Abstract
Purpose of review
The purpose of this paper is to review the evidence for radiofrequency ablation (RFA) as a treatment modality for facet-mediated low back pain. This review also evaluates gaps in evidence for RFA including optimal eligibility criteria and technique and safety concerns.
Recent findings
There is a lack of high quality evidence supporting RFA for facet-mediated low back pain. Six randomized control studies and multiple observational studies have been carried out, with mixed results for the efficacy of RFA for pain relief. There is a high rate of variability in the eligibility criteria and technique used for RFA and little evidence to support the appropriate inclusion and procedure. There remain safety questions about RFA, especially with regard to long-term effects of denervating the multifidus muscle.
Summary
Radiofrequency ablation is an interventional technique performed with the goal of reducing facet-mediated low back pain, but evidence to support it as an effective treatment modality is lacking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain is a complex biopsychosocial condition with a global prevalence estimated at 31% [1]. Despite its prevalence, the pathophysiology of acute and chronic low back pain, defined as pain lasting longer than 3 months, often remains unclear, even after appropriate and detailed clinical and radiographic evaluation [2,3,4,5]. There are a number of proposed nociceptive contributors to chronic low back pain including intervertebral disc degeneration, spondylolisthesis, injury of paraspinal muscles and tendons, and facet joint degeneration, and treatment efforts are often directed at these proposed pathologic contributors [6]. Lumbar radiofrequency ablation (RFA) is an increasingly used treatment designed to interrupt afferent input from facet joints, with the goal of reducing chronic low back pain [7, 8].
Despite its common use in clinical practice, lumbar RFA is an intervention with a dearth of evidence to support and guide its use. There remain many unanswered questions about the appropriate eligibility criteria for RFA, optimal RFA technique, appropriate use of repeated RFA, and long-term safety issues. In addition, the role of lumbar RFA within the context of a comprehensive, biopsychosocial model for chronic low back pain treatment remains unclear. The purpose of this narrative review is to evaluate the evidence as it relates to these gaps in knowledge and to consider this procedure in the broader context of chronic low back pain management.
The Role of Facet Joints in Chronic Low Back Pain
Facet joints are formed by the articulation of the superior articular process of one vertebra with the inferior articular process of the above vertebra. This synovial joint is exposed to multidirectional mechanical stress and can undergo degenerative changes such as the development of facet joint edema, osteophytes, cysts or synovitis, cartilage degeneration, and joint capsule injury [9,10,11,12,13,14]. Changes in the height of the contiguous intervertebral disc may also alter the articulation of the facet joint, increase joint loading, and cause further degeneration.
These degenerative changes of the facet joints have been proposed to account for 15–45% of the back pain [15,16,17,18,19], and, since more than 80% of the people suffer from low back pain in their lifetime, lumbar facet pain may impact a substantial population. RFA was first described as an interventional treatment for this facet-mediated low back pain by Shealy in 1975 [20]. Shealy proposed that lesion of nerves responsible for innervation of the degenerated joint via application of a heat generating electrical current would lead to relief of pain, as had been demonstrated after surgical severing of facet innervating nerves. RFA is performed by inserting an electrode between the superior articulating process and the transverse process of an involved level, resulting in a small lesion of adjacent nerves and subsequent disruption of pain signals (Fig. 1) [20,21,22].
Right RFA of the L2-3, L3-4, and L4-5 facet joints on anterior (a), lateral oblique (b), and lateral views (c). The tips of RFA electrodes at the junction of the superior articulating process and transverse process where the medial branch of the dorsal ramus lies can be best seen on the lateral oblique image
However, degenerative facet changes are also commonly noted on imaging of asymptomatic individuals and are not specific as a contributor to back pain [19, 23]. Consequently, facet-mediated pain is commonly identified in practice by medial branch blocks (MBBs), diagnostic local anesthetic blocks of the nerves innervating the facet joint at a painful spinal level, rather than imaging alone [12, 24,25,26,27]. Each facet joint is innervated by the medial branch of the dorsal ramus with contributions from the two vertebrae superior (e.g., the L3-L4 joint is innervated by branches from L2 to L3), and so, full anesthetic block of the sensory nerves to a single facet joint requires targeting of both nerve branches [14] (Fig. 2). If MBB results in an immediate reduction in the patient’s typical low back pain, and pain relief continues through the expected duration of the injected local anesthetic, the facet is posited to be the source of pain. At this point, RFA of the involved medial branch nerve for longer lasting pain relief can be considered [28,29,30,31,32,33]. However, the criteria for the amount of pain relief that defines a successful MBB and the number of repeat confirmatory blocks that should be performed before moving forward with RFA varies between practitioners [34].
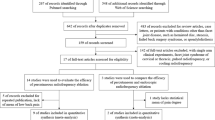
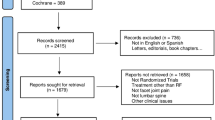
Summary of Evidence Related to Lumbar RFA Effectiveness
The effectiveness of lumbar RFA with regard to pain and function for patients with facet-mediated pain remains unclear [35••]. There are both observational studies and randomized trials that have attempted to answer important questions about the effectiveness of lumbar RFA, with resultant mixed outcomes [36]. Additionally, several systematic reviews about lumbar RFA have been published. Most evidence-based systematic reviews and guidelines use only data from randomized controlled trials to account for regression to the mean, the natural history of disease, and the high rate of non-specific effects, including placebo response, associated with interventional pain treatments [32, 33]. The consequence of these high rates of non-specific effects, which are thought to be of greater magnitude for invasive procedures, is that even ineffective or sham procedures will produce an apparent effect when comparisons are not made with an appropriate control group. Therefore, randomized trials that use a sham comparison, and the systematic reviews that incorporate them, are the most direct source of evidence for clinical efficacy for an interventional treatment such as RFA.
