. [13] reported a higher number of subjects with diarrhea (56%) had lower MPA AUCs (on day 28) than subjects with elevated MPA AUCs, although no statistical analyses were provided. Similarly, in a retrospective study by Pillans et al. [14] in a Caucasian cohort, GI adverse events were found in subjects with reduced exposure (n = 4, AUC 23.7 ± 2.43 mg h/L, days 2–5) compared with individuals with no documented GI events (n = 23, AUC 33.2 ± 1.73 mg h/L) (Table 1). This observation may be explained by the direct insult of MPA or its metabolites on luminal surfaces of the GI tract (i.e., the lower the absorption, the higher the local concentration) or an artefact of not capturing MPA exposure at the same time as the occurrence of GI side effects, which may explain the apparent inverse association between systemic exposure and toxicity.
Further support for an exposure-GI toxicity relationship was not evident in other studies using mycophenolate mofetil in primarily Caucasian populations. Atcheson et al. [15] did not find an association between MPA AUC (measured on day 5) and the occurrence of GI events within 1 month post-transplant. In a randomized controlled study, active MPA concentration adjustment led to increased MPA AUC on day 14 (33.7 vs. 27.1 mg h/L, respectively) and day 30 (45.0 vs. 30.9 mg h/L) post-transplant compared with a fixed-dosing regimen, but the higher exposure did not translate to increased GI events (97% vs. 90%, respectively) within 12 months of follow-up [16]. In an extended-duration (5 years) observational study [6], the proportion of subjects with non-infectious diarrhea was similar in patients with an AUC < 30 mg h/L (5.8%) compared with those with an AUC of 30–60 mg h/L (3.9%) or an AUC > 60 mg h/L (4.4%). In patients subjected to intensified MPA dosing for the first 5 days [17], increased MPA AUC on day 3 (59.3 mg h/L vs. 40.3 mg h/L standard dosing) and day 5 (59.3 mg h/L vs. 46.8 mg h/L) did not translate to increased incidence of constipation (35.3% vs. 29.9%), diarrhea (51.5% vs. 41.8%), dyspepsia (13.2% vs. 19.4%), nausea (50% vs. 49.3%), or vomiting (22.1% vs. 28.4%) during the 6 months of follow-up. Lack of differences in the incidence of GI effects between the two groups was further confirmed in a categorical analysis using an MPA AUC cut-off of 60 mg h/L determined at 5 days post-transplant [17]. Furthermore, in patients with early corticosteroid withdrawal, Le Meur et al. [18] also did not observe a difference in the overall incidence of diarrhea between the concentration-control (15%) or fixed-dosing (8.8%) groups over 12 months, despite significantly higher MPA AUCs at week 2 (36.2 ± 14.8 mg h/L vs. 29.3 ± 12.4 mg h/L, respectively) and week 6 (44.2 ± 16.1 mg h/L vs. 36.8 ± 18.1 mg h/L) post-transplant (Table 1). Finally, in a Chinese cohort, concentration control of MPA led to reduced MPA AUC (54.06 mg h/L, day 30) compared with fixed dosing (61.38 mg h/L), but this did not translate to differences in diarrhea occurrence (19.8% vs. 22%, respectively] over the 12-month follow-up period [19] (Table 1).
The lack of association between MPA exposure and GI toxicity was also observed in studies that have utilized enteric-coated mycophenolate. In a short parallel-controlled study in primarily Caucasian patients, Glander et al. [20] did not observe a difference in GI disorders (18% vs. 14%) despite higher MPA AUCs in the intensified group on day 3 (45 ± 15.70 mg h/L vs. 32.60 ± 18.71 [standard dosing]), day 10 (42.80 ± 17.40 mg h/L vs. 31.30 ± 18.40), and day 21 (41.60 ± 17.20 mg h/L vs. 31.60 ± 15.80) post-transplant. In a similarly designed study with a larger sample size and longer follow-up period of 6 months, Budde et al. [21] also did not draw a relationship between elevated MPA AUCs (week 6) in their intensified MPA dosing group and increased frequencies of total GI adverse events (Table 1). Moreover, the incidence of GI adverse events appeared to occur more frequently within the first 6 months post-transplant, as demonstrated by Arns et al. [22] where relatively fewer events were identified within the follow-up period between 6 and 12 months in comparison to the entire study period from 1 to 12 months. Consistent with other studies, irrespective of the follow-up period, no differences in the incidences of GI adverse events were observed by Arns et al. [22]. Furthermore, negative findings were also observed in Chinese subjects taking enteric-coated mycophenolate, where neither Ding et al. [23] nor Peng et al. [24] reported differences in GI adverse effects (including abdominal pain, constipation, diarrhea, dyspepsia, flatulence, nausea, vomiting) between the intensified dosing group that exhibited higher MPA AUCs (measured at 2 weeks in Ding et al. and day 7 in Peng et al.) and standard dosing groups (Table 1).
