Abstract
Purpose of Review
Review current evidence-based treatment outcomes and future management directions for children with obstructive sleep apnea (OSA).
Recent Findings
Effective medical therapies include weight loss, leukotriene modifiers, nasal corticosteroids, oral appliances, and positive airway pressure. The first randomized controlled trials for adenotonsillectomy in childhood OSA show improved polysomnography results but no postoperative change in neurocognitive outcomes when compared to watchful waiting. Factors have been identified (e.g., craniofacial disorders and obesity) which can lead to decreased adenotonsillectomy success. The tongue base and supraglottis are common additional sites of obstruction, and supraglottoplasty and lingual tonsillectomy are commonly performed procedures for persistent OSA. Additional surgical targets include the nasal cavity, palate/pharynx, tongue base, and larynx.
Summary
The management of pediatric OSA is multidisciplinary and includes a variety of medical and surgical therapies. Although adenotonsillectomy remains first-line treatment, favorable outcomes exist for nonsurgical modalities. In children with persistent OSA after adenotonsillectomy, several procedures exist to address additional obstruction, but further investigation to delineate their appropriate indications is warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstruction sleep apnea (OSA) is characterized by episodes of partial or complete upper airway obstruction leading to reduced or absent airflow with consequent arousals and/or oxygen desaturations. For children, OSA prevalence ranges from 1.2 to 5.7% [1••]. The management of pediatric OSA is diverse and includes behavioral modifications, medical devices, pharmaceuticals agents, and surgical procedures. This review aims to summarize the most up-to-date evidence regarding management of pediatric OSA.
Medical Management
Weight Loss
While adults typically have residual mild to moderate OSA after weight loss, children are more likely to have complete resolution of OSA. A recent systematic review and meta-analysis of multidisciplinary weight loss interventions in youth with obesity revealed significant improvement in OSA, including a reduction in apnea-hypopnea index (AHI) of − 0.51 (95% CI: − 0.94 to − 0.08), oxygen desaturation index (ODI) of − 0.28 (95% CI: − 0.50 to − 0.05), as well as improved sleep duration. Towards this end, the 2018 Bariatric Surgery Guidelines from the American Society for Metabolic and Bariatric Surgery (MBS) Pediatric Committee state that MBS is indicated for adolescents with BMI ≥ 35 kg/m2 or 120% of the 95th percentile with clinical significant comorbidities, such as OSA with AHI > 5 [2]. While the outcomes of bariatric surgery for adolescents are still under investigation, Kalra et al. demonstrated a decrease in median AHI from 9.1 to 0.65 events/hour in ten extremely overweight adolescents who underwent bariatric surgery after a mean weight loss of 58 kg [3]. A 2019 study showed that OSA severity may improve early and disproportionately with weight loss after bariatric surgery in adolescents, with a 60% decline in AHI with only a 5–6% weight loss in 7 at 3 weeks after surgery [4]. In addition to polysomnography (PSG) parameters, this unique study also showed a median decrease of 9% in systolic blood pressure, along with a concomitant rise in orexin and decrease in leptin levels compared to baseline measures. These small-scale results represent an initial look at the effect of bariatric surgery on OSA severity as determined by PSG results as well as downstream metabolic and physiologic changes. Finally, weight loss has also been shown to lower positive airway pressure (PAP) requirements and increase compliance in children with OSA [5].
Oral Appliances and Positional Sleep Devices
Maxillofacial anomalies and malocclusion issues contribute to pediatric OSA, and oral appliances are recommended for patients with mild to moderate OSA. Modified monobloc oral appliances have been worn with good compliance over a 6-month treatment period and subjectively improve sleep symptoms in children 4–8 years old [6, 7]. A recent meta-analysis found that mandibular advancement appliances were effective for mild to severe pediatric OSA patients with a mean difference in AHI of − 1.75 (95%CI: − 1.44 to − 2.07) with long-term treatment, defined as at least 6 months, more effective than short-term treatment [8•]. Maxillary expansion devices, which are adjusted over time to flatten and increase the width of the maxilla, thus widening the nasal vault and oral cavity space, have also demonstrated good outcomes in the appropriate patient population. Camacho et al. performed a meta-analysis encompassing 314 children with transverse maxillary deficiency who underwent rapid maxillary expansion with improvements in AHI and oxygen saturation nadir in both short-term (< 3 years) and long-term (12 years) follow-ups [9•]. Oral appliances have also improved PAP compliance [10]; however, as they both exert prolonged mechanical forces on the facial skeleton, further craniofacial deformities are a risk.
Positional OSA occurs frequently in children with studies reporting rates of 19% overall and 58% in children with obesity [11, 12]. Specialized pillows, clothing, belts, and vibratory devices have shown good results in a subset of adult patients who have positional sleep apnea [11,12,13], but outcomes data in the pediatric population are lacking.
