Abstract
Introduction
The bioequivalence of two formulations of desmopressin (dDAVP), a vasopressin analogue prescribed for nocturnal enuresis treatment in children, has been previously confirmed in adults but not in children. In this study, we aimed to study the pharmacokinetics (PK) and pharmacodynamics (PD) of these two formulations, in both fasted and fed children, including patients younger than 6 years of age.
Methods
Previously published data from one PK study and one PK/PD study in children aged between 6 and 16 years were combined with a new PK/PD study in children aged between 6 months and 8 years, and analysed using population PK/PD modelling. Simulations were performed to further explore the relative bioavailability of both formulations and evaluate current dosing strategies.
Results
The complex absorption behaviour of the lyophilizate was modelled using a double input, linked to a one-compartmental model with linear elimination and an indirect response model linking dDAVP concentration to produced urine volume and osmolality. The final model described the observed data well and elucidated the complexity of bioequivalence and therapeutic equivalence of the two formulations. Simulations showed that current dosing regimens using a fixed dose of lyophilizate 120 μg is not adequate for children, assuming children to be in the fed state when taking dDAVP. A new age- and weight-based dosing regimen was suggested and was shown to lead to improved, better tailored effects.
Conclusions
Bioequivalence and therapeutic equivalence data of two formulations of the same drug in adults cannot be readily extrapolated to children. This study shows the importance of well-designed paediatric clinical trials and how they can be analysed using mixed-effects modelling to make clinically relevant inferences. A follow-up clinical trial testing the proposed dDAVP dosing regimen should be performed.
Clinical Trial Registration
This trial has been registered at www.clinicaltrials.gov (identifier NCT02584231; EudraCT 2014-005200-13).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
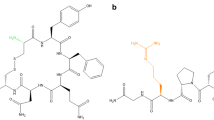
Desmopressin (1-deamino-8-d-arginine vasopressin, dDAVP) is indicated for the treatment of central diabetes insipidus and primary nocturnal enuresis, in practice mostly used for the treatment of monosymptomatic nocturnal enuresis (MNE). It is recommended to be taken in a fasted state before bedtime, which is challenging for young children due to the short time between the last meal in the evening and bedtime. Two oral formulations of dDAVP are currently labelled for the indication of nocturnal enuresis: a tablet (TAB) and a lyophilizate (MELT). Their bioequivalence at dose strengths of 200 and 120 µg, respectively, has been established in adults [1, 2] but not in children. Bioequivalence has been established at the pharmacokinetic (PK) level in adults only [3] and was explored using the population approach in children [4]. The potential differences between these formulations at the pharmacodynamic (PD) level were explored both clinically [5, 6] and by using the population approach [7], without consistent conclusions regarding the link between effect and formulation. Therefore, an integrated analysis of the PK and PD in the paediatric population is warranted.
Currently, treatment for MNE is started, irrespective of age or weight, with the same dose of dDAVP, i.e. 120 and 200 µg once daily for the lyophilizate and the tablet formulation, respectively. Previous studies have been inconsistent regarding the need for age- or weight-dependent dDAVP dosing, but suggest there might be a correlation between body size and PK that could culminate in a potentially relevant PD effect [4, 6,7,8]. The lack of a consensus might be attributed to the lack of paediatric PK/PD data across the entire age range. Indeed, previous analyses focused on children older than 6 years of age, and were not able to detect a clinically significant effect of age or weight on dDAVP PK/PD [4, 6,7,8].
Furthermore, previous studies applied a sparse sampling design, specifically in the early phase postdosing. An earlier model-based analysis suggested that these early time points are important to correctly describe the absorption behaviour of the lyophilizate formulation [7]. The complex absorption behaviour of this formulation has already been observed in pigs, and has been described using a double input absorption model to reflect absorption, both buccally and at the level of the gut following ingestion of part of the dose [9].
A new clinical trial was set up to tackle these challenges. In this study, the PK and PD of dDAVP in young children (< 8 years of age) was investigated using a sampling scheme with more intense sampling in the early phase [10]. In order to amalgamate these new data with previous work and to elucidate differences in PK and PD between young children, children and adults, a modelling and simulation strategy was applied. This work describes this model-based analysis of these data combined with previously analysed data from older (> 6 years) children. Building on previous hypotheses tested in animal models, a new PK/PD model was constructed in order to further understand dDAVP PK/PD and to see how it translates to clinical outcomes. This model was consequently used to obtain better dosing recommendations across the full paediatric age range.
