Abstract
Introduction
By inhibiting apolipoprotein B (ApoB) synthesis, mipomersen can significantly reduce ApoB-containing lipoproteins in hypercholesterolemic patients.
Objective
This study sought to ascertain both the extent to which mipomersen can decrease ApoB-containing lipoproteins and the safety of mipomersen therapy.
Methods
Studies were identified through PubMed, CENTRAL, Embase, Clinical Trials, reviews, and reference lists of relevant papers. The efficacy endpoints were the changes in low-density lipoprotein cholesterol (LDL-C), non-high-density lipoprotein cholesterol (non-HDL-C), ApoB, and lipoprotein (a) [Lp(a)]. The safety endpoints were the incidence of injection-site reactions, flu-like symptoms, and elevated transaminases.
Results
Six randomized controlled trials with 444 patients were included in the analysis. Compared with the placebo group, patients who received mipomersen therapy had a significant reduction in LDL-C (33.13 %), as well as a reduction in non-HDL-C (31.70 %), ApoB (33.27 %), and LP(a) (26.34 %). Mipomersen therapy was also associated with an obvious increase in injection-site reactions with an odds ratio (OR) of 14.15, flu-like symptoms with an OR of 2.07, and alanine aminotransferase levels ≥3 × the upper limit of normal with an OR of 11.21.
Conclusions
Mipomersen therapy is effective for lowering ApoB-containing lipoproteins in patients with severe hypercholesterolemia. Future studies exploring how to minimize side effects of mipomersen therapy are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mipomersen is a novel option for patients with hypercholesterolemia. |
Our analysis confirms the efficacy and safety of mipomersen therapy. |
1 Introduction
Low-density lipoprotein cholesterol (LDL-C) is crucial in the pathogenesis of coronary heart disease and thus is the primary target of lipid-lowering therapy [1, 2]. Although the 2013 American College of Cardiology/American Heart Association (ACC/AHA) lipid guideline abolishes the target of LDL-C, it still supports lowering LDL-C levels, especially in high-risk patients [3]. However, conventional lipid-lowering therapies such as statins often result in insufficient LDL-C reduction, even when administered at maximally tolerated doses [4]. Patients in whom statins are often inadequate can be classified into four groups: (1) patients with homozygous familial hypercholesterolemia (HoFH); (2) those with heterozygous familial hypercholesterolemia (HeFH); (3) patients with severe hypercholesterolemia; and (4) those who are statin intolerant. Thus, novel approaches for lipid lowering are needed.
Apolipoprotein B (ApoB), which is produced in the liver, is an essential component of LDL-C and all other atherogenic lipoproteins [5, 6]. Studies have indicated that ApoB synthesis inhibition may be an attractive therapeutic strategy to achieve target levels for LDL-C in subjects with hypercholesterolemia [7]. Mipomersen is a second-generation antisense oligonucleotide and specifically binds to ApoB messenger RNA (mRNA), then blocks the translation of the gene product [8–10]. Previous studies have demonstrated that mipomersen can significantly reduce LDL-C and ApoB levels in patients with hypercholesterolemia [10–13]. Moreover, mipomersen was recently approved by the US FDA for the treatment of HoFH [14]. However, mipomersen was not approved by the European Medicines Agency due to findings of fat build-up in the liver and increased enzyme levels [15].
To the best of our knowledge, no study has yet comprehensively and quantitatively evaluated the efficacy and safety of mipomersen therapy. In fact, it is crucial to summarize the previous work and provide guidance for our clinical work. Accordingly, we performed a meta-analysis of available randomized controlled trial (RCT) data.
2 Methods
2.1 Search Strategy
The review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We systematically searched (November 2013) the PubMed, CENTRAL, Embase, and Clinical Trials databases using the keywords ‘(mipomersen OR kynamro OR ISIS 301012 OR ISIS301012 OR ISIS-301012) AND clinical trial’ without language or time limitations. We also checked conference proceedings, reference lists of identified articles, previous meta-analyses, and original studies identified by the electronic search to find other potentially eligible studies.
2.2 Study Selection
Inclusion criteria for this meta-analysis were (1) RCTs; (2) prospective comparison of mipomersen therapy versus placebo in patients with hypercholesterolemia; and (3) administration of mipomersen at 200 mg/week.
