Abstract
Hypertension is a major risk factor for cardiovascular diseases and is known to contribute to complications, such as atherosclerosis and diabetes. The aim of this study was to investigate the possible synergistic effects of candesartan, an angiotensin II receptor blocker (ARB), and ramipril, an angiotensin-converting enzyme inhibitor (ACEI), in lowering high blood pressure in spontaneously hypertensive rats (SHRs). SHRs were given oral candesartan (1.53 mg/kg/day) and ramipril (0.48 mg/kg/day) for 2 weeks. The combination of candesartan and ramipril improved systolic blood pressure (SBP), mean arterial pressure (MAP), and heart rate (HR) significantly compared with monotherapy. Additionally, combined treatment with candesartan (3.06 mg/kg/day) and ramipril (0.96 mg/kg/day) significantly decreased cuff-induced neointima hyperplasia and media thickness in C57BL/6 mice. In oral glucose tolerance tests (OGTTs), the combination of candesartan and ramipril significantly controlled blood glucose levels within 2 h after glucose loading in low-dose (38 mg/kg, i.p.) streptozotocin-treated Wistar rats. Taken together, the present study suggests that combination therapy with candesartan and ramipril may be a beneficial therapeutic strategy for the treatment of hypertensive patients with related complications, such as atherosclerosis and diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension has long been recognized as a risk factor for atherosclerosis, stroke, heart failure, and myocardial infarction, and is defined by a blood pressure (BP) higher than 140/90 mmHg (Gupta and Guptha 2010; Kannel 2009). Approximately 25% of the adult population of the United States, and 30% of Korean adults over the age of 30 years, have hypertension (Ahluwalia and Bangalore 2017; Lee and Park 2015). According to the Eighth Joint National Committee (JNC 8) report, a BP less than 140/90 mmHg is recommended for hypertensive patients between 30 and 59 years of age and over the age of 60 (James et al. 2014).
The renin-angiotensin system (RAS) plays an important role in the pathogenesis of cardiovascular and renal disease. Renin is a glycoprotein enzyme synthesized by juxtaglomerular (JG) cells that cleaves angiotensinogen to angiotensin I. Under physiological conditions, angiotensin-converting enzyme (ACE) hydrolyzes angiotensin I to angiotensin II (the active form), the major effector of the RAS, which can bind to the angiotensin II type 1 (AT1) receptor and thus mediate nervous physiological actions including increased BP, cardiac vasoconstriction, insulin resistance, renal sodium retention, and aldosterone synthesis by the adrenal cortex (Atlas 2007; Carey and Siragy 2003; Ribeiro-Oliveira et al. 2008).
Many anti-hypertensive drugs have been developed, including thiazides, loop diuretics and potassium-sparing diuretics, angiotensin II receptor blockers (ARBs), ACE inhibitors (ACEIs), renin inhibitors, β-blockers, and calcium channel blockers (CCBs) (Nguyen et al. 2010). In the JNC 8 guidelines, thiazide-based diuretics, CCBs, ACEIs, and ARBs are recommended, whereas β-blockers were excluded from primary treatment guidelines (James et al. 2014). European Society of Hypertension and European Society of Cardiology (ESH/ESC) guidelines also recommend using therapeutic drugs (including β-blockers) in treatment, and combination therapy is typically required for high-risk patients with cardiovascular disease (Mancia et al. 2014).