In addition to MPA data, attempts to correlate MPA metabolite exposures and GI side effects have not been successful. Heller et al. [25] characterized the exposures of both acyl MPA glucuronide and MPA glucuronide in patients administered mycophenolate mofetil and found no differences in subjects with or without diarrhea. van Agteren et al. [26] also did not report altered AUCs of acyl MPA glucuronide (measured at day 3 or month 3) in relation to episodes of diarrhea reported within the first month or between 3 and 12 months post-transplant. Likewise, in subjects administered enteric-coated mycophenolate, Tornatore et al. [27] found no associations between MPA glucuronide AUC (characterized at time of event) and GI adverse effects. However, the authors did find a trend of female subjects having a higher GI score compared with male patients in a subset of subjects with an AUC > 60 mg h/L, which might indicate a potential sex sensitivity toward these GI adverse events (Table 1).
3.2 Infections
Of the 28 identified papers, 18 have characterized infection events either independently or as a composite of adverse outcomes (Table 1). The most commonly reported events were cytomegalovirus (CMV), BK virus, upper respiratory tract, pneumonia, and urinary tract infections. The frequencies of infections varied significantly between studies (Table 1). Overall, only a limited number (n = 4) of studies have supported a relationship between MPA exposure and the occurrence of infections. In a primarily Caucasian population, Atcheson et al. [15] reported higher free MPA exposure (1.9 ± 0.3 mg h/L, measured on day 5) in subjects taking mycophenolate mofetil with a composite of thrombocytopenia, leukopenia, or infection compared with patients exhibiting no adverse effects (free MPA AUC 1.1 ± 0.1 mg h/L) within 1 month of transplant. However, the significance was lost with total MPA AUC and no analysis on infection events itself was conducted. In a German population taking enteric-coated mycophenolate, subjects with infections exhibited higher total MPA AUC (65 mg h/L, timing not specified) compared with those without infections (37 mg h/L) during a follow-up period of 56 days. These findings were supported by further multiple regression analyses where MPA AUC was identified as the only variable capable of predicting infection (r = 0.44) [12], although the specific details of the infection events were not available.
Similarly, in a larger study with a longer follow-up period (24–60 months), it was determined that an MPA AUC > 50 mg h/L (measured at 3 months post-transplant) was associated with viremia and polyomavirus-associated nephropathy based on a receiver operating characteristic analysis, although other clinical factors such as tacrolimus concentration also have contributed to BK viremia [28]. In the same study, both BK virus viruria and viremia occurred relatively early ~ 7.6 to 7.9 months post-transplant, with up to 48% of the subjects experiencing an episode of viruria (Table 1). However, because the majority (77.5%) of the patients were administered anti-thymocyte globulin, it was not clear whether this specific induction therapy had a role in enhancing the association or manifestation of this viral infection. Finally, in a Chinese population, Fu et al. [19] reported a lower infection rate in their concentration-control group compared with the fixed-dosing group (16.8% vs. 31.7%) during the 12-month follow-up period. This observation correlated with differences in MPA exposures (i.e., 54.06 mg h/L vs. 61.38 mg h/L) documented in the concentration-controlled vs. fixed-dosing groups, respectively, suggesting an AUC of 60 mg h/L might be the threshold for the escalation of infection events. However, further analyses on specific types of infection (e.g., bacterial, viral, and fungal) did not lead to significant findings between their treatment groups (Table 1). Consistent with the findings of Borni-Duval et al. [28], the majority of infections were also documented within 6 months post-transplant. Taken together, these data provide some evidence supporting an MPA exposure-infection relationship.