2 Materials and Methods
2.1 Study Data
Two previously published paediatric PK studies on oral dDAVP and one paediatric PD study were included in the current analysis and their characteristics are summarized in Table 1 [6, 8, 11]. Østerberg et al. compared the PK of an oral lyophilizate in 72 children with MNE with the PK in 28 healthy, adult volunteers using a double-blind, randomized, parallel group, multicentre study [8]. Data from 25 of these children were available for the current analysis. In a second study, De Bruyne et al. used a two-period crossover design to compare oral lyophilizate with a tablet formulation in children with MNE [11]. Of the 23 children that were included, 22 successfully completed the study, of whom the PK data were available for the current analysis. The PD of 18 children of the same group were also investigated by De Guchtenaere et al. The data were supplemented with data from a new study, optimally designed based on the previously constructed models [4]. The characteristics of these patients are also described in Table 1. In short, 25 children who needed a urinary concentration test, or who suffered from therapy resistant nocturnal enuresis (based on nocturnal polyuria) were recruited in an open label, non-randomized, interventional PK/PD study. After a 15 ml/kg water load to achieve maximal diluting capacity, dDAVP was provided sublingually as a one-time age-adapted dose (see Table 1). After 3 h, urinary voids were compensated to maintain fluid homeostasis. Blood and urine samples were taken at different time points and dDAVP concentrations were measured in both matrices. Furthermore, urine volume and urine osmolality were recorded as PD markers. The study was approved by the local Ethics Committee (EC/2015/0616), EudraCT (2014-005200-13) and registered at www.clinicaltrials.gov (NCT02584231) [10].
2.2 Model Development
A previously constructed porcine two-compartmental PK model with double input absorption was used as a starting point to describe the dDAVP concentrations [9]. This model was extended with a renal clearance component to accommodate the urine concentrations, and linked to our earlier constructed indirect response model [7]. Furthermore, separate absorption processes were implemented for the tablet and lyophilizate formulation. The log-transform both sides (LTBS) approach was used for the plasma concentrations, whereas the PD endpoints were modelled in the normal domain. Interindividual variability (IIV) was implemented on most parameters and was assumed to follow a log-normal distribution. Several residual error models (additive, proportional and mixed, for all outputs) were tested. Furthermore, different PK (one- vs. two-compartment, different absorption models, and addition of renal clearance) and PD [simple inverse, maximum effect (Emax) style, or dDAVP-inhibited link between urine volume and osmolality] models were compared in order to obtain the final structural model. Once an appropriate mixed-effects model was obtained, covariate relationships were investigated using a forward selection approach, adding them to the model one at a time and selecting the models with the best performance metrics to proceed. The covariates that were tested, were formulation (MELT), fed state (FED), age (AGE), body weight (WT), sex (SEX), and theory-based allometric models [12, 13]. Once the full model was obtained, backwards deletion was performed in order to obtain the most appropriate parsimonious model [14].
The decision to include or exclude certain model components, both in the construction of the base model and the covariate model was guided by several performance metrics: objective function value (OFV), Akaike’s Information Criterion (AIC), physiological plausibility, and population and individual predictions versus observations and versus time. A drop in OFV of 3.84 (p = 0.05 using the Chi square distribution with q degrees of freedom (the difference in estimated parameters between the two compared models) as an approximation of the OFV distribution) was assumed to indicate a significantly better fit. In the backwards deletion step, a rise in OFV < 6.63 (p = 0.01, same approximation) after deletion was assumed to indicate a non-significantly worse model, thus leading to deletion of the covariate.
2.3 Model Evaluation
The final PK/PD model was evaluated using different standard tools [15] for all three model outputs (dDAVP plasma concentration, urine volume and urine osmolality). (1) Visual and numerical predictive checks were performed, based on 1000 simulations of the final model and binning into 10 bins containing the same amount of observations to assure equal distribution of the observed data; (2) individual and population predictions versus observation plots were constructed and a Loess smoother was added to visually check for deviations from the unity line; and (3) a bias-corrected bootstrap with acceleration constant (BCa) was performed to obtain second-order 90% confidence intervals (CIs) around the parameter estimates [16]. For this, 1000 datasets of 64 subjects were resampled with replacement from the original dataset, and used to estimate the model parameters again.