Exclusion criteria were (1) irretrievable or unclear data; (2) lack of control group; (3) ongoing or unpublished studies; and (4) duplicate reports. If two articles reported results of the same study, the article with more complete data was included.
2.3 Risk of Bias Assessment
To assess the risk of bias in included studies, we followed the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0), and its recommended “risk of bias” assessment tool for RCTs [16]. Each study was examined according to the following items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. The judgements were expressed simply as ‘low risk,’ ‘high risk,’ or ‘unclear risk’ of bias.
2.4 Data Extraction
Study features extracted included study design, the dose of mipomersen, treatment duration, and participant characteristics. The efficacy endpoints were the changes in LDL-C, non-high-density lipoprotein cholesterol (non-HDL-C), ApoB, and lipoprotein (a) [Lp(a)] from baseline to the primary efficacy time point. The safety endpoints were the incidence of adverse events (AEs) (i.e., injection-site reactions, flu-like symptoms, elevated transaminases) evaluated during on-treatment periods. Moreover, we analyzed the discontinuation of therapy. All of the outcomes analyzed were used as defined in individual trials.
Study search, selection, appraisal, and abstraction were all performed by two independent reviewers, with disparities resolved by discussion.
2.5 Statistical Analysis
Continuous variables were presented as weighted mean difference (WMD) and 95 % confidence interval (CI), and binary outcomes as odds ratio (OR) and 95 % CI. The outcomes from individual studies were combined with the fixed-effect model first; if heterogeneity existed, then the random-effect model was used. Heterogeneity of effects was assessed with Chi-squared tests and I 2; an I 2 > 50 % was considered to indicate significant heterogeneity between the trials [17]. Sensitivity analyses were conducted to evaluate the robustness of our results by removing each study in turn and recalculating the pooled effect. Publication bias was assessed with the fail-safe number (N fs) but not the funnel plot because the number of included studies was small. Any calculated N fs value smaller than the number of retrieved studies indicated publication bias. The N fs0.05 was calculated as N fs0.05 = (ΣZ/1.64)2 − k, where k was the number of studies included in the meta-analysis. Statistical analyses were performed with Review Manager 5.0 (The Cochrane Collaboration, Copenhagen, Denmark). A two-sided p-value <0.05 was considered to be statistically significant.
3 Results
3.1 Search Results
From the initial 108 hits, 92 citations were initially excluded at the title/abstract level (Fig. 1). Among the articles retrieved in completed form, the following were excluded: one (lack of control group), one (investigated a different endpoint), one (duplicate report), three (ongoing studies), and four (mipomersen dose-escalation studies) [10–13]. Eventually, six trials with 444 patients were included in the analysis [18–23].
3.2 Study Characteristics
The main features of the included studies are shown in Table 1. All studies were published over the period 2010–2013. Study size ranged from 21 to 157 patients. All studies were designed with subcutaneous administration of placebo or mipomersen 200 mg weekly for 26 weeks, except the study by Visser et al. [19], which was for 13 weeks. Patients had familial hypercholesterolemia or severe hypercholesterolemia, and were already receiving maximally tolerated lipid-lowering therapy, stable lipid-lowering therapy, or were not receiving statin therapy because of statin intolerance.
Patient characteristics are detailed in Table 2, and baseline lipid parameters are summarized in Table 3. Mean age ranged from 30 to 59 years with baseline body mass index (BMI) greater than 25 kg/m2. The percentage of male patients, White patients, and patients with metabolic syndrome was 27–68 %, 77–98 %, and 6–77 %, respectively. All patients had hypercholesterolemia.
3.3 Risk of Bias in Included Studies
The assessment of risk of bias in the included studies is illustrated in Table 4. Overall, the risk of bias was generally low. All studies were randomized, double-blind, placebo-controlled trials. Detailed randomization and concealment procedures were only reported in the studies by Raal et al. [18] and Visser et al. [19].
Blinding was performed relatively well in all studies. All randomized patients were included in the studies. All outcomes mentioned in Sect. 2 were reported in Sect. 3, so selective reporting was of unclear risk of bias. Other bias was also of unclear risk because of insufficient information reported.