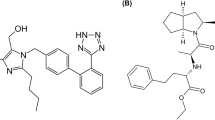
Candesartan, an ARB, selectively inhibits angiotensin II binding to the AT1 receptor, which has been reported to inhibit CCl4-induced hepatic fibrosis in rats (Tuncer et al. 2003), improve coronary endothelial dysfunction in patients (Iino et al. 2012), and reduce the risk of stroke and myocardial infarction in hypertensive patients (Suzuki and Kanno 2005). Ramipril, an ACEI, reduces the conversion of angiotensin I to angiotensin II and also prevents the degradation of bradykinin and other kinins; however, continued inhibition of ACE can lead to the accumulation of angiotensin I and bradykinin, resulting in the generation of angiotensin II by an ACE-independent pathway (Erdos et al. 2010). Previous reports showed that dual blockade of aldosterone and ACE had a greater effect than monotherapy in patients with heart failure (Pitt et al. 1999) and myocardial infarction (Pitt et al. 2003). Additionally, the combination of an ACE inhibitor and an ARB confers more pharmacological benefit than monotherapy on BP and heart weight (evaluated by hypertrophy) in spontaneously hypertensive rats (SHRs) (Menard et al. 1997). Thus, in the present study, we investigated the beneficial effects of candesartan and ramipril, alone and in combination, on BP in SHRs, vascular remodeling in C57BL/6 mice, and glucose homeostasis in streptozotocin (STZ)-treated diabetic Wistar rats.
Materials and methods
Materials
Candesartan and ramipril were purchased from Masung Co. (Seongnam, Korea). Formaldehyde was purchased from Samchun Co. (Yeosoo, Korea), phosphate-buffered saline (PBS) from Gibco (Grand Island, NY, USA), and polyethylene tubing-50 (PE-50) from Becton, Dickinson & Co. (Franklin Lakes, NJ, USA). Normal saline was purchased from Daehan Co. (Seoul, Korea) and pentobarbital sodium from Hanlim (Seoul, Korea). Mouse anti-bromodeoxyuridine (BrdU) monoclonal antibody was purchased from Chemicon International, Inc. (Seongnam, Korea) and anti-mouse IgG from Vector (Burlingame, CA, USA).
Animal
Male SHRs (7–8 weeks of age; Charles River Laboratory, Wilmington, MA, USA), male C57BL/6 mice (10–12 weeks of age; Charles River Japan, Inc., Kanagawa, Japan), and Wistar rats (8–9 weeks of age; weight, 140–160 g) were purchased from Orient Bio, Inc. (Seongnam, Korea). Animals were fed tap water and a normal diet (Ralston Purina, St. Louis, MO, USA) and housed at a temperature of 22 ± 2 °C under a 12/12-h light-dark cycle. Animals were used in experiments after 1 week of acclimatization. All experimental procedures were performed in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals, as approved by Chungnam National University Animal Care and Use Committee.
Drug administration protocol
The dose of candesartan and ramipril were the human clinical equivalents (Table 1) listed in the Guidance for Industry on Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers document of the Food and Drug Administration. Drug administration groups were treated with vehicle (0.9% NaCl and 0.15 N NaOH), candesartan (1.53 mg/kg/day for rats and 3.06 mg/kg/day for mice), ramipril (0.48 mg/kg/day for rats and 0.96 mg/kg/day for mice), and a combination of both drugs (Table 2). The doses of candesartan and ramipril were equivalent to 16 mg and 5 mg, respectively.
Measurement of blood pressure (BP) and heart rate (HR)
Measurements of systolic blood pressure (SBP), mean arterial pressure (MBP) and HR were made using a telemetry system (Data Sciences International, St. Paul, MN, USA) (Shin et al. 2009; Lee et al. 2010; Park et al. 2016). The telemetric equipment consisted of a receiver (type RMC-1), transmitter, and data analysis software (Data Quest). Briefly, SHRs were anesthetized with sodium pentobarbital (60 mg/kg, i.p.), and then a BP catheter attached to the telemeter was inserted into the abdominal aorta. After 2 weeks, the SBP of SHRs was higher than 180 mmHg, drug administration was performed. Hemodynamic data of SHRs were measured at intervals of 5 min.
Myocardial ischemia/reperfusion (MI/R) injury
SHRs were anesthetized with sodium pentobarbital (100 mg/kg, i.p.). To generate myocardial ischemia, the left thoracic was incised after exposing the heart and then a knot was made in the coronary artery between the left and right atria. After 40 min, the knot was untied and the myocardium reperfused for 4 h. In the control group of SHRs, the thorax was closed after a thoracotomy. SHRs were sacrificed at 4 h after reperfusion and ischemia was assessed after 5% Evans blue staining.
