Abstract
Purpose
For a new formulation of a drug, only pharmacokinetic bioequivalence with the original formulation has to be demonstrated in healthy, young adults. However, “children are not small adults,” and to guarantee a safe and effective treatment, age-adapted drug development is required. Desmopressin, a vasopressin analogue prescribed for nocturnal enuresis in children, was studied as an example formulation first developed in adults and then extrapolated to a pediatric indication.
Methods
Population pharmacokinetic and pharmacodynamic modeling was used to analyze previously published desmopressin data of 18 children suffering from nocturnal enuresis. The main objective was the comparison of the therapeutic equivalence of two desmopressin formulations: tablet and lyophilisate. The measurements for pharmacokinetics and pharmacodynamics were respectively plasma desmopressin concentration and urine osmolality and diuresis.
Results
The half maximal inhibitory concentration for inhibition of urine production was 0.7 pg/mL lower for the lyophilisate than for the tablet. The effect of formulation on the half maximal inhibitory concentration seems to suggest that the 120-μg lyophilisate has a more pronounced effect on the urine volume and osmolality than the 200-μg tablet, even when the same exposure is achieved.
Conclusions
A new indirect response model for desmopressin was constructed and validated, using a previously built pharmacokinetic model and additional pharmacodynamic data. In order to draw solid conclusions regarding the efficacy and safety of desmopressin in children, pharmacokinetics and pharmacodynamics data should be analyzed together. This study adds proof to potential differences in pediatric and adult pharmacokinetic and pharmacodynamic properties of desmopressin and exemplifies the need for pediatric clinical trials, not only for every new drug but also for every new formulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical drug studies in children are characterized by several practical and ethical issues [1]. In order to reassure safe prescription, the Food and Drug Administration (FDA) and European Medicines Agency (EMA) regulations on pediatric drug research have tried to find a compromise between minimal exposure of children to a pediatric research program and acquiring sufficient pharmacokinetics and pharmacodynamics (PKPD) and safety data. To obtain registration for a new or generic formulation of an existing drug in children, pediatric bioequivalence studies are not required. Rather, PK studies are performed in a limited number of healthy young male volunteers, assuming that PK is a surrogate for the PD, hardly ever accounting for the potential effects of gender-, size-, age-, and maturation-specific differences [2, 3]. However, “children are not small adults,” and to guarantee a safe and effective treatment, age-adapted drug development is required [4].The SAFE-PEDRUG project (http://safepedrug.eu) aims to redefine the current premises in pediatric drug research. Therefore, this project aspires to develop a new strategy, using a multidisciplinary bottom-up approach starting from knowledge of the pediatric physiology and pharmacology.
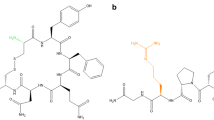
Desmopressin (dDAVP, 1-deamino-8-D-arginine vasopressin), a synthetic vasopressin analogue originally developed for central diabetes insipidus, is one of the index drugs under study in the SAFE-PEDRUG project. Since 1980, this oligopeptide was approved for primary monosymptomatic nocturnal enuresis (MNE) in children, based on the finding that enuretic children lack the nocturnal rise in vasopressin levels, resulting in a relatively high overnight urine production [5]. It is an interesting drug to be studied because of its peptidic nature, which leads to low bioavailability with large between-subject variability (tablet: 0.08–0.16% of the administered dose; for the lyophilisate: 0.25% of the administered dose in adults) [6, 7]. Moreover, in contrast with the most pediatric drug dosing regimens, the available dDAVP formulations do not require an age- or size-adapted dose [8, 9]. Nevertheless, the lack of age- and size dependency was recently questioned, not only in children but also in the elderly [10,11,12].
