Abstract
Asthma is increasingly recognised as a heterogeneous group of diseases with similar clinical presentations rather than a singular disease entity. Asthma was historically categorised by clinical symptoms; however, newer methods of subgrouping, describing and categorising the disease have sub-defined asthma. These sub-definitions are intermittently called phenotypes or endotypes, but the real meanings of these words are poorly understood. Novel treatments are currently and increasingly available, partly in the monoclonal antibody environment, and also some physical therapies (bronchial thermoplasty), but additionally small molecules are not far away from clinical practice. Understanding the disease pathogenesis and the mechanism of action more completely may enable identification of treatable traits, biomarkers, mediators and modifiable therapeutic targets. However, there remains a danger that clinicians become preoccupied with the concept of endotypes and biomarkers, ignoring therapies that are hugely effective but have no companion biomarker. This review discusses our understanding of the concept of phenotypes and endotypes in appreciating and managing the heterogeneous condition that is asthma. We consider the role of functional imaging, physiology, blood-, sputum- and breath-based biomarkers and clinical manifestations that could be used to produce a personalised asthma profile, with implications on prognosis, pathophysiology and most importantly specific therapeutic responses. With the advent of increasing numbers of biological therapies and other interventional options such as bronchial thermoplasty, the importance of targeting expensive therapies to patients with the best chance of clinical response has huge health economic importance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Asthma encompasses a heterogeneous group of conditions, rather than being a single disease entity |
Asthma can be subdivided into clinically similar groups called phenotypes or pathogenically comparable groups called endotypes |
Understanding the disease pathogenesis may enable identification of biomarkers that could predict treatment response |
The future of asthma management may lie in the targeted use of novel localised treatments and directed immunotherapy |
1 Introduction
Asthma is typically characterised by varying degrees of bronchial hyper-responsiveness, reversible airway obstruction, airway inflammation and associated respiratory symptoms. However, it is now widely appreciated that asthma is not a single disease and may instead encompass a wide range of heterogeneous conditions.
Most asthmatics are managed in primary care settings using a standardised treatment pathway [1]. But with a diverse spectrum of disorders being grouped under the asthma umbrella, increasing numbers of patients will be subject to inappropriate treatment, with associated delays, expense, morbidity and mortality. By understanding the pathophysiological, genetic and basic molecular mechanisms and developing methods for individual profiling, it may be possible to tailor personalised therapy and more effectively manage asthma.
This article aims to review the current concepts of phenotypes, endotypes and sub-classifications in asthma, and the implications this will have on personalising asthma management.
2 Classifying Asthma
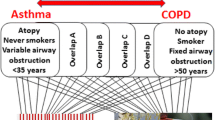
Traditionally asthma has been subgrouped on the basis of observable characteristics or identifiable patterns, such as intrinsic or extrinsic, or atopic or non-atopic asthma.
Clinical subtypes may focus around triggers (exercise-induced, occupational or atopic), symptoms (shortness of breath, wheeze, cough), response to treatment (steroid responsive/unresponsive) or grouped by severity (mild, severe, life-threatening) [2,3,4]. Clinical classifications can be achieved with relative ease (using questionnaires, examination and spirometry); however, they cannot predict treatment responses accurately and therefore may be relatively redundant in terms of therapy decision making.
The asthma severity model was the foundation for the stepwise approach to asthma management, where with increasing symptoms or inadequate response to initial measures [typically short-acting beta-agonists (SABA)], increasing doses of inhaled corticosteroids (ICS), long-acting beta-agonists (LABA), other bronchodilators and oral corticosteroids (OCS) are added in a step-wise fashion [1]. This approach led to the basic, but perhaps over-simplified concept that severity progressed in a linear fashion, with severe asthma requiring greater complexity or scope of the treatment algorithm. Such concepts potentially exacerbate the use of polypharmacy, much of which could at least in theory be ineffective.
Problematically, classical clinical observation of disease severity and treatment response do not always correlate [5]. This discrepancy can lead to a great burden from medication side effects, with little therapeutic benefit, compounded by uncontrolled disease. In severe asthma, there became a need to more fully understand the disease pathogenesis and molecular/genetic mechanisms in order to effectively target and manage asthma with more precision.
3 Clinical Mechanism Led Classification: Asthma Phenotypes and Endotypes
There has been an increasing drive to sub-define asthma using clinical, pathophysiology and cytokine/biomarker profiling. Common methods of sub-classification focus on dividing by phenotypes or endotypes; however, the nomenclature is often poorly defined, adding to potential confusion. Traditionally, phenotypic classification grouped subtypes on the basis of observable or measurable characteristics, whereas endotypic classification aims to separate by pathophysiological mechanism.
In 2011, Lötvall et al. [6] specified several pathophysiologically distinct (but not all-inclusive) endotypes of asthma. This method of subgrouping gave the potential to provide some clinical separation that may lead to targeted treatment algorithms. Whilst other endotypic classifications have been subsequently hypothesised by various other sources [7,8,9] and may arguably show superiority, for the purpose of this review, we will focus on and discuss the original specified endotypes as described by Lötvall et al. [6]:
-
Aspirin-associated respiratory disease (AARD): The AARD endotype characteristically has adult onset, severe/frequent exacerbations, associated nasal polyps/chronic rhinitis and exacerbations triggered by non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, and is usually associated with an eosinophilic inflammatory process [10]. Aspirin desensitisation and anti-eosinophilic monoclonal antibodies may in theory be specifically effective and preferable for this endotype.
-
Allergic bronchopulmonary mycosis (ABPM)/severe asthma with fungal sensitisation (SAFS)/fungal allergic asthma (FAA): It is also recognised that a subtype of asthma is associated with fungal allergy, severe symptoms and notably fungal airway colonisation [measured by either extended fungal culture or using polymerase chain reaction (PCR) analysis of sputum or bronchoalveolar lavage samples] [11, 12]. The group potentially portrays a spectrum of allergic asthma with a recognised progressive pattern and higher risk of life-threatening or fatal outcomes triggered by an allergic response to filamentous fungal antigens (commonly Aspergillus) [13]. ABPM may lead to or be associated with pre-existing central bronchiectasis and a more progressive disease course. Antifungal therapies in conjunction with or replacing OCS may be effective in this disease subgroup [14].
-
Allergic asthma: This subtype often commences in childhood, commonly in those with a history of other atopic conditions. There clearly are a wide range of potential sub-classifications based on the nature of the allergen and exposure patterns, which may or may not lead to differences in outcomes/prognosis. A further potential subgroup of allergic asthma is asthma-predictive indices (API)-positive preschool wheezers (more than three wheezing episodes occuring in the first three years of life and API-criteria positive) [6]. API criteria requires the infant has either one major factor (sensitivity to aeroallergen, known atopic dermatitis or parental asthma) or two minor criteria (peripheral eosinophilia >4%, food allergen sensitivity or non-viral-induced wheezing). Nearly two-thirds of these children will display asthmatic symptoms by the age of 6 [15].
-
Severe late-onset (hyper-eosinophilic) asthma (SLOHA): The SLOHA subgroup is characterised as severe non-atopic asthma manifesting in adulthood [16], which may be most amenable to treatment with novel anti-eosinophilic monoclonal antibodies or even ultimately small molecules [17,18,19,20,21,22].
-
Asthma of cross-country skiers (ACCS): ACCS typically presents as asthmatic symptoms triggered by strenuous exercise especially in combination with cold, dry air. Focussing specifically on cross-country skiers may just be targeting one end of the spectrum of other forms of predominant exercise-induced asthma or even of normal physiological process under extreme conditions. The impact of high air flow, especially with cold, dry air, is a trigger factor [6]. No pattern-specific therapy has yet been postulated, as unlike exercise-induced asthma, it is not typically responsive to ICS [23]. This pattern of asthma also needs careful separation from inducible laryngeal obstruction, which can often be induced by cold air challenge, especially in conjunction with exercise and high inspiratory flow. Failure to separate these patterns will delay understanding of correct therapeutic approaches in this group of athletes.
In each individual, a mixture or change over time of pathophysiological processes may occur during the disease course, highlighting the importance of an individualised approach to therapy.
3.1 Aspirin-Associated Respiratory Disease (AARD)
3.1.1 Pathophysiology
AARD is triggered by cyclooxygenase-1 (COX-1) inhibition by non-selective NSAIDs/aspirin. COX-1 and COX-2 manufacture prostaglandin H2 from arachidonic acid, which in turn promotes synthesis of prostaglandins, thromboxanes and prostacyclins. Many of these downstream mediators exhibit anti-inflammatory effects such as prostaglandin E2, which via receptor subtype 2 dampens eosinophil responses and inhibits mast cell degranulation [24]. COX-2 levels appear reduced in AARD [25], suggesting COX-1-dependant homeostatic cascade. When COX-1 is inhibited by NSAIDs/aspirin, prostaglandin E2 receptor-2 actions are blocked, disinhibiting the eosinophilic/mast cell inflammatory response. Concordantly, inhaled prostaglandin E2 can negate aspirin-induced bronchoconstriction [24, 26]. In AARD pro-inflammatory cysteinyl leukotrienes (CysLTs) are upregulated at baseline and dramatically increase following aspirin challenge compared to non-AARD asthmatic controls [27, 28]. AARD bronchial tissues, nasal polyps and sinus tissues demonstrate overexpression of CysLT-producing enzymes (such as leukotriene C4 synthase) by local mast cells and eosinophil recruitment [29, 30]. Pro-inflammatory CysLTs and reduced anti-inflammatory prostaglandin E2 drive the exaggerated eosinophilic and mast cell-mediated inflammation in response to aspirin/NSAIDs. Figure 1 demonstrates the pathophysiological mechanisms involved in the different asthma endotypes. Figure 1a concerns AARD.
