Abstract
Purpose of Review
The purpose of this review is to synthetize the latest evidence on the pharmacological management of postpartum hemorrhage (PPH) and apply it to the clinical context.
Recent Findings
The incidence of PPH in the developed world is rising. Oxytocin and its analogue carbetocin remain the number one choice as first-line uterotonics for the prevention of PPH due to excellent clinical efficacy and a favorable side effect profile. Doses of oxytocin and carbetocin currently recommended for prophylaxis are in excess to that required for clinical efficacy. There is no robust evidence suggesting that one second-line uterotonic drug is superior to another. Tranexamic acid is safe and highly effective and should be administered both for cases at high risk for PPH as well as early in established hemorrhage.
Summary
Choosing a uterotonic drug strategy that uses the most appropriate agent in the clinical context at the minimal effective dose is essential for improving maternal safety and the quality of postpartum care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and Clinical Context
Postpartum hemorrhage (PPH) is the most common cause of major obstetric hemorrhage and the leading cause of direct maternal death worldwide, resulting in enormous social and economic cost [1, 2]. It is estimated that 99% of global deaths due to PPH occur in developing countries [1••]. However, in advanced healthcare systems, PPH is still common, and a large cohort of women suffer invasive medical interventions or serious morbidity including postpartum hysterectomy and multiorgan failure [3]. Approximately 80% of cases of PPH are due to poor uterine tone in the immediate postpartum period. The incidence of uterine atony causing PPH is rising across the developed world, attributed to an increase in cesarean delivery rates, obesity, multiple pregnancy, advancing maternal age, and the rise in oxytocin-augmented labor [3,4,5]. If PPH is proactively managed, maternal morbidity and mortality can be significantly reduced [6].
Uterotonics are the primary preventative therapy for the management of atonic PPH, with excellent clinical efficacy, and are widely recommended by the major international societies [1, 7,8,9]. Timely administration of uterotonics not only mitigates against poor maternal outcomes but also reduces the requirement for further medical intervention including second-line drugs, blood transfusion, and surgery [7••]. PPH has many identifiable risk factors; however, most women suffering from PPH have low-risk pregnancies and no identifiable risk factors, necessitating a strategy where prophylaxis against PPH is recommended for all women [9]. There is significant variability in the dosage recommendations of uterotonics by international societies as well as in those administered in clinical practice [8••]. Improving both the safety and efficacy of uterotonic drug strategy is key to improving the quality of maternal peripartum care globally.
First-Line Uterotonic Drugs: Oxytocin
Indications and Efficacy
Oxytocin is the longest serving and most widely used uterotonic drug and, along with its analogue carbetocin, is the first-line prophylaxis for PPH [1••]. Oxytocin is the first choice uterotonic drug in most society and international guidelines due to both its low cost and an attractive combination of excellent efficacy with a relatively favorable side effect profile for most women [7••].
Pharmacology
Oxytocin is a neuroendocrine reproductive hormone that is produced in the hypothalamus and secreted from the pituitary gland in humans [10]. Oxytocin binds to oxytocin receptors on the myometrial cell membrane to induce its contractile effect (Table 1) [15]. Oxytocin also stimulates the production of prostaglandin PGF2α [10]. The efficacy of exogenous oxytocin is proportional to both the number and affinity of transmembrane oxytocin receptors on the myometrium to oxytocin. There is exponential proliferation of these receptors during pregnancy and early labor, resulting in myometrium that is exquisitely sensitive to oxytocin at term; hence, effective contractility may be obtained with very small doses of oxytocin [16]. Myometrium is poorly responsive to oxytocin prior to term due to a paucity of receptors. Oxytocin has a short plasma half-life (3–5 min) necessitating a continuous infusion for sustained contractility effect [17].
Prolonged exposure to oxytocin leads to oxytocin receptor desensitization and failure of oxytocin to elicit effective myometrial contractions, termed the oxytocin desensitization phenomenon [18]. Oxytocin desensitization is dependent on both the concentration and length of time that the myometrium is exposed to oxytocin [19, 20]. Oxytocin receptor desensitization is homologous (specific only to oxytocin and its analogues) and does not affect the response to other uterotonic agents such as prostaglandins and ergot alkaloids [21].
Safety and Side Effects
Oxytocin is a complex hormone associated with a range of extrauterine effects, most serious of which are effects on the cardiovascular system [22]. These effects strongly correlate with both the dose and speed of administration [23, 24]. The risk of adverse outcome due to cardiovascular collapse is particularly high in two risk groups where a number of deaths have occurred: in the setting of hypovolemia and in women with pre-existing cardiovascular disease [25, 26]. The cardiovascular effects of oxytocin are due to stimulation of oxytocin receptors in the heart releasing atrial natriuretic peptide (ANP) and brain-type natriuretic peptide (BNP), as well as the release of nitric oxide (NO) in the peripheral vasculature [22]. These are potent vasodilators that drop the systemic vascular resistance and cause hypotension, a reflex tachycardia, and a compensatory increase in cardiac output. Oxytocin may also have a direct negative effect on cardiac inotropy. Chest pain, ST-T changes, and dysrhythmias may also occur [27]. Other side effects include nausea and vomiting, shortness of breath, and abdominal pain [28]. Oxytocin has a structure similar to ADH giving it a strong antidiuretic effect at high concentrations [29]. Women in labor have a lower baseline plasma sodium as well as an impaired ability to excrete water in the third trimester [30]. This predisposes them to dilutional hyponatraemia, which may cause seizures and coma [31]. One randomized controlled trial comparing IV and IM oxytocin after vaginal delivery reported similar side effects in each group [32•]. There is a growing body of evidence suggesting that oxytocin is involved in complex social behavior and cognition with important roles in maternal mood, anxiety, and mother-infant bonding [33, 34].