Currently, only the tablet and the lyophilisate are labeled for the use in children with MNE. Bioequivalence studies in adults have shown that the average bioavailability of the lyophilisate is approximately 60% higher than the tablet [7]. The existing 200/400-μg tablet formulations are thus considered to be bioequivalent to the 120/240-μg lyophilisate. Moreover, the bioavailability of dDAVP lyophilisate is less influenced by food interactions, most likely due to the fact that the absorption mainly occurs through oral and/or buccal mucosae [10, 13]. Following the aforementioned FDA and EMA regulations, the same dosing regimen is applied in children, despite the absence of pediatric data [8, 14].
lPrevious pilot studies of our research group already questioned the claimed PK bioequivalence features, especially when administered in children [10, 11, 15]. Furthermore, the correlation between PK and PD shows some temporal delays as was demonstrated in a recent study [16], and it might be expected to be even more complex in infants and small children because renal medullary concentrating activity develops progressively during the first years of life [17]. Moreover, additional research in children on the equivalence of PD effects, the therapeutic equivalence, of dDAVP is required, concerning the anti-enuretic effect (number of wet nights per week), the antidiuretic effect (urinary volume per time unit), and the renal concentrating capacity (urinary osmolality). Finally, in order to draw solid conclusions regarding the efficacy and safety of dDAVP in children, PK and PD data should be analyzed together. The aim of this study was to investigate the therapeutic equivalence of dDAVP tablet and lyophilisate in children with MNE.
Material and methods
Study data
Previously published data from a pilot study were analyzed using population PKPD modeling. The design of this interventional prospective study was a two-period cross-over trial, which is the preferred design for bioequivalence studies of two formulations according to the EMA guidelines. Data was collected on two separate days in identical standardized conditions, in children who were fed a standard meal (Fig. 1). The tested formulae of dDAVP were a 200-μg tablet (Desmotab®, Ferring N.V. Aalst, Belgium) and a 120-μg lyophilisate (Minirin®, Melt, Ferring) at respectively day one and day two.On arrival, participants had been fasting since the morning. A 15 mL/kg water load was administered to suppress the subjects’ own vasopressin secretion. If complete dilution was reached, a standardized meal of 510 kcal (McDonald’s® - Happy Meal™) was served, immediately followed by dDAVP administration. To maintain hydration, produced urine was compensated by drinking an equal amount of water and insensible loss (estimated as 500 mL/m2 body surface area per 24 h) was compensated 5 h post-dDAVP dose. Patients between 5 and 18 years old, suffering from MNE, and partially responding to dDAVP tablet or nasal spray were included. All children were recruited in a tertiary enuresis center (Ghent University Hospital, Belgium). Exclusion criteria were dDAVP hypersensitivity, abnormalities of the oral cavity, use of antibiotics, diuretics or any other drug known to have an effect on dDAVP–plasma concentrations, or any clinically significant disease likely to interfere with the evaluations.
Study design (adapted from De Guchtenaere A. et al., J Urol 2011 [10])
In this PKPD population modeling study, data of 18 out of the 23 originally included children were analyzed. The reasons to exclude data of five patients were the following: one patient was not able to take oral medication, one patient did not stop dDAVP treatment the day before the test, one patient did not reach full dilution after fluid intake, and two patients had collection errors (Table 1).Written informed consent was signed by all parents and/or a legal guardian, while children of appropriate intellectual maturity completed an assent form (age > 12 years). Approval was obtained from the local ethical committee (EC 2009/653), and the study was performed in accordance with the ICH guidelines of Good Clinical Practice [18].
Model development
The dDAVP–plasma concentrations, urinary volumes, and urine osmolalities were used as the PK and PD endpoints, respectively. A sequential PKPD approach was applied to these data. For this, a previously built and published one-compartmental PK model with first-order absorption, based on the same patients, was used to predict the dDAVP–plasma concentrations at the PD time points [15]. As dDAVP works by regulating a physiological process, i.e., water reabsorption, an indirect response model was found to best describe the link between plasma concentrations and PD endpoints [19, 20]. In previous work by Callreus et al., a type 2 indirect response model was used to describe the influence of dDAVP on the urine osmolality in adults [21]. This osmolality was then linked to the urine production via an effect compartment. This model was considered at the start of the model building process but soon replaced by another model structure. In this alternative, urine is considered to be produced according to a zero-order function, which is inhibited by dDAVP, i.e., a type 1 indirect response model was applied [19]. A type 1 indirect response model is the inhibition of the appearance rate of response (in this case, inhibition of urine production), whereas a type 2 indirect response model indicates the inhibition of the disappearance of a response (in previous models used to inhibit the inhibition of the disappearance of the concentrating capacity).
At each measurement, the urine compartment was reset to simulate bladder voiding, and the total urine volume at the time of measurement was linked to the osmolality using an Emax-type model. The model structure and link between predicted urine volume and measured urine osmolality are depicted in Fig. 2.
