Abstract
Purpose of Review
The management of paranasal/sinonasal malignancies continues to evolve with improvements in surgical techniques, advances in the delivery of radiation therapy, and development of new systemic therapies. We aim to discuss the management of paranasal sinus malignancies, which often involves multimodality therapy, with a primary focus on the radiotherapy aspects of care.
Recent Findings
Advances in the delivery of radiation therapy have led to a variety of new strategies for the treatment of paranasal sinus malignancies, often allowing for an improved therapeutic ratio maximizing the dose to the target while reducing the dose to the surrounding normal structures.
Summary
Radiation therapy plays a key role in the management of many paranasal sinus malignancies. Continued advances in the delivery of radiation therapy may provide futher improvement in the risk/benefit ratio for radiotherapy as primary, neoadjuvant, or advant treatment in this setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sinonasal malignancies are a rare tumor population, making up only 3–5% of all head and neck cancers, with approximately 2000 Americans being diagnosed with this type of neoplasm per year [1,2,3]. This group includes those tumors denominated as sinonasal or paranasal sinus tumors which originate from the nasal cavity and/or the maxillary, ethmoid, sphenoid, and frontal sinuses, and represents a diverse group of tumor histologies with distinct biologic and pathologic behaviors, requiring different treatment approaches. Tumors located in this region present unique challenges in determining the best treatment approach due to the complex anatomy in the region.
Due to the nonspecific nature of many of the presenting symptoms of these tumors, they are often diagnosed in a later stage. Symptoms include nasal obstruction, epistaxis, rhinorrhea, or pain in the region that may initially be thought of coming from a benign etiology [4]. Treatment of sinonasal tumors often requires multimodality treatment, including a combination of surgery, radiation therapy (RT), and chemotherapy, and should be done under the supervision of a multidisciplinary team. Surgery is the primary treatment modality for many of these tumors, which may be proceed or be followed by radiation and/or chemotherapy; however, in some cases, tumors may be unresectable or would result in unacceptable morbidity/cosmetic outcomes [5,6,7,8]. Surgical techniques have evolved over the years from more extensive craniofacial resections to an increased utilization of endoscopic or combined approaches. In the age of intensity modulated radiation therapy (IMRT) and proton therapy (PT), treatment with radiation therapy, either as the primary local treatment modality or in some specific clinical situations as a neoadjuvant or adjuvant treatment, has significantly improved over the years [9,10,11]. With either local treatment modality, care must be taken in determining the best treatment(s) to minimize morbidity in this anatomically complex region.
While there are a diverse group of histologies that can develop in this region, our primary aim is to review treatment advances in radiation therapy for management of this diverse group of malignant histologies.
Histologies
Squamous Cell Carcinoma
Squamous cell carcinomas (SCC) represent the most common histology of all sinonasal cancers, accounting for approximately 80% of tumors diagnosed in this location [3]. This histologic subtype has a higher risk of nodal involvement compared to other nasal and paranasal sinus tumor histologies, with rates of up to 30% of patients having cervical neck or retropharyngeal nodal involvement at diagnosis [9, 12,13,14]. Like many tumors in this location, SCC often presents at a late stage. Local failures are a major concern for relapse. There have been some studies that have shown a relationship with HPV and a subgroup of SCC of the sinonasal region, but the prognostic significance of HPV has not been clearly established [15, 16]. One retrospective single institutional study reporting on their outcomes of SCC of the paranasal cavity found some discordance in tumor specimens testing positive (n = 11) or doubtful (n = 5) for p16 on immunohistochemistry but did not test positive for HPV (n = 9) on HPV RNAscope testing. They noted a numerical improvement in OS and PFS in p16 + patients treated with curative intent, and there was a statistically significant improvement in curatively treated HPV + patients. Looking specifically at HPV + patients who had surgery with adjuvant RT, they trended toward improved OS and had significantly better PFS. Notably, HPV + patients tended to be younger at diagnosis with mainly nasal fossa primary location, with primaries in this location tending to have improved outcomes prior to stratifying by HPV status [17].
If resectable, standard treatment for these tumors is surgery upfront followed by adjuvant RT with or without chemotherapy, depending on pathologic features. Surgery may be done via an endoscopic, craniofacial, or combined approach, depending on the location and extent of disease [18]. Adjuvant radiation doses range from 60–66 Gy to the postoperative primary surgical bed, depending on the surgical margin and presence of high-risk pathologic features such as lymphovascular invasion or perineural invasion. If the tumor is unresectable, RT may be used as the primary local treatment modality and typically uses doses around 66–70 Gy to target the gross disease [19,20,21,22,23]. Current data suggests 3- and 5-year local control rates ranging from 75–85% and 50–70%, respectively and overall survival rates of 60–80% and 40–55% at the same time points for SCC in the sinonasal region [3, 11, 19, 21, 23,24,25,26].
The maxillary sinus is the most common subsite of malignancy. Tumors in this location have a reported incidence of up to 20% of nodal involvement at diagnosis in T3-T4 lesions, and it is not uncommon for initially clinically N0 patients to develop regional nodal recurrences later on, with reports of over 30% of these patients having nodal relapse without elective nodal irradiation (ENI). The at risk areas for nodal involvement at diagnosis and for regional recurrences include ipsilateral level IB, II, preauricular area and contralateral level II; however, the decision to treat the at risk neck regions should be made on an individual patient basis, with the primary benefit seen in improved loco-regional control. If there is posterior nasal cavity or posterior ethmoid sinus involvement, there should be consideration for including the retropharyngeal lymph nodes in the ENI volume. For tumors that do not cross the midline and present with N0 disease, it is reasonable to include only the ipsilateral neck, particularly levels Ib-III, VIIa, and IX [27, 28]. ENI has demonstrated a reduction in the risk of neck recurrence from 36 to 7% and distant metastasis from 20 to 3% at 5 years, although this did not translate into an improvement in overall survival [29]. Locally, these tumors may extend into the nasal cavity, nasopharynx, ethmoid cells, orbits, pterygopalatine fossa, palate, and even the skull base and cavernous sinus. It is important to consider the potential at risk routes of spread when designing radiation treatment volumes to minimize the chance of a local recurrence and treatment related toxicities.