Pathophysiology of asthma endotypes. a Arachidonic acid is converted into numerous inflammatory mediators including downstream prostaglandin-E2 (PGE2). PGE2-receptor-2 dampens eosinophil activation and impairs mast cell degranulation. In aspirin-associated respiratory disease (AARD) this anti-inflammatory pathway is dependent upon cyclooxygenase (COX)-1, which is blocked by aspirin/non-steroidal anti-inflammatory drugs. In AARD, production of cysteinyl leukotrienes is enhanced, leading to bronchoconstriction. b In allergic bronchopulmonary mycosis, fungal proteases cause epithelial damage. Antigen-presenting cells (APCs) recognise and process antigens, and via mediators stimulate T helper cell type 2 (Th2) phenotype. Th2 cytokines stimulate eosinophil activation and immunoglobulin E production from plasmacytes, sensitising mast cells to fungal antigens and triggering bronchoconstriction upon re-exposure. c In one allergic asthma theory, exposure to low-dose endotoxin via APC may potentiate a Th2 type inflammatory response. High-dose endotoxin exposure may trigger a neutrophilic Th17 type response. d In asthma of cross-country skiers, exercise associated with cold, dry conditions leads to excessive airway drying, cellular water loss and subsequent increase in intracellular ionic concentration. Such epithelial stress stimulates an inflammatory cascade associated with neutrophilia and bronchoconstriction [6, 24,25,26,27,28,29,30,31, 38, 39, 50,51,52,53, 75,76,77]. IL interleukin, TNF tumour necrosis factor, TGF transforming growth factor, TSLP thymic stromal lymphopoietin
3.1.2 Genetics
In AARD, prostaglandin E2 receptor-2 gene polymorphism (reducing anti-inflammatory capabilities) is implicated in susceptibility [31]. Furthermore, microsomal prostaglandin E2 synthase-1 deficient mice also develop an AARD-like syndrome [32]. Polymorphisms at pro-inflammatory CysLT receptor-1 promoter and CysLT receptor-2 have shown concordance with AARD and correlation with the degree of aspirin sensitivity [33, 34].
3.1.3 Biomarkers
AARD is associated with raised urinary CysLTs and increased periostin levels; however, due to significant overlap with other endotypes, biomarkers alone cannot specifically differentiate AARD [9, 35].
3.1.4 Management
In AARD, ICS and beta-agonists are commonly used, but leukotriene antagonists may play a key role in management. Leukotriene receptor antagonists (montelukast and zafirlukast) selectively block receptors for CysLT-1. Zileuton inhibits 5-lipoxygenase, thereby dampening production of all CysLTs, and impairing all downstream effects. By a broader range of activity, zileuton has displayed greater superiority to traditional leukotriene receptor antagonists [36]. Dietary avoidance of aspirin and desensitisation are also therapeutic options [37]. Aspirin desensitisation downregulates pro-inflammatory CysLTs and interleukin (IL)-4, and with subsequent daily aspirin therapy, appears to reduce severity and frequency of exacerbations [30, 36].
3.2 Allergic Bronchopulmonary Mycosis (ABPM)
3.2.1 Pathophysiology
In ABPM, fungal proteases damage bronchial epithelial cells, triggering an inflammatory response and hindering mucociliary clearance. Hyphal antigens from filamentous fungi are isolated by antigen-presenting cells (APCs). The APCs work together with activated respiratory epithelia to manufacture T helper cell type 2 (Th2)-promoting cytokines and chemokines [38, 39]. These inflammatory factors induce differentiation, recruitment and activation of CD4+ T cells into the Th2 subtype, producing biomarkers such as IL-4/IL-5. IL-4/IL-5 stimulate fungal-specific immunoglobulin E (IgE) production from plasmacytes, IgE priming of mast cells/basophils, and eosinophil recruitment and activation. This response sensitises the airways to specific fungal antigens, triggering a hypersensitivity response upon exposure (Fig. 1b). Chronic hypersensitivity with associated bronchiolar inflammation, cellular damage and impaired mucociliary clearance can progress to bronchiectasis and without intervention, ultimately, to fibrosis [13, 39].
3.2.2 Genetics
Susceptibility to ABPM is associated with polymorphisms in genes encoding for cystic fibrosis transmembrane conductance regulator, CHIT1 (innate immune system digestive enzyme with fungal activity), surfactant protein A2 or toll-like receptor-9, which all cause altered clearance of fungal spores/hyphae [40,41,42,43,44]. Individuals with polymorphisms in these genes have increased exposure and pathogen burden by fungal hyphae. Human leukocyte antigen (HLA) genes DR2/DR5 have also been implicated as susceptibility foci, certain alleles potentially promoting Th2 type response to pathogens [40, 45]. Furthermore, genetic variability affecting Th2 inflammatory pathways such as IL-4α receptor polymorphism (increasing receptor activity) is seen with increased frequency in ABPM patients [40, 46]. Combination of susceptibility genes may synergistically increase risk, and with the appropriate environmental exposure, ABPM can develop.
3.2.3 Biomarkers
Specific ABPM investigation includes total serum IgE measurement, serum Aspergillus IgE (Aspergillus-specific sensitisation) and Aspergillus skin testing. Results of these investigations are typically positive in active disease; however, ABPM caused by non-Aspergillus fungi may be more difficult to identify, and many physicians do not have access to advanced culture techniques or PCR, which would more accurately define airway colonisation [40].
3.2.4 Management
ABPM commonly fails to respond to inhaled beta-agonists and ICS, whilst OCS have historically been the mainstay of treatment. High-dose intravenous corticosteroid pulses have been suggested for controlling ABPM with reduced (but not nullified) steroid burden [8]. Anti-fungal agents, most commonly itraconazole (or newer posaconazole/voriconazole), aim to reduce the triggering allergen and destructive proteases which contribute to airway damage. Azoles have variable absorption, metabolism, drug interaction and toxicity and therefore require close monitoring [13]. An alternative anti-fungal is amphotericin, which can be delivered to the airways via nebulisation, but is poorly tolerated in asthma [13, 47, 48]. Another steroid-sparing agent utilised in ABPM is omalizumab (monoclonal anti-IgE antibody), which demonstrates reduction in exacerbation frequency and fractional exhaled nitric oxide (FeNO) levels [49].
3.3 Allergic Asthma
3.3.1 Pathophysiology
In allergic asthma, inhaled antigens trigger an allergic type response with Th2 type T cells producing inflammatory mediators such as IL-4, IL-5, IL-13 and eotaxin, which synergistically act to recruit, activate and target eosinophils to the lungs and regulate IgE synthesis [50,51,52]. Activated eosinophils and mast cells release CysLTs, triggering bronchoconstriction, smooth muscle proliferation and mucous secretion [50]. Mouse models have implicated sensitisation with low doses of bacterial endotoxin in triggering Th2 type responses via IL-4 and tumour necrosis factor-α (TNFα) signalling. Sensitisation with higher dose endotoxin may, however, stimulate Th1/Th17 type responses more typically associated with neutrophilic type inflammation [53] (Fig. 1c). In chronic obstructive pulmonary disease patients, a similar phenomenon of low bacterial load being associated with airway eosinophilia and higher bacterial loads correlating with neutrophilic/non-Th2 response has also been observed [54].
3.3.2 Genetics
Allergic asthma is associated with polymorphisms in genes mediating Th2 type immune responses. Single nucleotide polymorphisms of IL-4/IL-13 pathway genes are clustered amongst allergic asthmatics, and the number of variants an individual has correlates with severity [55]. Certain genotypes at the 17q12–21 locus correlate with raised IgE levels and eosinophil counts [56, 57]. Allergic asthma may also be potentiated by epigenetic processes, including methylation of genes promoting Th2 differentiation and IgE regulation. Protective factors such as childhood farm environment may exert effects on an epigenetic level [58]. Similar genetic profiles are observed in asthmatic API preschool wheezers with association with polymorphism in ORMDL3 (locus 17q21) and IL-4 [59]. Genetic variance of the ADAM33 gene (metalloproteinase crucial in bronchial hyper-responsiveness [60]) was also implicated in predicting childhood asthma amongst infant wheezers [59].
3.3.3 Management
Allergic asthma typically is steroid responsive; however, subsets of particularly severe asthmatics may be steroid unresponsive or OCS dependant. Key allergic asthma targets include IL4, IL-5, IL-13 and IgE, and biological inhibition of these target molecules has shown good therapeutic benefit [6, 61, 62].