3.4 Efficacy of Mipomersen Therapy
The data for mean percentage change in LDL-C was pooled from six trials. The average reductions from baseline were significantly higher in the mipomersen group than in the placebo group, with a clinically and statistically significant difference of 33.13 % (95 % CI −40.85 to −25.42; p < 0.05; I 2 = 67 %) (Fig. 2a). In addition, concordant reductions were found in non-HDL-C (WMD −31.70 %; 95 % CI −39.04 to −24.36; p < 0.05; I 2 = 68 %) (Fig. 2b), ApoB (WMD −33.27 %; 95 % CI −39.03 to −27.51; p < 0.05; I 2 = 56 %) (Fig. 2c) and LP(a) (WMD −26.34 %; 95 % CI −31.65 to −21.03; p < 0.05; I 2 = 0 %) (Fig. 2d).
Impact of mipomersen therapy on apolipoprotein B-containing lipoproteins. Forest plots show the significantly beneficial impact of mipomersen therapy on a low-density lipoprotein cholesterol, b non-high-density lipoprotein cholesterol, c apolipoprotein B, and d lipoprotein (a). CI confidence interval, IV inverse variance, SD standard deviation
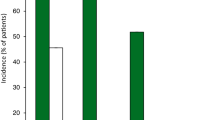
3.5 Safety of Mipomersen Therapy
For the safety endpoints, the incidence of injection-site reactions in the mipomersen group was 76–100 %, which was significantly higher than that in the placebo group, with an OR of 14.15 (95 % CI 8.67–23.11; p < 0.05; I 2 = 0 %) (Fig. 3a). As the second most common AE, the incidence of flu-like symptoms was 29–70 % in the mipomersen group, with an OR of 2.07 (95 % CI 1.34–3.19; p < 0.05; I 2 = 0 %) to the placebo group (Fig. 3b). In addition, alanine aminotransferase (ALT) levels ≥3 × the upper limit of normal (ULN) occurred in more patients treated with mipomersen than placebo by about tenfold (OR 11.21; 95 % CI 3.43–36.68; p < 0.05; I 2 = 0 %) (Fig. 3c).
Impact of mipomersen therapy on adverse events. Forest plots show the significantly increased incidence of adverse events of mipomersen therapy, such as a injection-site reactions, b flu-like symptoms, and c alanine aminotransferase levels ≥3 × the upper limit of normal. CI confidence interval, M–H Mantel–Haenszel
3.6 Discontinuation of Mipomersen Therapy
As shown in Fig. 4, more patients discontinued therapy in the mipomersen group than in the placebo group, with an OR of 4.76 (95 % CI 2.17–7.99; p < 0.05; I 2 = 0 %). Moreover, most of the discontinuations were caused by AEs and/or serious AEs (SAEs), and the incidence ranged from 11 to 25 %, with an OR of 6.33 (95 % CI 2.45–16.33; p < 0.05; I 2 = 0 %) to the placebo group.
3.7 Sensitivity Analysis and Publication Bias Assessment
Sensitivity analysis by removing one study at a time confirmed the results from the overall analysis both in direction and in magnitude of statistical significance (all p values <0.05, data not shown). The N fs0.05 for each comparison was calculated and the values for LDL-C (N fs0.05 = 435.96), non-HDL-C (N fs0.05 = 452.35), ApoB (N fs0.05 = 580.33), LP(a) (N fs0.05 = 167.61), and injection-site reactions (N fs0.05 = 193.35) were found to be much greater than the number of studies included in the meta-analysis. The values for flu-like symptoms (N fs0.05 = 20.12), ALT (N fs0.05 = 44.74), discontinuation (N fs0.05 = 29.91), and AE/SAE-induced discontinuation (N fs0.05 = 26.58) were relatively small, but still much greater than the number of retrieved studies.
4 Discussion
The main findings of the present study indicate that subcutaneous mipomersen 200 mg/week significantly lowers LDL-C, non-HDL-C, ApoB and Lp(a) levels. In addition, analysis of safety endpoints demonstrates that mipomersen increases the incidence of AEs, such as injection-site reactions, flu-like symptoms, and elevated liver transaminases.
European Society of Cardiology (ESC) guidelines recommend that the treatment target for patients with very high cardiovascular risk is LDL-C <70 mg/dL or a ≥50 % reduction from baseline, and for subjects at high cardiovascular risk the target is <100 mg/dL [24]. A meta-analysis of statin trials suggest that for each 1 mmol/L reduction in LDL-C, there is a corresponding 22 % reduction in cardiovascular disease mortality and morbidity, and a 10 % reduction in all cause mortality [25]. However, a substantial proportion of patients remain unable to achieve an optimal LDL-C concentration despite maximally tolerated lipid-lowering therapy [26–28]. Moreover, the number of statin-intolerant patients is rising, which is manifested by the use of higher statin doses to achieve more stringent LDL-C targets [1, 29]. One main reason may be that higher-dose statins are more likely to cause side effects; as physicians are using higher doses of statins, more patients are developing intolerance to statins.