Randomized Trials of Lumbar RFA
There have been seven randomized control trials where lumbar RFA is compared to a sham procedure in which the RFA device is inserted but no heating or ablation of the medial branch nerve occurs. These seven trials demonstrated substantial heterogeneity in the methods used for diagnosing facet-mediated pain, the procedural technique, and the outcomes assessed (Table 1). In general, the quality of these trials is very low to moderate [35••]. Of these seven studies, three reported statistically significant differences favoring RFA, although the magnitude of the differences was not clinically meaningful in two of these studies [37,38,39]. Although it can be difficult to determine the minimally important difference between treatment groups, differences of less than 1.5 on the 0–10 pain VAS or 15 on the 0–100 pain VAS are typically not considered to be clinically important [40, 41]. Only the Van Kleef trial reported a difference of 1.9 points on the 0–10 VAS between RFA and sham at 8 weeks (no long-term results reported).
Several other trials have compared lumbar RFA to either no treatment [50••] or to another treatment such as intra-articular facet joint injections [45,46,47]. The recent randomized trial by Juch et al. indicated no significant differences in pain improvement at durations up to 1 year between patients who had ≥ 50% relief with a positive single MBB who were randomized to receive RFA versus a standardized exercise program without RFA [50••]. Since no sham RFA was provided for patients in the control arm of this trial, patients and clinicians were not blinded. Although lack of blinding would be expected to favor the interventional arm, such a tendency was not noted in this study.
Observational Trials
A number of observational studies without comparison to control interventions suggest benefit of lumbar RFA [32, 36, 51,52,53]. One of the most widely cited uncontrolled studies of lumbar RFA was conducted in 2000 by Dreyfuss et al. [31]. In this study, 15 patients who had > 80% improvement in pain after dual medial branch blocks underwent lumbar RFA and were followed for 1 year. A variety of outcomes were collected, most of which demonstrated a statistically significant and clinically meaningful improvement from baseline, including average pain VAS reduction from 5.1 to 0.2 at 3 months and from 5.1 to 1.0 at 12 months. The magnitude of these improvements was much greater than that seen in most randomized controlled trials and likely reflects the combination of placebo effect, regression to the mean, natural history, treatment effect, and highly selective eligibility criteria. Additionally, those 15 patients were identified through stringent inclusion criteria, with only 2% of the initially surveyed patients achieving sustained reduction of 90% of their baseline pain score. Taken in the context of other research, these results suggest that in highly selective populations there may be a benefit of lumbar RFA but that, given the full scope of the data, the magnitude of benefit experienced in typical clinical practice is low.
Systematic Reviews
The inconsistent findings of recent studies reflect the challenge of synthesizing this existing evidence for lumbar RFA. There have been three recent systematic reviews on this topic, including a Cochrane review, with similar findings but varying conclusions [35••, 54, 55]. The 2015 Cochrane review by Maas et al. concluded that there was low to moderate quality evidence that RFA of the facet joint could offer greater pain relief and improvement in function than placebo or steroid injections, but that there is no high-quality evidence of effectiveness of lumbar RFA for facet-mediated pain. Two additional reviews had similar findings but came to different overall conclusions about the efficacy of lumbar RFA, although all reviews agreed that additional large, high-quality randomized trials were needed to determine the true efficacy of lumbar RFA. Most recently, Juch et al., in the multicenter unblinded randomized Mint study, conducted a large, high-quality trial but this study has not yet been included in any systemic reviews [50••].
Eligibility Criteria
One of the critical evidence gaps relates to determining eligibility criteria for lumbar RFA. There is currently no gold standard diagnostic test for facet-mediated pain and strategies for diagnosis include varying combinations of clinical history, physical examination findings, imaging findings [56,57,58], and response to diagnostic MBBs with local anesthetic [14, 25, 59, 60]. In clinical trials, eligibility criteria for RFA range from physical exam findings consistent with facet joint pain to single diagnostic MBBs with local anesthetic [37, 38] to dual diagnostic MBBs using different local anesthetics in each block [31, 61] with requirements for pain improvement ranging from 50 to 100%. This variability reflects the uncertainty in diagnostic criteria for RFA, has led to disagreement as to the best methods to study its effectiveness [28, 62], and makes it challenging to compare study results.
Some studies have demonstrated a high false-positive rate of single diagnostic medial branch blocks for diagnosing facet-mediated pain when compared to actual pain relief post-RFA [31, 32, 47, 63, 64]. Two studies also suggested against overall improvements in outcomes when using more stringent criteria, either according to percentage cutoffs for pain improvement (e.g., 50 vs. 80%) or number of blocks (2 vs. 1) [61, 65].