In contrast to the aforementioned studies, the majority of the studies (n = 14) have not supported an MPA exposure-infection relationship. This is evident in several studies with Caucasian subjects taking mycophenolate mofetil (Table 1). In a double-blinded concentration-controlled study, the incidence of pneumonia (3.8–6.4%) within the 6-month follow-up period was not different between patients with varying MPA AUCs [5]. Throughout a follow-up period of 12 months, patients with documented infection had similar MPA AUCs compared to subjects without active infections [29]. Moreover, active concentration-control of MPA resulted in elevated MPA AUCs early post-transplant but did not translate to increased occurrence of overall infection (77% vs. 74%) [16], CMV (1.5% vs. 9% [17] or 24.4% vs. 16.0% [18]), herpes simplex (10.3% vs. 9% [17] or 7.9% vs. 4.8% [18]), bacterial (48.8% vs. 44.8% [18]), or urinary tract infections (16.2% vs. 25.4%) [17] captured over 6–12 months. In the study by Gourishankar et al. [17], the occurrence of infections was also similar between patients with MPA AUC < 60 mg h/L or AUC > 60 mg h/L. Likewise, over a 5-year follow-up period, the proportion of subjects with infection was similar between patients with AUC < 30 mg h/L (9.9%), AUC 30–60 mg h/L (10%), or AUC > 60 mg h/L (7.1%) when MPA exposure was captured around the time of the event [6]. Finally, in a multi-arm comparative study, the occurrence of opportunistic infections (7–16%) was similar between patients in the MPA concentration-control group (with or without reduced calcineurin inhibitor dosing) compared to fixed MPA dosing, despite apparent differences in MPA exposure [30].
Similar negative findings were evident in subjects taking enteric-coated sodium mycophenolate (Table 1). In a primarily Caucasian population, intensified treatment for 2 weeks resulted in increased MPA AUCs from day 3 to day 21 (31.60 ± 15.80 mg h/L of standard dosing vs. 41.60 ± 17.20 mg h/L), but no differences in the incidence of infections within the 3-month period were observed (14% vs. 15%) [20]. Using a larger sample size over a longer follow-up period, intensified treatment further increased the MPA AUC by 47% by week 6 (vs. standard dosing), but the total number of infections (61.5% vs. 63.5% respectively; including CMV [7.5% vs. 12.8%], BK virus [3.8% vs. 1.8%], upper respiratory tract [8% vs. 5.9%], urinary tract [34.7% vs. 32.9%], herpes zoster [2.8% vs. 2.3%], nasopharyngitis [2.8% vs. 2.3%], or pneumonia [3.3% vs. 5%]) during the 6-month follow-up period remained the same [21]. Moreover, using the same experimental design but extending the follow-up to 12 months, the incidence of overall infection (73% vs. 80%; including CMV [11.1% vs. 13.8%], BK viremia [6.3% vs. 3.1%], respiratory infection [4.8% vs. 9.2%], upper respiratory tract [3.2% vs. 1.5%], pneumonia [14.3% vs. 12.3%], or urinary tract infection [46% vs. 47.7%]) also remained comparable [22]. Consistent with other MPA-associated adverse effects, most infection events were documented within 6 months post-transplant (Table 1).
In Japanese populations taking mycophenolate mofetil, Okamoto et al. [31] found trends of increased MPA AUC (39.2 ± 22.8 mg h/L, n = 12) in subjects identified to have adverse effects (composites of CMV infection, varicella infection, and GI side effects) compared with subjects with no side effects (AUC of 30.1 ± 8.0 mg h/L, n = 21) over a 2-week observational period. In a subgroup analysis, patients taking tacrolimus exhibiting adverse effects appeared to have further elevated MPA AUCs (55.7 ± 31.1 mg h/L, n = 5) compared with subjects without adverse events (32.6 ± 6.7 mg h/L), but none of these differences were statistically significant (Table 1). Similarly, Satoh et al. [32] also reported trends of increased MPA AUCs (61.5 mg h/L, n = 5) in Japanese patients with viral infections (i.e., CMV, varicella zoster, adenovirus, and malignancy related to Epstein–Barr virus) compared with patients without viral infections (AUC of 50.4 ± 31.6 mg h/L, n = 16) during 28 days post-transplant (p > 0.05). The MPA AUC levels were comparable between the two Japanese studies for subjects taking concurrent tacrolimus, and these values were higher than those obtained in subjects taking cyclosporine [31], possibly owing to the inhibitory effects of cyclosporine on the enterohepatic recirculation of mycophenolate. Although MPA exposure can vary significantly based on the co-administered calcineurin inhibitor, it is not clear whether this can lead to different thresholds of toxicities. Similar to the Japanese population, Chinese patients taking enteric-coated mycophenolate receiving intensified dosing had elevated MPA AUCs early post-transplant (e.g., 59.3 mg h/L vs. 44.8 mg h/L [standard dosing] on day 5), but this did not translate to increased infection (40.6% vs. 42.9%, including CMV [6.3% vs. 10.7%], respiratory tract [12.5% vs. 21.4%], pneumonia [6.3% vs. 10.7%], or urinary tract infection [31.3% vs. 35.7%]) over 6 months. These findings were reproduced by Peng et al. [24] in another Chinese cohort where increased AUCs in their intensified treatment group (66.18 ± 35.48 mg h/L vs. 45.30 ± 23.5 mg h/L [standard group] on day 7) also did not translate to increased incidences of infection (29% vs. 48%, including pulmonary [11% vs. 20%], urinary tract [8% vs. 11%], digestive tract [3% vs. 5%], BK virus-associated nephropathy [3% vs. 4%], or soft-tissue infection [4% vs. 7%]) during 12 months post-transplant. Overall, the observation of a lack of association between MPA exposure and infection is consistent between ethnicities.
