Abstract
Purpose of Review
Genetic counseling is an increasingly important component of cardiovascular care in the era of precision medicine.
Recent Findings
Over the last 15 years, genetic testing for inherited cardiovascular diseases has exponentially increased and as such increased the need for complex genetic discussions with patients and their family members. Inherited cardiovascular conditions have an inherent risk for sudden cardiac death, and explaining the risks to at-risk family members and discussing the options for genetic testing to identify those truly at risk is an essential component of complete cardiovascular genetics care. Genetic counselors are trained experts who are increasingly filling this role and embracing the complexities that present as genetic technology evolves.
Summary
The incorporation of genetics into clinical cardiovascular care continues to expand, and genetic counselors play an integral role for families and clinicians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is a very exciting time in cardiovascular genetics. Barriers to genetics services are being reduced and the opportunities for using genetic technology in cardiovascular care are increasing.
Heart disease is the number one cause of death in the United States, killing over 370,000 people a year [1]. Heart disease can include coronary artery disease, cardiomyopathy, arrhythmia, aneurysm, and hypertension. Many forms of heart disease have a genetic component. Between the estimated prevalence of hypertrophic cardiomyopathy and familial hypercholesterolemia, up to 1 in 250 individuals are at risk for inherited cardiovascular disease. Most of the familial cardiovascular diseases are inherited in an autosomal dominant fashion. This means that often, multiple family members are affected or at risk for the cardiovascular disease and typically those with an underlying genetic cause tend to have disease onset at an earlier age than what is expected compared to those of non-genetic causes. Obtaining and documenting a detailed (three-generation) family history is a key component to appropriately identifying those at risk for inherited cardiovascular conditions. Genetic counselors are specifically trained in taking and documenting these detailed family histories as well as being afforded more time with the patients to obtain these histories and share them with the cardiologist [2]. For each type of inherited cardiovascular disease, there are key family history questions that should be asked to elicit who is affected, ages of diagnosis, and identification of an underlying disease etiology. For example, clarifying whether a family member’s early onset dilated cardiomyopathy is a result from an ischemic event versus idiopathic significantly changes the risk assessment of a familial idiopathic cardiomyopathy versus possibly a familial hypercholesterolemia with early onset ischemic heart disease.
Genetics of Cardiovascular Disease
Cardiovascular genetic testing is currently available for such inherited conditions as familial hypercholesterolemia, cardiomyopathies (idiopathic dilated cardiomyopathy, hypertrophic cardiomyopathy, left ventricular non-compaction cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy), arrhythmia syndromes (Long QT, Brugada syndrome, CPVT), familial aortopathies (Marfan syndrome and other connective tissue conditions), congenital heart disease, and sudden cardiac arrest (Table 1). Our understanding of the genetics of cardiovascular disease has exponentially increased over the last 15 years. Looking back, 15 years ago researchers had solid evidence for only one gene causing idiopathic dilated cardiomyopathy, whereas now dilated cardiomyopathy is known to have hundreds of genes contributing to disease causation. And the other inherited cardiovascular conditions have had the same increase in numbers of genes that have been identified.
The genes responsible for causing the majority of inherited hypertrophic cardiomyopathy and also a sizeable amount of idiopathic dilated cardiomyopathy code for proteins that make up the sarcomere, which is the basic unit of muscle [3, 4]. Within each sarcomere element are the proteins that allow muscle cells relax and contract, and as such, if one of the proteins is not functioning as a result of a mutation in a sarcomere, then the entire sarcomeric function is compromised, hence leading to hypertrophic or dilated cardiomyopathy. As a secondary feature of some of the inherited cardiomyopathies, significant arrhythmias can still be present despite the gene having an underlying mechanism of affecting the muscle cells of the heart. With regard to hypertrophic cardiomyopathy, there are approximately 18 genes when mutated are known to be responsible for causing the disease. In the case of dilated cardiomyopathy, the field is much more diverse, with more than 40 genes now known to be responsible for causing non-ischemic, non-syndromic DCM. As few of these genes have hallmark presentations when looking at the heart, genetic testing is the only way to identify the underlying etiology of cardiomyopathy. This is one of the primary reasons cardiac genetic testing has moved rapidly toward panel testing which involves testing a large number of genes at a time for one disease.