The lack of consensus on the appropriate diagnostic criteria for lumbar RFA leads to high variability in actual clinical practice and inconsistencies in patient outcomes. Loosening eligibility criteria may result in higher false positive rates of diagnostic MBBs, with increased use of RFA and decreased rates of effectiveness, increased cost, and increased rates of adverse procedure effects. However, there are substantial logistical barriers to performing the most stringent eligibility criteria of dual MBBs with documented > 80% improvement in pain, concordant with the length of duration of action of the local anesthetic, including need for two separate additional procedures with associated cost, time use, and risk [61]. Nevertheless, the null finding from the largest RCT of lumbar RFA to date by Juch et al., which used one set of MBBs with ≥ 50% pain relief for selection of RFA candidates, suggests that more stringent selection, either by percentage pain relief or number of MBBs, may be necessary [50••].
Additionally, there is no standardized method of asking patients about pain relief after diagnostic MBBs. There are inherent biases in determining actual amount of pain relief from MBBs when patients are aware of the thresholds of relief necessary to obtain RFA, an intervention that they may believe is the best treatment option for them. For example, there may be large differences in response if patients are asked what percentage of pain relief they obtained versus measuring current pain on a numeric rating scale before and after a procedure [40, 41, 66]. Given these challenges, it is imperative that future research is directed towards identifying the optimal eligibility criteria for lumbar RFA that selects patients who are likely to experience a reduction in their pain, while balancing costs and patient experience during the selection process.
Optimal RFA Technique
RFA can be performed using different techniques that vary by method used to localize involved branches and the extent of heat ablation with regard to the number of sites ablated, size of the area ablated, and duration of heat applied [6, 20, 21]. One recommended technique to localize the involved branches of the medial nerve is to stimulate the sensory nerve to elicit paresthesias and to observe a multifidus twitch with stimulation of the motor nerve [22]. However, the techniques described to localize involved branches varies in the clinical trials vary from positive sensory stimulation only [34, 42], stimulation of the sensory nerve solely to rule out spinal nerve root localization [64], no sensory stimulation of the medial branch nerve [44], to positive responses to both sensory and motor stimulation [31, 47].
Some also argue that RFA techniques that use a needle approach parallel to the medial branch nerve will allow for a wider surface area of ablation of the nerve as compared to an older technique that approaches the medial branch nerve using a perpendicular approach [29]. From a biological plausibility standpoint increasing the size of the lesion of the nerve through needle placement alongside the nerve, using a larger diameter needle probe, creating multiple lesions, and using adequate probe temperature should all improve the efficacy of the procedure to ablate the targeted pain generator, the medial branch nerve. However, there are few studies that have directly compared these different procedural techniques and subsequent clinical outcomes for patients with facet-mediated pain receiving lumbar RFA. One recent retrospective comparative study attempted to determine whether or not the needle approach and subsequent area of nerve ablation impacts clinical outcomes [64]. In this study, the authors reported that patients in the parallel or advanced technique obtained similar pain relief post-ablation compared to patients who received the perpendicular or early technique in terms of mean reduction in pain on a 0–10 numerical rating scale from baseline to 1 month post-procedure (2.82 vs. 2.28, p = 0.08). Although this study found a modestly higher percentage of people in the parallel or advanced technique group reported “benefit” from the procedure (85.4 vs. 70.5%, p = 0.012), benefit was not clearly defined. They also reported that the median duration of pain relief was higher in the advanced technique group compared to the early technique group (4 vs. 1.5 months, p = 0.022). Based on these two findings, the authors concluded that the advanced technique demonstrated greater magnitude and duration of pain relief. However, given that there was no difference between the two groups in terms of mean pain reduction and that this was an uncontrolled retrospective study, the clinical implications of these findings are still unclear and are yet to be replicated in a controlled, prospective randomized trial.
Safety Questions
Although safety data is limited to randomized controlled trials, which are not designed to determine the frequency of adverse events, there have been relatively few reported short-term complications associated with lumbar RFA. The most commonly reported complication is transiently increased pain immediately after the procedure [35••]. Other reported complications include transient paresthesias [34], lower limb weakness [67], and superficial burns [68]. There is even less data on potential long-term consequences of RFA to the facet joints and intervertebral discs [69]. However, there is growing concern that denervating the multifidus, a core stabilizing muscle that is also innervated by medial branch nerves, may have negative long-term effects on low back pain and potentially could worsen spondylolisthesis with or without pars defects [6, 42, 54, 55, 63, 70,71,72,73]. Multifidus atrophy has been associated with chronic low back pain, and multilevel multifidus denervation, as can be confirmed with EMG after RFA [74, 75], may result in weakening and atrophy of these muscles and worsened low back pain [76,77,78,79,80,81]. One small study of five patients who had undergone only unilateral lumbar RFA showed widespread, bilateral atrophy of the multifidus muscles at 17–21 months post-procedure [82]. In another retrospective study of 27 patients who underwent lumbar RFA, the pre and post-procedure MRIs revealed no significant difference in multifidus atrophy [72]. However, there was evidence of statistically greater disc degeneration at levels where RFA was performed compared to unaffected levels (14.9 vs. 4.6%, p = 0.049). Given these preliminary studies, it is difficult to determine the long-term clinical impact of denervating the multifidus muscle or the effects of repeat RFA over time, but further studies are needed to address these questions.