3.3 Hematological Disorders
Of the 28 identified papers, 19 have characterized hematological side effects either independently or as a composite of adverse outcomes (Table 1). The most commonly reported events were leukopenia and anemia, with only a limited number of studies investigating neutropenia. The frequencies of hematological disorders varied significantly between studies (Table 1). Similar to the other adverse effects discussed in this paper, only a limited number (n = 6) of studies have supported a relationship between MPA exposure and the occurrence of hematological toxicities. Inconsistent findings have also been reported from different investigators.
In patients taking a low-dose mycophenolate mofetil regimen co-administered with tacrolimus, Mourad et al. [33] found a significant difference in MPA exposure in subjects presenting with composite adverse events (leukopenia, anemia, diarrhea, esophagitis, thrombocytopenia) [n = 31 sample profiles, AUC of 48.38 ± 18.50 mg h/L) compared with subjects with no adverse events (n = 47, 36.04 ± 10.82 mg h/L) during the 3-month follow-up period. A further receiver operating characteristic analysis also indicated an MPA exposure cut-off of 37.6 mg h/L for developing toxicity (Table 1). However, in a similarly designed trial by the same investigators using a higher dose of mycophenolate mofetil co-administered with cyclosporine, the relationships between MPA exposure and the same composite adverse outcomes were lost [34]. Consistent with the occurrence of GI or infectious complications, this observation supports the notion that other clinical factors (e.g., type of concurrent calcineurin inhibitor) should be considered when interpreting the adverse outcomes of MPA. Furthermore, Kuypers et al. [29] reported higher total MPA exposure for subjects with leukopenia compared with those with no leukopenia at 3 months (61.4 ± 30.9 mg h/L vs. 42.3 ± 25.3 mg h/L) or 12 months post-transplant (84.4 ± 45.6 mg h/L vs. 44.2 ± 21.9 mg h/L). Similar associations between MPA exposure and anemia were also observed (Table 1).
However, in a previous study in a much smaller sample (n = 39), the same authors did not observe statistically significant correlations between total MPA AUC, free MPA AUC, MPA glucuronide AUC, or MPA acyl-glucuronide AUCs with respect to anemia and leukopenia, despite trends indicating higher exposure in patients with documented hematological toxicities [35]. These findings further underscore the importance of a power analysis in these relatively small observational studies. However, Atcheson et al [15] were able to find a relationship between free MPA AUC (characterized on day 5) and either thrombocytopenia or leukopenia within 1 month post-transplant, as evident by patients exhibiting side effects having higher exposure (MPA AUCfree 1.9 ± 0.3 mg h/L) compared with those with no adverse effects (MPA AUCfree 1.1 ± 0.1 mg h/L). However, inconsistent with Kuypers et al. [29], the relationship was lost when total exposure was characterized (Table 1).
Furthermore, in a longer term, 5-year follow-up study using a categorical approach, Kuypers et al. [6] were able to estimate the exposure thresholds for developing hematological toxicities. In this study, an exposure-effect relationship was clearly evident in subjects with leukopenia (AUC < 30 mg h/L [5%] vs. AUC 30–60 mg h/L [7%] vs. AUC > 60 mg h/L [12.4%]), anemia < 12 g/L/day (AUC < 30 mg h/L [40.8%] vs. AUC 30–60 mg h/L [52.2%] vs. AUC > 60 mg h/L [64.3%]), or anemia < 10 g/L/day (AUC < 30 mg h/L [14.2%] vs. AUC 30–60 mg h/L [17%] vs. AUC > 60 mg h/L [25%]). These findings provided support for using an MPA AUC cut-off of 60 mg h/L for the detection of leukopenia or anemia, but further receiver operating characteristic analyses are needed to establish the specificity and sensitivity of this specific threshold. Finally, in a corticosteroid-free population, Kiang et al. [36] found significant correlations between total MPA exposure and neutropenia in three different periods within the first year of transplant (Table 1). While a strong correlation was observed, further analyses are still needed to identify the specific MPA AUC thresholds for developing neutropenia. As well, the relationship between MPA exposure and neutropenia still remains to be established in the corticosteroid-based population.