For select stage I tumors of the sinonasal tract (nasal cavity and ethmoid sinus), single modality treatment with surgery or RT may be curative. For locally advanced tumors, multimodality treatment with surgery followed by adjuvant RT is usually indicated [30,31,32].
Adenocarcinoma
Adenocarcinomas of the paranasal sinus region represent a diverse group of malignancies that account for 10–20% of all nasal cavity and paranasal sinus tumors [33]. These tumors are classified as salivary and non-salivary type adenocarcinomas, with the latter group being further divided into intestinal and non-intestinal type [34, 35].
The primary treatment modality of these tumors, similar to those with SCC histology, is surgery if resectable, followed by RT ± chemotherapy used in the adjuvant setting, depending on the final pathology. Doses of 60–66 Gy are used in the adjuvant setting, with higher doses in the realm of 70 Gy being used as primary local treatment in the case of unresectable and/or inoperable tumors. These tumors tend to be more aggressive compared to SCC, with 5-yr OS rates of 40–60% in salivary-type tumors; however, there are low grade adenocarcinomas that tend to have a less aggressive natural history [2, 36, 37]. Non-salivary, intestinal-type adenocarcinoma (ITAC) tends to have a behavior similar to that of a high-grade malignancy, with rates of over 50% local recurrences, 8% cervical lymph node metastases, and 13% distant metastasis in an analysis of 213 cases, with 60% of patients ultimately dying from their disease, most within 3 years of diagnosis [33], Compared to SCC, high grade adenocarcinomas tend to have an increased propensity for distant metastasis, with 11% versus 37%, respectively, of maxillary sinus patients developing distant metastasis at 5 years [29]. Low grade nonintestinal-type adenocarcinomas represent a small subset of sinonasal adenocarcinomas, accounting for approximately 13% of all sinonasal adenocarcinomas, and are most commonly found in the ethmoid sinus, nasal cavity, and maxillary sinus. Standard treatment consists of surgical resection, with adjuvant RT as an option. While local recurrences are possible, these tumors rarely metastasize, and the overall outlook for these patients is quite favorable, with only 2 of 23 patients dying of disease in one retrospective study with a median follow up of 6.3 years [38].
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma (ACC) may also develop in this region. One of the distinguishing characteristics of this tumor type is its propensity for perineural spread and extension into the skull base, with reports of at least half of ACCs having perineural invasion (PNI) [39, 40]. PNI is associated with a poorer prognosis, with increased local recurrence and reduced overall survival [41]. From a symptomatic perspective, extensive PNI can cause debilitating neurologic symptoms, including neuropathic pain, numbness, and motor nerve dysfunction.
Conversely, these tumors have a low propensity of lymphatic spread. The mainstay of treatment involves primary surgical resection, if resectable, followed by adjuvant radiation therapy to improve local control. Radiation doses of 60–66 Gy are standard for the adjuvant therapy, with higher doses reaching 70 Gy used if there is gross residual disease or when radiation is the primary local treatment modality [24, 26, 42, 43].
Any involved nerves should be included within the treatment field, covering the nerve’s path to the skull base, and in some cases, may track all the way to the brainstem, pending the degree of nerve involvement. The RT dose used for nerve coverage depends on the extent of nerve involvement. For microscopic PNI, 50–60 Gy may be used. For positive margin along the nerve or gross disease or PNI visualized on imaging, higher doses reaching 70 Gy may be used. Due to the proximity of critical neurologic structures, this is an area where the use of proton therapy is especially beneficial in minimizing dose to non-target tissues while maintaining coverage of the target [22, 25, 26, 42]. The use of proton therapy has also demonstrated an advantage in local control compared to photon treatments. Historically, 5- year local/locoregional control rates ranging from 26–61% have been reported using photons. With the use of protons, there have been reports of 5-year local control ranging from 65–90% [44, 45]. Due to the low risk of lymph node involvement, it is not necessary to include prophylactic lymphatic coverage in the radiation treatment volumes in those with an N0 neck, with only 1 of 37 ACC of the maxillary sinus patients, all N0 at diagnosis, developing nodal recurrence in one retrospective study; however, distant metastasis remain a significant concern, with 37% of patients developing distant metastatic disease at 5 years [29]. Distant metastatic disease can develop several years after initial diagnosis, so it is especially important to follow these patients closely after treatment completion.
There has not been a proven benefit of adding standard chemotherapy agents in the treatment of ACC; however, several recent studies are investigating the use of novel agents, with one potential target being the NOTCH pathway [46]. NOTCH1, 2, 3, and 4 belong to the NOTCH gene family, which encode a large transmembrane receptor signaling protein that has been found to have activating mutations in numerous cancer types, including approximately 20% of ACCs. Unfortunately, multiple retrospective studies have demonstrated worse median overall and progression free survival in patients with ACC that contains a NOTCH mutation [47,48,49]. While pre-clinical studies have demonstrated promise in targeting NOTCH as a potential treatment, this has not yet translated to clinical benefit. To date, there has been a single phase I clinical trial published regarding the use of NOTCH inhibitor Crenigacestat, which had limited clinical activity [50]. A phase II trial using AL101, an inhibitor of gamma secretase-mediated NOTCH signaling, has recently closed to accrual with results pending [51]. Tyrosine kinase inhibitors have also been investigated in the treatment of metastatic, recurrent, or progressive adenoid cystic carcinoma, with a 9–16% objective response rate observed with sorafenib, axitinib, and lenvatinib [46, 52,53,54,55,56,57], with one study of lenvatinib demonstrating a median progression-free survival of 17.5 months [56]. The sequencing and combination of these agents with RT if used in the curative setting remains an unanswered question to date.