2.4 Simulations
Once confidence in the model had been achieved during the evaluation step, it was used for simulations. In a first step, standard adult doses of lyophilizate 120 µg and tablet 200 µg [17, 18] were compared in the fasted and fed state in the paediatric population. As the analysed dataset did not contain fasted patients taking the tablet formulation, assessing a food effect reliably was only possible for lyophilizate. The original dataset of 64 patients was thus simulated 1000 times after lyophilizate 120 μg + fed, lyophilizate 120 μg + fasted, and tablet 200 μg + fed, resulting in three times 64,000 simulated patients.
Plasma concentrations over time were plotted together with produced urine volume over time. Because in the simulation a virtual sample was taken every 0.1 h, the diuresis rate was calculated from the simulated urine volume by dividing it by its corresponding time interval. To assess the differences in PK, the area under the plasma concentration–time curve from zero to 12 h (AUC12) and maximum plasma concentration (Cmax) were calculated and compared. The differences in PD were assessed using the duration of the effect, which was defined as the time interval during which the diuresis rate was below 1.5 ml/h/kg. This target was chosen as being in-between normal urine outputs of 1–2 ml/h/kg in healthy and critically ill children [19,20,21].
In order to compare dosing regimens, three targets were defined to mimic a ‘successful therapy’ (simulating both a reduction in urine production and a recovery of functionality in the morning). A dosing regimen was deemed applicable when at least 75% (P75) of patients reached at least 6 h of decreased diuresis, 50% (P50) reached at least 8 h, and < 25% (P25) stayed 10 h or longer below the defined target. In other words, the percentage of the population reaching the target longer than 6 h and < 10 h should be maximized and should at least reach 50%. The first two criteria can be seen as markers of efficacious treatment, whereas the last marker is indicative of a good recovery of normal urine production in the morning (limited carryover effect).
The variability in AUC and Cmax was described using the ratio of the interquartile range over the median, which is a non-parametric description less sensitive to outliers expected in such a heterogeneous population:
A second simulation study investigated alternative dosing schemes. The standard dose of lyophilizate 120 μg was compared with two age-based and three weight-based dosing schemes. The first age-based scheme was identical to the one used in the current clinical study, extrapolated to include children older than 8 years. The second scheme followed the same logic but used half the normal doses. The weight-based schemes were chosen similarly. All simulated dosing schemes are shown in Table 2.
Simulation parameters were identical to the first simulation study, applied to patients taking the lyophilizate formulation. All simulations were carried out in the fed state to account for the fact that children are not fasted when taking dDAVP (1 h before bedtime). The same targets of at least 6 h, 8 h and < 10 h of decreased diuresis were used, first again with a target diuresis of 1.5 ml/h/kg and then stratified per age with a target of 1 ml/h/kg for children older than 2 years of age and 2 ml/h/kg for younger children [20].
2.5 Software
Model development and parameter estimation were performed using NONMEM version 7.4 [22], with first-order conditional estimation with interaction (FOCE + I) as the estimation algorithm, accessed using the Perl-Speaks-NONMEM (PsN) software [23], embedded in the workbench Piraña [24]. R version 3.4.2, accessed via RStudio version 1.1.383 (http://www.rstudio.com/), was used to prepare the datasets, perform the simulations, and post-process all results, including the statistical calculations and plot generation.
3 Results
Visual inspection of the new patient data containing samples obtained at early time points postdosing indicated that two absorption processes occurred [10]. This confirmed the hypothesis of a double input absorption and prompted the construction of a model describing this behaviour.
3.1 Model Development
Before starting full model development, the PK data alone were analysed using the earlier published porcine model [9]. From this analysis, it was decided to start from a one-compartment model instead of a two-compartment model as two compartments were not supported by the data, similar to our previous analysis [4]. Furthermore, as no IV data were included, the bioavailability could not be estimated from the data, implying that clearance (CL) and volume of distribution (Vd) are estimated as apparent parameters relative to bioavailability. As the data consisted of data from the two formulations under different scenarios, a reference bioavailability was chosen. As all children taking the tablet formulation were also fed (no fasted data were available), the reference bioavailability (fixed to 1) was defined to be the bioavailability of the tablet formulation after food intake (FTab,Fed). The bioavailability of lyophilizate, both in the fasted and fed state, could thus be estimated relative to FTab,Fed.