Similar to other discussed side effects, a large number of studies have not supported an MPA exposure-hematological toxicity relationship, irrespective of MPA formulation or patient ethnicity (Table 1). In a prospective, double-blinded, concentration-controlled study, the incidences of leukopenia within 6 months of a transplant were not statistically significant between patients with different levels of MPA exposure, although a trend was identified where subjects having elevated AUCs (96.7 ± 32.2 mg h/L) appeared almost twice more likely to develop neutropenia [5]. In a randomized prospective controlled study by van Agteren et al. [26], 16% of the subjects were found to have developed leukopenia between 3 and 12 months post-transplant; but, this was only observed in the tacrolimus, and not cyclosporine, co-treated patients. No difference in acyl MPA glucuronide exposure (measured at month 3) in patients with (1.36 mg h/L) or without (1.15 mg h/L) leukopenia was identified in this study. Similarly, Gaston et al. [30] did not report a difference in the incidence of leukopenia between concentration-controlled or fixed-dosing MPA regimens with either normal- or reduced-dose calcineurin inhibitor co-administration. In support of these findings, Sobiak et al. [37] found no consistent associations between MPA or MPA glucuronide exposures and levels of hemoglobin (some correlation with glucuronide observed), hematocrit, erythrocyte count, leukocytes, or platelets in their relatively lengthy (4.7 years) observational study. Furthermore, in a series of studies that have examined the effects of intensified vs. standard dosing (of either MPA formulation), early increases in MPA AUCs did not generally translate to increased incidences of hematological disorders over 3 months [20], 6 months [17, 21, 23], or 12 months [16, 22, 24] post-transplant. More specifically, in individuals with an MPA AUC ≤ 60 mg h/L vs. an MPA AUC > 60 mg h/L, Gourishankar et al. [17] found no difference in the incidence of leukopenia (20 vs. 18.4%), neutropenia (5.0 vs. 5.3%), and thrombocytopenia (3.8 vs. 2.6%). Moreover, based on the study by Arns et al. [22], it was clearly evident that the majority of the hematological events (e.g., leukopenia, thrombocytopenia, anemia) occurred within the first 6 months post-transplant, an observation that is consistent with the other identified adverse effects of MPA (Table 1).
4 Conclusion and Future Directions
The overall collective data can be best described as inconclusive to support a relationship between MPA exposure and the manifestation of specific (i.e., GI, infection, or hematological) adverse effects. While promising exposure thresholds (i.e., > 40–60 mg h/L for total MPA) or exposure-toxicity correlations for MPA have been suggested by a few studies presented in this review, many were observational in nature and of relatively short duration. Furthermore, the limited and conflicting experimental evidence supporting free MPA exposure or MPA metabolites as potentially better markers of toxicity indicates that further validations are required. The number of papers with negative findings also outnumbered those that have reported associations (Table 1). With respect to clinical factors affecting MPA toxicity, concurrent calcineurin inhibitor administration (i.e., either tacrolimus or cyclosporine) does have significant effects on MPA exposure, but clear relationships with MPA-associated toxicity have not always been documented (Table 1). Tornatore et al. [27] suggested that female subjects were more likely to develop GI adverse events, but the majority of other studies have not conducted sex-based analyses. Moreover, although there does not appear to be significant differences in the MPA exposure-toxicity relationship based on ethnic makeup, the majority of the data were obtained from Caucasian-based populations (with the remaining from Asian subjects) with no single paper having conducted a properly controlled comparison (Table 1). Additional systematic analyses with other clinical markers (e.g., the type of transplant [live vs. cadaveric], age, induction therapy, or concurrent supportive medications) were also difficult because of the heterogeneous nature, limited number, and inconsistent reporting (i.e., with missing data) of the included papers (Table 1).