Model structure and graphical depiction of the link between predicted urine volume and urine osmolality. A one-compartmental model with first-order absorption is used to predict the dDAVP–plasma concentration, which then inhibits the zero-order production of urine. F bioavailiability, k a first-order absorption rate constant, k e first-order elimination rate constant, k o zero-order urine production rate)
The estimation of the population parameters proceeded iteratively using FOCE in NONMEM version 7.3(Ellicott City, Maryland), and the interindividual variability (IIV) was assumed to follow a log-normal distribution [22]. Different residual error models were tested and eventually an additive residual error model was used for the osmolality, whereas a proportional residual error was chosen for the urine volume. Once an appropriate mixed effects model was obtained, covariate relationships were investigated using forward selection by adding them to the model one at a time and selecting the models with the best performance metrics to proceed with. The covariates that were tested were the formulation (MELT), age (AGE), body weight (WT), sex (SEX), the Tanner Index (TAN), and the urinary creatinine level (UCREA). The model development decisions were driven by the following metrics: the objective function value (OFV), physiological plausibility, Akaike’s information criterion (AIC), condition number (CN), and the relative standard error (RSE) of the parameter estimates. A drop in the OFV of 3.84 was assumed to indicate a significantly better fit. Since in the end, only one covariate was included in the model, no backward deletion step was performed (Fig. 3).
Model evaluation results. On the bottom, the visual predictive checks are shown for urinary volume (left) and osmolality (right). The red dotted line represents the total median model prediction, and the blue shaded area between the blue dotted lines represents the 90% prediction interval. The observed median and 90% interval are depicted by the full lines. On the top, the normalized prediction error distribution (NPDE) for urinary volume (left) and osmolality (right) are shown. Red lines show the NPDE distribution with the standard normal distribution (black line) overlaid. The mean of this distribution was − 0.001 for the urinary volume and − 0.023 for the urine osmolality, whereas the standard deviation was 1.003 and 0.909, respectively
Model evaluation
To assess the quality of the model, different evaluation techniques were applied. Both a prediction-corrected visual predictive check (pcVPC) and a numerical predictive check (NPC) were performed [23, 24]. Individual and population predictions were compared with the data, and a normalized prediction distribution error (NPDE) analysis was performed. For this, the final model was simulated 1000 times, after which the NPDEs were calculated [25]. Under the null hypothesis that the model describes the data, the distribution of NPDEs should be equal to the standard normal distribution N (0, 1). This hypothesis was formally tested using the Wilcoxon signed-rank test (H0: μ = 0), the Fisher variance ratio test (H0: σ 2 = 1), and the Shapiro–Wilks normality test (H0: Z ~ N (μ, σ 2)). Bootstrap analysis was also performed. For this, 2000 datasets of 18 subjects were resampled with replacement from the original dataset. The bias-corrected bootstrap with acceleration constant (BCa) method was used in order to obtain second-order correct 90% CIs around the parameter estimates [26]. This method corrects for bias and skewness in the standard bootstrap CIs and thus provides a more reliable estimate of the parameter CIs.
Results
The parameters of the final model are shown in Table 2. All model parameters could be estimated with adequate imprecision (RSE < 50%). Inter-individual variabilities could be estimated for K 0 (zero-order urine production rate), IC50 (dDAVP concentration which results in half the maximum urine production inhibition), and O 50 (urine volume resulting in 50% of maximal osmolality). A lag time mixture model was added to the PD model to account for differences in time to reach complete dilution versus the timing of drug administration between patients. Because the tablet and lyophilisate were dosed on separate days, an interoccasion variability was included as well, to account for differences within the patient between the two study days. The only covariate that significantly improved the model was the formulation: the IC50(for inhibition of urine production) was 0.7 pg/mL lower for the lyophilisate than for the tablet. The visual predictive check plots and NPDE results for both urine production and osmolality are depicted in Fig. 2, indicating good model performance. The numerical predictive check showed that 8.24% of the urinary volume observations lie above and 9.61% below the 90% prediction interval (PI), whereas for osmolality, these values are 3.23 and 3.01%, respectively.