After this, the PD data were added and simultaneous PK/PD modelling commenced. In line with previous analyses [7], the IIV on the maximal effect and Hill coefficients (if present) were fixed to 0. Furthermore, an interoccasion variability on urine production was included as tablet and lyophilizate were administered on separate days for some patients. The separate renal clearance pathway was omitted from the model for two reasons. First, an earlier analysis [10] attributed < 1% of the clearance to the renal pathway, which was confirmed by the parameter estimates of the population PK model. Second, as dDAVP influences the urinary output, the urinary dDAVP concentrations are dependent on the PD and are thus not a clear marker for renal clearance. The analysis was continued using dDAVP plasma concentrations, urine volume and osmolality as model outputs.
Several indirect response PD models were compared with one another, and ultimately the original Emax-style inhibition of urine volume production [7] was supplemented with a similar inhibition of the production of urine osmolality response, comparable to a previously published dDAVP PD model in adults [25]. Furthermore, addition of the PD data allowed to further characterize the PK absorption part: a shared absorption rate constant and lag time (LAG) could be estimated for the gastrointestinally (non-buccally) absorbed part of the lyophilizate and for the tablet, but D1 and LAG needed to be fixed to their final values obtained after log likelihood profiling, for stability reasons. In the final model, an inverse effect of age on bioavailability, age on urine production, and food and formulation on bioavailability were retained as significant covariates. The final model structure and parameter estimates are shown in Fig. 1 and Table 3.
3.2 Model Evaluation
In Fig. 2, the population and individual prediction versus observation plots are shown for all outputs. Some underprediction of the lowest urine volumes, and consequently highest osmolality values, can be seen, but, in general, the model describes the data well. The visual predictive checks are shown in Fig. 3 and showed good prediction properties of the general trend and variability for plasma concentrations, urine volume and urine osmolality for the three scenarios (FAST + MELT, FED + MELT and FED + TAB) for which data were available. The numerical predictive check confirmed this: 5.54% and 5.18% of observations lie above the predicted 95% and below the predicted 5% percentiles, respectively. The results of the bootstrap analysis are shown in Table 3. Average bias was 0.16% and varied between − 5.24 and 5.45% for the structural model parameters and − 5.13 and 12.2% for the stochastic model parameters.
Basic goodness-of-fit plots. On top, the population (first row) and individual (second row) predictions versus observed values are shown. The dotted line represents the unity line and the solid line represents a Loess smoother through the data points. The CWRES are shown versus the population predictions (third row) and versus time after dose (fourth row). The dotted line represents the zero line and the solid line represents a Loess smoother through the data points. dDAVP desmopressin, CWRES conditionally weighted residuals, PRED predicted, LOESS locally estimated scatterplot smoothing
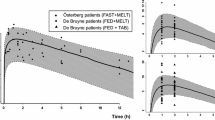
Visual predictive checks for the different scenarios. On top, the plasma concentration–time profiles are shown, whereas the pharmacodynamic responses, depicted as the diuresis rate and urine osmolality, are shown below. The solid line indicates the prediction median, the shaded area represents the 90% prediction interval, the dashed lines represent the 25th–75th percentile, and the dots represent the observed data in the different studies
3.3 Standard Dosing
The simulation results of the standard doses are shown in Fig. 4 and the derived AUC, Cmax, variability estimates and patients reaching the targets are depicted in Table 4. Taking the dDAVP lyophilizate in the fasted state results in a 50% increase in exposure compared with the fed state. This is also propagated to the PD effect: 51.5% of the fasted patients reached 1.5 ml/h/kg for at least 8 h after taking the lyophilizate, compared with 25.0% of the fed patients. The percentage of patients in between the target range of 6 and 10 h was quite similar: 53.3% of the fasted patients versus 45.5% of the fed patients.
Simulation results after lyophilizate 120 μg (fasted and fed) or tablet 200 μg (fed). On top, the plasma concentration–time profiles are shown, whereas the pharmacodynamic response, depicted as the diuresis rate per kilogram body weight, is shown below. The horizontal line marks the target of 1.5 ml/h/kg and the solid line marks the median response, with the shaded area representing the 90% prediction interval and the dashed lines representing the 25th–75th percentiles. Vertical lines mark the targets of 6 h effect, 8 h effect and no more than 10 h effect
Comparing the two formulations in the fed state, a slightly higher exposure for the MELT compared with the tablet was observed, with lower variability. On the PD level, lyophilizate performed better than the tablet: 45.5% of the fed patients reached the target range after taking lyophilizate, compared with 36.7% after taking the tablet.