Measurement of endothelial NOS (eNOS) content
The left ventricles (LVs) of SHRs were dissected and homogenized using a tissue grinder. Subsequently, the homogenized tissue centrifuged (10,000 g, 10 min, 4 °C), and the supernatant transferred to an e-tube for use in the eNOS assay. Myocardial eNOS content was measured using an ELISA kit (R&D Systems, Minneapolis, MN, USA) with human eNOS as the standard. The absorbance was measured at 450 nm using a microplate reader (Packard Instrument Co., Downers Grove, IL, USA).
Analysis of neointima formation using a cuff
Cuff-induced vascular injury was described previously (Akishita et al. 2000; Yi et al. 2010). C57BL/6 mice were anesthetized with sodium pentobarbital (100 mg/kg, i.p.), and the femoral artery was separated from peripheral tissue. Then, a polyethylene tube cuff (2 mm PE-50) was placed loosely around the artery. After cuff placement for 2 weeks, mice were sacrificed with a lethal dose of pentobarbital and perfused with PBS for 5 min, immediately followed by 4% paraformaldehyde through catheterization of the LV. The cuffed femoral artery tissue was fixed in 4% paraformaldehyde for 12 h and then embedded in paraffin wax. Sections were cut at 5 µm and subjected to hematoxylin and eosin staining and combined Masson’s elastin staining. The intima area (between the lumen and internal elastic lamina), medial area (between the internal and external elastic lamina), and intima/media ratio were assessed using Image J software (National Institutes of Health, Bethesda, MD, USA).
BrdU incorporation assay
Incorporation of 5-bromo-2′-deoxyuridine (BrdU), a marker of DNA synthesis, was used to quantify the ratio of cell proliferation in the cuffed arterial segment. Mice were injected with BrdU (30 mg/kg, i.p.) at 18 and 12 h prior to sacrifice. Arterial sections were incubated with anti-BrdU antibodies (BrdU-Cell Proliferation Kit, Amersham, Little Chalfont, UK). The ratio of BrdU-positive nuclei was assessed using the Image J software, counted in six equal spaces.
Oral glucose tolerance test (OGTT) and insulin tolerance test (ITT)
Wistar rats (8–9 weeks of age; weight, 140–160 g) were administered a low dose of STZ (38 mg/kg, i.p.), maintained for 4 weeks to induce a diabetic state. After overnight fasting, drugs were administered to the animal groups (candesartan or ramipril monotherapy, or combination therapy with both drugs) for 2 weeks. At 2 h after drug treatments, rats were given 2 g/kg of 20% glucose solution (p.o.), and blood glucose level was measured at 0, 0.5, 1, 1.5, and 2 h after glucose loading. The ITT was performed by injecting insulin (2 unit/kg, s.c.) after glucose loading, and measuring blood glucose levels at the same times as in the OGTT. The blood glucose level was measured using Accu-Chek Active strips (Roche, Mannheim, Germany). The area under the curve (AUC) was calculated using GraphPad Prism software (ver. 5.0; GraphPad, Inc., San Diego, CA, USA).
Statistical analysis
Data are expressed as means ± SEM, we performed Student’s t test using GraphPad Prism software (ver. 5.0). The area over the curve (AOC) and AUC were calculated and we performed one-way analysis of variance (ANOVA) using the Student–Newman–Keuls method. A p value <0.05 was considered to indicate statistical significance.