Medication
Leukotriene modifiers, intranasal corticosteroids, and combination therapy have shown varying degrees of success in the treatment of pediatric OSA. A recent meta-analysis, encompassing a total of 668 children, demonstrated that montelukast alone imparted a 55% improvement in AHI (6.2 to 2.8 events/hour) and that montelukast combined with intranasal steroids produced a 70% improvement in AHI (4.7 to 1.4 events/hour) in 502 children [14••]. Yang et al. showed that montelukast and intranasal mometasone when used individually and in combination all resulted in symptom improvement on telephone questionnaires, increased oxygen saturation nadir, and decreased AHI, with a shortened response duration in the combination group [15]. Medical treatment also has a role in the treatment of persistent pediatric OSA following surgery. Several studies demonstrated that children with mild OSA after adenotonsillectomy who received either montelukast alone or montelukast combined with intranasal budesonide had improved AHI, oxygen saturation, and subjective symptom scores when compared to a control group [16, 17•].
Positive Airway Pressure
Continuous positive airway pressure (CPAP) has been approved for pediatric OSA since 2006 and is commonly used in children for whom surgery is contraindicated or as an adjunctive therapy in children with persistent OSA following adenotonsillectomy. It is generally delivered via a nasal or full-face mask and has been demonstrated to produce improvements in objective sleep outcomes and subjective symptoms. In a prospective, multicenter study, Marcus et al. showed that PAP therapy produced robust results with a reduction in AHI from 27 to 3 events/hour, an improvement in oxygen saturation nadir from 77 to 89%, and subjective improvement in daytime sleepiness [18]. Although PAP can produce dramatic improvements in disease severity, this study also revealed that adherence is a significant issue in children as approximately one-third of the cohort stopped using PAP before 6 months. Moreover, there are concerns that prolonged PAP use in children may increase the risk of skin and/or midface flattening [19].
Surgical Management
Adenotonsillectomy
Regarded as first-line treatment for pediatric OSA, adenotonsillectomy resulted in a 79% normalization rate for the AHI in children with OSA when compared to those who underwent watchful waiting in the first multicenter, randomized, controlled childhood adenotonsillectomy trial (CHAT) [20••]. A number of observational studies [21,22,23] have suggested that children with OSA may suffer from downstream consequences like neurocognitive dysfunction; however, both CHAT and the recent Preschool Obstructive Sleep Apnea Tonsillectomy and Adenoidectomy (POSTA) study of children aged 3 to 5 years with mild OSA showed no significant cognitive benefit in the adenotonsillectomy group when compared to the nonsurgical group [20••, 24••]. Future studies with a more diverse population, longer follow-up period, and including children with severe OSA and ADHD are needed to further elucidate the long-term neuropsychiatric effects of adenotonsillectomy. In addition to PSG results and neurocognitive function, downstream cardiovascular effects of adenotonsillectomy for pediatric OSA are still under investigation [25•].
Partial (intracapsular, subtotal) tonsillectomy or tonsillotomy is also associated with similar short-term rates of subjective symptom improvements and PSG changes compared to total tonsillectomy, with decreased risk for complications, including postoperative pain, poor oral intake, and hemorrhage. However, partial tonsillectomy has been shown to have a higher risk of symptom recurrence when compared to total tonsillectomy (4.5% vs. 2.6%) [26•]. In addition, mostly short-term studies of the risk of tonsil regrowth have been reported to range from 0.5 to 17% [27].
Adenoidectomy
Adenoidectomy alone may be appropriate for the treatment of pediatric OSA when the palatine tonsils are small and adenoid tissue is enlarged and obstructive on nasopharyngoscopy or lateral neck radiography. Domany et al. retrospectively evaluated adenoidectomy alone vs. adenotonsillectomy in 515 consecutive children with moderate to severe OSA; they found no difference in failure rate between the groups in non-obese children with AHI < 10 and small tonsils (< 3+) [28]. Another 2020 retrospective study of adenoidectomy alone in children under 3.5 years of age with large (3+ and 4+) adenoids and small (1+ and 2+) tonsils showed a decrease in mean AHI of 3.2 events/hour, with a 23% rate of complete PSG normalization, and a reduction in the prevalence of moderate to severe OSA from 65.4 to 30.8% (P = .03) [29]. At an average of 12 months following adenoidectomy, 14.1% of children, primarily the younger patients (1.5 vs. 2 years old), underwent tonsillectomy.
Persistent Disease After Adenotonsillectomy
The success rate of adenotonsillectomy for pediatric OSA is generally robust but can be low in select patient populations, such as those with obesity, black race, severe OSA, craniofacial abnormalities, Down syndrome, and neuromuscular disorders [30,31,32,33,34]. One systematic review of children with Down syndrome from 2017 showed that although adenotonsillectomy is associated with an improvement in PSG outcomes, the majority of children had persistent OSA after adenotonsillectomy and did not improve as much as nonsyndromic children did after surgery [35•].