RFA in the Context of Overall Treatment of Chronic Low Back Pain
Often lost in the debate over the technical aspects and idealized efficacy of RFA is the actual clinical utility of the procedure. The ultimate goal of treating patients with chronic LBP is to improve their function and quality of life. As is evidenced by a wealth of literature on both surgical and non-surgical care for chronic pain, true resolution of pain is often an elusive goal. Using lumbar fusion as an example, Carragee and Cheng surveyed patients undergoing lumbar fusion for spondylolisthesis to ascertain what the patients felt would be minimally acceptable outcomes for the surgery [83]. The majority of patients wanted to achieve pain levels of 3/10 or less, a reduction in their ODI score of at least 20 points, cessation of opioid pain medication, and return to work. Unfortunately, these expectations far exceed the benefits of either operative or non-operative care for chronic LBP in the major RCTs of lumbar fusion [84, 85]. In the seminal, non-controlled, non-blinded study by Dreyfuss et al., only 2% of the 460 initially considered patients actually obtained 90% pain relief for 12 months [74]. Extrapolating this proportion of response to all individuals with chronic LBP would seem to imply that clinically meaningful relief from RFA is doubtful for most people with chronic back pain.
Chronic LBP is a complex, biopsychosocial problem, and psychological factors including depression, anxiety, poor coping skills, somatization, and personality disorders are strongly correlated to poor outcomes from interventions intended to treat LBP [86,87,88]. Clinicians and patients also need to balance the risk of one or multiple invasive procedures against the unknown benefit of short-term pain relief of chronic pain, especially in patients identified as less likely to benefit from interventional procedures. For these patients, more active treatment strategies including goal-directed paced activity, exercise, cognitive-behavioral therapy, and redefining of expectations that may allow patients to take charge of their own pain control and enhance their quality of life, independent of a short-term reduction in pain offered by RFA, may be more beneficial [86,87,88,89].
Discussion/Conclusions
Lumbar RFA is commonly used in clinical practice to treat pain thought to originate from nociceptive input from the lumbar facet joints. Research over the last several decades has attempted to quantify the benefits and risks associated with this treatment, but there are many lingering questions that need to be answered to fully understand how to responsibly use this procedure for the treatment of facet-mediated low back pain. First, we must clarify the appropriate eligibility criteria for lumbar RFA and balance the depth of the diagnostic workup with the likelihood of successful RFA, the patient experience, and the risk of inappropriate patients undergoing the procedure. We must also determine if there is an optimal RFA technique to maximize outcomes while minimizing risk of the procedure, and we need to better understand the long-term effectiveness of RFA and its impact on physical, psychological, and social functioning. The cost effectiveness of lumbar RFA, particularly relative to other evidence-based treatment approaches to back pain, will benefit from more investigation. The long-term ramifications of denervating the multifidus muscle need to be further investigated, as do the impacts of repeated RFAs at the same or at multiple levels. Future trials of lumbar RFA should adhere to commonly accepted standards for clinical trial conduct to raise the quality and transparency of the evidence [90, 91]. These standards include registering the trials according to the International Committee of Medical Journal Editors policy [92], publishing protocols including detailed descriptions of the interventions and outcomes in advance, blinding of providers, and conducting multicenter trials to enhance generalizability whenever possible [93,94,95].
Clinicians, researchers, and patients need to consider the risks and benefits of lumbar RFA compared with other available treatment strategies that address the broader biopsychosocial complex of chronic low back pain and are directed at enhancing long-term quality of life and improving function. In the absence of definitive answers to these questions, we should exercise caution and restraint with the use of lumbar RFA and should fully disclose these uncertainties to patients when discussing risks, costs, and benefits of available treatments for their chronic low back pain.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37. https://doi.org/10.1002/art.34347.
Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a US national survey. Spine. 1995;20(1):11–9. https://doi.org/10.1097/00007632-199501000-00003.
Friedman BW, Chilstrom M, Bijur PE, Gallagher EJ. Diagnostic testing and treatment of low back pain in United States emergency departments: a national perspective. Spine. 2010;35(24):E1406–11. https://doi.org/10.1097/BRS.0b013e3181d952a5.
Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine. 1987;12(7):632–44. https://doi.org/10.1097/00007632-198709000-00002.
Goertz, M, ThorsonD, BonsellJ. Healthcare guidelines: adult acute and subacute low back pain. Institute for Clinical Systems Improvement
Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American pain society. Ann Intern Med. 2007;147(7):478–91. https://doi.org/10.7326/0003-4819-147-7-200710020-00006.
Stone JA, Bartynski WS. Treatment of facet and sacroiliac joint arthropathy: steroid injections and radiofrequency ablation. Tech Vasc Interv Radiol. 2009;12(1):22–32. https://doi.org/10.1053/j.tvir.2009.06.009.
Manchikanti L, Hirsch JA, Pampati V, Boswell MV. Utilization of facet joint and sacroiliac joint interventions in Medicare population from 2000 to 2014: explosive growth continues! Curr Pain Headache Rep. 2016;20(58):58. https://doi.org/10.1007/s11916-016-0588-2.
