Abstract
Epilepsies occur across the entire age range, and their incidence peaks in the first years of life and in the elderly. Therefore, antiepileptic drugs (AEDs) are commonly used at the extremes of age. Rational prescribing in these age groups requires not only an understanding of the drugs’ pharmacodynamic properties, but also careful consideration of potential age-related changes in their pharmacokinetic profile. The present article, which updates a review published in 2006 in this journal, focuses on recent findings on the pharmacokinetics of new-generation AEDs in neonates, infants, children, and the elderly. Significant new information on the pharmacokinetics of new AEDs in the perinatal period has been acquired, particularly for lamotrigine and levetiracetam. As a result of slow maturation of the enzymes involved in glucuronide conjugation, lamotrigine elimination occurs at a particularly slow rate in neonates, and becomes gradually more efficient during the first months of life. In the case of levetiracetam, elimination occurs primarily by renal excretion and is also slow at birth, but drug clearance increases rapidly thereafter and can even double within 1 week. In general, infants older than 2–3 months and children show higher drug clearance (normalized for body weight) than adults. This pattern was confirmed in recent studies that investigated the pediatric pharmacokinetics of several new AEDs, including levetiracetam, rufinamide, stiripentol, and eslicarbazepine acetate. At the other extreme of age, in the elderly, drug clearance is generally reduced compared with younger adults because of less efficient drug-metabolizing activity, decreased renal function, or both. This general pattern, described previously for several AEDs, was confirmed in recent studies on the effect of old age on the clearance of felbamate, levetiracetam, pregabalin, lacosamide, and retigabine. For those drugs which are predominantly eliminated by renal excretion, aging-related pharmacokinetic changes could be predicted by measuring creatinine clearance (CLCR). Overall, most recent findings confirm that age is a major factor influencing the pharmacokinetic profile of AEDs. However, pharmacokinetic variability at any age can be considerable, and the importance of other factors should not be disregarded. These include genetic factors, co-morbidities, and drug interactions, particularly those caused by concomitantly administered AEDs which induce or inhibit drug-metabolizing enzymes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Epilepsies occur across the entire age range, and their incidence is known to peak in the first years of life and in the elderly [1]. Therefore, antiepileptic drugs (AEDs) are often used at the extremes of age, and age-related factors need to be considered in selecting the most appropriate drug and in optimizing dosage and dosing schedule in the individual patient. Treatment decisions must consider not only the spectrum of efficacy and adverse effect profile of the different medications, but also their pharmacokinetic properties and the implications of age-related changes in pharmacokinetics. Mastering the required information is an increasing challenge that physicians need to face, in view of the increasing number of AEDs which entered the market in the last two decades [1].
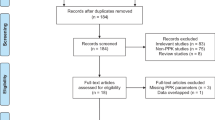
The influence of pediatric and old age on the pharmacokinetics of new-generation AEDs (defined as the AEDs introduced in the market after 1989), was reviewed comprehensively in 2006 [2]. Over the last few years, however, several studies have provided important new findings, which have implications for clinical management. The purpose of the present article is to review such findings by providing an update on the pharmacokinetics of new-generation AEDs in newborns, infants, children, and in the elderly. A summary of the main pharmacokinetic parameters of the same drugs in non-elderly adults, to be used as reference, is provided in Table 1. For complete information on this topic, the present article should be read in conjunction with our previous publication [2].
2 Pharmacokinetics of New-Generation Antiepileptic Drugs (AEDs) During Development
2.1 General Considerations
As discussed in greater detail in our earlier review [2], physiological changes during development can influence considerably the pharmacokinetics of many drugs. Specifically, compared with children and adults, neonates and infants exhibit higher total body water to body fat ratios, lower concentrations of plasma proteins, and altered tissue binding, all of which can affect volume of distribution (V d), unbound drug fraction in plasma, and elimination half-life (t ½) [3–5]. Renal function and drug-metabolizing enzyme activity are also reduced in newborns, particularly in those born prematurely, but increase rapidly during postnatal life. When expressed per unit of body weight, metabolic clearance (CL), in particular, can reach higher levels in infants and children than those found in adults [6].
Age-dependent changes in drug CL are reflected in parallel changes in serum drug concentration at steady state which, in turn, may impact on individual dose requirements. The shorter t ½ values that are often found in older infants and children may also result in greater fluctuation in serum drug levels during a dosing interval compared with adults. This could require more frequent daily dosing in order to minimize the risk of transient toxicity at time of peak and the risk of breakthrough seizures at time of trough.
A summary of age-related changes in the pharmacokinetics of new-generation AEDs in newborns, infants, and children is provided in Tables 2 and 3. A detailed description of findings reported for each of these drugs is provided in Sects. 2.2 and 2.3.
2.2 Newborns and Infants
2.2.1 Lamotrigine
Lamotrigine is approved in many countries worldwide for the treatment on focal and certain generalized seizure types in adults and children. Lamotrigine shows linear pharmacokinetics, complete oral bioavailability, and elimination primarily by uridine diphosphate-glucuronosyltransferase (UGT) 1A4-mediated glucuronidation [7, 8]. Its CL and t ½ are highly variable primarily because of the influence of drug interactions, which include inhibition of lamotrigine metabolism by valproic acid and stimulation of lamotrigine metabolism by enzyme-inducing AEDs and by estrogen-containing products [7, 8]. A reduction in the efficiency of lamotrigine metabolism in neonates was anticipated on the basis of the observation that glucuronide conjugation is poorly developed in neonates, particularly those born prematurely [2]. In agreement with this prediction, early studies [9, 10], reviewed previously in detail [2], provided evidence that transplacentally acquired lamotrigine is eliminated very slowly in the newborn, and that in early postnatal life the modest amounts of drug present in breast milk can produce appreciable serum lamotrigine concentrations in breast-fed infants, though not to an extent which would contraindicate breast-feeding. Preliminary data obtained in infants treated with lamotrigine were also consistent with a reduced drug CL, at least for the first 2 months after birth [9, 10].
Results of more recent studies provide an improved understanding of the pharmacokinetics of lamotrigine in the perinatal period. In a prospective investigation of six neonates born from mothers on lamotrigine monotherapy, the serum concentration of the drug in the infants at birth was similar to that in the mother and declined very slowly, with median serum concentration at 12 and 24 h post-birth being 92 and 90.5 % of maternal serum concentrations, respectively [11]. In the same study, the ratio of breast milk to maternal serum lamotrigine concentration ranged between 0.35 and 0.86, consistent with earlier reports [9]. Serum lamotrigine concentrations in the breast-fed infants ranged between 1.7 and 3.3 μg/mL during the first 12 weeks postpartum, or about 26 % (range 18–39 %) of the maternal concentration. In a larger study specifically focused on infant exposure through breast milk, the mean milk to plasma concentration in 25 mothers was 0.41, with considerable intra- and interindividual variability [12]. The relative infant dose ingested through breast milk was estimated to be on average 9 % of the maternal dose. The mean infant to maternal plasma concentration ratio, measured in 12 breast-fed infants 1.7–30 weeks after birth, was 0.18 (95 % CI 9.5–27 %) for total lamotrigine, and 0.31 for unbound lamotrigine, indicating that infants had a higher plasma unbound lamotrigine fraction than their mothers (53.5 vs 29.5 %). While these findings suggest that total plasma lamotrigine concentrations measured in the newborn may underestimate the amount of unbound, pharmacologically active drug, overall the available evidence suggests that exposure to lamotrigine through breast milk is relatively modest and that breast-feeding should not be contraindicated in lamotrigine-treated mothers.
2.2.2 Levetiracetam
Levetiracetam is approved in Europe and the USA for the adjunctive treatment of focal seizures and of certain generalized seizure types in adults and children. In the EU it is also approved as monotherapy in the treatment of focal seizures with or without secondary generalization in adults and adolescents from 16 years of age with newly diagnosed epilepsy. Levetiracetam shows linear pharmacokinetics, complete oral bioavailability, and a relatively short t ½ (6–8 h in adults). It is eliminated by urinary excretion in unchanged form (about 75 % of the administered dose) and by esterase-mediated hydrolysis to the inactive metabolite L057 [2, 7]. There is evidence that levetiracetam’s oral clearance (CL/F) is increased in subjects co-medicated with enzyme-inducing AEDs [13, 14].
Virtually all information on the pharmacokinetics of levetiracetam in neonates and infants has been acquired after publication of our previous review [2]. An early report by Johannessen et al. [15] indicated that neonatal serum levetiracetam concentrations at birth are similar to maternal serum concentrations and decline to low levels (<1.7–2.5 μg/mL) at reassessment 3–5 days later. Although levetiracetam is found in breast milk at concentrations similar to maternal serum concentrations, serum levetiracetam concentrations measured in infants during prolonged breast-feeding remain very low (<3.4 μg/mL), at about 13 % of the mother’s serum levels [15, 16].
An initial assessment of the rate of elimination of transplacentally acquired levetiracetam was provided by a study conducted in two bottle-fed healthy twins [16]. The t ½ of the drug during the first 36 h after birth was estimated at 16–18 h, which is considerably longer than that reported for older infants and adults (5–8 h) [17], presumably because of immaturity of renal excretory function in the newborn. In agreement with these data, the t ½ of levetiracetam in another study conducted in 13 neonates born from levetiracetam-treated mothers was found to average 18 h (range 6–28 h) [18]. All but one of these neonates were breast-fed, but the decline in plasma levetiracetam concentrations in the non-breast-fed neonate was not more rapid than in the other infants.