3.4 Alternative Dosing Schemes
In a second simulation study, alternative dosing schemes to the standard lyophilizate dose of 120 μg were investigated. As can be seen in Table 5, the original age-dependent dosing scheme from the present study results in almost thrice the exposure (compared with lyophilizate 120 μg), with long reductions in the diuresis rate for the majority of the simulated patients (> 8 h for 79.0% of the simulations). However, 63.9% of the simulated patients still experienced effects after 10 h, and 42.3% still had low urine production 12 h after dosing. Consequently, only 31.1% of the simulated patients reached the target range of between 6 and 10 h of effect. Another age-dependent dosing scheme with half the original dose resulted in a slightly higher exposure (compared with standard dosing) and a much better PD profile as the doses were better tailored to the individual patients, and thus individual exposures were vastly different from the conventional dose. In this case, the targets of P25 at 6 h, P50 at 8 h and P75 at 10 h were reached, and 59.1% of patients reached the target range of between 6 and 10 h of effect (Fig. 5).
Simulation results after age-dependent dosing schemes in the fed state. On top, the plasma concentration–time profiles are shown, whereas the pharmacodynamic response, depicted as the diuresis rate, is shown below. The lines represent the median response and the shaded areas represent the 90% prediction intervals. The horizontal line marks the target of 1.5 ml/h/kg enuresis and the solid line marks the median response, with the shaded area representing the 90% prediction interval and the dashed lines representing the 25th–75th percentiles. Vertical lines mark the targets of 6 h effect, 8 h effect and no more than 10 h effect
Applying the weight-dependent dosing scheme, an slight increase in PK variability and overall higher exposure was observed, resulting in a longer persistence of the effect on diuresis rate. Scheme 1 resulted in similar overall effects as the conventional dosing, whereas scheme 2 reached the targets of P25 at 6 h, P50 at 8 h, and P75 at 10 h, with 47.8% of patients reaching the target range of between 6 and 10 h of effect. Scheme 3 resulted in too high exposure and thus too long-lasting effects, with 53.4% of patients having lowered enuresis for more than 10 h (Fig. 6).
Simulation results after weight-dependent dosing schemes in the fed state. On top, the plasma concentration–time profiles are shown, whereas the pharmacodynamic response, depicted as the diuresis rate, is shown below. The lines represent the median response and the shaded areas represent the 90% prediction intervals. The horizontal line marks the target of 1.5 ml/h/kg enuresis and the solid line marks the median response, with the shaded area representing the 90% prediction interval and the dashed lines representing the 25th–75th percentiles. Vertical lines mark the targets of 6 h effect, 8 h effect and no more than 10 h effect
Based on these results, it was concluded that age-based dosing scheme 2 and weight-based dosing scheme 2 were the most optimal for paediatric dDAVP therapy. Indeed, weight-based dosing scheme 1 barely improves upon the conventional 120 μg dosing (only 28.5% of patients would reach at least 8 h diuresis under 1.5 ml/h/kg), whereas weight-based dosing scheme 3 and age-based dosing scheme 1 resulted in an overdosing situation, evident by the large portions of simulated patients who stayed under 1.5 ml/h/kg for longer than 10 h.
In order to further investigate the appropriateness of these schemes compared with conventional dosing, the simulations were stratified by age. This is shown in Fig. 7 and Table 6. From these simulations, assuming the fed state, it can be seen that conventional dosing of 120 μg is not appropriate. Indeed, for children younger than 4 years of age, this dose results in prolonged effects: 95.5% of children younger than 2 years of age, and 36.8% of children between 2 and 4 years of age, experienced effects longer than 10 h. In older children, the effect reached does not last long enough: only 25% of children between 4 and 8 years of age, 7.2% of children between 8 and 12 years of age, and 5% of children older than 12 years of age reached 8 h of lowered enuresis.
Stratification of diuresis simulations by age. The horizontal line marks the target of 2 ml/h/kg for children between 0 and 2 years of age and of 1 ml/h/kg for children above 2 years of age, and the solid line represents the median response, with the shaded area representing the 90% prediction interval and the dashed lines representing the 25th–75th percentiles. The targets of 6 h effect, 8 h effect and no more than 10 h effect are marked by vertical lines
Looking at the age- and weight-dependent dosing schemes, exposure is better matched with the simulated patients, and targets are reached more often. For the age-based scheme, 31.6%, 50.6%, 51.2%, 42.6% and 49.1% of children aged between 0 and 2 years, 2 and 4 years, 4 and 8 years, 8 and 12 years, and older than 12 years, respectively, reached the target range of between 6 and 10 h of effect, versus 4.5%, 59.2%, 51.2%, 26.2% and 26.1%, respectively, following flat dosing. The weight-based scheme also performs better than flat dosing, i.e. 40.0%, 54.2%, 46.2%, 39.6% and 30.8% of children aged between 0 and 2 years, 2 and 4 years, 4 and 8 years, 8 and 12 years, and older than 12 years, respectively, reached the target range of between 6 and 10 h of effect.