3.4 Severe Late-Onset (Hyper-Eosinophilic) Asthma (SLOHA)
3.4.1 Pathophysiology
SLOHA demonstrates more progressive loss of lung function compared with atopic/early-onset asthma. SLOHA classically exhibits a Th2 type response, characterised by sputum and blood eosinophilia and basement membrane thickening. However, in contrast to atopic type asthma, in SLOHA there is an absence of lymphocytic/mast cell-medicated processes and the Th2 response is elicited by non-atopic mechanisms [63]. Hormonal factors may be involved in triggering SLOHA. Females of reproductive age or using exogenous hormone replacement appear to be at increased risk [64, 65], showing a similar demographic profile to autoimmune conditions. Akin to other autoimmune conditions, SLOHA patients also commonly require systemic treatments, with poorer responses to local/inhaled therapy [6]. Autoantibodies selective to bronchial tissues have been identified in SLOHA patients; however, causation or consequence of bronchial damage has not yet been determined. Potential target antigens include alpha-enolase (glycolytic enzyme) [66] and cytokeratin-18 (cytoskeletal protein) [67].
3.4.2 Genetics
SLOHA development shows association with specific CCL5/RANTES promoter region polymorphisms, producing exaggerated inflammatory responses to exogenous pathogenic stimuli. Response is exaggerated following cumulative exposure, suggesting manifestation at an older age [68]. Polymorphism of the anti-inflammatory Clara cell secretory protein gene shows concordance with airway hyper-responsiveness and SLOHA [69].
3.4.3 Biomarkers
SLOHA probably represents a variety of individual “endotypes” as there is marked heterogeneity in the cytokine profile of SLOHA patients; in the future when we successfully personalise therapies, choice could be made using the monoclonal antibody to antagonise the specific cytokine found in highest concentration in each individual. SLOHA demonstrates Th2 responses and associated raised biomarkers such as FeNO and eotaxins (eosinophilic chemotactic agents) in the absence of allergic stimuli [70]. Eotaxins correlate with severity of asthma, and eotaxin-2 showed greatest association with SLOHA [70, 71]. Eotaxins are raised in allergic asthma, but appear even higher in hyper-eosinophilic autoimmune conditions such as eosinophilic granulomatosis with polyangiitis [72].
3.4.4 Management
SLOHA often requires OCS for control; however, novel monoclonal antibody therapy may hold the key [6]. Antagonism of Th2 mediators (IL-4, IL5 and IL-13) has demonstrated effectiveness in managing SLOHA, even in steroid refractory disease [70]. Mepolizumab (an anti-IL-5 monoclonal antibody) shows steroid-sparing effects, reduced sputum and blood eosinophils and better asthma control, especially in steroid-dependant or resistant patients [17]. Likewise, reslizumab reduces exacerbation frequency and improves lung function in patients with elevated blood eosinophils and a history of frequent exacerbations [18]. Benralizumab, a monoclonal that targets the IL-5 receptor may also soon be available, and the relative efficacy and cost effectiveness of each of these will require careful assessment. Dupilumab is also undergoing research evaluation as an anti-IL4/5 combined antagonist [20].
Prostaglandin D2 receptor antagonism has also demonstrated beneficial reduction in airway eosinophilic inflammation [22].
3.5 Asthma of Cross-Country Skiers (ACCS)
3.5.1 Pathophysiology
Exercise is a common trigger in asthmatics, particularly when poorly controlled. However, a population of otherwise healthy individuals who have respiratory symptoms stimulated by intense exercise in cold, dry conditions has been recognised and named to reflect the initial population in which it was observed (cross-country skiers) [73]. Despite the name, it is likely the phenotype applies to all competitive athletic performance where high flow inspiratory intensity is achieved at maximum exercise. In contrast to allergic and other forms of asthma, ACCS does not demonstrate marked elevation in sputum eosinophil, mast cell and macrophage counts, but instead exhibits increased airway neutrophil numbers. In both allergic asthma and ACCS, airways demonstrate a greater number of T lymphocytes, indicating inflammatory processes [74]. ACCS is triggered during high-intensity training (in particular in cold, dry conditions such as cross-country skiing) where excessive ventilation causes extreme cooling/drying of the epithelial surface. Epithelial cells dehydrate and concentrate their ionic composition, attempting to maintain osmotic homeostasis [75, 76]. Stressed epithelial cells stimulate an inflammatory cascade producing mediators such as eicosanoids, CysLTs and histamine, and reducing anti-inflammatory prostaglandin E2 and thromboxane B2. The overall effect triggers bronchoconstriction [75, 77] (Fig. 1d). Alternative theories hypothesised that airway cooling elicits parasympathetic bronchoconstriction and vasoconstriction to minimise heat loss. When exercise stops and the cooling trigger is removed, rebound vasodilation with resultant mucosal oedema and smooth muscle constriction occurs [75]; this alternative proposed mechanism has been more difficult to validate. Following high-intensity activity, athletes demonstrate increased apoptosis of bronchial epithelial cells and excess neutrophils in induced sputum [78, 79]. Neutrophil counts correlate with training frequency. The type of exercise or exercise environment may also affect pathophysiology; swimmers develop neutrophilia and mild eosinophilia in sputum thought to be in relation to chlorine or chloramine exposure [78].
3.5.2 Genetics
ACCS susceptibility may be conveyed through polymorphism/loss of function in aquaporin water channels. Aquaporin-5 knockout mice display bronchiolar hyper-responsiveness to methacholine, whilst in athletes methacholine responsiveness correlates with sweat, tear and salivary production. Reduced activity aquaporin polymorphism could hypothetically confer risk for ACCS via accelerating airway drying [80]; however, specific genetic links are yet to be proven.
3.5.3 Biomarkers
ACCS demonstrates normal blood eosinophil counts and FeNO, as expected from non-Th2 inflammation. ACCS does exhibit raised urinary CysLTs [6, 36], but this is not specific to ACCS.
3.5.4 Management
The mainstay of treatment for ACCS is reducing training intensity; ICS alone are rarely sufficient to control symptoms. Protection from/avoidance of extreme cold/dry conditions whilst training is crucial, and pre-exercise and as-required bronchodilators may be beneficial [80]. In contrast to this, exercise-induced asthma will typically reflect poor asthma control from other forms (commonly allergic asthma), whereby an increase in standard therapies including bronchodilators and ICS will provide benefit [73].
It is also key in this condition to differentiate the genuine lower airway symptoms from the additional common feature of such athletes, exercise inducible laryngeal obstruction (EILO).
3.6 Other Endotypes: Neutrophilic Asthma
3.6.1 Pathophysiology
The Lötvall et al. system of classification is not all inclusive, and there are subgroups of patients who do not comply with the previous categories. For example, a subgroup of asthmatic patients with neutrophilic driven inflammation (without exercise association) has also been described. This subgroup typically exhibits severe asthma symptoms non-responsive to corticosteroids, often with associated triggers such as smoking or exhaust fumes [81, 82]. Such triggers have precipitated Th17 type inflammation in asthmatics [81, 82]. CD4 Th cells differentiate under the influence of transforming growth factor-β (TGF-β), IL-6, IL-1β and IL-23 into Th17 cells. Th17 cells secrete mediators including IL-17A, IL-17F, and IL-22, which increase mucous cell metaplasia, expand airway smooth muscle volume and stimulate airway epithelial activation and attraction of neutrophils [83]. IL-17A and IL-17F expression also correlates with severity of asthma [84]. Airway neutrophilia may occur reactively in response to pathogens. IL-17F knockout mice have attenuated neutrophil airway recruitment compared with wild-type in response to fungal proteinase [85]. High-dose bacterial endotoxin exposure induces Th1/Th17 type responses and neutrophil-mediated inflammation [53].
3.6.2 Genetic
Glutathione S-transferase M1 (GSTM1) functional genotype (present in approximately half of northern European descendants) promotes greater allergen-induced neutrophilia than GSTM1 null patients, and is associated with increased production of pro-neutrophilic mediators such as CXCL-8, IL-1β and IL-6 [86]. Certain IL-17F alleles with increased activity have also shown correlation with asthma, and mouse models with raised IL-17F levels demonstrate bronchial neutrophilic infiltration [87].
3.6.3 Biomarkers
Sputum neutrophilia correlates with raised sputum IL-1ß and matrix metalloproteinase-9 (MMP-9) (a protein involved in the degradation of extracellular matrices), whilst sputum intracellular adhesion molecule-1 (ICAM-1) (an epithelial/immune cell surface receptor) levels were increased in patients with low sputum neutrophil counts [88]. Sputum fibrinogen levels demonstrate correlation with luminal narrowing in the presence of sputum neutrophilia [88].
3.6.4 Management
Adult-onset non-eosinophilic (neutrophilic) asthma is commonly steroid unresponsive with relatively few treatment options. Maintenance macrolides have been used in this subgroup, with moderate success [89]. Chemokine CXCR2 inhibition has demonstrated modest improvement in neutrophilic asthma control and reducing mild-moderate exacerbations [90]. Surprisingly, blockade of IL-17 (Th17 neutrophilic mediator) has not translated into clinical improvement; however, further investigation may be warranted [70, 91].