Two recent studies assessed the pharmacokinetics of levetiracetam in neonates receiving the drug for the treatment of ongoing seizures. Sharpe et al. [19] applied a nonlinear mixed-effects population analysis to assess changes in levetiracetam CL over time in 18 neonates (gestational age 36–41 weeks) treated with levetiracetam intravenously, starting with a bolus dose of 20 or 40 mg/kg followed by 5–10 mg/kg/day for 1 week. All neonates had seizures which had failed to respond to a 20 mg/kg dose of phenobarbital, and five were also treated with hypothermia during the study period. Levetiracetam CL increased from a mean of 42.6 ± 16.2 mL/h/kg on the first day of life, which is greater than expected from the immaturity in renal function, to 78.6 ± 21.0 mL/h/kg on day 7. The increase in CL during the first week of life was associated with a shortening of levetiracetam t ½, from 18.5 ± 7.1 h on day 1 to 9.1 ± 2.0 h on day 7. Mean V d remained stable over time at 1.01 ± 0.13 L/kg, which is considerably greater than that reported for older children (0.6–0.7 L/kg) [20] and adults (0.5–0.7 L/kg) [21]. Overall, these data indicate that levetiracetam CL increases rapidly after birth, virtually doubling during the first week of life. Measurements of unchanged drug and its metabolite L057 in urine suggested that both renal excretion and hydrolytic pathways increased in efficiency during this period. In the other study, Merhar et al. [22] evaluated 18 neonates given initial loading doses ranging from 14.4 to 39.9 mg/kg. The median gestational age of the neonates was 38 weeks, and the drug was administered after a median of 2 days after birth (range 0–32 days). The mean t ½ of levetiracetam in these neonates was 8.9 h (range 3.2–13.3 h) and correlated positively with serum creatinine levels, which is consistent with levetiracetam elimination being primarily dependent on renal function. Median V d was 0.89 L/kg (range 0.37–1.26 L/kg), which is higher than that previously reported for older children (0.6–0.7 L/kg) [20] and adults (0.5–0.7 L/kg) [21]. Median CL was 72.6 mL/h/kg (range 28.2–173.4 mL/h/kg), which is comparable to that reported by Sharpe et al. [19] 7 days after birth and intermediate between the value reported for children aged 6–12 years (85.8 mL/h/kg) [20] and that reported for adults (56.4 mL/h/kg) [21].
Information on the comparative pharmacokinetics of levetiracetam in infants and young children with epilepsy was provided by Glauser et al. [18]. Their study investigated 12 subjects aged 2–46 months (<24 months for 9 of the participants), who were administered a single 20 mg/kg dose as a 10 % oral solution. Levetiracetam was found to be rapidly absorbed and reached peak plasma concentrations (C max) of 31.3 ± 6.7 μg/mL at 1.4 ± 0.9 h after dosing. The drug was eliminated rapidly, with a mean t ½ of 5.3 ± 1.3 h, and a CL/F of 87.6 ± 25.2 mL/h/kg. There were modest pharmacokinetic differences across the age range investigated, with CL/F being fastest in children aged 6 months and older (94.2 mL/h/kg) and slowest in infants under 6 months of age (73.8 mL/h/kg), a finding which presumably reflects the gradual increase in glomerular filtration rate during the first 6 months of life. Overall, CL/F values in these children and infants were comparable to those reported in children aged 6–12 years [20] and higher than those reported in adults [21]. Systemic exposure to the inactive metabolite ucb L057 was similar to that found in older children and adults. These data indicate that there are no pharmacokinetic reasons to expect major differences in levetiracetam dose requirements between 2 months and 12 years of age, and that infants and children require larger doses than adults to achieve comparable serum drug concentrations.
2.2.3 Oxcarbazepine
Oxcarbazepine, a carbamazepine derivative, is approved in Europe and the USA for the treatment of focal seizures in adults and children. After oral administration, it undergoes extensive first-pass metabolism by non-microsomal keto reduction to the active monohydroxy derivative (MHD), for which it can be considered as a prodrug [2, 7]. In adults, MHD shows linear pharmacokinetics, a t ½ of 7–15 h, and clearance predominantly by glucuronide conjugation. Enzyme-inducing AEDs can stimulate the metabolism of MHD and reduce its concentration in serum [7].
Northam et al. [23] applied a population pharmacokinetic model to describe the plasma levels of MHD in 23 infants and children aged 2–45 months (mean 20 months) who underwent gradual titration of oxcarbazepine from a dose of 10 up to 60 mg/kg/day. Serum MHD concentrations were linearly related to dose. Mean MHD CL/F in the group receiving enzyme-inducing co-medication (96 ± 24 mL/h/kg, n = 12) was 35 % higher than in the group receiving monotherapy or co-medication with AEDs devoid of enzyme-inducing properties (71 ± 15 mL/h/kg, n = 11). No clear age-related trends in CL/F were reported, although this observation should be interpreted cautiously because of the limited number of subjects included in the study.
Another study investigated plasma MHD levels in 119 infants and young children aged 1 month to less than 4 years, who were randomized to receive either high-dosage (60 mg/kg/day) or low-dosage (10 mg/kg/day) oxcarbazepine on a twice daily schedule as oral suspension [24]. The median trough plasma MHD concentration in the high-dosage group (14.9 μg/mL, range 1.8–38.7 μg/mL) was about sixfold greater than that recorded in the low-dosage group (2.5 μg/mL, 0.5–9.3 μg/mL), which is consistent with a linear relationship between dose and plasma concentration.
2.2.4 Topiramate
Topiramate is approved in Europe and the USA for the treatment of focal seizures and certain generalized seizure types in adults and children. After oral administration, topiramate is well absorbed from the gastrointestinal tract, shows linear pharmacokinetics, and is eliminated partly in unchanged form in urine and partly by oxidative metabolism to several inactive metabolites. Its t ½ in adults is about 20–30 h and considerably shorter (10–15 h) in patients co-medicated with enzyme-inducing AEDs [2, 7].
Information on the elimination of transplacentally acquired topiramate appears to be limited to a report in five newborns from mothers treated with topiramate and carbamazepine during pregnancy [25]. The t ½ of the drug in these newborns was 24 h on average, which is similar to values reported in healthy adults. In view of the interest in evaluating topiramate as a potential neuroprotective agent against hypoxic brain damage, its pharmacokinetics were also investigated in neonates receiving prolonged whole body hypothermia, a treatment for hypoxic ischemic encephalopathy [26]. Thirteen full-term asphyxiated newborns (age at inclusion 4.0 ± 1.7 h) receiving mild or deep whole body hypothermia for 72 h were given topiramate 5 mg/kg orally once daily for 3 days, in monotherapy or in combination with phenobarbital. Plasma topiramate concentrations were within the reference range (5–20 μg/mL) [7, 27] in 11 neonates, and above range in the remaining two cases. Pharmacokinetic parameters were calculated for the nine neonates who had achieved steady state by 48 h. In these neonates, plasma topiramate concentrations were 18.0 ± 4.2 μg/mL at time of peak and 10.3 ± 2.5 μg/mL at time of trough, t ½ was estimated to be 35.6 ± 19.3 h, and CL/F was 15.4 ± 4.6 mL/h/kg. Although sample size was inadequate to assess potential pharmacokinetic differences among subgroups, there was a trend for plasma topiramate concentrations to be higher and more variable in neonates exposed to deep hypothermia than in those exposed to mild hypothermia, and for CL/F to be higher and t ½ values to be shorter in the neonates co-treated with phenobarbital. On the basis of these data, the authors suggested that plasma topiramate concentrations are higher in neonates exposed to hypothermia than in normothermic infants and children treated with similar doses [25, 26, 28]. Whether hypothermia per se affects topiramate pharmacokinetics, however, would require a direct comparison in normothermic neonates comparable for gestational and postnatal age.
In a separate study, Manitpisitkul et al. [29] assessed the pharmacokinetic profile of topiramate in 55 infants (age 1–24 months) who received 7-day treatment with the drug. Topiramate was administered twice daily in addition to at least another AED, at dosages ranging between 3 and 25 mg/kg/day in different patient subgroups. The drug was found to exhibit linear pharmacokinetics over the assessed dose range, and CL/F values were independent of age. Topiramate CL/F was approximately twofold greater in infants receiving concomitant enzyme-inducing AEDs (84.6 ± 22.8 mL/h/kg, n = 10) or enzyme-inducing AEDs combined with valproic acid (86.4 ± 46.8 mL/h/kg, n = 5) than in those receiving valproic acid without an inducer (42.6 ± 10.8 mL/h/kg, n = 19). CL/F values in this study were comparable to those described by Mikaeloff et al. [30] in 22 infants and young children (range 6 months–4 years), receiving co-medication with enzyme-inducing AEDs (85.2 ± 85.2 mL/h/kg) or with valproic acid (42.6 ± 49.2 mL/h/kg). The mean CL/F in the co-medication subgroups of infants investigated by Manitpisitkul et al. [29] was also twice as high as that reported earlier in adults receiving comparable treatments (39.6 mL/h/kg for those on enzyme-inducing co-medications and 19.2 mL/h/kg for those on valproic acid co-medication) [7, 27], an observation which confirms the general pattern of drug CL to be higher in infants and children compared to adults.
Using previously published data from 22 children aged 6 months to 4 years [30], Bouillon-Pichault et al. [31] developed a pharmacokinetic model to predict topiramate dosing requirements in infants and young children. According to the model, the currently recommended topiramate dosage regimen of 3–6 mg/kg/day in monotherapy provides area under the serum concentration time curve from 0 to 12 h (AUC12) values between 19.6 ± 3.1 and 39.2 ± 11.7 mg·h/L for 6-month-old children and between 40.8 ± 6.5 and 81.6 ± 24.5 mg·h/L for 4-year-old children. When topiramate is combined with enzyme-inducing AEDs, the currently recommended topiramate dosage regimen of 5–9 mg/kg/day provides a mean AUC12 between 17.3 ± 15.18 and 31.08 ± 9.33 mg·h/L for 6-month-old children and between 35.9 ± 10.8 and 64.7 ± 19.5 mg·h/L for 4-year-old children. On the basis of these estimations, topiramate CL/F appears to be on average about twofold greater in 6-month-old infants than in older children, both in the presence and in the absence of associated enzyme-inducing AEDs.