Assessments of children with suspected persistent OSA following adenotonsillectomy include a detailed history and physical exam, PSG, and quality of life assessments. Additional diagnostic modalities, such as drug-induced sleep endoscopy (DISE) or cine magnetic resonance imaging (MRI), can be considered to identify areas of upper airway obstruction and potential surgical targets [36,37,38]. A 2021 published expert consensus statement recommends the use of DISE for children with persistent OSA prior to performing additional surgery as well as for concurrent DISE with adenotonsillectomy in children at high risk of persistent OSA [39]. Finally, shared decision making is recommended with a multidisciplinary approach to optimize the management of persistent OSA. Options for treatment include observation, lifestyle modifications, medical management, and surgical therapy. If multilevel surgery is undertaken, a staged approach or modifications may be considered to avoid scarring that narrows the oropharyngeal aperture or results in tongue base or pharyngeal stenosis.
Nasal Surgery
Surgeries that address nasal obstruction in children with OSA include inferior turbinate hypertrophy and septoplasty. While adult literature often notes that nasal surgery is not directly associated with resolution of OSA, it is recognized that these surgeries can improve nasal patency and aid in patient compliance, as well as reduce therapeutic levels for PAP therapy [40]. A meta-analysis of the impact of OSA on nasal surgery (based on 2 studies) noted that nasal surgery can result in an improvement of 11 events/hour [41]. While this change in adults is not typically enough to resolve OSA in adults, its impact on children is not well studied. In addition, there is currently little literature regarding the effect of septoplasty in the management of pediatric OSA. In children with nasal obstruction and inferior turbinate hypertrophy, turbinate reduction has been studied in conjunction with adenotonsillectomy and was associated with a larger decrease in postoperative AHI, as well as improved symptoms scores, and daytime function when compared to children who underwent adenotonsillectomy alone [42, 43].
Palate Surgery
Historically, uvulopalatopharyngoplasty (UPPP), which shortens the palate in order to improve anterior-posterior collapse, was the primary procedure used to address palatal obstruction in OSA, with documented improvements in PSG parameters [44, 45]. For both adults and children, expansion sphincter pharyngoplasty (ESP) has evolved to become the technique of choice for children with lateral pharyngeal collapse. This technique consists of rearrangement of palatal musculature (primarily the palatopharyngeus) intended to address posterior and lateral pharyngeal collapse. Outcomes of ESP in children are limited, but one study showed that children with severe OSA and lateral pharyngeal wall collapse who underwent ESP had reduced postoperative AHI (2.4 vs. 6.2) and greater cure rates when compared to children who underwent adenotonsillectomy alone (64% vs. 8%) [46].
Tongue Base Surgery
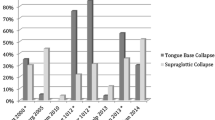
With rates ranging from 35 to 85%, tongue base obstruction is one of the most commonly identified sources of obstruction in children with persistent OSA following adenotonsillectomy [31, 36, 38, 47•]. In particular, children with Down syndrome have been found to have a significantly higher rate of lingual tonsil hypertrophy when compared to nonsyndromic children [48]. Multiple surgical procedures have been described to address obstruction at the level of the tongue, including lingual tonsillectomy, posterior midline glossectomy, tongue base ablation, tongue-lip adhesion, genioglossus advancement, tongue suspension, and hyoid suspension.
Lingual tonsillectomy is the most common tongue surgery performed in children with persistent OSA following adenotonsillectomy [49•]. There are several studies that support the efficacy of lingual tonsillectomy in children with persistent OSA, with one 2017 meta-analysis that calculated a success (AHI < 5 events/hour) rate of 52% and a mean AHI reduction of 6.6 events/hour [50•]. Complications following lingual tonsillectomy are reported to be similar to those seen after adenotonsillectomy and include poor oral intake, dehydration, bleeding, and postoperative pain [51].
For children evaluated with flexible endoscopy, lingual tonsil size may be overestimated, especially when there is a prominent tongue base underneath a thin layer of lingual tonsil tissue. In these cases, a posterior midline glossectomy (PMG), which can be performed using a number of different techniques, is considered in addition to a lingual tonsillectomy. Propst et al. demonstrated a reduction in postoperative AHI from 47 to 5.6 events/hour in non-obese children with Down syndrome who underwent lingual tonsillectomy and PMG [52]. This study was underpowered to assess differences by obesity status as it only included 13 children, but they found that obese children were not likely to have improvement after PMG. Another study of 10 children who underwent combined lingual tonsillectomy and tongue base reduction reported a reduction in postoperative AHI but complete resolution of OSA was only observed in children with normal weight [53]. Further study is warranted in this area.