Kim J-S, Ali MH, Wydra F, Li X, Hamilton JL, An HS, et al. Characterization of degenerative human facet joints and facet joint capsular tissues. Osteoarthr Cartil. 2015;23(12):2242–51. https://doi.org/10.1016/j.joca.2015.06.009.
Boody BS, Savage JW. Evaluation and treatment of lumbar facet cysts. J Am Acad Orthop Surg. 2016;24(12):829–42. https://doi.org/10.5435/JAAOS-D-14-00461.
Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol. 2013;9(4):216–24. https://doi.org/10.1038/nrrheum.2012.199.
Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapophysial joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994;19(Supplement):1132–7. https://doi.org/10.1097/00007632-199405001-00006.
Suri P, Hunter DJ, Rainville J, Guermazi A, Katz JN. Presence and extent of severe facet joint osteoarthritis are associated with back pain in older adults. Osteoarthr Cartil. 2013;21(9):1199–206. https://doi.org/10.1016/j.joca.2013.05.013.
Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106(3):591–614. https://doi.org/10.1097/00000542-200703000-00024.
Dreyer SJ, Dreyfuss PH. Low back pain and the zygapophysial (facet) joints. Arch Phys Med Rehabil. 1996;77(3):290–300. https://doi.org/10.1016/S0003-9993(96)90115-X.
Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25:353–71.
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8. https://doi.org/10.1001/archinternmed.2008.543.
Hancock MJ, Maher CG, Latimer J, Spindler MF, McAuley JH, Laslett M, et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2007;16:1539–50.
Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine. 2008;33(23):2560–5. https://doi.org/10.1097/BRS.0b013e318184ef95.
Shealy CN. Percutaneous radiofrequency denervation of spinal facets. Treatment for chronic back pain and sciatica. J Neurosurg. 1975;43(4):448–51. https://doi.org/10.3171/jns.1975.43.4.0448.
Miedema ML, Pangarkar S. Pulsed versus conventional radio frequency ablation for lumbar facet joint dysfunction. Curr Phys Med Rehabil Rep. 2010;2:61–5.
Practice Guidelines for Spinal Diagnostic and Treatment Procedures. Practice Guidelines for Spinal Diagnostic and Treatment Procedures. International Spine Intervention Society. Practice Guidelines for Spinal Diagnostic and Treatment Procedures. 2nd ed. San Rafael (CA): International Spine Intervention Society; 2013. 2nd ed. San Rafael (CA): International Spine Intervention Society; 2013.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6. https://doi.org/10.3174/ajnr.A4173.
Revel M, Poiraudeau S, Auleley GR, Payan C, Denke A, Nguyen M, et al. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine. 1998;23(18):1972–6; discussion 1977. https://doi.org/10.1097/00007632-199809150-00011.
Schwarzer AC, Wang SC, O’Driscoll D, Harrington T, Bogduk N, Laurent R. The ability of computed tomography to identify a painful zygapophysial joint in patients with chronic low back pain. Spine. 1995;20(8):907–12. https://doi.org/10.1097/00007632-199504150-00005.
Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54(2):100–6. https://doi.org/10.1136/ard.54.2.100.
Schwarzer AC, Derby R, Aprill CN, Fortin J, Kine G, Bogduk N. Pain from the lumbar zygapophysial joints: a test of two models. J Spinal Disord. 1994;7:331–6.
Cohen SP, Huang JHY, Brummett C. Facet joint pain—advances in patient selection and treatment. Nat Rev Rheumatol. 2013;9(2):101–16. https://doi.org/10.1038/nrrheum.2012.198.
Gofeld M, Faclier G. Radiofrequency denervation of the lumbar zygapophysial joints—targeting the best practice. Pain Med. Malden Mass. 2008;9(2):204–11. https://doi.org/10.1111/j.1526-4637.2007.00345.x.
Burnham RS, Holitski S, Dinu I. A prospective outcome study on the effects of facet joint radiofrequency denervation on pain, analgesic intake, disability, satisfaction, cost, and employment. Arch Phys Med Rehabil. 2009;90(2):201–5. https://doi.org/10.1016/j.apmr.2008.07.021.
Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000;25(10):1270–7. https://doi.org/10.1097/00007632-200005150-00012.
MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med Malden Mass. 2013;14(5):639–45. https://doi.org/10.1111/pme.12000.
Friedly J, Standaert C, Chan L. Epidemiology of spine care: the back pain dilemma. Phys Med Rehabil Clin N Am. 2010;21(4):659–77. https://doi.org/10.1016/j.pmr.2010.08.002.
Cohen SP, Stojanovic MP, Crooks M, Kim P, Schmidt RK, Shields CH, et al. Lumbar zygapophysial (facet) joint radiofrequency denervation success as a function of pain relief during diagnostic medial branch blocks: a multicenter analysis. Spine J. Off. J. North Am. Spine Soc. 2008;8(3):498–504. https://doi.org/10.1016/j.spinee.2007.04.022.