Rather than LDL-C or non-HDL-C targets, the 2013 ACC/AHA lipid guideline uses the intensity of statin therapy as the goal of treatment. High-intensity statin therapy on average lowers LDL-C by approximately ≥50 %, moderate-intensity statin therapy lowers LDL-C by approximately 30 to <50 %, and lower-intensity statin therapy lowers LDL-C by <30 %. When clinicians treat high-risk patients who have a less-than-anticipated response to statins, who are unable to tolerate a less-than-recommended intensity of a statin, or who are completely statin intolerant, they may consider the addition of a non-statin cholesterol-lowering therapy [3]. For example, patients with HoFH and HeFH have life-long elevations of LDL-C, which places them at very high risk for future heart disease. Therefore, in these patients, it is appropriate to very aggressively target their LDL-C; simply utilizing maximum doses of statins is not enough [30]. Furthermore, mipomersen is a promising lipid-lowering drug to further lower LDL-C levels in combination with statins or not.
Several novel therapeutic strategies to lower LDL-C have been developed. These include inhibitors of PCSK9, microsomal triglyceride transfer protein, and cholesteryl ester transfer protein, as well as mipomersen, the focus of this meta-analysis [30]. Mipomersen represents a first-in-class injectable antisense therapy. Given its half-life of approximately 31 days, mipomersen was administered once weekly for 26 weeks to achieve a steady state level [10]. Mipomersen significantly decreased LDL-C level in hyperlipidemic patients regardless of etiology. But it is still unknown whether and to what extent mipomersen can decrease LDL-C in patients treated with regular apheresis, and an ongoing trial will answer the question (Clinicaltrials.gov: NCT01598948).
More importantly, obvious reductions in other atherogenic lipoproteins can be seen, especially in non-HDL-C, ApoB, and Lp(a). In contrast, other commonly used LDL-C-reducing agents, such as statins, ezetimibe, and bile acid sequestrants, decrease the levels of ApoB and Lp(a) less significantly than LDL-C [28, 31–33]. Moreover, these agents have virtually no impact on Lp(a) [34]. In fact, ApoB and other ApoB-containing lipoproteins, such as non-HDL-C and Lp(a), are independent risk factors for cardiovascular disease [35–39] and are also the targets of lipid-lowering therapy [24]. Therefore, mipomersen is expected to provide additional cardiac benefit in hypercholesterolemic patients. In fact, no study has yet evaluated cardiovascular outcomes in mipomersen therapy patients. It is the direction of our future study. We need studies to ascertain whether mipomersen can reduce cardiovascular events.
Mipomersen produced significant lipid-lowering effects in hypercholesterolemic subjects. Further, if future studies continue to show such promising efficacy results, mipomersen would likely be a viable additional lipid-lowering therapy for patients who are intolerant to statins, and/or not at target lipid levels despite maximum doses of current lipid-lowering therapy.
In terms of safety, mipomersen may lead to many AEs, such as injection-site reactions, flu-like symptoms, liver toxicity, and so on. While none of these AEs is life threatening, they can lead to discontinuation of therapy. We found that the proportion of discontinuations caused by AEs/SAEs can be as high as 25 %. A randomized, double-blind, placebo-controlled, clinical trial (Clinicaltrials.gov: NCT01475825) is exploring lower, more frequent dosing as a means to minimize the incidence of AEs. Meanwhile, an open-label extension trial (Clinicaltrials.gov: NCT00694109) to evaluate the long-term safety of mipomersen is ongoing.
So far as we know, this is the first systematic and comprehensive meta-analysis to evaluate the efficacy and safety of mipomersen therapy. However, there are three major limitations of our study. First, the studies are divergent, so the conclusions are relatively less reliable. Second, the sample size was small. Third, the follow-up duration was short, so it is hard to predict outcomes in the long run.
5 Conclusion
These efficacy and safety results indicate that mipomersen can be used as an adjunctive agent to lower LDL-C concentrations in patients with severe hypercholesterolemia not adequately controlled on currently available lipid-lowering medications. Further well-designed studies with larger sample sizes and longer follow-ups are needed to elucidate the long-term safety and efficacy of mipomersen.