Studies regarding outcomes of less commonly utilized tongue surgeries, such as suspension procedures and tongue-lip adhesion, are limited. One study of tongue suspension in combination reported that a success (AHI < 5 events/hour) rate of 61% in 31 patients following tongue base ablation and suspension [54]. Alternatively, tongue-lip adhesion has been shown to be effective in improving AHI, oxygen saturation nadir, hypercarbia, as well as bradycardia in children with Pierre Robin sequence; however, residual OSA is often reported [55,56,57]. Finally, published literature on the efficacy of procedures such as genioglossus advancement and hyoid suspension for pediatric OSA is limited to case reports and has not been reported for solo procedures.
Hypoglossal Nerve Stimulation
Hypoglossal nerve stimulation in children with Down syndrome and OSA is currently under investigation. Preliminary results from 20 patients in this population are promising and show a reduction in postoperative, titrated AHI of 85% from a median of 24 to 3 events/hour [58•, 59]. Median nightly usage across all participants was 9.2 h/night between the initial 1-month postoperative PSG titration and the 2-month PSG titration. Study participants also demonstrated an improvement in OSA-related quality of life as measured by the OSA-18, with a median score change of 1.2 [58•, 60]. Two participants experienced adverse events requiring revision surgery without long-term deleterious consequences. In one patient, there was extrusion of the stimulation lead, which required wound exploration and reimplantation. In the second patient, there was poor connectivity at the time of device activation, and wound exploration was carried out to perform device adjustments.
Laryngeal Surgery
Prolapse of the epiglottis and/or laryngomalacia can contribute to pediatric OSA and may be reliably identified on endoscopy and addressed with epiglottopexy and/or supraglottoplasty. There are limited outcomes studies on epiglottopexy, which involves de-mucosalizing the lingual surface of the epiglottis and either suturing or allowing it to scar to the tongue base. One recent study by Zalzal et al. demonstrated a success (AHI < 5 events/hour) rate of 53.6% in 28 children who underwent either epiglottopexy alone or epiglottopexy with division of the aryepiglottic folds [61].
Sleep state-dependent laryngomalacia or occult laryngomalacia can lead to persistent OSA and present beyond infancy. It is characterized by profound arytenoid redundancy and prolapse, as well as a retroflexed or omega-shaped epiglottis. In a 2015 systematic review of sites of obstruction in persistent pediatric OSA, supraglottoplasty was the second most common procedure reported in the literature for OSA following adenotonsillectomy. A systematic review and meta-analysis conducted in 2015 showed that supraglottoplasty in 64 patients with sleep state-dependent laryngomalacia resulted in a decrease in AHI from 14.0 to 3.3 events/hour [62•]. In 74 patients with congenital laryngomalacia, AHI decreased from 20.4 to 4.0 events/hour. Similarly, a 2019 retrospective case series of 41 children with laryngomalacia who underwent supraglottoplasty showed an improvement in AHI from 26.3 to 7.3 events/hour [63]. Earlier studies from 2012 on supraglottoplasty for the treatment of persistent OSA report resolution rates between 58 and 72% [64,65,66,67]. These studies show that supraglottoplasty can significantly improve, though not always completely resolve, PSG parameters in persistent OSA secondary to laryngomalacia.
Craniofacial Surgery
Maxillary and/or mandibular advancement is performed in children with OSA and craniofacial abnormalities, especially for children with micrognathia including infants with Pierre Robin sequence. In particular, there are successful outcomes for mandibular distraction osteogenesis, a popular surgical treatment for retrognathia and airway obstruction. One meta-analysis included 376 children with mandibular insufficiency and OSA who underwent mandibular advancement surgeries and demonstrated overall AHI-based surgical cure rates of 25.5%, with a reduction in AHI from 41.1 to 4.5 events/hour. Other orthognathic surgeries, such as maxillomandibular advancement, have substantial evidence for efficacy in adults; however, outcomes in children are limited, and ideal timing for surgery with regard to the impact on craniofacial development [68] is still unknown. One retrospective cohort study from 2020 examined 16 adolescents (mean age 17.4 years) who underwent maxillomandibular osteotomy primarily for correction of occlusion and found among other outcomes [69]. In this cohort, mean AHI decreased from 28 to 5.4 events/hour and oxygen saturation nadir improved from 88 to 91%. More sleep-specific research is needed to evaluate outcomes of orthognathic surgery in children.
Tracheostomy
Tracheostomy is a highly effective treatment for children with severe, refractory OSA and is most commonly recommended for children with cardiopulmonary comorbidities such as pulmonary hypertension or those with neurological disorders. It is also utilized, although infrequently, as a temporary measure in patients who require multilevel, staged procedures. The use of tracheostomy solely for the purpose of managing OSA is rare, and outcomes research is limited. Rizzi et al. described the effect of tracheostomy in 29 children who underwent tracheostomy for severe OSA. The mean preoperative AHI was 60.2 events/hour. While the majority of children remained tracheostomy dependent for OSA at 2-year follow-up, six patients were eventually decannulated and underwent capped PSG which showed a mean AHI of 6.6. Of note, the majority of this cohort had an underlying comorbidity such as craniofacial abnormalities or a neurologic disorder/hypotonia.