These values should be around 5% in a good performing model. Plots of individual and population predictions plotted against the observations showed no significant deviations from the line of unity (data not shown). Regarding the NPDE results, no significant deviations from the standard normal distribution could be detected for either of the PD endpoints (Table 3), indicating that the model describes the data well. The 90% CIs of the BCa bootstrap analysis (1967/2000 runs completed minimization) are included in Table 2. The bootstrap estimates deviated between − 6.42 and + 14.12% from the model estimates, with an average deviation of − 0.08%.
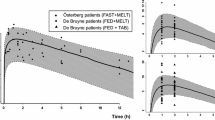
The effect of formulation on the IC50 seems to suggest that the lyophilisate has a more pronounced effect on the urine volume and osmolality than the tablet, even when the same exposure is achieved. This is shown in Fig. 4, which is the result of 1000 simulations of the study population after administration of a 120-μg lyophilisate or a 200-μg tablet. The 120-μg lyophilisate results in a lower urine volume and a higher urine concentration than the 200-μg tablet.
Discussion
Using dDAVP as an example drug, this study indicates that therapeutic equivalence between two different formulations of a drug (with narrow therapeutic range) established in adults does not necessarily guarantee therapeutic equivalence in children. This may lead to questioning the existing legislation for children in clinical practice. To the best of our knowledge, this is the first study where a population PKPD modeling approach was applied to previously obtained dDAVP data in children, with a reduced urine flow rate and a rise in urine osmolality as PD parameters [27]. The strength of this analysis is that the limitations of the original study, with limited plasma concentration samples but rich PD sampling, were partially overcome by using nonlinear mixed effects modeling to obtain the PKPD parameters [28].
Interestingly, by linkinga previously published PK model to a PD model, a significant effect of the pharmaceutical formulation on the IC50 was found. Since this is physiologically implausible, it must be explained by the use of the (predicted) plasma concentration as the input for the PD model, which causes formulation to lose its meaning. Only at the PK side, one could expect a formulation effect, as was found in the previous PK analysis [15], be it that higher doses of the lyophilisate seemed to be required to reach bioequivalence to the tablet in children, contrary to the findings in the current analysis. Assuming no contribution of metabolites to the PD effect, this effect of formulation on IC50 (IC50,MELT is 0.692 pg/mL lower than IC50,TAB) indicates that there is either a formulation effect in the PK part that was not captured by the PK model or a mismatch between the PK and PD models. Most likely, this discrepancy is explained by the PK sampling design of the original study [11]. Indeed, as was shown previously [15], the absorption of desmopressin is happening in the first hour after dosing. Unfortunately, in the original study, there was no blood sampling in the first hour, which is why an important part of the PK data (the absorption characteristics) is missing [11]. It is possible that the lyophilisate is absorbed so fast that a large peak in the concentration–time profile is not identified. Another possibility is the occurrence of two peaks, corresponding with a small fraction that is swallowed and a large fraction that is absorbed through the buccal mucosae. This implies that the true plasma concentrations of this formulation are underestimated, and the formulation effect on the PK side is thus also underestimated, which could also explain the findings of our previous PK analysis, where a higher dose of the lyophilisate seemed to be required to reach bioequivalence to the tablet. This would in turn lead to an overestimation on the PD side, as the (predicted) plasma concentrations linked to their respective osmolality and urine volume would be too low. This hypothesis is exemplified in Fig. 5. In this case, the use of population modeling revealed flaws in study design and suggested improvements for future clinical trials, i.e., the inclusion of more PK sampling in the absorption part.
Sampling too late can result in missing an early occurring peak in plasma concentrations. The black circles are the sampling times of the PK study that was analyzed [11], while the dotted line shows the part of the hypothetical lyophilisate concentration time profile that could have been missed (MISS)
Notwithstanding the aforementioned discrepancy between PK data and the PD effects, some inferences can already be gathered from the PD model. Both the high Hill factor (4.70) and low IC50 (2.08 pg/mL) indicate that dDAVP has a profound and fast effect, starting already at very low concentrations.
In adults, an even higher Hill factor (13) was found using the previous indirect response model by Callreus et al. [21], whereas the IC50 (3.7 ± 1.2 pg/mL) was comparable. Our model however starts from the urine volume as a response as opposed to the osmolality, which is more in line with the mechanism of action of desmopressin. The assumption of a zero-order urine production is supported within the scope of this study, as the children were pre-hydrated in order to suppress their endogenous AVP secretion, until minimum concentrating capacity was reached. The dDAVP has an approximately ten times higher antidiuretic potency than AVP, effectively removing the link between plasma osmolality and urine production.