Dosing
There is significant variability in the dose of oxytocin recommended to be administered as prophylaxis and therapy for PPH [8••]. Most of the obstetric society guidelines recommend doses between 5 IU and 10 IU administered diluted as slow IV infusions for prophylaxis after both vaginal and cesarean delivery [1, 35,36,37]. The World Health Organization (WHO) recommends a dose of 10 IU IM or IV [1••]. An international consensus statement on the use of uterotonic agents at cesarean delivery was published in 2019 to address clinical variability in dosing [8••]. These guidelines draw on existing evidence and consequently recommend much lower doses of oxytocin: 1 IU bolus followed by a maintenance infusion at 2.5–7.5 IU.h−1 at elective cesarean delivery and 3 IU bolus followed by a maintenance infusion at 7.5–15 IU.h−1 at intrapartum cesarean delivery.
Due to the phenomenon of oxytocin receptor desensitization, there are significant differences in dose requirements at elective and intrapartum cesarean delivery. Women undergoing an intrapartum cesarean delivery following an oxytocin-augmented labor require a dose of oxytocin that is nine times greater (90% effective dose [ED90] 2.99 IU; 95% CI 2.32–3.67 IU) compared with that required at elective cesarean delivery (ED90 0.35 IU; 95% CI 0.18–0.52 IU) [38, 39]. Adequate uterine tone at elective cesarean delivery can be achieved with lower doses of oxytocin (0.5–3 IU), resulting in reduced side effects [24]. These studies, although conducted with small sample sizes in low-risk populations, provide convincing evidence that the doses that are widely recommended are significantly greater than those required for efficacy in most women.
Timing of Administration
For maximum efficacy, the uterotonic should be given immediately after fetal extraction to reduce time to effect and the potential for blood loss. Rapid bolus administration may be associated with a precipitous drop in maternal blood pressure. Women who had 5 IU oxytocin administered as an infusion over 5 min had less cardiovascular deviation compared with those who received a rapid bolus dose [23]. Slowing the rate of oxytocin bolus administration is associated with greater cardiovascular stability and has been recommended by the recent consensus statement [8••].
Route of Administration
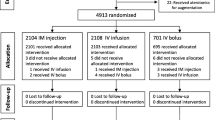
Oxytocin must be administered IV or IM and cannot be administered via the oral or rectal routes. Some oxytocin preparations require cold storage and transport to maintain its stability, which may limit its availability in settings where women are cared for with limited resources [40]. A double-blind randomized control trial allocated women to receive 10 IU of oxytocin either IV or IM [32•]. There was no difference in the primary outcome of PPH >500 mL, but the IV group suffered significantly less severe PPH (PPH> 1000 mL) (4.6% vs. 8.1%), blood transfusion (1.5% vs. 4.5%), and admissions to the high dependency unit (1.7% vs. 3.7%).
First-Line Uterotonic Drugs: Carbetocin
Indications and Efficacy
Carbetocin is an oxytocin analogue. The drug is currently not available for use in the USA or Japan. It is at least as effective as oxytocin and shares a similarly favorable side effect profile compared to other uterotonic drug classes [7••]. Use is limited by its relatively high price, often multiples of the cost of oxytocin [41]. However, there is good evidence to suggest that carbetocin may be superior and more cost-effective than conventional uterotonic drug combinations for the prevention of PPH [7, 42]. Due to its clinical effectiveness, reduction in the requirement for further therapy, and low risk of adverse events, economic viability has been demonstrated in high resource settings [43]. In a multi-center, randomized, non-inferiority trial comparing carbetocin (heat-stable formulation) 100 μg IM and oxytocin 10 IU in nearly 30,000 women, carbetocin was non-inferior to oxytocin with regard to blood loss >500 ml or the need for an additional uterotonic drugs after vaginal delivery [44•]. Carbetocin is also associated with a reduced need for additional uterotonics when compared to oxytocin at elective cesarean delivery [42]. The Society of Obstetricians and Gynecologists of Canada (SOGC) is the only group recommending carbetocin over oxytocin at cesarean delivery for prophylaxis of PPH [45].
Pharmacology
Carbetocin is a synthetic analogue of oxytocin and causes activation of oxytocin receptors via the same mechanism [46]. It has been pharmacologically designed for sustained contractility, with a duration of action approximately 4–7 times that of oxytocin due to both a longer biological half-life (40 min) and increased duration of action at the oxytocin receptor, avoiding the need for continuous infusion [47]. This increased half-life is due to increased lipophilicity, tissue distribution, and resistance to peptidase degradation. Onset of action is similar to oxytocin, within about 2 min of administration. In the laboratory, myometrial contractions stimulated by carbetocin are attenuated by prior exposure to oxytocin as both drugs work via the oxytocin receptor. Therefore, women who have been exposed to oxytocin in labor will have a reduced response to carbetocin postpartum, requiring higher dosing [48].
Carbetocin is available in a heat-stable formulation, which offers it a substantial advantage in terms of cold chain storage. Heat-stable carbetocin does not require refrigeration and therefore eliminates the costs associated with refrigerated storage and transport for non-heat-stable uterotonics.
Safety and Side Effects
The adverse effects and hemodynamic consequences of carbetocin are similar to those described for oxytocin [49]. Doses larger than 100 μg are associated with a high incidence of tachycardia and arrhythmia and are not recommended [50].
Dose
Carbetocin has one-thirtieth the potency of oxytocin. The dose widely recommended is 100μg, which is based on initial clinical trials and information from the manufacturer [1, 45]. However, at elective cesarean delivery (oxytocin-naïve women), the dose required has been demonstrated to be significantly lower than that recommended by the manufacturer and widely used in many randomized controlled trials. One sequential allocation dose finding study demonstrated the ED90 to be 14.8 μg (95% CI 14–16) [51]. The dose of carbetocin at cesarean delivery for labor arrest, however, is 121 μg (95% CI 111–130), reflecting desensitization of the oxytocin receptors [50]. Interestingly, another dose finding study determined the dose to be 63 (95% CI 57–69) μg in a population of women with a BMI ≥ 40 kg.m [52]. This is approximately four times higher than in a similar population of women with BMI <40 kg.m. Uterotonics are currently not given on a by-weight basis, although this suggests dose adjustment in women with BMI ≥ 40 kg.m. The increase in dose requirement for women with high BMI may be related to volume of distribution, lipophilicity, or poorer myometrial contractility in women with obesity [53].