However, many confounding factors that could have attributed to false-negative findings were also evident in these studies. (1) In many cases, the identified toxicity may not be attributed to MPA alone, and other concurrent drugs (e.g., tacrolimus for diarrhea; type of induction therapy for infection or leukopenia) may have masked the contribution of MPA. Perhaps a “combined” therapeutic window as proposed by Kuypers et al. [29] might be able to mitigate part of this limitation with the co-administered maintenance immunosuppressant therapies. (2) The majority of the studies lacked sufficient power for detecting differences in toxicity events that were often characterized as secondary endpoints. Where power analyses have been conducted, they were mostly tailored to the primary end-point for MPA efficacy (i.e., rejection frequency). (3) The MPA-associated toxicities were often not consistently or clearly defined between the studies. As examples, different definitions based on individual center practices for diarrhea (with or without baseline consideration) or leukopenia/neutropenia (severity, cut-off) were evident. (4) Different analytical assays for MPA were used between studies, which could have resulted in different exposure estimations (Table 1). For example, several studies have utilized immunoassays that are known to over-estimate MPA concentrations as a result of cross-reactivity with the acyl MPA glucuronide. With the majority of centers now electing to use liquid-chromatography mass spectrometry for improved selectivity and sensitivity, it is unclear whether these historical data collected with different assays can still be relevant for current practice today. (5) With the exception of a few studies, the majority did not capture exposure data at the same time as the occurrence of MPA adverse events. Many studies were also designed to only increase early MPA exposure, which led to mostly negative associations with adverse outcomes that were captured over a longer period of time. The inconsistencies between the timing of MPA exposure estimation and the occurrence of toxicity could have severely minimized the sensitivity of the correlations. Finally, (6) the majority of the studies presented in Table 1 had a follow-up period within 12 months; therefore, very limited data on the longer term toxicity threshold, which may be different than the acute period (i.e., within the first year post-transplant), were available.
Collectively, we have summarized the literature that suggests promising MPA exposure-toxicity relationships in adult kidney transplant recipients. Although it is not yet possible to define toxicity threshold(s) for the purpose of therapeutic drug monitoring, the information obtained and the limitations identified in these studies have provided a good foundation for future investigations using properly powered, controlled, randomized, or blinded trials with the primary aim to investigate specific toxicities.
References
Staatz CE, Tett SE. Pharmacology and toxicology of mycophenolate in organ transplant recipients: an update. Arch Toxicol. 2014;88(7):1351–9. https://doi.org/10.1007/s00204-014-1247-1.
Le Meur Y, Borrows R, Pescovitz MD, Budde K, Grinyo J, Bloom R, et al. Therapeutic drug monitoring of mycophenolates in kidney transplantation: report of The Transplantation Society consensus meeting. Transplant Rev (Orlando). 2011;25(2):58–64. https://doi.org/10.1016/j.trre.2011.01.002.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin Pharmacokinet. 2007;46(1):13–58.
Kiang TK, Ensom MH. Therapeutic drug monitoring of mycophenolate in adult solid organ transplant patients: an update. Expert Opin Drug Metab Toxicol. 2016;12(5):545–53. https://doi.org/10.1517/17425255.2016.1170806.
van Gelder T, Hilbrands LB, Vanrenterghem Y, Weimar W, de Fijter JW, Squifflet JP, et al. A randomized double-blind, multicenter plasma concentration controlled study of the safety and efficacy of oral mycophenolate mofetil for the prevention of acute rejection after kidney transplantation. Transplantation. 1999;68(2):261–6.
Kuypers DR, de Jonge H, Naesens M, de Loor H, Halewijck E, Dekens M, et al. Current target ranges of mycophenolic acid exposure and drug-related adverse events: a 5-year, open-label, prospective, clinical follow-up study in renal allograft recipients. Clin Ther. 2008;30(4):673–83.
Kiang TK, Ensom MH. Anti-rejection drugs. In: Murphy JE, editor. Clinical pharmacokinetics. 6th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2017. p. 205–20.
Kiang TK, Ensom MH. Immunosuppressants. In: Beringer PE, editor. Basic clinical pharmacokinetics. 6th ed. Baltimore, MD: Wolters Kluwer; 2017. p. 320–57.
Helderman JH, Goral S. Gastrointestinal complications of transplant immunosuppression. J Am Soc Nephrol. 2002;13(1):277–87.
Zafrani L, Truffaut L, Kreis H, Etienne D, Rafat C, Lechaton S, et al. Incidence, risk factors and clinical consequences of neutropenia following kidney transplantation: a retrospective study. Am J Transplant. 2009;9(8):1816–25. https://doi.org/10.1111/j.1600-6143.2009.02699.x.
Filler G, Bendrick-Peart J, Christians U. Pharmacokinetics of mycophenolate mofetil and sirolimus in children. Ther Drug Monit. 2008;30(2):138-4. https://doi.org/10.1097/FTD.0b013e31816ba73a.
Sommerer C, Muller-Krebs S, Schaier M, Glander P, Budde K, Schwenger V, et al. Pharmacokinetic and pharmacodynamic analysis of enteric-coated mycophenolate sodium: limited sampling strategies and clinical outcome in renal transplant patients. Br J Clin Pharmacol. 2010;69(4):346–57. https://doi.org/10.1111/j.1365-2125.2009.03612.x.