Conclusions
The evaluation and management of pediatric OSA are continuing to evolve. Although adenotonsillectomy and PAP are still widely utilized and regarded as treatment mainstays, there are a multitude of additional medical and surgical therapies available to treat primary and persistent OSA. Further investigation is needed to determine the best indications for each treatment modality. Finally, while PSG-based outcomes for popular treatments like adenotonsillectomy are well-studied, more research is needed to evaluate treatment effects on patient-reported outcomes, neurocognitive function, and cardiopulmonary sequelae in children with OSA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:576–84 This reference provides up-to-date clinical practice guidelines, geared for primary care physicians, for the overall evaluation and management of pediatric OSA.
Pratt JSA, Browne A, Browne NT, Bruzoni M, Cohen M, Desai A, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14:882–901.
Kalra M, Inge T, Garcia V, Daniels S, Lawson L, Curti R, et al. Obstructive sleep apnea in extremely overweight adolescents undergoing bariatric surgery. Obes Res. 2005;13:1175–9.
Amin R, Simakajornboon N, Szczesniak R, Inge T. Early improvement in obstructive sleep apnea and increase in orexin levels after bariatric surgery in adolescents and young adults. Surg Obes Relat Dis. 2017;13:95–100.
Arens R, Muzumdar H. Childhood obesity and obstructive sleep apnea syndrome. J Appl Physiol. 2010;108:436–44. https://doi.org/10.1152/japplphysiol.00689.2009.
Cozza P, Polimeni A, Ballanti F. A modified monobloc for the treatment of obstructive sleep apnoea in paediatric patients. Eur J Orthod. 2004;26(5):523–30. https://doi.org/10.1093/ejo/26.5.523.
Cozza P, Gatto R, Ballanti F, Prete L. Management of obstructive sleep apnoea in children with modified monobloc appliances. Eur J Paediatr Dent. 2004;5(1):24–9.
• Yanyan M, Min Y, Xuemei G. Mandibular advancement appliances for the treatment of obstructive sleep apnea in children: a systematic review and meta-analysis. Sleep Med. 2019;60:145–51 Findings from this systematic review and meta-analysis reflect four randomized controlled trials (RCT) and three non-RCT studies that overall demonstrate effectiveness of mandibular advancement appliances for pediatric OSA.
• Camacho M, Chang ET, Song SA, Abdullatif J, Zaghi S, Pirelli P, et al. Rapid maxillary expansion for pediatric obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2017;127:1712–9 Findings from this systematic review and meta-analysis reflect improved polysomnogram outcomes (AHI and oxygen saturation nadir) in children undergoing RME on short-term follow-up (< 3 years).
Holley AB, Lettieri CJ, Shah AA. Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest. 2011;140:1511–6. https://doi.org/10.1378/chest.10-2851.
Selvadurai S, Voutsas G, Massicotte C, Kassner A, Katz SL, Propst EJ, et al. Positional obstructive sleep apnea in an obese pediatric population. J Clin Sleep Med. 2020;16:1295–301. https://doi.org/10.5664/jcsm.8496.
Verhelst E, Clinck I, Deboutte I, Vanderveken O, Verhulst S, Boudewyns A. Positional obstructive sleep apnea in children: prevalence and risk factors. Sleep Breath. 2019;23:1323–30. https://doi.org/10.1007/s11325-019-01853-z.
Krachman S, Swift I, Vega ME. Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. In: de Vries N., Ravesloot M., van Maanen J. (eds) Positional Therapy in Obstructive Sleep Apnea. Springer, Cham. 2015. https://doi.org/10.1007/978-3-319-09626-1_31.
•• Liming BJ, Ryan M, Mack D, Ahmad I, Camacho M. Montelukast and nasal corticosteroids to treat pediatric obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2019;160:594–602. Findings from this systematic review and meta-analaysis demonstrate that treatment with montelukast alone or combined with intranasal steroid therapy is effective for mild pediatric OSA.
Yang DZ, Liang J, Zhang F, Yao HB, Shu Y. Clinical effect of montelukast sodium combined with inhaled corticosteroids in the treatment of OSAS children. Medicine (Baltimore). 2017;96:e6628. https://doi.org/10.1097/MD.0000000000006628.
Kheirandish L, Goldbart AD, Gozal D. Intranasal steroids and oral leukotriene modifier therapy in residual sleep-disordered breathing after tonsillectomy and adenoidectomy in children. Pediatrics. 2006;117:e61–6.
• Wang B, Liang J. The effect of montelukast on mild persistent OSA after adenotonsillectomy in children: a preliminary study. Otolaryngol Head Neck Surg. 2017;156:952–4 Findings from this study demonstrate that montelukast may improve sleep disturbance in children with persistent OSA following adenotonsillectomy.