Olfactory Neuroblastoma/Esthesioneuroblastoma
Esthesioneuroblastoma, also known as olfactory neuroblastoma, is a rare tumor that accounts for approximately 5% of sinonasal malignancies. It was first identified by Berger et al. in 1924 and arises from the neural crest cells of the olfactory epithelium located along the roof of the nasal cavity [58,59,60,61]. These tumors have a propensity for direct spread into the orbit, skull base, and/or intracranially and may present with nodal disease 5–12% of the time, with nodal levels I-III being the most commonly involved [62, 63].
ONB has its own unique staging systems, including the Kadish, modified Kadish, and Dulguerov staging methods [64,65,66]. Histologically, these tumors are graded using the Hyams grading system based on their degree of differentiation [67].
If resectable, surgery is the standard treatment modality upfront using either open (craniofacial) or endoscopic when feasible, or a combination of both techniques to try to achieve a gross total resection while preserving function. Small, low grade tumors may be treated by surgery alone without adjuvant treatment. Radiation with or without chemotherapy is primarily used in the adjuvant setting, with several studies showing improved outcomes with the addition of adjuvant RT compared to surgery alone [63, 68,69,70,71,72]. Radiation delivered in the adjuvant setting typically uses a dose of 60–66 Gy, with doses of 70 Gy being considered if there is gross residual disease or if radiation is the primary local treatment modality in unresectable patients. Elective nodal radiation (ENI) in ONB patients is a topic of controversy and still undergoing investigation, and perhaps should be considered especially in patients with adverse risk factors, such as Hyams grade 3–4 or Kadish C-D [73,74,75,76,77,78,79,80,81]. One recent analysis published in 2021 reported regional recurrence rates of 1.6% in clinically node negative patients who did receive ENI and 18.8% in those who did not receive ENI although this did not translate into an improvement in overall or distant-metastasis free survival [82]. Lymph node levels I-III and retropharyngeal nodes should be included as part of the treatment volume as the at risk regions if ENI is done as part of the treatment.
There is very limited prospective data available regarding the treatment of ONB; however, one study from MGH evaluated the use of induction chemotherapy followed by radiation therapy and additional chemotherapy. Patients received treatment with 2 cycles of chemotherapy, consisting of cisplatin (33 mg/m2 per day for 3 days) and etoposide (100 mg/m.2 per day for 3 days), every 2 weeks followed by MRI to assess treatment response. Those who had a good response proceeded to radiation therapy delivered over the course of 5 weeks, followed by 2 additional cycles of chemotherapy using the previously noted regiment. 19 patients were included in the study, with a median follow up of 45 months (range, 20–92 months), and 13 patients had some response to chemotherapy, with only 1 patient having progressive disease. Any response to chemotherapy was predictive of prolonged survival, with significant differences in overall and metastasis-free survival; however, this did not also translate into differences in local control. This was also one of the earliest studies exploring the use of proton RT in this group, with patients being treated with a combination of photon and proton RT to a dose of 68 Gy to the primary tumor pre-chemotherapy volume, with 48 Gy delivered in the morning with 3-D conformal photon RT and 20 Gy delivered in the afternoon using proton RT, separated by 7 h in between treatments. Patients received 45 Gy with photon RT to the bilateral neck, including supraclavicular nodes. Even in the use of mixed RT modalities, the authors report achieving higher radiation doses than those reported in the literature available at the time and noted lower rates of radiation related toxicities compared to historical controls, with no patient developing late visual loss or corneal ulceration. Five patients did develop significant late grade 2–3 complications that were at least partially attributable to radiation therapy, including radiation necrosis (4), soft tissue necrosis (1), and CSF leak with meningitis (1) [83].
The rare incidence of ONB makes identifying unique molecular or genetic markers that could serve as targets of systemic agents or provide additional prognostic information especially challenging. Similar to other cancers, high grade tumors tended to have more cytogenetic alterations than low grade tumors. The most common chromosomal alteration was loss of 3p, which has been shown to be associated with resistance to chemotherapy and RT in other tumor types. The most frequently mutated gene in ON was TP53, which has a loss of function mutation in approximately 50% of human cancers [84].
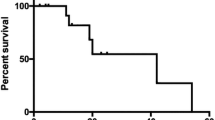
Outcomes of ONB patients have ranged from 40–70% local recurrence rate with 5-yr OS of 60–80%. One recent publication reporting on a single institutional experience from 1960–2020 consisting of 143 patients, reported a 5-year OS of 82.3%, with 5-year PFS of 51.6%, which had improved in the more modern area, defined as 2005-Present. Multivariate analysis identified Hyams grade (3 or 4), high modified Kadish stage (C or D), and increasing age as independent negative prognostic factors for overall survival, which is largely consistent with previous institutional or large database reviews [63]. Of note, due to its propensity to recur either locally or distantly even 5 years following treatment, it is important to monitor these patients closely in followup.
SNUC
Sinonasal undifferentiated carcinomas (SNUC) are a very rare tumor of the sinonasal region with a neuroendocrine cell of origin. Only a few hundred cases have been identified since first being described in 1986 by Frierson et al. These tumors are particularly aggressive, with patients often presenting late with skull base invasion and developing recurrences following treatment, with up to 30% of patients presenting with clinically positive adenopathy [85,86,87]. 5-year OS of 20–50% have been reported. Multimodality treatment is important in trying to provide the best possible outcome for these patients, with one meta-analysis of 390 patients demonstrating improved survival with double modality therapy (surgery and RT or RT and chemotherapy) compared to single modality treatment (surgery or RT) [88]. It has also been demonstrated that the dose of radiation delivered locally has an impact on outcomes, with an improvement in local control in patients who received > / = 60 Gy to the primary site/surgical bed (5-yr OS 73 vs 23%). The use of IMRT also demonstrated improved survival compared to patients who were treated with 2-D or 3-D conformal RT (5-yr OS 59% vs 16%), while also demonstrating a trend towards improvement in late toxicities [89]. ENI should be considered for these patients, with rates of regional relapse being much lower in those who did receive ENI vs those who did not (3.7% vs 26.4%).