4 Exploration of Phenotypes Using Cluster Analysis
Individual asthma subgroups have also been pursued by cluster analysis. Cluster analysis allows grouping of patients by using similarities in measurable characteristics, for example, demographic details, exhaled compounds, serum biomarkers or lung function [92, 93]. Cluster analysis may help to find clinically applicable methods of grouping a patient’s characteristics and help predict likely treatment response. However, the ‘cluster’ is by definition the identification of a group of closely allied features and may contain a plethora of actual endotypes.
The Severe Asthma Research Program (SARP) has undertaken large cluster analysis (in the form of SARP 1/2/3) in order to differentiate and elucidate some phenotypically distinct groups. Univariate analysis of data from lung function, FeNO, blood and sputum cellular and biochemical contents, subjective symptom questionnaires, demographic characteristics (such as gender, height and weight) and genetic profiling, was undertaken in an attempt to statistically group patients [94,95,96,97,98].
In 2010, the initial SARP analysis identified five clusters, which are roughly outlined as follows [97]:
-
1.
Predominantly young, female, atopic, childhood onset, with mild and often exercise-induced disease
-
2.
Slightly older, predominantly female, atopic, childhood onset, reversible or well-controlled asthma, but requiring more intervention than cluster 1
-
3.
Mainly older women, with a raised body mass index, late-onset asthma, high symptom burden, severe disease and requiring higher therapeutic intervention
-
4.
Severe atopic, childhood onset, demonstrates good reversibility
-
5.
Severe asthma, poor control and relatively fixed airflow obstruction.
There is some obvious overlap seen between the distinct clusters identified during the SARP analysis, and this may therefore make it difficult on an individual basis to determine which specific cluster a patient may fall into. It is also possible to observe similarities or differences between the suggested clusters with groups from the Lötvall et al. endotype classification, such as SLOHA and cluster 3, whilst other endotypes such as allergic asthma would appear to be spread across clusters 1, 2 and 4.
The TENOR cohort analysis identified clusters in both childhood, and adolescent and adult cohorts. These again were distinct from the SARP studies, yet demonstrated considerable overlap with SARP clusters, but also with Lötvall et al.’s endotypes [99]. Within the adult/non-adolescent analysis, clusters were identified with early onset, atopic type asthma (relatable to SARP clusters 1/2), and other clusters were also identified with severe asthma associated with aspirin sensitivity—reminiscent of AARD [99].
The results of many of these cluster analysis studies have identified groups with typical disease patterns and behaviours, but cluster analysis would only show translational benefit if it were a way of predicting response to treatment. By performing cluster analysis with an outcome variable of treatment response, it is possible to identify traits, characteristics or clusters, which can predict specific success of a therapeutic intervention. Cluster analysis in this way has been successfully used to identify subgroups and enable prediction of response to systemic corticosteroids [98], or to newer targeted therapies such as the IL-5 antagonist mepolizumab [100].
This retrospective cluster analysis may be the first step towards the new age of personalised medicine—with the futuristic ideal of being able to input patient characteristics and be given an individual outcome/predicted response profile to all available treatments. But in such an environment, it will also be important to recognise that with any type of classification there will still be specific individual patients who do not fit neatly into any one endotype/phenotype/cluster, and will not behave as predicted. Certain patients may be deemed to have a low chance of success from a specific treatment and therefore be inappropriately precluded from access to a therapeutic option which could have been beneficial. Additionally, groups of patients will have overlapping pathophysiological processes or even aspects from more than one endotype, making it important to always retain focus on the individual patient and the potential to help produce tailored management.
5 Investigations
Whilst creating a personalised approach to asthma management, it is important to identify methods of detecting specific features that might lead to targeted therapies. For the most part this work is done using a formalised investigation profile, using generic tests and then adding some specific phenotype-targeted investigations.
5.1 Imaging
Imaging the lungs effectively in asthma can be useful in solidifying the diagnosis, identifying severity and also the regional or generalisability of changes, for planning targeted treatments. Regional tissues within asthmatic patients may show heterogeneity in their chronic structural changes, reactivity and pathophysiology, suggesting that a wide dispersal of an individual therapy may not be universally successful or optimal. However, local or regionally focussed treatments such as bronchial thermoplasty may produce added benefits in such cases [101,102,103,104].
Additionally, by identifying patients with peripheral disease, we may be able to target therapies, such as the need for inhaled therapies to concentrate on small particle deposition in those in whom small airway disease has been identified [102, 104].
Furthermore, ventilatory defects have been identified radiologically in well controlled patients with normalised lung function and who are asymptomatic, suggesting the pathological processes may be ongoing despite apparent physiological inactivity [101].
5.1.1 High-Resolution Computed Tomography (HRCT) in Routine Practice
It is now widely accepted in UK clinical practice [105] that high-resolution computer tomography (HRCT), should be performed on all patients with severe or refractory asthma. Airway wall thickening on HRCT positively correlates with severity of asthma and inversely correlates with gas transfer coefficient [106]. HRCT-determined airway geometry has revealed that high luminal and total airway volume is associated with low sputum neutrophil counts and raised sputum CCL11 (eotaxin-1, an eosinophil chemotactic protein). Reduced luminal area identified on HRCT is associated with raised IL-1α levels [88].
By accurately assessing lung geometry, it may be possible to define severity, progression and predict suitable treatment options. Despite the common use of HRCT imaging, the American Thoracic Society (ATS)/European Respiratory Society (ERS) joint guidelines do not advise routine HRCT scanning unless there is an alternate indication or atypical presentation [62]. However, there is clear evidence that alternative diagnoses made by HRCT are very common (e.g. bronchiectasis being identified on HRCT in 35% of scanned asthmatics in one UK study [107]). Failure to perform HRCT may result in missed critical alternative diagnoses in many patients, which would be key in guiding successful treatment strategies.
The presence and even the extent of bronchial wall thickening have been used to determine the suitability of asthma patients for the treatment modality of bronchial thermoplasty. At present, the extent of thickening has been established with bronchial biopsy [108] or by optical coherence tomography (OCT) (see Sect. 5.1.4) [63]; however, it is hoped these data will be compared to quantitative or qualitative HRCT analysis for dissemination of these results to the broader population, hopefully without the need for bronchial biopsy or complex research level airway imaging techniques first.
5.1.2 Other Imaging Modalities
Other imaging techniques are largely research tools at this stage, but examples of complex imaging strategies include xenon ventilation CT with dual energy and dual source, hyperpolarised noble gases helium-3 (3He) or xenon-129 (129Xe) ventilatory contrast magnetic resonance imaging (MRI) and dynamic oxygen-enhanced MRI imaging. These are all functional imaging techniques that can determine distal small airway obstruction with local ventilatory variation, which correlates with degree of asthma control, disease severity and degree of methacholine-induced bronchoconstriction [101, 102, 109]. Helium is difficult to produce in a polarised state; therefore, oxygen-enhanced imaging may have practical superiority, resulting in more extensive clinical dissemination [102].
5.1.3 Forced Oscillation Technique (FOT)
Other functional measurements are becoming increasingly explored, such as forced oscillation technique (FOT), which provides measurement of the mechanical properties of the airways using responses to external vibration during normal respiration. Variation in frequency can be used to identify airway calibre, and FOT has been reliably used to demonstrate bronchial hyper-responsiveness through a non-invasive method [101, 110].
5.1.4 Optical Coherence Tomography (OCT)
OCT detects the backscatter from near infrared light waves to produce high-resolution images in the range of 1–20 µm. OCT can monitor real-time airway thickness, which correlates with the degree of bronchial hyper-responsiveness, and has demonstrated accurate methods of quantifying reduction in airway thickness post-bronchial thermoplasty [63, 111].
Whilst certain imaging modalities have been correlated with disease severity and standard HRCT has been used to explore the diagnosis, there is hope that current techniques used in the research arena will prove to be clinically useful and guide exploratory or locally targeted therapies.
5.2 Using Predictive Biomarkers
The advent of monoclonal antibodies and small molecules has allowed specific biological mechanisms and pathophysiological processes to be targeted during treatment. When using a therapy which targets a specific pathological process, in order for the treatment to be effective, it is essential that the specific pathological process is active. Given the heterogeneous nature of severe asthma, it becomes imperative that we are able to correctly identify the pathological processes and targeted mechanisms to effectively identify suitable candidates for given treatment options. This need is heightened when these therapies are expensive and health economic models of cost/benefit are applied to their availability.
The current drive with pharmacotherapy is to provide biomarkers, which identify patients most likely to respond to specific therapies. This will lead to a more individualised patient treatment plan. However, the work revolves around cluster analysis, correlation and averages. Hence it is entirely possible that individual patients will lose out with this approach, as treatments that may have worked for an individual will not be offered because they do not carry the generalisable specific marker of response. Nevertheless, such approaches will improve health economic efficiency, by giving expensive novel therapies only to those with the highest statistical chance of success. The following section explores the currently viable examples of biomarkers or best clinically available equivalent tests.