2.2.5 Vigabatrin
Vigabatrin, an irreversible GABA-transaminase inhibitor which is considered to exert its activity by increasing brain GABA levels, is approved in Europe and the USA as monotherapy for infantile spasms, its current main indication. Vigabatrin is also approved for the adjunctive treatment of focal seizures, but it is rarely used today in this indication because of the risk of irreversible visual field defects and the availability of safer alternatives. The main pharmacokinetic features of vigabatrin in adults include rapid absorption from the gastrointestinal tract, a t ½ of 6–8 h, and elimination by renal excretion in unchanged form. Although vigabatrin is a racemate, only the S-enantiomer is pharmacologically active. After oral intake, peak plasma concentrations of the S-enantiomer are about one-half those of the R-enantiomer (probably as a result of lower bioavailability), but the t ½ (6–8 h) is comparable for both enantiomers [32].
An early study, not cited in our previous review, investigated the pharmacokinetics of vigabatrin in 6 neonates (mean age 21 days, range 15–26 days) who received a single 125 mg oral dose (about 40 mg/kg) after emptying the contents of a capsule in a few milliliters of water [33]. Compared with the inactive R-enantiomer, the active S-enantiomer showed on average lower peak plasma concentrations (14.3 vs 34.1 μg/mL, respectively) and lower AUC values (143 vs 231 mg·h/L, respectively), whereas t ½ (7.5 h on average) was identical for the two enantiomers. Comparison with data from another study by the same group [34] suggested that AUC values for both enantiomers are higher in neonates than in children. In particular, after normalization for dose and body weight, the AUC of the S-enantiomer in neonates was on average 98 % higher than in young children aged 5 months to 2 years and 52 % higher than in older children aged 4 to 14 years.
2.2.6 Other Drugs
Limited information on the pharmacokinetics of gabapentin [35, 36] and zonisamide [37–40] in neonates and infants was summarized in our earlier review [2]. No information appears to be available on the pharmacokinetics of eslicarbazepine acetate, felbamate, lacosamide, perampanel, pregabalin, retigabine (ezogabine), rufinamide, stiripentol, and tiagabine in infants and neonates.
2.3 Children
2.3.1 Eslicarbazepine Acetate
Eslicarbazepine acetate is an oxcarbazepine derivative approved in the EU in 2009 as adjunctive treatment for adults with focal seizures, with and without secondary generalization. The compound acts primarily as a prodrug of eslicarbazepine [(S)-licarbazepine], which corresponds to the S-enantiomer of the MHD of oxcarbazepine [41]. In adults, eslicarbazepine has a t ½ of about 12–20 h and is eliminated in urine partly in unchanged form and partly in conjugated form.
Almeida et al. [42] compared the pharmacokinetics of eslicarbazepine acetate at steady state in 11 children aged 2–6 years, 8 children aged 7–11 years, and 10 adolescents aged 12–17 years. As in adults, the drug was rapidly metabolized to eslicarbazepine, with (R)-licarbazepine and oxcarbazepine being minor metabolites. Plasma eslicarbazepine concentrations were linearly related to dose over the 5–30 mg/day (or up to 1,800 mg/day, whichever was less) dosage range. Peak eslicarbazepine concentrations were usually reached 0.5–3 h after dosing and were similar across the three age groups. However, AUC values during a 24-h interval increased with increasing age, as a result of higher eslicarbazepine CL/F values in the younger groups. Compared with adolescents, mean CL/F calculated at a dosage of 15 mg/kg/day was 51 % higher in children aged 2–6 years, and 25 % higher in those aged 7–11 years. These findings indicate that in children there is an inverse relationship between eslicarbazepine CL/F and age, as reported for other AEDs.
2.3.2 Lamotrigine
Because lamotrigine has been used extensively in the treatment of pediatric epilepsies since the mid 1990s, most pharmacokinetic studies with this drug in children were performed several years ago [10, 43–46]. As summarized in our previous review [2], lamotrigine CL/F values have been found be on average 35–125 % higher in children than in adults. In general, CL/F values tend to be highest in the youngest age groups and to decline gradually with increasing age [47, 48]. Children typically show a marked variability in serum lamotrigine concentrations achieved at the same dosage. Factors that contribute to such variability include not only differences in age, but also changes in lamotrigine metabolism caused by concomitant administration of other AEDs. Specifically, serum lamotrigine levels are markedly increased by valproic acid, and reduced by enzyme-inducing AEDs such as carbamazepine, phenytoin, and barbiturates [43–49].
A recent study investigated differences in the plasma concentrations of several new-generation AEDs in relation to age in a large population of patients referred to a therapeutic drug monitoring (TDM) service [50]. For lamotrigine, there was a trend for CL/F values to decrease with increasing age from a mean of 115 mL/h/kg in young children (age 2–9 years, n = 48) to a mean of 99 mL/h/kg in older children (age 10–17 years, n = 29) and 95 mL/h/kg in adults (age 18–64 years, n = 251). The influence of age on lamotrigine pharmacokinetics, however, was probably underestimated in this comparison because of the confounding effects of interacting co-medications. Most notably, co-medication with valproic acid, which is known to reduce lamotrigine CL/F, was used much more commonly in children than in adults. Several recent studies, some of which included Chinese populations [51, 52], used population pharmacokinetics to model the distribution of serum lamotrigine concentrations in children [51–54]. In one such study, Reimers et al. [53] applied the linear mixed model to investigate factors affecting dose-normalized serum lamotrigine concentrations in a TDM service. A total of 744 measurements in 296 subjects aged 2–19 years were assessed. According to the model, lamotrigine concentration/dose ratio decreased by 6 % per year of age, which seems to contradict prior evidence indicating that lamotrigine CL/F values are highest in younger children. A probable explanation for this apparent discrepancy is that, unlike the vast majority of studies, Reimers et al. [53] expressed concentration/dose ratios without normalizing for body weight. The same study confirmed that lamotrigine levels are reduced by carbamazepine and oral contraceptives, and increased by valproic acid. Other drugs were also suggested to possibly affect lamotrigine levels, but the significance of these observations is unclear because of the potential role of confounders and the small number of children receiving these co-medications.
2.3.3 Levetiracetam
Following the initial report by Pellock et al. [20] suggesting that levetiracetam CL/F is about 30–40 % higher in children aged 6–12 years than in adults, several studies have assessed the pharmacokinetics of levetiracetam in pediatric age. In a prospective multiple-dose investigation in 21 children aged 4–12 years (mean 10.2 ± 2.2 years) receiving combination therapy with carbamazepine or valproic acid, Fountain et al. [55] found that levetiracetam displays linear and dose-proportional pharmacokinetics over the dose range of 20–60 mg/kg/day. The t ½ of the drug in these children was 4.9 h on average, and CL/F values were 7–13 % higher in those co-medicated with carbamazepine (n = 13) than in those co-medicated with valproic acid (n = 8). Overall, this study supported the earlier finding [20] that levetiracetam CL/F is higher in children than in adults.
A recent analysis of data collected by a large TDM service confirmed that age has a prominent influence on levetiracetam pharmacokinetics [50]. Specifically, mean levetiracetam CL/F values in children aged 2–9 years (375 mL/h/kg, n = 42) were 60 % higher than those found in adults (233 mL/h/kg, n = 167). In older children (age 10–17 years), CL/F values were similar to those reported for adults. Another study used TDM data to investigate the factors influencing levetiracetam dose/concentration ratios in 103 children aged 0.66–17.9 years [56]. CL/F was calculated using trough serum levetiracetam concentrations, and therefore they are likely to represent overestimates. CL/F values were found to be higher in children below 5 years of age (221 ± 87 mL/h/kg) than in those aged 5–11.9 years (171 ± 71 mL/h/kg) and those aged 12 years and older (125 ± 46 mL/h/kg). In the overall population, CL/F was on average about 30 % higher in children receiving enzyme-inducing AEDs (200 mL/h/kg, n = 24) than in those receiving levetiracetam in monotherapy (140 mL/h/kg, N = 10) or in combination with non-enzyme inducers (153 mL/h/kg, n = 69). A 22 % increase in levetiracetam CL/F in children receiving enzyme inducers compared with those not receiving enzyme inducers was also reported by Toublanc et al. [57] in a population pharmacokinetic study that included 228 children aged 3 months to 18 years. The latter study confirmed that children have higher CL/F than adults and that, on average, a levetiracetam dosage of 10 mg/kg twice daily ensures the same exposure in children as does 500 mg twice daily in adults. Similar dosing estimates were reported in a smaller population pharmacokinetic study that included 44 children between 4 and 16 years of age [58]. Population pharmacokinetic modeling of levetiracetam after intravenous dosing in children has also been reported [59].
In a pooled analysis of randomized adjunctive-therapy trials in children receiving one or two concomitant AEDs, levetiracetam was found not to affect the plasma concentrations of carbamazepine, valproic acid, topiramate, or lamotrigine [60]. This is consistent with previously reported results in adults and in children [61, 62].
2.3.4 Oxcarbazepine
As reported in more detail in our previous review [2], the serum concentrations of MHD, for which oxcarbazepine is a prodrug, are considerably lower in children than in adults receiving comparable oxcarbazepine doses (mg/kg), presumably because of accelerated elimination of the metabolite [63]. Children aged 2–5 years have lower serum MHD concentrations than children aged 6–12 years [64, 65]. Because the t ½ of MHD is shorter in children than in adults, children also show greater fluctuations in the serum MHD concentrations during a dosing interval compared with adults [64, 65]. Enzyme-inducing AEDs have a lowering effect on serum MHD concentrations, an interaction that occurs not only in adults but also in children [63, 65]. No novel findings on oxcarbazepine pharmacokinetics in children appear to have been reported in recent years, except for a TDM-based study in which mean MHD CL/F values were found to be only slightly increased in children aged 2–9 years compared with older children and adults [50]. These data, however, should be interpreted cautiously because the number of children included in the analysis was small and a potential confounding effect of interacting co-medications cannot be excluded.