In contrast to the cardiomyopathies, the inherited arrhythmia syndromes do not have an intrinsic problem with the myofibers of the heart, but instead with the electrical signals transmitting through the heart. The majority of arrhythmia syndromes are due to the incorrect formation of an ion channel within the muscle cells as the result of a gene mutation, allowing the cell’s ions (sodium, potassium) to flow through irregularly [5]. Many of these arrhythmia syndromes confer a significantly increased risk for fatal arrhythmias (5). Similar to the genetics of cardiomyopathies, many mutations in channel genes are responsible for the arrhythmia syndromes. There are some instances where subtle changes on EKG can be identified to give clues as to which channelopathy might be occurring in an individual; however, typically there are non-specific findings, and therefore, an arrhythmia syndrome is suspected but the specific type is clarified through genetic testing.
The familial aortopathies comprise a group of inherited connective tissue conditions. The most common of the inherited connective tissue conditions is Marfan syndrome, caused by a mutation in the FBN1 gene. The prevalence of Marfan syndrome is the highest of the connective tissue conditions, and the genetic testing has the highest detection rate when an affected individual meets the clinical criteria for Marfan syndrome (called the Ghent criteria) [6]. The remaining genes associated with an increased risk for aortic aneurysms and dissections, around 20 genes, are responsible for a much smaller proportion of familial aortopathies [7].
Current Genetic Testing in Cardiovascular Disease
Genetic testing can be ordered by suspected diagnosis with panels ranging from 2 to 40 genes or even larger panels (up to 200 genes). Because of the large number of genes in the current cardiac gene panels, genetic testing is expected to expand toward routine ordering of clinical exome in the near future as the price of sequencing an entire exome rivals the cost of sequencing a large gene panel. The number and type of genes tested is up to the discretion and expertise of the ordering clinician. For example, a young patient who has suffered a cardiac arrest with unknown cause may be tested with an arrhythmia panel or combined arrhythmia and cardiomyopathy panel to evaluate both arrhythmia genes and cardiomyopathy genes where arrhythmias may precede the development of overt heart disease. There is extensive phenotypic and genotypic overlap in many of the cardiovascular genes particularly those that cause inherited cardiomyopathies and arrhythmias. There are a large number of genes on the inherited cardiac panels, and the panels are growing as additional genes are being added as they are discovered.
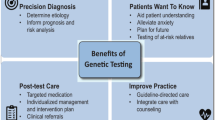
Although clinical genetic testing is not routinely utilized for common multi-factorial conditions such as coronary artery disease and hypertension, individuals with a family history or early age of onset may still benefit from genetic counseling. Genetic counseling can help with prevention recommendations and identification of other individuals at risk in the family. Genetic counselors are trained to explain the benefits, limitations, and risks of genetic testing to individuals and families interested in pursuing genetic testing for risk assessment or diagnosis. Utilizing the information learned from genetic testing and incorporating this knowledge into the patients’ care plan is key to altering medical management based on the genetic results and in some cases using that knowledge to aid with preventative care in cardiology, which is the forefront of precision medicine [8••]. For example, an individual with a mutation in a gene that carries a very high arrhythmia risk can benefit from tailored medical therapy for the arrhythmias in the form of medications or implantable cardioverter defibrillators (ICD), and this could save someone from dying of a life threatening arrhythmia. Genetic counselors are well suited and increasingly filling the role for providing cardiovascular genetic care to meet the rising demand for cardiovascular genetic services [9••]. Beyond recognition by cardiologists, insurers are starting to address the need for genetic counseling in heart disease [10].
Family Follow-up and Care
Identification of a gene mutation that further clarifies a cardiac diagnosis in the initial case is critical but the power of genetics is realized with family follow-up and cascade testing. Recommendations exist for evaluation of family members at risk for inherited heart disease [2, 11••, 12]. One key role for a genetic counselor is taking a three-generation family history, which has importance for pinpointing key family members throughout the family tree who should be clinically and genetically screened. Genetic counselors have been uniquely trained to communicate the importance of getting the genetic information to their at-risk family members and facilitating family member cardiac screening. Cardiology is a key area within the medical profession where there are preventative therapies for some inherited cardiovascular disease, whether it be medications to slow the progression of dilated cardiomyopathy or implantable defibrillators to prevent sudden cardiac death in those at highest risk. The World Health Organization has a goal of eliminating preventable sudden cardiac arrest in children and youth by 2030 [13]. Genetic diagnosis in families will help identify disease in at-risk individuals at an early age and help realize this goal.
