Abstract
Purpose of Review
Even though there are latest advances on immunocompromised patient care, the mortality by invasive fungal infection still high. Invasive aspergillosis is one of the main complications during immunosuppression and on hematological malignancy patients, with a mortality varying from 50 to 80%. Imaging studies are fundamental on the evaluation of fungal suspicion, and concerns related to radiation dose on image examinations are high nowadays. Magnetic resonance imaging should be considered on brain and facial sinuses evaluation to reduce radiation exposure.
Recent Findings
Whenever fungal material is present, the sinus content becomes a low STIR signal and a middle-high signal on T1. The T2 low signal or signal void is attributed to metal concentration, as well as the high protein and low free water content. Adjacent structures should also be evaluated to characterize disease involvement and its extension.
Summary
MRI should be used to reduce radiation exposure on the evaluation of fungal suspicion on immunocompromised patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Even though there are latest advances on chemotherapy patient care, the mortality by invasive fungal infection is still high among immunocompromised patients. Among more than 400,000 fungal species and 50 that can cause systemic infection, aspergillosis is the most common cause [1•, 2].
Invasive aspergillosis is one of the main complications during immunosuppression and on hematological malignancy patients. It is considered invasive whenever the fungal hyphae is found within the mucosa, submucosa, bone, or blood vessels [2]. Acute Invasive Fungal Sinusitis is the most lethal form of fungal sinusitis, with a mortality varying from 50 to 80%, is rare in immunocompetent patients, and is usually associated to poorly controlled diabetes and immunocompromised conditions [3, 4••].
Imaging studies are fundamental in the evaluation of fungal suspicion in patients with febrile neutropenia, after bone marrow transplantation, and during immunosuppression [5].
Nowadays, concerns related to radiation dose on image examinations are high, especially among young patients and those submitted to multiple studies during cancer treatment follow-up. The use of magnetic resonance (MR) should be considered for brain and facial sinuses evaluation.
Technical Considerations
The following sequences are considered usually sufficient to this evaluation: sinuses coronal STIR and axial T1 (Fig. 1) FLAIR. No contrast media is necessary to determine fungal infection.
8 years and 10 months old girl, post-bone marrow transplantation treating large cell non-Hodgkin’s lymphoma. a Coronal STIR shows low signal intensity within the walls of the hyperintense maxillary and ethmoid sinuses. b Unenhanced axial T1 shows characteristic hyperintense material within maxillary sinuses
Imaging Findings
Facial sinuses and brain MRI should confirm the presence of fungal disease. The mucosa sinus edema is associated with a high STIR signal and low T1 (water). Whenever fungal material is present (Fig. 2) the sinus content becomes to a low STIR and a middle-high signal on T1. The T2 low signal or signal void is attributed to metal concentration, such as iron, magnesium, and manganese (Fig. 3) as well as the high protein and low free water content. Usually multiple sinuses are involved and they can be expanded. The adjacent fat and the posterior maxillary wall should also be evaluated, looking for inflammatory changes, obliteration of periantral fat, (Fig. 4) as well as the intraorbital and intracranial extension, leptomeningeal thickness, cerebritis, abscess, and intracranial granulomas, to characterize disease involvement and extension.
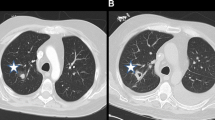
15-year-old girl post-bone marrow transplant to treat acute lymphocytic leukemia . a Coronal STIR shows signal void within the left maxillary sinus and hypersignal content within the ethmoid and right maxillary sinuses. b Unenhanced axial T1 shows hyperintense material within maxillary sinuses with anterior and posterior extension at the left sinus
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Aribandi M, McCoy VA, Bazan C. Imaging features of invasive and non-invasive fungal sinusitis: a review. Radiographics. 2007;27:1283–96. Imaging findings review on fungal sinusitis.
Soler ZM, Schlosser RJ. The role of fungi in diseases of the nose and sinuses. Am J Rhinol Allergy. 2012;26:351–8.
Gorovoy IR, Kazanjian M, Kersten RC, Kim HJ, Vagefi MR. Fungal rhinosinusitis and imaging modalities. Saudi J Ophthalmol. 2012;26:419–26.
•• Mossa-Basha M, Ilica AT, Maluf F, Karakoç Ö, Izbudak I, Aygün N. The many faces of fungal disease of the paranasal sinuses: CT and MRI findings. Diagn Interv Radiol. 2013;19:195–200. CT/MRI findings review on fungal sinusitis.
Middlebrooks EH, Frost CJ, De Jesus RO, Massini TC, Schmalfuss IM, Mancuso AA. Acute invasive fungal rhinosinusitis: a comprehensive update of CT findings and design of an effective diagnostic imaging model. AJNR Am J Neuroradiol. 2015;36:1529–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Vivian Siqueira Tostes and Jose Luiz de Oliveira Schiavon each declare no potential conflicts of interest. Henrique Manoel Lederman is a section editor for Current Radiology Reports.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Pediatrics.
Rights and permissions
About this article
Cite this article
Tostes, V.S., de Oliveira Schiavon, J.L. & Lederman, H.M. Fungal Sinusitis: Magnetic Resonance Image Findings on Immunocompromised Patients. Curr Radiol Rep 5, 9 (2017). https://doi.org/10.1007/s40134-017-0202-3
Published:
DOI: https://doi.org/10.1007/s40134-017-0202-3