Induction chemotherapy has also been an area of exploration in this group to help guide the selection of local therapies. In one study from MD Anderson that included 137 patients, those who had a good response to induction chemotherapy with cisplatin (60–80 mg/m2 on day 1) and etoposide (100–120 mg/m2) or docetaxel (75 mg/m2) on days 1 to 3 had improved survival when treated with definitive chemoradiation as opposed to definitive surgery followed by RT/chemoradiation (5-year DSS: 81% vs 54%). In patients who did not demonstrate response to chemotherapy, including 22 patients who had stable disease and 9 who had progression, surgery followed by RT or chemoRT provided significantly improved disease-specific survival and overall survival compared to non-responders who were treated with definitive chemoRT after induction [90]. Additionally, a study from Ohio State regarding their experience in utilizing induction chemotherapy using TPF (cisplatin, docetaxel, 5-FU) followed by concurrent chemoradiotherapy reported favorable outcomes in these patients, having no evidence of disease at an average follow up of 16.8 months [91]. This supports a nuanced approach that accounts for response to induction chemotherapy in determining the best definitive local treatment in these patients.
Studies have done to try to identify any molecular markers that may carry treatment or prognostic significance. SMARCB1 (INI-1, BAF47, or hSNF5) is a tumor suppressor gene that, when mutated, has been noted to carry a worse prognosis in other malignancies, such as rhabdoid tumors and epithelioid sarcomas, and this loss of function mutation has been seen in SNUCs as well [92,93,94,95]. In one study that included 14 patients with a SNUC diagnosis, 6 were noted to have a complete loss of SMRCB1 expression in tumor cells. Patients with the mutation were found to have worse recurrence and mortality rates, 75% vs 17% and 67% vs 14%, respectively [96]. Figures 1 and 2 demonstrate differing responses to induction chemotherapy leading to different definitive management strategies.
Radiation Treatment Planning
Target Delineation
While the exact pattern of spread for different histologies and for each anatomical subsite of the paranasal sinuses may vary, general concepts when delineating target volumes may be applied. In the setting of adjuvant radiation therapy, The primary high risk clinical target volume (CTV) receiving a dose of 60 Gy may include the primary tumor bed with a 3–5 mm margin, accounting for anatomical constraints. Some may consider a boost to 66–70 Gy for adverse features such as a positive margin or gross residual disease. A low risk CTV to a dose of 54 Gy may be used to cover additional at risk areas, such as the uninvolved neck when treating elective nodal volumes.
In the definitive setting, doses of 70 Gy are standardly used to target gross disease, or gross target volume (GTV). A high risk CTV is created by adding a 3–5 mm margin from the GTV; however, consideration of adjacent normal tissues should be taken when determining the margin and any appropriate adjustments. Particularly, for tumors abutting the brainstem, brain, or optic structures, a smaller margin may be utilized to protect these organs at risk. Intermediate and low risk CTVs are also used in the definitive setting, utilizing doses in the range of 63 Gy and 56 Gy, respectively, for each. An intermediate risk CTV includes pathways of predictable tumor spread concerning for microscopic disease and/or the involved neck nodal levels. A low risk CTV may be used for ENI to the uninvolved at risk nodal regions in the neck. When using IMRT, a 3 mm expansion is used for the planning target volume (PTV) to each treatment volume to account for daily set up variation. These expansions are utilized in the modern era of daily image guidance radiation therapy (IGRT) in both the definitive and post-op RT setting.
There are many important additional considerations when defining target volumes. Any diagnostic imaging, including CT, MRI, and PET-CT, should be fused to the planning CT to aid in target delineation. This should include all pre-surgical and/or pre-induction chemotherapy imaging as well. If possible, an MRI in treatment position done at the time of radiation simulation is also useful. A discussion with neuroradiology, especially if there is a question on if an area is disease versus post-operative changes, is beneficial as well. In the setting of adjuvant RT, a careful review of the surgical note with the operating surgeon is also important in ensuring appropriate target coverage.
Protons
Charged particle therapy, including the use of proton therapy, is one modern radiation therapy technique that provides dosimetric advantages to tumors in this location. Unlike traditional radiation therapy using photons, protons have a finite, energy-dependent range in tissue that results in energy deposition as the protons come to rest in the Bragg peak, with lower entrance dose than photons and a sharp dose fall off that also minimizes exit dose [97]. This provides the benefits of reducing the radiation dose to the surrounding non-target organs at risk (OARs) and allowing improved target coverage, potentially even escalating the dose, without exceeding OAR constraints [10, 22, 42, 98,99,100].
The characteristics of proton depth dose deposition requires them to pass through several centimeters of tissue prior to depositing dose, which may be challenging with tumors located in the sinonasal region. To combat this and still be able to deliver treatment safely and effectively, different external range shifting devices have been developed, with range shifting devices often being attached to the proton gantry head. The challenge of this approach is that while this dose help with shifting the effective dose more superficially, the spot size is increased, which increases the beam penumbra and OAR dose. This has led to the development of other range shifting devices that may be placed closer to the patient’s head, allowing the interaction between the range shifter and beam to be directly above the patient. One such device is the “bolus helmet” (BH), developed at the Mayo Clinic in Rochester, MN. Since it is directly above the patient, the spot size is reduced with a sharper beam penumbra, which improves target coverage while also decreasing dose to the surrounding OARs. One limitation of the BH is that due to the size, the neck is not covered, thus not allowing ENI to be done simultaneously [101]. Other groups have also developed different devices to assist in addressing maintaining spot size integrity, with the group from University of Pennsylvania publishing on their use of a U-shaped universal bolus (UB) with a water-equivalent thickness of 5.5 cm that provided proton plans with improved spot size compared to those plans done with the range-shifter [102].