4 Discussion
In the present study, new paediatric PK/PD data for the peptide drug dDAVP were added to existing data and were re-analysed using the mixed-effects modelling approach. Questions that were raised in previous analyses of PK and PD data were further investigated [4, 7]. During these previous analyses, a discrepancy between PK and PD data was found, resulting in a formulation effect on some of the PD parameters. It was then hypothesized that this discrepancy was caused by a lack of a sufficient number of samples in the absorption part, precluding the reliable description of the plasma concentration–time profile following the lyophilizate intake, and the possible occurrence of a double absorption peak after buccal administration of the lyophilizate formulation, which might have been missed.
This hypothesis was further supported by a juvenile animal study in pigs [9]. Therefore, new clinical data were generated using an optimized clinical trial design based on the previously constructed PK/PD models, which were added to the already available dataset. A double absorption peak could indeed be seen in the newly generated raw data, serving as a first confirmation of the initial hypothesis [10]. A simultaneous PK/PD analysis was thus performed on all combined data, using a double input, first-order absorption model linked to a one-compartmental model with first-order elimination, which in turn was linked to a zero-order production of urine using an indirect response model.
A profound food effect was again detected on bioavailability, as has been previously described for adults [3] and children, based on PK data alone [4]. However, as in the analysed dataset, only a small part of the data came from fed patients, who were all older than 8 years of age; this effect could also be a study effect or a maturational effect. It would be beneficial for the current PK/PD analysis to complete the dataset with fed data in younger children and fasted data for patients taking the tablet formulation. These data should be collected following a similar sampling scheme as in the present study to appropriately capture the complex absorption behaviour.
The importance of this food effect was emphasized by simulating conventional versus age- and weight-dependent dosing regimens. It was found that the standard dosing might not be appropriate in children as the average target attainment over the different age groups is only 33.4%, compared with 45.0% for the age-dependent dosing scheme and 42.2% for the weight-dependent dosing scheme. Looking closer at the stratified data, the weight-dependent dosing scheme was identified to provide the most favourable paediatric PD profile for children younger than 4 years of age, and the age-dependent scheme performed the best for children older than 4 years of age, as opposed to conventional dosing. Indeed, children under the standard dosing regimen often suffer from either suboptimal or too prolonged effects, which occur significantly less frequently with the newly proposed scheme. However, even with the proposed schemes, a large portion of children remain outside of the target ranges. Indeed, a large unexplained variability in the exposure–response relationship remains that should be further investigated using, for example, biomarkers such as the baseline urine osmolality or aquaporin levels [26].
Several new growth effects could also be detected by the addition of the new dataset containing younger children. Indeed, an inverse effect of age on bioavailability was found. As no IV data were included in this model, CL and Vd are apparent parameters, and thus this inverse effect translates to a directly proportional effect of age on these parameters. However, as all patients younger than 7 years of age originated from a single study where they only received lyophilizate, the age effect on bioavailability might be formulation-dependent, and extrapolations to the tablet formulation should thus be handled with care. Apart from PK, age was also found to be a significant covariate on urine production. This link between size/age and PK/PD shows the benefit of adapted dosing schemes to ensure efficacy during the entire night and to prevent overdosing.
Compared with previous published paediatric PK/PD models, this model stands out due to its younger population, quantified maturation effects on both PK and PD, and the simultaneous consideration of PK, urine volume and urine osmolality. Few models describing the PK/PD of dDAVP have been published. An indirect response model in hydrated adults modelled urine osmolality as the primary response and linked diuresis to it using the same inhibition function. Model parameters were estimated using individual curve fitting in WinNonlin and were, on average, 3.7 pg/ml for the half maximal inhibitory concentration (IC50) and 0.80 for the maximum inhibition (Imax) [25]. Juul et al. investigated dDAVP PK/PD in adults and used the previously described indirect response model in order to link urine osmolality to dDAVP plasma concentrations using non-linear mixed-effects modelling [27]. They found IC50 and Imax values of 1.14 pg/ml and 0.93, respectively, comparable with our values of 1.91 pg/ml and 0.863, respectively. The seemingly higher potency of dDAVP in adults might explain the differences in efficacious doses between children and adults [27, 28].