New and Expanding Roles for Genomics in Cardiology
Variant Interpretation
The number of genes included on cardiovascular panels has consistently increased since 2004 when multi-gene cardiovascular panels were launched. Along with an increasing number of genes come more data and the need for careful interpretation and appropriate counseling of families and medical providers on the significance of identified variants. Multiple tools exist including ClinGen and ClinVar to help with interpretation of genetic variants from clinical genetic testing. In addition, the graduate level genetic counseling training programs are incorporating training on variant databases such as ClinVar and control databases such as ESP/EVS, 1000 Genomes, as well as assessment of potential variant function such as in silico and Polyphen. A growing number of genetic counselors are now working at genetic testing laboratories to help address the challenges of exponential data growth and frequently updated guidelines present [14]. Therefore, genetic counselors have the appropriate training and background to interpret the data from these larger panels and handle the information available from them. In addition, genetic counselors are able to take more time explaining the meaning of these variants to patients and discuss the next steps to further clarify the variants identified (i.e., testing other family members for segregation).
Data Sharing
In addition to variant interpretation based on existing literature and knowledge, data sharing is key to increasing our future understanding of genetic variants. Public and private databases are expanding both in scope and utility with the goal of improving the process of variant interpretation and genotype/phenotype studies. Data sharing is being encouraged in both clinical and research realms, and as such, in January 2015, the NIH Genomic Data Sharing Policy [15] took effect for NIH funded researchers.
Precision Medicine
Using genetic technology to understand the cause of and guide treatment for cardiovascular disease is key to incorporating precision medicine into clinical practice. Personalized medicine, also referred to as “precision medicine,” is an emerging approach for disease diagnosis and treatment that uses genetic, genomic, and molecular information to guide diagnosis, prognosis, and therapy [8••]. Family history and genetic testing help with not only diagnosis but also gene-specific and mutation-specific risk stratification and management. For example, mutations in some genes versus other genes are known to predispose to high-risk arrhythmias, and as such, more aggressive therapy should be recommended in these cases [11••, 12]. Some gene mutations might be specific to each individual family and with a dearth of published literature in these cases; family history can be a driving factor in risk interpretation. For example, gene mutation plus a family history of sudden cardiac arrest segregating with the mutation could possibly yield a more aggressive therapy in affected family members. Or some inherited aortopathies, such as Loeys Dietz, have a greater risk for aortic dissection at aortic diameter sizes below the current surgical threshold limits and thus could impact timing of surgical intervention [16••]. In addition, as more is learned about genotype/phenotype correlations, there are some genetic variants that could be more amenable to targeted therapies, and such is increasingly evident in clinical trials addressing specific cardiovascular genetic variants [17, 18].
Developing Education and Partnerships
Expanding the care teams for patients with genetic heart disease will help identify affected and at-risk patients. There are many important partners moving forward that can help recognize and refer patients including the public health sector, medical examiners, and Mark Zuckerberg, co-founder of facebook and philanthropist. Cardiovascular disease is a major public health issue. Early identification and treatment will reduce the healthcare burden [19]. Medical examiners play one key role in the public health sector. Premature cardiovascular disease and early sudden death are potential indicators of a genetic susceptibility [20]. Partnerships with the medical examiner community exist [21], but additional education is needed to include genetics [22] so that family members of those who die at a young age and suddenly can gain answers and understanding, but most importantly, families need to be informed so that a sudden death never happens twice in the same family. Genetic counselors are in a unique position to work with the public health sector and medical examiners to provide genetics education for the community. Patient support foundations exist for many of the inherited cardiac conditions. Included in the primary mission of many foundations are public education to raise awareness of these life-threatening conditions and raising funds to help prevent sudden cardiac arrest. Foundations work directly with genetic counselors to help bridge the gap between genetics and the community. In response to Mark Zuckerberg’s question posted to facebook on December 1, 2015 in the Letter to Our Daughter—“Can our generation cure disease so you live much longer and healthier lives?” [23] The answer is yes. There are opportunities to help people live longer healthier lives and help us save the kids and people at risk for inherited heart disease. We need to identify better screening methods, increase identification of people at risk for heart disease, and provide better education and preventative measures.
Future Directions
The spectrum of ion channel conditions covers many disease phenotypes including arrhythmias, cardiomyopathies, and epilepsy. As genetic testing expands beyond disease specific panels to whole exome or whole genome testing, the overlap of gene mutations and in some cases the multiple genetic variants that cause disease will be better understood. Future research into the genetic causes of cardiovascular disease will lead to better comprehension of the underlying disease mechanism and genotype driven therapies, furthering precision medicine.