2.3.5 Perampanel
Perampanel is a selective non-competitive AMPA receptor antagonist, which was approved in 2013 in the EU and the USA for the adjunctive treatment of focal seizures in patients aged 12 years and older [66, 67]. Perampanel shows linear pharmacokinetics, almost complete oral bioavailability, and elimination by cytochrome P450 (CYP) 3A4-mediated oxidation followed by glucuronidation [66]. The t ½ of perampanel is approximately 105 h in adults not receiving enzyme inducers, and considerably shorter (25 h) in adults co-medicated with carbamazepine, presumably owing to induction of oxidative metabolism [66].
Information on perampanel pharmacokinetics in children appears to be limited to an analysis of serum perampanel levels in a group of 74 subjects aged less than 18 years with complete dosing and sampling information who participated in adjunctive-therapy phase III studies [66]. The mean weight-uncorrected CL/F value of perampanel in these subjects (787 mL/h) was slightly higher than that found in adult patients (730 mL/h in males, 605 mL/h in females).
2.3.6 Rufinamide
Rufinamide is an AED recently approved in the EU and the USA for the adjunctive treatment of seizures associated with the Lennox–Gastaut syndrome in patients aged 4 years and older [68]. Rufinamide is absorbed relatively slowly from the gut because of poor dissolution into gastrointestinal fluids. Its pharmacokinetics are non-linear because bioavailability decreases with increasing doses within the clinically used dose range [69]. The t ½ of rufinamide is about 10 h in healthy adults and 7 h in patients co-medicated with enzyme-inducing AEDs. The drug is extensively metabolized and the primary pathway involves conversion by carboxylesterases to an inactive carboxylacid derivative. Serum rufinamide levels are reduced by co-medication with enzyme-inducing AEDs, and increased by co-medication with valproic acid [69].
Despite rufinamide’s frequent use in pediatric age, differences in its pharmacokinetics between children and adults have not been investigated systematically in formal studies. Moreover, in most studies conducted to date, it has been difficult to disentangle the effect of age from that of other variables affecting rufinamide pharmacokinetics, including body weight, dose, pharmaceutical formulation, and co-medication with interacting drugs [69]. In a pooled pharmacokinetic analysis of data collected by the manufacturer, rufinamide CL/F (mL/h/kg) at a dose of 45 mg/kg, in the absence of interacting co-medications, was predicted to be about 50 % higher in a 17-kg, 4-year-old boy compared with an 80-kg man [69]. However, because of the small number of subjects not receiving interacting drugs, these estimates were considered to be theoretical values to be confirmed in prospective studies. Co-administered AEDs not interacting with rufinamide in this analysis included lamotrigine, topiramate, and benzodiazepines. On the other hand, co-medication with carbamazepine, vigabatrin, phenytoin, phenobarbital, and primidone were associated with modest-to-moderate (<50 %) decreases in plasma rufinamide concentrations. Valproic acid was associated with an elevation in rufinamide concentrations, which was much greater in children (average increase by 55 % in boys and 70 % in girls) than in adolescents and adults (15–26 % increase). The greater effect of valproic acid in children compared with older age groups could be due to the fact that the degree of interaction, presumably mediated by inhibition of rufinamide metabolism, was proportional to plasma valproic acid concentrations, which were highest in children.
In a retrospective analysis of TDM data, May et al. [70] evaluated 292 serum rufinamide measurements from 119 patients, 43 of whom were younger than 12 years. In agreement with previous findings [69], trough rufinamide concentrations increased less than proportionally with increasing dose. At comparable doses (mg/kg), serum concentrations were 19 % lower in children younger than 12 years than in adults. The study also confirmed that serum rufinamide levels are increased by valproic acid (+34 % on average) and decreased by enzyme-inducing AEDs (−23.7 %) compared with a reference group of patients receiving neither valproic acid nor enzyme inducers. The concentration-dependency of the interaction with valproic acid was also confirmed. Compared with subjects not receiving valproic acid, mean serum rufinamide levels were 86.6 % higher at valproic acid concentrations greater than 90 μg/mL, 45.4 % higher at valproic acid concentrations between 50 and 90 μg/mL, and not significantly different (+4.4 %) at valproic acid concentrations less than 50 μg/mL.
The complex relationships between age and interactions from concomitant AEDs were highlighted by another retrospective study in 51 children aged 1.7 to 17.9 years [71]. Mean rufinamide CL/F values in young children (<5 years) receiving enzyme inducers without valproic acid were threefold higher than those found in similarly treated older children. Young children neither on valproic acid nor on enzyme inducers also had higher rufinamide CL/F values than older children. In children on valproic acid, on the other hand, with or without enzyme inducers, no major age-related differences in rufinamide CL/F were identified. Young children on valproic acid, with or without enzyme inducers, had much lower rufinamide CL/F than young children not on valproic acid. Children of any age on valproic acid showed only modest differences in rufinamide CL/F in relation to co-administration of enzyme inducers.
In a placebo-controlled trial that included 171 adolescents and adults with focal seizures, neither age nor gender was found to influence rufinamide pharmacokinetics [72]. As in other studies, patients co-medicated with valproic acid showed a decrease in rufinamide CL/F which was proportional to the serum valproic acid concentration (23 % decrease at a valproic acid concentration of 100 μg/mL).
2.3.7 Stiripentol
Stiripentol was approved in the EU in 2007 for use in conjunction with clobazam and valproic acid as adjunctive therapy for refractory generalized tonic-clonic seizures in patients with severe myoclonic epilepsy in infancy (Dravet syndrome) whose seizures are not adequately controlled with clobazam and valproic acid. Information on stiripentol pharmacokinetics is mostly derived from studies in adults, which demonstrated rapid gastrointestinal absorption, extensive (>95 %) binding to plasma proteins, and a non-linear relationship between plasma concentration and dose [73, 74]. In particular, stiripentol CL/F has been found to decrease with increasing doses. In a study in adults with epilepsy, an increase in dose from 600 to 2,400 mg was associated with a fivefold decrease in CL/F, from approximately 1,650 mL/h/kg to about 330 mL/h/kg [73]. The t ½ of stiripentol is in the range of 4.5–13 h, increasing with dose. Stiripentol is cleared extensively by metabolism involving CYPs and other enzymes. The main CYP enzymes which metabolize stiripentol in vitro include CYP1A2, CYP2C19, and CYP3A4 [73]. Stiripentol is a potent inhibitor of the activity of CYP2C19, CYP3A34, and CYP2D6 and can increase by this mechanism the plasma levels of many concurrently administered drugs, the dose of which may need to be reduced [73, 75].
Despite the fact that stiripentol is used primarily in children, there is surprisingly little information on stiripentol pharmacokinetics in pediatric populations; the only information mentioned relates to its use in the EU. The summary of product characteristics [73] refers to a population pharmacokinetic study conducted in 35 children with Dravet syndrome aged 1–17.6 years (median 7.3 years), who received stiripentol (27–89 mg/kg/day in two or three divided doses) in addition to valproic acid and clobazam. In this analysis, CL/F and V d were related to body weight by an allometric model with exponents of 0.433 and 1, respectively. As body weight increased from 10 to 60 kg, CL/F increased from 2.60 to 5.65 L/h (a change which, after normalizing for body weight, corresponds in fact to a decrease in CL/F from 260 to 94 mL/h/kg), and V d increased from 32.0 to 191.8 L. As a result, the elimination t ½ increased from 8.5 h for a child weighing 10 kg to 23.5 h for a child weighing 60 kg [73].
More recently, May et al. [76] used TDM data from three German epilepsy centers to evaluate the influence of age and other factors on serum stiripentol concentrations in 75 patients (age range 0.3–47.5 years), who were mostly children or adolescents (<6 years, 26.7 %; 6–11.9 years, 21.3 %; 12–17.9 years, 20.0 %). The study confirmed that stiripentol shows non-linear pharmacokinetics and that serum stiripentol concentrations increase more than proportionally with increasing dose. Compared with patients older than 12 years, serum stiripentol concentrations were 39.6 % lower in children aged 6–12 years, and 57.5 % lower in children aged less than 6 years. Concomitant treatment with valproic acid did not appear to affect serum stiripentol concentrations. Conversely, serum stiripentol concentrations appeared to be reduced by about 60 % by co-administration of phenobarbital or phenytoin, and to be increased by about 25 % by co-administration of clobazam. The authors concluded that stiripentol is a good candidate for TDM, owing to its variable, age- and dose-dependent pharmacokinetics and its vulnerability to drug interactions.
2.3.8 Topiramate
Topiramate has been commercially available since 1996 and most of the studies describing its pharmacokinetics in children were conducted several years ago and summarized in detail in our previous review [2]. It was generally found that topiramate CL/F is higher in children than in adults. In particular, a study using TDM data reported topiramate CL/F values which were on average 42–66 % higher in children (depending on the absence or presence of enzyme-inducing co-medication) than those found in adults matched for age and co-medication [77]. Within a pediatric population, the highest CL/F values are generally found in younger children [78]. For example, in another study based on TDM data, topiramate CL/F values in children aged less than 8 years co-medicated with enzyme inducers were twofold higher than those found in similarly co-medicated children aged 9–17 years [79]. In the absence of enzyme inducers, the difference between the two groups was 1.5-fold. Overall, existing data confirm that, within any age group, co-medication with enzyme inducers increases topiramate CL/F up to twofold [2]. Because of the compounded influence of age and co-medication, the variability in serum topiramate concentrations within a typical population is prominent. In an early study, average serum topiramate concentration (μg/mL)/dose (mg/kg) ratios ranged from 0.4 in children younger than 11 years receiving enzyme inducers to 1.8 in patients older than 11 years not receiving enzyme inducers [80]. A recent study based on comparison of TDM data confirmed that topiramate CL/F values are higher in children than in adults. Although the influence of age in that study was relatively modest, results may have been confounded by differences in the use of interacting co-medications across age groups [50].