5.2.1 Sputum Eosinophilia
Airway eosinophilia indicates asthma severity (assuming adherence to standard ICS therapy) and is the best predictor of short-term corticosteroid responsiveness. Asthma treatment based on normalising sputum eosinophil count [in comparison to standard British Thoracic Society (BTS) guidelines] has been shown to reduce exacerbations and admissions without corresponding increases in anti-inflammatory treatments [112]. The BTS standard algorithm would increase therapy on the basis of increasing symptoms, reduced peak flow measurements, increase in frequency of beta2-agonist use or following an exacerbation. Similarly, treatment would be theoretically reduced if symptoms had remained stable for 2 consecutive months. However, measuring bronchial eosinophilia accurately is relatively invasive (airway biopsy, bronchial lavage for cell differential or sputum induction) [113]. Peripheral markers of bronchial eosinophilia including FeNO, serum eosinophil counts and IgE, all show correlation with sputum eosinophil count, but alone have a substantial false-positive/negative potential [114]. Serum eosinophilia is associated with superior efficacy in IL-5 antagonism by mepolizumab; unselected asthmatic patients show heterogeneity in their response [115].
5.2.2 Immunoglobulin E (IgE) Levels
Initially IgE levels were thought to be beneficial in targeting anti-IgE (omalizumab) therapy; however, large pooled population analysis has demonstrated that IgE levels are unable to consistently identify responders from non-responders [116]. More recent evaluation of baseline characteristics has demonstrated a predictive relationship between serum eosinophils, FeNO and periostin in forecasting response to omalizumab [117].
5.2.3 Fractional Exhaled Nitric Oxide (FeNO)
Inflammatory triggers stimulate epithelial nitric oxide synthase, which upregulates production of nitric oxide, providing a measurable representation of the inflammatory process [118]. FeNO levels display negative correlation with asthma control. Patients displaying allergic phenotypes with positive skin prick tests, allergic rhinitis or allergic conjunctivitis all show higher levels of FeNO than those without. FeNO also associates with number of emergency room visits, suggesting a prognostic application [119].
5.2.4 Periostin
Periostin is an extracellular and matri-cellular protein produced downstream of Th2 immune responses via IL-13 signalling. The exact actions of periostin in asthma have not been fully elucidated; however, periostin has been identified as a surrogate for IL-13, IgE and Th2 type responses. Periostin levels correlate with sputum eosinophilia and FeNO [35].
Raised periostin levels can predict responses to anti-IgE antibodies (omalizumab) [120], especially in ICS unresponsive patients. Studies had initially identified high periostin levels as a marker to determine benefit in reducing exacerbation rates in response to anti-IL-13 antibodies (lebrikizumab) [117]; however, subsequent studies have been unable to replicate these results, and thus lebrikizumab is no longer being evaluated as an asthma therapy [121].
5.2.5 Volatile Organic Compounds
Novel research has highlighted that volatile organic compounds in exhaled air differ between asthmatic and non-asthmatic patients. What’s more, distinct subgroups of patients have been identified by cluster analysis into potential endotypes, with a range of phenotypic manifestations, but similar exhaled biochemical profiles [88]. Other evaluations of exhaled air have demonstrated that poorly controlled asthma and acute attacks are associated with lower pH of the breath condensate [122].
5.2.6 Other Biomarkers
Galectin-3 is a lectin involved in cellular adhesion, chemo-attraction and IgE binding. Sputum galectin-3 is present in low levels in patients with neutrophilic/non-Th2 type inflammation, and high levels in patients who morphologically respond to anti-IgE (omalizumab) treatment [118]. Other markers in sputum of Th2/IgE type inflammation have also been described, such as IL-33 and thymic stromal lymphopoietin, and these markers also appear to be linked with lower lung function [123].
6 Targeted Management for Asthma
6.1 Relevance of Asthma Phenotyping/Endotyping to Existing Therapies and Guidance
Leukotriene pathway inhibitors act synergistically with ICS to improve lung function and reduce exacerbation frequency [124]. They are key in the management of AARD; however, response to anti-leukotriene drugs is not specific to aspirin sensitivity [125].
Typically eosinophilic asthma responds to corticosteroid treatment, although long-term OCS are potentially highly toxic, and so a number of steroid-sparing techniques are being increasingly employed. Conventional disease-modifying anti-rheumatic drugs such as methotrexate, ciclosporin, mycophenolate and azathioprine are occasionally used in severe asthma as steroid-sparing agents. Despite their use, the ATS/ERS guidelines advise against them, but for some patients the only alternative is increasing OCS, which is almost certainly a worse option.
The main objection to the steroid-sparing therapies is surrounding toxicity, when weighed against modest disease benefit, but on a case-by-case basis in specialist centres, certain patients requiring daily OCS may have clinical justification [62, 126].
As discussed previously, azole antifungal treatment demonstrates therapeutic benefit in managing ABPM.
Low-dose macrolides have been used to reduce non-eosinophilic (neutrophilic) inflammation, but results are contradictory [89, 127]. ATS/ERS guidelines do not currently support the routine use of macrolides unless for alternate indications, e.g. bacterial infections [62]. The recent double-blind, placebo-controlled AMAZES trial showed significant reduction in exacerbation frequency and improvement in quality of life from the use of oral azithromycin compared to placebo in asthmatic patients [128]. The patients entered into this trial were poorly controlled, however, and had not been selected on the basis of biochemical markers or phenotype/endotype. Benefit from macrolides may not be limited to a single subgroup (e.g. neutrophilic asthma), and by limiting treatment to specific patients, we may be precluding certain groups from potential therapeutic options.
6.2 Biomarker-Guided Biological Therapies
Generic use of many monoclonal antibodies in asthma initially showed modest or disappointing results, which led investigators to attempt to use biological therapies in select subgroups or populations targeted by specific biomarkers. Mepolizumab, benralizumab (anti-IL-5 receptor-α antibody) and reslizumab (anti-IL-5 antibody) have shown beneficial results, with specificity for eosinophilic asthmatics [18, 19, 115, 129]. Selectivity in determining treatment response appears for these therapies to be the key in developing a personalised approach.
Not all immune-modulatory targets have translated into successful treatments. Lebrikizumab (anti-IL-13 monoclonal antibody) was initially shown to increase lung function in steroid unresponsive patients, with high periostin levels specifically identifying likely benefit [117]. However, subsequent phase III studies failed to replicate these initially evident responses, and this led to the withdrawal of its planned use in asthma [121]. Tralokinumab (anti-IL-13) similarly failed to reduce annual exacerbation rates in phase III trials; however, potential reduction in exacerbation rates were identified in subgroups of patients with elevated surrogate markers of increased IL-13 activity [21, 23].
TNF-α antagonism showed no clinical benefit and was associated with significant toxicity [130]. These studies were in unselected patient groups, and so investigation into selective patient subpopulations may show potential benefit in future [21].
Inhaled pitrakinra (IL-4/IL-13 pathway antagonist) treatment has been shown to reduce the frequency of asthma exacerbations specifically in high-eosinophil asthma [131]. Other biomarkers for response were also identified, with specific IL-4 receptor-α genotypes demonstrating increased responsiveness to treatment [132]. However, phase IIb trials failed to meet their primary endpoint, resulting in discontinuation of the pitrakinra in asthma.
IL-4/IL-5 pathway inhibitors such as the anti-IL-4Rα antibody (dupilumab) have demonstrated effects of increasing lung function and reducing exacerbation frequency [20].
Therapy with antibodies blocking thymic stromal lymphopoietin (epithelial derived pro-inflammatory cytokine) has demonstrated a reduction in allergen-induced bronchoconstriction and airway inflammation [133].
6.3 Bronchial Thermoplasty
Bronchial thermoplasty uses radiofrequency pulses to target airway smooth muscle in the bronchial tree. Three consecutive bronchoscopic procedures are performed under conscious sedation or general anaesthesia in 3-weekly intervals, reducing airway smooth muscle mass, bronchial nerve endings and neuroendocrine epithelial cells [134]. Bronchial thermoplasty improves quality of life and reduces exacerbation frequency and hospital admissions for up to 5 years.
In the immediate post-procedure period (first 6 weeks), there is substantial risk of exacerbation, so careful monitoring is essential at this time [126, 135]. ATS/ERS guidelines advise use only in severe asthmatics in the context of a trial or with institutional review board authorisation [62].
Bronchial thermoplasty has also not been investigated fully in terms of which specific patient population might be the biggest responder. As such it can be labelled as “not having a companion biomarker”. This may lead to a restriction in its use, whilst in practice it might work with high effect over a range of asthma phenotypes. It is hoped that ongoing research will help answer this question. In the interim, there is a fear that over-fixation on “therapy related biomarkers” or treatable traits may result in patients not having access to a potentially effective treatment modality.
7 Therapeutic Barriers
Whilst some patients will have severe refractory disease which is uncontrolled by all measures attempted, there are a number of other reasons why patients may not be responding to treatment. Non-compliance, continued exposure to allergen or smoking represent a significant burden of potentially treatable patients. Education and enabling patients to take control of their illness are essential in disease management. Co-morbidities can also complicate asthma and limit therapeutic effects. For example, obesity-related airway obstruction, gastro-oesophageal reflux, dysfunctional breathing and tracheobronchomalacia can all cause significant symptoms, which mimic or coincide with asthma and worsen apparent control. Without identifying and controlling such co-morbidities, any asthma management will not be sufficient to result in a successful clinical outcome [126, 136].