Results and discussion
Effects of candesartan and ramipril on BP and HR in SHRs
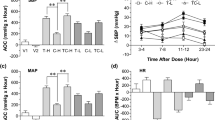
The antihypertensive effects of candesartan and ramipril were examined using telemetric monitoring (Shin et al. 2009; Lee et al. 2010; Park et al. 2016). After 2 weeks of drug administration, candesartan (1.53 mg/kg) reduced SBP in SHRs (Fig. 1a). Compared with candesartan, ramipril (0.48 mg/kg) attenuated SBP more effectively. Additionally, the combination of candesartan and ramipril produced a significant synergistic reduction of SBP in SHRs. The change in SBP was the most effective for 3–4 h and there were time-dependent changes in SBP (Fig. 1b). As shown in Fig. 2a, the effects of candesartan and ramipril on MAP were analogous to those on SBP. In terms of HR, single treatment with each drug did not produce changes, but with combination therapy HR declined significantly (Fig. 2b). These results also indicated that despite lowering BP, the combination of candesartan and ramipril did not result in side effects, such as reflex tachycardia or sympathetic activation (Loga-Zec et al. 2014).
Effects of candesartan and ramipril on the area over the curve (AOC) of systolic blood pressure (SBP) (a) and the change of SBP (b) in spontaneously hypertensive rats (SHRs). The basal blood pressure (BP) in SHRs were measured for 3 days before drug administration. SHRs were administered candesartan (1.53 mg/kg) and ramipril (0.48 mg/kg) orally for 2 weeks. Data are expressed as means ± SEM. n = 6 per group. *p < 0.05. V (vehicle, 0.15 N NaOH), C (candesartan), R (ramipril), CR (candesartan + ramipril)
Effects of candesartan and ramipril on the area over the curve (AOC) of mean arterial pressure (MAP) (a) and area under the curve (AUC) of heart rate (HR) change (b) in SHRs. The basal BP of SHRs was measured for 3 days before drug administration. SHRs were administered candesartan (1.53 mg/kg) and ramipril (0.48 mg/kg) orally for 2 weeks. Data are expressed as means ± SEM. n = 6 per group. *p < 0.05.V (vehicle, 0.15 N NaOH), C (candesartan), R (ramipril), CR (candesartan + ramipril)
Effects of candesartan and ramipril on MI/R injury
Hypertension and myocardial infarction are closely related (McBride et al. 2014; Pedrinelli et al. 2012). Thus, we investigated the cardioprotective effects of candesartan and ramipril in SHRs. SHRs were pretreated with candesartan and ramipril for 2 weeks before 40 min of myocardial ischemia and 4 h of reperfusion. The myocardial area at risk (AAR)/left ventricle (LV) was reduced slightly by the combination of candesartan and ramipril (Fig. 3a). However, the change in the infarct zone (IZ)/AAR was not significant, and it seems likely that single treatment with each drug was more effective than the combination treatment. The content of eNOS in cardiac tissues of SHRs was unchanged, comparing each treatment group (Fig. 3b). eNOS is the major subtype of nitric oxide (NO) synthase contributing to the development of LV hypertrophy (Flaherty et al. 2007) in eNOS-deficient mice, and telmisartan (an ARB) confers cardioprotective effects by producing eNOS through peroxisome proliferator-activated receptor-γ (PPAR-γ) activation (Kobayashi et al. 2008). Thus, these results indicated that neither monotherapy nor combined therapy with candesartan and ramipril affected eNOS activation or NO formation.
Effects of candesartan and ramipril on myocardial ischemia/reperfusion (MI/R) injury (a) and eNOS content (b) in SHRs. SHRs were administered candesartan (1.53 mg/kg) and ramipril (0.48 mg/kg) orally for 2 weeks. Data are expressed as means ± SEM. n = 6 per group. V1 (vehicle 1, 0.9% NaCl), V2 (vehicle 2, 0.15 N NaOH), AAR (area at risk), LV (left ventricle), IZ (infarct zone), C (candesartan), R (ramipril), CR (candesartan + ramipril)
Effects of candesartan and ramipril on cuff-induced neointima formation
Neointima hyperplasia can be induced not only by coronary angioplasty, but also by persistently high BP (Dickinson et al. 2011; Maor et al. 2008). Thus, we next evaluated the effect of candesartan and ramipril in a cuff-induced vascular injury mouse model. After 2 weeks of cuff placement, neointima for mation and media thickness was observed (Yi et al. 2010). Administration of candesartan (3.06 mg/kg) for 2 weeks decreased cuff-induced neointima formation significantly in C57BL/6 mice (Fig. 4a). However, neither ramipril (0.96 mg/kg) alone nor in combination with candesartan showed any significant effect on the reduction of neointima formation. Regarding cuff-induced media thickness, monotherapy with candesartan or ramipril, and the combination of both drugs, showed no significant effect (Fig. 4b).