Our data support the earlier observation that the lyophilisate has superior PD effects in children in comparison with the tablet [10], despite lower plasma concentrations in PK studies [11]. In the past, PD studies of dDAVP were mainly performed in young healthy men or in patients with diabetes insipidus or nocturia. Moreover, most PD data were collected in fasting state, while there is clearly an effect of concomitant food intake in adults and in children [10, 13, 15]. It is a well-known phenomenon that after oral dosing, there is a large inter-individual variability in plasma concentrations of dDAVP [29, 30]. However, an earlier PK analysis of these data showed a significantly smaller variability in plasma concentrations after lyophilisate dosing compared to tablet dosing [15]. Not only is this advantageous for the efficacy in individual patients, i.e., the antidiuretic effect (urinary volume per time unit) and the renal concentrating capacity (urinary osmolality); it is even more important for the safety, since the dose of dDAVP tends to be more correlated to the duration of action than to the maximal concentrating capacity [31]. This is especially important in children, in view of the increased risk of hyponatremia when the effect is prolonged and the ability to regain diluting capacity the next morning is lost [32].
A possible pitfall of this study is the fact that all patients in the study had a full stomach at the moment of dDAVP administration, since the main aim of the original study was to investigate the effect of food [10]. Urinary osmolality and diuresis correlate not only with the concentrating activity of dDAVP, but also with the renal osmotic load due to the meal. However, since all patients received a standard meal and were in a fed state, the relative effect of osmotic load does not obscure the findings. Furthermore, the study population was relatively small, and extra data should be gathered.
In order to confirm our hypothesis of a potential therapeutic difference between the two formulations, a formal, well-designed PKPD study should be performed in the pediatric population. Only then, the true difference between tablet and lyophilisate can be thoroughly characterized. A design for such a study was already proposed previously and includes more samples in the first hour after dosing [15]. We realize that our findings may put the current legislation into question and might induce reflections concerning generic products and maybe even biosimilars (since desmopressin is an oligopeptide). It is undeniable that there are ethical and practical considerations in performing large PKPD studies with multiple blood sampling in children. However, they should never overrule safety considerations when exposing children to drugs. Moreover, sensitive biomarkers are extremely important to explore the drug effect in pediatric drug studies. They can help to minimize the necessary number of patients to be exposed to study drug. Finally, practical issues in performing pediatric clinical drug trials can largely be overcome by population approaches as an option to explore the bioequivalence and therapeutic profile and minimize the burden for pediatric patients by optimizing trial design. This study indicates that minor changes in formulation make bioequivalence studies in children necessary and the collection of safety data required, in view of the derived therapeutic equivalence. Appropriate PKPD studies are thus pivotal in the pediatric population, not only for every new drug but also for every new formulation.