The original observations that sparked this investigation were inconsistent results regarding bioequivalence and therapeutic equivalence of dDAVP in children. In the current PK/PD model, the formulation effect on the PD side was no longer present, solving the earlier observed physiologically implausible discrepancy. These results suggest that the two formulations indeed have a complex bioequivalence relationship, influenced by the differences in absorption and the impact of food and age on these complexities. Taken over the entire population, the lyophilizate 120 μg and tablet 200 μg have a similar exposure in the fed state, but a different effect. This difference is probably due to the higher variability in exposure after taking the tablet, possibly caused by a more profound food effect. However, care must be taken as only a small portion of the data were tablet concentrations, all coming from older, fed children. To compare the formulations more thoroughly, fasted tablet data and data from younger children taking the tablet should be incorporated. As the effect of food on the tablet formulation has thus far not been tested in young children, we caution its use in this population and suggest lyophilizate according to the abovementioned dosing scheme.
5 Conclusions
This study again exemplifies the need for a good study design as discrepancies present in the previous analyses of this compound in the paediatric population were resolved by the inclusion of new data originating from a trial with a model-based design. It was shown that current dosing using lyophilizate might be inappropriate in children who are not fasted when taking dDAVP before bedtime. Simple dosing schemes based on age or weight were proposed as an alternative and could now be tested in clinical practice. However, simulations showed that even these schemes will not achieve therapeutic success for a large portion of patients due to the remaining unexplained variability, and additional driving factors for this exposure–response variability should be investigated in further paediatric clinical trials.
References
Kaehler ST, Steiner IM, Sauermann R, Scheidl H, Mueller M, Joukhadar C. A bioequivalence study of two oral desmopressin tablet formulations. Pharmacology. 2006;77(1):46–52.
Fjellestad-Paulsen A, Wille S, Harris AS. Comparison of intranasal and oral desmopressin for nocturnal enuresis. Arch Dis Child. 1987;62(7):674–7.
Rittig S, Jensen AR, Jensen KT, Pedersen EB. Effect of food intake on the pharmacokinetics and antidiuretic activity of oral desmopressin (DDAVP) in hydrated normal subjects. Clin Endocrinol (Oxf). 1998;48:235–41.
Michelet R, Dossche L, de Bruyne P, Colin P, Boussery K, Vande Walle J, et al. Effects of food and pharmaceutical formulation on desmopressin pharmacokinetics in children. Clin Pharmacokinet. 2016;55(9):1159–70.
Vande Walle JGJ, Bogaert GA, Mattsson S, Schurmans T, Hoebeke P, Deboe V, Norgaard JP. A new fast-melting oral formulation of desmopressin: a pharmacodynamic study in children with primary nocturnal enuresis. BJU Int. 2006;97(3):603–9.
De Guchtenaere A, Van Herzeele C, Raes A, Dehoorne J, Hoebeke P, Van Laecke E, et al. Oral lyophylizate formulation of desmopressin: superior pharmacodynamics compared to tablet due to low food interaction. J Urol. 2011;185(6):2308–13.
Michelet R, Dossche L, Van Herzeele C, Van Bocxlaer J, Vermeulen A, Vande Walle J. Claiming desmopressin therapeutic equivalence in children requires pediatric data: a population PKPD analysis. Eur J Clin Pharmacol. 2018;74(3):297–305.
Østerberg O, Savic RM, Karlsson MO, Simonsson USH, Nørgaard JP, Vande Walle J, et al. Pharmacokinetics of desmopressin administrated as an oral lyophilisate dosage form in children with primary nocturnal enuresis and healthy adults. J Clin Pharmacol. 2006;46(10):1204–11.
Gasthuys E, Vermeulen A, Croubels S, Millecam J, Schauvliege S, van Bergen T, et al. Population pharmacokinetic modeling of a desmopressin oral lyophilisate in growing piglets as a model for the pediatric population. Front Pharmacol. 2018;9:41.
Dossche L, Michelet R, De Bruyne P, Gasthuys E, Rittig S, Vermeulen A, et al. What young children teach us about pharmacokinetics and pharmacodynamics of desmopressin oral lyophylisate—one size does not fit all. 2019 (manuscript under preparation).