Two other recent studies explored further the pharmacokinetics of topiramate in children by using population pharmacokinetic modeling. On the basis of assessment of a small population of 26 subjects (9 children, 17 adults, age range 8–54 years), Vovk et al. [81] found that weight-normalized topiramate CL/F was approximately 50 % higher in children than in adults, which is in agreement with earlier findings. Using data from 11 double-blind studies, Girgis et al. [82] integrated 4,640 observations from 1,217 patients, including 751 observations from 258 children aged 2–15 years. The final analysis focused on the relationship between trough serum topiramate concentration and dose (mg/kg) in the age group between 2 and 10 years. The model confirmed that topiramate pharmacokinetics are strongly dependent on age, body weight, and concomitant medication, which mostly included enzyme-inducing AEDs. In the overall pediatric population, serum topiramate concentrations at any given dose (mg/kg) were on average twofold higher at age 10 years than at age 2 years, confirming the inverse relationship between CL/F and age. Topiramate CL/F was also twofold higher in patients on adjunctive therapy than in those on monotherapy. Interestingly, the influence of body weight and age on CL/F was more pronounced in the adjunctive therapy group than in the monotherapy group. The same study also investigated the relationship between serum topiramate concentration and antiseizure response, and found that such a relationship did not differ between children and adults.
2.3.9 Other Drugs
A summary of the pharmacokinetics of felbamate, gabapentin, tiagabine, vigabatrin, and zonisamide in children was provided in our earlier review [2], and no significant additional information seems to have become available more recently. On the other hand, there seems to be no data on the pediatric pharmacokinetics of pregabalin and of the more recently developed drugs lacosamide and retigabine.
3 Pharmacokinetics of New-Generation AEDs in the Elderly
3.1 General Considerations
Although there have been relatively few studies on the pharmacokinetics of new AEDs in old age, available evidence indicates that on average the CL/F of most of these drugs is reduced by about 20–40 % in elderly patients compared with non-elderly adults [83, 84]. Depending on the characteristics of the drug, the reduction in CL/F can be ascribed to an age-related decrease in rate of drug metabolism, to a decrease in renal excretion rate, or to both [85]. Whereas for drugs which undergo extensive metabolic elimination there are no reliable means for predicting accurately aging-related CL/F changes in the individual patient, for drugs which are primarily cleared by renal excretion an estimate of individual drug eliminating capacity can be obtained by measuring CLCR.
It should be stressed that elderly patients are not a homogeneous group. Pharmacokinetics in these patients can be influenced not only by anagraphical age, but also by other factors such as frailty, nutritional status, co-morbidities, and interactions with concomitantly administered medications [83, 84]. Measurement of serum drug concentrations may aid in the individualization of dosage in these patients, taking into account that for drugs that are highly bound to plasma proteins total serum concentrations may underestimate the level of unbound, pharmacologically active drug [86].
A summary of the influence of old age on the pharmacokinetics of new-generation AEDs is provided in Table 4. Few of the studies cited in this table were published after 2006. These will be discussed in some detail in the section below.
3.2 Eslicarbazepine Acetate
In a study in healthy volunteers, Almeida et al. [87] compared the single- and multiple-dose pharmacokinetics of eslicarbazepine acetate in 12 subjects aged 65–80 years (mean 69.9 years) and 12 controls aged 18–38 years (mean 29.8 years). All subjects were initially given a single 600 mg oral dose, followed by a multiple-dose phase in which they received 600 mg once daily for 8 days. Eslicarbazepine acetate was not detectable in plasma in either group, and eslicarbazepine accounted for 95–98 % of total drug exposure. (R)-Licarbazepine was a minor metabolite. Plasma eslicarbazepine concentration profiles after single and multiple dosing in older subjects were similar to those found in young subjects, and none of the pharmacokinetic parameters differed significantly between the two groups. Although this study did not identify an effect of aging on the pharmacokinetics of eslicarbazepine acetate, the mean age of the elderly group was just under 70 years and results may not be necessarily extrapolated to older people.
3.3 Felbamate
Felbamate, a drug found to be effective against focal seizures and against drop-attacks associated with the Lennox–Gastaut syndrome, is rarely prescribed today because of high risk of aplastic anemia and liver toxicity associated with its use. Felbamate is completely absorbed from the gastrointestinal tract and is eliminated partly by renal excretion in unchanged form (about 40 % of the dose) and partly by hydroxylation followed by conjugation [7]. The drug shows linear pharmacokinetics and its t ½ is in the order of 14–23 h in patients not taking enzyme inducers, and 10–20 h in patients on enzyme inducers.
White et al. [88] explored the influence of age on felbamate CL/F in 40 chronically treated patients with epilepsy not receiving interacting co-medications. All patients were adults (age 19–68 years) except for a 10-year-old child. Felbamate CL/F was found to be inversely related to age. Compared with patients aged less than 50 years (n = 11), patients aged 50 years or older (n = 29) showed a mean 31 % reduction in felbamate CL/F (19.6 vs 28.3 mL/h/kg), but the degree of interindividual variability was considerable. These findings are consistent with those from an earlier study in healthy volunteers, which reported an approximate 20 % reduction in felbamate CL/F in a group of 24 elderly subjects aged 66–78 years compared with 11 younger adults aged 18–45 years [89].
3.4 Lacosamide
Lacosamide is approved in the EU and the USA for the adjunctive treatment of focal seizures in adults. It shows linear pharmacokinetics, virtually complete oral bioavailability, and elimination partly in unchanged form in urine (about 40 % of the administered dose) and partly by oxidative biotransformation mediated by CYP2C9, CYP2C19, and CYP3A4 [41]. Its pharmacokinetics in old age have not been reported in detail. In a study published in abstract form only, plasma lacosamide concentrations at steady state after normalization for differences in body weight were about 10–35 % higher in 23 subjects aged over 65 years (age range not stated) than in non-elderly adults [90]. The EU Summary of Product Characteristics mentions that in a study in elderly men and women that included four patients older than 75 years, lacosamide AUC values were increased by about 30 and 50 % compared to young men, respectively [90]. After normalization for body weight, however, the magnitude of the differences was less prominent (26 and 23 %, respectively). These older subjects showed only a minor reduction in lacosamide renal CL. According to the same source, the variability in lacosamide exposure was greater in the elderly than in the young [90].
3.5 Lamotrigine
In an early study, lamotrigine pharmacokinetics were compared in 12 young subjects aged 26–38 years and 12 elderly volunteers aged 65–76 years. On average, lamotrigine CL/F was found to be 37 % lower in the older group, which also showed a mean 6.3-h prolongation in lamotrigine t ½ [91]. In a more recent study based on a retrospective assessment of serum lamotrigine levels, Arif et al. [92] found that, within the cohort receiving lamotrigine monotherapy, median lamotrigine CL/F among patients aged 55–92 years (n = 145) was approximately 22 % lower than in younger patients aged 29–36 years (n = 191). A reduction in lamotrigine CL/F in older patients was also observed in the cohorts receiving other AEDs in combination, although the magnitude of age-related differences appeared to be less among patients co-medicated with enzyme inducers and those co-medicated with valproic acid. Older patients in this study were also found to be more prone to develop adverse effects than younger patients, a finding which could not be ascribed solely to differences in serum drug levels because rates of intolerability associated with any given serum lamotrigine concentration were also increased in the older groups. Another study evaluated the population pharmacokinetics of lamotrigine in old age and was based on 875 serum concentrations from 148 mostly male patients (age range 59–92 years) who had participated in a randomized trial [93]. The estimated population mean CL/F for patients using lamotrigine monotherapy in this study was 2.64 L/h, which is comparable to that reported in other population pharmacokinetic studies in adults [54, 94, 95]. Surprisingly, no relationship between CL/F and age was found in this group of 148 patients. Two earlier population pharmacokinetic studies in adults [94, 95] and a recent comparison of TDM-based data [50] also had failed to identify a clear-cut influence of old age on lamotrigine CL/F, but these findings should be interpreted cautiously because only few elderly subjects were assessed in these studies [94, 95].