When designing treatment plans with PT, an additional consideration is the relative biologic effective (RBE) dose, typically reported as a 1.1 dose enhancement; however, this can be quite higher at the end of range in the Bragg peak of the beam. Different institutions have varying methods of accounting for this when evaluating treatment plans. One such method is the utilization of an institutional GPU-based Monte Carlo calculation algorithm that calculates the biologic dose based on RBE and linear energy transfer considerations [103,104,105,106].
Due to the properties of protons, additional imaging verification may be needed throughout the course of RT to assess for anatomical changes, such as tumor shrinkage or patient weight loss. Protons are much more sensitive to changes in tissue density, and there may be substantial deviations from the original RT plan if the anatomy has changed. Weekly verification CT scans, in addition to daily IGRT, may be utilized to assess treatment response and aid in the decision of replanning RT to account for any anatomical changes.
Multiple studies have demonstrated the effectiveness and advantages of using proton therapy in this region, either as definitive treatment or in the adjuvant setting. In one of the largest studies evaluating the use of PT in the management of sinonasal tumors, outcomes of 69 patients treated with curative PT at multiple institutions were found to be favorable. In patients who received de novo PT, 3-year OS, freedom from distant metastasis, freedom from disease progression, and freedom from locoregional recurrence were 100%, 84.0%, 77.3%, and 92.9%, respectively [26]. Additionally, a meta-analysis of sinonasal malignancies demonstrated improved OS and DFS in patients who received proton therapy compared to photon therapy [107]. With respect to non-target tissues, proton RT has been shown to reduce the dose to these areas and provided a reduction in toxicity. In the previously mentioned multiinstitutional study, the toxicity profile of PT was also favorable, with 11/69 patients having acute grade 3 toxicities and no grade > / = 3 late toxicities, vision loss, or symptomatic brain necrosis. Additionally, one study directly comparing IMRT vs PT toxicity outcomes described a significant reduction in gastrostomy tube dependence and opioid pain medication requirements in patients with nasopharyngeal and paranasal sinus malignancies treated with PT compared to IMRT [10] (Fig. 3).
Proton and IMRT photon comparison plans in the treatment of a paranasal sinus malignancy. Prescription dose of 6996 cGy in 33 fractions. 20% isodose line as minimum and 115% as maximum in proton plan (a and b) and IMRT plan (c and d). 50% isodose line as minimum in proton (e and f) and IMRT (g and h) plans. 90% isodose line as minimum in proton (i and j) and IMRT (k and l) plans. 100% isodose line as minimum in proton (m and n) and IMRT (o and p) plans
Conclusion
Sinonasal malignancies represent a rare group of tumors with a challenging management. Tumors in this location may consist of a number of histologies, each with unique considerations for patterns of spread and recurrence that must be considered when determining the best treatment options. Multidisciplinary approach and multimodality treatment consisting of surgery, radiation, and/or chemotherapy is typically mandated in providing the best possible outcome for these patients. Advances in radiation therapy techniques, such as proton therapy, provide improved therapeutic ratios in enabling radiation oncologists the ability to maximize dose to the target area while minimizing the dose to surrounding organs at risk, with the hope of maximizing curative potential while reducing toxicity profiles.
Availability of Data and Materials
Not applicable.
References
Ayiomamitis A, Parker L, Havas T. The epidemiology of malignant neoplasms of the nasal cavities, the paranasal sinuses and the middle ear in Canada. Arch Otorhinolaryngol. 1988;244(6):367–71.
Batsakis JG, Rice DH, Solomon AR. The pathology of head and neck tumors: squamous and mucous-gland carcinomas of the nasal cavity, paranasal sinuses, and larynx, part 6. Head Neck Surg. 1980;2(6):497–508.
Turner JH, Reh DD. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck. 2012;34(6):877–85.
Danesh-Sani SA, et al. Paranasal sinuses malignancies: A 12-year review of clinical characteristics. Med Oral Patol Oral Cir Bucal. 2016;21(5):e626–30.
Chen NX, et al. A clinical study of multimodal treatment for orbital organ preservation in locally advanced squamous cell carcinoma of the nasal cavity and paranasal sinus. Jpn J Clin Oncol. 2016;46(8):727–34.
Jansen EP, et al. Does the combination of radiotherapy and debulking surgery favor survival in paranasal sinus carcinoma? Int J Radiat Oncol Biol Phys. 2000;48(1):27–35.
Lee MM, et al. Multimodality therapy in advanced paranasal sinus carcinoma: superior long-term results. Cancer J Sci Am. 1999;5(4):219–23.
Resto VA, et al. Extent of surgery in the management of locally advanced sinonasal malignancies. Head Neck. 2008;30(2):222–9.
Guan X, et al. Lymph node metastasis in sinonasal squamous cell carcinoma treated with IMRT/3D-CRT. Oral Oncol. 2013;49(1):60–5.
McDonald MW, et al. Acute toxicity in comprehensive head and neck radiation for nasopharynx and paranasal sinus cancers: cohort comparison of 3D conformal proton therapy and intensity modulated radiation therapy. Radiat Oncol. 2016;11:32.
Russo AL, et al. Long-term outcomes after proton beam therapy for sinonasal squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2016;95(1):368–76.
Cantu G, et al. Lymph node metastases in malignant tumors of the paranasal sinuses: prognostic value and treatment. Arch Otolaryngol Head Neck Surg. 2008;134(2):170–7.
Jiang GL, et al. Maxillary sinus carcinomas: natural history and results of postoperative radiotherapy. Radiother Oncol. 1991;21(3):193–200.
Kim GE, et al. Clinical significance of neck node metastasis in squamous cell carcinoma of the maxillary antrum. Am J Otolaryngol. 1999;20(6):383–90.
Stelow EB. Human papillomavirus-related head and neck squamous cell carcinoma. Cancer Cytopathol. 2013;121(11):599–600.
Stelow EB, Bishop JA. Update from the 4th edition of the world health organization classification of head and neck tumours: Tumors of the Nasal Cavity, paranasal sinuses and skull base. Head Neck Pathol. 2017;11(1):3–15.