Timing of Administration
Carbetocin and oxytocin have similar onset times. Bolus dosing of carbetocin is associated with a precipitous drop in maternal blood pressure [54]. Similar to oxytocin, carbetocin should be administered as a slow IV bolus.
Route of Administration
Carbetocin can be administered IV or IM, the latter resulting in a longer time to peak effect and increased duration of action [46]. Carbetocin cannot be administered via the oral, rectal, or vaginal route.
Second-Line Uterotonic Drugs: the Prostaglandins
Indications and Efficacy
Carboprost and sulprostone are used to treat PPH where oxytocin or carbetocin has failed. The ability of prostaglandins to induce myometrial contractility in vitro is inferior to oxytocin [55]. Furthermore, they are not currently used as first-line prophylaxis due to significant adverse effects. The effects of prostaglandins are unaffected by prior exposure to oxytocin [21]. There is currently a multi-center randomized control trial underway to compare carboprost to oxytocin as first-line treatment of PPH [56]. Misoprostol is an orally stable prostaglandin E1 analogue. It is recommended to be used as first-line treatment of PPH where oxytocin is not available, due to problems with cold chain storage or if skilled healthcare staff are unavailable to administer IV or IM medication. It has efficacy that is broadly similar to that of oxytocin but is limited by an unfavorable side effect profile [7, 57]. Furthermore, it has a much slower onset time.
Pharmacology
Prostaglandins act via stimulation of the prostaglandin receptor, which include PGE1, PGE2, and PGF2α subtypes. Carboprost is a synthetic PGF2α analogue, and sulprostone is a PGE2 analogue. These are G-coupled receptors leading to stimulation of second messenger pathways and a rise in intracellular calcium. The rise in intracellular calcium ion concentration causes myometrial contractility. In contrast to oxytocin receptors, prostaglandin receptors are present and functional throughout pregnancy. Misoprostol, a PGE1 analogue, is water- and heat-stable and has a long shelf life and pharmacological stability in hot climates [58]. It has a slow onset of action and is effective between 9 and 15 min after administration with a half-life of 20–40 min.
Safety and Side Effects
Prostaglandins cause bronchospasm, particularly in women with asthma. Other side effects may include hypertension, hypotension, pulmonary edema, diarrhea, nausea, vomiting, flushing, pyrexia, and myalgia [7, 59, 60]. Sulprostone may additionally cause painful uterine contractions and has contributed to a cardiac arrest when administered during hemorrhagic shock [61].
Side effects of misoprostol include vomiting, abdominal pain, diarrhea, shivering, and pyrexia [62]. When misoprostol is added to oxytocin in combination to treat PPH, the likelihood of vomiting (RR 2.11, 95% CI 1.39–3.18) and fever (RR 3.14, 95% CI 2.20 to 4.49) is increased [7••]. Unlike the other prostaglandins, misoprostol does not cause bronchoconstriction and therefore may be administered safely to women with asthma [63•].
Dose
There is very little evidence in the literature regarding appropriate dosing of prostaglandins. Carboprost is recommended at a dose of 250μg every 15 min up to a maximum of 8 doses [8••]. Doses between 400 and 600 μg of misoprostol are currently recommended. Dosing can be repeated every 15 min up to a total of 800 μg [8••]. Sulprostone is administered at a dose of 500 μg IV at 100 μg.h−1 up to a maximum dose of 1500 μg [8••].
Timing of Administration
Prostaglandins are not currently recommended as first-line prophylaxis for PPH. As with all second-line drugs, they should be administered soon after it is recognized that the first-line agent, oxytocin or carbetocin, was ineffective at producing adequate uterine tone.
Route of Administration
Carboprost may be administered IM or intramyometrial (unlicensed); its intravenous route is contraindicated. Misoprostol is highly flexible in terms of the mode of administration as it can be administered via oral, vaginal, rectal, or sublingual routes. Oral and sublingual routes have a rapid onset of action compared to rectal and vaginal routes [64]. Rectal and vaginal routes have a more prolonged action as well as greater bioavailability [65]. Rates of shivering and fever are higher when the oral or sublingual route is used [66]. Sulprostone is the only prostaglandin that may be administered IV and may also be administered IM. Carboprost and sulprostone both require refrigeration.
Second-Line Uterotonic Drugs: Ergometrine and Methylergonovine
Indications and Efficacy
Ergometrine and methylergonovine are currently recommended as a second-line drug for the treatment of PPH. Evidence from the clinical setting describes very little difference in efficacy between ergot alkaloids and oxytocin [1••]. Inferior efficacy to both oxytocin and carbetocin has been demonstrated in vitro [55]. A combination preparation with oxytocin is available in some countries called Syntometrine. Ergometrine with oxytocin is a highly efficacious and cost-effective drug strategy for the prevention of PPH (>500 mL) with significant additional benefit vs. oxytocin alone (rr = 0.69, 95% CI 0.57–0.83) [7••]. Ergometrine can only be administered in situations where hypertensive disorders are absent, which may limit its use where they cannot be excluded [67]. The use of ergometrine for the management of retained placenta is not recommended as this may cause tetanic uterine contractions that can delay expulsion of the placenta [1••].
Pharmacology
Ergonovine maleate (ergometrine) and methylergonovine are crystalline ergot alkaloid derivatives. The plasma half-life of ergometrine is less predictable than that of the oxytocin analogues with a range of 30 to 120 min [68]. The drugs are unstable in heat requiring refrigeration. Activity is via alpha receptors triggering an intracellular rise in calcium and culminating in myometrial contraction [69, 70]. There is also action via dopamine receptors and a partial 5-HT signalling effect. Agonism of alpha and 5-HT3 receptors are likely responsible for its vasoconstrictor effect, which is advantageous in the uterine vasculature during hemorrhage but may also cause systemic hypertension and ischemia.
Safety and Side Effects
The ergot alkaloids are contraindicated in situations of hypertension as peripheral vasoconstriction leads to elevated systemic arterial pressure. Severe nausea is common [7••]. Ischemic heart disease and myocardial infarction have been reported, even in women without pre-existing cardiovascular disease [71]. Women suffering from anemia due to hemorrhage are particularly susceptible. Ergot alkaloids can cause uterine rupture due to the strength of uterine contractions when given in high doses [72]. Ergometrine may cause porphyria.