3.6 Levetiracetam
Early reports indicated that levetiracetam CL/F is reduced by 20–40 % in the elderly [20, 21]. Likewise, the t ½ of levetiracetam has been reported to be longer in the elderly (10–11 h) than in the young (6–8 h) [21]. In a more recent retrospective study based on TDM data, Hirsch et al. [13] compared levetiracetam CL/F values in the youngest (16–31 years; n = 151) and oldest (55–88 years; n = 157) quartiles of 629 adult outpatients. Mean levetiracetam CL/F was 41 % lower in the older cohort than in the young (46.5 vs 78.2 mL/h/kg), and the difference was even greater (59 %, or 33.8 vs 83.3 mL/h/kg) when the comparison was restricted to patients on monotherapy. The decline in levetiracetam CL/F with age occurred in parallel with aging-related decrease in CLCR, in line with earlier studies indicating a clear relationship between levetiracetam CL and renal function [96]. On the basis of these data, the authors suggested that older patients require on average 40–50 % lower doses of levetiracetam to achieve a similar serum concentration as a younger adult. In the same study, co-administration of enzyme-inducing AEDs was associated with higher levetiracetam CL/F, an observation which applied to both age groups. Another study by Johannessen Landmark et al. [50] investigated the influence of age on levetiracetam pharmacokinetics among patients referred to a TDM service, and found that on average levetiracetam CL/F was 40 % lower in elderly subjects compared with non-elderly adults. A progressive reduction in levetiracetam CL/F in old age was also found in a recent prospective study in 272 patients with epilepsy [97]. Compared with patients aged 30–65 years (n = 97), median levetiracetam CL/F values were reduced by 33 % in elderly patients aged 66–80 years (n = 105) and by 52 % in very elderly patients aged 81–96 years (n = 70). Actual CL/F values (median and 25th and 75th percentiles) decreased from 73.8 (56.4–93.0) mL/h/kg in non-elderly subjects to 49.8 (384–696) mL/h/kg in the elderly and 35.4 (27.6–49.2) mL/h/kg in the very elderly subjects. This study also confirmed that, within any age group, levetiracetam CL/F values are higher in patients receiving concomitant enzyme inducers than in those not on enzyme inducers. The authors concluded that, on the basis of their findings, the levetiracetam dose (mg/kg) to achieve any given serum concentration should be reduced by around 30 % in patients over 65 years and by around 50 % in patients over 80 years compared to non-elderly adults.
3.7 Perampanel
There is no detailed published information on the pharmacokinetics of perampanel in old age. According to the EU Summary of Product Characteristics, a population pharmacokinetic analysis of patients with focal epilepsy ranging in age from 12 to 74 years and receiving perampanel dosages up to 12 mg/day in placebo-controlled trials did not identify a significant effect of age on perampanel CL/F. However, the number of aged subjects included in this analysis, and the power of the study to identify an effect of age on perampanel pharmacokinetics, are unknown [67].
3.8 Pregabalin
Pregabalin was initially approved in the EU in 2004 for the adjunctive treatment of focal seizures with and without secondary generalization. Since then, it has been approved in many countries worldwide for the same indication. Subsequent indications approved in the EU and/or other countries include the treatment of central and peripheral neuropathic pain, generalized anxiety disorders, and fibromyalgia in adults. Pregabalin shows linear pharmacokinetics, virtually complete bioavailability, a t ½ of 5–7 h, and elimination in urine in unchanged form [7, 98].
Because pregabalin is cleared primarily by renal excretion in unchanged form, its CL/F would be expected to decline in old age in parallel with the aging-related physiological decrease in renal function. In agreement with this prediction, a study that investigated factors affecting dose-normalized trough serum pregabalin concentrations at steady state in 167 patients aged 17–73 years found that the highest concentrations occurred in older patients [99]. A more recent population pharmacokinetic study assessed the distribution of serum pregabalin concentrations in 195 mostly non-elderly volunteers (including a subgroup with altered renal function), 267 patients with post-herpetic neuralgia (mean age 73 years) and 154 patients with diabetic peripheral neuropathy (mean age 61 years) [100]. The study confirmed that CLCR is the strongest predictor of pregabalin CL/F. For a decrease in CLCR from 60 to 30 mL/min, pregabalin CL/F decreased proportionally by 50 %. A similar study assessed the population pharmacokinetics of pregabalin in a pooled cohort of subjects encompassing an age range from 13 to 100 years, which included healthy volunteers and subjects with renal impairment (n = 123), patients with focal seizures (n = 626), and patients with chronic pain (n = 974) [101]. The findings confirmed the dependency of pregabalin pharmacokinetics on CLCR, and no specific age-dependency of pregabalin CL/F could be identified. It was concluded that changes in pregabalin CL/F can be explained by changes in renal function, and no additional adjustments for age are necessary.
3.9 Retigabine (Ezogabine)
Retigabine, a drug recently approved in the EU and the USA for the adjunctive treatment of focal seizures in adults, is considered to exert its antiseizure effects by enhancing neuronal M-type potassium currents. Retigabine has linear pharmacokinetics, incomplete oral bioavailability probably related to first-pass metabolism, and a t ½ of 6–10 h [41]. It is cleared party by urinary excretion in unchanged form (20–30 % of the administered dose) and partly by conversion to various metabolites, including glucuronide conjugates and a weakly active N-acetyl derivative [41].
Hermann et al. [102] compared the pharmacokinetics of retigabine in 24 healthy young subjects (age range 18–40 years) and 24 elderly subjects aged 66–82 years. There were 12 men and 12 women in each age group, thereby allowing an assessment of potential gender-related influences on pharmacokinetics. After a single oral dose (1,200 mg), peak plasma retigabine concentrations were similar in the two age groups. Compared with young subjects, however, elderly subjects showed a slower elimination of the drug as reflected by 30 % lower CL/F, 42 % higher AUC, and a 30 % longer t ½. Exposure to the N-acetyl metabolite was also moderately increased in the elderly group. Although there were no sex-related differences in weight-normalized CL/F values between men and women in either age group, mean plasma retigabine concentrations at time of peak were on average about 55 % higher in young women than in young men, and twice as high in elderly women than in elderly men.
3.10 Rufinamide
A study reported in summarized form did not identify differences in rufinamide pharmacokinetics between eight elderly subjects (age 66–77 years) and eight young adults (age 18–40 years) evaluated after a single 400 mg oral dose [69].
3.11 Other AEDs
Early findings on the pharmacokinetics of gabapentin [103, 104], oxcarbazepine [105, 106], tiagabine [107], topiramate [108], vigabatrin [109], and zonisamide [110, 111] in old age were summarized in our previous review [2], and no significant additional information appears to have accrued in recent years.
4 Conclusions
Studies conducted in the last 6 years provided important information on age-related changes in the pharmacokinetics of several new AEDs, particularly those introduced most recently. In general, findings from these studies are consistent with the notion that drug CL is often reduced in the neonate, particularly for agents which are eliminated by renal excretion and by glucuronide conjugation. Conversely, older infants and children usually eliminate drugs at a faster rate compared with adults, and therefore require larger doses (when expressed as mg/kg) to achieve any given serum concentration. At the other extreme of age, in the elderly, drug CL is generally lower compared with younger adults as a result of less efficient drug-metabolizing activity, decreased renal function, or both. For drugs which are cleared primarily in unchanged form by the kidney, pharmacokinetic changes in old age are usually proportional to the decline in CLCR.
For all drugs investigated, pharmacokinetic variability at any given age is considerable, under the influence of variables such as genetic factors, co-morbid conditions, and interactions with concomitantly given medications. Both in pediatric age and in the elderly, monitoring serum drug concentrations can assist physicians in controlling for pharmacokinetic variability, and may facilitate individualization of dosing. However, because differences in age and other factors may also affect the relationship between serum drug concentration and pharmacological effects [7, 112], careful monitoring of clinical response remains the mainstay in the optimization of AED therapy.
References
Neligan A, Hauser WA, Sander JW. The epidemiology of the epilepsies. Handb Clin Neurol. 2012;107:113–33.
Perucca E. Clinical pharmacokinetics of new-generation antiepileptic drugs at the extremes of age. Clin Pharmacokinet. 2006;45(4):351–63.
Stewart CF, Hampton EM. Effect of maturation on drug disposition in pediatric patients. Clin Pharm. 1987;6(7):548–64.
Morselli PL, Franco Morselli R, Bossi L. Clinical pharmacokinetics in newborns and infants—age-related differences and therapeutic implications. Clin Pharmacokinet. 1980;5(6):485–527.
Kearns GL, Abdel-Rahman SM, Alander SW, et al. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349(12):1157–67.
Perucca E. Drug metabolism in pregnancy, infancy and childhood. Pharmacol Ther. 1987;34(1):129–43.
Patsalos PN, Berry DJ, Bourgeois BF, et al. Antiepileptic drugs—best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring. ILAE Commission on Therapeutic Strategies. Epilepsia. 2008;49(7):1239–76.
Chen H, Yang K, Choi S, et al. Up-regulation of UDP-glucuronosyltransferase (UGT) 1A4 by 17beta-estradiol: a potential mechanism of increased lamotrigine elimination in pregnancy. Drug Metab Dispos. 2009;37(9):1841–7.
Ohman I, Vitols S, Tomson T. Lamotrigine in pregnancy: pharmacokinetics during delivery, in the neonate, and during lactation. Epilepsia. 2000;41(6):709–13.
Mikati MA, Fayad M, Koleilat M, et al. Efficacy, tolerability, and kinetics of lamotrigine in infants. J Pediatr. 2002;141(1):31–5.
Fotopoulou C, Kretz R, Bauer S, et al. Prospectively assessed changes in lamotrigine-concentration in women with epilepsy during pregnancy, lactation and the neonatal period. Epilepsy Res. 2009;85(1):60–4.
Newport DJ, Pennell PB, Calamaras MR, et al. Lamotrigine in breast milk and nursing infants: determination of exposure. Pediatrics. 2008;122(1):e223–31.
Hirsch LJ, Arif H, Buchsbaum R, et al. Effect of age and comedication on levetiracetam pharmacokinetics and tolerability. Epilepsia. 2007;48(7):1351–9.
Freitas-Lima P, Alexandre V Jr, Pereira LR, et al. Influence of enzyme inducing antiepileptic drugs on the pharmacokinetics of levetiracetam in patients with epilepsy. Epilepsy Res. 2011;94(1–2):117–20.
Johannessen SI, Helde G, Brodtkorb E. Levetiracetam concentrations in serum and in breast milk at birth and during lactation. Epilepsia. 2005;46(5):775–7.
Tomson T, Palm R, Kallen K, et al. Pharmacokinetics of levetiracetam during pregnancy, delivery, in the neonatal period, and lactation. Epilepsia. 2007;48(6):1111–6.
Allegaert K, Lewi L, Naulaers G, et al. Levetiracetam pharmacokinetics in neonates at birth. Epilepsia. 2006;47(6):1068–9.