References
Steinbrook R (2002) Testing medications in children. N Engl J Med 347(18):1462–1470. https://doi.org/10.1056/NEJMhpr021646
European Agency for the Evaluation of Medicinal Products. Note for guidance on the investigation of bioavailability and bioequivalence. London: EMEA. 2001
Food and Drug Administration. Guidance for industry bioequivalence studies with pharmacokinetic endpoints for drugs submitted under an ANDA. Silver Spring: CDER. 2013
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE (2003) Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med 349(12):1157–1167. https://doi.org/10.1056/NEJMra035092
Rittig S, Knudsen UB, Norgaard JP et al (1989) Abnormal diurnal rhythm of plasma vasopressin and urinary output in patients with enuresis. Am J Phys 256:F664–F671
Fjellestad-Paulsen A, Höglund P, Lundin S, Paulsen O (1993) Pharmacokinetics of 1-deamino-8-d-arginine vasopressin after various routes of administration in healthy volunteers. Clin Endocrinol 38(2):177–182. https://doi.org/10.1111/j.1365-2265.1993.tb00990.x
van Kerrebroeck P, Norgaard JP (2009) Desmopressin for the treatment of primary nocturnal enuresis. Ped Health 3:317–327
Østerberg O, Savic RM, Karlsson MO, Simonsson USH, Nørgaard JP, Walle JV, Agersø H (2006) Pharmacokinetics of desmopressin administrated as an oral lyophilisate dosage form in children with primary nocturnal enuresis and healthy adults. J Clin Pharmacol 46(10):1204–1211. https://doi.org/10.1177/0091270006291838
Schulman SL, Stokes A, Salzman PM (2001) The efficacy and safety of oral desmopressin in children with primary nocturnal enuresis. J Urol 166(6):2427–2431. https://doi.org/10.1016/S0022-5347(05)65608-X
De Guchtenaere A, Van Herzeele C, Raes A, Dehoorne J, Hoebeke P, van Laecke E, Vande Walle J (2011) Oral lyophylizate formulation of desmopressin: superior pharmacodynamics compared to tablet due to low food interaction. J Urol 185(6):2308–2313. https://doi.org/10.1016/j.juro.2011.02.039
De Bruyne P, De Guchtenaere A, Van Herzeele C, Raes A, Dehoorne J, Hoebeke P, van Laecke E, Vande Walle J (2014) Pharmacokinetics of desmopressin administered as tablet and oral lyophilisate formulation in children with monosymptomatic nocturnal enuresis. Eur J Pediatr 173(2):223–228. https://doi.org/10.1007/s00431-013-2108-2
Goessaert A-S, Everaert K, Hoebeke P, Vande Walle J (2015) Pharmacokinetics and pharmacodynamics of the oral disintegrating tablet of desmopressin in adults with nocturnal polyuria: a pilot study. Adv Ther Published Online First 32(9):799–808. https://doi.org/10.1007/s12325-015-0247-8
Rittig S, Jensen a R, Jensen KT et al (1998) Effect of food intake on the pharmacokinetics and antidiuretic activity of oral desmopressin (DDAVP) in hydrated normal subjects. Clin Endocrinol 48(2):235–241. https://doi.org/10.1046/j.1365-2265.1998.00340.x
Lottmann H, Froeling F, Alloussi S, el-Radhi AS, Rittig S, Riis A, Persson BE (2007) A randomised comparison of oral desmopressin lyophilisate (MELT) and tablet formulations in children and adolescents with primary nocturnal enuresis. Int J Clin Pract 61(9):1454–1460. https://doi.org/10.1111/j.1742-1241.2007.01493.x
Michelet R, Dossche L, De Bruyne P, Colin P, Boussery K, Vande Walle J, van Bocxlaer J, Vermeulen A (2016) Effects of food and pharmaceutical formulation on desmopressin pharmacokinetics in children. Clin Pharmacokinet 55(9):1159–1170. https://doi.org/10.1007/s40262-016-0393-4
Juul KV, Erichsen L, Robertson GL (2013) Temporal delays and individual variation in antidiuretic response to desmopressin. Am J Physiol Renal Physiol 304(3):268–278. https://doi.org/10.1152/ajprenal.00502.2012
Aperia A, Celci G (1992) Ontogenic processes in nephron epithelia. In: Giebisch DW, Seldin G (eds) The kidney: physiology and pathophysiology. Raven, New York, pp 803–828
ICH Harmonised Tripartite Guideline. Guideline for good clinical practice E6(R1). ICH Harmon Tripart Guidel 1996;1996:i-53. doi:https://doi.org/10.1056/NEJMp1012246
Jusko WJ, Ko HC (1994) Physiologic indirect response models characterize diverse types of pharmacodynamic effects. Clin Pharmacol Ther 56(4):406–419. https://doi.org/10.1038/clpt.1994.155
Dayneka NL, Garg V, Jusko WJ (1993) Comparison of four basic models of indirect pharmacodynamic responses. J Pharmacokinet Biopharm 21(4):457–477. https://doi.org/10.1007/BF01061691