Marcus CL, Rosen G, Davidson Ward SL, Halbower AC, Sterni L, Lutz J, et al. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. Pediatrics. 2006;117:e442–51. https://doi.org/10.1542/peds.2005-1634.
Fauroux B, Lavis JF, Nicot F, Picard A, Boelle PY, Clément A, et al. Facial side effects during noninvasive positive pressure ventilation in children. Intensive Care Med. 2005;31:965–9. https://doi.org/10.1007/s00134-005-2669-2.
•• Marcus CL, Moore RH, Rosen CL, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368:2366–76 Findings from this landmark study showed that compared to watchful waiting, adenotonsillectomy improved symptoms, behavior, quality of life, and polysomnographic findings in school-age children with OSA. However, there were no significant improvements in attention or executive function on neuropsychological testing.
Beebe DW, Wells CT, Jeffries J, Chini B, Kalra M, Amin R. Neuropsychological effects of pediatric obstructive sleep apnea. J Int Neuropsychol Soc. 2004;10:962–75. https://doi.org/10.1017/S135561770410708X.
Kennedy JD, Blunden S, Hirte C, Parsons DW, Martin AJ, Crowe E, et al. Reduced neurocognition in children who snore. Pediatr Pulmonol. 2004;37:330–7. https://doi.org/10.1002/ppul.10453.
Gozal D, Kheirandish-Gozal L, Bhattacharjee R, Spruyt K. Neurocognitive and endothelial dysfunction in children with obstructive sleep apnea. Pediatrics. 2010;126:e1161–7. https://doi.org/10.1542/peds.2010-0688.
•• Waters KA, Chawla J, Harris MA, Heussler H, Black RJ, Cheng AT, et al. Cognition after early tonsillectomy for mild OSA. Pediatrics. 2020. https://doi.org/10.1542/peds.2019-1450Findings from this prospective randomized controlled study showed no treatment-related cognitive benefit in preschool-aged children 12 months following adenotonsillectomy.
• Kang KT, Chiu SN, Lin CY, Weng WC, Lee PL, Hsu WC. Effect of adenotonsillectomy on ambulatory blood pressure in pediatric obstructive sleep apnea: 6-month follow-up study. Otolaryngol Head Neck Surg. 2019;160:911–21 Findings from this prospective cohort study demonstrated minimal ambulatory blood pressure changes overall after adenotonsillectomy for children with OSA. Hypertensive children compared to nonhypertensive children exhibited more prominent ambulatory blood pressure decreases after surgery.
• Zhang LY, Zhong L, David M, Cervin A. Tonsillectomy or tonsillotomy? A systematic review for paediatric sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2017;103:41–50 Findings from this systematic review of 32 studies support the effectiveness of tonsillotomy, compared to tonsillectomy, for pediatric patients with sleep-disordered breathing. Results also show decreased postoperative hemorrhage, improved postoperative pain, and a faster return to normal diet following tonsillotomy compared to tonsillectomy.
Solares CA, Koempel JA, Hirose K, Abelson TI, Reilly JS, Cook SP, et al. Safety and efficacy of powered intracapsular tonsillectomy in children: a multi-center retrospective case series. Int J Pediatr Otorhinolaryngol. 2005;69:21–6. https://doi.org/10.1016/j.ijporl.2004.07.006.
Domany KA, Dana E, Tauman R, Gut G, Greenfeld M, Yakir B-E, et al. Adenoidectomy for obstructive sleep apnea in children. J Clin Sleep Med. 2016;12:1285–91.
Chorney SR, Zur KB. Adenoidectomy without tonsillectomy for pediatric obstructive sleep apnea. Otolaryngol Head Neck Surg. 2020;164:1100–7. https://doi.org/10.1177/0194599820955172.
Brietzke SE, Gallagher D. The effectiveness of tonsillectomy and adenoidectomy in the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: a meta-analysis. Otolaryngol Head Neck Surg. 2006;134:979–84. https://doi.org/10.1016/j.otohns.2006.02.033.
Ehsan Z, Ishman SL. Pediatric obstructive sleep apnea. Otolaryngol Clin North Am. 2016;49(6):1449–64. https://doi.org/10.1016/j.otc.2016.07.001.
Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: outcome evaluated by pre- and postoperative polysomnography. Laryngoscope. 2007;117:1844–54. https://doi.org/10.1097/MLG.0b013e318123ee56.
O’Brien LM, Sitha S, Baur LA, Waters KA. Obesity increases the risk for persisting obstructive sleep apnea after treatment in children. Int J Pediatr Otorhinolaryngol. 2006;70:1555–60. https://doi.org/10.1016/j.ijporl.2006.04.003.
Tauman R, Gulliver TE, Krishna J, Montgomery-Downs HE, O’Brien LM, Ivanenko A, et al. Persistence of obstructive sleep apnea syndrome in children after adenotonsillectomy. J Pediatr. 2006;149:803–8. https://doi.org/10.1016/j.jpeds.2006.08.067.