Dose
There is evidence lacking in relation to the dose of ergometrine that should be administered with guidelines recommending a range from 200 to 500 μg [8••]. The dose of ergometrine may be repeated every 2 h in exceptional circumstances up to a total dose of 1000 μg. Ergometrine may be particularly useful where there is a paucity of myometrial oxytocin receptors, for example, at extreme pre-term delivery where the number of uterine oxytocin receptors has not yet reached those at term.
Timing of Administration
Ergometrine is a second-line drug and should be administered to treat postpartum hemorrhage where the uterotonic administered for hemorrhage prophylaxis has failed. Quick progression to second-line drugs after hemorrhage is important to prevent excessive blood loss. Ergometrine causes sustained contraction of the uterus and therefore should not be administered until the placenta is delivered [1••].
Route of Administration
Ergot derivatives can be administered IV, IM, or via the oral route. Oral ergometrine offers no benefit over placebo [73]. There are no trials comparing the IV versus IM routes of administration. The IV route has an immediate onset of action, whereas the IM route induces uterine contractions within 2–5 min and is less likely to precipitate hypertension [74]. Ergometrine requires refrigeration.
Adjunctive Drugs to Uterotonics: Tranexamic Acid
Indications and Efficacy
Tranexamic acid (TXA) is an exciting and novel addition to the pharmacological management of PPH as it acts via a different mechanism than uterotonics to reduce hemorrhage [63•]. TXA reduces bleeding by inhibiting the enzymatic breakdown of fibrin [75•]. TXA has an established history of reducing blood loss over many decades in non-obstetric situations, including in elective surgery and trauma [76, 77].
For the Treatment of PPH
In 2017 the WOMAN trial was published [78••]. This was a large, multi-center, randomized placebo-controlled trial with 20,060 women from mostly developing countries. The primary outcome was death from all causes or hysterectomy within 42 days of randomization. Although there was no difference in the primary composite endpoint, the trial showed that by administering TXA, deaths from bleeding were reduced by about 20% (1.9% vs. 1.5%, rr 0.81, 95%CI 0.65–1.0, p= 0.005). The greatest benefit was seen when TXA was administered within 3 h of childbirth. A reduction in surgery required to control severe bleeding was also demonstrated. A Cochrane review of anti-fibrinolytic agents including the WOMAN trial as well as a smaller French randomized controlled trial supported these results [79, 80]. Due to the low unit cost of TXA and considerable efficacy, it is highly cost-effective, particularly in countries with higher maternal mortality [81]. TXA may not be beneficial for all causes of postpartum hemorrhage, with likelihood of benefit greater in the group of patients with delayed bleeding from lacerations or trauma as in this case, primary hemostasis occurs due to blood clotting—rather than in cases of atony with large open bleeding vessels [82].
Prevention of PPH at Cesarean Delivery
TXA reduces bleeding if given prophylactically at cesarean delivery [83]. One meta-analysis of more than 27 randomized control trials determined that TXA decreases blood loss, the incidence of severe PPH, blood transfusion requirements, and further medical intervention when given as prophylaxis at cesarean delivery without increasing the risk of a thrombotic event [84,84,86]. There is currently a larger multi-center randomized, double-blind, placebo-control trial underway, which will further evaluate TXA as PPH prophylaxis at cesarean delivery [87].
Prevention of PPH at Vaginal Delivery
Evidence for TXA as prophylaxis at vaginal deliveries has been less convincing than at cesarean delivery. A large French multi-center, double-blind randomized controlled trial determined that amongst women who received prophylactic oxytocin, the use of TXA did not result in a rate of PPH greater than 500 mL compared to those who did not receive TXA [88]. One smaller study demonstrated benefit of TXA when given as part of standard active management of the third stage of labor [89].
Pharmacology
After placental separation from the uterine wall, the uterus contracts. There is an increase in the concentration of coagulation factors and platelets at the site of bleeding as well as an increase in fibrinolysis [90, 91]. Fibrinolysis starts when plasminogen is converted to plasmin by tissue plasminogen activator (tPA); plasmin then increases blood clot breakdown (Fig. 1). Tranexamic acid inhibits this process of fibrinolysis. It exerts its effects as a lysine analogue by blocking lysine binding sites on plasminogen molecules. This inhibits the enzymatic breakdown of fibrinogen and fibrin by plasmin [92]. The effect is stabilization of existing blood clots, rather than accelerating the creation of new ones [93].
Mechanism of action of tranexamic acid. (a) Fibrinolysis starts when plasminogen is converted to plasmin by tissue plasminogen activator (tPA). Plasmin increases blood clot breakdown and breaks down fibrin into fibrin degradation products. (b) Tranexamic acid (TXA) inhibits this process of fibrinolysis, exerting its effects as a synthetic lysine analogue by blocking lysine binding sites on plasminogen molecules, thus preventing plasmin formation
Safety and Side Effects
The WOMAN trial demonstrated TXA to be remarkably safe, and a subsequent Cochrane review debunked the theory that TXA might be associated with an increased risk of thrombosis in healthy women [78, 80]. The side effects of TXA usually occur at doses much higher than those recommended currently and include hypersensitivity reactions, renal cortical necrosis, and an increase in seizures [83, 94]. TXA injected inadvertently into the intrathecal or epidural space can be catastrophic; therefore, extra caution should be taken in the obstetric setting, where regional anesthesia and TXA are commonly used [95•]. One meta-analysis demonstrated a higher incidence of nausea and vomiting after tranexamic acid administration at vaginal delivery [96].
Dose
The WHO recommends a fixed dose of 1 g in 10 mL of TXA in normal saline, intravenously at a rate of 100mg/min [1••]. A second dose may be administered if bleeding extends over 30 min or it restarts within 24 h of the first dose.
Timing of Administration
Death from bleeding occurs soon after the onset of hemorrhage. Data shows that during bleeding, the survival benefit of TXA decreases 10% for every 15 min of treatment delay, and after 3 h, there is no benefit [97]. Therefore tranexamic acid is recommended to be administered immediately, and the drug should be readily available to care givers. Peak plasma concentrations are achieved rapidly after administration of an intravenous dose [75•].