Effects of candesartan and ramipril on cuff-induced neointima (a) and media (b) thickness in C57BL/6 mice. Mice were administered candesartan (3.06 mg/kg) and ramipril (0.96 mg/kg) orally for 2 weeks after cuff placement. Data are expressed as means ± SEM. *p < 0.05. n = 6 per group. C (candesartan), R (ramipril)
Effects of candesartan and ramipril on vascular DNA synthesis
BrdU is inserted into the DNA of the growing cell (S-phase), indicating cell proliferation (Mead and Lefebvre 2014). The BrdU assay was used to measure cell proliferation in the neointima and media. Treatment with candesartan and ramipril reduced the proportion of BrdU-positive cells in the neointima (Fig. 5a). Combined treatment with candesartan and ramipril showed a greater inhibitory effect than monotherapy. BrdU incorporation in media showed results similar to those seen in the intima (Fig. 5b). Thus, these results suggest that DNA synthesis in both the intima and media was suppressed by monotherapy and combination therapy, but the differences were not sufficient to see a significant reduction in cuff-induced neointima formation or media thickness.
Effects of candesartan and ramipril on mouse anti-bromodeoxyuridine (BrdU) incorporation into the neointima (a) and media (b) of cuff-placed C57BL/6 mice. Mice were administered candesartan (3.06 mg/kg) and ramipril (0.96 mg/kg) orally for 2 weeks after cuff placement. Data are expressed as mean ± SEM. *p < 0.05 and **p < 0.01. n = 6 per group. C (candesartan), R (ramipril)
Effects of candesartan and ramipril on glucose tolerance and insulin sensitivity
High BP is closely associated with the risk of diabetes (Conen et al. 2007; Golden et al. 2003; Wei et al. 2011). Diabetes is a non-traditional risk factors for cardiovascular disease, the complications of which can lead to death in diabetic patients (Martin-Timon et al. 2014). A meta-analysis of randomized controlled studies showed that combination therapy with an ARB and an ACEI reduced cardiovascular events and mortality in hypertensive patient with type 2 diabetes mellitus (Hao et al. 2014). Thus, we determined the effects of candesartan and ramipril on glucose tolerance and insulin action in diabetic Wistar rats. As shown in Fig. 6a, administration of each drug alone did not decrease the blood glucose level, but combination treatment with candesartan and ramipril showed significant attenuation (c.f. the decrease in the AUC in Fig. 6b). However, the ITT results did not differ among groups (Fig. 6c, d).
Effects of candesartan and ramipril on blood glucose levels during the oral glucose tolerance test (OGTT) and the insulin tolerance test (ITT) in diabetic Wistar rats. Rats were administered candesartan (1.53 mg/kg) and ramipril (0.48 mg/kg) orally for 2 weeks. Changes in blood glucose levels (a) and the area under the curve (AUC) for 2 h during OGTT. The blood glucose (c) and AUC (d) were measured after insulin (2 unit/kg, s.c.) loading. Data are expressed as means ± SEM. *p< 0.05. n = 6 per group. Con (control), C (candesartan), R (ramipril), CR (candesartan + ramipril)
Conclusions
Combination therapy with candesartan and ramipril showed a synergistic antihypertensive effect with no reflex tachycardia, suggesting that this combination may be appropriate for cases where there is a need for a large reduction in BP. Furthermore, this combination reduced cuff-induced DNA synthesis in the intima and media of blood vessels and controlled blood glucose levels against high-glucose input in diabetes. Thus, combination therapy with candesartan and ramipril may be useful for treating hypertensive patients with complications, such as atherosclerosis and diabetes.