Kagaya H, Miura M, Satoh S, Inoue K, Saito M, Inoue T, et al. No pharmacokinetic interactions between mycophenolic acid and tacrolimus in renal transplant recipients. J Clin Pharm Ther. 2008;33(2):193–201. https://doi.org/10.1111/j.1365-2710.2008.00906.x.
Pillans PI, Rigby RJ, Kubler P, Willis C, Salm P, Tett SE, et al. A retrospective analysis of mycophenolic acid and cyclosporin concentrations with acute rejection in renal transplant recipients. Clin Biochem. 2001;34(1):77–81.
Atcheson BA, Taylor PJ, Mudge DW, Johnson DW, Hawley CM, Campbell SB, et al. Mycophenolic acid pharmacokinetics and related outcomes early after renal transplant. Br J Clin Pharmacol. 2005;59(3):271–80.
Le Meur Y, Buchler M, Thierry A, Caillard S, Villemain F, Lavaud S, et al. Individualized mycophenolate mofetil dosing based on drug exposure significantly improves patient outcomes after renal transplantation. Am J Transplant. 2007;7(11):2496–503.
Gourishankar S, Houde I, Keown PA, Landsberg D, Cardella CJ, Barama AA, et al. The CLEAR study: a 5-day, 3-g loading dose of mycophenolate mofetil versus standard 2-g dosing in renal transplantation. Clin J Am Soc Nephrol. 2010;5(7):1282–9. https://doi.org/10.2215/CJN.09091209.
Le Meur Y, Thierry A, Glowacki F, Rerolle JP, Garrigue V, Ouali N, et al. Early steroid withdrawal and optimization of mycophenolic acid exposure in kidney transplant recipients receiving mycophenolate mofetil. Transplantation. 2011;92(11):1244–51. https://doi.org/10.1097/TP.0b013e318234e134.
Fu L, Huang Z, Song T, He S, Zeng D, Rao Z, et al. Short-term therapeutic drug monitoring of mycophenolic acid reduces infection: a prospective, single-center cohort study in Chinese living-related kidney transplantation. Transpl Infect Dis. 2014;16(5):760–6. https://doi.org/10.1111/tid.12275.
Glander P, Sommerer C, Arns W, Ariatabar T, Kramer S, Vogel EM, et al. Pharmacokinetics and pharmacodynamics of intensified versus standard dosing of mycophenolate sodium in renal transplant patients. Clin J Am Soc Nephrol. 2010;5(3):503–11. https://doi.org/10.2215/CJN.06050809.
Budde K, Tedesco-Silva H, Arns W, Shoker A, Zeier M, Klinger M, et al. Improved rejection prophylaxis with an initially intensified dosing regimen of enteric-coated mycophenolate sodium in de novo renal transplant recipients. Transplantation. 2011;92(3):321–7. https://doi.org/10.1097/TP.0b013e318223d7f3.
Arns W, Sommerer C, Glander P, Ariatabar T, Porstner M, May C, et al. A randomized trial of intensified vs. standard dosing for enteric-coated mycophenolate sodium in de novo kidney transplant recipients: results at 1 year. Clin Nephrol. 2013;79(6):421–31. https://doi.org/10.5414/cn107908.
Ding C, Xue W, Tian P, Ding X, Pan X, Xiang H, et al. Which is more suitable for kidney transplantation at the early post-transplantation phase in China: low dosing or standard dosing of enteric-coated mycophenolate sodium? Int J Clin Pract Suppl. 2014;181:10–6. https://doi.org/10.1111/ijcp.12401.
Peng W, Liu G, Huang H, Wu J, Chen J. Short-term intensified dosage regimen of mycophenolic acid is associated with less acute rejection in kidney transplantation from donation after circulatory death. Urol Int. 2018;101(4):443–9. https://doi.org/10.1159/000494361.
Heller T, van Gelder T, Budde K, de Fijter JW, Kuypers D, Arns W, et al. Plasma concentrations of mycophenolic acid acyl glucuronide are not associated with diarrhea in renal transplant recipients. Am J Transplant. 2007;7(7):1822–31.
van Agteren M, Armstrong VW, van Schaik RH, de Fijter H, Hartmann A, Zeier M, et al. AcylMPAG plasma concentrations and mycophenolic acid-related side effects in patients undergoing renal transplantation are not related to the UGT2B7-840G > A gene polymorphism. Ther Drug Monit. 2008;30(4):439–44. https://doi.org/10.1097/FTD.0b013e318180c709.
Tornatore KM, Meaney CJ, Wilding GE, Chang SS, Gundroo A, Cooper LM, et al. Influence of sex and race on mycophenolic acid pharmacokinetics in stable African American and Caucasian renal transplant recipients. Clin Pharmacokinet. 2015;54(4):423–34. https://doi.org/10.1007/s40262-014-0213-7.