Agarwal A, Philips R, Chitguppi C, Gargano S, Sahin Z, Curry J, Luginbuhl A, Cognetti D, Toskala E, Rabinowitz MR, Rosen MR, Nyquist GG. Effect of p16 status on survival outcomes in sinonasal squamous cell carcinoma. Ann Otol Rhinol Laryngol. 2023;132(8):917–25. https://doi.org/10.1177/00034894221121401. Epub 2022 Aug 29. PMID: 36031858.
Robin TP, et al. A comprehensive comparative analysis of treatment modalities for sinonasal malignancies. Cancer. 2017;123(16):3040–9.
Al-Mamgani A, et al. Highly-conformal intensity-modulated radiotherapy reduced toxicity without jeopardizing outcome in patients with paranasal sinus cancer treated by surgery and radiotherapy or (chemo)radiation. Oral Oncol. 2012;48(9):905–11.
Wiegner EA, et al. Intensity-modulated radiotherapy for tumors of the nasal cavity and paranasal sinuses: clinical outcomes and patterns of failure. Int J Radiat Oncol Biol Phys. 2012;83(1):243–51.
Daly ME, et al. Intensity-modulated radiation therapy for malignancies of the nasal cavity and paranasal sinuses. Int J Radiat Oncol Biol Phys. 2007;67(1):151–7.
Fan M, et al. Outcomes and toxicities of definitive radiotherapy and reirradiation using 3-dimensional conformal or intensity-modulated (pencil beam) proton therapy for patients with nasal cavity and paranasal sinus malignancies. Cancer. 2020;126(9):1905–16.
Toyomasu Y, et al. Outcomes of patients with sinonasal squamous cell carcinoma treated with particle therapy using protons or carbon ions. Int J Radiat Oncol Biol Phys. 2018;101(5):1096–103.
Dagan R, et al. Outcomes of sinonasal cancer treated with proton therapy. Int J Radiat Oncol Biol Phys. 2016;95(1):377–85.
Zenda S, et al. Proton beam therapy for unresectable malignancies of the nasal cavity and paranasal sinuses. Int J Radiat Oncol Biol Phys. 2011;81(5):1473–8.
Yu NY, et al. A multi-institutional experience of proton beam therapy for sinonasal tumors. Adv Radiat Oncol. 2019;4(4):689–98.
Biau J, et al. Selection of lymph node target volumes for definitive head and neck radiation therapy: a 2019 Update. Radiother Oncol. 2019;134:1–9.
Gregoire V, et al. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol. 2014;110(1):172–81.
Bristol IJ, et al. Postoperative radiotherapy for maxillary sinus cancer: long-term outcomes and toxicities of treatment. Int J Radiat Oncol Biol Phys. 2007;68(3):719–30.
Allen MW, et al. Long-term radiotherapy outcomes for nasal cavity and septal cancers. Int J Radiat Oncol Biol Phys. 2008;71(2):401–6.
Chen AM, et al. Carcinomas of the paranasal sinuses and nasal cavity treated with radiotherapy at a single institution over five decades: are we making improvement? Int J Radiat Oncol Biol Phys. 2007;69(1):141–7.
Hoppe BS, et al. Treatment of nasal cavity and paranasal sinus cancer with modern radiotherapy techniques in the postoperative setting–the MSKCC experience. Int J Radiat Oncol Biol Phys. 2007;67(3):691–702.
Barnes L. Intestinal-type adenocarcinoma of the nasal cavity and paranasal sinuses. Am J Surg Pathol. 1986;10(3):192–202.
Leivo I. Sinonasal adenocarcinoma: update on classification, immunophenotype and molecular features. Head Neck Pathol. 2016;10(1):68–74.
Thompson LDR, Franchi A. New tumor entities in the 4th edition of the World Health Organization classification of head and neck tumors: Nasal cavity, paranasal sinuses and skull base. Virchows Arch. 2018;472(3):315–30.
Duprez F, et al. IMRT for sinonasal tumors minimizes severe late ocular toxicity and preserves disease control and survival. Int J Radiat Oncol Biol Phys. 2012;83(1):252–9.
Lund VJ, et al. Evidence for treatment strategies in sinonasal adenocarcinoma. Head Neck. 2012;34(8):1168–78.
Heffner DK, et al. Low-grade adenocarcinoma of the nasal cavity and paranasal sinuses. Cancer. 1982;50(2):312–22.
Fordice J, et al. Adenoid cystic carcinoma of the head and neck: predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg. 1999;125(2):149–52.
Lupinetti AD, et al. Sinonasal adenoid cystic carcinoma: the M. D. Anderson Cancer Center experience. Cancer. 2007;110(12):2726–31.
Bakst RL, et al. Perineural invasion and perineural tumor spread in head and neck cancer. Int J Radiat Oncol Biol Phys. 2019;103(5):1109–24.
Dagan R, et al. Long-term outcomes from proton therapy for sinonasal cancers. Int J Part Ther. 2021;8(1):200–12. This article demonstrates the safety and efficacy of proton radiation therapy in the treatment of sinonasal malignancies, with respect to both overall survival and long-term local control.
Miller ED, et al. Sinonasal adenoid cystic carcinoma: Treatment outcomes and association with human papillomavirus. Head Neck. 2017;39(7):1405–11.
Ebner DK, et al. The role of particle therapy in adenoid cystic carcinoma and mucosal melanoma of the head and neck. Int J Part Ther. 2021;8(1):273–84.
Pelak MJ, et al. Clinical outcomes of head and neck adenoid cystic carcinoma patients treated with pencil beam-scanning proton therapy. Oral Oncol. 2020;107: 104752.
Sahara S, Herzog AE, Nor JE. Systemic therapies for salivary gland adenoid cystic carcinoma. Am J Cancer Res. 2021;11(9):4092–110.