•• Maas ET, Ostelo RWJG, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, et al. Radiofrequency denervation for chronic low back pain. Cochrane Database Syst. Rev. 2015;CD008572 This is a Cochrane review summarizing the evidence behind RFA as a modality for chronic low back pain. The key result was that there is no high-quality evidence showing that radiofrequency denervation provides pain relief or improves function for patients with chronic low back pain
McCormick ZL, Marshall B, Walker J, McCarthy R, Walega DR. Long-term function, pain and medication use outcomes of radiofrequency ablation for lumbar facet syndrome. Int J Anesth Anesthesiol. 2015;2(2) https://doi.org/10.23937/2377-4630/2/2/1028.
van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24(18):1937–42. https://doi.org/10.1097/00007632-199909150-00013.
Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23(6):524–9. https://doi.org/10.1097/AJP.0b013e318074c99c.
Gallagher J, Wedley J. Radiofrequency facet joint denervation in the treatment of low back pain: a prospective controlled double-blind study to assess its efficacy. Pain Clin. 1994;7:193–8.
Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J EMJ. 2001;18(3):205–7. https://doi.org/10.1136/emj.18.3.205.
Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101.
Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001;26(13):1411–6; discussion 1417. https://doi.org/10.1097/00007632-200107010-00003.
van Wijk RMAW, Geurts JWM, Wynne HJ, Hammink E, Buskens E, Lousberg R, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21(4):335–44. https://doi.org/10.1097/01.ajp.0000120792.69705.c9.
Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine. 2008;33(12):1291–7; discussion 1298. https://doi.org/10.1097/BRS.0b013e31817329f0.
Civelek E, Cansever T, Kabatas S, Kircelli A, Yilmaz C, Musluman M, et al. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg. 2012;22(2):200–6. https://doi.org/10.5137/1019-5149.JTN.5207-11.1.
Duger C, Ozdemir Kol I, Kaygusuz K, Gursoy S, Mimaroglu C. Effects of facet joint nerve block addition to radiofrequency in the treatment of low back pain. HealthMED. 2012;6:2052–6.
Lakemeier S, Lind M, Schultz W, Fuchs-Winkelmann S, Timmesfeld N, Foelsch C, et al. A comparison of intraarticular lumbar facet joint steroid injections and lumbar facet joint radiofrequency denervation in the treatment of low back pain: a randomized, controlled, double-blind trial. Anesth Analg. 2013;117(1):228–35. https://doi.org/10.1213/ANE.0b013e3182910c4d.
• Moussa WMM, Khedr W. Percutaneous radiofrequency facet capsule denervation as an alternative target in lumbar facet syndrome. Clin. Neurol. Neurosurg. 2016;150:96–104. This study compared RFA to RFA coagulation of the facet joint capsule or sham procedure. This study is included as important as it is a randomized controlled study that evaluates RFA versus a sham procedure
• Zhou Q, Zhou F, Wang L, Liu K. An investigation on the effect of improved X-rays-guided radiofrequency thermocoagulation denervation on lumbar facet joint syndrome. Clin. Neurol. Neurosurg. 2016;148:115–20. This is a randomized study comparing RFA to intraarticular facet joint injection with steroid. This study is important as it compares the efficacy of RFA to another commonly performed interventional treatment
•• Juch JNS, Maas ET, Ostelo RWJG, Groeneweg JG, Kallewaard J-W, Koes BW, et al. Effect of radiofrequency denervation on pain intensity among patients with chronic low back pain: the Mint randomized clinical trials. JAMA. 2017;318:68–81. This is a recent large, high-quality randomized control study comparing RFA to standardized exercise program without RFA. No significant difference in pain improvement were found when patients were followed for up to a year
Trinidad JM, Carnota AI, Failde I, Torres LM. Radiofrequency for the treatment of lumbar radicular pain: impact on surgical indications. Pain Res Treat. 2015;2015(392856)
Roy C, Chatterjee N, Ganguly S, Sengupta R. Efficacy of combined treatment with medial branch radiofrequency neurotomy and steroid block in lumbar facet joint arthropathy. J Vasc Interv Radiol JVIR. 2012;23(12):1659–64. https://doi.org/10.1016/j.jvir.2012.09.002.
Tomé-Bermejo F, Barriga-Martín A, Martín JLR. Identifying patients with chronic low back pain likely to benefit from lumbar facet radiofrequency denervation: a prospective study. J Spinal Disord Tech. 2011;24(2):69–75. https://doi.org/10.1097/BSD.0b013e3181dc9969.
Poetscher AW, Gentil AF, Lenza M, Ferretti M. Radiofrequency denervation for facet joint low back pain: a systematic review. Spine. 2014;39(14):E842–9. https://doi.org/10.1097/BRS.0000000000000337.
Leggett LE, Soril LJJ, Lorenzetti DL, Noseworthy T, Steadman R, Tiwana S, et al. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag. 2014;19(5):e146–53. https://doi.org/10.1155/2014/834369.
Lehman VT, Murphy RC, Kaufmann TJ, Diehn FE, Murthy NS, Wald JT, et al. Frequency of discordance between facet joint activity on technetium Tc99m methylene diphosphonate SPECT/CT and selection for percutaneous treatment at a large multispecialty institution. AJNR Am J Neuroradiol. 2014;35(3):609–14. https://doi.org/10.3174/ajnr.A3731.
Koh WU, Kim SH, Hwang BY, Choi WJ, Song JG, Suh JH, et al. Value of bone scintigraphy and single photon emission computed tomography (SPECT) in lumbar facet disease and prediction of short-term outcome of ultrasound guided medial branch block with bone SPECT. Korean J Pain. 2011;24(2):81–6. https://doi.org/10.3344/kjp.2011.24.2.81.