Glauser TA, Mitchell WG, Weinstock A, et al. Pharmacokinetics of levetiracetam in infants and young children with epilepsy. Epilepsia. 2007;48(6):1117–22.
Sharpe CM, Capparelli EV, Mower A, et al. A seven-day study of the pharmacokinetics of intravenous levetiracetam in neonates: marked changes in pharmacokinetics occur during the first week of life. Pediatr Res. 2012;72(1):43–9.
Pellock JM, Glauser TA, Bebin EM, et al. Pharmacokinetic study of levetiracetam in children. Epilepsia. 2001;42(12):1574–9.
Patsalos PN. Clinical pharmacokinetics of levetiracetam. Clin Pharmacokinet. 2004;43(11):707–24.
Merhar SL, Schibler KR, Sherwin CM, et al. Pharmacokinetics of levetiracetam in neonates with seizures. J Pediatr. 2011;159(1):152–4 e3.
Northam RS, Hernandez AW, Litzinger MJ, et al. Oxcarbazepine in infants and young children with partial seizures. Pediatr Neurol. 2005;33(5):337–44.
Pina-Garza JE, Espinoza R, Nordli D, et al. Oxcarbazepine adjunctive therapy in infants and young children with partial seizures. Neurology. 2005;65(9):1370–5.
Ohman I, Vitols S, Luef G, et al. Topiramate kinetics during delivery, lactation, and in the neonate: preliminary observations. Epilepsia. 2002;43(10):1157–60.
Filippi L, la Marca G, Fiorini P, et al. Topiramate concentrations in neonates treated with prolonged whole body hypothermia for hypoxic ischemic encephalopathy. Epilepsia. 2009;50(11):2355–61.
Johannessen SI, Tomson T. Pharmacokinetic variability of newer antiepileptic drugs: when is monitoring needed? Clin Pharmacokinet. 2006;45(11):1061–75.
Rosenfeld WE, Doose DR, Walker SA, et al. A study of topiramate pharmacokinetics and tolerability in children with epilepsy. Pediatr Neurol. 1999;20(5):339–44.
Manitpisitkul P, Shalayda K, Todd M, et al. Pharmacokinetics and safety of adjunctive topiramate in infants (1–24 months) with refractory partial-onset seizures: a randomized, multicenter, open-label phase 1 study. Epilepsia. 2013;54(1):156–64. doi:10.1111/epi.12019.
Mikaeloff Y, Rey E, Soufflet C, et al. Topiramate pharmacokinetics in children with epilepsy aged from 6 months to 4 years. Epilepsia. 2004;45(11):1448–52.
Bouillon-Pichault M, Nabbout R, Chhun S, et al. Topiramate pharmacokinetics in infants and young children: contribution of population analysis. Epilepsy Res. 2011;93(2–3):208–11.
Rey E, Pons G, Olive G. Vigabatrin. Clinical pharmacokinetics. Clin Pharmacokinet. 1992;23:267–78.
Vauzelle-Kervroëdan F, Rey E, Pons G, et al. Pharmacokinetics of the individual enantiomers of vigabatrin in neonates with uncontrolled seizures. Br J Clin Pharmacol. 1996;42(6):779–81.
Rey E, Pons G, Richard MO, et al. Pharmacokinetics of the individual enantiomers of vigabatrin (gamma-vinyl GABA) in epileptic children. Br J Clin Pharmacol. 1990;30(2):253–7.
Ohman I, Vitols S, Tomson T. Pharmacokinetics of gabapentin during delivery, in the neonatal period, and lactation: Does a fetal accumulation occur during pregnancy? Epilepsia. 2005;46(10):1621–4.
Haig GM, Bockbrader HN, Wesche DL, et al. Single-dose gabapentin pharmacokinetics and safety in healthy infants and children. J Clin Pharmacol. 2001;41(5):507–14.
Kawada K, Itoh S, Kusaka T, et al. Pharmacokinetics of zonisamide in perinatal period. Brain Dev. 2002;24(2):95–7.
Kimura S. Placental transfer, neonatal pharmacokinetics (elimination), transfer via mother milk of zonisamide. Case report of a neonate of mother treated with zonisamide. No To Hattatsu. 1998;30(4):350–1.
Miura H. Developmental and therapeutic pharmacology of antiepileptic drugs. Epilepsia. 2000;41(Suppl 9):2–6.
Miura H. Zonisamide monotherapy with once-daily dosing in children with cryptogenic localization-related epilepsies: clinical effects and pharmacokinetic studies. Seizure. 2004;13(Suppl 1):S17–23.
Fattore C, Perucca E. Novel medications for epilepsy. Drugs. 2011;71(16):2151–78.
Almeida L, Minciu I, Nunes T, et al. Pharmacokinetics, efficacy, and tolerability of eslicarbazepine acetate in children and adolescents with epilepsy. J Clin Pharmacol. 2008;48(8):966–77.
Chen C, Casale EJ, Duncan B, et al. Pharmacokinetics of lamotrigine in children in the absence of other antiepileptic drugs. Pharmacotherapy. 1999;19:437–41.
Eriksson AS, Hoppu K, Nergardh A, et al. Pharmacokinetic interactions between lamotrigine and other antiepileptic drugs in children with intractable epilepsy. Epilepsia. 1996;37:769–73.
Battino D, Croci D, Granata T, et al. Single-dose pharmacokinetics of lamotrigine in children: influence of age and antiepileptic comedication. Ther Drug Monit. 2001;23:217–22.
Chen C. Validation of a population pharmacokinetic model for adjunctive lamotrigine therapy in children. Brit J Clin Pharmacol. 2000;50:135–45.
Bartoli A, Guerrini R, Belmonte A, et al. The influence of dosage, age and comedication on steady-state plasma lamotrigine concentrations in epileptic children: a prospective study with preliminary assessment of correlations with clinical response. Ther Drug Monit. 1997;19:252–60.
Armijo JA, Bravo J, Cuadrado A, et al. Lamotrigine serum concentration-to-dose ratio: influence of age and concomitant antiepileptic drugs and dosage implications. Ther Drug Monit. 1999;21:182–90.
Vauzelle-Kervroedan F, Rey E, et al. Influence of concurrent antiepileptic medication on the pharmacokinetics of lamotrigine as add-on therapy in epileptic children. Br J Clin Pharmacol. 1996;4:325–30.
Johannessen Landmark C, Baftiu A, et al. Pharmacokinetic variability of four newer antiepileptic drugs, lamotrigine, levetiracetam, oxcarbazepine, and topiramate: a comparison of the impact of age and comedication. Ther Drug Monit. 2012;34(4):440–5.
He DK, Wang L, Qin J, et al. Population pharmacokinetics of lamotrigine in Chinese children with epilepsy. Acta Pharmacol Sin. 2012;33(11):1417–23.
Zhang S, Wang L, Lu W. Population pharmacokinetics of lamotrigine in Chinese children with epilepsy. Zhongguo Dang Dai Er Ke Za Zhi. 2008;10(2):105–9.
Reimers A, Skogvoll E, Sund JK, et al. Lamotrigine in children and adolescents: the impact of age on its serum concentrations and on the extent of drug interactions. Eur J Clin Pharmacol. 2007;63(7):687–92.
Milovanovic JR, Jankovic SM. Population pharmacokinetics of lamotrigine in patients with epilepsy. Int J Clin Pharmacol Ther. 2009;47(12):752–60.
Fountain NB, Conry JA, Rodríguez-Leyva I, et al. Prospective assessment of levetiracetam pharmacokinetics during dose escalation in 4- to 12-year-old children with partial-onset seizures on concomitant carbamazepine or valproate. Epilepsy Res. 2007;74(1):60–9.
Dahlin MG, Wide K, Ohman I. Age and comedications influence levetiracetam pharmacokinetics in children. Pediatr Neurol. 2010;43(4):231–5.
Toublanc N, Sargentini-Maier ML, Lacroix B, et al. Retrospective population pharmacokinetic analysis of levetiracetam in children and adolescents with epilepsy: dosing recommendations. Clin Pharmacokinet. 2008;47(5):333–41.
Chhun S, Jullien V, Rey E, et al. Population pharmacokinetics of levetiracetam and dosing recommendation in children with epilepsy. Epilepsia. 2009;50(5):1150–7.
Snoeck E, Jacqmin P, Sargentini-Maier ML, et al. Modeling and simulation of intravenous levetiracetam pharmacokinetic profiles in children to evaluate dose adaptation rules. Epilepsy Res. 2007;76(2–3):140–7.
Otoul C, De Smedt H, Stockis A. Lack of pharmacokinetic interaction of levetiracetam on carbamazepine, valproic acid, topiramate, and lamotrigine in children with epilepsy. Epilepsia. 2007;48(11):2111–5.
Perucca E. Is there a role for therapeutic drug monitoring of new anticonvulsants? Clin Pharmacokinet. 2000;38:191–204.
Gidal BE, Baltès E, Otoul C, et al. Effect of levetiracetam on the pharmacokinetics of adjunctive antiepileptic drugs: a pooled analysis of data from randomized clinical trials. Epilepsy Res. 2005;64(1–2):1–11.
Sallas WM, Milosavljev S, D’souza J, et al. Pharmacokinetic drug interactions in children taking oxcarbazepine. Clin Pharmacol Ther. 2003;74:138–49.
Pariente-Khayat A, Fran A, Vauzelle-Kervroedan F, et al. Pharmacokinetics of oxcarbazepine as add-on therapy in children. Epilepsia. 1994;35(Suppl. 8):119.
Rey E, Bulteau C, Motte J, et al. Oxcarbazepine pharmacokinetics and tolerability in children with inadequately controlled epilepsy. J Clin Pharmacol. 2004;44:1290–300.