Route of Administration
TXA is recommended to be administered by the IV route [1••]. Administration via the oral or IM routes is also possible. Oral bioavailability is 46% [98]. Further research into the efficacy of the different routes of administration has been identified as a priority by the WHO (https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/postpartum-care/who-recommendation-tranexamic-acid-treatment-postpartum-haemorrhage). The administration of oral TXA in addition to misoprostol did not demonstrate benefit over misoprostol alone [99].
E) Optimizing a Prevention Strategy—Balancing Safety and Efficacy. The Role of the 2019 Uterotonic Consensus Guidelines on the Use of Uterotonic Drugs During Cesarean Delivery
In 2019, a consensus statement on the use of uterotonics at cesarean delivery was published [8••]. This statement was developed to address the huge variation in the clinical use of uterotonic drugs at cesarean delivery as well as the heterogeneity in recommendations from the major international society guidelines [8, 100, 101]. This statement aims to disseminate the latest evidence to the clinical context, dealing specifically with the unique situation of prophylactic uterotonic administration at cesarean delivery and seeks to encourage constructive discussion on the topic with our obstetric colleagues. The existing evidence base for uterotonic dosing is limited as most studies are performed on small numbers of low-risk patients, which may limit the external validity of results [102]. However, there is clear evidence suggesting that women undergoing elective cesarean delivery (oxytocin naïve) should be considered a separate entity compared to those undergoing intrapartum cesarean delivery (potential for oxytocin receptor desensitization) [50, 51]. Choosing the minimum dose of uterotonic that is effective is important to reduce adverse effects and ensure patient safety. A universal prophylaxis dose for all women is not appropriate. Drug dosing should reflect the patients’ medical and obstetric comorbidities as well as the clinical context. Attention is drawn to the potential for drug error and inadvertent uterotonic administration prior to delivery of the fetus with potentially catastrophic consequences.
Conclusion
There is convincing evidence in the literature suggesting that doses of uterotonics for prophylaxis of PPH are given in doses that are excess to those required for efficacy. Oxytocin or its analogue carbetocin are universally recommended first-line drugs where they are available due to both excellent clinical efficacy and a favorable side effect profile. Oxytocin should be administered initially as a small bolus and then as a titrated infusion. There is not yet enough evidence to universally recommend carbetocin over oxytocin, but carbetocin has a number of advantages including the availability of a heat-stable formulation, a longer half-life, and evidence suggesting there is less requirement for second-line drugs. Misoprostol is recommended by the WHO in situations where skilled health personnel are not present to administer oxytocin [1••]. Second-line drugs should be guided by the clinical context, any contraindications, and local availability and considered early for maximum efficacy. There is no substantial evidence in the literature to suggest one second-line drug over another. TXA has demonstrated excellent clinical efficacy and safety for mothers and should be readily available and administered in cases at high risk for PPH as well as early in established PPH. Standardizing and protocolizing uterotonic drug strategy at an institutional level is important to improve patient safety and the quality of care patients receive.
Change history
28 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40140-021-00449-2
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• WHO. WHO recommendations uterotonics for the prevention of postpartum haemorrhage. 2018. https://apps.who.int/iris/bitstream/handle/10665/277276/9789241550420-eng.pdf?ua=1. Accessed 30th December 2020. Global recommendations on PPH management with recommendations for high and low resource settings
Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33.
Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle MH, Ford JB, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009;9:55.
Mehrabadi A, Liu S, Bartholomew S, Hutcheon JA, Kramer MS, Liston RM, et al. Temporal trends in postpartum hemorrhage and severe postpartum hemorrhage in Canada from 2003 to 2010. J Obstet Gynaecol Can. 2014;36(1):21–33.
Lutomski JE, Byrne BM, Devane D, Greene RA. Increasing trends in atonic postpartum haemorrhage in Ireland: an 11-year population-based cohort study. BJOG. 2012;119(3):306–14.
Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2011;11:CD007412.
•• Gallos ID, Papadopoulou A, Man R, Athanasopoulos N, Tobias A, Price MJ, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev. 2018;12:CD011689 Cochrane network metanalysis supports use of carbetocin.
•• Heesen M, Carvalho B, Carvalho JCA, Duvekot JJ, Dyer RA, Lucas DN, et al. International consensus statement on the use of uterotonic agents during caesarean section. Anaesthesia. 2019;74(10):1305–19 International consensus statement provides evidence based guidance at caesarean delivery.
NICE. Intrapartum care: care of healthy women and their babies during childbirth. Clinical Guideline 190. 2014.
Gimpl G, Fahrenholz F. The oxytocin receptor system: structure, function, and regulation. Physiol Rev. 2001;81(2):629–83.
Syntocinon®. Product information, Novartis Pharmaceuticals Australia Pty Ltd.
Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet. 2007;99(Suppl 2):S160–7.
Gizzo S, Patrelli TS, Gangi SD, Carrozzini M, Saccardi C, Zambon A, et al. Which uterotonic is better to prevent the postpartum hemorrhage? Latest news in terms of clinical efficacy, side effects, and contraindications: a systematic review. Reprod Sci. 2013;20(9):1011–9.
Schimmer BP, Parker KL. Contraception and pharmacotherapy of obstetrical and gynecological disorders. In: Brunton L, Chabner B, Knollman B, editors. Goodman & Gilman’s the Pharmacological Basis of Therapeutics. 12th ed. New York, NY: McGraw-Hill Medical; 2011.
Arrowsmith S, Wray S. Oxytocin: its mechanism of action and receptor signalling in the myometrium. J Neuroendocrinol. 2014;26(6):356–69.
Fuchs AR, Fuchs F, Husslein P, Soloff MS. Oxytocin receptors in the human uterus during pregnancy and parturition. Am J Obstet Gynecol. 1984;150(6):734–41.
Ryden G, Sjoholm I. Half-life of oxytocin in blood of pregnant and non-pregnant women. Acta Endocrinol. 1969;61(3):425–31.
Phaneuf S, Rodriguez Linares B, TambyRaja RL, MacKenzie IZ, Lopez BA. Loss of myometrial oxytocin receptors during oxytocin-induced and oxytocin-augmented labour. J Reprod Fertil. 2000;120(1):91–7.