• Farhood Z, Isley JW, Ong AA, Nguyen SA, Camilon TJ, LaRosa AC, et al. Adenotonsillectomy outcomes in patients with Down syndrome and obstructive sleep apnea. Laryngoscope. 2017;127:1465–70 Findings from this systematic review in patients with Down syndrome and OSA show that although there is an improvement in AHI following adenotonsillectomy, the majority of patients do not experience disease cure (AHI < 1).
Wilcox LJ, Bergeron M, Reghunathan S, Ishman SL. An updated review of pediatric drug-induced sleep endoscopy. Laryngoscope Investig Otolaryngol. 2017;2:423–31.
Baldassari CM, Lam DJ, Ishman SL, et al. Expert consensus statement: pediatric drug-induced sleep endoscopy [published online ahead of print, 2021 Jan 5]. Otolaryngol Head Neck Surg. 2021;194599820985000. https://doi.org/10.1177/0194599820985000.
Ishman SL, Chang KW, Kennedy AA. Techniques for evaluation and management of tongue-base obstruction in pediatric obstructive sleep apnea. Curr Opin Otolaryngol Head Neck Surg. 2018;26:409–16.
Bluher AE, Ishman SL, Baldassari CM. Managing the child with persistent sleep apnea. Otolaryngol Clin North Am. 2019;52(5):891–901.
Mickelson SA. Nasal surgery for obstructive sleep apnea syndrome. Otolaryngol Clin N Am. 2016;49:1373–81. https://doi.org/10.1016/j.otc.2016.07.002.
Ishii L, Roxbury C, Godoy A, Ishman S, Ishii M. Does nasal surgery improve OSA in patients with nasal obstruction and OSA? A meta-analysis. Otolaryngol Head Neck Surg. 2015;153:326–33. https://doi.org/10.1177/0194599815594374.
Cheng PW, Fang KM, Su HW, Huang TW. Improved objective outcomes and quality of life after adenotonsillectomy with inferior turbinate reduction in pediatric obstructive sleep apnea with inferior turbinate hypertrophy. Laryngoscope. 2012;122:2850–4.
Sullivan S, Li K, Guilleminault C. Nasal obstruction in children with sleep-disordered breathing. Ann Acad Med Singap. 2008;37(8):645–8.
Wiet GJ, Bower C, Seibert R, Griebel M. Surgical correction of obstructive sleep apnea in the complicated pediatric patient documented by polysomnography. Int J Pediatr Otorhinolaryngol. 1997;41:133–43. https://doi.org/10.1016/S0165-5876(97)00065-7.
Com G, Carroll JL, Tang X, Melguizo MS, Bower C, Jambhekar S. Characteristics and surgical and clinical outcomes of severely obese children with obstructive sleep apnea. J Clin Sleep Med. 2015;11:467–74. https://doi.org/10.5664/jcsm.4608.
Ulualp SO. Modified expansion sphincter pharyngoplasty for treatment of children with obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2014;140:817–22.
• Isaiah A, Kiss E, Olomu P, Koral K, Mitchell RB. Characterization of upper airway obstruction using cine MRI in children with residual obstructive sleep apnea after adenotonsillectomy. Sleep Med. 2018;50:79–86. https://doi.org/10.1016/j.sleep.2017.10.006. This study describes cine MRI as a sensitive and noninvasive diagnostic modality to evaluate upper airway obstruction in children with persistent OSA following adenotonsillectomy.
Fricke BL, Donnelly LF, Shott SR, Kalra M, Poe SA, Chini BA, et al. Comparison of lingual tonsil size as depicted on MR imaging between children with obstructive sleep apnea despite previous tonsillectomy and adenoidectomy and normal controls. Pediatr Radiol. 2006;36:518–23.
• Manickam PV, Shott SR, Boss EF, Cohen AP, Meinzen-Derr JK, Amin RS, et al. Systematic review of site of obstruction identification and non-CPAP treatment options for children with persistent pediatric obstructive sleep apnea. Laryngoscope. 2016;126:491–500 Findings from this systematic review show that drug-induced sleep endoscopy and cine MRI are commonly used to evaluate sites of airway obstruction in children with persistent OSA following adenotonsillectomy.
• Rivero A, Durr M. Lingual tonsillectomy for pediatric persistent obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2017;157:940–7 Findings from this systematic review and meta-analysis show that lingual tonsillectomy is a safe and effective procedure to manage persistent OSA after adenotonsillectomy.
DeMarcantonio MA, Senser E, Meinzen-Derr J, Roetting N, Shott S, Ishman SL. The safety and efficacy of pediatric lingual tonsillectomy. Int J Pediatr Otorhinolaryngol. 2016;91:6–10.