Ferrarotto R, et al. Activating NOTCH1 mutations define a distinct subgroup of patients with adenoid cystic carcinoma who have poor prognosis, propensity to bone and liver metastasis, and potential responsiveness to notch1 inhibitors. J Clin Oncol. 2017;35(3):352–60.
Atallah S, et al. Beyond surgical treatment in adenoid cystic carcinoma of the head and neck: a literature review. Cancer Manag Res. 2022;14:1879–90.
Feeney L, et al. Clinical disease course and survival outcomes following disease recurrence in adenoid cystic carcinoma with and without NOTCH signaling pathway activation. Oral Oncol. 2022;133: 106028.
Even C, et al. Safety and clinical activity of the Notch inhibitor, crenigacestat (LY3039478), in an open-label phase I trial expansion cohort of advanced or metastatic adenoid cystic carcinoma. Invest New Drugs. 2020;38(2):402–9.
Ferrarotto R, et al. AL101, a gamma-secretase inhibitor, has potent antitumor activity against adenoid cystic carcinoma with activated NOTCH signaling. Cell Death Dis. 2022;13(8):678.
Ho AL, et al. A phase II study of axitinib (AG-013736) in patients with incurable adenoid cystic carcinoma. Ann Oncol. 2016;27(10):1902–8.
Locati LD, et al. Phase II trial with axitinib in recurrent and/or metastatic salivary gland cancers of the upper aerodigestive tract. Head Neck. 2019;41(10):3670–6.
Locati LD, et al. Patients with adenoid cystic carcinomas of the salivary glands treated with lenvatinib: Activity and quality of life. Cancer. 2020;126(9):1888–94.
Locati LD, et al. A phase II study of sorafenib in recurrent and/or metastatic salivary gland carcinomas: Translational analyses and clinical impact. Eur J Cancer. 2016;69:158–65.
Tchekmedyian V, et al. Phase II study of lenvatinib in patients with progressive, recurrent or metastatic adenoid cystic carcinoma. J Clin Oncol. 2019;37(18):1529–37.
Thomson DJ, et al. Phase II trial of sorafenib in advanced salivary adenoid cystic carcinoma of the head and neck. Head Neck. 2015;37(2):182–7.
Arnold MA, Farnoosh S, Gore MR. Comparing kadish and modified dulguerov staging systems for olfactory neuroblastoma: an individual participant data meta-analysis. Otolaryngol Head Neck Surg. 2020;163(3):418–27.
Marinelli JP, et al. Esthesioneuroblastoma with distant metastases: Systematic review & meta-analysis. Head Neck. 2018;40(10):2295–303.
Marinelli JP, et al. Dural invasion predicts the laterality and development of neck metastases in esthesioneuroblastoma. J Neurol Surg B Skull Base. 2018;79(5):495–500.
Jethanamest D, et al. Esthesioneuroblastoma: a population-based analysis of survival and prognostic factors. Arch Otolaryngol Head Neck Surg. 2007;133(3):276–80.
Gore MR, Zanation AM. Salvage treatment of late neck metastasis in esthesioneuroblastoma: a meta-analysis. Arch Otolaryngol Head Neck Surg. 2009;135(10):1030–4.
McMillan RA, et al. Long-term oncologic outcomes in esthesioneuroblastoma: an institutional experience of 143 patients. Int Forum Allergy Rhinol. 2022;12(12):1457–67. This study is one of the larger studies reporting on long-term outcomes in esthesioneuroblastoma patients and provides information on factors associated with more favorable survival outcomes.
Foote RL, et al. Esthesioneuroblastoma: the role of adjuvant radiation therapy. Int J Radiat Oncol Biol Phys. 1993;27(4):835–42.
Kadish S, Goodman M, Wang CC. Olfactory neuroblastoma. A clinical analysis of 17 cases. Cancer. 1976;37(3):1571–6.
Dulguerov P, Calcaterra T. Esthesioneuroblastoma: the UCLA experience 1970–1990. Laryngoscope. 1992;102(8):843–9.
Michaels L, Hyams VJ. Objectivity in the classification of tumours of the nasal epithelium. Postgrad Med J. 1975;51(600):695–707.
Miller KC, et al. Induction therapy prior to surgical resection for patients presenting with locally advanced esthesioneuroblastoma. J Neurol Surg B Skull Base. 2021;82(Suppl 3):e131–7.
Miller KC, et al. Utility of adjuvant chemotherapy in patients receiving surgery and adjuvant radiotherapy for primary treatment of esthesioneuroblastoma. Head Neck. 2019;41(5):1335–41.
Orton A, et al. Esthesioneuroblastoma: a patterns-of-care and outcomes analysis of the national cancer database. Neurosurgery. 2018;83(5):940–7.
Ow TJ, et al. Esthesioneuroblastoma. Neurosurg Clin N Am. 2013;24(1):51–65.
Su SY, et al. Outcomes for olfactory neuroblastoma treated with induction chemotherapy. Head Neck. 2017;39(8):1671–9.
Banuchi VE, et al. Patterns of regional and distant metastasis in esthesioneuroblastoma. Laryngoscope. 2016;126(7):1556–61.
Demiroz C, et al. Esthesioneuroblastoma: is there a need for elective neck treatment? Int J Radiat Oncol Biol Phys. 2011;81(4):e255–61.
Jiang W, et al. The role of elective nodal irradiation for esthesioneuroblastoma patients with clinically negative neck. Pract Radiat Oncol. 2016;6(4):241–7.
Noh OK, et al. Radiotherapy for esthesioneuroblastoma: is elective nodal irradiation warranted in the multimodality treatment approach? Int J Radiat Oncol Biol Phys. 2011;79(2):443–9.
Peacock JG, et al. Risk of delayed lymph node metastasis in clinically N0 esthesioneuroblastoma. J Neurol Surg B Skull Base. 2017;78(1):68–74.
Rinaldo A, et al. Esthesioneuroblastoma and cervical lymph node metastases: clinical and therapeutic implications. Acta Otolaryngol. 2002;122(2):215–21.