References
Ahluwalia M, Bangalore S (2017) Management of hypertension in 2017: targets and therapies. Curr Opin Cardiol. doi:10.1097/HCO.0000000000000408
Akishita M, Horiuchi M, Yamada H, Zhang L, Shirakami G, Tamura K, Ouchi Y, Dzau VJ (2000) Inflammation influences vascular remodeling through AT2 receptor expression and signaling. Physiol Genomics 2:13–20
Atlas SA (2007) The renin-angiotensin aldosterone system: pathophysiological role and pharmacologic inhibition. J Manag Care Pharm 13:S9–S20
Carey RM, Siragy HM (2003) Newly recognized components of the renin-angiotensin system: potential roles in cardiovascular and renal regulation. Endocr Rev 24:261–271
Conen D, Ridker PM, Mora S, Buring JE, Glynn RJ (2007) Blood pressure and risk of developing type 2 diabetes mellitus: the Women’s Health Study. Eur Heart J 28:2937–2943
Dickinson MG, Bartelds B, Molema G, Borgdorff MA, Boersma B, Takens J, Weij M, Wichers P, Sietsma H, Berger RM (2011) Egr-1 expression during neointimal development in flow-associated pulmonary hypertension. Am J Pathol 179:2199–2209
Erdos EG, Tan F, Skidgel RA (2010) Angiotensin I-converting enzyme inhibitors are allosteric enhancers of kinin B1 and B2 receptor function. Hypertension 55:214–220
Flaherty MP, Brown M, Grupp IL, Schultz JE, Murphree SS, Jones WK (2007) eNOS deficient mice develop progressive cardiac hypertrophy with altered cytokine and calcium handling protein expression. Cardiovasc Toxicol 7:165–177
Golden SH, Wang NY, Klag MJ, Meoni LA, Brancati FL (2003) Blood pressure in young adulthood and the risk of type 2 diabetes in middle age. Diabetes Care 26:1110–1115
Gupta R, Guptha S (2010) Strategies for initial management of hypertension. Indian J Med Res 132:531–542
Hao G, Wang Z, Guo R, Chen Z, Wang X, Zhang L, Li W (2014) Effects of ACEI/ARB in hypertensive patients with type 2 diabetes mellitus: a meta-analysis of randomized controlled studies. BMC Cardiovasc Disord 14:148–154
Iino K, Watanabe H, Iino T, Katsuta M, Koyama T, Kosaka T, Terui G, Ito H (2012) Candesartan improves impaired endothelial function in the human coronary artery. Coron Artery Dis 23:278–283
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Narva AS, Ortiz E (2014) 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311:507–520
Kannel WB (2009) Hypertension: reflections on risks and prognostication. Med Clin North Am 93:541–558
Kobayashi N, Ohno T, Yoshida K, Fukushima H, Mamada Y, Nomura M, Hirata H, Machida Y, Shinoda M, Suzuki N, Matsuoka H (2008) Cardioprotective mechanism of telmisartan via PPAR-γ-eNOS pathway in Dahl salt-sensitive hypertensive rats. Am J Hypertens 21:576–581
Lee HY, Park JB (2015) The Korean Society of Hypertension Guidelines for the Management of Hypertension in 2013: its essentials and key points. Pulse (Basel) 3:21–28
Lee JJ, Shin CY, Park HJ, Zhang WY, Kim Y, Kim IS, Lee KH, Myung CS (2010) Drug synergism of antihypertensive action in combination of telmisartan with lercanidipine in spontaneous hypertensive rats. Arch Pharm Res 33:1411–1418
Loga-Zec S, Asceric M, Loga-Andrijic N, Kapetanovic B, Zerem E (2014) The incidence of antihypertensive drug-induced side effects in patients with diabetes mellitus type 2 and hypertension. Med Arch 68:372–375
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2014) 2013 ESH/ESC guidelines for the management of arterial hypertension. The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (EGC). J Hypertens 31:1281–1357
Maor E, Ivorra A, Leor J, Rubinsky B (2008) Irreversible electroporation attenuates neointimal formation after angioplasty. IEEE Trans Biomed Eng 55:2268–2274