Propst EJ, Amin R, Talwar N, Zaman M, Zweerink A, Blaser S, et al. Midline posterior glossectomy and lingual tonsillectomy in obese and nonobese children with down syndrome: biomarkers for success. Laryngoscope. 2017;127:757–63.
Ulualp S. Outcomes of tongue base reduction and lingual tonsillectomy for residual pediatric obstructive sleep apnea after adenotonsillectomy. Int Arch Otorhinolaryngol. 2019;23:415–21.
Wootten CT, Shott SR. Evolving therapies to treat retroglossal and base-of-tongue obstruction in pediatric obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2010;136:983–7.
Broucqsault H, Lamblin MD, Hosana G, Fayoux P. Evaluation of the efficacy of tongue-lip adhesion in Pierre Robin sequence. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135:155–8.
Resnick CM, Dentino K, Katz E, Mulliken JB, Padwa BL. Effectiveness of tongue-lip adhesion for obstructive sleep apnea in infants with robin sequence measured by polysomnography. Cleft Palate Craniofac J. 2016;53:584–8.
Camacho M, Noller MW, Zaghi S, Reckley LK, Fernandez-Salvador C, Ho E, et al. Tongue-lip adhesion and tongue repositioning for obstructive sleep apnoea in Pierre Robin sequence: a systematic review and meta-analysis. J Laryngol Otol. 2017;131:378–83.
• Caloway CL, Diercks GR, Keamy D, Guzman V, Soose R, Raol N, et al. Update on hypoglossal nerve stimulation in children with down syndrome and obstructive sleep apnea. Laryngoscope. 2020;130:E263–7 This study is one of the first to describe the safety and efficacy of hypoglossal nerve stimulation in pediatric patients with Down syndrome.
Diercks GR, Keamy D, Kinane TB, Skotko B, Schwartz A, Grealish E, et al. Hypoglossal nerve stimulator implantation in an adolescent with Down syndrome and sleep apnea. Pediatrics. 2016;137:e20153663.
Franco RA Jr, Rosenfeld RM, Rao M. First place--resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;123(1 Pt 1):9–16. https://doi.org/10.1067/mhn.2000.105254.
Zalzal HG, Davis K, Carr MM, Coutras S. Epiglottopexy with or without aryepiglottic fold division: comparing outcomes in the treatment of pediatric obstructive sleep apnea. Am J Otolaryngol Head Neck Med Surg. 2020;41:102478. https://doi.org/10.1016/j.amjoto.2020.102478.
• Camacho M, Dunn B, Torre C, Sasaki J, Gonzales R, Liu SY-C, et al. Supraglottoplasty for laryngomalacia with obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2016;126:1246–55 Findings from this systematic review and meta-analysis show that supraglottoplasty improves polysomnogram outcomes in children with congenital or sleep-dependent laryngomalacia and OSA.
Bhushan B, Schroeder JW, Billings KR, Giancola N, Thompson DM. Polysomnography outcomes after supraglottoplasty in children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2019;161:694–8.
Truong MT, Woo VG, Koltai PJ. Sleep endoscopy as a diagnostic tool in pediatric obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2012;76:722–7. https://doi.org/10.1016/j.ijporl.2012.02.028.
Digoy GP, Shukry M, Stoner JA. Sleep apnea in children with laryngomalacia: diagnosis via sedated endoscopy and objective outcomes after supraglottoplasty. Otolaryngol Head Neck Surg. 2012;147(3):544–50. https://doi.org/10.1177/0194599812446903.
Chan DK, Jan TA, Koltai PJ. Effect of obesity and medical comorbidities on outcomes after adjunct surgery for obstructive sleep apnea in cases of adenotonsillectomy failure. Arch Otolaryngol Head Neck Surg. 2012;138:891–6. https://doi.org/10.1001/2013.jamaoto.197.
Chan DK, Truong MT, Koltai PJ. Supraglottoplasty for occult laryngomalacia to improve obstructive sleep apnea syndrome. Arch Otolaryngol Head Neck Surg. 2012;138:50. https://doi.org/10.1001/archoto.2011.233.
Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, Part 1: Mandibular deformities. Am J Orthod Dentofac Orthop. 2001;119:95–101. https://doi.org/10.1067/mod.2001.111401.
Best DL, Chadha S, Wang C, Harriman E, Aronovich S. Surgical outcomes of maxillomandibular advancement to treat obstructive sleep apnea in an adolescent population. J Oral Maxillofac Surg. 2020;78:e4–5. https://doi.org/10.1016/j.joms.2020.07.036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Ishman reports personal fees from Inspire Medical, outside the submitted work. The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on SLEEP MEDICINE: Sleep Apnea
Rights and permissions
About this article
Cite this article
Li, C., Kou, YF. & Ishman, S.L. Pediatric OSA: Evidence-Based Review of Treatment Results. Curr Otorhinolaryngol Rep 9, 246–253 (2021). https://doi.org/10.1007/s40136-021-00348-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-021-00348-4