References
Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–39.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486–97.
Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013. doi:10.1016/j.jacc.2013.11.002. (Epub ahead of print).
Grigore L, Norata GD, Catapano AL. Combination therapy in cholesterol reduction: focus on ezetimibe and statins. Vasc Health Risk Manag. 2008;4:267–78.
Davidson NO, Shelness GS. APOLIPOPROTEIN B: mRNA editing, lipoprotein assembly, and presecretory degradation. Annu Rev Nutr. 2000;20:169–93.
Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture P, et al. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med. 2006;259:247–58.
Gaffney D, Forster L, Caslake MJ, Bedford D, Stewart JP, Stewart G, et al. Comparison of apolipoprotein B metabolism in familial defective apolipoprotein B and heterogeneous familial hypercholesterolemia. Atherosclerosis. 2002;162:33–43.
Toth PP. Antisense therapy and emerging applications for the management of dyslipidemia. J Clin Lipidol. 2011;5:441–9.
Yu RZ, Kim TW, Hong A, Watanabe TA, Gaus HJ, Geary RS. Cross-species pharmacokinetic comparison from mouse to man of a second-generation antisense oligonucleotide, ISIS 301012, targeting human apolipoprotein B-100. Drug Metab Dispos. 2007;35:460–8.
Kastelein JJ, Wedel MK, Baker BF, Su J, Bradley JD, Yu RZ, et al. Potent reduction of apolipoprotein B and low-density lipoprotein cholesterol by short-term administration of an antisense inhibitor of apolipoprotein B. Circulation. 2006;114:1729–35.
Akdim F, Visser ME, Tribble DL, Baker BF, Stroes ES, Yu R, et al. Effect of mipomersen, an apolipoprotein B synthesis inhibitor, on low-density lipoprotein cholesterol in patients with familial hypercholesterolemia. Am J Cardiol. 2010;105:1413–9.
Akdim F, Tribble DL, Flaim JD, Yu R, Su J, Geary RS, et al. Efficacy of apolipoprotein B synthesis inhibition in subjects with mild-to-moderate hyperlipidaemia. Eur Heart J. 2011;32:2650–9.
Akdim F, Stroes ES, Sijbrands EJ, Tribble DL, Trip MD, Jukema JW, et al. Efficacy and safety of mipomersen, an antisense inhibitor of apolipoprotein B, in hypercholesterolemic subjects receiving stable statin therapy. J Am Coll Cardiol. 2010;55:1611–8.
FDA Briefing Document, NDA 203568. Mipomersen sodium injection 200 mg/mL. Materials for the endocrinologic and metabolic drugs advisory committee meeting, 18 October 2012. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/EndocrinologicandMetabolicDrugsAdvisoryCommittee/UCM323927.pdf. Accessed 15 Nov 2013.
Genzyme and Isis provide update on CHMP opinion on KYNAMRO™ (mipomersen). Press release, Genyzme and Isis Pharmaceuticals. http://en.sanofi.com/Images/31557_20121214_KYNAMRO_en.pdf. Accessed 15 Nov 2013.
Rodriguez JA, Grau A, Eguinoa E, Nespereira B, Perez-Ilzarbe M, Arias R, et al. Dietary supplementation with vitamins C and E prevents downregulation of endothelial NOS expression in hypercholesterolemia in vivo and in vitro. Atherosclerosis. 2002;165:33–40.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Raal FJ, Santos RD, Blom DJ, Marais AD, Charng MJ, Cromwell WC, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, for lowering of LDL cholesterol concentrations in patients with homozygous familial hypercholesterolaemia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375:998–1006.
Visser ME, Akdim F, Tribble DL, Nederveen AJ, Kwoh TJ, Kastelein JJ, et al. Effect of apolipoprotein-B synthesis inhibition on liver triglyceride content in patients with familial hypercholesterolemia. J Lipid Res. 2010;51:1057–62.
Stein EA, Dufour R, Gagne C, Gaudet D, East C, Donovan JM, et al. Apolipoprotein B synthesis inhibition with mipomersen in heterozygous familial hypercholesterolemia: results of a randomized, double-blind, placebo-controlled trial to assess efficacy and safety as add-on therapy in patients with coronary artery disease. Circulation. 2012;126:2283–92.