Conclusions
Incorporating genetics and genetic counseling into cardiovascular care will improve patient management and care. It will also raise the awareness of the risk of cardiovascular disease in relatives and prevent sudden death, leading to longer, healthier lives.
How do I find a Genetic Counselor?
To find a cardiovascular genetic counselor on this map, use the “Find A Genetic Counselor” tool on the National Society of Genetic Counselors website and enter cardiology as the specialty.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Woo D, Yeh RW, Turner MB; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association [published online ahead of print December 16, 2015]. Circulation. doi: 10.1161/CIR.0000000000000350.
Hershberger R, Lindenfeld J, Mestroni L, et al. Genetic evaluation of cardiomyopathy—a Heart Failure Society of America practice guideline. J Card Fail. 2009;15(2):83–97.
Maron, et al. Hypertrophic cardiomyopathy: present and future, with translation into contemporary cardiovascular medicine. J Am Coll Cardiol. 2014;64:83–99.
Towbin JA. Inherited cardiomyopathies. Circ J. 2014;78:2347–56.
Spears DA, Gollob MH. Genetics of inherited primary arrhythmia disorders. Appl Clin Genet. 2015;8:215–33.
Milewicz DM, Carlson AA, Regalado ES. Genetic testing in aortic aneurysm disease: PRO. Cardiol Clin. 2010;28:191–7.
Loeys BL, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47:476–85.
•• Arscott P, Caleshu C, Kotzer K, Kreykes S, Kruisselbrink T, Orland K, Rigelsky C, Smith E, Spoonamore K, Haidle JL, Marvin M, Ackerman MJ, Hadi A, Mani A, Ommen S, Cherny S. A case for inclusion of genetic counselors in cardiac care: a case for genetic counselors. Cardiol Rev 2015. [Epub ahead of print]. Personalized Medicine Coalition: http://www.personalizedmedicinecoalition.org/Userfiles/PMC-Corporate/file/pmc_age_of_pmc_factsheet.pdf. This review details a series of cases in cardiovascular genetics regarding issues related to cost and utilization of genetic testing. These cases include current information stating that involvement of a genetic counselor promotes the efficient use of healthcare dollars.
•• Priori S, et al. HRS/EHRA/APHRS 2013 expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Heart Rhythm 2013;10(12):1932–63. Cigna Coverage Policy 0193: http://s-rm3.cigna.com/assets/docs/health-care-professionals/coverage_positions/mm_0193_coveragepositioncriteria_genetic_testing_for_long_qt_syndrome.pdf. Accessed 20 Jan 2016. A detailed consensus statement providing practical information on the diagnosis and management of patients and families with inherited heart disease.
Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Catheter Cardiovasc Interv. 2010;76(2):E43–86.
•• Richards S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015 ;17(5):405-24. WHO Resolution adopted by the General Assembly on 25 September 2015 [without reference to a Main Committee (A/70/L.1)] 70/1. Transforming our world: the 2030 Agenda for Sustainable Development. Current recommendations that are implemented in most clinical laboratories on the interpretation of sequence variants in genetic testing.
NIH Genomic Data Sharing Policy https://gds.nih.gov (accessed 1/20/16).
Loeys B, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355(8):788–98.
http://www.myokardia.com (accessed 1/20/16).
http://www.alnylam.com/ (accessed 1/20/16).
•• Middleton O et al., NAME position paper: retaining postmortem samples for genetic testing. Acad Forensic Pathol 2013 3(2):191–4. Healthcare 2015, 3, 830–7; doi:10.3390/healthcare3030830. An important position paper that recommends medical examiners save appropriate samples for postmortem genetic testing.
www.nsgc.org/postmortem. Accessed 20 Jan 2016.
Arch Pathol lab Med Vol 138 November 2014.
Mark Zuckerberg, Tuesday December 1, 2015 FACEBOOK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Lisa Castillo declares that she has no conflict of interest. Heather MacLeod provided an education webinar for Ambry, outside of the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Genetic Counseling and Clinical Testing.
Rights and permissions
About this article
Cite this article
MacLeod, H., Castillo, L. Current Cardiovascular Genetic Counseling. Curr Genet Med Rep 4, 142–146 (2016). https://doi.org/10.1007/s40142-016-0095-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-016-0095-0