De Bruyne P, De Guchtenaere A, Van Herzeele C, Raes A, Dehoorne J, Hoebeke P, et al. Pharmacokinetics of desmopressin administered as tablet and oral lyophilisate formulation in children with monosymptomatic nocturnal enuresis. Eur J Pediatr. 2014;173(2):223–8.
Anderson BJ, Holford NH. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol. 2008;48(1):303–32.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24(1):25–36.
Hutmacher MM, Kowalski KG. Covariate selection in pharmacometric analyses: a review of methods. Br J Clin Pharmacol. 2015;79(1):132–47.
Nguyen THT, Mouksassi MS, Holford N, Al-Huniti N, Freedman I, Hooker AC. Model evaluation of continuous data pharmacometric models: metrics and graphics. CPT Pharmacomet Syst Pharmacol. 2017;6(2):87–109.
Efron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82(397):171–85.
Ferring Pharmaceuticals. MINIRIN® Melt Desmopressin Product Information File. 2007. Available online from http://secure.healthlinks.net.au/content/ferring/pi.cfm?product=fppminiw10611. Accessed 19 July 2019.
Medicines and Healthcare products Requlatory Agency (MHRA). DDAVP MELT Oral Lyophilisate (Desmopressin Acetate) License File. 2006. Available online from http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con2023731.pdf. Accessed 19 July 2019.
Rittig S, Kamperis K, Siggaard C, Hagstroem S, Djurhuus JC. Age related nocturnal urine volume and maximum voided volume in healthy children: reappraisal of International Children’s Continence Society definitions. J Urol. 2010;183(4):1561–7.
Dossche L, Raes A, Hoebeke P, De Bruyne P, Vande Walle J. Circadian rhythm of glomerular filtration and solute handling related to nocturnal enuresis. J Urol. 2016;195(1):162–7.
Hazinski MF. Understanding fluid balance in the seriously ill child. Pediatr Nurs. 1988;14(3):231–6.
Bauer R. NONMEM users guide: introduction to NONMEM 7. Ellicott City: ICON Development Solutions; 2010. p. 1–61.
Lindbom L, Pihlgren P, Jonsson N. PsN-Toolkit—a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79(3):241–57.
Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: Tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol. 2013;2:e50.
Callreus T, Odeberg J, Lundin S. Indirect-response modeling of desmopressin at different levels of hydration. J Pharmacokinet Biopharm. 2000;27(5):513–29.
Liu J, Sharma N, Zheng W, Ji H, Tam H, Wu X, et al. Sex differences in vasopressin V2 receptor expression and vasopressin-induced antidiuresis. Am J Physiol Renal Physiol. 2011;300(2):F433–40.
Juul KV, Van Herzeele C, De Bruyne P, Goble S, Vande Walle J, Nørgaard JP. Desmopressin melt improves response and compliance compared with tablet in treatment of primary monosymptomatic nocturnal enuresis. Eur J Pediatr. 2013;172(9):1235–42.
Schulman S, Stokes A, Salzman P. The efficacy and safety of oral desmopressin in children with primary nocturnal enuresis. J Urol. 2001;166(6):2427–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Agency for Innovation by Science and Technology in Flanders (IWT) through the SAFE-PEDRUG project (IWT/SBO 130033).
Conflict of interest
An Vermeulen is an employee of Johnson & Johnson and holds stock/stock options in the company. Pauline De Bruyn, Lien Dossche and Charlotte Van Herzeele received travel reimbursement from Ferring Pharmaceuticals for a presentation at the Ghent-Aarhus Springschool. Johan Vande Walle has received consulting fees and travel reimbursements from Ferring Pharmaceuticals, as well as payment for lectures from Ferring Pharmaceuticals and Astellas Pharma. Robin Michelet, Elke Gasthuys and Jan Van Bocxlaer have no potential conflicts of interest that might be relevant to this article.
Additional information
Robin Michelet, Lien Dossche, Charlotte Van Herzeele, Pauline De Bruyne, Elke Gasthuys, Jan Van Bocxlaer, Johan Vande Walle, An Vermeulen: In name of the SAFEPEDRUG consortium, http://safepedrug.eu.
Rights and permissions
About this article
Cite this article
Michelet, R., Dossche, L., Van Herzeele, C. et al. An Integrated Paediatric Population PK/PD Analysis of dDAVP: How do PK Differences Translate to Clinical Outcomes?. Clin Pharmacokinet 59, 81–96 (2020). https://doi.org/10.1007/s40262-019-00798-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00798-6