McGowan MP, Tardif JC, Ceska R, Burgess LJ, Soran H, Gouni-Berthold I, et al. Randomized, placebo-controlled trial of mipomersen in patients with severe hypercholesterolemia receiving maximally tolerated lipid-lowering therapy. PLoS One. 2012;7:e49006.
Visser ME, Wagener G, Baker BF, Geary RS, Donovan JM, Beuers UH, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, lowers low-density lipoprotein cholesterol in high-risk statin-intolerant patients: a randomized, double-blind, placebo-controlled trial. Eur Heart J. 2012;33:1142–9.
Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, Davidson M. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol. 2013;62:2178–84.
Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, et al. ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769–818.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Davidson MH, Maki KC, Pearson TA, Pasternak RC, Deedwania PC, McKenney JM, et al. Results of the National Cholesterol Education (NCEP) Program Evaluation ProjecT Utilizing Novel E-Technology (NEPTUNE) II survey and implications for treatment under the recent NCEP Writing Group recommendations. Am J Cardiol. 2005;96:556–63.
Marks D, Thorogood M, Neil HA, Humphries SE. A review on the diagnosis, natural history, and treatment of familial hypercholesterolaemia. Atherosclerosis. 2003;168:1–14.
Stein E, Stender S, Mata P, Sager P, Ponsonnet D, Melani L, et al. Achieving lipoprotein goals in patients at high risk with severe hypercholesterolemia: efficacy and safety of ezetimibe co-administered with atorvastatin. Am Heart J. 2004;148:447–55.
Armitage J, Bowman L, Wallendszus K, Bulbulia R, Rahimi K, Haynes R, et al. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet. 2010;376:1658–69.
Bell DA, Hooper AJ, Watts GF, Burnett JR. Mipomersen and other therapies for the treatment of severe familial hypercholesterolemia. Vasc Health Risk Manag. 2012;8:651–9.
Stein EA, Ose L, Retterstol K, Tonstad S, Schleman M, Harris S, et al. Further reduction of low-density lipoprotein cholesterol and C-reactive protein with the addition of ezetimibe to maximum-dose rosuvastatin in patients with severe hypercholesterolemia. J Clin Lipidol. 2007;1:280–6.
Bays HE, Conard SE, Leiter LA, Bird SR, Lowe RS, Tershakovec AM. Influence of age, gender, and race on the efficacy of adding ezetimibe to atorvastatin vs. atorvastatin up-titration in patients at moderately high or high risk for coronary heart disease. Int J Cardiol. 2011;153:141–7.
Ballantyne CM, Raichlen JS, Cain VA. Statin therapy alters the relationship between apolipoprotein B and low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol targets in high-risk patients: the MERCURY II (measuring effective reductions in cholesterol using rosuvastatin) trial. J Am Coll Cardiol. 2008;52:626–32.
Holmes DT, Schick BA, Humphries KH, Frohlich J. Lipoprotein(a) is an independent risk factor for cardiovascular disease in heterozygous familial hypercholesterolemia. Clin Chem. 2005;51:2067–73.
Sniderman AD, Williams K, Contois JH, Monroe HM, McQueen MJ, de Graaf J, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes. 2011;4:337–45.
Grundy SM. Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Circulation. 2002;106:2526–9.
Nordestgaard BG, Chapman MJ, Ray K, Boren J, Andreotti F, Watts GF, et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J. 2010;31:2844–53.
Bennet A, Di Angelantonio E, Erqou S, Eiriksdottir G, Sigurdsson G, Woodward M, et al. Lipoprotein(a) levels and risk of future coronary heart disease: large-scale prospective data. Arch Intern Med. 2008;168:598–608.
Robinson JG, Wang S, Smith BJ, Jacobson TA. Meta-analysis of the relationship between non-high-density lipoprotein cholesterol reduction and coronary heart disease risk. J Am Coll Cardiol. 2009;53:316–22.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (81000091, 81170129).
Conflict of interest disclosures
None of the authors have any potential conflict of interest that might be relevant to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, N., Li, Q., Tian, XQ. et al. Mipomersen is a Promising Therapy in the Management of Hypercholesterolemia: A Meta-Analysis of Randomized Controlled Trials. Am J Cardiovasc Drugs 14, 367–376 (2014). https://doi.org/10.1007/s40256-014-0077-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-014-0077-0