Sun M, et al. Long-term analysis of multimodality treatment outcomes and prognosis of esthesioneuroblastomas: a single center results of 138 patients. Radiat Oncol. 2020;15(1):219.
Van Gompel JJ, et al. Long-term outcome of esthesioneuroblastoma: hyams grade predicts patient survival. J Neurol Surg B Skull Base. 2012;73(5):331–6.
Wolfe AR, et al. Clinical outcomes and multidisciplinary patterns of failure for olfactory neuroblastoma: The Ohio State experience. J Neurol Surg B Skull Base. 2020;81(3):287–94.
De Virgilio A, et al. Elective neck irradiation in the management of esthesioneuroblastoma: a systematic review and meta-analysis. Rhinology. 2021;59(5):433–40.
Fitzek MM, et al. Neuroendocrine tumors of the sinonasal tract. Results of a prospective study incorporating chemotherapy, surgery, and combined proton-photon radiotherapy. Cancer. 2002;94(10):2623–34.
Kaur RP, et al. The genomics and epigenetics of olfactory neuroblastoma: a systematic review. Laryngoscope Investig Otolaryngol. 2021;6(4):721–8.
Frierson HF Jr, et al. Sinonasal undifferentiated carcinoma An aggressive neoplasm derived from schneiderian epithelium and distinct from olfactory neuroblastoma. Am J Surg Pathol. 1986;10(11):771–9.
Levine PA, et al. Sinonasal undifferentiated carcinoma: a distinctive and highly aggressive neoplasm. Laryngoscope. 1987;97(8 Pt 1):905–8.
Mendenhall WM, et al. Sinonasal undifferentiated carcinoma. Am J Clin Oncol. 2006;29(1):27–31.
Mourad WF, et al. Trimodality management of sinonasal undifferentiated carcinoma and review of the literature. Am J Clin Oncol. 2013;36(6):584–8.
Gamez ME, et al. Outcomes and patterns of failure for sinonasal undifferentiated carcinoma (SNUC): The Mayo Clinic Experience. Head Neck. 2017;39(9):1819–24.
Amit M, et al. Induction chemotherapy response as a guide for treatment optimization in sinonasal undifferentiated carcinoma. J Clin Oncol. 2019;37(6):504–12.
London NR Jr, et al. Sinonasal undifferentiated carcinoma: Institutional trend toward induction chemotherapy followed by definitive chemoradiation. Head Neck. 2020;42(11):3197–205.
Agaimy A, et al. SMARCB1 (INI-1)-deficient sinonasal carcinoma: a series of 39 cases expanding the morphologic and clinicopathologic spectrum of a recently described entity. Am J Surg Pathol. 2017;41(4):458–71.
Dogan S, et al. Frequent IDH2 R172 mutations in undifferentiated and poorly-differentiated sinonasal carcinomas. J Pathol. 2017;242(4):400–8.
Dogan S, et al. Genetic basis of SMARCB1 protein loss in 22 sinonasal carcinomas. Hum Pathol. 2020;104:105–16.
Laco J, et al. SMARCB1/INI1-deficient sinonasal carcinoma shows methylation of RASSF1 gene: a clinicopathological, immunohistochemical and molecular genetic study of a recently described entity. Pathol Res Pract. 2017;213(2):133–42.
Chitguppi C, et al. Loss of SMARCB1 expression confers poor prognosis to sinonasal undifferentiated carcinoma. J Neurol Surg B Skull Base. 2020;81(6):610–9.
Suit H, et al. Proton beams to replace photon beams in radical dose treatments. Acta Oncol. 2003;42(8):800–8.
Lomax AJ, Goitein M, Adams J. Intensity modulation in radiotherapy: photons versus protons in the paranasal sinus. Radiother Oncol. 2003;66(1):11–8.
Mock U, et al. Treatment planning comparison of conventional, 3D conformal, and intensity-modulated photon (IMRT) and proton therapy for paranasal sinus carcinoma. Int J Radiat Oncol Biol Phys. 2004;58(1):147–54.
van de Water TA, et al. The potential benefit of radiotherapy with protons in head and neck cancer with respect to normal tissue sparing: a systematic review of literature. Oncologist. 2011;16(3):366–77.
Larsen K, et al. Case study of a bolus helmet used to maintain optic chiasm and nerve sparing while improving target coverage using IMPT. Med Dosim. 2022;47(3):242–6.
Both S, et al. Development and clinical implementation of a universal bolus to maintain spot size during delivery of base of skull pencil beam scanning proton therapy. Int J Radiat Oncol Biol Phys. 2014;90(1):79–84.
Beltran C, et al. Clinical implementation of a proton dose verification system utilizing a GPU accelerated monte carlo engine. Int J Part Ther. 2016;3(2):312–9.
Ma J, et al. A GPU-accelerated and Monte Carlo-based intensity modulated proton therapy optimization system. Med Phys. 2014;41(12): 121707.
Pepin MD, et al. A Monte-Carlo-based and GPU-accelerated 4D-dose calculator for a pencil beam scanning proton therapy system. Med Phys. 2018;45(11):5293–304.
Tseung Wan Chan, H., J. Ma, and C. Beltran,. A fast GPU-based Monte Carlo simulation of proton transport with detailed modeling of nonelastic interactions. Med Phys. 2015;42(6):2967–78.
Patel SH, et al. Charged particle therapy versus photon therapy for paranasal sinus and nasal cavity malignant diseases: a systematic review and meta-analysis. Lancet Oncol. 2014;15(9):1027–38.
Funding
None.
Author information
Authors and Affiliations
Contributions
K.Q. wrote the main manuscript text. M.G., S.P., and C.C. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not required.
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiements with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsink declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qualls, K.W., Patel, S.H., Coddington, C.A. et al. Paranasal Sinus Malignances: Advances in Radiation Treatment Strategies. Curr Otorhinolaryngol Rep (2024). https://doi.org/10.1007/s40136-024-00508-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s40136-024-00508-2