Robinson C, Schumann R, Zhang P, Young RC. Oxytocin-induced desensitization of the oxytocin receptor. Am J Obstet Gynecol. 2003;188(2):497–502.
Balki M, Erik-Soussi M, Kingdom J, Carvalho JC. Oxytocin pretreatment attenuates oxytocin-induced contractions in human myometrium in vitro. Anesthesiology. 2013;119(3):552–61.
Balki M, Cristian AL, Kingdom J, Carvalho JC. Oxytocin pretreatment of pregnant rat myometrium reduces the efficacy of oxytocin but not of ergonovine maleate or prostaglandin F 2 alpha. Reprod Sci. 2010;17(3):269–77.
Petersson M. Cardiovascular effects of oxytocin. Prog Brain Res. 2002;139:281–8.
Thomas JS, Koh SH, Cooper GM. Haemodynamic effects of oxytocin given as i.v. bolus or infusion on women undergoing caesarean section. Br J Anaesth. 2007;98(1):116–9.
Butwick AJ, Coleman L, Cohen SE, Riley ET, Carvalho B. Minimum effective bolus dose of oxytocin during elective Caesarean delivery. Br J Anaesth. 2010;104(3):338–43.
G L. The National Institute for Clinical Excellence; The Scottish Executive Health Department; The Department of Health, Social Services and Public Safety: Northern Ireland. Why Mothers Die 1997–1999. The fifth report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. London. 2001.
Farina Z, Fawcus S. Oxytocin--ensuring appropriate use and balancing efficacy with safety. S Afr Med J. 2015;105(4):271–4.
Svanstrom MC, Biber B, Hanes M, Johansson G, Naslund U, Balfors EM. Signs of myocardial ischaemia after injection of oxytocin: a randomized double-blind comparison of oxytocin and methylergometrine during Caesarean section. Br J Anaesth. 2008;100(5):683–9.
Dansereau J, Joshi AK, Helewa ME, Doran TA, Lange IR, Luther ER, et al. Double-blind comparison of carbetocin versus oxytocin in prevention of uterine atony after cesarean section. Am J Obstet Gynecol. 1999;180(3 Pt 1):670–6.
Li C, Wang W, Summer SN, Westfall TD, Brooks DP, Falk S, et al. Molecular mechanisms of antidiuretic effect of oxytocin. J Am Soc Nephrol. 2008;19(2):225–32.
Shakhmatova EI, Osipova NA, Natochin YV. Changes in osmolality and blood serum ion concentrations in pregnancy. Hum Physiol. 2000;26(1):92–5.
Bergum D, Lonnee H, Hakli TF. Oxytocin infusion: acute hyponatraemia, seizures and coma. Acta Anaesthesiol Scand. 2009;53(6):826–7.
• Adnan N, Conlan-Trant R, McCormick C, Boland F, Murphy DJ. Intramuscular versus intravenous oxytocin to prevent postpartum haemorrhage at vaginal delivery: randomised controlled trial. BMJ. 2018;362:k3546 Recent RCT comparing the most common methds of oxytocin administration.
Kirsch P. Oxytocin in the socioemotional brain: implications for psychiatric disorders. Dialogues Clin Neurosci. 2015;17(4):463–76.
Kroll-Desrosiers AR, Nephew BC, Babb JA, Guilarte-Walker Y, Moore Simas TA, Deligiannidis KM. Association of peripartum synthetic oxytocin administration and depressive and anxiety disorders within the first postpartum year. Depress Anxiety. 2017;34(2):137–46.
Prevention and Management of Postpartum Haemorrhage. BJOG: An Int J Obstet Gynaecol. 2017;124(5):e106-e49.
Committee on Practice B-O. Practice Bulletin No. 183. 183: Postpartum Hemorrhage. Obstet Gynecol. 2017;130(4):e168–e86.
Intrapartum care for healthy women and babies. NICE Clinical Guideline 190. London: National Institute for Health and Care Excellence; 2014.
Carvalho JC, Balki M, Kingdom J, Windrim R. Oxytocin requirements at elective cesarean delivery: a dose-finding study. Obstet Gynecol. 2004;104(5 Pt 1):1005–10.
Balki M, Ronayne M, Davies S, Fallah S, Kingdom J, Windrim R, et al. Minimum oxytocin dose requirement after cesarean delivery for labor arrest. Obstet Gynecol. 2006;107(1):45–50.
Torloni MR, Gomes Freitas C, Kartoglu UH, Metin Gulmezoglu A, Widmer M. Quality of oxytocin available in low- and middle-income countries: a systematic review of the literature. BJOG. 2016;123(13):2076–86.
Pickering K, Gallos ID, Williams H, Price MJ, Merriel A, Lissauer D, et al. Uterotonic drugs for the prevention of postpartum haemorrhage: a cost-effectiveness analysis. Pharmacoecon Open. 2019;3(2):163–76.
Onwochei DN, Van Ross J, Singh PM, Salter A, Monks DT. Carbetocin reduces the need for additional uterotonics in elective caesarean delivery: a systematic review, meta-analysis and trial sequential analysis of randomised controlled trials. Int J Obstet Anesth. 2019;40:14–23.
Voon HY, Shafie AA, Bujang MA, Suharjono HN. Cost effectiveness analysis of carbetocin during cesarean section in a high volume maternity unit. J Obstet Gynaecol Res. 2018;44(1):109–16.
• Widmer M, Piaggio G, Nguyen TMH, Osoti A, Owa OO, Misra S, et al. Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med. 2018;379(8):743–52 RCT demonstrates non-inferiority of heat stable carbetocin to oxytocin.
Leduc D, Senikas V, Lalonde AB. No. 235-active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. J Obstet Gynaecol Can. 2018;40(12):e841–e55.
Hunter DJ, Schulz P, Wassenaar W. Effect of carbetocin, a long-acting oxytocin analog on the postpartum uterus. Clin Pharmacol Ther. 1992;52(1):60–7.
Atke A, Vilhardt H. Uterotonic activity and myometrial receptor affinity of 1-deamino-1-carba-2-tyrosine(O-methyl)-oxytocin. Acta Endocrinol. 1987;115(1):155–60.