Martin-Timon I, Sevillano-Collantes C, Segura-Galindo A, del Canizo-Gomez FJ (2014) Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes 5:444–470
McBride CA, Hale SA, Subramanian M, Badger GJ, Bernstein IM (2014) The relationship of a family history for hypertension, myocardial infarction, or stroke with cardiovascular physiology in young women. Reprod Sci 21:509–516
Mead TJ, Lefebvre V (2014) Proliferation assays (BrdU and EdU) on skeletal tissue sections. Methods Mol Biol 1130:233–243
Menard J, Campbell DJ, Azizi M, Gonzales MF (1997) Synergistic effects of ACE inhibition and Ang II Antagonism on blood pressure, cardiac weight, and renin in spontaneously hypertensive rats. Circulation 96:3072–3078
Nguyen Q, Dominguez J, Nguyen L, Gullapalli N (2010) Hypertension management: an UPDATE. Am Health Drug Benefits 3:47–56
Park HS, Han JH, Jung SH, Jo EJ, Myung CS (2016) The combination of valsartan and ramipril protects against blood vessel injury and lowers blood pressure. J Pharm Invest 46:265–272
Pedrinelli R, Ballo P, Fiorentini C, Denti S, Galderisi M, Ganau A, Germano G, Innelli P, Paini A, Perlini S, Salvetti M, Zaca V (2012) Hypertension and acute myocardial infarction: an overview. J Cardiovasc Med 13:194–202
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 341:709–717
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M (2003) Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 348:1309–1321
Ribeiro-Oliveira A, Nogueira AI, Pereira RM, Boas WW, Dos Santos RA, Simoes e Silva AC (2008) The renin-angiotensin system and diabetes: An update. Vasc Health Risk Manag 4:787–803
Shin CY, Choi WS, Yi I, Nan MH, Myung CS (2009) Synergistic decrease in blood pressure by captopril combined with losartan in spontaneous hypertensive rats. Arch Pharm Res 32:955–962
Suzuki H, Kanno Y (2005) Effects of candesartan on cardiovascular outcomes in Japanese hypertensive patients. Hypertens Res 28:307–314
Tuncer I, Ozbek H, Ugras S, Bayram I (2003) Anti-fibrogenic effects of captopril and candesartan cilexetil on the hepatic fibrosis development in rat. The effect of AT1-R blocker on the hepatic fibrosis. Exp Toxicol Pathol 55:159–166
Wei GS, Coady SA, Goff DC Jr, Brancati FL, Levy D, Selvin E, Vasan RS, Fox CS (2011) Blood pressure and the risk of developing diabetes in African Americans and Whites: ARIC, CARDIA, and the Framingham Heart Study. Diabetes Care 34:873–879
Yi I, Lee JJ, Park JS, Zhang WY, Kim IS, Kim Y, Shin CY, Kim HS, Myung CS (2010) Enhanced effect of losartan and rosuvastatin on neointima hyperplasia. Arch Pharm Res 33:593–600
Acknowledgements
None of the authors (D. H. Lee, E. J. Jo, E. J. Ga, J. H. Han, S. H. Jung, H. S. Park, K. S. Heo, or C. S. Myung) has any potential conflicts of interest. The study was supported financially by the research fund of Chungnam National University (2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All experimental procedures were performed in accordance with the Guide for the National Institutes of Health Guide for the Care and Use of Laboratory Animals as approved by Chungnam National University Animal Care and Use Committee.
Rights and permissions
About this article
Cite this article
Lee, DH., Jo, E.J., Ga, EJ. et al. Effects of combination therapy with candesartan and ramipril on hypertension and related complications. Journal of Pharmaceutical Investigation 47, 365–371 (2017). https://doi.org/10.1007/s40005-017-0339-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40005-017-0339-3