Stojanovic MP, Sethee J, Mohiuddin M, Cheng J, Barker A, Wang J, et al. MRI analysis of the lumbar spine: can it predict response to diagnostic and therapeutic facet procedures? Clin J Pain. 2010;26(2):110–5. https://doi.org/10.1097/AJP.0b013e3181b8cd4d.
Laslett M, McDonald B, Aprill CN, Tropp H, Oberg B. Clinical predictors of screening lumbar zygapophyseal joint blocks: development of clinical prediction rules. Spine J. Off. J. North Am. Spine Soc. 2006;6(4):370–9. https://doi.org/10.1016/j.spinee.2006.01.004.
Binder DS, Nampiaparampil DE. The provocative lumbar facet joint. Curr Rev Musculoskelet Med. 2009;2(1):15–24. https://doi.org/10.1007/s12178-008-9039-y.
Cohen SP, Strassels SA, Kurihara C, Griffith SR, Goff B, Guthmiller K, et al. Establishing an optimal “cutoff” threshold for diagnostic lumbar facet blocks: a prospective correlational study. Clin J Pain. 2013;29(5):382–91. https://doi.org/10.1097/AJP.0b013e31825f53bf.
Cohen SP, Rathmell JP. Tackling the technical challenges that hinder the success of facet joint radiofrequency treatment for spinal pain. Reg Anesth Pain Med. 2010;35(4):327–8. https://doi.org/10.1097/AAP.0b013e3181e82d66.
Van Zundert J, Mekhail N, Vanelderen P, van Kleef M. Diagnostic medial branch blocks before lumbar radiofrequency zygapophysial (facet) joint denervation: benefit or burden? Anesthesiology. 2010;113(2):276–8. https://doi.org/10.1097/ALN.0b013e3181e33b02.
Loh JT, Nicol AL, Elashoff D, Ferrante FM. Efficacy of needle-placement technique in radiofrequency ablation for treatment of lumbar facet arthropathy. J Pain Res. 2015;8:687–94. https://doi.org/10.2147/JPR.S84913.
Cohen SP, Williams KA, Kurihara C, Nguyen C, Shields C, Kim P, et al. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010;113(2):395–405. https://doi.org/10.1097/ALN.0b013e3181e33ae5.
Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. 2001;95(6):1356–61. https://doi.org/10.1097/00000542-200112000-00013.
Oh WS, Shim JC. A randomized controlled trial of radiofrequency denervation of the ramus communicans nerve for chronic discogenic low back pain. Clin J Pain. 2004;20(1):55–60. https://doi.org/10.1097/00002508-200401000-00011.
Moon JY, Lee PB, Kim YC, Choi SP, Sim WS. An alternative distal approach for the lumbar medial branch radiofrequency denervation: a prospective randomized comparative study. Anesth Analg. 2013;116(5):1133–40. https://doi.org/10.1213/ANE.0b013e31828b35fe.
Kornick C, Kramarich SS, Lamer TJ, Todd Sitzman B. Complications of lumbar facet radiofrequency denervation. Spine. 2004;29(12):1352–4. https://doi.org/10.1097/01.BRS.0000128263.67291.A0.
Slipman CW, Bhat AL, Gilchrist RV, Issac Z, Chou L, Lenrow DA. A critical review of the evidence for the use of zygapophysial injections and radiofrequency denervation in the treatment of low back pain. Spine J. Off. J. North Am. Spine Soc. 2003;3(4):310–6. https://doi.org/10.1016/S1529-9430(03)00025-1.
Ozcan-Eksi EE, Yagci I, Erkal H, Demir-Deviren S. Paraspinal muscle denervation and balance impairment in lumbar spinal stenosis. Muscle Nerve. 2016;53(3):422–30. https://doi.org/10.1002/mus.24759.
Smuck M, Crisostomo RA, Demirjian R, Fitch DS, Kennedy DJ, Geisser ME. Morphologic changes in the lumbar spine after lumbar medial branch radiofrequency neurotomy: a quantitative radiological study. Spine J. Off. J. North Am. Spine Soc. 2015;15(6):1415–21. https://doi.org/10.1016/j.spinee.2013.06.096.
Gossner J. The lumbar multifidus muscles are affected by medial branch interventions for facet joint syndrome: potential problems and proposal of a pericapsular infiltration technique. AJNR Am J Neuroradiol. 2011;32(11):E213. https://doi.org/10.3174/ajnr.A2901.
Dreyfuss P, Baker R, Leclaire R, Fortin L, Lambert R, Bergeron Y, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2002;27(5):556–7.
Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Nishida N, Taguchi T. Percutaneous radiofrequency facet joint denervation with monitoring of compound muscle action potential of the multifidus muscle group for treating chronic low back pain: a preliminary report. J Spinal Disord Tech. 2014;27(7):E262–7. https://doi.org/10.1097/BSD.0000000000000107.
Fortin M, Macedo LG. Multifidus and paraspinal muscle group cross-sectional areas of patients with low back pain and control patients: a systematic review with a focus on blinding. Phys Ther. 2013;93(7):873–88. https://doi.org/10.2522/ptj.20120457.