Cole NM, Carvalho JC, Erik-Soussi M, Ramachandran N, Balki M. In vitro comparative effect of carbetocin and oxytocin in pregnant human myometrium with and without oxytocin pretreatment. Anesthesiology. 2016;124(2):378–86.
Mannaerts D, Van der Veeken L, Coppejans H, Jacquemyn Y. Adverse effects of carbetocin versus oxytocin in the prevention of postpartum haemorrhage after caesarean section: a randomized controlled trial. J Pregnancy. 2018;2018:1374150.
Nguyen-Lu N, Carvalho JC, Farine D, Seaward G, Ye XY, Balki M. Carbetocin at cesarean delivery for labour arrest: a sequential allocation trial to determine the effective dose. Can J Anaesth. 2015;62(8):866–74.
Khan M, Balki M, Ahmed I, Farine D, Seaward G, Carvalho JC. Carbetocin at elective cesarean delivery: a sequential allocation trial to determine the minimum effective dose. Can J Anaesth. 2014;61(3):242–8.
Drew T, Balki M, Farine D, Ye XY, Downey K, Carvalho JCA. Carbetocin at elective caesarean section: a sequential allocation trial to determine the minimum effective dose in obese women. Anaesth 2020:75;331–37. https://doi.org/10.1111/anae.14944.
Zhang J, Bricker L, Wray S, Quenby S. Poor uterine contractility in obese women. BJOG. 2007;114(3):343–8.
Dell-Kuster S, Hoesli I, Lapaire O, Seeberger E, Steiner LA, Bucher HC, et al. Efficacy and safety of carbetocin given as an intravenous bolus compared with short infusion for caesarean section - double-blind, double-dummy, randomized controlled non-inferiority trial. Br J Anaesth. 2017;118(5):772–80.
Balki M, Erik-Soussi M, Ramachandran N, Kingdom J, Carvalho JC. The contractile effects of oxytocin, ergonovine, and carboprost and their combinations: an in vitro study on human myometrial strips. Anesth Analg. 2015;120(5):1074–84.
The carboprost or oxytocin postpartum haemorrhage effectiveness study. Available from: http://copestudy.uk/.
Hofmeyr GJ, Gulmezoglu AM. Misoprostol for the prevention and treatment of postpartum haemorrhage. Best Pract Res Clin Obstet Gynaecol. 2008;22(6):1025–41.
Smith JM, Dimiti A, Dwivedi V, Ochieng I, Dalaka M, Currie S, et al. Advance distribution of misoprostol for the prevention of postpartum hemorrhage in South Sudan. Int J Gynaecol Obstet. 2014;127(2):183–8.
Kilpatrick AW, Thorburn J. Severe hypotension due to intramyometrial injection of prostaglandin E2. Anaesthesia. 1990;45(10):848–9.
Baduni N, Sanwal MK, Jain A. Acute pulmonary edema after intramyometrial prostodin. J Anaesthesiol Clin Pharmacol. 2011;27(2):275–7.
Chen FG, Koh KF, Chong YS. Cardiac arrest associated with sulprostone use during caesarean section. Anaesth Intensive Care. 1998;26(3):298–301.
Bilgin Z, Komurcu N. Comparison of the effects and side effects of misoprostol and oxytocin in the postpartum period: a systematic review. Taiwan J Obstet Gynecol. 2019;58(6):748–56.
• Dey T, Weeks AD. Identification, prevention and management of post-partum haemorrhage. Obstetr Gynaecol Reprodu Medi. 2020;30(8):231–41 Clear review of PPH management from the surgical perspective.
Chong YS, Chua S, Shen L, Arulkumaran S. Does the route of administration of misoprostol make a difference? The uterotonic effect and side effects of misoprostol given by different routes after vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2004;113(2):191–8.
Zieman M, Fong SK, Benowitz NL, Banskter D, Darney PD. Absorption kinetics of misoprostol with oral or vaginal administration. Obstet Gynecol. 1997;90(1):88–92.
Khan RU, El-Refaey H. Pharmacokinetics and adverse-effect profile of rectally administered misoprostol in the third stage of labor. Obstet Gynecol. 2003;101(5 Pt 1):968–74.
Vogel JP, Williams M, Gallos I, Althabe F, Oladapo OT. WHO recommendations on uterotonics for postpartum haemorrhage prevention: what works, and which one? BMJ Glob Health. 2019;4(2):e001466.
de Groot AN, van Dongen PW, Vree TB, Hekster YA, van Roosmalen J. Ergot alkaloids. Current status and review of clinical pharmacology and therapeutic use compared with other oxytocics in obstetrics and gynaecology. Drugs. 1998;56(4):523–35.
DM RH, JM R. Rang and Dale’s Pharmacology: Churchill Livingstone; 2011.
Hollingsworth M, Edwards D, Miller M. Ergometrine--a partial agonist at 5-HT receptors in the uterus isolated from the oestrogen-primed rat. Eur J Pharmacol. 1988;158(1-2):79–84.
Spencer SPE, Lowe SA. Ergometrine for postpartum hemorrhage and associated myocardial ischemia: Two case reports and a review of the literature. Clin Case Rep. 2019;7(12):2433–42.
van Dongen PW, de Groot AN. History of ergot alkaloids from ergotism to ergometrine. Eur J Obstet Gynecol Reprod Biol. 1995;60(2):109–16.
Liabsuetrakul T, Choobun T, Peeyananjarassri K, Islam QM. Prophylactic use of ergot alkaloids in the third stage of labour. Cochrane Database Syst Rev. 2018;6:CD005456.
G. M. Ergonovine maleate and methylergonovine maleate. AHFS drug information. 2004.
• Brenner A, Ker K, Shakur-Still H, Roberts I. Tranexamic acid for post-partum haemorrhage: what, who and when. Best Pract Res Clin Obstet Gynaecol. 2019;61:66–74 Detailed review of tranexamic acid.
Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, et al. The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess. 2013;17(10):1–79.
•• Collaborators WT. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105–16 Global trial supporting use of traexamic acid for the prevention of PPH.