8 Conclusion
As ‘asthma’ encompasses a wide range of conditions with differing pathophysiological processes and phenotypic outcomes, responses to individual treatments are variable. Whilst understanding the pathophysiological mechanisms and endotyping/phenotyping is important, the key will be to produce a personalised profile for each patient with regard to disease course, prognosis and personalised management. This is especially important in severe or refractory asthma.
Certain treatments that have previously appeared to be of no statistical clinical benefit may indeed be useful in particular subsets of asthma, indicating the potential for further targeted research into previously disregarded therapies. With the advent of newer treatments, soon a wide range of therapeutic options will be available for refractory asthma, and it will be important to identify readily measurable biomarkers and non-invasive imaging techniques to guide treatment. Ideally producing an individual profile for each patient will help predict treatment response and enable personalised and more effective management.
References
British Thoracic Society, Scottish Intercollegiate Guidance Network. British guideline on the management of asthma: a national clinical guideline. 2016. http://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2016 Accessed 08 Oct 2016.
Kiley J, Smith R, Noel P. Asthma phenotypes. Curr Opin Pulm Med. 2007;13(1):19–23.
Bel EH. Clinical phenotypes of asthma. Curr Opin Pulm Med. 2004;10(1):44–50.
Hekking PPW, Bel EH. Developing and emerging clinical asthma phenotypes. J Allergy Clin Immunol. 2014;2(6):671–80.
Drazen JM, Silverman EK, Lee TH. Heterogeneity of therapeutic responses in asthma. Brit Med Bull. 2000;56(4):1054–70.
Lötvall J, Akdis CA, Bacharier LB, et al. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy Clin Immunol. 2011;127(2):355–60.
Wesolowska-Anderson A, Seibold MA. Airway molecular endotypes of asthma: dissecting the heterogeneity. Curr Opin Allergy Clin Immunol. 2015;15(2):163–8.
George BJ, Reif DM, Gallagher JE, et al. Data-driven asthma endotypes defined from blood biomarker and gene expression data. PLoS One. 2015;10(2):e0117445. doi:10.1371/journal.pone.0117445.
Agache I, Akdis C, Jutel M, et al. Untangling asthma phenotypes and endotypes. Allergy. 2012;67(7):835–46.
Rajan JP, Wineinger NE, Stevenson DD, et al. Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: a meta-analysis of the literature. J Allergy Clin Immunol. 2015;135(3):676–81.
Denning DW, O’Driscoll BR, Hogaboam CM, et al. The link between fungi and severe asthma: a summary of the evidence. Eur Respir J. 2006;27:615–26.
Farrant J, Brice H, Fowler S. Fungal sensitisation in severe asthma is associated with the identification of Aspergillus fumigatus in sputum. J Asthma. 2016;53(7):732–5.
Meyer N, Dallinga JW, Nuss S, et al. Defining adult asthma endotypes by clinical features and patterns of volatile organic compounds in exhaled air. Resp Res. 2014;15:136.
Denning DW, O’Driscoll BR, Powell G, et al. Randomized controlled trial of oral antifungal treatment for severe asthma with fungal sensitization: the Fungal Asthma Sensitization Trial (FAST) study. Am J Respir Crit Care Med. 2009;179(1):11–8.
Castro-Rodriguez JA, Holberg CJ, Wright AL, et al. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med. 2000;162:1403–6.
Walford HH, Doherty TA. Diagnosis and management of eosinophilic asthma: a US perspective. J Asthma Allergy. 2014;7:53–65.
Nair P, Pizzichini MMM, Kjarsgaard M, et al. Mepolizumab for prednisolone-dependant asthma with sputum eosinophilia. N Engl J Med. 2009;360:985–93.
Castro M, Zangrilli J, Wechsler ME, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Resp Med. 2015;3(5):355–66.
Fitzgerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016. doi:10.1016/S0140-6736(16)31322-8.
Wenzel S, Castro M, Coreen J, et al. Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high dose inhaled corticosteroids pus a long-acting β2 agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet. 2016;388(10039):31–44.
Brightling CE, Chanez P, Leigh R, et al. Efficacy and safety of tralokinumab in patients with severe uncontrolled asthma: a randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Resp Med. 2015;3(9):692–701.
Gonem S, Berair R, Singapuri, et al. Fevipiprant, a prostaglandin D2 receptor 2 antagonist, in patients with persistent eosinophilic asthma: a single-centre, randomised, double-blind, parallel-group, placebo-controlled trial. Lancet. 2016;4(9):699–707.
Helenius I, Lumme A, Haahtela T. Asthma, airway inflammation and treatment in elite athletes. Sports Med. 2005;35(7):565–74.
Sestini P, Armetti L, Gambaro G, et al. Inhaled PGE2 prevents aspirin-induced bronchoconstriction and urinary LTE4 excretion in aspirin-sensitive asthma. Am J Respir Crit Care Med. 1996;153(2):572–5.
Picado C, Fernandez-Morata JC, Juan M, et al. Cyclooxygenase-2 mRNA is down expressed in nasal polyps from aspirin-sensitive asthmatics. Am J Respir Crit Care Med. 1999;160:291–6.
Szczeklsik A, Mastalerz L, Nizankowska E, et al. Protective and bronchodilator effects of prostaglandin E and salbutamol in aspirin-induced asthma. Am J Respir Crit Care Med. 1996;153(2):567–71.
Sladek K, Szczeklik A. Cysteinyl leukotrienes overproduction and mast cell activation in aspirin-provoked bronchospasm in asthma. Eur Respir J. 1993;6:391–9.
Christie PE, Tagari P, Ford-Hutchinson AW, et al. Urinary leukotriene E4 concentrations increase after aspirin challenge in aspirin-sensitive asthmatic subjects. Am Rev Respir Dis. 1991;143(5Pt1):1025–9.
Cowburn AS, Krzysztof S, Soja J, et al. Overexpression of leukotriene C4 synthase in bronchial biopsies from patients with aspirin-intolerant asthma. J Clin Investig. 1998;101(4):834–46.
Steinke JW, Borish L. Factors driving the aspirin exacerbated respiratory disease phenotype. Am J Rhinol Allergy. 2015;29(1):35–40.
Jinnai N, Sakagami T, Sekigawa T, et al. Polymorphisms in the prostaglandin E2 receptor subtype 2 gene confer susceptibility to aspirin-intolerant asthma: a candidate gene approach. Hum Mol Genet. 2004;13(24):3203–17.
Liu T, Laidlaw TM, Katz HR, et al. Prostaglandin E2 deficiency causes and phenotype of aspirin sensitivity that depends on platelets and cysteinyl leukotrienes. P Natl Acad Sci Biol. 2013;110(42):16987–92.
Kim S-H, Oh J-M, Kim Y-S, et al. Cysteinyl leukotriene receptor 1 promoter polymorphism is associated with aspirin-intolerant asthma in males. Clin Exp Allergy. 2006;36:433–9.
Laidlaw TM, Boyce JA. Pathogenesis of aspirin-exacerbated respiratory disease and reactions. Immunol Allergy Clin North Am. 2013;33(2):195–210.
Izuhara K, Ohta S, Ono J. Using periostin as a biomarker in the treatment of asthma. Allergy Asthma Immunol Res. 2016;8(6):491–8.
Steinke JW, Wilson JM. Aspirin-exacerbated respiratory disease: pathophysiological insights and clinical advances. J Asthma Allergy. 2016;9:37–43.
Levy JM, Rudmik L, Peters AT, et al. Contemporary management of chronic rhinosinusitis with nasal polyposis in aspirin-exacerbated respiratory disease: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2016;6(12):1273–83.
Knutsen AP, Slavin RG. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin Dev Immunol. 2011;843763:1–14.
Hogan C, Denning DW. Allergic bronchopulmonary aspergillosis and related allergic syndromes. Semin Respir Crit Care Med. 2011;32(6):682–92.
Agarwal R, Chakrabarti A, Shah A, et al. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43:850–73.
Vincenzo AG, Chupp GL, Tsirilakis K, et al. CHIT1 mutations: genetic risk factor for severe asthma with fungal sensitization? Pediatrics. 2010;126(4):e982–5.
Vaid M, Kaur S, Sambatakou H, et al. Distinct alleles of mannose binding lectin (MBL) and surfactant proteins A (SP-A) in patients with chronic cavitatory pulmonary aspergillosis and allergic bronchopulmonary aspergillosis. Clin Chem Lab Med. 2007;45(2):183–6.
Carvalho A, Pasqualotto AC, Pitzurra L, et al. Polymorphisms in toll-like receptor genes and susceptibility to pulmonary aspergillosis. J Infect Dis. 2008;197(4):618–21.
Agarwal R, Khan A, Aggarwal AN, et al. Link between CFTR mutations and ABPA: a systematic review and meta-analysis. Mycoses. 2012;55(4):357–65.