Hosseinifar M, Akbari M, Behtash H, Amiri M, Sarrafzadeh J. The effects of stabilization and McKenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: a randomized controlled trial in nonspecific chronic low back pain. J Phys Ther Sci. 2013;25:1541–5.
Huang Q, Li D, Zhang J, Yang D, Huo M, Maruyama H. Comparison of the efficacy of different long-term interventions on chronic low back pain using the cross-sectional area of the multifidus muscle and the thickness of the transversus abdominis muscle as evaluation indicators. J Phys Ther Sci. 2014;26(12):1851–4. https://doi.org/10.1589/jpts.26.1851.
Kalichman L, Hodges P, Li L, Guermazi A, Hunter DJ. Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2010;19:1136–44.
Kliziene I, Sipaviciene S, Klizas S, Imbrasiene D. Effects of core stability exercises on multifidus muscles in healthy women and women with chronic low-back pain. J Back Musculoskelet Rehabil. 2015;28(4):841–7. https://doi.org/10.3233/BMR-150596.
Massé-Alarie H, Beaulieu L-D, Preuss R, Schneider C. Corticomotor control of lumbar multifidus muscles is impaired in chronic low back pain: concurrent evidence from ultrasound imaging and double-pulse transcranial magnetic stimulation. Exp Brain Res. 2016;234(4):1033–45. https://doi.org/10.1007/s00221-015-4528-x.
Dreyfuss P, Stout A, Aprill C, Pollei S, Johnson B, Bogduk N. The significance of multifidus atrophy after successful radiofrequency neurotomy for low back pain. PM R. 2009;1(8):719–22. https://doi.org/10.1016/j.pmrj.2009.05.014.
Carragee EJ, Cheng I. Minimum acceptable outcomes after lumbar spinal fusion. Spine J Off J North Am Spine Soc. 2010;10(4):313–20. https://doi.org/10.1016/j.spinee.2010.02.001.
Mannion AF, Brox J-I, Fairbank JC. Consensus at last! Long-term results of all randomized controlled trials show that fusion is no better than non-operative care in improving pain and disability in chronic low back pain. Spine J. Off. J. North Am. Spine Soc. 2016;16(5):588–90. https://doi.org/10.1016/j.spinee.2015.12.001.
Fritzell P, Knutsson B, Sanden B, Strömqvist B, Hägg O. Recurrent versus primary lumbar disc herniation surgery: patient-reported outcomes in the Swedish Spine Register Swespine. Clin Orthop. 2015;473(6):1978–84. https://doi.org/10.1007/s11999-014-3596-8.
Chaichana KL, Mukherjee D, Adogwa O, Cheng JS, Mc Girt MJ. Correlation of preoperative depression and somatic perception scales with postoperative disability and quality of life after lumbar discectomy. J Neurosurg Spine. 2011;14(2):261–7. https://doi.org/10.3171/2010.10.SPINE10190.
Celestin J, Edwards RR, Jamison RN. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: a systematic review and literature synthesis. Pain Med. Malden Mass. 2009;10(4):639–53. https://doi.org/10.1111/j.1526-4637.2009.00632.x.
Daubs MD, Norvell DC, McGuire R, Molinari R, Hermsmeyer JT, Fourney DR, et al. Fusion versus nonoperative care for chronic low back pain: do psychological factors affect outcomes? Spine. 2011;36(21 Suppl):S96–109. https://doi.org/10.1097/BRS.0b013e31822ef6b9.
Qaseem A, Wilt TJ, Mc Lean RM, Forciea MA. for the Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30. https://doi.org/10.7326/M16-2367.
Gunzburg R. Randomized clinical trials: in pursuit of higher standards. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2014;23(8):1605. https://doi.org/10.1007/s00586-014-3460-2.
Chalmers I. Raising the standards of clinical trials and research. Bull World Health Organ. 2007;85:658–9.
ICMJE: Frequently asked questions about clinical trials registration [Internet]. 2010 [cited 2017Nov 7]. Available from:https://web.archive.org/web/20100706183418/http://www.icmje.org/faq_clinical.html
Gianola S, Frigerio P, Agostini M, Bolotta R, Castellini G, Corbetta D, et al. Completeness of outcomes description reported in low back pain rehabilitation interventions: a survey of 185 randomized trials. Physiother Can Physiother Can. 2016;68(3):267–74. https://doi.org/10.3138/ptc.2015-30.
Gianola S, Castellini G, Agostini M, Bolotta R, Corbetta D, Frigerio P, et al. Reporting of rehabilitation intervention for low back pain in randomized controlled trials: is the treatment fully replicable? Spine. 2016;41(5):412–8. https://doi.org/10.1097/BRS.0000000000001290.
Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, et al. Report of the NIH Task Force on research standards for chronic low back pain. Int J Ther Massage Bodyw. 2015;8:16–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Musculoskeletal Rehabilitation
Rights and permissions
About this article
Cite this article
Coles, A., Suri, P., Rundell, S. et al. Radiofrequency Ablation for Facet-Mediated Low Back Pain: Current Knowledge and Limitations of the Evidence. Curr Phys Med Rehabil Rep 6, 26–35 (2018). https://doi.org/10.1007/s40141-018-0170-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-018-0170-4