Callreus T, Odeberg J, Lundin S (2000) Indirect-response modeling of desmopressin at different levels of hydration. J Pharmacokinet Biopharm 27(5):513–529. https://doi.org/10.1023/A:1023238514015
Boeckmann AJ, Sheiner LB, Beal SL. NONMEM Users Guide - Part VIII Help Guide. 2006
Brendel K, Comets E, Laffont C, Mentré F (2010) Evaluation of different tests based on observations for external model evaluation of population analyses. J Pharmacokinet Pharmacodyn 37(1):49–65. https://doi.org/10.1007/s10928-009-9143-7
Holford N. An introduction to visual predictive checks outline what is a VPC ? Page 2012
Comets E, Brendel K, Mentré F (2008) Computing normalised prediction distribution errors to evaluate nonlinear mixed-effect models: the npde add-on package for R. Comput Methods Prog Biomed 90(2):154–166. https://doi.org/10.1016/j.cmpb.2007.12.002
Efron B (1987) Better bootstrap confidence intervals. J Am Stat Assoc 82(397):171–185. https://doi.org/10.2307/2289144
Fjellestad-Paulsen a WS, Harris a S (1987) Comparison of intranasal and oral desmopressin for nocturnal enuresis. Arch Dis Child 62(7):674–677. https://doi.org/10.1136/adc.62.7.674
De Cock RFW, Piana C, Krekels EHJ, Danhof M, Allegaert K, Knibbe CAJ (2011) The role of population PK-PD modelling in paediatric clinical research. Eur J Clin Pharmacol 67(S1):5–16. https://doi.org/10.1007/s00228-009-0782-9
Kaehler ST, Steiner IM, Sauermann R, Scheidl H, Mueller M, Joukhadar C (2006) A bioequivalence study of two oral desmopressin tablet formulations. Pharmacology 77(1):46–52. https://doi.org/10.1159/000092625
Steiner I, Kaehler S, Sauermann R et al (2006) Plasma pharmacokinetics of desmopressin following sublingual administration: an exploratory dose-escalation study in healthy male volunteers. Int J Clin Pharmacol Ther 44(04):172–179. https://doi.org/10.5414/CPP44172
Vande Walle JGJ, Bogaert GA, Mattsson S et al (2006) A new fast-melting oral formulation of desmopressin: a pharmacodynamic study in children with primary nocturnal enuresis. BJU Int 97(3):603–609. https://doi.org/10.1111/j.1464-410X.2006.05999.x
Walle JV, Stockner M, Raes A et al (2007) Desmopressin 30 years in clinical use : a safety review. Curr Drug Saf 2:1–7
Acknowledgements
This study was funded by the “Agency for Innovation by Science and Technology in Flanders (IWT)” through the “SAFE-PEDRUG” project (IWT-SBO 130033).
Contributions of authors statement
C. Van Herzeele, A. Vermeulen, and J. Vande Walle conceptualized the study. L. Dossche and J. Vande Walle prepared and delivered the dataset. R. Michelet and L. Dossche contributed equally to the interpretation of the data for the work, literature search, drafting of the initial manuscript, and revising of the subsequent drafts. R. Michelet and A. Vermeulen performed the population PKPD modeling analysis. C. Van Herzeele, J. Van Bocxlaer, A. Vermeulen, and J. Vande Walle critically reviewed and revised the manuscript. All the authors approve the final manuscript as submitted. All the authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflicts of interest
This study was funded by the “Agency for Innovation by Science and Technology in Flanders (IWT)” through the “SAFE-PEDRUG” project (IWT-SBO 130033).
L. Dossche received a travel reimbursement from Ferring Pharmaceuticals for a presentation at the Ghent-Aarhus Spring School.
R. Michelet declares that he has no conflict of interest.
C. Van Herzeele received a travel reimbursement from Ferring Pharmaceuticals for a presentation at the Ghent-Aarhus Spring School.
A. Vermeulen is a part-time employee of Janssen R&D and holds stock/stock options of J&J.
J. Van Bocxlaer declares that he has no conflict of interest.
J. Vande Walle has received consulting fees and travel reimbursements from Ferring Pharmaceuticals and payment for lectures from Ferring pharmaceuticals and Astellas Pharma.
R. Michelet J. Van Bocxlaer declares that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed consent
“Informed consent was obtained from all individual participants included in the study.”
Rights and permissions
About this article
Cite this article
Michelet, R., Dossche, L., Van Herzeele, C. et al. Claiming desmopressin therapeutic equivalence in children requires pediatric data: a population PKPD analysis. Eur J Clin Pharmacol 74, 297–305 (2018). https://doi.org/10.1007/s00228-017-2386-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2386-0