Chauhan B, Santiago L, Hutcheson PS, et al. Evidence for the involvement of two different MHC class II regions in susceptibility of protection in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 2000;106(4):723–9.
Knutsen AP, Kariuki B, Concolino JD, et al. IL-4 alpha chain receptor (IL-4Rα) polymorphisms in allergic bronchopulmonary aspergillosis. Clin Mol Allergy. 2006;4(1):1–4.
Godet C, Goudet V, Laurent F, et al. Nebulised liposomal amphotericin B for Aspergillus lung diseases: case series and literature review. Mycoses. 2015;58:173–80.
Chishimba L, Landridge P, Powell G, et al. Efficacy and safety of nebulised amphotericin B (NAB) in severe asthma with fungal sensitisation (SAFS) and allergic bronchopulmonary aspergillosis (ABPA). J Asthma. 2015;52(3):289–95.
Voskamp AL, Gillman A, Symons K, et al. Clinical efficacy and immunologic effects of omalizumab in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol: In Practice. 2015;3(2):192–9.
Possa S, Leick EA, Prado CM, et al. Eosinophilic inflammation in allergic asthma. Front Pharmacol. 2013;4:46. doi:10.3389/fphar.2013.00046.
Brightline CE. Eosinophils, bronchitis and asthma: pathogenesis of cough and airflow obstructions. Pulm Pharmacol Ther. 2011;24:324–7.
Lemanske RF Jr, Busse WW. Asthma: clinical expression and molecular mechanisms. J Allergy Clin Immunol. 2010;125:S95–102.
Kim Y-M, Kim Y-S, Jeon SG, et al. Immunopathogenesis of allergic asthma: more than the th2 hypothesis. Allergy Asthma Immunol Res. 2013;5(4):189–96.
Kolsum U, Donaldson GC, Singh R, et al. Blood and sputum eosinophils in COPD; relationship with bacterial load. Respir Res. 2017;18:88. doi:10.1186/s12931-017-0570-5.
Slager RE, Li H, Moore W, et al. Predictive model of severe atopic asthma phenotypes using interleukin 4/13 pathway polymorphisms. In: American Thoracic Society International Conference. A33. Genetic and Epigenetic Regulation of Lung Disease. 2011, A1332.
Moffatt MF, Kabesch M, Liang L, et al. Genetic variants regulating ORMDL3 expression contribute to the risk of childhood asthma. Nature. 2007;448:470–3.
Andiappan AK, Sio YY, Lee B, et al. Functional variants of 17q12-21 are associated with allergic asthma but not allergic rhinitis. J Allergy Clin Immunol. 2016;137(3):758–66.
Michel S, Busato F, Genuneit J, et al. Farm exposure and time trends in early childhood may influence DNA methylation in genes related to asthma and allergy. Allergy. 2013;68(3):355–64.
Klaassen EMM, Penders J, Jöbsis Q, et al. An ADAM33 polymorphisms associated with progression of preschool wheeze into childhood asthma: a prospective case control study with replication in a birth cohort study. PLoS One. 2015;10(3):e0119349.
Holgate ST, Davies DE, Murphy G, et al. ADAM33: just another asthma gene or a breakthrough in understanding the origins of bronchial hyperresponsiveness? Thorax. 2003;58(6):466–9.
Durham AL, Caramoiri G, Chung KF, et al. Targeted anti-inflammatory therapeutics in asthma and chronic obstructive lung disease. Transl Res. 2016;167(1):192–203.
Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Resp J. 2014;43:343–73.
D’Hooghe JNS, De Bruin DM, Wijmans L, et al. Bronchial wall thickness assessed by optical coherence tomography (OCT) before and after bronchial thermoplasty (BT). Eur Respir J. 2015;46(59):OA1763.
Salam MT, Wenten M, Gilliland FD. Endogenous sex steroid hormones and asthma and wheeze in young women. J allergy Clin Immunol. 2006;117(5):100–7.
Troisi RJ, Speizer FE, Willett WC, et al. Menopause, postmenopausal estrogen preparations and the risk of adult-onset asthma. A prospective cohort study. Am J Crit Care Med. 1995;152(4):1183–8.
Nahm D-H, Lee K-H, Shin J-Y, et al. Identification of α-enolase as an autoantigen associated with severe asthma. J Allergy Clin Immunol. 2006;118(2):376–81.
Nahm D-H, Lee Y-E, Yim E-J, et al. Identification of cytokeratin 18 as a bronchial epithelial autoantigen associated with nonallergic asthma. Am J Respir Crit Care Med. 2002;165(11):1536–9.
Hizawa N, Yamaguchi E, Konno S, et al. A functional polymorphism in the RANTES gene promoter is associated with the development of late-onset asthma. Am J Resp Crit Care Med. 2002;166(5):686–90.
Taniguchi N, Konno S, Hattori T, et al. The CC16 A38G polymorphism is associated with asymptomatic airway hyper-responsiveness and development of late-onset asthma. Ann Allergy Asthma Immunol. 2013;111(5):376–81.
Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med. 2012;18(5):716–25.
Coleman JM, Naik C, Holguin F, et al. Epithelial eotaxin-2 and eotaxin-3 expression: relation to asthma severity, luminal eosinophilia and age of onset. Thorax. 2012;201634:1–6.
Labrador-Horillo M, Ramentol M, Martinez-Valle F, et al. Eotaxin is overexpressed in Churg-Strauss syndrome compared to allergic asthma. Ann Rheum Dis. 2013;72:A800.
Schwartz LB, Delgado L, Craig T, et al. Exercise-induced hypersensitivity syndromes in recreational and competitive athletes: a PRACTALL consensus report (what the general practitioner should know about sports and allergy). Allergy. 2008;63(8):953–61.
Karjalainen EM, Laitinen A, Sue-Chu M, et al. Evidence of airway inflammation and remodelling in ski athletes with and without bronchial hyperresponsiveness to methacholine. Am J Respir Crit Care Med. 2000;161:2086–91.
Carlsen KH. Mechanism of asthma development in elite athletes. Breathe. 2012;8(4):279–84.
Carlsen KH, Anderson SD, Bjermer L, et al. Exercise-induced asthma, respiratory and allergic disorders in elite athletes: epidemiology, mechanisms and diagnosis: part 1 of the report from the joint task force of the European Respiratory Society (ERS) and the European Academy of Allergy and Clinical Immunology (EAACI) in cooperation with GA2LEN. Allergy. 2008;63(4):387–403.
Hallstrand TS, Moody MW, Wurfel MM, et al. Inflammatory basis of exercise-induced bronchoconstriction. Am J Respir Crit Care Med. 2005;172(6):679–86.
Bougault V, Turmel J, St-Laurent J, et al. Asthma, airway inflammation and epithelial damage in swimmers and cold air athletes. Eur Respir J. 2009;33:740–6.
Chimenti L, Morici G, Paternò A, et al. Bronchial epithelial damage after a half-marathon in nonasthmatic amateur runners. Am J Physiol Lung C. 2010;298(6):L857–62.
Carlsen KH. Sports in extreme conditions: the impact of exercise in cold temperatures on asthma and bronchial hyper-responsiveness in athletes. Brit J Sport Med. 2012;46:796–9.
Pelaia G, Vatrella A, Busceti MT, et al. Cellular mechanisms underlying eosinophilic and neutrophilic airway inflammation in asthma. Mediat Inflamm. 2015;879783:1–8.
Polosa R, Thomson NC. Smoking and asthma: dangerous liaisons. Eur Respir J. 2013;41:716–26.
Newcomb DC, Stokes-Peebles R Jr. Th17-mediated inflammation in asthma. Curr Opin Immunol. 2013;25(6):1–12.
Al-ramil W, Préfontaine D, Chouiali F, et al. Th17-associated cytokines (IL-17A and IL-17F) in severe asthma. J Allergy Clin Immunol. 2009;123(5):1185–7.
Yang XO, Chang SH, Park H, et al. Regulation of inflammatory responses by IL-17F. J Exp Med. 2008;205(5):1063–75.
Hoskins A, Reiss S, Wu P, et al. Asthmatic airway neutrophilia after allergen challenge is associated with the glutathione S-transferase M1 genotype. Am J Resp Crit Care Med. 2013;187(1):34–41.
Kawaguchi M, Takahashi D, Hizawa N, et al. IL-17F sequence variant (HI161Arg) is associated with protection against asthma and antagonizes wild-type IL-17F activity. J Allergy Clin Immunol. 2006;117(4):795–801.
Desai D, Gupta S, Siddiqui S, et al. Sputum mediator profiling and relationship to airway wall geometry imaging in severe asthma. Resp Res. 2013;14(17):1–13.
Simpson JL, Powell H, Boyle MJ, et al. Clarithromycin targets neutrophilic airway inflammation in refractory asthma. Am J Respir Crit Care Med. 2008;177(2):148–55.
Nair P, Gaga M, Zervas E, et al. Safety and efficacy of a CXCR2 antagonist in patients with severe asthma and sputum neutrophils: a randomised placebo-controlled clinical trial. Clin Exp Allergy. 2012;42(7):1097–103.