Borni-Duval C, Caillard S, Olagne J, Perrin P, Braun-Parvez L, Heibel F, et al. Risk factors for BK virus infection in the era of therapeutic drug monitoring. Transplantation. 2013;95(12):1498–505. https://doi.org/10.1097/TP.0b013e3182921995.
Kuypers DR, Claes K, Evenepoel P, Maes B, Vanrenterghem Y. Clinical efficacy and toxicity profile of tacrolimus and mycophenolic acid in relation to combined long-term pharmacokinetics in de novo renal allograft recipients. Clin Pharmacol Ther. 2004;75(5):434–47. https://doi.org/10.1016/j.clpt.2003.12.009.
Gaston RS, Kaplan B, Shah T, Cibrik D, Shaw LM, Angelis M, et al. Fixed- or controlled-dose mycophenolate mofetil with standard- or reduced-dose calcineurin inhibitors: the Opticept trial. Am J Transplant. 2009;9(7):1607–19. https://doi.org/10.1111/j.1600-6143.2009.02668.x.
Okamoto M, Wakabayashi Y, Higuchi A, Kadotani Y, Ogino S, Ushigome H, et al. Therapeutic drug monitoring of mycophenolic acid in renal transplant recipients. Transplant Proc. 2005;37(2):859–60.
Satoh S, Tada H, Murakami M, Tsuchiya N, Inoue T, Togashi H, et al. The influence of mycophenolate mofetil versus azathioprine and mycophenolic acid pharmacokinetics on the incidence of acute rejection and infectious complications after renal transplantation. Transplant Proc. 2005;37(4):1751–3.
Mourad M, Malaise J, Chaib Eddour D, De Meyer M, Konig J, Schepers R, et al. Pharmacokinetic basis for the efficient and safe use of low-dose mycophenolate mofetil in combination with tacrolimus in kidney transplantation. Clin Chem. 2001;47(7):1241–8.
Mourad M, Malaise J, Chaib Eddour D, De Meyer M, Konig J, Schepers R, et al. Correlation of mycophenolic acid pharmacokinetic parameters with side effects in kidney transplant patients treated with mycophenolate mofetil. Clin Chem. 2001;47(1):88–94.
Kuypers DR, Vanrenterghem Y, Squifflet JP, Mourad M, Abramowicz D, Oellerich M, et al. Twelve-month evaluation of the clinical pharmacokinetics of total and free mycophenolic acid and its glucuronide metabolites in renal allograft recipients on low dose tacrolimus in combination with mycophenolate mofetil. Ther Drug Monit. 2003;25(5):609–22.
Kiang TKL, Partovi N, Shapiro RJ, Berman JM, Collier AC, Ensom MHH. Regression and genomic analyses on the association between dose-normalized mycophenolic acid exposure and absolute neutrophil count in steroid-free, de novo kidney transplant recipients. Clin Drug Investig. 2018;38(11):1011–22. https://doi.org/10.1007/s40261-018-0694-5.
Sobiak J, Kaminska J, Glyda M, Duda G, Chrzanowska M. Effect of mycophenolate mofetil on hematological side effects incidence in renal transplant recipients. Clin Transplant. 2013;27(4):E407–14. https://doi.org/10.1111/ctr.12164.
van Gelder T, Silva HT, de Fijter JW, Budde K, Kuypers D, Tyden G, et al. Comparing mycophenolate mofetil regimens for de novo renal transplant recipients: the fixed-dose concentration-controlled trial. Transplantation. 2008;86(8):1043–51. https://doi.org/10.1097/TP.0b013e318186f98a.
Sommerer C, Glander P, Arns W, Ariatabar T, Kramer S, Vogel EM, et al. Safety and efficacy of intensified versus standard dosing regimens of enteric-coated mycophenolate sodium in de novo renal transplant patients. Transplantation. 2011;91(7):779–85. https://doi.org/10.1097/TP.0b013e31820d3b9b.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding or editorial assistance was received for the preparation of this article.
Conflict of Interest
Tony K.L. Kiang and Mary H.H. Ensom have no conflicts of interest that are directly related to the content of this article.
Rights and permissions
About this article
Cite this article
Kiang, T.K.L., Ensom, M.H.H. Exposure-Toxicity Relationships of Mycophenolic Acid in Adult Kidney Transplant Patients. Clin Pharmacokinet 58, 1533–1552 (2019). https://doi.org/10.1007/s40262-019-00802-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00802-z