Franco V, Crema F, Iudice A, et al. Novel treatment options for epilepsy: focus on perampanel. Pharmacol Res. 2013;70(1):35–40.
Fycompa (Perampanel). Summary of Product Characteristics. European Medicines Agency. http://www.medicines.org.uk/emc/medicine/26951/SPC#PHARMACOKINETIC_PROPS. Accessed 6 Feb 2013.
Ferrie CD. Rufinamide: a new antiepileptic drug treatment for Lennox–Gastaut syndrome. Expert Rev Neurother. 2010;10(6):851–60.
Perucca E, Cloyd J, Critchley D, et al. Rufinamide: clinical pharmacokinetics and concentration-response relationships in patients with epilepsy. Epilepsia. 2008;49(7):1123–41.
May TW, Boor R, Rambeck B, et al. Serum concentrations of rufinamide in children and adults with epilepsy: the influence of dose, age, and comedication. Ther Drug Monit. 2011;33(2):214–21.
Dahlin MG, Ohman I. Rufinamide in children with refractory epilepsy: pharmacokinetics, efficacy, and safety. Neuropediatrics. 2012;43(5):264–70.
Biton V, Krauss G, Vasquez-Santana B, et al. A randomized, double-blind, placebo-controlled, parallel-group study of rufinamide as adjunctive therapy for refractory partial-onset seizures. Epilepsia. 2011;52(2):234–42.
Diacomit (Stiripentol). Summary of Product Characteristics. European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000664/WC500036518.pdf. Accessed 2 Feb 2013.
Bebin M, Bleck TP. New anticonvulsant drugs. Focus on flunarizine, fosphenytoin, midazolam and stiripentol. Drugs. 1994;48(2):153–71.
Luszczki JJ. Third-generation antiepileptic drugs: mechanisms of action, pharmacokinetics and interactions. Pharmacol Rep. 2009;61(2):197–216.
May TW, Boor R, Mayer T, et al. Concentrations of stiripentol in children and adults with epilepsy: the influence of dose, age, and comedication. Ther Drug Monit. 2012;34(4):390–7.
Battino D, Croci D, Rossini A, et al. Topiramate pharmacokinetics in children and adults with epilepsy: a case-matched comparison based on therapeutic drug monitoring data. Clin Pharmacokinet. 2005;44:407–16.
Dahlin MG, Ohman IK. Age and antiepileptic drugs influence topiramate plasma levels in children. Pediatr Neurol. 2004;31:248–53.
May TW, Rambeck B, Jürgens U. Serum concentrations of topiramate in patients with epilepsy: influence of dose, age, and comedication. Ther Drug Monit. 2002;24(3):366–74.
Adín J, Gómez MC, Blanco Y, et al. Topiramate serum concentration-to-dose ratio: influence of age and concomitant antiepileptic drugs and monitoring implications. Ther Drug Monit. 2004;26(3):251–7.
Vovk T, Jakovljević MB, Kos MK, et al. A nonlinear mixed effects modelling analysis of topiramate pharmacokinetics in patients with epilepsy. Biol Pharm Bull. 2010;33(7):1176–82.
Girgis IG, Nandy P, Nye JS, et al. Pharmacokinetic-pharmacodynamic assessment of topiramate dosing regimens for children with epilepsy 2 to <10 years of age. Epilepsia. 2010;51(10):1954–62.
Perucca E, Birnbaum A, Cloyd JC, et al. Pharmacological and clinical aspects of antiepileptic drug use in the elderly. Epilepsy Res. 2006;68(Suppl 1):849–63.
Turnheim K. When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol. 2003;38:843–53.
Gidal BE. Antiepileptic drug formulation and treatment in the elderly: biopharmaceutical considerations. Int Rev Neurobiol. 2007;81:299–311.
Perucca E. Age-related changes in pharmacokinetics: predictability and assessment methods. Int Rev Neurobiol. 2007;81:183–99.
Almeida L, Potgieter JH, Maia J, et al. Pharmacokinetics of eslicarbazepine acetate in patients with moderate hepatic impairment. Eur J Clin Pharmacol. 2008;64(3):267–73.
White JR, Leppik IE, Beattie JL, et al. Long-term use of felbamate: clinical outcomes and effect of age and concomitant antiepileptic drug use on its clearance. Epilepsia. 2009;50(11):2390–6.
Richens A, Banfield CR, Salfi M, et al. Single and multiple dose pharmacokinetics of felbamate in the elderly. Br J Clin Pharmacol. 1997;44:129–34.
Schiltmeyer B, Cawello W, Kropeit D, et al. Pharmacokinetics of the new antiepileptic drug SPM 927 in human subjects with different age and gender [abstract]. Epilepsia. 2004;45(Suppl. 7):313.
Posner J, Holdich T, Crome P. Comparison of lamotrigine pharmacokinetics in young and elderly healthy volunteers. J Pharm Med. 1991;1:121–8.
Arif H, Svoronos A, Resor SR, et al. The effect of age and comedication on lamotrigine clearance, tolerability, and efficacy. Epilepsia. 2011;52(10):1905–13.
Punyawudho B, Ramsay RE, Macias FM, et al. Population pharmacokinetics of lamotrigine in elderly patients. J Clin Pharmacol. 2008;48(4):455–63.
Hussein Z, Posner J. Population pharmacokinetics of lamotrigine monotherapy in patients with epilepsy: retrospective analysis of routine monitoring data. Br J Clin Pharmacol. 1997;43:457–65.
Chan V, Morris RG, Ilett KF, et al. Population pharmacokinetics of lamotrigine. Ther Drug Monit. 2001;23:630–5.
French J. Use of levetiracetam in special populations. Epilepsia. 2001;42(suppl 4):40–3.
Contin M, Mohamed S, Albani F, et al. Levetiracetam clinical pharmacokinetics in elderly and very elderly patients with epilepsy. Epilepsy Res. 2012;98(2–3):130–4.
Bockbrader HN, Wesche D, Miller R, et al. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49(10):661–9.
May TW, Rambeck B, Neb R, et al. Serum concentrations of pregabalin in patients with epilepsy: the influence of dose, age, and comedication. Ther Drug Monit. 2007;29:789–94.
Shoji S, Suzuki M, Tomono Y, et al. Population pharmacokinetics of pregabalin in healthy subjects and patients with post-herpetic neuralgia or diabetic peripheral neuropathy. Br J Clin Pharmacol. 2011;72(1):63–76.
Bockbrader HN, Burger P, Knapp L, et al. Population pharmacokinetics of pregabalin in healthy subjects and patients with chronic pain or partial seizures. Epilepsia. 2011;52(2):248–57.
Hermann R, Ferron GM, Erb K, et al. Effects of age and sex on the disposition of retigabine. Clin Pharmacol Ther. 2003;73(1):61–70.
Armijo JA, Pena MA, Adín J, et al. Association between patient age and gabapentin serum concentration-to-dose ratio: a preliminary multivariate analysis. Ther Drug Monit. 2004;26(6):633–7.
Boyd RA, Türck D, Abel RB, et al. Effects of age and gender on single-dose pharmacokinetics of gabapentin. Epilepsia. 1999;40(4):474–9.
Arnoldussen W, Hulsman J, Rentmeester T. Oxcarbazepine (OXBZ) twice daily as effective as OXBZ three times daily: a clinical and pharmacokinetic study in 24 volunteers and 6 patients. Epilepsia. 1992;32(suppl 1):69.
van Heiningen PN, Eve MD, Oosterhuis B, et al. The influence of age on the pharmacokinetics of the antiepileptic agent oxcarbazepine. Clin Pharmacol Ther. 1991;50(4):410–9.
Snel S, Jansen JA, Mengel HB, et al. The pharmacokinetics of tiagabine in healthy elderly volunteers and elderly patients with epilepsy. J Clin Pharmacol. 1997;37(11):1015–20.
Doose DR, Larsson KL, Natarajan J, et al. Comparative single-dose pharmacokinetics of topiramate in elderly versus young men and women. Epilepsia. 1998;39(Suppl 6):56.
Haegele KD, Huebert ND, Ebel M, et al. Pharmacokinetics of vigabatrin: implications of creatinine clearance. Clin Pharmacol Ther. 1988;44(5):558–65.
Shah J, Shellenberger K, Canafax D. Zonisamide: biotransformation and pharmacokinetics. In: Levy RH, Mattson RH, Meldrum BS, et al, editors. Antiepileptic drugs. 5th ed. Philadelphia (PA): Lippincott Williams and Wilkins, 2002: p. 872–84.
Wallace J, Shellenberger K, Groves L. Pharmacokinetics of zonisamide in young and elderly subjects. Epilepsia. 1998;39(Suppl 6):190–1.
Perucca E. The pharmacology of new antiepileptic drugs: does a novel mechanism of action really matter? CNS Drugs. 2011;25(11):907–12.
Gustavson LE, Boellner SW, Granneman GR, et al. A single-dose study to define tiagabine pharmacokinetics in pediatric patients with complex partial seizures. Neurology. 1997;48(4):1032–7.
Acknowledgments
Domenico Italiano has no conflicts of interest to report. Emilio Perucca received research grants from the European Union, the Italian Medicines Agency, the Italian Ministry of Health, and the Italian Ministry for Education, University and Research. He also received speaker’s or consultancy fees and/or research grants from Bial, Eisai, GSK, Lundbeck, Medichem, Pfizer, Sun Pharma, Supernus, UCB Pharma, Upsher-Smith, and Vertex. No funding has been received by the authors for this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Italiano, D., Perucca, E. Clinical Pharmacokinetics of New-Generation Antiepileptic Drugs at the Extremes of Age: An Update. Clin Pharmacokinet 52, 627–645 (2013). https://doi.org/10.1007/s40262-013-0067-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-013-0067-4