Bruijnzeel PLB, Uddin M, Koenderman L. Targeting neutrophilic inflammation in severe neutrophilic asthma: can we target the disease-relevant neutrophil phenotype? J Leukocyte Biol. 2015;98(4):549–56.
Meyer N, Dallinga JW, Nuss S, et al. Defining adult asthma endotypes by clinical features and patterns of volatile organic compounds in exhaled air. Resp Res. 2014;15:136.
Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Resp Crit Care Med. 2010;181(4):315–23.
Moore WC, Li X, Li H, et al. Clinical cluster phenotypes from the Severe Asthma Research Program (SARP1/2): reproducibility in SARP 3 and the importance of baseline lung function in disease stability and progression. Am J Respir Crit Care Med. 2016;193:A7852.
Wu W, Bleecker ER, Meyers DA, et al. Differential response to systemic corticosteroids as assessed by cluster analysis of data from the Severe Asthma Research Program (SARP). Am J Respir Crit Care Med. 2017;195:A1362.
Haldar P, Pavord ID, Shaw DE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. 2008;178:218–24.
Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Car Med. 2010;181:315–23.
Hastie A, Mauger D, Denlinger LC, et al. Sputum and blood eosinophil and neutrophil associations with a more severe asthma phenotype in the NHLBI Severe Asthma Research Program (SARP). Am J Respir Crit Care Med. 2017;195:A4695.
Schatz M, Hsu JWY, Zeiger RS. Phenotypes determined by cluster analysis in severe or difficult-to-treat asthma. J Allergy Clin Immunol. 2014;133:1549–56.
Ortega H, Li H, Suruki R. Cluster analysis and characterisation of response to mepolizumab: a step closer to personalised medicine for patients with severe asthma. Ann Am Thorac Soc. 2014;11(7):1011–7.
Thien F. Measuring and imaging small airways dysfunction in asthma. Asia Pac Allergy. 2013;3(4):224–30.
Zhang WJ, Niven RM, Young SS, et al. Dynamic oxygen-enhanced magnetic resonance imaging of the lung in asthma—initial experience. Eur J Radiol. 2015;84:318–26.
Aysola R, de Lange EE, Castro M, et al. Demonstration of the heterogeneous distribution of asthma in the lungs using CT and hyperpolarized helium-3 MRI. J Magn Reson Imaging. 2010;32(6):1379–87.
Thomen RP, Sheshadri A, Quirk JD, et al. Regional ventilation changes in severe asthma after bronchial thermoplasty with 3He MR imaging and CT. Radiology. 2015;274(1):250–9.
NHS England. Service specification: specialised respiratory services (adult)—severe asthma. https://www.engage.england.nhs.uk/consultation/clinical-commissioning-wave4/user_uploads/drft-severe-asthma-serv-spec.pdf Accessed 13/11/2016.
Little SA, Sproule MW, Cowan MD, et al. High resolution computed tomographic assessment of airway wall thickness in chronic asthma: reproducibility and relationship with lung function and severity. Thorax. 2002;57:247–53.
Menzies D, Holmes L, McCumesky G, et al. Aspergillus sensitization is associated with airflow limitation and bronchiectasis in severe asthma. Allergy. 2011;66(5):679–85.
Laxmanan B, Hogarth DK. Bronchial thermoplasty in asthma: current perspectives. J asthma allergy. 2015;8:39–49.
Jung JW, Kwon JW, Kim TW, et al. New insight into the assessment of asthma using xenon ventilation computed tomography. Ann Allergy Asthma Immunol. 2013;111(2):90–5.
Oostveen E, MacLeod D, Lorino H, et al. The forced oscillation technique in clinical practice: methodology, recommendations and future development. Eur Resp J. 2003;22:1026–41.
McLaughlin RA, Noble PB, Sampson DD. Optical coherence tomography in respiratory science and medicine: from airways to alveoli. Physiology. 2014;29(5):369–80.
Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet. 2002;360(9347):1715–21.
Brightling CE, Green RH, Pavord ID. Biomarkers predicting response to corticosteroid therapy in asthma. Treatments Respir Med. 2005;4(5):309–16.
Korevaar DA, Westerhof GA, Wang J, et al. Diagnostic accuracy of minimally invasive markers for detection of airway eosinophilia in asthma: a systematic review and meta-analysis. Lancet Resp Med. 2015;3(4):290–300.
Powell C, Milan SJ, Dwan K, et al. Mepolizumab versus placebo for asthma. Cochrane DB Syst Rev. 2015;27(7):CD010834.
Bousquet J, Rabe K, Humbert M, et al. Predicting and evaluating response to omalizumab in patients with severe allergic asthma. Respir Med. 2007;101(7):1483–92.
Corren J, Lemanske RF, Hanania NA, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365(12):1088–98.
Chiappori A, De Ferrari L, Folli C, et al. Biomarkers and severe asthma: a critical appraisal. Clin Mol Allergy. 2015;13(20):1–11.
Gemicioglu B, Musellim B, Dogan I, et al. Fractional exhaled nitric oxide (FeNo) in different asthma phenotypes. Allergy Rhinol. 2014;5:e157–61.
Hanania NA, Wenzel S, Resén K, et al. Exploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA study. Am J Resp Crit Care Med. 2013;187(8):804–11.
Hanania NA, Korenblat P, Chapman KR, et al. Efficacy and safety of lebrikizumab in patients with uncontrolled asthma (LAVOLTA I and LAVOLTA II): replicate, phase 3, randomised double-blind, placebo-controlled trials. Lancet Respir Med. 2016;4(10):781–96.
Vijverberg SJH, Hilvering B, Raaijmakers JAM, et al. Clinical utility of asthma biomarkers: from bench to bedside. Biol: Targets Ther. 2013;7:199–210.
Wang W, Li Y, Lv Z, et al. The Th2 cell-promoting cytokines IL-33 and TSLP, but not IL-25 are potential biomarkers for endotypes of asthma. Chest. 2016;149(4S):A34.
Miligkos M, Bannuru RR, Alkofide H, et al. Leukotriene-receptor antagonists versus placebo in the treatment of asthma in adults and adolescents: a systematic review and meta-analysis. Ann Intern Med. 2015;163(10):756–67.
Mastalerz L, Nizankowska E, Sanak M, et al. Clinical and genetic features underlying the response of patients with bronchial asthma to treatment with a leukotriene receptor antagonist. Eur J Clin Investig. 2002;32(12):949–55.
Kane B, Fowler SJ, Niven RM. Refractory asthma—beyond step 5, the role of new and emerging adjuvant therapies. Chronic Resp Dis. 2015;12(1):69–77.
Kew KM, Undela K, Kotortsi I, et al. Macrolides for chronic asthma (review). Cochrane DB Syst Rev. 2015;9:CD002997.
Gibson PG, Yang IA, Upham JW, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial. Lancet. 2017; In press. https://doi.org/10.1016/S0140-6736(17)31281-3.
Deeks ED. Mepolizumab: a review in eosinophilic asthma. Biodrugs. 2016;30(4):361–70.
Wenzel SE, Barnes PJ, Bleecker ER, et al. A randomized, double-blind, placebo-controlled study of tumor necrosis factor-α blockage in severe persistent asthma. Am J Resp Crit Care Med. 2009;179(7):549–58.
Bice JB, Leechawengwongs E, Montanaro A, et al. Biologic targeted therapy in asthma. Ann Allergy Asthma Immunol. 2014;112:108–15.
Slager RE, Otulana BA, Hawkins GA, et al. IL-4 receptor polymorphisms predict reduction in asthma exacerbations during response to an anti-IL-4 receptor α antagonist. J Allergy Clin Immunol. 2012;130(2):516–22.
Gauvreau GM, O’Byrne PM, Boulet LP, et al. Effects of an Anti-TSLP antibody on allergen-induced asthmatic response. N Engl J Med. 2014;370:2102–10.
Pretolani M, Bergqvist A, Thabut G, et al. Effectiveness of bronchial thermoplasty in patients with severe refractory asthma: clinical and histopathological correlations. J Allergy Clin Immunol. 2016. doi:10.1016/j.jaci.2016.08.009.
Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Clin Immunol. 2013;132(6):1295–302.
Taylor DR, Bateman ED, Boulet LP, et al. A new perspective on concepts of asthma severity and control. Eur Respir J. 2008;32(3):545–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for preparation of this manuscript.
Conflicts of interest
Katrina Dean reports no conflicts of interest. Robert Niven has received honorarium for speaker fees from AstraZeneca, Boehringer Ingelheim, Booston Scientific, Novartis, Napp, Teva and honorarium for advisory boards from AstraZeneca, Boehringer Ingelheim, Booston Scientific, Novartis, Teva and Vectura. RN has received support to attend international meetings from AstraZeneca, Boehringer Ingelheim, Cheisi and Novartis.
Rights and permissions
About this article
Cite this article
Dean, K., Niven, R. Asthma Phenotypes and Endotypes: Implications for Personalised Therapy. BioDrugs 31, 393–408 (2017). https://doi.org/10.1007/s40259-017-0242-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-017-0242-5