Ducloy-Bouthors AS, Jude B, Duhamel A, Broisin F, Huissoud C, Keita-Meyer H, et al. High-dose tranexamic acid reduces blood loss in postpartum haemorrhage. Crit Care. 2011;15(2):R117.
Shakur H, Beaumont D, Pavord S, Gayet-Ageron A, Ker K, Mousa HA. Antifibrinolytic drugs for treating primary postpartum haemorrhage. Cochrane Database Syst Rev. 2018;2:CD012964.
Li B, Miners A, Shakur H, Roberts I, Collaborators WT. Tranexamic acid for treatment of women with post-partum haemorrhage in Nigeria and Pakistan: a cost-effectiveness analysis of data from the WOMAN trial. Lancet Glob Health. 2018;6(2):e222–e8.
Weeks AD. Tranexamic acid for postpartum haemorrhage: a major advance. Lancet Glob Health. 2018;6(2):e132–e3.
Lecker I, Wang DS, Whissell PD, Avramescu S, Mazer CD, Orser BA. Tranexamic acid-associated seizures: causes and treatment. Ann Neurol. 2016;79(1):18–26.
Gungorduk K, Yildirim G, Asicioglu O, Gungorduk OC, Sudolmus S, Ark C. Efficacy of intravenous tranexamic acid in reducing blood loss after elective cesarean section: a prospective, randomized, double-blind, placebo-controlled study. Am J Perinatol. 2011;28(3):233–40.
Franchini M, Mengoli C, Cruciani M, Bergamini V, Presti F, Marano G, et al. Safety and efficacy of tranexamic acid for prevention of obstetric haemorrhage: an updated systematic review and meta-analysis. Blood Transfus. 2018;16(4):329–37.
Vasichko PE, Ireland KE, Boyd AR, Acosta OM, Ramsey PS. Use of tranexamic acid to prevent postpartum hemorrhage in women undergoing cesarean delivery: a meta-analysis. Obstet Gynecol. 2018;131:90S.
Sentilhes L, Daniel V, Deneux-Tharaux C, Group TS, the Groupe de Recherche en Obstetrique et G. TRAAP2 - TRAnexamic acid for preventing postpartum hemorrhage after cesarean delivery: a multicenter randomized, doubleblind, placebo- controlled trial - a study protocol. BMC Pregnancy Childbirth. 2020;20(1):63.
Sentilhes L, Winer N, Azria E, Senat MV, Le Ray C, Vardon D, et al. Tranexamic acid for the prevention of blood loss after vaginal delivery. N Engl J Med. 2018;379(8):731–42.
Gungorduk K, Asicioglu O, Yildirim G, Ark C, Tekirdag AI, Besimoglu B. Can intravenous injection of tranexamic acid be used in routine practice with active management of the third stage of labor in vaginal delivery? A randomized controlled study. Am J Perinatol. 2013;30(5):407–13.
Hellgren M. Hemostasis during normal pregnancy and puerperium. Semin Thromb Hemost. 2003;29(2):125–30.
Shakur-Still H, Roberts I, Fawole B, Kuti M, Olayemi OO, Bello A, et al. Effect of tranexamic acid on coagulation and fibrinolysis in women with postpartum haemorrhage (WOMAN-ETAC): a single-centre, randomised, double-blind, placebo-controlled trial. Wellcome Open Res. 2018;3:100.
Prentice CR. Basis of antifibrinolytic therapy. J Clin Pathol Suppl (R Coll Pathol). 1980;14:35–40.
Goobie SM, Frank SM. Tranexamic acid: what is known and unknown, and where do we go from here? Anesthesiology. 2017;127(3):405–7.
Frimat M, Decambron M, Lebas C, Moktefi A, Lemaitre L, Gnemmi V, et al. Renal cortical necrosis in postpartum hemorrhage: a case series. Am J Kidney Dis. 2016;68(1):50–7.
• Patel S, Robertson B, McConachie I. Catastrophic drug errors involving tranexamic acid administered during spinal anaesthesia. Anaesthesia. 2019;74(7):904–14 Important paper highlighting dangers of tranexamic acid and potential neuraxial administration.
Xia Y, Griffiths BB, Xue Q. Tranexamic acid for postpartum hemorrhage prevention in vaginal delivery: a meta-analysis. Medicine (Baltimore). 2020;99(3):e18792.
Gayet-Ageron A, Prieto-Merino D, Ker K, Shakur H, Ageron FX, Roberts I, et al. Effect of treatment delay on the effectiveness and safety of antifibrinolytics in acute severe haemorrhage: a meta-analysis of individual patient-level data from 40 138 bleeding patients. Lancet. 2018;391(10116):125–32.
Grassin-Delyle S, Semeraro M, Foissac F, Bouazza N, Shakur-Still H, Roberts I, et al. Tranexamic acid through intravenous, intramuscular and oral routes: an individual participant data meta-analysis of pharmacokinetic studies in healthy volunteers. Fundam Clin Pharmacol. 2019;33(6):670–8.
Diop A, Abbas D, Ngoc NTN, Martin R, Razafi A, Tuyet HTD, et al. A double-blind, randomized controlled trial to explore oral tranexamic acid as adjunct for the treatment for postpartum hemorrhage. Reprod Health. 2020;17(1):34.
Orbach-Zinger S, Einav S, Yona A, Eidelman LA, Fein S, Davis A, et al. A survey of physicians' attitudes toward uterotonic administration in parturients undergoing cesarean section. J Matern Fetal Neonatal Med. 2018;31(23):3183–90.
Weale N, Laxton C. Prophylactic use of oxytocin at caesarean section: where are the guidelines? Anaesthesia. 2013;68(10):1006–9.
Monks DT, Palanisamy A. Intrapartum oxytocin: time to focus on longer term consequences? Anaesthesia. 2019;74(10):1219–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any potential conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obstetric Anesthesia
Rights and permissions
About this article
Cite this article
Drew, T., Carvalho, J.C.A. Pharmacologic Prevention and Treatment of Postpartum Hemorrhage. Curr Anesthesiol Rep 11, 37–47 (2021). https://doi.org/10.1007/s40140-021-00444-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00444-7